Abstract
Background.
Globally, noroviruses cause infections year-round but have recognized winter seasonality in the Northern Hemisphere and yearly variations in incidence. With candidate norovirus vaccines in development, understanding temporal and geographic trends in norovirus disease is important to inform potential vaccination strategies and evaluate vaccine impact.
Methods.
We analyzed data from the National Outbreak Reporting System (NORS) and CaliciNet on single-state norovirus outbreaks that occurred during August 2009–July 2019 in the contiguous United States. We defined norovirus season onset and offset as the weeks by which 10% and 90% of norovirus outbreaks in a surveillance year occurred, respectively, and duration as the difference in weeks between onset and offset. We compared norovirus seasons across surveillance years and geographic regions.
Results.
During August 2009–July 2019, 24 995 single-state norovirus outbreaks were reported to NORS and/or CaliciNet. Nationally, the median norovirus season duration was 24 weeks, with onset occurring between October and December and offset occurring between April and May. Across all years combined, we observed a west-to-east trend in seasonality, with the earliest onset (October) and latest offset (May) occurring in western regions and the latest onset (December) and earliest offset (April) occurring in northeastern regions.
Conclusions.
Timing and duration of the US norovirus season varied annually but generally occurred during October–May. Norovirus wintertime seasonality was less distinct in western regions and was progressively more pronounced moving east. Further understanding the drivers of spatiotemporal dynamics of norovirus could provide insights into factors that promote virus transmission and help guide future interventions.
Keywords: norovirus, seasonality, acute gastroenteritis, surveillance
Noroviruses are the leading cause of acute gastroenteritis among all ages in the United States [1]. Noroviruses are genetically diverse viruses and can be grouped into 10 genogroups and at least 49 genotypes [2], although variants of GII.4 norovirus have caused the majority of illnesses worldwide since 2001 [3]. Virus transmission can occur through multiple routes including ingestion of aerosolized vomitus, direct contact with an infected person, consumption of contaminated food or water, or contact with contaminated environmental surfaces [4, 5]. Gaps remain in our understanding of duration of immunity after norovirus infection. Modeling studies have suggested that immunity can last between 4 and 9 years [6], while other studies suggest a much shorter duration of immunity of 2 months–2 years [7]. On average, each person in the United States is estimated to experience 5 norovirus episodes during his or her lifetime [1].
Noroviruses circulate year-round but have a recognized seasonal pattern in the Northern Hemisphere, with norovirus cases peaking during the winter months (December–February) [8]. However, factors that contribute to this pattern are not well understood. Previous studies have suggested that norovirus activity can be influenced by climatic factors, with increases in norovirus transmission associated with both cold, dry temperatures [9] and rainfall [8, 10]. Transmission may further be mediated by host behavioral factors such as time spent indoors with other individuals, as often occurs during periods of colder and wetter conditions, and by circulation of new GII.4 variants [9].
As several candidate norovirus vaccines are currently in development [11], it is important to characterize seasonal, temporal, and geographic patterns in norovirus disease in order to evaluate potential vaccine impacts and inform vaccination strategies, including timing of vaccination. Here, we describe trends in norovirus disease in the United States based on an analysis of 10 years of outbreak data.
METHODS
Data for this study were extracted from 2 surveillance systems that were launched in 2009 by the US Centers for Disease Control and Prevention (CDC). The National Outbreak Reporting System (NORS) is used by state, local, and territorial health departments in the United States to voluntarily report to CDC all foodborne and waterborne outbreaks, as well as enteric outbreaks transmitted through contact with infected people, animals, and contaminated environmental surfaces or by an unknown mode of transmission. CaliciNet is a national laboratory surveillance network that collects data on confirmed norovirus outbreaks in the United States. Outbreaks in both CaliciNet and NORS are defined as ≥2 cases of illness associated with a common exposure (eg, food, setting). Health departments may report outbreaks to NORS, CaliciNet, or both systems, as applicable. Reports in NORS and CaliciNet can be linked using a common identifier to provide more complete data on norovirus outbreaks. We extracted epidemiologic data on 18 March 2021 for all suspected (<2 laboratory-confirmed norovirus cases) and confirmed (≥2 laboratory-confirmed norovirus cases) norovirus outbreaks spread by any mode of transmission and reported to NORS with onset of the first illness occurring from 1 August 2009 through 31 July 2019. Data on all confirmed norovirus outbreaks during the same time were extracted from CaliciNet. Reports were linked and de-duplicated.
