Abstract
Background
Nursing interns often faced moral distress in clinical practice, similar to registered nurses, which can lead to compassion fatigue. The roles of moral resilience and professional identity in influencing the psychological well-being of nursing interns are recognized, but the interrelationships among moral distress, moral resilience, professional identity, and compassion fatigue in this group remain unclear.
Objectives
This study aimed to investigate the impact of moral distress on compassion fatigue among nursing interns and to explore the mediating role of moral resilience and professional identity.
Methods
A quantitative cross-sectional study was conducted with 467 nursing interns. Data were collected using Compassion Fatigue Short Scale, Moral Distress Scale-revised, Rushton Moral Resilience Scale, and Professional Identity Scale. Data analyses were performed using SPSS 22.0 and Amos 21.0, adhering to the STROBE statement.
Results
The mean scores for compassion fatigue, moral distress, moral resilience, and professional identity were 35.876, 44.887, 2.578, and 37.610, respectively. Moral distress was positively correlated with compassion fatigue. Structural equation modeling showed that moral resilience and professional identity partially mediated the relationship between moral distress and compassion fatigue (β = 0.448, P < 0.001).
Conclusion
The findings suggest that moral distress directly influences compassion fatigue among nursing interns and also exerts an indirect effect through moral resilience and professional identity. Interventions aimed at enhancing moral resilience and fostering a strong professional identity may help mitigate the adverse effects of moral distress on compassion fatigue among nursing interns.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12912-024-02307-y.
Keywords: Nursing interns, Compassion fatigue, Moral distress, Moral resilience, Professional identity
Introduction
The aging population and the growing prevalence of chronic disease are driving a significant increasing in the need for nursing services. However, with only 3.7 registered nurses per 1,000 people as of 2022, this figure falls short of the World Health Organization’s recommended minimum of 4.45 per 1,000 people, leading to a nursing shortage that negatively affects patient care and healthcare efficiency [1–3]. To address this, healthcare system is significantly hiring more new graduate nurses and utilizing nursing interns [4, 5]. In China, nursing interns, recruited during their final year, undergo an 8-month clinical internship, contributing significantly to hospital operations. However, approximately 13.9% of nursing interns experience compassion fatigue [6, 7], leading many to reconsider pursuing a career in nursing [8].
Compassion fatigue, characterized by emotional and psychological distress from chronic exposure to patient suffering [9, 10], manifests in two domains: secondary traumatic stress (STS) and burnout (BO). Nursing interns, akin to experienced nurses, frequently encounter real-life traumatic scenarios during internships, rendering them highly susceptible to compassion fatigue [8]. Research demonstrates a significant prevalence of compassion fatigue among this population [8, 11, 12]. For instance, a US study reported moderate levels among Doctor of Nursing Practice (DNP) students, while a Turkish study identified a high average score on the Compassion Fatigue Short Scale (CFSS) among nursing interns [11, 12]. In China, an online survey of 2,256 nursing interns revealed that nearly 20% scored above the CFSS threshold for compassion fatigue [8]. The consequences of compassion fatigue on nursing interns include sleep disturbances, increased alcohol consumption, depressive symptoms, intrusive thoughts, and decline in self-reflection. Ultimately, this can lead to burnout, career uncertainties, and a higher likelihood of attrition from the nursing workforce [13, 14]. Given the significant detrimental effects of compassion fatigue on the physical and mental health, as well as career development of nursing interns, a deeper exploration of its causes and mechanisms is imperative.
Moral distress arises when nurses recognize the ethically sound course of action but are unable to act on their convictions due to internal or external constraints [15]. Nursing interns are particularly susceptible to moral distress due to challenges in patient communication, inadequacy or lack of confidence when trying to communicate personal opinions and concerns during interactions with physicians, exposure to inaccurate treatment information, and a sense of isolation inherent to trainee’s roles [16, 17]. Chronic exposure to moral distress can have deleterious consequences for nursing interns, manifesting as anxiety, self-doubt, guilt, and emotional exhaustion, ultimately contributing to compassion fatigue [18]. A robust of research demonstrates a positive correlation between moral distress and compassion fatigue among nurses [19–22]. Maiden et al. identified a positive association between moral distress and compassion fatigue among 205 American critical care nurses [19]. Furthermore, several studies have documented this positive association among clinical nurses in emergency department and department of rheumatological immunology [20–22]. However, a critical gap exists in research regarding the specific influence of moral distress on compassion fatigue among nursing interns.
Moral resilience, the capacity to maintain or restore one’s ethical integrity despite encountering moral complexities, confusion, distress, or setbacks [23], is a critical protective factor for nurses’ mental health and ethical decision-making [24]. Moral resilience is particularly crucial for nursing interns who are more susceptible to compassion fatigue [25]. Some studies support this notion, demonstrating a negative association between moral resilience and compassion fatigue [12, 26].
Professional identity encompasses the nurse’s perception of their professional worth and the ongoing development of their skills within the nursing field [27]. A robust professional identity could serve as a critical source of psychological resilience in the face of ethical and clinical challenges [28]. Research reveals that programs fostering professional identity can significantly reduce job burnout among clinical nurses. Two cross-sectional studies demonstrate an inverse relationship between professional identity and compassion fatigue among nurses and nursing interns [8, 29]. This indicates that a well-developed professional identify may buffer against compassion fatigue experienced by both registered nurses and nursing interns.
Given the high prevalence of compassion fatigue and moral distress among nursing interns, it is essential to explore their causes and mechanisms. While existing literature primarily explores the bivariate relationship between these factors [14], the potential for moral resilience and professional identity to mediate the influence of moral distress on compassion fatigue remains unexamined in nursing interns. This knowledge gap hinders the development of targeted interventions for mitigating compassion fatigue in this vulnerable population [3, 24, 28, 30–33]. Addressing this gap could lead to targeted interventions to support the well-being and professional development of nursing interns. This study aims to investigate five key hypotheses:
H1
Nursing interns’ moral distress is positively correlated with their compassion fatigue.
H2
Nursing interns’ moral distress is negatively correlated with their moral resilience and professional identity.
H3
Nursing interns’ moral resilience is positively correlated with their professional identity.
