Abstract
Antibiotic use is a risk factor for development of inflammatory bowel diseases (IBDs). IBDs are characterized by a damaged mucus layer, which does not separate the intestinal epithelium from the microbiota. Here, we hypothesized that antibiotics affect the integrity of the mucus barrier, which allows bacterial penetrance and predisposes to intestinal inflammation. We found that antibiotic treatment led to breakdown of the colonic mucus barrier and penetration of bacteria into the mucus layer. Using fecal microbiota transplant, RNA sequencing followed by machine learning, ex vivo mucus secretion measurements, and antibiotic treatment of germ-free mice, we determined that antibiotics induce endoplasmic reticulum stress in the colon that inhibits colonic mucus secretion in a microbiota-independent manner. This antibiotic-induced mucus secretion flaw led to penetration of bacteria into the colonic mucus layer, translocation of microbial antigens into circulation, and exacerbation of ulcerations in a mouse model of IBD. Thus, antibiotic use might predispose to intestinal inflammation by impeding mucus production.
Antibiotics inhibit production of the protective mucus in the colon, thus predisposing to gut inflammation.
INTRODUCTION
Antibiotics are a broad family of drugs that disrupt multiple crucial processes in microbes. Since their discovery, antibiotics have become life-saving therapeutics used to treat microbial infections. The prolific use of antibiotics in both medicine and agriculture has resulted in the rise of antibiotic-resistant microbes, which pose a major challenge to modern health care (1, 2). This extensive use of antibiotics is based on the assumption that, other than toxicity issues when used in large doses, antibiotics disrupt biological processes in microbes and not the host. Yet, recent research in germ-free (GF) animals is beginning to uncover the overlooked effects that antibiotics have on the host (3–6).
The growing exposure to antibiotics in the past centuries has been linked to multiple diseases that are now common in industrialized countries. For example, an interaction between diet and antibiotic-induced alteration to the gut microbiota is associated with obesity and diabetes (1, 2). Another group of diseases with rising prevalence in the industrialized world are inflammatory bowel diseases (IBDs) (7). While the exact etiology of IBDs is not clear (8), recent epidemiological studies have shown a strong and dose-dependent link between these diseases and antibiotic use (9, 10). Studies in mice have shown that nutritional changes together with antibiotic use can drive intestinal inflammation (11). Yet, the exact mechanism is not completely understood.
The colonic mucus layer separates the host from the trillions of microbes that inhabit the gut lumen (12). If this mucus barrier is breached, bacteria can encroach on the host intestinal epithelium and trigger a proinflammatory response (13). Breakdown of this barrier is a hallmark of IBDs and perhaps a driving factor in the development of these diseases (14–16). Antibiotic treatment in mice leads to translocation and uptake of bacteria to gut-draining lymph nodes while predisposing to development of intestinal inflammation (17). Yet, whether antibiotics directly damage the mucus barrier is not clear. Here, we set out to test the hypothesis that antibiotics predispose to development of intestinal inflammation by disrupting the mucus barrier.
RESULTS
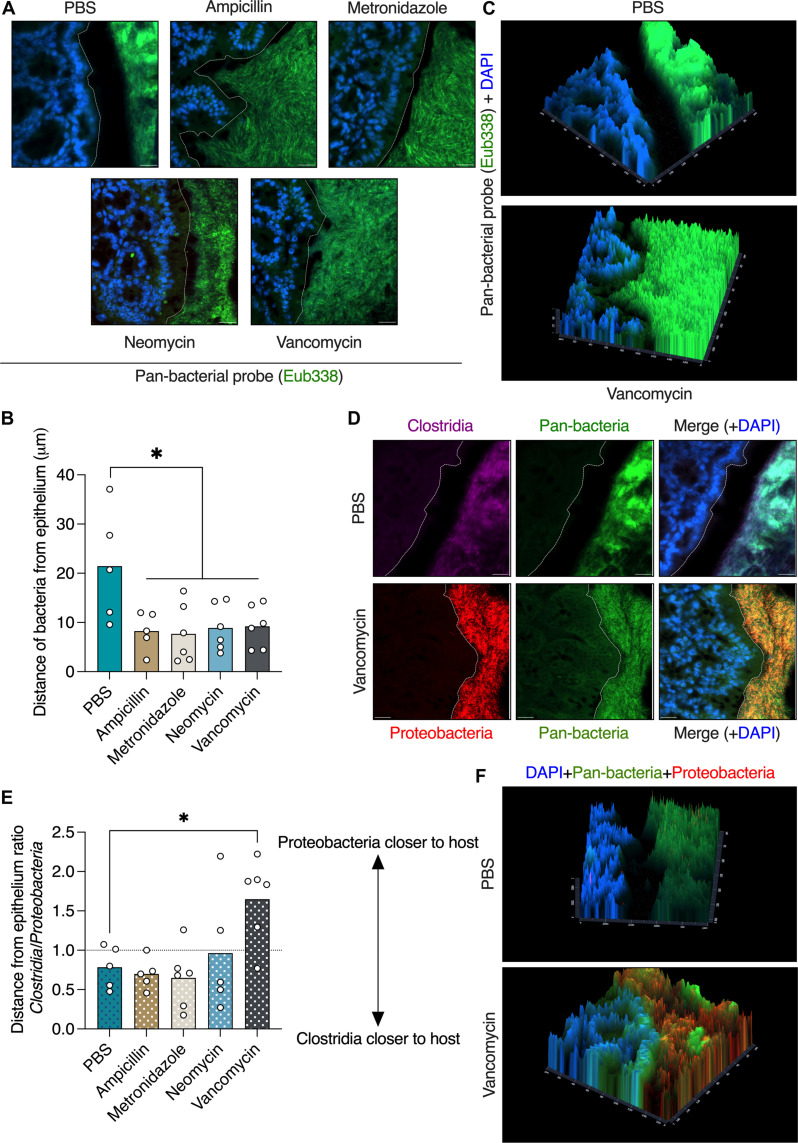
Oral antibiotic treatment disrupts the colonic mucus barrier
To determine whether antibiotic treatment affects the mucus barrier, we orally treated mice with antibiotics. We aimed to mimic short-term antibiotic treatment in patients; thus, we treated the mice twice a day for only 3 days. We used four different antibiotics, each belonging to a different class of antibiotics: ampicillin (aminopenicillin class), metronidazole (nitroimidazole class), neomycin (aminoglycoside class), and vancomycin (glycopeptide class). To quantify bacterial penetration into the colonic mucus barrier, we fixed the tissues in Carnoy’s fixative, which preserves the mucus barrier and the native bacterial spatial localization (18, 19), and stained bacteria using a pan-bacterial fluorescent in situ hybridization (FISH) probe. We found that all four antibiotics tested led to breakdown of the mucus barrier and encroachment of bacteria upon the colonic epithelium (Fig. 1, A and B). Spatial fluorescent intensity imaging also revealed bacterial signals originating in the colonic epithelium (Fig. 1C). Thus, short-term oral antibiotic treatment leads to disruption of the mucus barrier.
Fig. 1. Oral antibiotic treatment disrupts the colonic mucus barrier.
(A) FISH images of colonic tissues from mice treated orally with antibiotics as indicated. Bacteria are stained in green and host nuclei in blue. The dashed white lines mark the edge of the host epithelium. Scale bars, 20 μm. (B) Quantification of distance between luminal bacteria and host epithelium as in (A). (C) Fluorescent intensity imaging of colonic sections from mice treated as indicated. Bacteria are represented by green signal and host epithelium by blue signal. DAPI, 4′,6-diamidino-2-phenylindole. (D) FISH images of colonic tissues from mice treated with antibiotics as indicated and stained with the indicated probes. The dashed white lines mark the edge of the host epithelium. Scale bars, 20 μm. (E) Quantification of the ratio of the distances between Clostridia or Gammaproteobacteria and the host epithelium as in (D). (F) Fluorescent intensity imaging of colonic sections from mice treated as indicated. Pan-bacteria are represented by green signal, Gammaproteobacteria by red signal, and host epithelium by blue signal. (B and E) Each dot represents a mouse. At least 25 measurements per mouse were taken. One-way analysis of variance (ANOVA). *P < 0.05.
