Abstract
We examined past-year intimate partner violence (IPV), including psychological violence without physical/sexual violence, and health outcomes among people with HIV (PWH) in care in a multi-site U.S. cohort. Between 2016–2022, PWH reported 12-month psychological, physical, and sexual IPV in a routine assessment. We used linear and logistic regression models adjusted for age, race/ethnicity, and site to examine relationships with health outcomes. Among 9748 PWH (median age 50 years, 81% cisgender male/16% cisgender female/1% transgender female; 44% non-Hispanic white/36% non-Hispanic Black/15% Hispanic), 9.3% (n=905) reported any IPV in the past 12 months; half reported psychological IPV without physical/sexual IPV (n=453). PWH reporting any type of IPV were on average younger than those who did not experience IPV. In adjusted models, any IPV was associated with increased likelihood of unstable housing, HIV viral load detection (HIV viral load ≥75 copies/mL), moderate-to-severe depressive symptoms, anxiety with panic symptoms, substance use (methamphetamines, cocaine/crack, illicit opioids, marijuana, heavy episodic/hazardous drinking), and concern about exposure to sexually transmitted infection. PWH reporting any IPV in the past 12 months had 4.2% lower adherence to antiretroviral therapy, 2.4 more HIV-related symptoms, a 1.9 point higher HIV stigma score, and a 9.5% lower quality of life score than those without IPV. We found similar associations among PWH reporting only psychological IPV, without physical/sexual IPV. IPV was common among PWH. Half reporting IPV reported only psychological IPV and had similarly poor outcomes as those reporting physical/sexual IPV, demonstrating the need to assess psychological as well as physical and sexual IPV.
Resumen
Examinamos la violencia de la pareja íntima (intimate partner violence, IPV) del año anterior, incluida la violencia psicológica sin violencia física y sexual, así como los resultados sanitarios entre las personas con VIH (people with HIV, PWH) que reciben atención en una cohorte multicéntrica de los Estados Unidos. Entre 2016 y 2022, las PWH informaron situaciones de IPV psicológica, física y sexual durante los 12 meses en una evaluación de rutina. Se utilizaron modelos de regresión lineal y logística ajustados por edad, raza/etnia y centro para examinar las relaciones con los resultados sanitarios. Entre 9748 PWH (mediana de edad de 50 años, 81 % de hombres cisgénero/16 % de mujeres cisgénero/1 % de mujeres transgénero; 44 % de blancos no hispanos/36 % de negros no hispanos/15 % de hispanos), el 9,3 % (n = 905) informaron haber sufrido algún tipo de IPV en los últimos 12 meses; la mitad informó situaciones de IPV psicológica sin IPV física y sexual (n = 453). Las PWH que informaron de cualquier tipo de IPV fueron, en promedio, más jóvenes que las que no sufrieron IPV. En los modelos ajustados, cualquier IPV se asoció con una mayor probabilidad de vivienda inestable, detección de carga viral del VIH (carga viral del VIH ≥75 copias/ml), síntomas depresivos de moderados a graves, ansiedad con síntomas de pánico, consumo de sustancias (metanfetaminas, cocaína/crack, opioides ilícitos, marihuana, consumo excesivo episódico/peligroso de alcohol) y preocupación por la exposición a infecciones de transmisión sexual. Las PWH que informaron alguna situación de IPV en los últimos 12 meses tuvieron un 4,2 % menos de cumplimiento de la terapia antirretrovírica, un 2,4 % más de síntomas relacionados con el VIH, una puntuación de estigma del VIH 1,9 puntos más alta y una puntuación de calidad de vida un 9,5 % más baja que las que no sufrieron IPV. Se encontraron asociaciones similares entre las PWH que informaron solo IPV psicológica, sin IPV física y sexual. La IPV fue común entre las PWH. La mitad de las personas que informaron IPV solo informaron IPV psicológica y tuvieron resultados igualmente deficientes que los que informaron IPV física y sexual, lo que demuestra la necesidad de evaluar la IPV psicológica, al igual que la IPV física y sexual.
Introduction
Intimate partner violence (IPV), with “intimate partner” defined as a current or former dating partner or spouse[1], is a major public health problem in the U.S. According to the Centers for Disease Control and Prevention, approximately 1 in 3 women and 1 in 4 men experience severe physical violence from an intimate partner in their lifetime[1] with 10 million affected each year[2]. IPV has been associated with poor physical and mental health outcomes, as well as injury and death[1]. The definition of IPV extends beyond physical/sexual IPV alone, and includes “stalking and psychological aggression by a current or former intimate partner”[3]. Studies have consistently found psychological IPV to be more common than physical IPV[4–7], and evidence has shown impacts on health outcomes including mental health issues[8], fatigue[8], chronic pain[9], GI problems[9], and disability preventing ability to work[9].
Among people with HIV (PWH) in the U.S., IPV is highly prevalent, with a national survey reporting a lifetime prevalence of 26% and a 12-month prevalence of 4%[10]. While 12-month prevalence among cisgender women and men are similar (4.5% vs. 4.4%, respectively), there is a higher prevalence of 7.7% among transgender-identified PWH[10]. Lifetime prevalence is highest among cisgender women and transgender people (36% and 29%, respectively), with high prevalence also among bisexual women (51%) and gay men (28%)[10], demonstrating the breadth of the problem regardless of gender identity or sexual orientation. Psychological IPV among PWH has also been found to be more common than physical IPV[7, 11, 12]. Among PWH, IPV in general has been associated with greater depression[7], substance use[7, 13], and HIV transmission risk behaviors[13]. IPV has also been associated with higher odds of detectable viral load[7, 14, 15], poorer adherence to antiretroviral therapy (ART) and engagement in care[7, 13, 15–19] and higher likelihood of HIV-related hospitalizations[18]. Smaller population studies of PWH have found psychological violence to be associated with decline in cellular immunity, higher viral load, and poorer engagement in HIV care[14, 20].
Despite the high prevalence of psychological IPV relative to other forms, few studies in any population have assessed differences in effects of experiencing IPV by violence type that have included effects of psychological violence in the absence of physical violence. Exceptions include a study of women recruited from family practice clinics in the southern U.S., and a large population study of Spanish women; both found similarly strong associations with adverse physical and mental health outcomes for those experiencing only psychological violence vs. those experiencing physical violence[8, 9]. Further, no known studies in any population have examined psychological violence independent of physical/sexual violence using a large mixed-gender, geographically diverse sample.
We hypothesize that the experience of psychological IPV alone, even in the absence of physical or sexual IPV, may yield similarly adverse outcomes to the experience of physical and/or sexual IPV among PWH. We sought to determine differences in the impact of both physical and psychological IPV on key health outcomes in a large mixed-gender, geographically, racially/ethnically and sexual-orientation-diverse sample of PWH, to determine the potential value added to clinical HIV care of routine assessment of psychological violence in addition to physical/sexual violence.
Methods
Study Population
Data for this study come from the Centers for AIDS Research Network of Integrated Clinical Sites (CNICS) cohort (https://www.uab.edu/cnics/), an open, clinical cohort study of PWH in care at ten sites across the U.S.[21]. The CNICS cohort is a geographically and demographically diverse sample of adult PWH (age 18+) in clinical care. This analysis includes data from the seven CNICS sites with IPV data available: the 1917 Clinic at University of Alabama-Birmingham; Case Western Reserve University in Cleveland, OH; Fenway Community Health-Boston, MA; Owen Clinic at University of California at San Diego; University of California at San Francisco; University of North Carolina at Chapel Hill; and Madison Clinic at Harborview Medical Center/University of Washington-Seattle. Data collection is approved by Institutional Review Boards at each site.
Data sources
CNICS has a data repository that includes demographic, clinical, laboratory, and other data such as patient-reported outcome measures (PROs) including IPV[22]. PROs are collected at point-of-care via electronic tablets self-administered by PWH prior to their routine medical appointment[23] every ~4–6 months. Patients are universally offered the PROs unless 1) they are too acutely ill to complete a questionnaire, or 2) indicate low literacy in its available languages (English and Spanish for this study; PROs have since been added for speakers of Amharic, Brazilian Portuguese, and Haitian Creole). Data on HIV viral load, CD4 count, and visit attendance was obtained from electronic medical record data.
IPV measure
The PRO assessment includes a brief (4-item), self-administered, validated screening instrument for intimate partner violence, which was administered in both English and Spanish: the IPV-4[24]. As previously described [24], we developed this measure using the NIH-Patient Reported Outcomes Measurement Information System (PROMIS) protocols for instrument development[25] and used a qualitative review process of assessing suitability of legacy measures, with the goal of identifying aspects of IPV most likely to threaten patients’ short-and-long-term safety/well-being, focusing on items that were not prone to misinterpretation (e.g., potentially yielding ‘false positive’ results). We then conducted cognitive interviews with PWH in order to further ensure comprehensibility[24].