Outbreaks were assigned to an August through July surveillance year according to date of onset of the first reported illness and categorized into 52 epidemiologic weeks (EW), with the first EW of each surveillance year starting on 1 August. Seasonal parameters were defined previously by Rha et al [12]. Norovirus season onset was defined as the EW by which 10% of all norovirus outbreaks for that surveillance year had occurred, and season offset was defined as the EW by which 90% of norovirus outbreaks had occurred. Season duration was thus the difference in weeks between season onset and offset during which approximately 80% of outbreaks in the surveillance year occurred. We used season duration as the primary indicator of season strength, or the increase in norovirus activity during certain months of the year, with shorter seasons representing a greater clustering of outbreaks over a shorter period of time. The peak week was the first EW of each season during which the highest number of norovirus outbreaks occurred. We also used a peak-to-mean ratio, defined as a ratio of the number of outbreaks that had occurred during the peak week to the mean number of outbreaks that had occurred per week to serve as a secondary indicator of season strength.
As we sought to examine geographical trends in norovirus outbreak activity, outbreaks included in this analysis were limited to those that occurred in a single state within the 48 contiguous United States and the District of Columbia; multistate outbreaks were excluded. To examine differences in spatiotemporal dynamics from season to season, outbreak data from all included states were analyzed together by surveillance year. Data from all surveillance years were then combined and analyzed by region1 to examine geographic variations in norovirus outbreak activity across time. Regions were defined as the following: Mid-Atlantic: Delaware, Maryland, New Jersey, Pennsylvania, Virginia, Washington, DC, West Virginia; Northeast: Connecticut, Maine, Massachusetts, New Hampshire, New York, Rhode Island, Vermont; Midwest: Illinois, Indiana, Michigan, Ohio; Northwest: Idaho, Montana, Oregon, Washington, Wyoming; Midcentral: Minnesota, North Dakota, South Dakota, Wisconsin; Southcentral: Arkansas, Colorado, Iowa, Kansas, Louisiana, Missouri, Nebraska, New Mexico, Oklahoma, Texas; Southeast: Alabama, Florida, Georgia, Kentucky, Mississippi, North Carolina, South Carolina, Tennessee; and West: Arizona, California, Nevada, Utah. Regional groupings were based on proximity and were developed to evenly distribute the number of reports per region and allow for more stable estimates of seasonality indicators.
Sensitivity analyses were conducted to examine potential areas for surveillance bias and examine potential factors contributing to seasonal patterns by repeating analyses after restricting the dataset to outbreaks within certain strata: outbreaks reported to NORS and/or CaliciNet during 1 August 2012–31 July 2019, outbreaks reported to NORS (excluding those that were only reported to CaliciNet), outbreaks spread via person-to-person transmission, foodborne outbreaks, confirmed norovirus outbreaks, confirmed norovirus outbreaks with a GII.4 capsid (GII.4 norovirus outbreaks), and confirmed norovirus outbreaks with a non-GII.4 capsid (non-GII.4 norovirus outbreaks). We also examined an alternate regional grouping developed by the US National Oceanic and Atmospheric Administration, known as the Climate Extremes Index (CEI) [13]. All analyses were conducted in SAS version 9.4 (SAS Institute, Cary, NC) and ArcGIS (ESRI, Redlands, CA).