Next, we wanted to identify which bacteria come in close contact with the host epithelium after antibiotic treatment. To this end, we performed FISH staining using probes specific to either the Clostridia or the Gammaproteobacteria classes. We chose Clostridia as they are the major Gram-positive class of the gut commensal microbiota and Gammaproteobacteria as representatives of Gram-negative bacteria that are associated with antibiotic-induced dysbiosis and are associated with multiple diseases (1, 2). In agreement with a previous report (18), we found that bacteria from the Clostridia class were spatially closer to the host than Gammaproteobacteria in phosphate-buffered saline (PBS)–treated mice (Fig. 1, D to F). Ampicillin, metronidazole, and neomycin treatments did not affect this spatial segre–gation between Clostridia and Gammaproteobacteria. Vancomycin treatment, which targets Gram-positive bacteria such as Clostridia and is known to cause a bloom of Gammaproteobacteria, led to close contact of Gammaproteobacteria with the host epithelium (Fig. 1, D to F, and fig. S1). Thus, vancomycin is unique as it reverses the spatial position of different bacterial groups in the colon.
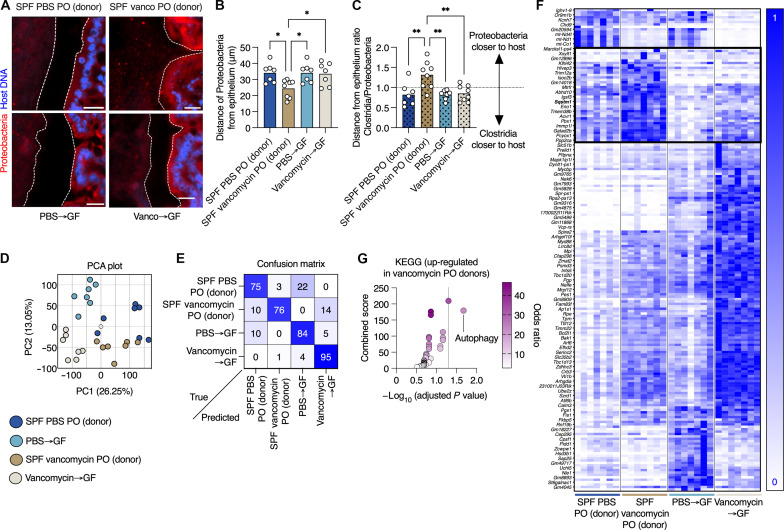
Microbiota transfer from antibiotic-treated mice to GF mice does not transfer the antibiotic’s effect on the mucus barrier
Next, we wanted to determine how antibiotic treatment grants the gut microbes access to the niche nearest to the host epithelium. We hypothesized that the effects of antibiotics on microbiota composition disrupts certain microbial communities, thus allowing others to move closer to the host. Because vancomycin is a narrow-spectrum antimicrobial, which leads to a bloom of potentially pathogenic Gammaproteobacteria (18), we chose to focus on it. We treated mice reared in the specific pathogen–free (SPF) facility with PBS or vancomycin, as above, and transferred their gut microbiota to GF mice via fecal microbiota transfer (FMT). To confirm reliable transfer of the microbiota and confirm that the microbiota of vancomycin-treated mice did not revert back to pretreatment status after transplant, we performed analysis on the microbiota from donor and recipient mice. We focused on the relative abundance of the Bacteroides genus, as these bacteria are both obligate anaerobes and also sensitive to vancomycin treatment in vivo (20). This approach allowed to us validate both the effectiveness of the FMT under anaerobic conditions (PBS donor to GF), as Bacteroides levels would diminish when exposed to oxygen, and the sustained effect of vancomycin (vancomycin donor to GF) as Bacteroides diminish ~100-fold in response to vancomycin in vivo (20). We found that the relative abundance of Bacteroides was nearly identical in PBS-treated donors and their GF recipients, while in both vancomycin-treated donors and their GF recipients, levels of these microbes diminished by several orders of magnitude (fig. S2), confirming that the FMT has reliably transferred the microbiota of SPF mice to GF recipients. As above, FISH staining in colonic sections from mice treated with vancomycin showed barrier dysfunction and presence of Gammaproteobacteria in close contact with the host epithelium (Fig. 2, A to C). However, GF mice that received an FMT from vancomycin-treated mice did not show a barrier defect or encroachment of Gammaproteobacteria (Fig. 2, A to C). Expression of epithelial-derived antimicrobial transcripts was induced in both vancomycin-treated mice and GF mice that received the FMT from vancomycin-treated mice (fig. S3, A and B). This indicates that while the mucus barrier defect cannot be transferred by transferring the microbiota, the antimicrobial gene signature is induced in response to the vancomycin-induced proteobacteria bloom. Thus, the effect of vancomycin on the gut microbiota cannot explain the penetrance of bacteria to the close vicinity of the host epithelium.
Fig. 2. Vancomycin-induced changes to the gut microbiota cannot explain treatment impact on the mucus barrier and gut transcription.
(A) FISH images of colonic tissues from SPF mice treated with vancomycin as indicated or GF mice that received an FMT from vancomycin-treated mice and stained with the indicated probes. The dashed white lines mark the edge of the host epithelium. Scale bars, 20 μm. (B) Quantification of distance between luminal Gammaproteobacteria and host epithelium as in (A). (C) Quantification of the ratio of the distances between Clostridia or Gammaproteobacteria and the host epithelium as in (A). (D) PCA plot of colonic transcriptional profiles of mice treated as indicated. (E) A confusion matrix depicting the percentage of predictions for each category against the true classifications in a four-way Random Forest classification task. Diagonal entries represent the accuracy of predictions for each category (true positives), while off-diagonal entries indicate the model’s misclassifications. (F) Heatmap showing transcriptional changes of the top 200 genes that distinguish between the treatment groups on the basis of the classifier in (E). Each column represents a mouse. (G) Kyoto Encyclopedia of Genes and Genomes (KEGG) pathways of transcripts which are uniquely altered in vancomycin-treated mice (donors) as plotted in (F) (in the black box). (B to D) Each dot represents a mouse. (B and C) One-way ANOVA. At least 25 measurements per mouse were taken. *P < 0.05; **P < 0.01. PO, per os.
The effect of antibiotics on host transcription cannot be explained solely by antibiotic-induced changes to the gut microbiota
Given our observation that antibiotic-induced changes to the gut microbiota cannot explain penetration of bacteria into the mucus barrier, we wanted to test whether vancomycin might be affecting the host directly. To this end, we performed RNA sequencing analysis on colonic tissues from mice raised under SPF conditions that were treated orally with PBS or vancomycin and GF mice that received an FMT from the PBS- or antibiotic-treated mice, as above. In this experimental setup, the SPF mice are exposed to the antibiotic, while the GF mice are exposed to the microbial changes which were induced by the antibiotic. We wanted to determine whether vancomycin induced a transcriptional profile in the SPF mice that was unique, compared to the GF mice or the SPF mice that received PBS. Therefore, we pursued this clustering using two different approaches. First, we subjected the RNA sequencing data to principal components analysis (PCA). This analysis revealed that each experimental group clustered separately and that the first two principal components accounted for 39% of the variance (Fig. 2D). Next, we trained a random-forest (RF) classifier on the four groups (SPF versus GF and PBS versus vancomycin) resulting in high-confidence classification, as is apparent in the confusion matrix (Fig. 2E). The high values along the diagonal of the confusion matrix signify the high percentage of successful assignments of a mouse to the correct group by the RF algorithm. This indicated that each of the four conditions had a unique transcriptional signature and therefore that there are genes that are activated or suppressed solely in the vancomycin-treated mice. We plotted the gene expression for the 200 most predictive genes according to the RF classifier, with hierarchical clustering separating the different conditions into obvious clusters (Fig. 2F). Pathway analysis of those genes that clustered together and distinguished the mice that were orally treated with vancomycin (donors; Fig. 2F) revealed an enrichment in genes related to the autophagy process. These included the Sqstm1 gene, which encodes the P62 protein that sequesters cargo for degradation in autophagosomes (Fig. 2G). The enhanced expression of autophagy-related genes is consistent with the essential role of autophagy in preserving proper goblet cell function in response to accumulation of endoplasmic reticulum (ER) stress (21). The fact that autophagy-related genes are activated in response to vancomycin treatment, but not in response to the vancomycin-treated microbiota, along with the mucus barrier impairment in the mice (Fig. 2, A to C), implies that vancomycin might be causing stress to goblet cells. Thus, while vancomycin-induced changes to the gut microbiota can explain changes in transcription of many genes, it cannot explain all changes to gene expression in mice treated with vancomycin, especially activation of autophagy-related genes.