The IPV-4, initiated in 2016, assesses physical, sexual, and psychological (controlling behavior by an intimate partner and fearfulness of a partner in the past year) IPV in the prior 12 months (see Figure 1). Any IPV was dichotomized as PWH experiencing either physical, sexual, and/or psychological IPV in the prior 12 months on their most recent PRO. Of PWH with any IPV, individuals were categorized as experiencing “psychological IPV only” if they endorsed either psychological IPV questions and neither physical nor sexual IPV questions. Individuals were categorized as experiencing physical/sexual IPV if they endorsed either physical or sexual IPV questions. This analysis includes IPV assessments measured between 6/2016–5/2022.
Figure 1.
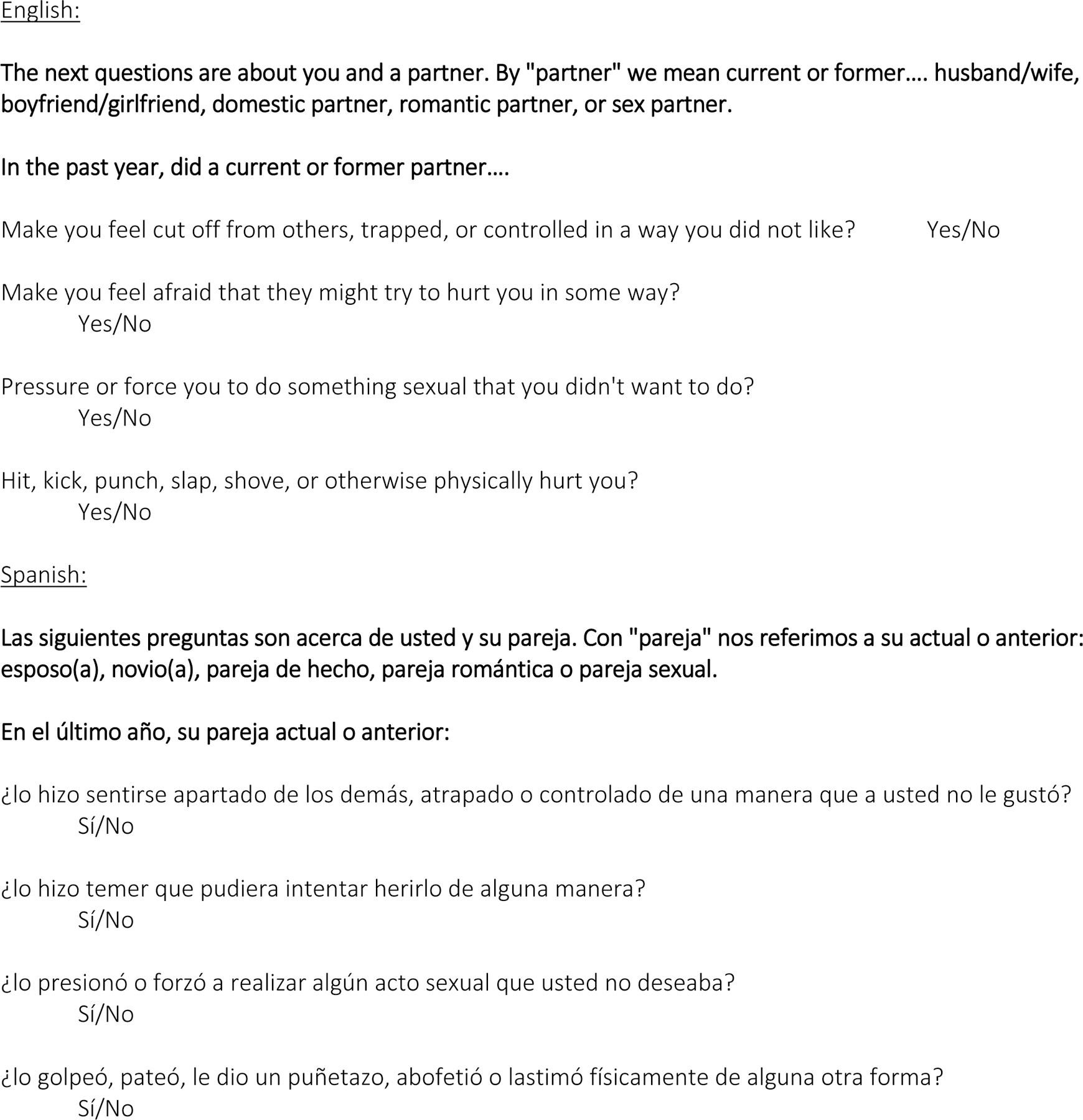
IPV-4
Safety protocols
PWH are informed that their responses to PRO measures are kept confidential and that any data used for research purposes is de-identified. In the CNICS clinical care setting, however, prior to taking the PRO assessment PWH are informed that their providers may see their responses. Patients are informed that they may skip any of the questions for any reason. While safety protocols for IPV are site-specific and vary slightly, the basic approach for most sites is that an indication of any type of violence on the IPV-4 prompts a pager alert for an on-site social worker to check-in with the individual during their clinic visit, at which point they are evaluated and availed of resources if needed.
Factors and outcomes
We examined the association between IPV and clinical outcomes of viral load and CD4 count. Additionally, we examined the association between IPV and being currently prescribed ART, as well as adherence; current use of methamphetamine, cocaine/crack, illicit opioids, marijuana, and alcohol, as well as current heavy episodic and hazardous drinking; and sexual risk behavior. Adherence to ART was measured as a percentage of HIV medication taken over the past 30 days[26]. Tobacco cigarette use was defined as self-reported current smoking of cigarettes[27–29]. Current heavy episodic drinking was defined as 5 or more drinks on one occasion for men and 4 or more drinks for women using the Alcohol Use Disorders Identification Test-Consumption (AUDIT-C)[30]. Hazardous drinking was defined as an AUDIT-C score of ≥3 for women and ≥4 for men. Current drug use (past 3 months) was measured using the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST)[31]. Sexual risk behaviors assessed included number of recent sex partners, self-reported concern for sexually transmitted infection (STI) exposure, and condomless sex in the past three months[32]. We examined the association of IPV with symptom burden defined as the number of symptoms on the HIV Symptoms Index[33] for which PWH reported ‘bothers some’ or ‘bothers a lot’. Moderate to severe depression was defined as a score of ≥10 on the PHQ-9[34, 35]. Anxiety with panic (PHQ-5)[34] was included as a binary response of experiencing an anxiety attack in the last four weeks. Other factors included HIV-related stigma (5 point Likert scale, level of agreement with one or more of four stigma-related statements, score 1–5, higher score indicates worse stigma)[36]; quality of life visual analog scale self-assessing health (0–100%, with 100% as best possible health)[37]; indication of current homelessness/unstable housing[38]; and indication of childhood household violence as per the ACE-IQ[39]. Detectable HIV viral load was defined as ≥ 75 copies/mL.
Statistical Analysis
We examined descriptive statistics to describe demographic and clinical characteristics of PWH that experienced any IPV, physical/sexual IPV, and psychological-only IPV. In the first set of analyses, we used multivariate linear (continuous outcomes) and multivariate logistic (binary outcomes) with robust standard error using the Huber-White estimator to model the association between any IPV and clinical outcomes and behaviors, adjusting for age, race/ethnicity, and site, with no IPV as the reference group. In the second set of analyses, we examined associations with individual types of IPV (physical/sexual IPV and psychological IPV only) and clinical outcomes and behaviors. We analyzed multivariate linear and multivariate logistic regressions with robust standard error using the Huber-White estimator to model the association between physical/sexual IPV and psychological only IPV and clinical and behavior outcomes, adjusting for age, race/ethnicity, and site, with no IPV as the reference group. In the third set of analyses, we examined associations with psychological IPV and clinical outcomes and behaviors, adjusting for physical/sexual IPV, age, race/ethnicity, and site. We analyzed multivariate linear and multivariate logistic with robust standard error using the Huber-White estimator to model these association, with no psychological IPV as the reference group.
Results
Study population
Overall, 9,748 PWH were included in our analysis. The median age was 50. Most were cisgender men (81%), while 16% were cisgender women, and 1% were transgender women (Table 1). Less than half (44%) were non-Hispanic White while 36% were non-Hispanic Black, and 15% Hispanic. There were 905 PWH (9%) who reported experiencing any type of IPV in the past 12 months; 452 participants reported physical and/or sexual IPV (5%) and 453 participants reported psychological IPV without physical/sexual IPV (5%). Half of those reporting any IPV, reported having experienced physical/sexual violence, and most (90%) participants reporting any IPV reported psychological violence. See Figure 2, a Venn diagram which illustrates overlap between violence categories.