H4
Nursing interns’ moral resilience and professional identity are negatively correlated with their compassion fatigue.
H5
Moral resilience and professional identity simultaneously mediate the influence of nursing interns’ moral distress on their compassion fatigue.
Methods
Study design
An online quantitative, cross-sectional survey study was conducted and the findings were reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for enhanced scientific rigor [34].
Study setting and sampling
The study employed a convenience sampling method to recruit eligible nursing interns from four public junior colleges in Hunan province, central China, in February, 2024. Participants were eligible if they had completed at least two years of nursing education. and participated in clinical internships for 8 months at a second-level or higher hospital. The professional requirements include basic nursing skills, knowledge of patient care protocols, and adherence to ethical standards. All participants provided informed consent and participated voluntarily. Nursing interns whose clinical practice positions solely involved clerical or administration duties without direct patient contact, were excluded.
Sample size
This study used structural equation modeling (SEM) technique with maximum likelihood estimation to examine the relationships between the designed variables. The sample size was determined using the N: q rule with a ratio of 10:1, where N represents the minimum required number of cases and q denotes the number of parameters requiring estimation [35]. Based on this approach, the q of 28 yielded a theoretical minimum sample of 339. To account for potential invalid response, we aimed to recruit a sample 20% larger. However, to enhance the representativeness and minimize sampling bias, we actively recruited nursing students participating in internships across public junior colleges. This recruitment strategy resulted in a final sample of 544 nursing interns.
Data collection
The data for this study were collected using Wenjuanxing (https://www.wjx.cn), a widely recognized online survey platform in China, known for its reliability and user-friendliness in research applications. This platform was selected due to its ability to securely host surveys and its accessibility to participants. To facilitate easy access, a Quick Response (QR) code was generated and shared via WeChat, a widely used mobile app in China. The principal investigator established collaborative relationships with full-time student counselors responsible for managing nursing interns at four public junior colleges in Hunan province. These counselors were provided with the survey link and were responsible for disseminating it to the nursing interns. Before participating, the nursing interns received comprehensive information about the study, including its purpose, significance, and procedures. This information was communicated both verbally by the counselors and in writing through an introductory page on the Wenjuanxing platform. The introduction emphasized the voluntary nature of participation, ensured confidentiality, and estimated the survey completion time to be between 10 and 15 min. Upon accessing the survey via the QR code or direct link, participants were required to read and agree to an informed consent statement before proceeding. The survey was designed to guide participants smoothly through each section, with all questions designated as mandatory to ensure thorough data collection. A pilot study was conducted on the Wenjuanxing platform with a small group of nursing interns to identify and address any potential technical issues or ambiguities in the questions. Based on the feedback, minor adjustments were made to enhance the clarity and user experience of the survey.
To maintain data integrity, several quality control measures were implemented. Responses completed in less than 8 min were flagged as potentially rushed and excluded from the final analysis. Additionally, responses exhibiting signs of inattention, such as uniformity in answers, regular patterns, or logical inconsistencies, were also excluded. These measures ensured that the data collected were both reliable and valid. After applying these quality control measures, the final sample consisted of 467 participants, resulting in an effective response rate of 85.9%.
Instruments
Demographic characteristics
A self-designed demographic characteristics questionnaire was used to collect data on participants’ gender, age, academic discipline (major), motivations for choosing their major, level of the internship hospital, prior exposure to ethics courses, receipt of ethics training during internship, degree of fondness for their major, employment intentions and self-reported health status over the past month.
Compassion fatigue short scale
The Chinese version of the CFSS was utilized to measure nursing interns’ CF in the present study, Which was originally developed and validated by Adams et al. [36]. The Chinese version of CFSS was developed by Sun et al. [37]. , consisting of 13 items with 2 subscales: BO subscale (items 1, 2, 4, 6, 7, 9, 11, and 13) and STS subscale (items 3, 5, 8,10, and12). The Cronbach’s α coefficient for the total scale was satisfactory, with a value of 0.90. Similarly, the BO subscale had a coefficient of 0.90, while the α coefficient of the STS subscale was 0.80. Each item is scored on a Likert scale ranging from “never” (1) to “always” (10), resulting in a total score range of 13–130. Higher scores indicate higher severity of CF. In this study, the Cronbach’s α values for the total scale was 0.925, with 0.894 and 0.897 for BO and STS, respectively.
Moral Distress Scale-revised
The Moral Distress Scale (MDS), a valid tool for assessing moral distress intensity and frequency, was employed in this study. The MDS-R, originally developed by Corley et al. and subsequently revised by Hamric et al. to a 21-item version [38, 39]. The Chinese adaptation of the Moral Distress Scale-revised (MDS-R) was translated and modified by Sun et al., resulting in a final version consisting of 22 items categorized into individual responsibility, not in the patient’s best interest, value conflict, and harming patient’s interest [40]. The Chinese version of MDS-R demonstrates high reliability and validity, with a Cronbach’s α coefficient of 0.894 for the total scale. MDS-R employs a 4-point Likert scale to assess the current intensity of moral distress (0 = none, 4 = great extent) and its frequency (0 = never occurs, 4 = very frequently). Each item score is calculated by multiplying the intensity and frequency scores, resulting in a range of 0 to 16. These individual scores are then summed up to generate a total score between 0 and 336, with higher scores indicating greater moral distress. In this study, the total scale exhibited excellent internal consistency, as evidenced by a Cronbach’s α coefficient of 0.966.
Rushton Moral Resilience Scale
The Rushton Moral Resilience Scale (RMRS), developed by Heinze et al., demonstrates a internal consistency, with a Cronbach’s α coefficient of 0.843. The original version consists of 17 items categorized into 4 subscales: response to moral adversity, personal integrity, relational integrity, and moral efficacy [41]. Tian et al. adapted the RMRS for the Chinese nurses, resulting in a 17-items version with 3 subscales: the ability to flexibly cope with adversity (items 2, 4, 5, 6, and 8), relational moral soundness (items 10, 11, 13, 14, 15, and 16), and moral efficacy (items1, 3, 7, 9, 12, and 17) [42]. The Chinese version maintains satisfactory reliability, with a Cronbach’s α of 0.811. Item are rated on a 4-point Likert scale ranging from “disagreement” (1) to “complete agreement” (4), with 11 items reverse-scored for accurate interpretation of the total score, including item 2, 4, 5, 6, 8, 10, 11, 13, 14, 15, and 16. The total score for this scale is calculated as the mean value of all items, where higher scores indicate greater moral resilience. In this study, the total scale achieved a Cronbach’s α coefficient of 0.802.