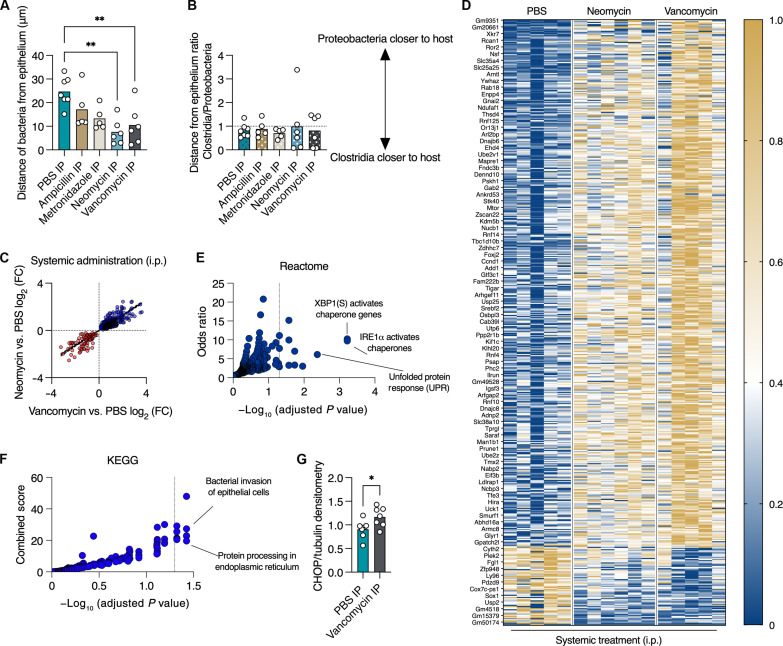
Systemic antibiotic administration induces ER stress, which disrupts the colonic mucus barrier by inhibiting mucus secretion in a microbiota-independent manner
Given our transcriptomic analysis, which suggested a microbiota-independent effect of vancomycin on the host, we next tested this concept. We hypothesized that antibiotic treatment impairs the mucus barrier via a direct effect on the host. We treated mice with the same four antibiotics as above but via systemic administration. We found that systemic administration of ampicillin and metronidazole did not change the distance of bacteria from the host epithelium (Fig. 3A). This implies that the effects of these two antibiotics on the mucus barrier seen in oral administration (Fig. 1, A and B) are microbiota dependent. However, neomycin and vancomycin treatment did impair the mucus barrier (Fig. 3A). Both neomycin and vancomycin have poor luminal availability when administered systemically, given their inability to cross the gastrointestinal mucosa (22, 23). Accordingly, systemic administration of antibiotics did not reverse the spatial position of Clostridia and Gammaproteobacteria (Fig. 3B), which was seen with oral treatment above (Fig. 1E).
Fig. 3. Systemic administration of antibiotics induces ER stress in the colon.
(A) Quantification of distance between luminal bacteria and host epithelium in colons of mice treated with the indicated antibiotics via intraperitoneal one-way ANOVA. (B) Quantification of the ratio of the distances between Clostridia or Gammaproteobacteria and the host epithelium in mice treated as in (A). (C) Expression levels of transcripts in colons of mice treated with vancomycin (x axis) or neomycin (y axis) via intraperitoneal injection as compared to PBS. Plotted are transcripts whose expression was induced by both antibiotics or suppressed by both antibiotics (P < 0.05, Mann-Whitney test). Each dot represents a transcript. Blue, genes that are more highly expressed under antibiotic treatment; red, genes with reduced expression after treatment. (D) Heatmap depicting normalized expression levels of genes shown in (C). Each column represents a mouse. (E and F) Analyses using (E) Reactome or (F) KEGG pathways of transcripts plotted in (C). Dotted line on the x axis represents a P value of 0.05. Each dot represents a category/pathway. (G) Protein levels of CHOP relative to tubulin using densitometry analysis of a Western blot of colonic lysates from mice treated as indicated. Student’s t test. (A, B, and G) Each dot represents a mouse. (A and B) At least 25 measurements per mouse were taken. *P < 0.05, **P < 0.01. IP, intraperitoneal; FC, fold change.
Next, we wanted to determine how systemic neomycin and vancomycin treatment leads to encroachment of the gut microbiota upon the host epithelium. To this end, we performed RNA sequencing using colonic tissues from mice treated systemically with either PBS, neomycin, or vancomycin. As treatment with these two antibiotics produced the same barrier-dysfunction phenotype (Fig. 3A), we tested whether these two antibiotics affect the same transcriptional pathways. We plotted the expression of genes that were induced or suppressed by both antibiotics. To our surprise, we found that the expression of these genes was influenced in a similar manner by the two distinct antibiotics (Fig. 3, C and D). Pathway analysis revealed that the genes that were similarly affected by both neomycin and vancomycin are involved in the ER stress response and the unfolded-protein response pathways (Fig. 3E). Analysis using Kyoto Encyclopedia of Genes and Genomes (KEGG) revealed that these genes are activated in response to bacterial invasion to epithelial cells and processing of proteins in the ER (Fig. 3F). To verify our RNA sequencing analysis, we quantified the levels of the ER stress response protein C/EBP homologous protein (CHOP) and found that it was indeed expressed at higher levels in the colons of mice treated systemically with vancomycin (Fig. 3G). Thus, systemic treatment with neomycin or vancomycin induces an ER stress response in the colon.
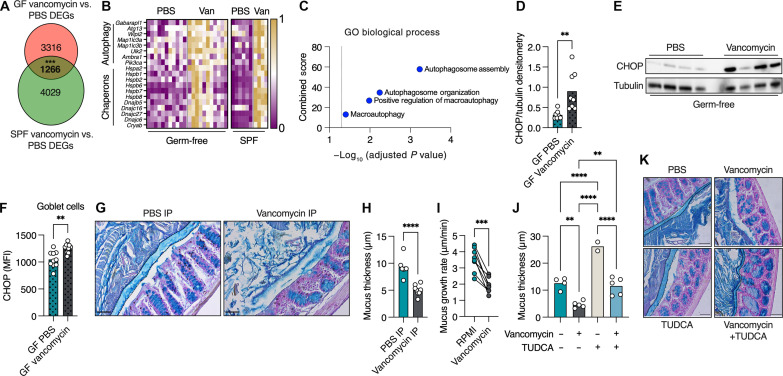
The results obtained by FMT (Fig. 2) and systemic antibiotic administration (Fig. 3) suggest that antibiotics might affect the host directly, in a microbiota-independent manner. To verify this hypothesis, we treated GF mice with vancomycin via systemic administration. We chose to focus on vancomycin as it is used both systemically and orally in the clinic, while neomycin is used mostly topically. We then compared transcripts that were affected by systemic vancomycin treatment in GF mice with those affected in SPF mice to determine which effects of vancomycin on the colon were microbiota independent. We found 1266 genes that were differently expressed in the same manner (i.e., up-regulated in both GF and SPF or down-regulated in both GF and SPF) in GF and SPF mice in response to vancomycin treatment (Fig. 4A). To assess the statistical significance of our findings, we conducted bootstrapped trials. We generated 10,000 random samples of the same size as the significant gene sets from the original data for each mouse and calculated the number of intersecting genes with consistent fold-change directions for each random sample. This analysis confirmed that the number of transcripts affected similarly in vancomycin-treated GF and SPF mice was far larger than expected randomly (P < 0.001). As predicted by the RF analysis (Fig. 2, E to G), we found multiple key autophagy genes to be induced by vancomycin treatment in both GF and SPF mice (Fig. 4, B and C). In addition, we found induction of multiple ER stress–related genes in response to vancomycin in both GF and SPF mice (Fig. 4B). Accordingly, and as seen in vancomycin-treated SPF mice, protein levels of the ER stress marker CHOP were higher in whole colonic tissues (Fig. 4, D and E) and specifically in goblet cells (Fig. 4F) of GF mice treated with vancomycin. Thus, vancomycin treatment induces ER stress and activation of autophagy in the colon by directly affecting the host in a microbiota-independent manner.