Table 1.
Demographic and clinical characteristics of people with HIV in care by Intimate Partner Violence (IPV) type, 2016–2022.
| Total | Any IPV | Physical/Sexual IPV* | Psychological IPV only | |
|---|---|---|---|---|
|
| ||||
| N (%) | N (%) | N (%) | N (%) | |
| 9,748 | 905 (9) | 452 (5) | 453 (5) | |
|
| ||||
| Age, median (IQR) | 50 (39–58) | 45 (35 – 54) | 41 (33–52) | 48 (37–56) |
| Gender | ||||
| Cis-gender men | 7,874 (81) | 714 (79) | 344 (76) | 370 (81) |
| Cis-gender women | 1,576 (16) | 145 (16) | 80 (18) | 65 (14) |
| Transgender women | 116 (1) | 18 (2) | 11 (2) | 7 (2) |
| Gender not listed above | 72 (<1) | 12 (1) | 7 (2) | 5 (1) |
| Sexual Orientation | ||||
| Gay/Lesbian | 5646 (58) | 509 (56) | 262 (58) | 247 (55) |
| Heterosexual | 2683 (28) | 230 (25) | 103 (23) | 127 (28) |
| Bisexual | 814 (8) | 97 (11) | 45 (10) | 52 (12) |
| Race/Ethnicity 1 | ||||
| Non-Hispanic White | 4,240 (44) | 401 (44) | 192 (42) | 209 (46) |
| Non-Hispanic Black | 3,486 (36) | 322 (36) | 166 (37) | 156 (34) |
| Hispanic | 1,500 (15) | 142 (16) | 74 (16) | 68 (15) |
| Non-Hispanic Other/Unknown | 522 (5) | 40 (4) | 20 (4) | 20 (4) |
| People experiencing homelessness/unstable housing, past month | 386 (4) | 88 (10) | 55 (12) | 33 (7) |
| Childhood household violence | 1,415 (15) | 200 (22) | 121 (27) | 79 (17) |
| No Missed Visits, past year | 6,295 (65) | 451 (50) | 217 (48) | 234 (52) |
| Current ART use | 9,240 (95) | 836 (92) | 415 (92) | 421 (93) |
| ART adherence (VAS), median (IQR) | 99 (94–100) | 97 (88–100) | 97 (86–100) | 97 (90–100) |
| HIV Viral Load Detected (75 copies/ml) | 1,169 (12) | 148 (16) | 80 (18) | 68 (15) |
| CD4 count (cells/uL), median (IQR) | 638 (436–862) | 662 (418–892) | 654 (415–864) | 667 (422–913) |
| HIV Symptom Index, past month median (IQR)2,3 | 1 (0–4) | 4 (1–8) | 4 (1–8) | 3 (1–7) |
| Internalized HIV stigma score, median (IQR)4,5 | 7 (4–11) | 9 (4–14) | 9 (4–14) | 9 (5–13) |
| Depressive symptoms, past 2 weeks6,7 | 1,798 (18) | 374 (41) | 199 (44) | 175 (39) |
| Anxiety with panic, past 4 weeks | 2,417 (25) | 466 (51) | 240 (53) | 226 (50) |
| Quality of Life (VAS) 8 | 80 (65–92) | 71 (50–86) | 71 (50–86) | 71 (50–86) |
| Heavy episodic drinking, past 12 months9 | 3,289 (34) | 393 (43) | 212 (47) | 181 (40) |
| Hazardous drinking, past 12 months10 | 2,692 (28) | 301 (33) | 153 (34) | 148 (33) |
| Current tobacco use | 2,689 (28) | 365 (40) | 191 (42) | 174 (38) |
| Substance use, past 3 months | ||||
| Illicit opioids | 277 (3) | 78 (9) | 43 (10) | 35 (8) |
| Methamphetamines | 1,011 (10) | 228 (25) | 131 (29) | 97 (21) |
| Cocaine/crack | 657 (7) | 123 (14) | 67 (15) | 56 (12) |
| Marijuana | 3,258 (33) | 408 (45) | 211 (47) | 197 (43) |
| Multiple sexual partners, past 3 months | 2279 (23) | 355 (39) | 191 (42) | 164 (36) |
| Condomless sex, past 3 months | 2083 (21) | 222 (25) | 118 (26) | 104 (23) |
| Concern about STI exposure, past 3 months | 1071 (11) | 213 (24) | 127 (28) | 86 (19) |
with or without psychological violence
Abbreviations: ART, antiretroviral therapy; VAS, visual analog scale; AUDIT-C, Alcohol Use Disorders Identification Test-Concise, STI, Sexually Transmitted Infection.
Race/ethnicity are mutually exclusive categories.
“Fatigue or loss of energy,” “Fever, chills, or sweats,” “Feeling dizzy or lightheaded,” “Pain, numbness, or tingling in the hands or feet,” “Trouble remembering,” “Nausea or vomiting,” “Diarrhea or loose bowel movements,” “Feeling sad or depressed,” “Feeling nervous or anxious,” “Difficulty falling or staying asleep,” “Skin problems such as rashes, dryness or itching,” “Cough or trouble catching your breath,” “Headache,” “Loss of appetite or a change in the taste of food,” “Bloating, pain, or gas in your stomach,” “Muscle aches or joint pain,” “Problems with having sex, such as loss of interest or lack of satisfaction,” Changes in the way your body looks, such as fat deposits or weight gain,” “Problems with weight loss or wasting,” “Hair loss or changes in the way your hair looks.”
Responses of “it bothers me a little,” “it bothers me,” and “it bothers me a lot” were considered endorsed. Aggregated measure of the number of symptoms that bother the patient. Score ranges from 0 to 20.
“Having HIV makes me feel like I am a bad person,” “I feel ashamed of having HIV,” “I think less of myself because I have HIV,” and “Having HIV is disgusting to me.”
Aggregated score ranges from 4 to 20. Each question is a Likert scale of strongly disagree (1) to strongly agree (5).
How often over the last 2 weeks have you been bothered by… “little interest or pleasure in doing things,” “feeling down, depressed or hopeless,” “trouble falling or staying asleep or sleeping too much,” “Feeling tired or having little energy,” “poor appetite or overeating,” feeling bad about self – or that you are a failure or have let yourself or your family down,” “Trouble concentrating on things such as reading the newspaper or watching television,” “Moving or speaking so slowly that other people could have noticed? Or the opposite- being so fidgety or restless that you have been moving around a lot more than usual,” “Thought that you would be better off dead or hurting yourself in some way.”
Aggregated score ranges from 0 to 27. Each question is a Likert scale scored from 0 to 3. The measure is endorsed if aggregated measure is greater than or equal to a score of 10.
Patients were asked to select between 0 to 100 what closely reflects their own health state.
Endorsed if drank 4 (women)/5 (men) or more drinks on an occasion more than never.
AUDIT-C scores used to classify hazardous alcohol consumption: ≥3 points for women and ≥4 points for men.
Figure 2.