RESULTS
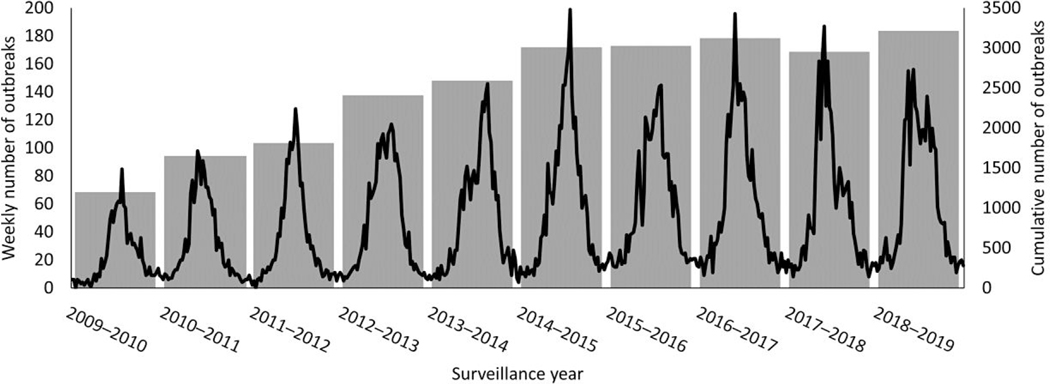
During 1 August 2009–31 July 2019, 24995 norovirus outbreaks were reported to NORS (16707 outbreaks), CaliciNet (3721 outbreaks), or both systems (4567 outbreaks) from the 48 contiguous United States and the District of Columbia. In total, 8409 (33.6%) outbreaks were confirmed due to norovirus. Outbreaks were predominantly spread through person-to-person transmission (19 031, 76.1%), with 3448 outbreaks (13.8%) spread by foodborne transmission and 83 outbreaks (0.33%) spread through environmental contamination or waterborne transmission. The mode of transmission was not determined for 2433 outbreaks (9.7%). The number of reported outbreaks ranged from 1201 during the 2009–2010 surveillance year to 3215 reported during the 2018–2019 surveillance year, with a median of 2773 outbreaks reported per surveillance year (Figure 1).
Figure 1.
Reported norovirus outbreaks by epidemiologic week and surveillance year, United States, August 2009–July 2019. The weekly number of outbreaks is represented by the line and presented on the left y-axis. The cumulative number of outbreaks reported each surveillance year is represented by the gray bars and presented on the right y-axis.
National norovirus season duration varied by surveillance year (Table 1). The median season duration was approximately 24 weeks (range, 22–28). National season onset occurred earliest (week of October 31) during the 2010–2011, 2015–2016, 2017–2018, and 2018–2019 surveillance years and latest (week of December 12) during the 2009–2010 surveillance year. National season offset occurred earliest (week of April 10) during the 2010–2011 surveillance year and latest (week of May 15) during the 2009–2010 surveillance year. The median peak week occurred during mid-February, with a range from late December to late March.
Table 1.
National Norovirus Season Characteristics by Surveillance Year, United States, 2009–2019
| Surveillance Year | Onset Week | Peak Week | Offset Week | Season Duration, Weeks | Number of Reported Norovirus Outbreaks | Peak-to-Mean Ratio |
|---|---|---|---|---|---|---|
| 2009–2010 | December 12 | February 20 | May 15 | 23 | 1201 | 3.7 |
