Abstract
Purpose
Traditionally, bilateral urolithiasis treatment involved staged interventions due to safety concerns. Recent studies have shown that same-sitting bilateral retrograde intrarenal surgery (SSB-RIRS) is effective, with acceptable complication rates. However, there’s no clear data on the optimum laser for the procedure. This study aimed to assess outcomes of SSB-RIRS comparing thulium fiber laser (TFL) and high-power holmium:yttrium-aluminum-garnet (Ho:YAG) laser in a multicenter real-world practice.
Materials and Methods
Retrospective analysis was conducted on patients undergoing SSB-RIRS from January 2015 to June 2022 across 21 centers worldwide. Three months perioperative and postoperative outcomes were recorded, focusing on complications and stone-free rates (SFR).
Results
A total of 733 patients were included, with 415 in group 1 (Ho:YAG) and 318 in group 2 (TFL). Both groups have similar demographic and stone characteristics. Group 1 had more incidence of symptomatic pain or hematuria (26.5% vs. 10.4%). Operation and lasing times were comparable. The use of baskets was higher in group 1 (47.2% vs. 18.9%, p<0.001). Postoperative complications and length of hospital stay were similar. Group 2 had a higher overall SFR. Multivariate regression analysis indicated that age, presence of stone at the lower pole, and stone diameter were associated with lower odds of being stone-free bilaterally, while TFL was associated with higher odds.
Conclusions
Our study shows that urologists use both lasers equally for SSB-RIRS. Reintervention rates are low, safety profiles are comparable, and single-stage bilateral SFR may be better in certain cases. Bilateral lower pole and large-volume stones have higher chances of residual fragments.
Keywords: Endoscopy, Laser, Ureteroscopy, Urinary tract stones, Urolithiasis
Graphical Abstract
INTRODUCTION
The worldwide incidence of nephrolithiasis has significantly risen over the past twenty years [1]. According to research by Boyce et al. [2], 10% of patients with asymptomatic renal stone disease presented with stones in both kidneys. It has been observed that up to one-third of asymptomatic kidney stones eventually necessitate medical intervention [3], and those with bilateral stones face a heightened risk of recurrence and the need for surgical procedures [4].
Traditionally, the treatment of bilateral kidney stones involved staged interventions due to safety concerns associated with increased complications when performing simultaneous bilateral surgeries. Castellani et al. [5] have shown that same-sitting bilateral retrograde intrarenal surgery (SSB-RIRS) is an effective treatment method for patients with bilateral kidney stones, with an acceptable complication rate of fever/infection needing prolonged stay (5.5%), sepsis (2%), and blood transfusion (1.3%).
Urologists have recently faced the introduction of new lasers for lithotripsy, each with its own proprieties. Particularly, the new high-power lasers, such as thulium fiber laser (TFL), have shown potential for better stone-free rate (SFR) and more efficient fragmentation rate as compared to the holmium:yttrium-aluminum-garnet (Ho:YAG) laser [6,7]. Moreover, there are discordant outcomes of studies comparing high-power Ho:YAG versus TFL in renal and ureteral lithotripsy. A randomized study showed no difference in terms of SFR and complications [8], whilst a real-life retrospective study using propensity score matching demonstrated higher SFR for TFL [9].
In the clinical scenario of bilateral renal stones being managed under the same sitting, no clear data is indicating if TFL outperforms high-power/pulse-modulated Ho:YAG lasers. Comparative studies assessing outcomes of SSB-RIRS using Ho:YAG laser and TFL are currently lacking. Hence, we aimed to assess the outcomes of SSB-RIRS comparing TFL and high-power Ho:YAG laser in a multicenter real-world practice.
MATERIALS AND METHODS
As part of the Team of Worldwide Endourological Researchers of the Endourological Society (TOWER), a retrospective analysis was conducted on all consecutive patients who underwent SSB-RIRS for renal stones from January 2015 to June 2022 across 21 centers worldwide. The consultant surgeons who contributed data for this study had extensive experience, each having performed over 100 RIRS procedures.
The inclusion criteria for the study were patients aged 18 years and older, with bilateral kidney stones of any size and location, diagnosed due to unilateral or bilateral symptomatic presentation who underwent bilateral RIRS under the same anaesthesia with either TFL or high power Ho:YAG lasers (>60 W or Ho:YAG laser with Moses technology). Exclusion criteria comprised cases involving concomitant ureteral lithotripsy, stones located in a calyceal diverticulum, anomalous kidney, and in-tandem procedures like RIRS performed as part of a joint procedure for endoscopic combined intrarenal surgery. Patients were categorized into two groups: group 1 included patients treated with the high-power Ho:YAG laser, while group 2 consisted of patients treated with TFL.