Fig. 4. Systemic vancomycin treatment induces ER stress in a microbiota-independent manner which inhibits mucus secretion in the colon.
(A) Venn diagram depicting the number of differentially expressed genes (DEGs) in colonic tissue from GF and SPF mice in response to vancomycin intraperitoneal injection. The overlapping area represents DEGs that are affected in the same manner (induced or suppressed) in both GF and SPF mice in response to vancomycin treatment (the P value for the observed intersection was computed on the basis of the proportion of random samples with intersections greater than or equal to the observed value). (B) Heatmap depicting normalized expression levels of autophagy- and ER stress–related genes in response to vancomycin intraperitoneal treatment. Each column represents a mouse. (C) Analysis of overlapping (in bold) DEGs depicted in (A) using Gene Ontology (GO), selecting for pathways associated with autophagy. (D and E) Protein levels of CHOP relative to Tubulin using densitometry analysis of a Western blot of colonic lysates from GF mice treated as indicated. (F) Quantification of protein levels of CHOP, specifically in colonic goblet cells via immunohistochemistry. (G) Colonic sections from mice treated systemically as indicated, stained with Alcian blue to visualize mucus. The mucus layer is defined by the dashed line. Scale bars, 50 μm. (H) Measurement of mucus thickness as shown in (G). (I) Mucus growth rate. Lines connect tissues from the same mouse. Paired t test. (J) Measurement of mucus thickness in mice treated as indicated. One-way ANOVA. (K) Colonic sections from mice treated systemically as indicated, stained with Alcian blue to visualize mucus. The mucus layer is defined by the dashed line. Scale bars, 50 μm. (D, F, H, and J) Each dot represents a mouse. (D, F, and H) Student’s t test. (H and J) At least 25 measurements per mouse were taken. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001. MFI, mean fluorescent intensity.
ER stress is an intracellular switch that limits mucus secretion by goblet cells (21, 24). Given our observation above, that vancomycin induces ER stress in the colon, and specifically in goblet cells, we hypothesized that vancomycin treatment leads to impairment of the separation between host and microbiota in the colon by inhibiting mucus secretion. To test this hypothesis, we treated mice with vancomycin and measured the colonic mucus thickness using Alcian blue staining. We found mice treated systemically with vancomycin lacked a clear mucus in most areas of the colonic epithelial circumference (Fig. 4, G and H). This observation raised the possibility that vancomycin impairs the ability of goblet cells to secrete mucus. The optimal way to test this hypothesis would be the use of GF mice treated with vancomycin. However, GF mice do not produce a fully formed mucus layer that can be measured using Alcian blue staining and also do not contain bacteria to be detected using FISH. To circumvent this problem, we measured colonic mucus secretion rates using an ex vivo system. We excised colonic sections from naive mice, split them into two sections, and fitted them into two measurement chambers. One colonic section from each mouse was infused with media and the other with media supplemented with vancomycin. Using this experimental approach, the treated and control tissues originate from the same mouse. We found that all tissues treated with vancomycin showed impaired mucus secretion rates (Fig. 4I). As the vancomycin was infused only on the basolateral side of the colonic tissue, and for only 45 min, this result demonstrates that the deleterious effect of vancomycin on mucus secretion is microbiota independent.
Next, we wanted to test whether we could reverse the mucus secretion defect caused by vancomycin treatment in vivo. We have previously found that the bile acid tauroursodeoxycholic acid (TUDCA) can increase mucus secretion rates by reducing ER stress in colonic goblet cells (21). As vancomycin treatment induces ER stress in the colon, we attempted to restore proper mucus secretion by alleviating this ER stress using TUDCA. We found that TUDCA treatment reversed the mucus secretion defect caused by vancomycin treatment, restoring a proper mucus barrier (Fig. 4, J and K). Thus, vancomycin treatment inhibits secretion from colonic goblet cells by inducing ER stress.
Inhibition of mucus secretion by vancomycin use impairs the colonic barrier function and aggravates colonic inflammation
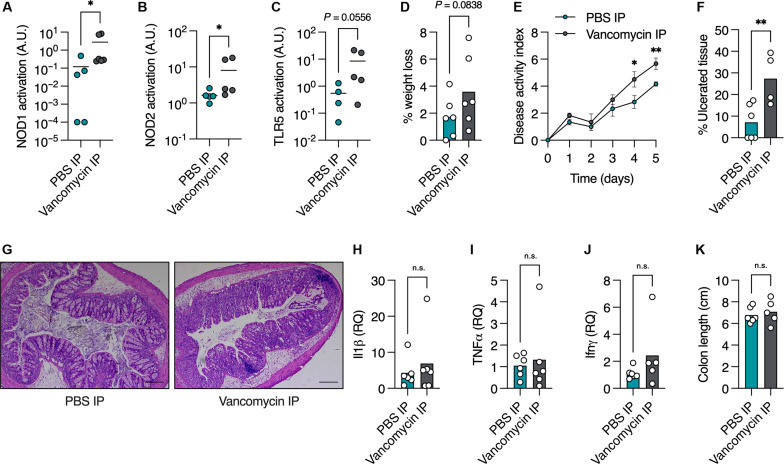
Last, we wanted to test whether this vancomycin-induced impairment in mucus secretion affects colonic host defense. First, we compared the levels of bacterial antigens in the bloodstream of mice treated systemically with vancomycin. Presence of microbial antigens in the blood is directly linked to intestinal barrier function (25). We found higher levels of NOD1, NOD2, and Toll-like receptor 5 (TLR5) agonists in the serum of vancomycin-treated mice (Fig. 5, A to C), indicating impaired colonic barrier function. We then challenged mice treated systemically with vancomycin in a model of dextran sulfate sodium (DSS)–induced colitis. We reasoned that this is the most suitable model of intestinal inflammation in this study, because DSS directly impairs the colonic mucus layer and severely affects mice with an impaired mucus barrier (14, 21). We treated PBS- and vancomycin-treated mice with 4% DSS in drinking water, which results in only mild colitis in Swiss Webster mice. We found that vancomycin-treated mice lost more weight and showed more severe signs of disease than control mice (Fig. 5, D and E). Vancomycin-treated mice had notably larger colonic areas with ulcers than control mice (Fig. 5, F and G), indicating poor protection by the mucus layer against the DSS. Other disease markers, such as proinflammatory cytokines and colon length, were not altered by vancomycin treatment (Fig. 5, H to K). Thus, vancomycin impairs mucus secretion from colonic goblet cells in a microbiota-independent manner that damages host protection against gut ulceration.
Fig. 5. Systemic vancomycin treatment impairs colonic barrier function and aggravates ulceration.
(A to C) Detection of NOD1 (A), NOD2 (B), and TLR5 (C) agonists in mouse serum using reporter cell lines. (D to K) Mice were treated with 4% DSS for 5 days. (D) Percentage weight change on day 5 of treatment compared to before treatment, (E) disease activity index ± SEM, (F) quantification of percent of colonic area with ulceration, and (G) representative histological images of colonic tissue from DSS-treated mice. (H to J) Expression of proinflammatory genes using quantitative polymerase chain reaction. (K) Colon length of mice treated as indicated. (A to D, F, and H to K) Each dot represents a mouse. Scale bars, 20 μm. (A to F and H to K) Student’s t test. *P < 0.05, **P < 0.01. n.s., not significant; RQ, relative quantity.