| 2010–2011 | October 31 | December 26 | April 10 | 24 | 1651 | 3.1 |
| 2011–2012 | November 21 | January 30 | April 17 | 22 | 1814 | 3.7 |
| 2012–2013 | November 14 | February 27 | April 17 | 23 | 2408 | 2.5 |
| 2013–2014 | November 28 | March 27 | May 8 | 24 | 2593 | 2.9 |
| 2014–2015 | November 21 | February 27 | May 1 | 24 | 3012 | 3.4 |
| 2015–2016 | October 31 | March 6 | May 8 | 28 | 3026 | 2.5 |
| 2016–2017 | October 31 | January 2 | April 24 | 26 | 3122 | 3.3 |
| 2017–2018 | October 31 | January 2 | April 24 | 26 | 2953 | 3.3 |
| 2018–2019 | November 7 | January 2 | April 24 | 25 | 3215 | 2.5 |
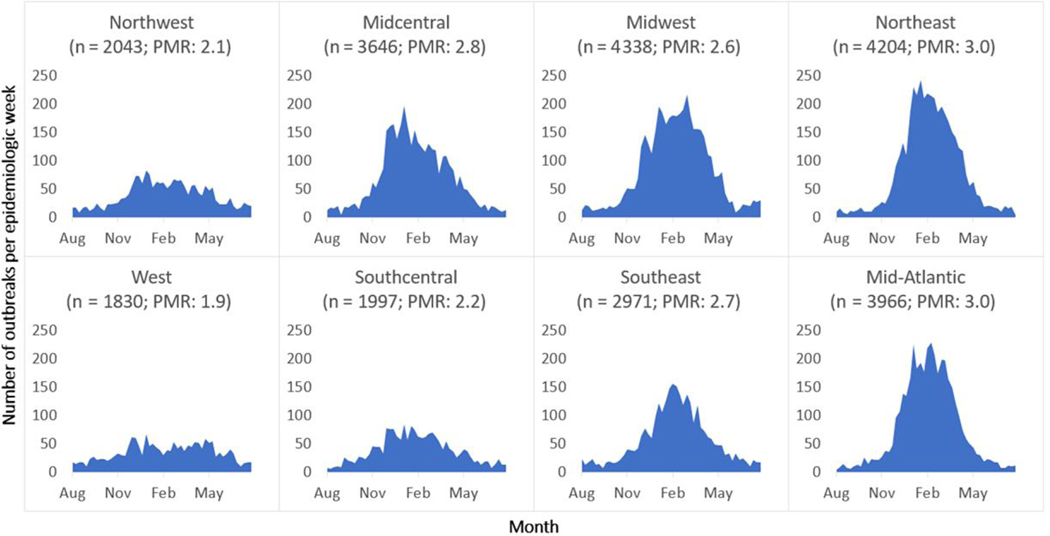
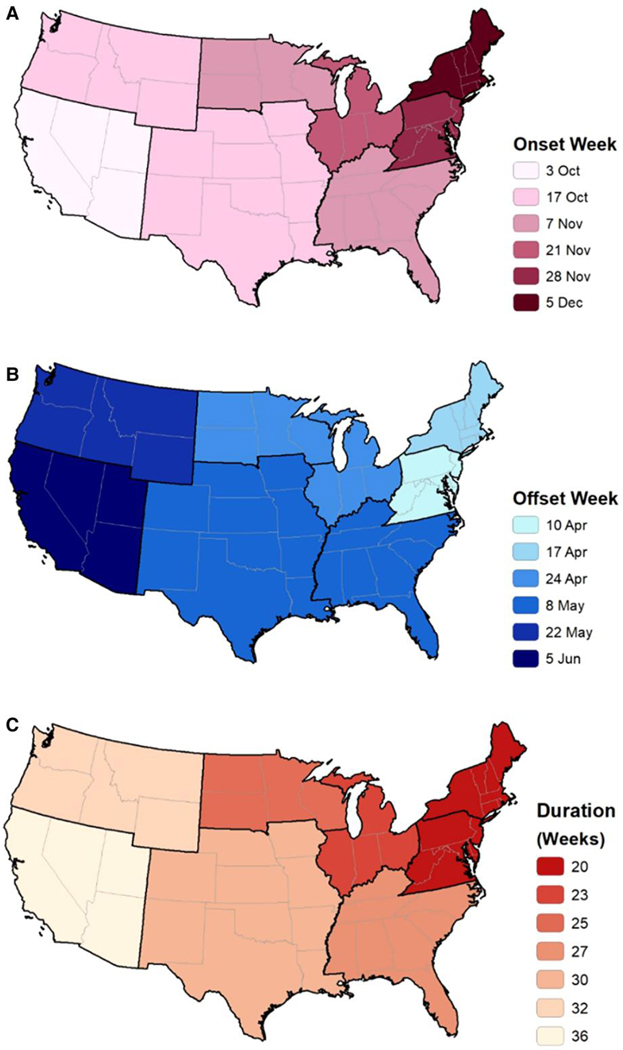
When examined by region across all surveillance years combined, norovirus wintertime seasonality was most distinct, with 80% of outbreaks clustering over a duration of 20 weeks and a peak-to-mean ratio of 3.0 in the eastern regions, specifically the Northeast and Mid-Atlantic (Figure 2, Figure 3C). This seasonality became less distinct moving westward, with the longest season duration (36 weeks) and lowest peak-to-mean ratio (1.9) in the West. The earliest norovirus season onset occurred in the western states during the week starting October 3 and occurred progressively later moving east, with the season starting latest in the Northeast region during the week starting December 5 (Figure 3A). Season offset first occurred in the Mid-Atlantic region during the week starting April 10 and occurred progressively later moving west, with the season ending latest in the West region during the week of June 5 (Figure 3B). While peak activity did not follow a distinct geographical pattern, the peak week occurred between the week starting December 26 and the week starting February 27 in all regions.
Figure 2.
Epidemiologic curves of norovirus outbreak activity by region, United States, August 2009–July 2019. The number of outbreaks are reported by epidemiologic week (listed by month) among all years, from 2009–2019. Regions are presented in approximate geographic order, along with the total number of outbreaks reported per region and PMR. Abbreviation: PMR, peak-to-mean ratio.