Stone size was determined based on the largest diameter measured in a preoperative non-contrast computed tomography (NCCT) scan, and in instances with multiple stones, data from the largest stone were reported. Antiplatelet and anticoagulant medications were discontinued at least 3–7 days before surgery and resumed according to each center’s protocol. Antibiotic prophylaxis was administered in each center with a single dose during surgery, selected based on local pathogen prevalence and antibiotic susceptibility profiles. Lithotripsy was performed using either the Ho:YAG laser or TFL, following the current standard RIRS technique [6]. Laser machines used were the Lumenis (Boston Scientific) high power >60 W holmium laser machine with and without MOSES technology or the Urolase 60 W (IPG Photonics) or Fibre dust (Quanta System) TFL machine.
Perioperative and postoperative outcomes up to 3 months were recorded for any complications and SFR. Any cases in which bilateral RIRS could not be completed and the reasons for same were also documented. Surgical time was measured from the start of cystoscopy to the placement of a bladder catheter. Sepsis was defined as “life-threatening organ dysfunction caused by a dysregulated host response to infection” [8]. SFR was evaluated within three months post-surgery using a NCCT scan and defined as the absence of any residual fragment (RF) larger than 3 mm and was independently assessed for each renal unit.
The study was approved by the institutional review board of the principle site: the Asian Institute of Nephrology and Urology (AINU #13/2022). Each participating center provided anonymized data and obtained approval from their respective institutional review boards if necessary. The written informed consent was waived due to the study’s retrospective design.
Categorical data are expressed as absolute numbers and percentages, while continuous data are reported as mean along with their standard deviations. To determine independent predictors of achieving bilateral stone-free status, univariate analysis was performed and factors associated with lower or higher odds of bilateral stone-free status were included in a multivariable logistic regression model. The results are presented as odds ratios (ORs) with 95% confidence intervals (CIs). Statistical significance was set as a two-tailed p-value of less than 0.05. All statistical tests were conducted using IBM SPSS software, version 25.0 (IBM Corp.).
RESULTS
Seven hundred thirty-three patients who fulfilled the criteria for inclusion were incorporated into the analysis. There were 415 patients (56.6%) in group 1, whilst group 2 comprised 318 patients (43.4%).
As this study assesses bilateral renal stone, a similar distribution for both groups was seen for age, sex proportion, or stone-related parameters such as stone diameter, Hounsfield units, stone location, and multiplicity (Table 1). However, patients in group 1 reportedly had a higher incidence of symptomatic pain or hematuria at presentation (26.5% vs. 10.4%) and there was a higher proportion of pre-stented patients (65.1% vs. 57.9%) in group 1. Additionally, a significantly higher proportion of recurrent stone formers was observed in group 1 (52.8% vs. 34.6%) (Table 1).
Table 1. Baseline characteristics.
| Group 1 (n=415) | Group 2 (n=318) | p-value | ||
|---|---|---|---|---|
| Age (y) | 50.1±16.5 | 45.4±15.4 | 0.810 | |
| Sex | ||||
| Male | 143 (34.5) | 103 (32.4) | 0.581 | |
| Female | 272 (65.5) | 215 (67.6) | 0.581 | |
| Presentation | <0.001* | |||
| Hematuria only | 64 (15.4) | 19 (6.0) | ||
| Pain only | 222 (53.5) | 196 (61.6) | ||
| Hematuria and pain | 110 (26.5) | 33 (10.4) | ||
| Incidental | 19 (4.6) | 70 (22.0) | ||
| Recurrent stone former | 219 (52.8) | 110 (34.6) | <0.001* | |
| Urine culture positive | 206 (49.6) | 161 (50.6) | 0.823 | |
| Pre-stented | 270 (65.1) | 184 (57.9) | <0.001* | |
| Preoperative antibiotics | 409 (98.6) | 314 (98.7) | 0.828 | |
| Stone parameters | ||||
| Left kidney stone size (mm) | 11.20±6.24 | 10.46±5.59 | 0.133 | |
| Right kidney stone size (mm) | 10.25±5.28 | 10.07±4.80 | 0.661 | |
| Hounsfield units | 1,095.54±373.37 | 1,045.39±378.77 | 0.860 | |
| Bilateral multiple stones | 175 (42.2) | 148 (46.5) | 0.312 | |
| Bilateral single stones | 131 (31.6) | 100 (31.4) | 0.972 | |
Values are presented as mean±standard deviation or number (%).