Professional Identity Scale
The present study employed the Chinese version of the Professional Identity Scale (PIS) to assess nursing interns’ professional identity. This scale was originally developed and validated by Brown et al., and subsequently adapted for the Chinese population by Lu et al. [43, 44]. The PIS consists of a single dimension with 10 items, where 5 items (items 1, 4, 5, 8, 9) are scored in a positive direction and the remaining 5 items (items 2, 3, 6, 7 ,10) are scored in a reverse direction. Each item is rated on a 5-point Likert scale ranging from “never” (1) to “always” (5), resulting in a total score range of 10–50. A higher score indicates stronger PI. The original scale demonstrated good internal consistency with a Cronbach’s α coefficient of 0.71; similarly, the Chinese version exhibited satisfactory reliability with a Cronbach’s α coefficient of 0.82. In this study, the Cronbach’s α coefficient for the scale was found to be 0.816.
Statistical analysis
Descriptive statistics were calculated using the IBM SPSS version 22.0 (Chicago, Illinois, USA). Categorical variables were represented as frequencies and percentages, while continuous variables were described using mean and standard deviation (SD). Given the adequate sample size, Pearson correlation analysis was employed to investigate the relationships between moral distress, moral resilience, professional identity, and compassion fatigue [45]. A mediation model was then constructed and analyzed using AMOS version 21.0 (Chicago, IL, United States). This analysis utilized 5,000 bootstrap samples with a focus on bias-corrected and accelerated confidence interval (CI). Model fit was assessed using established metrics including chi-square/degree of freedom (χ2/df) < 5, comparative fit index (CFI) > 0.90, Tucker-Lewis index (TLI) > 0.90, and root mean square error of approximation (RMSEA) < 0.08 [46]. A two-tailed p-value of less than 0.05 indicates statistical significance.
Results
Participant characteristics
Table 1 presents the demographic and professional characteristics of 467 participants. The average age of the nursing interns was 20.31 years, with female students constituting 90.6% (423/467) of the participants, and nearly all participants (97.9%, 457/467) majored in the nursing specialty. Approximately half of the participants (53.7%, 251/467) reported that their choice of nursing as a major was influenced by friends and family, and a same proportion expressed a positive or very positive attitude towards their future career working in nursing field. The majority of participants (88.7%, 414/467) completed their internships in tertiary hospitals. In addition, a significant majority (92.5%, 432/467) reported receiving nursing ethics education in their curriculum, while 366 students underwent ethics-related training during their internships. A total of 61.9% participants (289/467) perceived their health status over the past month as good, and 72.2% (337/467) expressed employment intentions to work in the nursing field.
Table 1.
The characteristics of the participants (n = 467)
| Characteristics | Frequency (%) | Mean ± SD | ||
|---|---|---|---|---|
| Age (years) | 20.31 ± 0.820 | |||
| Gender | Female | 423 (90.6) | ||
| Male | 44 (9.4) | |||
| Major | Nursing | 457 (97.9) | ||
| Midwife | 10 (2.1) | |||
| Reasons of choosing their major upon admission | Voluntary | 198 (42.4) | ||
| Influenced by friends and family | 251 (53.7) | |||
| Adjustment | 18 (3.9) | |||
| Hospital level | Tertiary hospital | 414 (88.7) | ||
| Secondary hospital | 53 (11.3) | |||
| Inclusion of ethics courses in their college curriculum | Nursing Ethics | 432 (92.5) | ||
| Medical Ethics | 14 (3.0) | |||
| Covered in other courses or not studied | 21 (4.5) | |||
| Receipt of ethics training during internship | Yes | 366 (78.4) | ||
| No | 101 (21.6) | |||
| Degree of fondness for their major | Extremely fond | 36 (7.7) | ||
| Fond | 215 (46.0) | |||
| Indifferent | 183 (39.2) | |||
| Dislike | 28 (6.0) | |||
| Strongly dislike | 5 (1.1) | |||
| Employment intentions | Working in the nursing field | 337 (72.2) | ||
| Working in other fields | 49 (10.5) | |||
| Continue to study | 81 (17.3) | |||
| Health status in the past month | Good | 289 (61.9) | ||
| Average | 146 (31.3) | |||
| Poor | 32 (6.9) | |||
Scores of variables measured in this study
Table 2 detailed the scores of participants across various scales. The overall mean score for compassion fatigue was 35.876 ± 19.103, subdivided into BO with a mean score of 24.281 ± 12.908 and STS with a mean score of 11.595 ± 7.944. The overall average score for professional identity was 37.610 ± 6.287. In terms of moral resilience, the overall mean score was 2.578 ± 0.294, with the subscales of flexible response to moral adversity, relational moral soundness, and moral efficacy scoring 2.343 ± 0.614, 2.378 ± 0.575, and 17.801 ± 2.916, respectively. Moreover, the overall mean score for moral distress was 44.887 ± 38.730, with the subscales of individual responsibility, not in the patient’s best interest, values conflicts, and harm to the patient’s interest scoring 14.355 ± 14.282, 10.647 ± 9.325, 13.274 ± 11.414, and 6.610 ± 6.278, respectively.
Table 2.