Figure 3.
Norovirus outbreak season onset (A), offset (B), and duration (C) by region, United States, August 2009–July 2019.
Sensitivity analyses that limited norovirus outbreaks to those reported during August 2012–July 2019, those reported to NORS, those spread by person-to-person transmission, and those that were laboratory-confirmed as norovirus all indicated the same overall pattern; seasonality was strongest in in the northeastern states and became progressively less distinct moving west (Supplementary Appendix). This pattern in seasonality was also visible when all outbreaks grouped into CEI regions were examined. When stratified by genotype, laboratory-confirmed GII.4 norovirus outbreaks had stronger seasonality than non-GII.4 norovirus outbreaks, though geographical patterns in seasonality were less evident. Similarly, when limited to norovirus outbreaks spread via foodborne transmission, season strength was overall less distinct and did not follow a discernible geographic pattern (Supplementary Appendix).
DISCUSSION
Our findings in this analysis of nearly 25 000 norovirus outbreaks indicate that the timing and duration of the norovirus season in the United States varies annually but generally occurs during October–May. The seasonal increase in prevalence of norovirus activity during the winter months also varies geographically; seasonality is less pronounced in western regions and is progressively more distinct moving east. These findings were not impacted by limiting observations to those reported to NORS, those that had a laboratory-confirmed etiology of norovirus, and those outbreaks spread through person-to-person transmission. These results also remained consistent after regional groupings were varied. However, the spatiotemporal pattern in norovirus seasonality was not apparent when limited to those outbreaks spread by foodborne transmission, nor when stratified by genotype. This may indicate that the spatiotemporal trends are driven, at least in part, by person-to-person transmission, which comprises the majority of norovirus outbreak transmissions [5].
Nationally, the number of reported norovirus outbreaks increased steadily during the 5 years after inception of NORS in 2009 and stabilized during the 2014–2015 surveillance year. As previously described, the increase in outbreaks reported from 2009 to 2014 may be generally attributable to improvements to the NORS platform and outreach efforts to expand reporting, including the inception of an enhanced surveillance network in 2012 [14, 15]. Our findings were not impacted by these shifts in reporting, as evidenced by our sensitivity analysis that limited data to outbreak reporting after 2012.
National norovirus season duration also varied, with the longest norovirus season occurring during the 2015–2016 surveillance year. While our study did not specifically assess the impact of emerging or predominantly circulating norovirus types on norovirus outbreak incidence, it should be noted that the GII.4 Sydney[P31] variant emerged during the 2012–2013 surveillance year and the GII.4 Sydney[P16] variant emerged during the 2015–2016 surveillance year [2, 16]. Previous studies have suggested that emergence of new GII.4 variants can contribute to increased norovirus activity and contribute to seasonal changes as a result of decreased population immunity to the new variant [9, 17]. While we found that the 2015–2016 norovirus season was longer than other surveillance years, the peak-to-mean ratio and number of reported norovirus outbreaks reported during the 2012–2013 and 2015–2016 surveillance years were generally similar to those from other surveillance years, consistent with previous analyses that did not find associations between emergence of GII.4 Sydney[P31] and GII.4 Sydney[P16] and the severity or magnitude of norovirus outbreaks in the United States [18, 19].
Though wintertime seasonality of norovirus has been well established in the temperate Northern Hemisphere [8], our findings suggest that this seasonal pattern is not uniform across the United States. States in the West, Northwest, and Southcentral regions had weaker, less distinct seasonality compared with states in the Midwest, Mid-Atlantic, and Northeast regions. An apparent lack of seasonal pattern has been described in other studies conducted in relatively warmer regions including Peru [20] and on the African continent [21], further reinforcing the need for additional research on factors that contribute to transmission, such as temperature, humidity, and rainfall.
Variations in seasonal trends across the continental United States were similarly observed in prevaccine detections for rotavirus. Prior to the introduction and widespread use of the vaccine in 2006, rotavirus was the most common cause of severe gastroenteritis in children aged <5 years [22]. Peak rotavirus detections each year followed an eastward-moving trend, beginning in southwestern states from October–December and ending in the northeast from April–May [23, 24]. This pattern became less apparent in the 2 years following vaccine introduction, and studies have suggested that the pattern was driven by geographical variability in birth rates, leading to accumulation of susceptible individuals (ie, newborns) in the population [25, 26]. However, unlike rotavirus, which predominantly affects children [27], norovirus infections occur among persons of all ages, and reinfections can occur multiple times during a lifetime [1].