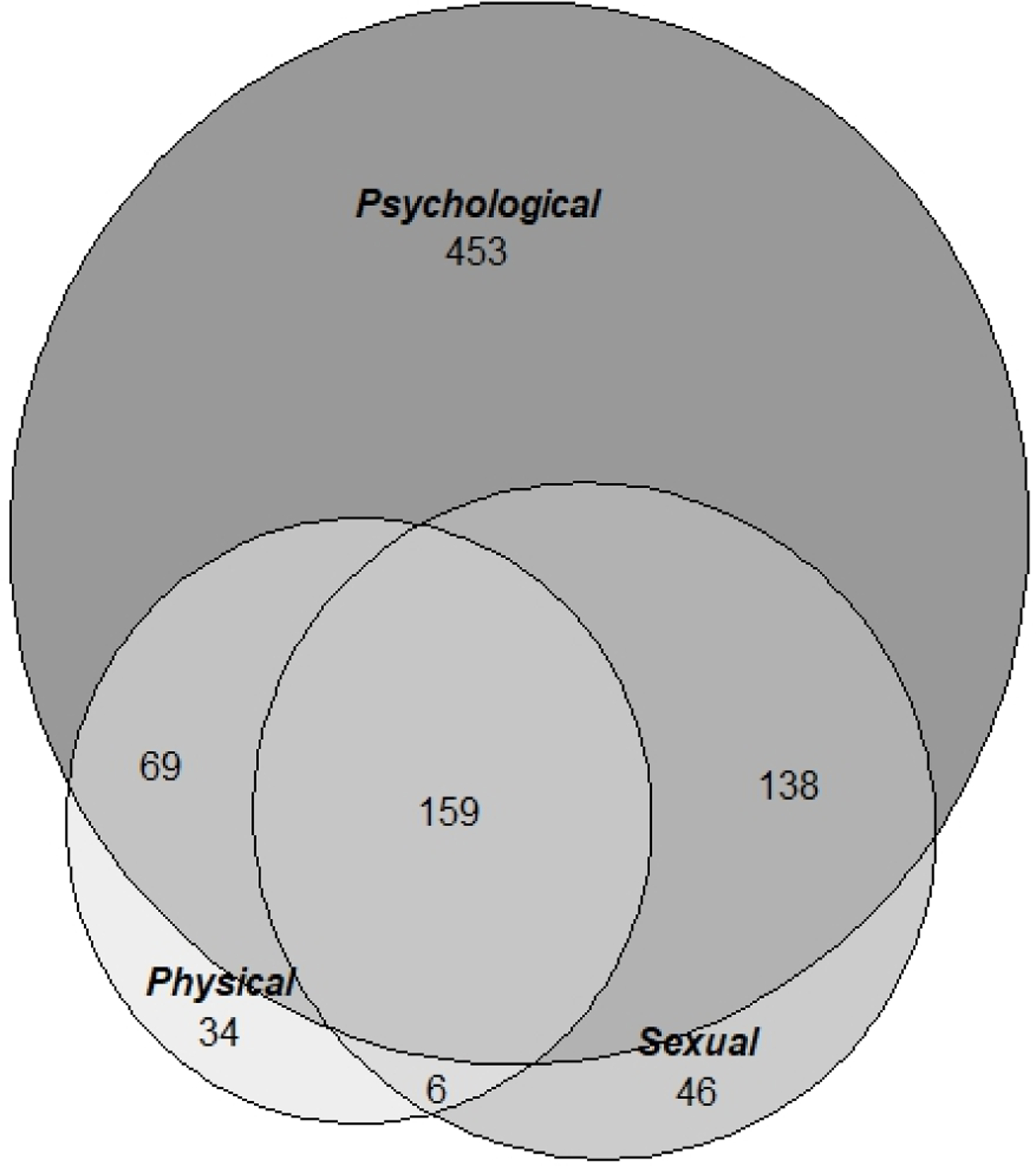
Venn Diagram of types of IPV reported by people with HIV in care, who report IPV
Table 1 shows demographic and clinical characteristics of PWH by overall IPV status and type of IPV. PWH who reported experiencing any type of IPV in the past 12 months were, on average, younger than the study population (45 vs. 50 years old). PWH who experienced psychological-only violence had older median age than those experiencing physical/sexual violence (48 vs. 41). Cisgender men were more likely to report psychological-only violence than physical/sexual violence, while cisgender women were more likely to report physical/sexual violence than psychological-only violence. There were no significant demographic differences in reporting IPV by race/ethnicity or sexual orientation.
Associations: Any IPV
In models adjusted for age, race/ethnicity, gender, and site, experience of any type of IPV in the past 12 months was associated with lower likelihood of ART use (OR=0.7 [95% Confidence Interval [95%CI]: 0.5, 0.9]; p=0.02), low ART adherence when prescribed ART (β=−4.2% on VAS scale [95%CI: −5.6%, −2.8%]; p<0.001), and having a detectable HIV viral load (OR=1.4 [95%CI: 1.1, 1.7]; p=0.002) (Table 2).
Table 2.
Association between any IPV and health-related outcomes, logistic and linear regression, adjusted for age, gender, race/ethnicity, and site.
| N | Any IPV OR | 95% Confidence Interval | p-value | |
|---|---|---|---|---|
| People experiencing homelessness/unstable housing, past month | 5385 | 3.8 | 2.9 – 4.9 | <0.001 |
| Childhood household violence | 7272 | 1.9 | 1.6 – 2.4 | <0.001 |
| Current ART use | 9631 | 0.7 | 0.5 – 0.9 | 0.02 |
| HIV Viral Load Detected (75 copies/ml) | 9621 | 1.4 | 1.1 – 1.7 | 0.002 |
| Depressive symptoms, past 2 weeks1,2 | 9635 | 3.5 | 3.0 – 4.1 | <0.001 |
| Anxiety with panic, past 4 weeks | 9631 | 3.4 | 2.9 – 3.9 | <0.001 |
| Heavy episodic drinking, past 12 months3 | 9632 | 1.4 | 1.2 – 1.6 | <0.001 |
| Hazardous drinking, past 12 months4 | 9615 | 1.2 | 1.1 – 1.4 | 0.006 |
| Current tobacco use | 9613 | 1.8 | 1.5 – 2.0 | <0.001 |
| Current illicit opioid use | 9570 | 3.4 | 2.6 – 4.6 | <0.001 |
| Current methamphetamine use | 9581 | 3.2 | 2.6 – 3.9 | <0.001 |
| Current cocaine/crack use | 9604 | 2.2 | 1.8 – 2.8 | <0.001 |
| Current marijuana use | 9619 | 1.5 | 1.3 – 1.8 | <0.001 |
| Multiple sexual partners, past 3 months | 9472 | 2.1 | 1.8 – 2.5 | <0.001 |
| Condomless sex, past 3 months | 5954 | 1.4 | 1.1 – 1.7 | 0.003 |
| Concern about STI exposure, past 3 months | 9441 | 2.5 | 2.1 – 2.9 | <0.001 |
| N | Coefficient Any IPV | 95% Confidence Interval | p-value | |
| ART adherence (VAS) | 9389 | −4.2 | −5.6 – −2.8 | <0.001 |
| CD4 count (cells/uL) | 9621 | 6.3 | −17.2 – 29.8 | 0.6 |
| HIV Symptom Index 5,6 | 9564 | 2.4 | 2.0 – 2.7 | <0.001 |
| Internalized HIV stigma score 7,8 | 8930 | 1.9 | 1.6 – 2.5 | <0.001 |
| Quality of Life (VAS) 9 | 9485 | −9.5 | −11.1 – −7.9 | <0.001 |
Abbreviations: OR, Odds ratio; ART, antiretroviral therapy; VAS, visual analog scale; AUDIT-C, Alcohol Use Disorders Identification Test-Concise, STI, Sexually Transmitted Infection.
How often over the last 2 weeks have you been bothered by… “little interest or pleasure in doing things,” “feeling down, depressed or hopeless,” “trouble falling or staying asleep or sleeping too much,” “Feeling tired or having little energy,” “poor appetite or overeating,” feeling bad about self – or that you are a failure or have let yourself or your family down,” “Trouble concentrating on things such as reading the newspaper or watching television,” “Moving or speaking so slowly that other people could have noticed? Or the opposite- being so fidgety or restless that you have been moving around a lot more than usual,” “Thought that you would be better off dead or hurting yourself in some way.”
Aggregated score ranges from 0 to 27. Each question is a Likert scale scored from 0 to 3. The measure is endorsed if aggregated measure is greater than or equal to a score of 10.
Endorsed if drank 4 (women)/5 (men) or more drinks on an occasion more than never.
AUDIT-C scores used to classify hazardous alcohol consumption: ≥3 points for women and ≥4 points for men.
“Fatigue or loss of energy,” “Fever, chills, or sweats,” “Feeling dizzy or lightheaded,” “Pain, numbness, or tingling in the hands or feet,” “Trouble remembering,” “Nausea or vomiting,” “Diarrhea or loose bowel movements,” “Feeling sad or depressed,” “Feeling nervous or anxious,” “Difficulty falling or staying asleep,” “Skin problems such as rashes, dryness or itching,” “Cough or trouble catching your breath,” “Headache,” “Loss of appetite or a change in the taste of food,” “Bloating, pain, or gas in your stomach,” “Muscle aches or joint pain,” “Problems with having sex, such as loss of interest or lack of satisfaction,” Changes in the way your body looks, such as fat deposits or weight gain,” “Problems with weight loss or wasting,” “Hair loss or changes in the way your hair looks.”
Responses of “it bothers me a little,” “it bothers me,” and “it bothers me a lot” were considered endorsed. Aggregated measure of the number of symptoms that bother the patient. Score ranges from 0 to 20.
“Having HIV makes me feel like I am a bad person,” “I feel ashamed of having HIV,” “I think less of myself because I have HIV,” and “Having HIV is disgusting to me.”
Aggregated score ranges from 4 to 20. Each question is a Likert scale of strongly disagree (1) to strongly agree (5).
Patients were asked to select between 0 to 100 what closely reflects their own health state.