DISCUSSION
Antibiotics were hailed as miracle drugs, making once fatal infections seem mundane and casual. This success of antibiotics in improving human lives has led to their overuse in both medicine and agriculture. For a person living in the industrialized world, avoiding antibiotic exposure has become very difficult. The consequences of this overuse and overexposure have led to the rise of antibiotic-resistant pathogens, and, according to casual association, also development of a plethora of chronic diseases. Diseases such as diabetes, growth defects, and chronic inflammations have been linked in multiple studies to antibiotic use (26–28). As antibiotics target microbes directly, it is widely assumed that the effects of antibiotics on the gut microbiota are the main drivers of these diseases (1, 2).
While antibiotic use affects the host by disrupting its microbiota, recent evidence suggests that antibiotics might act directly on host cells. By using GF mice, a few groups have shown that antibiotic drugs can activate an antiviral response (6), affect tolerance to infection (5), and influence host metabolism (4) in a microbiota-independent manner by acting directly on host cells. How antibiotics exert this effect on host cells is not completely clear, yet it is thought that they can interfere with mitochondrial function, DNA replication, and various other cellular processes (3). Even the use of antibiotics to protect cultured cells from infection, a staple of cellular and molecular biology, has come into question because of their effect on these cells (29).
Another group of chronic diseases that are linked to antibiotic use are IBDs. Recent epidemiological studies have provided a strong link between antibiotic use and risk for development of IBD (9), in a dose-dependent manner (10). Here, we hypothesized that antibiotic use might lead to development of intestinal inflammation by affecting the colonic mucus barrier. The ability of the mucus barrier to provide separation between the host and its gut microbiota is crucial for maintaining gut homeostasis (12). Breakdown of this barrier is observed both in animal models of IBD and in patients with IBD (14, 15). As IBDs are characterized by loss of tolerance to the gut microbiota (30), it is thought that impairment of the protective mucus barrier can drive these diseases. Without a proper mucus barrier, the microbes come in close contact with host tissues, triggering an immune response (13).
We found that short-term oral antibiotic treatment was sufficient to impair the separation between host and microbiota in the colon (Fig. 1). This phenomenon was true for all the antibiotics we tested. Using FMT and RNA sequencing followed by machine learning, we concluded that the effects of vancomycin on the mucus barrier could not be transferred to GF mice by transferring the microbiota alone (Fig. 2). Instead, we found that vancomycin could impede mucus secretion in the colon, in a microbiota-independent manner, by inducing ER stress in colonic cells (Figs. 3 and 4). Unexpectedly, this effect of vancomycin on the ability of goblet cells to secrete mucus was immediate, as a few minutes following vancomycin infusion into the ex vivo chamber, we observed a stark reduction in mucus secretion rates. Thus, we conclude that antibiotics have a deleterious effect on the mucus barrier, in part by acting directly on host cells. It is important to note that we do not rule out microbiota-dependent deleterious effects on the mucus barrier, but rather that a direct effect on the host also exists. A recent study has shown that transferring microbiota from humans with a history of antibiotic use to mice can cause mucus barrier defects in mice (31).
Our study answers one question (does antibiotic treatment impair the mucus barrier?) but raises two more questions. The first is: Does antibiotic treatment play a causative role in development of IBD? This question will be hard to answer in humans and will need to be tested in animal models of IBD. The major caveat of this approach is that animal models only partially reflect IBD pathology and development (32, 33). The second question is: How do antibiotics impair mucus production? Our experiments suggest that certain antibiotics induce ER stress in colonic cells, thus diminishing mucus production through a previously described mechanism (21, 34). We found it unexpected that two distinct antibiotics from different classes, neomycin and vancomycin, both induced an ER stress response in the colon. As both drugs have distinct antimicrobial mechanisms, it is not clear why both would induce ER stress in host cells. It would be interesting to test whether antibiotic treatment increases the risk for developing IBD in patients carrying predisposing mutations in autophagy-related genes, as autophagy is needed to relieve ER stress in goblet cells to allow proper mucus secretion (21). Mutations in autophagy-related genes are associated with development of IBD (8, 35).
Our ability to definitively determine that vancomycin treatment predisposes to development of intestinal inflammation by inhibiting mucus secretion in a microbiota-independent manner is limited by the tools available and the experimental settings themselves. First, as GF mice lack a fully formed mucus layer, we cannot measure whether vancomycin inhibits mucus secretion in a microbiota-independent manner. The microbiota plays a key role in shaping the mucus layer (12). However, our experiment using an ex vivo chamber (Fig. 4I) shows that, when administered basolaterally (i.e., not to the luminal side where the bacteria reside), vancomycin reduces mucus secretion rates twofold within 45 min. This rapid response of goblet cells to vancomycin cannot be explained by changes to the microbiota. Second, DSS treatment of GF mice results in increased hemorrhaging and high mortality but much lower signs of inflammation (36). Considering these, and the role microbes play in development of intestinal inflammation, we cannot test the effect of vancomycin on development of intestinal inflammation under GF settings. Thus, while our observations show that vancomycin affects the host in a microbiota-independent manner, the causative role of antibiotics in development of IBD still needs to be proven experimentally.
MATERIALS AND METHODS
Ethics statement
All experiments in mice were conducted in compliance with the European Union directive regarding the protection of animals used for experimental and other scientific purposes. Experiments were approved by the institutional animal care and use committee (IACUC) of the Bar-Ilan University (study ID no. 25-04-2019). Animal experiments performed at Umeå University, Sweden, were approved by the local animal ethical committee (Dnr A14-2019).
Mice
C57BL6/J and Swiss Webster mice were bred and maintained under a 12-hour light/dark cycle and fed standard chow in either SPF or GF conditions at the Azrieli Faculty of Medicine of the Bar-Ilan University. For ex vivo mucus measurements, C57BL6/J mice originally obtained from Charles River Laboratory Germany were bred in-house at Umeå University, Sweden, and maintained under a 12-hour light/dark cycle in individually ventilated cages in a pathogen-free environment at 22° ± 1°C. Mice were fed a standard chow diet and had ad libitum access to food and water (no. 801730, Special Diet Services, UK).
Antibiotic and TUDCA treatments
Eight- to 14-week-old mice were treated twice a day for 3 days with 2.5 mg of either ampicillin, metronidazole, neomycin, or vancomycin dissolved in 100 μl of drinking water (for oral treatment) or PBS (for intraperitoneal injection). On the fourth day, mice were euthanized according to IACUC guidelines, and tissues and blood were harvested. For treatment of GF mice, mice were transferred under a strike environment from GF isolators to Tecniplast IsoCages to prevent outside contamination. Feces were tested to rule out contamination using polymerase chain reaction (PCR) for bacterial 16S. For TUDCA treatment, mice were treated via intraperitoneal injection with TUDCA (250 mg/kg; Sigma-Aldrich T0266) dissolved in PBS twice daily in addition to vancomycin treatment.
FISH, mucus thickness, and bacterial distance from epithelium measurements
Midcolon tissues containing a fecal pellet were excised from euthanized mice and immediately fixed in Carnoy’s fixative to preserve the mucus layer. Tissues were then processed for paraffin embedding using a standard automated protocol. Sections (7 μm thick) were deparaffinized, and FISH was conducted according to standard protocol (37) with the following probes: pan-bacterial probes EUB338I (GCT GCC TCC CGT AGG AGT), EUB338II (GCA GCC ACC CGT AGG TGT), and EUB338III (GCT GCC ACC CGT AGG TGT); Gammaproteobacteria probes GAM42a (GCC TTC CCA CAT CGT TT) and BET42a (GCC TTC CCA CTT CGT TT); and Clostridia Clep866 (GGT GGA TWA CTT ATT GTG) and Erec482 (GCT TCT TAG TCA RGT ACC G). Slides were mounted with a 4′,6-diamidino-2-phenylindole–containing mount. Images were captured using an AxioImager M2 fluorescent microscope and distance between the host epithelium and bacteria quantified using Zeiss Zen Blue software. For mucus thickness, measurements sections were stained with Alcian blue, and mucus thickness was measured according to standard protocol (21).