Our findings should be interpreted within the context of some limitations. First, reporting to both NORS and CaliciNet is voluntary and may thus represent an underestimate of true norovirus outbreak activity in the United States, the degree of which may vary by individual state reporting to each system. We attempted to address potential biases through sensitivity analyses, which largely confirmed our primary findings. The analysis also includes norovirus outbreak data reported from 48 states and the District of Columbia over a 10-year period, providing a robust dataset. Second, only about one-third of reported norovirus outbreaks were laboratory-confirmed. Though the remaining outbreaks were reported as suspected norovirus based on epidemiological and clinical evidence, it is possible that some outbreaks may have been caused by another epidemiologically similar pathogen, such as sapovirus [28]. Despite this, our findings remained consistent even when limited to confirmed norovirus outbreaks. Finally, this analysis was based on data reported through July 2019. During the COVID-19 pandemic and, specifically, beginning in March 2020, norovirus outbreak incidence in the United States dropped dramatically, disrupting typical seasonal patterns [29]. While additional years of surveillance data are needed to determine long-term effects of the pandemic on norovirus outbreak incidence, these data provide a baseline for understanding these impacts.
The results of this analysis suggest that while norovirus outbreaks typically occur most frequently during the winter months in the United States, the specific timing of elevated norovirus activity and corresponding need for enhanced prevention measures may vary by region. Continued surveillance, particularly in the context of the coronavirus disease 2019 pandemic, and further understanding of the spatiotemporal dynamics of norovirus could provide insights into factors that promote virus transmission and help guide future norovirus prevention strategies, including seasonal education campaigns and vaccinations.
Supplementary Material
Acknowledgments.
The authors thank the state, local, and territorial health departments that report to the National Outbreak Reporting System and CaliciNet.
Financial support.
This work was supported by the US Centers for Disease Control and Prevention.
Disclaimer.
The findings and conclusions presented here are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Potential conflicts of interest. The authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
References
- 1.Hall AJ, Lopman BA, Payne DC, et al. Norovirus disease in the United States. Emerg Infect Dis 2013; 19:1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chhabra P, de Graaf M, Parra GI, et al. Updated classification of norovirus genogroups and genotypes. J Gen Virol 2019; 100:1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Siebenga JJ, Vennema H, Zheng D-P, et al. Norovirus illness is a global problem: emergence and spread of norovirus GII. 4 variants, 2001–2007. J Infect Dis 2009; 200:802–12. [DOI] [PubMed] [Google Scholar]
- 4.Hall AJ, Vinjé J, Lopman B, et al. Updated norovirus outbreak management and disease prevention guidelines. Morb Mortal Wkly Rep 2011; 60:1–15. [PubMed] [Google Scholar]
- 5.Hall AJ, Wikswo ME, Manikonda K, Roberts VA, Yoder JS, Gould LH. Acute gastroenteritis surveillance through the National Outbreak Reporting System, United States. Emerg Infect Dis 2013; 19:1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Simmons K, Gambhir M, Leon J, Lopman B. Duration of immunity to norovirus gastroenteritis. Emerg Infect Dis 2013; 19:1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parrino TA, Schreiber DS, Trier JS, Kapikian AZ, Blacklow NR. Clinical immunity in acute gastroenteritis caused by Norwalk agent. N Eng J Med 1977; 297: 86–9. [DOI] [PubMed] [Google Scholar]
- 8.Ahmed SM, Lopman BA, Levy K. A systematic review and meta-analysis of the global seasonality of norovirus. PloS One 2013; 8:e75922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lopman B, Armstrong B, Atchison C, Gray JJ. Host, weather and virological factors drive norovirus epidemiology: time-series analysis of laboratory surveillance data in England and Wales. PloS One 2009; 4:e6671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bruggink LD, Marshall JA. The incidence of norovirus-associated gastroenteritis outbreaks in Victoria, Australia (2002–2007) and their relationship with rainfall. Int J Environ Res Pub Health 2010; 7:2822–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cates JE, Vinjé J, Parashar U, Hall AJ. Recent advances in human norovirus research and implications for candidate vaccines. Expert Rev Vaccines 2020; 19: 539–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rha B, Burrer S, Park S, Trivedi T, Parashar UD, Lopman BA. Emergency department visit data for rapid detection and monitoring of norovirus activity, United States. Emerg Infect Dis 2013; 19:1214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Oceanic and Atmospheric Administration. US Climate Extremes Index (CEI). Available at: <https://www.ncei.noaa.gov/access/monitoring/cei/>. Accessed 18 March 2021.