In addition, IPV was associated with higher odds of being unhoused/experiencing housing instability in the past month (OR = 3.8 [95% CI: 2.9 – 4.9]; p<0.001), and a greater odds of reporting moderate to severe depressive symptoms and anxiety with panic symptoms (OR = 3.5 [95% CI: 3.0 – 4.1]; p<0.001; OR=3.4 [95% CI: 2.9 – 3.9]; p<0.001, respectively). Odds of substance use was also higher among PWH who experienced any IPV in the last 12 months, including heavy episodic drinking (OR = 1.4 [95% CI: 1.2 – 1.6]; p<0.001), hazardous drinking (OR = 1.2 [95% CI: 1.1 – 1.4]; p=0.006), current tobacco use (OR = 1.8 [95% CI: 1.5 – 2.0]; p<0.001), current marijuana use (OR = 1.5 [95% CI:1.3 – 1.8; p<0.001), current cocaine/crack use (OR = 2.2 [95% CI: 1.8 – 2.8]; p<0.001), current illicit opioid use (OR = 3.4 [95% CI: 2.6 – 4.6]; p<0.001], or current methamphetamine use (OR = 3.2 [95% CI: 2.6 – 3.9]; p<0.001]. We found a higher odds of reporting sex with 2 or more partners in the past 3 months (OR = 2.1 [95% CI: 1.8 – 2.5]; p<0.001), condomless sex (OR = 1.4 [95% CI: 1.1 – 1.7]; p=0.003], and concern for recent exposure to sexually transmitted infection (STI) (OR = 2.5 [95% CI: 2.1 – 2.9]; p<0.001) among PWH reporting any IPV compared to those who did not.
Additionally, PWH who reported any IPV had on average a 9.5% lower quality of life score on the visual rating scale (−9.5 [95% CI: −11.1 – −7.9]; p=<0.001), 2 points higher internalized HIV stigma score (1.9 [95% CI: 1.6 – 2.5]; p<0.001), 4% lower ART (−4.2 [95%CI: −5.6 – −2.8]; p<0.001) and 2.4 more HIV symptoms than those without IPV (2.4 [95%CI: 2.0 – 2.7]; p<0.001).
Associations: Psychological only IPV and Physical/Sexual IPV
In additional models adjusted for age, gender, race/ethnicity, and site, we found that most associations among PWH who experienced psychological only IPV or physical/sexual IPV were statistically significant (Table 3) including: ART adherence (−2.9 [95% CI: −4.6 – −1.2] and −5.6 [95% CI: −7.8 – −3.4]), having more HIV symptoms (2.1 [95% CI: 1.7 – 2.6] and 2.6 [95% CI: 2.1 – 2.6]), past-month experience of homelessness/unstable housing (OR=2.9 [95% CI: 1.9 – 4.4] and OR=4.6 [95% CI: 3.2 – 6.5]), depressive symptoms (OR=3.2 [95% CI: 2.6 – 3.9] and OR=3.9 [95% CI: 2.6 – 3.9]), anxiety with panic (OR=3.3 [95% CI: 2.7 – 4.1] and OR=3.5 [95% CI: 2.9 – 4.3]), internalized HIV stigma (2.1 [95% CI: 1.6 – 2.5] and 1.7 [95% CI: 1.2 – 2.2]), current methamphetamine use (OR=2.5 [95% CI: 1.9 – 3.3] and OR=3.9 [95% CI: 3.1 – 5.1]), current illicit opioid use (OR=3.2 [95% CI: 2.2 – 4.7] and OR=3.7 [95% CI: 2.6 – 5.2]), current cocaine/crack use (OR=2.0 [95% CI: 1.5 – 2.7] and OR=2.5 [95% CI: 1.8 – 3.3]), heavy episodic drinking (OR=1.3 [95% CI: 1.03 – 1.6] and OR=1.5 [95% CI: 1.2 – 1.8]), concern for STI exposure (OR=1.9 [95% CI: 1.5 – 2.5] and OR=3.1 [95% CI: 2.4 – 3.9]), and quality of life (−9.1 [95% CI: −11.2 – −6.9] and −10.0 [95% CI: −12.2 – −7.8]) (Table 3). However, we did not find associations between psychological only IPV and current ART use, detected HIV viral load, and condomless sex, hazardous drinking, and CD4 count.
Table 3.
Association of psychological and physical/sexual IPV with outcomes, logistic and linear regression, adjusted for age, gender, race/ethnicity, and site.
| N | OR Psychological only IPV | Psychological only IPV 95% CI |
OR Physical/Sexual IPV* | Physical/Sexual IPV 95% CI |
|
|---|---|---|---|---|---|
| People experiencing homelessness/unstable housing, past month | 5385 | 2.9 | 1.9 – 4.4 | 4.6 | 3.2 – 6.5 |
| Childhood household violence | 7272 | 1.4 | 1.1 – 1.9 | 2.6 | 2.0 – 3.4 |
| Current ART use | 9631 | 0.8 | 0.5 – 1.1 | 0.7 | 0.5 – 0.9 |
| HIV Viral Load Detected (75 copies/ml) | 9621 | 1.3 | 0.9 – 1.7 | 1.5 | 1.1 – 1.9 |
| Depressive symptoms, past 2 weeks1,2 | 9635 | 3.2 | 2.6 – 3.9 | 3.9 | 3.2 – 4.8 |
| Anxiety with panic, past 4 weeks | 9631 | 3.3 | 2.7 – 4.1 | 3.5 | 2.9 – 4.3 |
| Heavy episodic drinking, past 12 months3 | 9632 | 1.3 | 1.03 – 1.6 | 1.5 | 1.2 – 1.8 |
| Hazardous drinking, past 12 months4 | 9615 | 1.2 | 1.01 – 1.5 | 1.2 | 0.9 – 1.5 |
| Current tobacco use | 9613 | 1.7 | 1.4 – 2.0 | 1.8 | 1.5 – 2.2 |
| Current illicit opioid use | 9570 | 3.2 | 2.2 – 4.7 | 3.7 | 2.6 – 5.2 |
| Current methamphetamine use | 9581 | 2.5 | 1.9 – 3.3 | 3.9 | 3.1 – 5.1 |
| Current cocaine/crack use | 9604 | 2.0 | 1.5 – 2.7 | 2.5 | 1.8 – 3.3 |
| Current marijuana use | 9619 | 1.5 | 1.2 – 1.8 | 1.6 | 1.3 – 1.9 |
| Multiple sexual partners, past 3 months | 9472 | 1.9 | 1.5 – 2.4 | 2.4 | 1.9 – 2.9 |
| Condomless sex, past 3 months5 | 5954 | 1.2 | 0.9 – 1.5 | 1.6 | 1.2 – 2.1 |
| Concern about STI exposure, past 3 months | 9441 | 1.9 | 1.5 – 2.5 | 3.1 | 2.4 – 3.9 |
| N | Coefficient Psychological only IPV | Psychological only IPV 95% CI |
Coefficient Physical/Sexual IPV* | Physical/Sexual IPV 95% CI |
|
| ART adherence (VAS) | 9389 | −2.9 | −4.6 – −1.2 | −5.6 | −7.8 – −3.4 |
| CD4 count (cells/uL) | 9621 | 25.5 | −8.1 – 59.1 | −13.5 | −44.3 – 17.4 |
| HIV Symptom Index 6,7 | 9564 | 2.1 | 1.7 – 2.6 | 2.6 | 2.1 – 2.6 |
| Internalized HIV stigma score 8,9 | 8930 | 2.1 | 1.6 – 2.5 | 1.7 | 1.2 – 2.2 |
| Quality of Life (VAS) 10 | 9485 | −9.1 | −11.2 – −6.9 | −10.0 | −12.2 – −7.8 |
with or without psychological violence
Abbreviations: OR, Odds Ratio; CI, Confidence Interval ART, Antiretroviral Therapy; VAS, visual analog scale; AUDIT-C, Alcohol Use Disorders Identification Test-Concise, STI, Sexually Transmitted Infection.
. How often over the last 2 weeks have you been bothered by… “little interest or pleasure in doing things,” “feeling down, depressed or hopeless,” “trouble falling or staying asleep or sleeping too much,” “Feeling tired or having little energy,” “poor appetite or overeating,” feeling bad about self – or that you are a failure or have let yourself or your family down,” “Trouble concentrating on things such as reading the newspaper or watching television,” “Moving or speaking so slowly that other people could have noticed? Or the opposite- being so fidgety or restless that you have been moving around a lot more than usual,” “Thought that you would be better off dead or hurting yourself in some way.”
Aggregated score ranges from 0 to 27. Each question is a Likert scale scored from 0 to 3. The measure is endorsed if aggregated measure is greater than or equal to a score of 10.