Group 1: patients treated with the high-power Ho:YAG laser, Group 2: patients treated with thulium fiber laser.
*p<0.05.
SSB-RIRS was mainly performed under general anaesthesia in both groups (Table 2). In the majority of patients, the utility of bilateral ureteral access sheath placement (UAS) was reportedly higher in group 2 (65.4% vs. 69.9%) but the difference did not reach statistical significance. Operation time and lasing time were comparable between both groups. The usage of baskets for either repositioning or retrieval of fragments post-laser lithotripsy was significantly higher in group 1 (47.2% vs. 18.9%, p<0.001).
Table 2. Operative characteristics.
| Group 1 (n=415) | Group 2 (n=318) | p-value | ||
|---|---|---|---|---|
| Spinal anesthesia | 6 (1.4) | 4 (1.3) | 0.828 | |
| UAS used on either side | 344 (82.9) | 283 (89.0) | 0.236 | |
| Bilateral UAS | 290 (69.9) | 208 (65.4) | 0.228 | |
| Reusable scope | 154 (37.1) | 234 (73.6) | <0.001* | |
| Stone basketing (for removal or relocation) | 196 (47.2) | 60 (18.9) | <0.001* | |
| Total operation time (min) | 76.49±28.77 | 74.17±25.98 | 0.286 | |
| Laser time (min) | 38.44±14.04 | 36.97±15.56 | 0.326 | |
Values are presented as number (%) or mean±standard deviation.
Group 1: patients treated with the high-power Ho:YAG laser, Group 2: patients treated with thulium fiber laser.
UAS, ureteral access sheath.
*p<0.05.
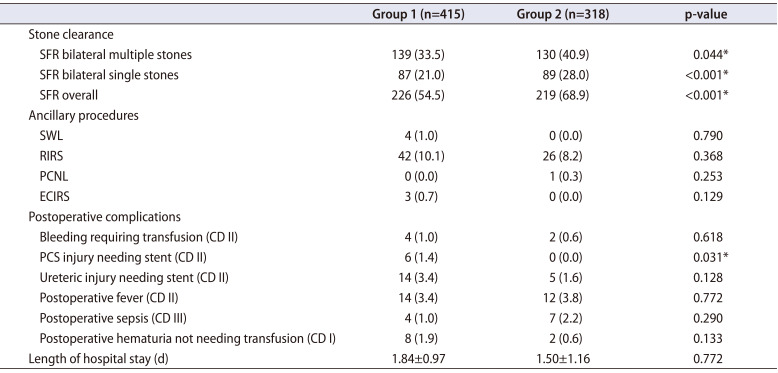
Postoperative complications are presented in Table 3. In group 1, six patients (1.4%) experienced pelvic-caliceal system (PCS) injuries that required prolonged stenting, whereas no patients in group 2 suffered PCS injuries. Other postoperative complications, including bleeding requiring transfusion, ureteric injury needing stenting, postoperative fever, postoperative sepsis, and postoperative hematuria not requiring transfusion, were similar between the groups, occurring at rates ranging from less than 1% to 4%. The length of hospital stay was comparable for both groups (1.84±0.97 days in group 1 and 1.50±1.16 days in group 2, p=0.772).
Table 3. Operative outcomes.
| Group 1 (n=415) | Group 2 (n=318) | p-value | ||
|---|---|---|---|---|
| Stone clearance | ||||
| SFR bilateral multiple stones | 139 (33.5) | 130 (40.9) | 0.044* | |
| SFR bilateral single stones | 87 (21.0) | 89 (28.0) | <0.001* | |
| SFR overall | 226 (54.5) | 219 (68.9) | <0.001* | |
| Ancillary procedures | ||||
| SWL | 4 (1.0) | 0 (0.0) | 0.790 | |
| RIRS | 42 (10.1) | 26 (8.2) | 0.368 | |
| PCNL | 0 (0.0) | 1 (0.3) | 0.253 | |
| ECIRS | 3 (0.7) | 0 (0.0) | 0.129 | |
| Postoperative complications | ||||
| Bleeding requiring transfusion (CD II) | 4 (1.0) | 2 (0.6) | 0.618 | |
| PCS injury needing stent (CD II) | 6 (1.4) | 0 (0.0) | 0.031* | |
| Ureteric injury needing stent (CD II) | 14 (3.4) | 5 (1.6) | 0.128 | |
| Postoperative fever (CD II) | 14 (3.4) | 12 (3.8) | 0.772 | |
| Postoperative sepsis (CD III) | 4 (1.0) | 7 (2.2) | 0.290 | |
| Postoperative hematuria not needing transfusion (CD I) | 8 (1.9) | 2 (0.6) | 0.133 | |
| Length of hospital stay (d) | 1.84±0.97 | 1.50±1.16 | 0.772 | |
Values are presented as number (%) or mean±standard deviation.