- 14.Wikswo ME, Kambhampati A, Shioda K, Walsh KA, Bowen A, Hall AJ. Outbreaks of acute gastroenteritis transmitted by person-to-person contact, environmental contamination, and unknown modes of transmission—United States, 2009–2013. Morb Mortal Wkly Rep 2015; 64:1–16. [DOI] [PubMed] [Google Scholar]
- 15.Shah MP, Wikswo ME, Barclay L, et al. Near real-time surveillance of US norovirus outbreaks by the Norovirus Sentinel Testing and Tracking Network—United States, August 2009–July 2015. Morb Mortal Wkly Rep 2017; 66:185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cannon JL, Barclay L, Collins NR, et al. Genetic and epidemiologic trends of norovirus outbreaks in the United States from 2013 to 2016 demonstrated emergence of novel GII. 4 recombinant viruses. J Clin Microbiol 2017; 55:2208–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Van Beek J, Ambert-Balay K, Botteldoorn N, et al. Indications for worldwide increased norovirus activity associated with emergence of a new variant of genotype II. 4, late 2012. Eurosurveillance 2013; 18:20345. [PubMed] [Google Scholar]
- 18.Barclay L, Cannon JL, Wikswo ME, et al. Emerging novel GII. P16 noroviruses associated with multiple capsid genotypes. Viruses 2019; 11:535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leshem E, Wikswo M, Barclay L, et al. Effects and clinical significance of GII. 4 Sydney norovirus, United States, 2012–2013. Emerg Infect Dis 2013; 19:1231–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Romero C, Tinoco YO, Loli S, et al. Incidence of norovirus-associated diarrhea and vomiting disease among children and adults in a community cohort in the Peruvian Amazon basin. Clin Infect Dis 2017; 65:833–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mans J, Armah GE, Steele AD, Taylor MB. Norovirus epidemiology in Africa: a review. PLoS One 2016; 11:e0146280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cortese MM, Parashar UD. Prevention of rotavirus gastroenteritis among infants and children: recommendations of the Advisory Committee on Immunization Practices (ACIP). Morb Mortal Wkly Rep 2009; 58:1–25. [PubMed] [Google Scholar]
- 23.Török TJ, Kilgore PE, Clarke MJ, Holman RC, Bresee JS, Glass RI. Visualizing geographic and temporal trends in rotavirus activity in the United States, 1991 to 1996. Pediatr Infect Dis J 1997; 16:941–6. [DOI] [PubMed] [Google Scholar]
- 24.Turcios RM, Curns AT, Holman RC, et al. Temporal and geographic trends of rotavirus activity in the United States, 1997–2004. Pediatr Infect Dis J 2006; 25:451–4. [DOI] [PubMed] [Google Scholar]
- 25.Pitzer VE, Viboud C, Lopman BA, Patel MM, Parashar UD, Grenfell BT. Influence of birth rates and transmission rates on the global seasonality of rotavirus incidence. J R Soc Interface 2011; 8:1584–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Curns AT, Panozzo CA, Tate JE, et al. Remarkable postvaccination spatiotemporal changes in United States rotavirus activity. Pediatr Infect Dis J 2011; 30:S54–5. [DOI] [PubMed] [Google Scholar]
- 27.Baker JM, Dahl RM, Cubilo J, Parashar UD, Lopman BA. Effects of the rotavirus vaccine program across age groups in the United States: analysis of national claims data, 2001–2016. BMC Infect Dis 2019; 19:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mattison CP, Dunn M, Wikswo ME, et al. Non-norovirus viral gastroenteritis outbreaks reported to the National Outbreak Reporting System, USA, 2009–2018. Emerg Infect Dis 2021; 27:560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kraay AN, Han P, Kambhampati AK, Wikswo ME, Mirza SA, Lopman BA. Impact of nonpharmaceutical interventions for severe acute respiratory syndrome coronavirus 2 on norovirus outbreaks: an analysis of outbreaks reported by 9 US states. J Infect Dis 2021; 224:9–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.