Endorsed if drank 4 (women)/5 (men) or more drinks on an occasion more than never.
AUDIT-C scores used to classify hazardous alcohol consumption: ≥3 points for women and ≥4 points for men.
Among participants reporting having current sexual activity.
“Fatigue or loss of energy,” “Fever, chills, or sweats,” “Feeling dizzy or lightheaded,” “Pain, numbness, or tingling in the hands or feet,” “Trouble remembering,” “Nausea or vomiting,” “Diarrhea or loose bowel movements,” “Feeling sad or depressed,” “Feeling nervous or anxious,” “Difficulty falling or staying asleep,” “Skin problems such as rashes, dryness or itching,” “Cough or trouble catching your breath,” “Headache,” “Loss of appetite or a change in the taste of food,” “Bloating, pain, or gas in your stomach,” “Muscle aches or joint pain,” “Problems with having sex, such as loss of interest or lack of satisfaction,” Changes in the way your body looks, such as fat deposits or weight gain,” “Problems with weight loss or wasting,” “Hair loss or changes in the way your hair looks.”
Responses of “it bothers me a little,” “it bothers me,” and “it bothers me a lot” were considered endorsed. Aggregated measure of the number of symptoms that bother the patient. Score ranges from 0 to 20.
“Having HIV makes me feel like I am a bad person,” “I feel ashamed of having HIV,” “I think less of myself because I have HIV,” and “Having HIV is disgusting to me.”
Aggregated score ranges from 4 to 20. Each question is a Likert scale of strongly disagree (1) to strongly agree (5).
Patients were asked to select between 0 to 100 what closely reflects their own health state
Associations: Psychological IPV, controlling for Physical/Sexual IPV
After additionally controlling for physical/sexual IPV, we found that psychological IPV was still significantly associated with most outcomes of interest (Table 4) including HIV viral load detection (OR=1.3 [95% CI: 1.0 – 1.7]; p=0.02), ART adherence (−2.9 [95% CI: −4.5 – −1.3]; p<0.001), past-month experience of homelessness/unstable housing (OR=2.5 [95% CI: 1.7 – 3.8]; p<0.001), current depressive symptoms (OR=2.8 [95% CI: 2.3 – 3.4]; p<0.001), anxiety with panic (OR=1.6 [95% CI: 1.2 – 2.2]; p=0.005), current methamphetamine use (OR=2.1 [95% CI: 1.6 −2.7]; p<0.001), current illicit opioid use (OR=2.6 [95% CI: 1.7 – 3.9]; p<0.001), current cocaine/crack use (OR=1.6 [95% CI: 1.2 – 2.2]; p=0.005), and concern about STI exposure (OR=1.8 [95% CI: 1.4 – 2.3]; p<0.001). We did not find associations, after controlling for physical/sexual IPV, between psychological IPV and heavy episodic drinking, hazardous drinking, condomless sex, and CD4 count.
Table 4.
Association of psychological IPV with outcomes, logistic and linear regression, adjusted for physical/sexual IPV, age, gender, race/ethnicity, and site.
| N | Psychological IPV | 95% Confidence Interval | p-value | |
|---|---|---|---|---|
| People experiencing homelessness/unstable housing, past month | 5385 | 2.5 | 1.7 – 3.8 | <0.001 |
| Childhood household violence | 7272 | 1.4 | 1.1 – 1.8 | 0.007 |
| Current ART use | 9631 | 0.7 | 0.5 – 0.9 | 0.04 |
| HIV Viral Load Detected (75 copies/ml) | 9621 | 1.3 | 1.0 – 1.7 | 0.02 |
| Depressive symptoms, past 2 weeks1,2 | 9635 | 2.8 | 2.3 – 3.4 | <0.001 |
| Anxiety with panic, past 4 weeks | 9631 | 2.9 | 2.4 – 3.5 | <0.001 |
| Heavy episodic drinking, past 12 months3 | 9632 | 1.2 | 0.9 – 1.4 | 0.06 |
| Hazardous drinking, past 12 months4 | 9615 | 1.2 | 0.9 – 1.5 | 0.05 |
| Current tobacco use | 9613 | 1.5 | 1.3 – 1.9 | <0.001 |
| Current illicit opioid use | 9570 | 2.6 | 1.7 – 3.9 | <0.001 |
| Current methamphetamine use | 9581 | 2.1 | 1.6 −2.7 | <0.001 |
| Current cocaine/crack use | 9604 | 1.6 | 1.2 – 2.2 | 0.005 |
| Current marijuana use | 9619 | 1.4 | 1.1 – 1.7 | 0.001 |
| Multiple sexual partners, past 3 months | 9472 | 1.7 | 1.4 – 2.1 | <0.001 |
| Condomless sex, past 3 months | 5954 | 1.0 | 0.8 – 1.3 | 0.9 |
| Concern about STI exposure, past 3 months | 9441 | 1.8 | 1.4 – 2.3 | <0.001 |
| N | Coefficient Psychological IPV | 95% Confidence Interval | p-value | |
| ART adherence (VAS) | 9389 | −2.9 | −4.5 – −1.3 | <0.001 |
| CD4 count (cells/uL) | 9621 | 18.9 | −11.6 – 49.6 | 0.2 |
| HIV Symptom Index 5,6 | 9564 | 2.0 | 1.6 – 2.4 | <0.001 |
| Internalized HIV stigma score 7,8 | 8930 | 1.9 | 1.5 – 2.4 | <0.001 |
| Quality of Life (VAS) 9 | 9485 | −8.1 | −10.1 – −6.1 | <0.001 |
Abbreviations: OR, Odds ratio; ART, antiretroviral therapy; VAS, visual analog scale; AUDIT-C, Alcohol Use Disorders Identification Test-Concise, STI, Sexually Transmitted Infection.
How often over the last 2 weeks have you been bothered by… “little interest or pleasure in doing things,” “feeling down, depressed or hopeless,” “trouble falling or staying asleep or sleeping too much,” “Feeling tired or having little energy,” “poor appetite or overeating,” feeling bad about self – or that you are a failure or have let yourself or your family down,” “Trouble concentrating on things such as reading the newspaper or watching television,” “Moving or speaking so slowly that other people could have noticed? Or the opposite- being so fidgety or restless that you have been moving around a lot more than usual,” “Thought that you would be better off dead or hurting yourself in some way.”
Aggregated score ranges from 0 to 27. Each question is a Likert scale scored from 0 to 3. The measure is endorsed if aggregated measure is greater than or equal to a score of 10.
Endorsed if drank 4 (women)/5 (men) or more drinks on an occasion more than never.
AUDIT-C scores used to classify hazardous alcohol consumption: ≥3 points for women and ≥4 points for men.
“Fatigue or loss of energy,” “Fever, chills, or sweats,” “Feeling dizzy or lightheaded,” “Pain, numbness, or tingling in the hands or feet,” “Trouble remembering,” “Nausea or vomiting,” “Diarrhea or loose bowel movements,” “Feeling sad or depressed,” “Feeling nervous or anxious,” “Difficulty falling or staying asleep,” “Skin problems such as rashes, dryness or itching,” “Cough or trouble catching your breath,” “Headache,” “Loss of appetite or a change in the taste of food,” “Bloating, pain, or gas in your stomach,” “Muscle aches or joint pain,” “Problems with having sex, such as loss of interest or lack of satisfaction,” Changes in the way your body looks, such as fat deposits or weight gain,” “Problems with weight loss or wasting,” “Hair loss or changes in the way your hair looks.”
Responses of “it bothers me a little,” “it bothers me,” and “it bothers me a lot” were considered endorsed. Aggregated measure of the number of symptoms that bother the patient. Score ranges from 0 to 20.
“Having HIV makes me feel like I am a bad person,” “I feel ashamed of having HIV,” “I think less of myself because I have HIV,” and “Having HIV is disgusting to me.”
Aggregated score ranges from 4 to 20. Each question is a Likert scale of strongly disagree (1) to strongly agree (5).
Patients were asked to select between 0 to 100 what closely reflects their own health state.
Discussion
In a large multi-site sample of PWH receiving care in the U.S., diverse in race/ethnicity, gender identity, and sexual orientation, approximately one in ten (9.3%) reported past-year IPV. IPV was present in every demographic group regardless of gender identity, race/ethnicity, sexual orientation, or age group, with elevated IPV among those of younger age, as well as people identifying as transgender. Of those reporting past-year IPV, half reported physical/sexual violence, and 90% reported psychological violence. Half reported the latter in the absence of past-year physical or sexual violence. IPV of any type was associated with a wide range of adverse health behaviors affecting the HIV care continuum, including poorer ART adherence, and was also associated with viral suppression. It was associated with increased number of HIV-related symptoms, greater mental health symptoms, and lower quality of life. It was adversely associated with every health behavior measured, including substance use of every type, heavy episodic drinking, and sexual risk behavior. IPV was also associated with higher internalized HIV stigma, and unstable housing. Psychological IPV, even in the absence of physical or sexual violence, showed strong associations with most outcomes. We believe our findings are unlikely unique to PWH, warranting further study of the effects of psychological violence in the general population.