Group 1: patients treated with the high-power Ho:YAG laser, Group 2: patients treated with thulium fiber laser.
SFR was assessed 3 months after surgery according to local standard of care with non-contrast computed tomography, and was defined as absence of any residual fragment >3 mm.
SFR, stone-free rate; SWL, shock wave lithotripsy; RIRS, retrograde intrarenal surgery; PCNL, percutaneous nephrolithotripsy; ECIRS, endoscopic combined intrarenal surgery; CD, Clavien–Dindo classification; PCS, pelvic-caliceal system.
*p<0.05.
SFR is reported in Table 3. RF as reported on NCCT done anytime between 6 weeks to 3 months postoperatively were lesser in group 2. Group 2 patients had a higher overall SFR when cumulatively assessed for both kidneys whether it was for bilateral multiple stones (40.9% vs. 33.5%), or bilateral single stones (28.0% vs. 21.0%). Reintervention by redo RIRS for either 1 kidney or both kidneys within 3 months was reportedly 10.1% in group 1 versus 8.2% in group 2.
In multivariate analysis on factors affecting bilateral SFR, age (OR 0.979, 95% CI 0.965–0.994, p=0.006), presence of stone at the lower pole (OR 0.523, 95% CI 0.381–0.719, p<0.001), and stone diameter (OR 0.917, 95% CI 0.868–0.970, p=0.002) were factors associated with lower odds of being stone-free bilaterally in a single setting, while the use of TFL with higher odds (OR 1.686, 95% CI 1.021–2.784, p=0.041) (Table 4).
Table 4. MVA on factors affecting overall bilateral SFR.
| Bilateral SFR | OR (95% CI) | p-value |
|---|---|---|
| Age | 0.979 (0.965–0.994) | 0.006* |
| Pre-stenting | 1.049 (0.823–1.336) | 0.700 |
| Use of UAS | 0.953 (0.509–1.785) | 0.880 |
| Bilateral single stone | 0.902 (0.327–2.488) | 0.842 |
| Bilateral multiple stone | 0.756 (0.429–1.330) | 0.332 |
| Bilateral lower pole stone | 0.523 (0.381–0.719) | <0.001* |
| Stone diameter | 0.917 (0.868–0.970) | 0.002* |
| TFL | 1.686 (1.021–2.784) | 0.041* |
MVA, multivariate analysis; SFR, stone-free rate; OR, odds ratio; CI, confidence interval; UAS, ureteral access sheath; TFL, thulium fiber laser.
*p<0.05.
DISCUSSION
Since its launch in 2018 in Russia [9], TFL has gained significant popularity, challenging the long-standing gold standard, Ho:YAG laser [10,11], as an alternative choice for laser lithotripsy. Several prospective studies and systematic reviews with meta-analyses have since been conducted to compare Ho:YAG and TFL [6,12,13,14]. To our knowledge, this is the first study to specifically compare the safety and efficacy of these two lasers in SSB-RIRS procedures.
Traditionally, the approach to treating bilateral renal stones has been to address one kidney at a time in a staged manner [15]. Despite recent advancements in endourology, including the miniaturization of instruments and improvements in laser technology, clear guidelines for the management of bilateral renal stones remain lacking. This uncertainty precludes many surgeons from performing bilateral RIRS, as theoretically, it can double the risk of complications and may not achieve the desired bilateral SFR [16]. However, recent publications have demonstrated that SSB-RIRS is feasible and effective, with an acceptable rate of complications [3,5,16], even in carefully selected elderly populations [17].
In our cohort, group 1 had a higher proportion of patients who were symptomatic at initial presentation, with 15.4% experiencing hematuria and 26.5% experiencing both hematuria and pain. This symptomatic presentation likely contributed to the higher rate of pre-stenting in group 1 before definitive RIRS.