Correlations for variables measured in this study (n = 467)
| Variables | Mean (SD) | a | b | c | d | e | f | g | h | i | j | k | l | m |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| a. PI | 37.610 (6.287) | 1 | ||||||||||||
| b. CF | 35.876 (19.103) | -0.527** | 1 | |||||||||||
| c. BO | 24.281 (12.908) | -0.569** | 0.950** | 1 | ||||||||||
| d. STS | 11.595 (7.944) | -0.342** | 0.861** | 0.659** | 1 | |||||||||
| e. MD | 44.887 (38.730) | -0.269** | 0.434** | 0.389** | 0.410** | 1 | ||||||||
| f. MD1 | 14.355 (14.282) | -0.299** | 0.439** | 0.397** | 0.410** | 0.946** | 1 | |||||||
| g. MD2 | 10.647 (9.325) | -0.209** | 0.376** | 0.337** | 0.358** | 0.952** | 0.849** | |||||||
| h. MD3 | 13.274 (11.414) | -0.211** | 0.377** | 0.319** | 0.388** | 0.944** | 0.829** | |||||||
| i. MD4 | 6.610 (6.278) | -0.288** | 0.432** | 0.418** | 0.361** | 0.886** | 0.794** | |||||||
| j. MR | 2.578 (0.294) | 0.295** | -0.361** | -0.349** | -0.302** | -0.343** | -0.343** | 0.012 | 0.058 | 0.051 | 1 | |||
| k. MR1 | 2.343 (0.614) | 0.133** | -0.246** | -0.235** | -0.208** | -0.238** | -0.208** | -0.241** | -0.223** | -0.222** | 0.763** | 1 | ||
| l. MR2 | 2.378 (0.575) | 0.146** | -0.210** | -0.196** | -0.187** | -0.257** | -0.253** | -0.183** | -0.158** | -0.176** | 0.834** | 0.657** | 1 | |
| m. MR3 | 17.801 (2.916) | 0.205** | -0.129** | -0.130** | -0.100* | -0.031 | -0.066 | 0.478** | 0.506** | 0.506** | -0.059 | -0.506** | -0.430** | 1 |
Note: PI: professional identity; CF: compassion fatigue; BO: burnout; STS: secondary traumatic stress; MD: moral distress; MD1: individual responsibility; MD2: not in patient’s best interest; MD3: values conflicts; MD4: harm to patient’s interest; MR: moral resilience; MR1: the ability to respond flexibly to moral adversity; MR2: relational moral soundness; MR3: moral efficacy. *Statistical significance at the level of 0.05 (two-tailed), **Statistical significance at the level of 0.01 (two-tailed)
Correlations for variables
Pearson correlation analysis revealed that higher level of moral distress was correlated to lower professional identify (r = − 0.269, P < 0.01) and moral resilience (r = − 0.343, P < 0.01) among nursing interns. Conversely, moral distress has a positive association with compassion fatigue (r = 0.434, P < 0.01). Additionally, a strong negative correlation was also found between professional identity and compassion fatigue (r = -0.527, P < 0.01). A detailed breakdown of all correlations is presented in Table 2.
The effect of moral distress on compassion fatigue
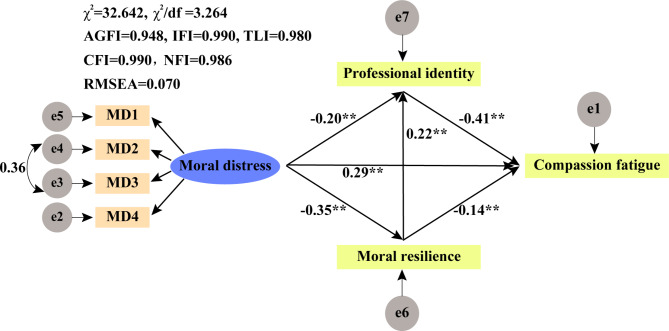
The results from the SEM were presented in Table 3; Fig. 1. The model fit indices showed an acceptable level of congruence between the hypothesized model and the observed data. Specifically, χ2/df was 3.264, indicating a good fit. Additionally, CFI of 0.990, TLI of 0.980, RMSEA of 0.070 [90% CI, 0.044–0.097]) further supported a satisfactory model fit. The SEM results revealed significant direct relationship within the cohort of nursing interns. Moral distress exerted a negative influence on moral resilience (β = -0.351, P < 0.001), professional identity (β = -0.199, P < 0.001), and compassion fatigue (β = 0.285, P < 0.001). Conversely, moral resilience positively impacted on professional identity (β = 0.225, P < 0.001) and negatively affected compassion fatigue (β = -0.141, P < 0.001). Similarly, professional identity exhibited a significant negative association with compassion fatigue (β = -0.405, P < 0.001). Further analysis using the bias-corrected bootstrap procedure demonstrated statistically indirect pathways from moral distress to compassion fatigue. These pathways functioned through moral resilience (β = 0.050, P < 0.001) and professional identity (β = 0.081, P < 0.001) independently, as well as concurrently through both factors (β = 0.032, P < 0.001) t. The specific results for these indirect pathways are summarized in Table 4.
Table 3.
Decomposition of standardized effects from the path model
| Variable of effect | Moral distress | Moral resilience | Professional identity | ||||
|---|---|---|---|---|---|---|---|
| Moral resilience | Professional identity | Compassion fatigue |
Professional identity |
Compassion fatigue |
Compassion fatigue |
||
| Total effects | -0.351 | -0.278 | 0.448 | 0.225 | -0.232 | -0.405 | |
| Direct effects | -0.351 | -0.199 | 0.286 | 0.225 | -0.141 | -0.405 | |
| Indirect effects | 0.000 | -0.079 | 0.162 | 0.000 | -0.091 | 0.000 | |
Fig. 1.
A path diagram of direct and indirect influences of moral distress, moral resilience and professional identity on compassion fatigue among Chinese nursing interns (n = 467). **P < 0.01
Table 4.
Bias‑corrected bootstrap test for all indirect pathways
| Pathway | Estimate | Standard errors | Bootstrap confidence | P |
|---|---|---|---|---|
| Moral distress → Moral resilience → Compassion fatigue | 0.081 | 0.021 | 0.042–0.124 | 0.001 |
| Moral distress → Professional identity → Compassion fatigue | 0.05 | 0.015 | 0.021–0.081 | 0.001 |
| Moral distress → Moral resilience → Professional identity → Compassion fatigue | 0.032 | 0.008 | 0.019–0.049 | 0.001 |
| Total indirect effects | 0.162 | 0.024 | 0.116–0.211 | 0.001 |
| Total direct effects | 0.286 | 0.041 | 0.205–0.369 | 0.001 |
| Total effects | 0.448 | 0.043 | 0.366–0.534 | 0.001 |
Discussion
Main findings
The present study stemmed from a fact that the mechanism by which moral distress influences compassion fatigue among nursing interns remains unclear. The findings of the present study revealed 4 significant outcomes: (1) moral distress is positively correlated with compassion fatigue but negatively correlated with moral resilience and professional identity, (2) moral resilience is positively correlated with professional identity, while negatively correlated with compassion fatigue, (3) professional identity is negatively associated with compassion fatigue, and (4) moral resilience and professional identity play a mediating role in the relationship between moral distress and compassion fatigue.