Building on the findings of prior studies, including those with PWH, psychological IPV was more common than physical or sexual IPV[4, 5, 7, 8, 11, 12]. Other studies of IPV (although not necessarily distinguishing psychological from other forms) among PWH have also found associations with adverse health and HIV related outcomes[7, 13–19]. The mechanisms by which psychological IPV affects these outcomes is known to be multifactorial and complex. Psychological IPV is well-known to be associated with depression and post-traumatic stress disorder[40]. IPV has also been strongly linked problematic substance use[41] with evidence of a bidirectional relationship[42]. Depression and mental health problems are associated with poor quality of life[16], substance use[43], and among PWH, ART adherence and viral load[16]. Recent work among PWH has found substance use and depression mediate the relationship between psychological IPV and virologic outcomes[7], supporting the theory of IPV as one component of a “syndemic” with other such risk factors[44]. Given the role of IPV in a syndemic involving multiple, co-occurring risk behaviors known to exacerbate one another, the assessment of IPV, along with associated symptoms and health behaviors, is essential to provision of comprehensive HIV care. The high rate of IPV among PWH, present across demographic groups regardless of gender, age, race, or sexual orientation demonstrates a need for routine universal IPV screening in this population.
In primary care in general, IPV is known to be poorly addressed, both in terms of low screening rates and appropriateness of interventions[45, 46]. While such screening is recommended by the HIV Medicine Association of the Infectious Diseases Society of America[47], other regulatory entities do not support universal screening for IPV: both the American Academy of Family Physicians and the U.S. Preventative Services Task Force limit recommendation for IPV screening to women of childbearing age[45], a recommendation discordant with its cross-demographic prevalence found among PWH in our study. IPV is more typically addressed after-the-fact, in emergency services, following assault and/or potentially life-threatening injury. Prevention is needed further upstream. The higher rate of psychological IPV relative to physical/sexual IPV, coupled with its near-identical associations with adverse health outcomes, underscores the importance of a multidimensional measure, particularly as psychological IPV has been found more likely to continue in the absence of physical or sexual IPV[48]. To the extent that psychological IPV may be a precursor to physical or sexual assault, there is clear value in identifying unwanted controlling behavior and/or fear of harm by an intimate partner in the relative safety of a routine care setting, for any population.
IPV screening is simple, quick and improves detection[49]. Brief, electronic PRO assessments have been shown to be superior to in-person interviewing for identifying IPV[49] and preferred by patients[50]. PROs significantly improve detection of other associated, difficult-to-discuss conditions and behaviors including depression, substance use, and medication adherence[51] and have been found to be acceptable to patients and useful to providers[52–57], rendering them an important tool for improving identification of IPV and addressing its related challenges. Future work investigating the relationship between psychological IPV and physical/sexual violence should utilize longitudinal data to investigate whether reporting psychological IPV predicts subsequent onset of physical and/or sexual violence.
Strengths and Limitations
This work is the first known study to examine psychological IPV in the absence of physical and sexual IPV in a large demographically and geographically diverse sample of PWH in care, with administration in English and Spanish. A study strength is our use of a computerized, self-administered assessment to elicit IPV data, as opposed to interviewer-administered screening[14, 49, 50]; the latter is known to less accurately identify IPV relative to computer-based, patient-administered questionnaires[50] and are less-preferred by patients[50, 58], with potential implications for social desirability bias. We note that psychological violence has many dimensions, yet the IPV-4 focuses on only two (unwanted controlling behavior, and fearfulness). Further work is warranted to identify aspects of psychological violence that may also be relevant to clinical outcomes, particularly in the absence of physical or sexual IPV. We note that the cross-sectional nature of this study limits inferences that can be made regarding the direction of the impact of specific factors either as exposures or outcomes, warranting longitudinal exploration of these relationships.
Conclusions
IPV was highly prevalent in a large, demographically and geographically diverse sample of PWH in care. Few demographic differences in prevalence existed, demonstrating a need for universal assessment in routine HIV care. Psychological IPV was far more common than physical or sexual IPV. Even in the absence of physical or sexual IPV, psychological IPV was associated with adverse health outcomes, including higher rates of substance use, lower ART adherence, and higher viral load, demonstrating the importance of including a psychological dimension when assessing IPV. The syndemic nature of problems interlinked with IPV warrants concurrent measurement of related health behaviors, symptoms, and psychosocial needs in HIV care.
Acknowledgements
CNICS is supported by the National Institute of Allergy and Infectious Diseases (NIAID) CNICS (R24 AI067039). Additional support from NIAID includes the University of Washington Center for AIDS Research (Grant No. P30 AI027757), and University of Alabama, Birmingham Center for AIDS Research (CFAR) (Grant No. P30 AI027767); support from the National Institute of Drug Abuse (NIDA) (Grants No. R01DA047045 and R01DA058938); and support from the Agency for Healthcare Research and Quality (AHRQ) (Grant No. U18HS026154).
Footnotes
Declarations
E. Cachay has received unrestricted research grants paid to the University of California Reagents from Gilead Sciences for unrelated hepatitis C virus research projects and has received payment honoraria from Gilead Science (symposium, educational event November 2021) and THERATechnologies (advisory board consulting fees for an unrelated topic in 2022).
K. Christopoulos has been a medical advisory board member for Gilead and a workshop participant for Janssen. J. Eron declares research funding from Gilead Sciences and ViiV Healthcare University of North Carolina-Chapel Hill as an investigator, and consulting fees paid to him from Merck & Co, ViiV Healthcare and Gilead Sciences. All other authors declare no conflicts of interest.
References
- 1.Centers for Disease Control. Fast facts: preventing intimate partner violence. 2023. January 23, 2023]; Available from: https://www.cdc.gov/violenceprevention/intimatepartnerviolence/fastfact.html. [Google Scholar]
- 2.Huecker MR, et al. , Domestic Violence, in StatPearls. 2022: Treasure Island (FL). [Google Scholar]
- 3.Centers for Disease Control. Violence prevention: intimate partner violence. 2021. October 10, 2022]; Available from: https://www.cdc.gov/violenceprevention/intimatepartnerviolence/index.html. [Google Scholar]
- 4.Ali B, et al. , Psychological violence and sexual risk behavior among predominantly African American women. J Interpers Violence, 2017: p. 886260517720734. [DOI] [PubMed] [Google Scholar]
- 5.Lovestad S, et al. , Prevalence of intimate partner violence and its association with symptoms of depression; a cross-sectional study based on a female population sample in Sweden. BMC Public Health, 2017. 17(1): p. 335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thompson RS, et al. , Intimate partner violence: prevalence, types, and chronicity in adult women. Am J Prev Med, 2006. 30(6): p. 447–57. [DOI] [PubMed] [Google Scholar]
- 7.Fredericksen RJ, et al. , Correlates of psychological intimate partner violence with HIV care outcomes on patients in HIV care. BMC Public Health, 2021. 21(1): p. 1824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Domenech Del Rio I and Sirvent E Garcia Del Valle, The Consequences of Intimate Partner Violence on Health: A Further Disaggregation of Psychological Violence-Evidence From Spain. Violence Against Women, 2017. 23(14): p. 1771–1789. [DOI] [PubMed] [Google Scholar]
- 9.Coker AL, et al. , Physical health consequences of physical and psychological intimate partner violence. Arch Fam Med, 2000. 9(5): p. 451–7. [DOI] [PubMed] [Google Scholar]
- 10.Lemons-Lyn AB, et al. , Intimate Partner Violence Experienced by Adults With Diagnosed HIV in the U.S. Am J Prev Med, 2021. 60(6): p. 747–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fiorentino M, et al. , Intimate partner violence against HIV-positive Cameroonian women: Prevalence, associated factors and relationship with antiretroviral therapy discontinuity-results from the ANRS-12288 EVOLCam survey. Womens Health (Lond), 2019. 15: p. 1745506519848546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu Y, et al. , Prevalence of Intimate Partner Violence and Associated Factors Among People With HIV: A Large-Sample Cross-Sectional Study in China. J Infect Dis, 2023. 228(11): p. 1592–1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kalokhe AS, et al. , Intimate partner violence among HIV-infected crack cocaine users. AIDS Patient Care STDS, 2012. 26(4): p. 234–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schafer KR, et al. , Intimate partner violence: a predictor of worse HIV outcomes and engagement in care. AIDS Patient Care STDS, 2012. 26(6): p. 356–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hatcher AM, et al. , Intimate partner violence and engagement in HIV care and treatment among women: a systematic review and meta-analysis. AIDS, 2015. 29(16): p. 2183–94. [DOI] [PubMed] [Google Scholar]
- 16.Pantalone DW, Hessler DM, and Simoni JM, Mental health pathways from interpersonal violence to health-related outcomes in HIV-positive sexual minority men. J Consult Clin Psychol, 2010. 78(3): p. 387–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Siemieniuk RA, et al. , The clinical implications of high rates of intimate partner violence against HIV-positive women. J Acquir Immune Defic Syndr, 2013. 64(1): p. 32–8. [DOI] [PubMed] [Google Scholar]
- 18.Siemieniuk RA, et al. , Prevalence, clinical associations, and impact of intimate partner violence among HIV-infected gay and bisexual men: a population-based study. HIV Med, 2013. 14(5): p. 293–302. [DOI] [PubMed] [Google Scholar]
- 19.Pantalone DW, et al. , Syndemic Indicators Predict Poor Medication Adherence and Increased Health Care Utilization for Urban HIV-Positive Men Who Have Sex with Men. J Gay Lesbian Ment Health, 2018. 22(1): p. 71–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jewkes R, et al. , Impact of exposure to intimate partner violence on CD4+ and CD8+ T cell decay in HIV infected women: longitudinal study. PLoS One, 2015. 10(3): p. e0122001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for AIDS Research Network of Integrated Clinical Systems. 2021. April 17. 2019]; Available from: https://www.uab.edu/cnics/.