Intraoperative characteristics, including total operation and laser time, were similar between the two groups. Even though our study reports this for bilateral RIRS, interestingly this finding aligns with a recent systematic review meta-analysis (SRMA) investigating both lasers used for single-side RIRS that reported no significant differences in total laser time and operating time between these two lasers [12]. In our study, the use of reusable scope was higher with TFL (73.6% vs. 37.1%). We postulate that this is due to surgeon preference and differences across centers. However, two recent SRMAs have shown no differences in the SFR, operation time, length of hospital stay, and complication rate between reusable and disposable ureteroscopes [18,19]. The use of a stone basket to remove stone fragments and/or relocate stones for laser lithotripsy was significantly higher in group 1 (47.2% vs. 18.9%, p<0.001). This reduction in the need for a stone basket as an adjunct to stone removal when using TFL has also been observed in other SRMAs [13]. We acknowledge that with regards to baskets and accessories we can only report the utility, this definitely could be influenced by surgeons own bias and intraoperative decisions. However, this could also be related to the fact that the primary advantage of TFL lies in its versatility across various parameters, including pulse energies (range, 0.025–6 J), frequencies (up to 2,400 Hz), and a peak power [20] which generates twice the amount of dust and has 4 times more ablation efficiency compared to even high power Ho:YAG laser in generating lesser and smaller fragments during lithotripsy, making it an ideal laser for dusting [20,21,22]. Despite the large variance in energy and frequency levels for TFL, recent studies have shown that a low power setting of 10 W or less is effective and has a lower risk of thermal injury [23]. Regarding the safety data of TFL in terms of mucosal damage, we have reported that the complication rate of ureteric injury requiring a stent is lower among TFL users (1.6%) compared to Ho:YAG users (3.4%) despite this difference did not reach statistical significance. Regardless, we should also acknowledge that both lasers if used carelessly can cause mucosal damage and users must take every precaution to avoid this.
Perhaps these different laser setting might have contributed to the higher overall SFR achieved in group 2 in our series (68.9% vs. 54.5%, p<0.001). Similarly, when analyzing SFR for both bilateral multiple stones (40.9% vs. 33.5%) and single stone disease (28.0% vs. 21.0%), group 2 outperformed group 1 in achieving a higher stone-free status. The superior SFR associated with the use of TFL compared to the Ho:YAG Laser is supported by multiple studies. Uleri et al. [12] in their SRMA explained that the significantly better SFR of TFL is due to its ability to perform effective dusting, producing smaller fragments (the so-called “microdust”) and leaving no clinically significant RFs behind. This clinical effectiveness of TFL in achieving better SFR is also corroborated by earlier in vitro studies, which demonstrated that TFL produces higher ablation rates and smaller fragments compared to Ho:YAG across various settings [24]. As this is a retrospective study, some patients had an NCCT 6 weeks after and some only 3 months post primary RIRS. This could have influenced the reporting of overall SFR. Since a NCCT was uniformly used, it helped in more accurate reporting RFs in both groups. Most studies agree on 2–3 mm as an acceptable RF size to avoid reintervention. Hence, this study also chose strict criteria of 3 mm or smaller on either or both sides using a NCCT scan as the definition for being stone-free [25]. Using an NCCT scan is the current best imaging not only to measure RF but also is highly recommended before any reintervention is planned [26].
Although the SFR for SSB-RIRS was 54.5% in group 1 and 68.9% in group 2, the re-intervention rates remained low in both groups. The most common re-intervention procedure for residual stones was repeat RIRS, with rates of 10.1% in group 1 and 8.2% in group 2. These re-intervention rates are comparable to a recent global study on unilateral RIRS, which recorded a re-intervention rate of 11.17% among 6,669 patients [27]. Whilst the overall RF may suggest that SSB-RIRS is not a good surgery to achieve single-stage complete clearance, we feel that with properly timed imaging in the hands of sufficiently experienced urologists, this could be improved and we think this is an important aspect for future studies to focus upon.
Postoperative complications were comparable between both groups, except for mild PCS injury in six cases but in one kidney only. There were no bilateral PCS or ureteric injuries. All six injuries were recognised during surgery on a retrograde pyelogram and required prolonged stenting only. We attribute these complications to various procedural factors, including stone size, location, and stone density [28].