The current study unveiled a direct positive relationship between moral distress and compassion fatigue among nursing interns (confirming hypothesis 1). Nursing is a profession that requires the ability to manage substantial stress, while also maintaining a compassionate and empathetic approach to patient care. When nursing interns encounter moral distress during internships, they are forced to grapple with complex ethical questions that can evoke strong emotions such as anxiety, guilt, helplessness, and hopelessness [47–49]. This emotional stress can accumulate over time, leading to compassion fatigue [17]. The findings align with previous researches investigating the relationship between moral distress and compassion fatigue among nurses [17, 19]. However, one study reported no significant association between moral distress and compassion fatigue among nurses working in the surgical intensive care unit, which might result from the limited sample size (26 participants), different study participants and work environments [50].
Our study also revealed that nursing interns’ moral distress had a negative relationship with their moral resilience (confirming hypothesis 2), which was consistent with Berdida et al. exploring the relationships between moral distress and moral resilience among 412 Philippine nurses [32]. When facing high level of moral distress, individuals may experience intense negative emotions, which can deplete individual psychological resources and reduce moral resilience in coping with stress [51]. Moreover, constant exposure to morally challenging situations can leave individuals feeling hopeless and questioning the point of striving for ethical behavior. This can make it difficult to find meaning in work and decrease overall moral resilience [18, 32, 52].
Moral resilience has emerged as a promising resource for promoting mental well-being and navigating ethical conflicts. A great deal of studies has established the importance of incorporating moral resilience-building strategies into ethical education and psychosocial interventions, particularly for nurses and nursing interns [53–55]. In current study, we found a direct negative correlation between moral resilience and compassion fatigue among nursing interns (confirming hypothesis 4). While it is intuitively understood that lower levels of moral resilience may lead to the increase in the level of compassion fatigue among nursing interns. This finding resonates with previous studies that has emphasized the role of moral resilience in mitigating the adverse psychological effects of ethical challenges in healthcare settings [25, 26]. Individuals with high moral resilience are typically better able to regulate their emotions [23]. When confronted with the suffering of others, they can effectively modulate their emotional responses, preventing excessive emotional involvement and thus mitigating compassion fatigue. They understand how to maintain compassion while also preserving their emotional resources. Meanwhile, moral resilience enables individuals to reappraise stressful situations in a more positive and constructive light. When faced with the hardships of others, they are more likely to view them as challenges to be overcome, rather than constant sources of negative emotions. This cognitive shift helps to reduce the psychological toll of compassion fatigue [12]. For above results, it could be inferred that moral distress can indirectly contribute to negative effects on compassion fatigue through moral resilience (confirming hypothesis 5).
We also found there was a negative correlation between professional identity and compassion fatigue (confirming hypothesis 4), which was consistent with previous studies [8, 29]. Professional identity acts as a protective factor against compassion fatigue and a strong professional identity can buffer the emotional impact resulting from caring patients [27]. When individuals have a clear sense of their purpose and values within their profession, they are more likely to view challenging situations as part of their role and responsibility, rather than as personally draining or overwhelming. Otherwise, moral distress had a negative relationship with professional identity (confirming hypothesis 2). One study which was performed to investigate the influencing factors on professional identity in intensive care nurses also consistently indicated that moral distress is one of the most important factors [56]. But another study only revealed a very low negative relationship and the inconsistent result could potentially be explained by the nature of the surveyed population [57]. The study primarily targeted nurses employed in general hospitals, rather than those specifically working in high-intensity environments like emergency departments or intensive care units (ICUs). Given this, nurses working in general departments within general hospitals may encounter significantly less severe ethical distress in comparison to their colleagues in ICUs or emergency departments. Moral distress can erode professional identity and sense of purpose. When nursing interns face moral distress that require them to compromise their values or principles, they may feel a sense of loss of meaning and purpose in their work. This erosion of professional identity can lead to feelings of helplessness and hopelessness, which in turn contribute to compassion fatigue [8]. Hence, our study further revealed professional identity played a mediating role between moral distress and compassion fatigue (confirming hypothesis 5).
Moral resilience is found to have a positive relationship with professional identity (confirming hypothesis 3). This relationship is consistent with existing literature, although the strength of the association varies across studies. One study reported a low positive correlation between professional identity and moral resilience among nursing students, as determined by a Pearson correlation test, suggesting that while the relationship exists, it may not be particularly strong in certain contexts [33]. In contrast, another study involving practicing nurses found a moderate positive correlation, indicating that as nurses gain professional experience, the relationship between moral resilience and professional identity may strengthen [58]. These findings suggest that the development of professional identity and moral resilience could be influenced by the transition from education to professional practice. In our study, the findings go further by revealing that moral resilience and professional identity play a chain-mediating role between moral distress and compassion fatigue (confirming hypothesis 5). This suggests that not only are moral resilience and professional identity interconnected, but they also collectively influence how nursing interns experience and cope with the emotional and ethical challenges of their work. The chain-mediating effect underscores the importance of fostering both moral resilience and a strong professional identity in nursing education and practice to mitigate the negative impacts of moral distress and reduce the risk of compassion fatigue. These findings contribute to a deeper understanding of the mechanisms through which moral resilience and professional identity interact and influence the well-being of nursing professionals.
Limitations
This study provides valuable insights, but some limitations warrant consideration. First, the cross-sectional design limits the ability to infer causality between the investigated variables. Longitudinal studies are necessary to elucidate how moral distress might mitigate the negative effects of compassion fatigue. Second, the study employed a convenience sampling method, recruiting nursing interns from four public junior colleges in Hunan province. While this approach facilitated data collection, it may have introduced sampling bias, limiting the generalizability of the findings. Future studies should consider random sampling techniques to enhance the representativeness of the sample. Despite this limitation, the study provides valuable insights into the factors influencing compassion fatigue among nursing interns Third, self-reported questionnaires were employed to measure key constructs. This approach introduces the potential for subjective biases from both participants and investigators, potentially inflating the results. Further studies incorporating physiological assessments and ecological momentary assessments are recommended to strengthen the objectivity of data.