Fecal microbiota transplant
Feces collected from vancomycin-treated mice housed at the SPF barrier facility were immediately transferred into an anaerobic chamber. Feces were vortexed in sterile PBS, debris allowed to settle by gravity, and supernatant transferred to fresh tubes. Sealed tubes were then removed from the anaerobic chamber and orally administered to GF Swiss Webster mice via gavage. Inoculated mice were then transferred to Tecniplast IsoCages to prevent outside contamination for 24 hours before tissue collection.
RNA sequencing
RNA from frozen colonic tissues was extracted using a Qiagen RNeasy Universal kit. Integrity of the isolated RNA was analyzed using the Agilent TS HS RNA Kit and TapeStation 4200 at the Genome Technology Center at the Azrieli Faculty of Medicine, Bar-Ilan University, and 1000 ng of total RNA was treated with the NEBNext poly (A) mRNA Magnetic Isolation Module (NEB, no. E7490L). RNA sequencing libraries were produced by using the NEBNext Ultra II RNA Library Prep Kit for Illumina (NEB #E7770L). Quantification of the library was performed using a dsDNA HS Assay Kit and Qubit (Molecular Probes, Life Technologies), and qualification was done using the Agilent TS D1000 kit and TapeStation 4200, and 250 nM of each library was pooled together and diluted to 4 nM according to the NextSeq manufacturer’s instructions; 1.6 pM was loaded onto the Flow Cell with 1% PhiX library control. Libraries were sequenced with the Illumina NextSeq 550 platform with single-end reads of 75 cycles according to the manufacturer’s instructions.
Mapping RNA sequences for transcriptome analysis
The RNA sequencing data were analyzed using the RASflow pipeline (38) mapping the reads to the transcriptome (Mus_musculus.GRCm39.cdna) using the hisat2 aligner (39) and counting features using featureCounts (40). For the genome and transcriptome datasets, any missing gene names (using mmusculus_gene_ensembl) are replaced with gene IDs.
We filtered out sparse genes, which we defined as those with over 50% zero values, to concentrate on genes with meaningful expression levels and to decrease computational complexity. We started with 35,453 genes and removed 14,981 sparse genes, leaving us with 20,472 genes. Following this, we normalized the data with a scaling factor of 106. The purpose of this normalization was to make the samples comparable by compensating for variations in library sizes. PCA plot was generated using RNAlysis (41). Pathway analysis was performed using Enrichr (42–44). The raw and normalized RNA sequencing data are available at National Center for Biotechnology Information (NCBI) Gene Expression Omnibus (GEO) GSE260592. The RASflow configuration scripts can be found in the GitHub repository: https://github.com/AmirErez/Manuscript-Antibiotics_Damage_The_Colonic_Mucus/
Four-way RF classification
To accurately distinguish among the four groups—Van donor, Van recipient, PBS donor, and PBS recipient, we trained a RF classifier. The classifier was trained using 20 samples, with 5 from each group, and tested on 8 samples, 2 from each group. The features were normalized to ensure each row’s sum equaled 1 million, standardizing the data scale for more effective learning. Using the RandomForestClassifier from scikit-learn, we configured each forest with 200 estimators (trees) and conducted 10,000 iterations. The scripts for the classification can be found in the GitHub repository: https://github.com/AmirErez/Manuscript-Antibiotics_Damage_The_Colonic_Mucus/
Barrier function analysis
Blood was collected post-mortem via cardiac puncture and incubated at room temperature for 30 min in 1.5-ml tubes to allow clotting. Samples were then centrifuged at 1500g for 20 min at 4°C after which serum was collected to fresh tubes. Serum (20 μl) was added to wells containing InvivoGen HEK-Blue reporter cells, and luminal antigens were detected following the manufacturer’s instructions.
Ex vivo mucus measurements and vancomycin treatment
Mucus growth rate in colonic tissue explant was measured as previously described (45). Briefly, distal colon tissue from 8- to 12-week-old wild-type mice was collected and washed with 4 to 5 ml of Kreb’s transport buffer to remove luminal content and unattached mucus. After muscle layer removal, the tissue was separated into two pieces. The tissues were mounted in horizontal perfusion chambers and maintained at 37°C. One piece of colon was incubated basolaterally with RPMI supplemented with vancomycin (1.25 mg/ml), while the other was mounted and incubated basolaterally with RPMI, as a control. The mucus was overlaid with 10-μm-sized beads to visualize the surface, and the mounted tissues were then covered by Kreb’s mannitol buffer to maintain a moist environment. Mucus thickness was measured repeatedly with a micromanipulator-connected glass needle over 45 min, and the mucus growth rate (micrometer per minute) was calculated as the change in mucus thickness per minute.
Chemical-induced colitis model
Swiss Webster mice housed under SPF conditions were treated with 4% DSS (colitis grade, 36,000 to 50,000 Da, MP) in drinking water. Fresh DSS was prepared daily. Disease activity index was measured daily, on the basis of weight loss, stool consistency, and rectal bleeding as previously described (37). Briefly, weight loss relative to initial weight, stool consistency (solid, loose, or diarrhea), and rectal bleeding were each individually scored on a 0 to 4 scale and summed for each mouse at the indicated time points. For measurements of ulceration area, hematoxylin and eosin–stained colonic sections from treated mice were visualized using a light microscope as above. Ulcerated surface area and healthy area were measured using Zeiss Zen Blue software. Percentage ulcerated area was calculated as [ulcerated area]/[healthy area + ulcerated area].
Quantitative PCR analysis
For analysis of proinflammatory cytokines, RNA was extracted from colonic tissues using the Qiagen RNeasy Universal kit, and cDNA prepared using the Thermo High-Capacity cDNA Reverse Transcription Kit. mRNA levels of proinflammatory cytokines were analyzed using TaqMan probes and normalized to 18S levels. For analysis of Bacteroides levels, microbial DNA was extracted from mouse feces using the PureLink Microbiome DNA Purification Kit, and 45 ng of DNA was used for quantitative PCR analysis using the following primers (46): Bacteroides F- GGTTCTGAGAGGAGGTCCC; R- CTGCCTCCCGTAGGAGT. Levels of Bacteroides were normalized to total bacterial DNA using the primers: Universal 16S F-ACTCCTACGGGAGGCAGCAGT; R-ATTACCGCGGCTGCTGGC.
Statistical analysis
Statistical analysis was performed using GraphPad Prism as detailed in figure legends.
Acknowledgments
Funding: This work was supported by the Azrieli Foundation Early Career Faculty Fellowship (to S.B.), the Israeli Science Foundation (ISF) (925/19 and 1851/19 to S.B.), the European Research Council (ERC) Starting Grant (GCMech 101039927 to S.B.), and Swedish Research Council grants 2018-02095 and 2021-06602 (to B.O.S.).
Author contributions: Conceptualization: J.S., L.Z., M.N.-O., A.E., and S.B. Methodology: B.O.S., A.E., and S.B. Investigation: J.S., L.Z., Y.L., R.F., M.N., A.G., M.Z., E.R., S.T., S.M., S.B.-S., A.A., S.H.-S., M.N.-O., M.W., B.O.S., A.E., and S.B. Visualization: Y.L., A.E., and S.B. Supervision: B.O.S., A.E., and S.B. Writing—original draft: S.B. Writing—review and editing: B.O.S., A.E., and S.B.
Competing interests: The authors declare that they have no competing interests.
Data and materials availability: All data needed to evaluate the conclusions in the paper are present in the paper and/or the Supplementary Materials. Bulk RNA sequencing data are available at NCBI GEO GSE270467. RNA sequencing analysis scripts and the RF classification scripts are available at AmirErez/Manuscript-Antibiotics_Damage_The_Colonic_Mucus: Zenodo. https://doi.org/10.5281/zenodo.13234054 as well as https://github.com/AmirErez/Manuscript-Antibiotics_Damage_The_Colonic_Mucus.