Our multivariate analysis revealed that age, the presence of bilateral lower pole stones, and larger stone size are factors that reduce the odds of achieving a high single-stage bilateral stone-free status when dealing with a same-sitting RIRS, whilst the use of TFL was associated with higher odds. We acknowledge that a lack of information on the settings used, and the inability to measure efficacy based on stone volume could be limitations. However, it is perhaps difficult to independently assess these factors and not feasible to easily infer these aspects when dealing with bilateral stones of different configurations and compositions being managed in the same sitting, unlike when done in a well-matched cohort for single-side RIRS.
The main limitation of this study is its retrospective nature. Hence, the choice of scope is entirely up to the treating physician, influenced by the available resources and the center’s practices. The variability in NCCT timing according to each center’s follow-up protocol is also a result of the retrospective nature of the study. As NCCT timing can influence the reporting of RF and it was done as per individual institutions protocol. However, on review with the centers in our study, all patients had NCCT after 6 weeks of index procedure. In view of the retrospective nature we could not gather data on exact timing of NCCT.
As the first study to compare the safety and efficacy of different high-power lasers in SSB-RIRS, it could serve as a prerequisite for initiating further prospective studies that could provide an in-depth comparison of the ideal laser type for SSB-RIRS. In our study, stone size was measured based on its maximum diameter and unfortunately we don’t have data on stone volume which is a better measure to understand laser efficacy. In future a prospective study evaluating different laser efficiency based on stone volume can perhaps overcome this limitation. However, considering this is a real-world study, it shows that TFL laser is equally comparable in safety and perhaps better than a high-power Ho:YAG laser for achieving bilateral stone-free status in patients undergoing SSB-RIRS. We must acknowledge that this study was performed only by sufficiently experienced urologists. Perhaps given this, a bilateral UAS was also preferred in both groups to avoid inadvertent damage due to increased intra-renal pressure or temperature when using high-power lasers [29]. As technology improves and suction aspiration shows much promise as a possible game changer in improving all aspects of RIRS, it will perhaps equally benefit surgeons doing SSB-RIRS [30].
CONCLUSIONS
Our real-world study shows that urologists are keen to use TFL as much as high-power Ho:YAG laser for SSB-RIRS. The reintervention rates are low, the safety profile is comparable, and single-stage bilateral SFR may be better in certain cases where stones are in a favourable position. Bilateral lower pole and large volume stones will have higher chances of RF and it remains to be assessed if indeed either laser can outperform the other to improve the SFR.
Footnotes
CONFLICTS OF INTEREST: The authors have nothing to disclose.
FUNDING: None.
- Research conception and design: Daniele Castellani and Vineet Gauhar.
- Data acquisition: all authors.
- Statistical analysis: Steffi Kar Kei Yuen and Deepak Ragoori.
- Data analysis and interpretation: Saeed Bin Hamri, Mohamed Amine Lakmichi, Mehmet Ilker Gokce, Azimdjon N. Tursunkulov, and Fernando Ramón de Fata Chillón.
- Drafting of the manuscript: Chu Ann Chai.
- Critical revision of the manuscript: Chu Ann Chai, Daniele Castellani, and Vineet Gauhar.
- Administrative, technical, or material support: Nariman Gadzhiev, Yiloren Tanidir, Esteban Emiliani, Vaddi Chandramohan, Angelo Naselli, Boyke Soebhali, and Ben Hall Chew.
- Supervision: Takaaki Inoue, Bhaskar Kumar Somani, Olivier Traxer, Daniele Castellani, and Vineet Gauhar.