Conclusions
This study contributes to understanding of the complex interplay between moral distress and its downstream effects on nursing interns. Our findings demonstrate a positive association between moral distress and compassion fatigue, suggesting that experiencing ethical dilemmas can lead to emotional exhaustion. Conversely, moral resilience and a strong professional identity emerged as protective factors, exhibiting negative correlations with compassion fatigue. Furthermore, the data support a mediating role for both moral resilience and professional identity, indicating that buffer the detrimental effects of moral distress on well-being of nursing interns.
Implications for practice
This study contributes to the growing body of knowledge concerning the association between moral distress, compassion fatigue, and the mediation roles of moral resilience and professional identity among nursing interns. Our findings highlight several practical implications at both organizational and managerial levels.
At the organizational level, healthcare institutions should consider integrating interventions that foster moral resilience into their broader workforce development strategies. This could involve the creation and implementation of comprehensive training programs that include emotional regulation techniques, cognitive reappraisal skills, and the development of robust social support systems. Organizations might also benefit from embedding regular workshops and mentorship programs that focus on ethical decision-making and emotional well-being into their training for nursing interns. These programs should be systematically incorporated into the organizational culture to ensure consistent support for all nursing interns as they navigate complex situations.
Moreover, organizational policies should be designed to promote a work environment where ethical concerns are not only acknowledged but actively addressed. This could include establishing clear channels for open communication and creating a non-punitive environment where nursing interns feel safe to voice their ethical concerns. Institutions might also implement policies that mandate the availability of mental health resources specifically tailored to the needs of nursing interns.
At the managerial level, nursing managers have a crucial role in fostering a supportive culture that prioritizes moral resilience and professional identity. Managers should be trained to recognized the early signs of moral distress and compassion fatigue among their teams. By doing so, they can intervene promptly with appropriate support and resources. Additionally, managers should actively promote and model ethical behavior, encourage reflective practice, and facilitate access to professional support networks. This proactive managerial approach can help nursing interns develop the resilience and professional identity needed to manage ethically challenging situations effectively.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors also gratefully acknowledge the teaching counselors of the colleges and the 467 nursing interns who volunteered to participate in the study, as well as the experts and members of the group for their help and advice.
Author contributions
TS: Conceptualization, data curation, formal analysis, methodology, writing & original draft; YX: Methodology, project administration, software; MFJ: formal analysis, methodology; LJY: Conceptualization, methodology, supervision, writing & review & editing; XT: Conceptualization, methodology, supervision, Writing & review & editing. All authors read and approved the final manuscript.
Funding
The research was partially supported by the Start-up Funding of Chongqing Traditional Chinese Medicine Hospital for the Full-time Postdoctoral Fellow.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due to the participant confidentiality, but are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The present study was approved by the Ethics Committee of the Hunan Traditional Chinese Medical College Medical Ethics Committee, located in Hunan Province, China (YXLL202401004). The survey was conducted anonymously, which fully protected the privacy of the respondents. All data were available only to the research team and were used for the purposes of this study only. All participants provided informed consent and participated voluntarily.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Ting Shuai and Yan Xuan contributed equally to this work.
Contributor Information
Lijuan Yi, Email: lijuan.yi@estudiants.urv.cat.
Xu Tian, Email: xu.tian@alumni.urv.cat.
References
- 1.National Health Commission of the People’s Republic of China[EB/. OL] 2023-05-11 [http://en.nhc.gov.cn/ [DOI] [PMC free article] [PubMed]
- 2.World Health Organization (WHO). Global strategy on human resources for health: health workforce 2030[EB/OL] 2016-5-31 [https://www.who.int/news/item/02-06-2022-global-strategy-on-human-resources-for-health--workforce-2030
- 3.Peng M, Saito S, Guan H, Ma X. Moral distress, moral courage, and career identity among nurses: a cross-sectional study. Nurs Ethics. 2023;30(3):358–69. 10.1177/09697330221140512 [DOI] [PubMed] [Google Scholar]
- 4.Zeng L, Chen Q, Fan S, Yi Q, An W, Liu H, et al. Factors influencing the professional identity of nursing interns: a cross-sectional study. BMC Nurs. 2022;21(1):200. 10.1186/s12912-022-00983-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jantara RD, Barlem JGT, Jantara A, Rocha LP, Rocha SSD, Stigger D. Analysis of moral courage and related factors among undergraduate nursing students: a scoping review. Rev Bras Enferm. 2023;76Suppl(3):e20220225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kachie ADT, Zhou L, Quansah PE, Xu X, Epalle TM, Ngajie BN. Role demands and turnover intention among Covid-19 frontline nurses: the mediating and moderating roles of compassion fatigue and spiritual leadership. PLoS ONE. 2023;18(8):e0289888. 10.1371/journal.pone.0289888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cao X, Chen L. Relationships between resilience, empathy, compassion fatigue, work engagement and turnover intention in haemodialysis nurses: a cross-sectional study. J Nurs Manag. 2021;29(5):1054–63. 10.1111/jonm.13243 [DOI] [PubMed] [Google Scholar]