Supplementary Materials
This PDF file includes:
Figs. S1 to S3
REFERENCES AND NOTES
- 1.de Nies L., Kobras C. M., Stracy M., Antibiotic-induced collateral damage to the microbiota and associated infections. Nat. Rev. Microbiol. 21, 789–804 (2023). [DOI] [PubMed] [Google Scholar]
- 2.Fishbein S. R. S., Mahmud B., Dantas G., Antibiotic perturbations to the gut microbiome. Nat. Rev. Microbiol. 21, 772–788 (2023). [DOI] [PubMed] [Google Scholar]
- 3.Yadav S., Shah D., Dalai P., Agrawal-Rajput R., The tale of antibiotics beyond antimicrobials: Expanding horizons. Cytokine 169, 156285 (2023). [DOI] [PubMed] [Google Scholar]
- 4.Yang J. H., Bhargava P., McCloskey D., Mao N., Palsson B. O., Collins J. J., Antibiotic-induced changes to the host metabolic rnvironment inhibit drug efficacy and alter immune function. Cell Host Microbe 22, 757–765.e3 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Colaço H. G., Barros A., Neves-Costa A., Seixas E., Pedroso D., Velho T., Willmann K. L., Faisca P., Grabmann G., Yi H. S., Shong M., Benes V., Weis S., Köcher T., Moita L. F., Tetracycline antibiotics induce host-dependent disease tolerance to infection. Immunity 54, 53–67.e7 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gopinath S., Kim M. V., Rakib T., Wong P. W., van Zandt M., Barry N. A., Kaisho T., Goodman A. L., Iwasaki A., Topical application of aminoglycoside antibiotics enhances host resistance to viral infections in a microbiota-independent manner. Nat. Microbiol. 3, 611–621 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alatab S., Sepanlou S. G., Ikuta K., Vahedi H., Bisignano C., Safiri S., Sadeghi A., Nixon M. R., Abdoli A., Abolhassani H., Alipour V., Almadi M. A. H., Almasi-Hashiani A., Anushiravani A., Arabloo J., Atique S., Awasthi A., Badawi A., Baig A. A. A., Bhala N., Bijani A., Biondi A., Borzì A. M., Burke K. E., Carvalho F., Daryani A., Dubey M., Eftekhari A., Fernandes E., Fernandes J. C., Fischer F., Haj-Mirzaian A., Haj-Mirzaian A., Hasanzadeh A., Hashemian M., Hay S. I., Hoang C. L., Househ M., Ilesanmi O. S., Balalami N. J., James S. L., Kengne A. P., Malekzadeh M. M., Merat S., Meretoja T. J., Mestrovic T., Mirrakhimov E. M., Mirzaei H., Mohammad K. A., Mokdad A. H., Monasta L., Negoi I., Nguyen T. H., Nguyen C. T., Pourshams A., Poustchi H., Rabiee M., Rabiee N., Ramezanzadeh K., Rawaf D. L., Rawaf S., Rezaei N., Robinson S. R., Ronfani L., Saxena S., Sepehrimanesh M., Shaikh M. A., Sharafi Z., Sharif M., Siabani S., Sima A. R., Singh J. A., Soheili A., Sotoudehmanesh R., Suleria H. A. R., Tesfay B. E., Tran B., Tsoi D., Vacante M., Wondmieneh A. B., Zarghi A., Zhang Z. J., Dirac M., Malekzadeh R., Naghavi M., The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 5, 17–30 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.T. A. Harris-Tryon, S. Bel, “Gene/environment interaction and autoimmune disease” in Beyond Our Genes: Pathophysiology of Gene and Environment Interaction and Epigenetic Inheritance, R. Teperino, Ed. (Springer International Publishing, 2020), pp. 139–156; 10.1007/978-3-030-35213-4_8. [DOI] [Google Scholar]
- 9.Nguyen L. H., Örtqvist A. K., Cao Y., Simon T. G., Roelstraete B., Song M., Joshi A. D., Staller K., Chan A. T., Khalili H., Olén O., Ludvigsson J. F., Antibiotic use and the development of inflammatory bowel disease: A national case-control study in Sweden. Lancet Gastroenterol. Hepatol. 5, 986–995 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Faye A. S., Allin K. H., Iversen A. T., Agrawal M., Faith J., Colombel J.-F., Jess T., Antibiotic use as a risk factor for inflammatory bowel disease across the ages: A population-based cohort study. Gut 72, 663–670 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee J.-Y., Cevallos S. A., Byndloss M. X., Tiffany C. R., Olsan E. E., Butler B. P., Young B. M., Rogers A. W. L., Nguyen H., Kim K., Choi S.-W., Bae E., Lee J. H., Min U.-G., Lee D.-C., Bäumler A. J., High-fat diet and antibiotics cooperatively impair mitochondrial bioenergetics to trigger dysbiosis that exacerbates pre-inflammatory bowel disease. Cell Host Microbe 28, 273–284.e6 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Inaba R., Vujakovic S., Bergstrom K., The gut mucus network: A dynamic liaison between microbes and the immune system. Semin. Immunol. 69, 101807 (2023). [DOI] [PubMed] [Google Scholar]
- 13.Van der Sluis M., De Koning B. A. E., De Bruijn A. C. J. M., Velcich A., Meijerink J. P. P., Van Goudoever J. B., Büller H. A., Dekker J., Van Seuningen I., Renes I. B., Einerhand A. W. C., Buller H. A., Dekker J., Van Seuningen I., Renes I. B., Einerhand A. W. C., Muc2-deficient mice spontaneously develop colitis, indicating that MUC2 is critical for colonic protection. Gastroenterology 131, 117–129 (2006). [DOI] [PubMed] [Google Scholar]
- 14.Johansson M. E., Gustafsson J. K., Holmen-Larsson J., Jabbar K. S., Xia L., Xu H., Ghishan F. K., Carvalho F. A., Gewirtz A. T., Sjovall H., Hansson G. C., Bacteria penetrate the normally impenetrable inner colon mucus layer in both murine colitis models and patients with ulcerative colitis. Gut 63, 281–291 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van der Post S., Jabbar K. S., Birchenough G., Arike L., Akhtar N., Sjovall H., Johansson M. E. V., Hansson G. C., Structural weakening of the colonic mucus barrier is an early event in ulcerative colitis pathogenesis. Gut 68, 2142–2151 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fancy N., Nitin, Kniffen D., Melvin M., Kazemian N., Sadeghi J., Letef C. A., D’Aloisio L., Copp A. G., Inaba R., Hans G., Jafaripour S., Haskey N., Raman M., Daneshgar P., Chadee K., Ghosh S., Gibson D. L., Pakpour S., Zandberg W., Bergstrom K. S. B., Fecal-adherent mucus is a non-invasive source of primary human MUC2 for structural and functional characterization in health and disease. J. Biol. Chem. 300, 105675 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Knoop K. A., McDonald K. G., Kulkarni D. H., Newberry R. D., Antibiotics promote inflammation through the translocation of native commensal colonic bacteria. Gut 65, 1100–1109 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Duncan K., Carey-Ewend K., Vaishnava S., Spatial analysis of gut microbiome reveals a distinct ecological niche associated with the mucus layer. Gut Microbes 13, 1874815 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.M. E. V. Johansson, G. C. Hansson, “Preservation of mucus in histological sections, immunostaining of mucins in fixed tissue, and localization of bacteria with FISH” in Mucins: Methods and Protocols, M. A. McGuckin, D. J. Thornton, Eds. (Humana Press, 2012), pp. 229–235; 10.1007/978-1-61779-513-8_13. [DOI] [PubMed] [Google Scholar]
- 20.Nazzal L., Soiefer L., Chang M., Tamizuddin F., Schatoff D., Cofer L., Aguero-Rosenfeld M. E., Matalon A., Meijers B., Holzman R., Lowenstein J., Effect of vancomycin on the gut microbiome and plasma concentrations of gut-derived uremic solutes. Kidney Int. Rep. 6, 2122–2133 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Naama M., Telpaz S., Awad A., Ben-Simon S., Harshuk-Shabso S., Modilevsky S., Rubin E., Sawaed J., Zelik L., Zigdon M., Asulin N., Turjeman S., Werbner M., Wongkuna S., Feeney R., Schroeder B. O., Nyska A., Nuriel-Ohayon M., Bel S., Autophagy controls mucus secretion from intestinal goblet cells by alleviating ER stress. Cell Host Microbe 31, 433–446.e4 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.S. Patel, C. V. Preuss, F. Bernice, “Vancomycin” in StatPearls (StatPearls Publishing, 2024); www.ncbi.nlm.nih.gov/books/NBK459263/. [PubMed] [Google Scholar]