References
- 1.Sorokin I, Mamoulakis C, Miyazawa K, Rodgers A, Talati J, Lotan Y. Epidemiology of stone disease across the world. World J Urol. 2017;35:1301–1320. doi: 10.1007/s00345-017-2008-6. [DOI] [PubMed] [Google Scholar]
- 2.Boyce CJ, Pickhardt PJ, Lawrence EM, Kim DH, Bruce RJ. Prevalence of urolithiasis in asymptomatic adults: objective determination using low dose noncontrast computerized tomography. J Urol. 2010;183:1017–1021. doi: 10.1016/j.juro.2009.11.047. [DOI] [PubMed] [Google Scholar]
- 3.Geraghty RM, Jones P, Somani BK. Simultaneous bilateral endoscopic surgery (SBES) for bilateral urolithiasis: the future? Evidence from a systematic review. Curr Urol Rep. 2019;20:15. doi: 10.1007/s11934-019-0877-5. [DOI] [PubMed] [Google Scholar]
- 4.Iremashvili V, Li S, Best SL, Hedican SP, Nakada SY. Clinical and demographic predictors of repeat stone surgery. BJU Int. 2019;124:836–841. doi: 10.1111/bju.14844. [DOI] [PubMed] [Google Scholar]
- 5.Castellani D, Traxer O, Ragoori D, Galosi AB, De Stefano V, Gadzhiev N, et al. Improving outcomes of same-sitting bilateral flexible ureteroscopy for renal stones in real-world practice: lessons learnt from global multicenter experience of 1250 patients. Eur Urol Open Sci. 2023;52:51–59. doi: 10.1016/j.euros.2023.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chua ME, Bobrowski A, Ahmad I, Kim JK, Silangcruz JM, Rickard M, et al. Thulium fibre laser vs holmium: yttrium-aluminium-garnet laser lithotripsy for urolithiasis: meta-analysis of clinical studies. BJU Int. 2023;131:383–394. doi: 10.1111/bju.15921. [DOI] [PubMed] [Google Scholar]
- 7.Chew BH, Koo KC, Halawani A, Lundeen CJ, Knudsen BE, Molina WR. Comparing dusting and fragmenting efficiency using the new SuperPulsed thulium fiber laser versus a 120 W Holmium:YAG laser. Investig Clin Urol. 2023;64:265–271. doi: 10.4111/icu.20230071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haas CR, Knoedler MA, Li S, Gralnek DR, Best SL, Penniston KL, et al. Pulse-modulated holmium:YAG laser vs the thulium fiber laser for renal and ureteral stones: a single-center prospective randomized clinical trial. J Urol. 2023;209:374–383. doi: 10.1097/JU.0000000000003050. [DOI] [PubMed] [Google Scholar]
- 9.Castellani D, Fong KY, Lim EJ, Chew BH, Tailly T, Emiliani E, et al. Comparison between holmium:YAG laser with MOSES technology vs thulium fiber laser lithotripsy in retrograde intrarenal surgery for kidney stones in adults: a propensity score-matched analysis from the FLEXible ureteroscopy outcomes registry. J Urol. 2023;210:323–330. doi: 10.1097/JU.0000000000003504. [DOI] [PubMed] [Google Scholar]
- 10.Adkins WC, Dulabon DA, Chorazy ZJ, Lund PS, Johnson LM, Jones WV. Consider Ho:YAG for low-cost, effective laser lithotripsy. Clin Laser Mon. 1994;12:139–141. [PubMed] [Google Scholar]
- 11.Matsuoka K, Iida S, Nakanami M, Koga H, Shimada A, Mihara T, et al. Holmium: yttrium-aluminum-garnet laser for endoscopic lithotripsy. Urology. 1995;45:947–952. doi: 10.1016/s0090-4295(99)80113-7. [DOI] [PubMed] [Google Scholar]
- 12.Uleri A, Farré A, Izquierdo P, Angerri O, Kanashiro A, Balaña J, et al. Thulium fiber laser versus holmium:yttrium aluminum garnet for lithotripsy: a systematic review and meta-analysis. Eur Urol. 2024;85:529–540. doi: 10.1016/j.eururo.2024.01.011. [DOI] [PubMed] [Google Scholar]
- 13.Tang X, Wu S, Li Z, Wang D, Lei C, Liu T, et al. Comparison of thulium fiber laser versus holmium laser in ureteroscopic lithotripsy: a meta-analysis and systematic review. BMC Urol. 2024;24:44. doi: 10.1186/s12894-024-01419-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Delbarre B, Baowaidan F, Culty T, Khelfat L, Brassier M, Ferragu M, et al. Prospective comparison of thulium and holmium laser lithotripsy for the treatment of upper urinary tract lithiasis. Eur Urol Open Sci. 2023;51:7–12. doi: 10.1016/j.euros.2023.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sreenevasan G. Bilateral renal calculi. Ann R Coll Surg Engl. 1974;55:3–12. [PMC free article] [PubMed] [Google Scholar]
- 16.Danilovic A, Torricelli FCM, Marchini GS, Batagello C, Vicentini FC, Traxer O, et al. Prospective evaluation of bilateral retrograde intrarenal surgery: is it really safe? J Endourol. 2021;35:14–20. doi: 10.1089/end.2020.0611. [DOI] [PubMed] [Google Scholar]