- 8.Yi LJ, Cai J, Ma L, Lin H, Yang J, Tian X, Jiménez-Herrera MF. Prevalence of compassion fatigue and its association with professional identity in junior college nursing interns: a cross-sectional study. Int J Environ Res Public Health. 2022;19(22). [DOI] [PMC free article] [PubMed]
- 9.Marshman C, Hansen A, Munro I. Compassion fatigue in mental health nurses: a systematic review. J Psychiatr Ment Health Nurs. 2022;29(4):529–43. 10.1111/jpm.12812 [DOI] [PubMed] [Google Scholar]
- 10.Xie W, Chen L, Feng F, Okoli CTC, Tang P, Zeng L, et al. The prevalence of compassion satisfaction and compassion fatigue among nurses: a systematic review and meta-analysis. Int J Nurs Stud. 2021;120:103973. 10.1016/j.ijnurstu.2021.103973 [DOI] [PubMed] [Google Scholar]
- 11.Bouchard L, Rainbow J. Compassion fatigue, presenteeism, adverse childhood experiences (ACES), and resiliency levels of doctor of nursing practice (DNP) students. Nurse Educ Today. 2021;100:104852. 10.1016/j.nedt.2021.104852 [DOI] [PubMed] [Google Scholar]
- 12.Karabey T. Compassion fatigue and psychological resilience levels of nursing final students: a descriptive, cross-sectional, and relational study. Palliat Support Care. 2023:1–7. [DOI] [PubMed]
- 13.Bayuo J, Agbenorku P. Compassion fatigue in the burn unit: a review of quantitative evidence. J Burn Care Res. 2022;43(4):957–64. 10.1093/jbcr/irab237 [DOI] [PubMed] [Google Scholar]
- 14.Cavanagh N, Cockett G, Heinrich C, Doig L, Fiest K, Guichon JR, et al. Compassion fatigue in healthcare providers: a systematic review and meta-analysis. Nurs Ethics. 2020;27(3):639–65. 10.1177/0969733019889400 [DOI] [PubMed] [Google Scholar]
- 15.Krautscheid L, DeMeester DA, Orton V, Smith A, Livingston C, McLennon SM. Moral distress and associated factors among baccalaureate nursing students: a multisite descriptive study. Nurs Educ Perspect. 2017;38(6):313–9. 10.1097/01.NEP.0000000000000214 [DOI] [PubMed] [Google Scholar]
- 16.Sasso L, Bagnasco A, Bianchi M, Bressan V, Carnevale F. Moral distress in undergraduate nursing students: a systematic review. Nurs Ethics. 2016;23(5):523–34. 10.1177/0969733015574926 [DOI] [PubMed] [Google Scholar]
- 17.Eche IJ, Phillips CS, Alcindor N, Mazzola E. A systematic review and meta-analytic evaluation of moral distress in oncology nursing. Cancer Nurs. 2023;46(2):128–42. 10.1097/NCC.0000000000001075 [DOI] [PubMed] [Google Scholar]
- 18.Lamoureux S, Mitchell AE, Forster EM. Moral distress among acute mental health nurses: a systematic review. Nurs Ethics. 2024:9697330241238337. [DOI] [PMC free article] [PubMed]
- 19.Maiden J, Georges JM, Connelly CD. Moral distress, compassion fatigue, and perceptions about medication errors in certified critical care nurses. Dimens Crit Care Nurs. 2011;30(6):339–45. 10.1097/DCC.0b013e31822fab2a [DOI] [PubMed] [Google Scholar]
- 20.Liao DJ, Zhang XX, Yan LL. Investigation on status of nurses’ compassion fatigue in emergency department and analysis of influencing factors. Hosp Manage Forum. 2019;36(03):47–50. [Google Scholar]
- 21.Gao CR, Yang WY, Li H. Mediating effect of achievement motivation strategy on compassion fatigue and moral distress of nurses in department of rheumatological immunology. Occup Health. 2019;35(10):1361–4. [Google Scholar]
- 22.Liu Y, Wang Y, Sha LY. Analysis of the mediating effect of moral dilemma between workplace violence and empathy fatigue of clinical nurses. Chin J Nurs Educ. 2023;20(07).
- 23.Young PD, Rushton CH. A concept analysis of moral resilience. Nurs Outlook. 2017;65(5):579–87. 10.1016/j.outlook.2017.03.009 [DOI] [PubMed] [Google Scholar]
- 24.Faraco MM, Gelbcke FL, Brehmer LCF, Ramos FRS, Schneider DG, Silveira LR. Moral distress and moral resilience of nurse managers. Nurs Ethics. 2022;29(5):1253–65. 10.1177/09697330221085770 [DOI] [PubMed] [Google Scholar]
- 25.Zhang J, Wang X, Xu T, Li J, Li H, Wu Y, et al. The effect of resilience and self-efficacy on nurses’ compassion fatigue: a cross-sectional study. J Adv Nurs. 2022;78(7):2030–41. 10.1111/jan.15113 [DOI] [PubMed] [Google Scholar]
- 26.Chen X, Zhang Y, Zheng R, Hong W, Zhang J. Latent profiles of nurses’ moral resilience and compassion fatigue. Nurs Ethics. 2023:9697330231222594. [DOI] [PubMed]
- 27.Fitzgerald A. Professional identity: a concept analysis. Nurs Forum. 2020;55(3):447–72. 10.1111/nuf.12450 [DOI] [PubMed] [Google Scholar]
- 28.Kim M, Oh Y, Lee JY, Lee E. Job satisfaction and moral distress of nurses working as physician assistants: focusing on moderating role of moral distress in effects of professional identity and work environment on job satisfaction. BMC Nurs. 2023;22(1):267. 10.1186/s12912-023-01427-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang Y, Peng Q, Dong W, Hou C, Chen C. Professional identity and sense of coherence affect the between compassion fatigue and work engagement among Chinese hospital nurses. BMC Nurs. 2023;22(1):472. 10.1186/s12912-023-01596-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gibson E, Duke G, Alfred D. Exploring the relationships among moral distress, moral courage, and moral resilience in undergraduate nursing students. J Nurs Educ. 2020;59(7):392–5. 10.3928/01484834-20200617-07 [DOI] [PubMed] [Google Scholar]
- 31.Talebian F, Hosseinnataj A, Yaghoubi T. The relationship between resilience and moral distress among Iranian critical care nurses: a cross-sectional correlational study. Ethiop J Health Sci. 2022;32(2):405–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Berdida DJE. The mediating roles of moral courage and moral resilience between nurses’ moral distress and moral injury: an online cross-sectional study. Nurse Educ Pract. 2023;71:103730. 10.1016/j.nepr.2023.103730 [DOI] [PubMed] [Google Scholar]