- 23.Jana S., Deb J. K., Molecular understanding of aminoglycoside action and resistance. Appl. Microbiol. Biotechnol. 70, 140–150 (2006). [DOI] [PubMed] [Google Scholar]
- 24.Naama M., Bel S., Autophagy-ER stress crosstalk controls mucus secretion and susceptibility to gut inflammation. Autophagy 19, 3014–3016 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Serradas P., Thaiss C. A., Gertler A., Aamar S., Blacher E., Halpern Z., Katz M. N., Geiger B., Grosheva I., Grosfeld A., Elinav E., Harmelin A., Ben-Zeev R., Tengeler A. C., Elazar M., Lehavi-Regev D., Barak O., Soffer E., Pevsner-Fischer M., Shapiro H., Braverman S., Levy M., Zheng D., Grosheva I., Zheng D., Soffer E., Blacher E., Braverman S., Tengeler A. C., Barak O., Elazar M., Ben-Zeev R., Lehavi-Regev D., Katz M. N., Pevsner-Fischer M., Gertler A., Halpern Z., Harmelin A., Aamar S., Serradas P., Grosfeld A., Shapiro H., Geiger B., Elinav E., Hyperglycemia drives intestinal barrier dysfunction and risk for enteric infection. Science 359, 1376–1383 (2018). [DOI] [PubMed] [Google Scholar]
- 26.Diaz Heijtz R., Keane L., Koren O., Early-life sensitive periods for antibiotic-induced shifts in neuro-immune developmental trajectories and vulnerability to brain disorders. Brain Behav. Immun. 114, 78–79 (2023). [DOI] [PubMed] [Google Scholar]
- 27.Uzan-Yulzari A., Turta O., Belogolovski A., Ziv O., Kunz C., Perschbacher S., Neuman H., Pasolli E., Oz A., Ben-Amram H., Kumar H., Ollila H., Kaljonen A., Isolauri E., Salminen S., Lagström H., Segata N., Sharon I., Louzoun Y., Ensenauer R., Rautava S., Koren O., Neonatal antibiotic exposure impairs child growth during the first six years of life by perturbing intestinal microbial colonization. Nat. Commun. 12, 443 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stocker M., Klingenberg C., Navér L., Nordberg V., Berardi A., el Helou S., Fusch G., Bliss J. M., Lehnick D., Dimopoulou V., Guerina N., Seliga-Siwecka J., Maton P., Lagae D., Mari J., Janota J., Agyeman P. K. A., Pfister R., Latorre G., Maffei G., Laforgia N., Mózes E., Størdal K., Strunk T., Giannoni E., Less is more: Antibiotics at the beginning of life. Nat. Commun. 14, 2423 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ryu A. H., Eckalbar W. L., Kreimer A., Yosef N., Ahituv N., Use antibiotics in cell culture with caution: Genome-wide identification of antibiotic-induced changes in gene expression and regulation. Sci. Rep. 7, 7533 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chang J. T., Pathophysiology of inflammatory bowel diseases. N. Engl. J. Med. 383, 2652–2664 (2020). [DOI] [PubMed] [Google Scholar]
- 31.Krigul K. L., Feeney R. H., Wongkuna S., Aasmets O., Holmberg S. M., Andreson R., Puértolas-Balint F., Pantiukh K., Sootak L., Org T., Tenson T., Org. E., Schroeder B. O., A history of repeated antibiotic usage leads to microbiota-dependent mucus defects. Gut Microbes 16, 2377570 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bamias G., Arseneau K. O., Cominelli F., Mouse models of inflammatory bowel disease for investigating mucosal immunity in the intestine. Curr. Opin. Gastroenterol. 33, 411–416 (2017). [DOI] [PubMed] [Google Scholar]
- 33.Kiesler P., Fuss I. J., Strober W., Experimental models of inflammatory bowel diseases. Cell. Mol. Gastroenterol. Hepatol. 1, 154–170 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Telpaz S., Bel S., Autophagy in intestinal epithelial cells prevents gut inflammation. Trends Cell Biol. 33, 817–819 (2023). [DOI] [PubMed] [Google Scholar]
- 35.S. Modilevsky, M. Naama, S. Bel, “Goblet and Paneth cells: Producers of the intestinal barrier” in Encyclopedia of Cell Biology, R. A. Bradshaw, G. W. Hart, P. D. Stahl, Eds. (Academic Press, ed. 2, 2023), pp. 66–71; www.sciencedirect.com/science/article/pii/B9780128216187001401. [Google Scholar]
- 36.Hernández-Chirlaque C., Aranda C. J., Ocón B., Capitán-Cañadas F., Ortega-González M., Carrero J. J., Suárez M. D., Zarzuelo A., Sánchez de Medina F., Martínez-Augustin O., Germ-free and antibiotic-treated mice are highly susceptible to epithelial injury in DSS colitis. J. Crohns Colitis 10, 1324–1335 (2016). [DOI] [PubMed] [Google Scholar]
- 37.Bel S., Elkis Y., Lerer-Goldstein T., Nyska A., Shpungin S., Nir U., Loss of TMF/ARA160 protein renders colonic mucus refractory to bacterial colonization and diminishes intestinal susceptibility to acute colitis. J. Biol. Chem. 287, 25631–25639 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang X., Jonassen I., RASflow: An RNA-Seq analysis workflow with Snakemake. BMC Bioinformatics 21, 110 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kim D., Paggi J. M., Park C., Bennett C., Salzberg S. L., Graph-based genome alignment and genotyping with HISAT2 and HISAT-genotype. Nat. Biotechnol. 37, 907–915 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liao Y., Smyth G. K., Shi W., featureCounts: An efficient general purpose program for assigning sequence reads to genomic features. Bioinformatics 30, 923–930 (2014). [DOI] [PubMed] [Google Scholar]
- 41.Teichman G., Cohen D., Ganon O., Dunsky N., Shani S., Gingold H., Rechavi O., RNAlysis: Analyze your RNA sequencing data without writing a single line of code. BMC Biol. 21, 74 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen E. Y., Tan C. M., Kou Y., Duan Q., Wang Z., Meirelles G. V., Clark N. R., A. Ma’ayan, Enrichr: Interactive and collaborative HTML5 gene list enrichment analysis tool. BMC Bioinformatics 14, 128 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kuleshov M. V., Jones M. R., Rouillard A. D., Fernandez N. F., Duan Q., Wang Z., Koplev S., Jenkins S. L., Jagodnik K. M., Lachmann A., McDermott M. G., Monteiro C. D., Gundersen G. W., Ma’ayan A., Enrichr: A comprehensive gene set enrichment analysis web server 2016 update. Nucleic Acids Res. 44, W90–W97 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xie Z., Bailey A., Kuleshov M. V., Clarke D. J. B., Evangelista J. E., Jenkins S. L., Lachmann A., Wojciechowicz M. L., Kropiwnicki E., Jagodnik K. M., Jeon M., Ma’ayan A., Gene set knowledge discovery with Enrichr. Curr. Protoc. 1, e90 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gustafsson J. K., Ermund A., Johansson M. E. V., Schütte A., Hansson G. C., Sjövall H., An ex vivo method for studying mucus formation, properties, and thickness in human colonic biopsies and mouse small and large intestinal explants. Am. J. Physiol. Gastroint Liver Physiol. 302, G430–G438 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Propheter D. C., Chara A. L., Harris T. A., Ruhn K. A., Hooper L. V., Resistin-like molecule β is a bactericidal protein that promotes spatial segregation of the microbiota and the colonic epithelium. Proc. Natl. Acad. Sci. U. S. A. 114, 11027–11033 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figs. S1 to S3