- 17.Chai CA, Somani B, Castellani D, Fong KY, Sarica K, Emiliani E, et al. Comparing same-sitting bilateral vs unilateral retrograde intrarenal surgery in the elderly. Urology. 2024;186:117–122. doi: 10.1016/j.urology.2024.02.031. [DOI] [PubMed] [Google Scholar]
- 18.Belkovsky M, Passerotti CC, Maia RS, de Almeida Artifon EL, Otoch JP, Da Cruz JAS. Comparing outcomes of single-use vs reusable ureteroscopes: a systematic review and meta analysis. Urolithiasis. 2024;52:37. doi: 10.1007/s00240-024-01537-8. [DOI] [PubMed] [Google Scholar]
- 19.Jun DY, Cho KS, Jeong JY, Moon YJ, Kang DH, Jung HD, et al. Comparison of surgical outcomes between single-use and reusable flexible ureteroscopes for renal stone management: a systematic review and meta-analysis. Medicina (Kaunas) 2022;58:1388. doi: 10.3390/medicina58101388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Traxer O, Corrales M. New lasers for stone treatment. Urol Clin North Am. 2022;49:1–10. doi: 10.1016/j.ucl.2021.07.006. [DOI] [PubMed] [Google Scholar]
- 21.Traxer O, Sierra A, Corrales M. Which is the best laser for lithotripsy? Thulium fiber laser. Eur Urol Open Sci. 2022;44:15–17. doi: 10.1016/j.euros.2022.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Andreeva V, Vinarov A, Yaroslavsky I, Kovalenko A, Vybornov A, Rapoport L, et al. Preclinical comparison of superpulse thulium fiber laser and a holmium:YAG laser for lithotripsy. World J Urol. 2020;38:497–503. doi: 10.1007/s00345-019-02785-9. [DOI] [PubMed] [Google Scholar]
- 23.Mishra A, Medairos R, Chen J, Soto-Palou F, Wu Y, Antonelli J, et al. Exploring optimal settings for safe and effective thulium fibre laser lithotripsy in a kidney model. BJU Int. 2024;133:223–230. doi: 10.1111/bju.16218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hardy LA, Vinnichenko V, Fried NM. High power holmium: YAG versus thulium fiber laser treatment of kidney stones in dusting mode: ablation rate and fragment size studies. Lasers Surg Med. 2019;51:522–530. doi: 10.1002/lsm.23057. [DOI] [PubMed] [Google Scholar]
- 25.Tzelves L, Geraghty R, Lombardo R, Davis NF, Petřík A, Neisius A, et al. Duration of follow-up and timing of discharge from imaging follow-up, in adult patients with urolithiasis after surgical or medical intervention: a systematic review and meta-analysis from the European Association of Urology guideline panel on urolithiasis. Eur Urol Focus. 2023;9:188–198. doi: 10.1016/j.euf.2022.06.016. [DOI] [PubMed] [Google Scholar]
- 26.Gauhar V, Castellani D, Chew BH, Smith D, Chai CA, Fong KY, et al. Does unenhanced computerized tomography as imaging standard post-retrograde intrarenal surgery paradoxically reduce stone-free rate and increase additional treatment for residual fragments? Outcomes from 5395 patients in the FLEXOR study by the TOWER group. Ther Adv Urol. 2023;15:17562872231198629. doi: 10.1177/17562872231198629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gauhar V, Chew BH, Traxer O, Tailly T, Emiliani E, Inoue T, et al. Indications, preferences, global practice patterns and outcomes in retrograde intrarenal surgery (RIRS) for renal stones in adults: results from a multicenter database of 6669 patients of the global FLEXible ureteroscopy Outcomes Registry (FLEXOR) World J Urol. 2023;41:567–574. doi: 10.1007/s00345-022-04257-z. [DOI] [PubMed] [Google Scholar]
- 28.Kronenberg P, Somani B. Advances in lasers for the treatment of stones-a systematic review. Curr Urol Rep. 2018;19:45. doi: 10.1007/s11934-018-0807-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pauchard F, Ventimiglia E, Corrales M, Traxer O. A practical guide for intra-renal temperature and pressure management during RIRS: what is the evidence telling us. J Clin Med. 2022;11:3429. doi: 10.3390/jcm11123429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gauhar V, Traxer O, Castellani D, Sietz C, Chew BH, Fong KY, et al. Could use of a flexible and navigable suction ureteral access sheath be a potential game-changer in retrograde intrarenal surgery? Outcomes at 30 days from a large, prospective, multicenter, real-world study by the European Association of Urology Urolithiasis Section. Eur Urol Focus. 2024 May 23; doi: 10.1016/j.euf.2024.05.010. [Epub] [DOI] [PubMed] [Google Scholar]