- 33.Jafarianamiri SR, Qalehsari MQ, Zabihi A. Investigating the professional identity and resilience in nursing students during the COVID-19 pandemic. J Educ Health Promot. 2022;11:151. 10.4103/jehp.jehp_388_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335(7624):806–8. 10.1136/bmj.39335.541782.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McDonald RP, Ho MH. Principles and practice in reporting structural equation analyses. Psychol Methods. 2002;7(1):64–82. 10.1037/1082-989X.7.1.64 [DOI] [PubMed] [Google Scholar]
- 36.Adams RE, Boscarino JA, Figley CR. Compassion fatigue and psychological distress among social workers: a validation study. Am J Orthopsychiatry. 2006;76(1):103–8. 10.1037/0002-9432.76.1.103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sun B, Hu M, Yu S, Jiang Y, Lou B. Validation of the compassion fatigue short scale among Chinese medical workers and firefighters: a cross-sectional study. BMJ Open. 2016;6(6):e011279. 10.1136/bmjopen-2016-011279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Corley MC, Elswick RK, Gorman M, Clor T. Development and evaluation of a moral distress scale. J Adv Nurs. 2001;33(2):250–6. 10.1111/j.1365-2648.2001.01658.x [DOI] [PubMed] [Google Scholar]
- 39.Hamric AB, Borchers CT, Epstein EG. Development and testing of an instrument to measure moral distress in healthcare careers. AJOB Prim Res. 2012;3(2):1–9.26137345 10.1080/21507716.2011.652337 [DOI] [Google Scholar]
- 40.Sun X, Cao FL, Yao J, Chen LP. Research in validity and reliability of the Chinese version of moral distress scale. Chin J Prac Nurs. 2012;28(36):52–5. [Google Scholar]
- 41.Heinze KE, Hanson G, Holtz H, Swoboda SM, Rushton CH. Measuring health care interprofessionals’ moral resilience: validation of the Rushton moral resilience scale. J Palliat Med. 2021;24(6):865–72. 10.1089/jpm.2020.0328 [DOI] [PubMed] [Google Scholar]
- 42.Tian X, He Q, Liu X, Gan X, Jiménez Herrera MF. Moral resilience in registered nurses: cultural adaption and validation study. Nurs Ethics. 2023:9697330231196229. [DOI] [PubMed]
- 43.Brown JD. Self-esteem and self-evaluation: feeling is believing. Psychological perspectives on the self. London, UK: Psychology; 2014. pp. 39–70. [Google Scholar]
- 44.Lu H, While AE, Barriball KL. Job satisfaction and its related factors: a questionnaire survey of hospital nurses in Mainland China. Int J Nurs Stud. 2007;44(4):574–88. 10.1016/j.ijnurstu.2006.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ghasemi A, Zahediasl S. Normality tests for statistical analysis: a guide for non-statisticians. Int J Endocrinol Metab. 2012;10(2):486–9. 10.5812/ijem.3505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schreiber JB. Update to core reporting practices in structural equation modeling. Res Social Adm Pharm. 2017;13(3):634–43. 10.1016/j.sapharm.2016.06.006 [DOI] [PubMed] [Google Scholar]
- 47.Paidipati CP, Lozano AJ, West J, Huang L, Hanlon AL, Ulrich CM. Understanding the mediated relationship between moral distress, depression, and suicide risk in undergraduate nursing students. Nurs Outlook. 2023;71(3):101966. 10.1016/j.outlook.2023.101966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Heng TJT, Shorey S. Experiences of moral distress in nursing students - a qualitative systematic review. Nurse Educ Today. 2023;129:105912. 10.1016/j.nedt.2023.105912 [DOI] [PubMed] [Google Scholar]
- 49.Mazzotta R, De Maria M, Bove D, Badolamenti S, Saraiva Bordignon S, Silveira LCJ, et al. Moral distress in nursing students: cultural adaptation and validation study. Nurs Ethics. 2022;29(2):384–401. 10.1177/09697330211030671 [DOI] [PubMed] [Google Scholar]
- 50.Mason VM, Leslie G, Clark K, Lyons P, Walke E, Butler C, Griffin M. Compassion fatigue, moral distress, and work engagement in surgical intensive care unit trauma nurses: a pilot study. Dimens Crit Care Nurs. 2014;33(4):215–25. 10.1097/DCC.0000000000000056 [DOI] [PubMed] [Google Scholar]
- 51.Caram CS, Peter E, Ramos FR, Brito MJ. The process of moral distress development: a virtue ethics perspective. Nurs Ethics. 2022;29(2):402–12. 10.1177/09697330211033408 [DOI] [PubMed] [Google Scholar]
- 52.Koonce M, Hyrkas K. Moral distress and spiritual/religious orientation: moral agency, norms and resilience. Nurs Ethics. 2023;30(2):288–301. 10.1177/09697330221122905 [DOI] [PubMed] [Google Scholar]
- 53.Boateng A, Aslakson R. Elisabeth Kübler-Ross as astrophysicist: emotional intelligence and resilience unlock the black hole of physician burnout, moral distress, and compassion fatigue. Am J Bioeth. 2019;19(12):54–7. 10.1080/15265161.2019.1674423 [DOI] [PubMed] [Google Scholar]
- 54.Li F, Zhong J, He Z. Moral distress, moral resilience, and job embeddedness among pediatric nurses. Nurs Ethics. 2023:9697330231218347. [DOI] [PubMed]
- 55.Kovanci MS, Atli Özbaş A. Examining the effect of moral resilience on moral distress. Nurs Ethics. 2023;30(7–8):1156–70. 10.1177/09697330231177420 [DOI] [PubMed] [Google Scholar]
- 56.Lin LY, Li XL, Chen J, Hu SC. The influence of moral distress on professional identification of intensive care unit nurses. Chin Nurs Manag. 2016;16(6):772–6. [Google Scholar]
- 57.Shen ZY, Zhong ZQ, Zheng F, Zhang QX, Ding SQ. Relationship between nurses’ moral distress and professional identity. Nurs J Chin PLA. 2018;35(18):34–8. [Google Scholar]
- 58.Meng Z, Zhang L, Zan H, Wang J. Psychological resilience and work engagement of Chinese nurses: a chain mediating model of career identity and quality of work life. Front Psychol. 2023;14:1275511. 10.3389/fpsyg.2023.1275511 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and/or analysed during the current study are not publicly available due to the participant confidentiality, but are available from the corresponding author on reasonable request.