- 22.Kitahata MM, et al. , Cohort profile: the Centers for AIDS Research Network of Integrated Clinical Systems. Int J Epidemiol, 2008. 37(5): p. 948–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fredericksen RJ, et al. , Integrating a web-based patient assessment into primary care for HIV-infected adults. Journal of AIDS and HIV Research, 2012. 4(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fredericksen RJ, Fitzsimmons E, Avendano-Soto S, Brown S, Christopoulos K, Dougherty S, Eron J, Kitahata M, Loo S, Mayer K, Mugavero M, Napravnik S, O’Cleirigh C, Potter J, Ruderman S, Smith L, Crane PK, Crane HM, Development and integration of the IPV-4, a patient-reported screening instrument of intimate partner violence for primary and HIV care. Journal of AIDS and HIV Research, 2022(In press). [Google Scholar]
- 25.Cella D, et al. , The Patient-Reported Outcomes Measurement Information System (PROMIS): progress of an NIH Roadmap cooperative group during its first two years. Med Care, 2007. 45(5 Suppl 1): p. S3–S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Simoni JM, et al. , Self-report measures of antiretroviral therapy adherence: A review with recommendations for HIV research and clinical management. AIDS Behav, 2006. 10(3): p. 227–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kiechl S, et al. , Active and passive smoking, chronic infections, and the risk of carotid atherosclerosis: prospective results from the Bruneck Study. Stroke, 2002. 33(9): p. 2170–6. [DOI] [PubMed] [Google Scholar]
- 28.Cropsey KL, et al. , Cigarette Smokers are Less Likely to Have Undetectable Viral Loads: Results From Four HIV Clinics. J Addict Med, 2016. 10(1): p. 13–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nance R DJ, Fredericksen R, Cropsey K, Chander G, Mugavero M, Christopoulos K, Geng E, Mathews W, Hahn A, Mayer K, O’Cleirigh C, Eron J, Saag M, Kitahata M, Crene H. E-cigarette use among persons living with HIV. in International AIDS Society Meeting. 2017: Paris, France. [Google Scholar]
- 30.Bush K, et al. , The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med, 1998. 158(16): p. 1789–95. [DOI] [PubMed] [Google Scholar]
- 31.Newcombe DA, Humeniuk RE, and Ali R, Validation of the World Health Organization Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): report of results from the Australian site. Drug Alcohol Rev, 2005. 24(3): p. 217–26. [DOI] [PubMed] [Google Scholar]
- 32.Fredericksen RJ, et al. , Development and Content Validation of a Patient-Reported Sexual Risk Measure for Use in Primary Care. J Gen Intern Med, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Justice AC, et al. , Development and validation of a self-completed HIV symptom index. J Clin Epidemiol, 2001. 54 Suppl 1: p. S77–90. [DOI] [PubMed] [Google Scholar]
- 34.Spitzer RL, Kroenke K, and Williams JB, Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. Jama, 1999. 282(18): p. 1737–44. [DOI] [PubMed] [Google Scholar]
- 35.Kroenke K, Spitzer RL, and Williams JB, The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med, 2001. 16(9): p. 606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Earnshaw VA, et al. , HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav, 2013. 17(5): p. 1785–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.EuroQol G, EuroQol--a new facility for the measurement of health-related quality of life. Health Policy, 1990. 16(3): p. 199–208. [DOI] [PubMed] [Google Scholar]
- 38.Whitney BM FE, Jackson MK, Brown SM, Nguyen J, Nance RN, Ruderman S, Delaney JAC, Crane HM, Fredericksen RJ, Patient perceptions and understanding of a housing status measure for use in HIV care, in 27th Annual Conference of International Society of Quality of Life. 2020: online. [Google Scholar]
- 39.World Health Organization. Adverse Childhood Experiences International Questionnaire. Adverse Childhood Experiences International Questionnaire (ACE-IQ) 2018; Available from: http://www.who.int/violence_injury_prevention/violence/activities/adverse_childhood_experiences/en/ [Google Scholar]
- 40.Dokkedahl SB, et al. , The psychological subtype of intimate partner violence and its effect on mental health: a systematic review with meta-analyses. Syst Rev, 2022. 11(1): p. 163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cafferky BM, Mendez M Anderson JR, Stith SM, Substance use and intimate partner violence: a meta-analytic review. Psychology of Violence, 2016. [Google Scholar]
- 42.Bacchus LJ, et al. , Recent intimate partner violence against women and health: a systematic review and meta-analysis of cohort studies. BMJ Open, 2018. 8(7): p. e019995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stubbs A and Szoeke C, The Effect of Intimate Partner Violence on the Physical Health and Health-Related Behaviors of Women: A Systematic Review of the Literature. Trauma Violence Abuse, 2022. 23(4): p. 1157–1172. [DOI] [PubMed] [Google Scholar]
- 44.Meyer JP, Springer SA, and Altice FL, Substance abuse, violence, and HIV in women: a literature review of the syndemic. J Womens Health (Larchmt), 2011. 20(7): p. 991–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Perone HR, et al. , Intimate partner violence: analysis of current screening practices in the primary care setting. Fam Pract, 2022. 39(1): p. 6–11. [DOI] [PubMed] [Google Scholar]
- 46.Morse DS, et al. , “They told me to leave”: how health care providers address intimate partner violence. J Am Board Fam Med, 2012. 25(3): p. 333–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Thompson MA, et al. , Primary Care Guidance for Persons With Human Immunodeficiency Virus: 2020 Update by the HIV Medicine Association of the Infectious Diseases Society of America. Clin Infect Dis, 2021. 73(11): p. e3572–e3605. [DOI] [PubMed] [Google Scholar]
- 48.Blasco-Ros C, Sanchez-Lorente S, and Martinez M, Recovery from depressive symptoms, state anxiety and post-traumatic stress disorder in women exposed to physical and psychological, but not to psychological intimate partner violence alone: a longitudinal study. BMC Psychiatry, 2010. 10: p. 98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.O’Doherty LJ, et al. , Screening women for intimate partner violence in healthcare settings: abridged Cochrane systematic review and meta-analysis. BMJ, 2014. 348: p. g2913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.El Morr C and Layal M, Effectiveness of ICT-based intimate partner violence interventions: a systematic review. BMC Public Health, 2020. 20(1): p. 1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Crane HM, et al. , HIV provider documentation and actions following patient reports of at-risk behaviors and conditions when identified by a web-based point-of-care assessment. AIDS Behav, 2017. 21(11): p. 3111–3121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sharma P, et al. , Evaluation of point-of-care PRO assessment in clinic settings: integration, parallel-forms reliability, and patient acceptability of electronic QOL measures during clinic visits. Qual Life Res, 2016. 25(3): p. 575–83. [DOI] [PubMed] [Google Scholar]
- 53.Stover A, et al. , Integrating patient-reported outcome measures into routine cancer care: cancer patients’ and clinicians’ perceptions of acceptability and value. EGEMS (Wash DC), 2015. 3(1): p. 1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jones J, et al. , Acceptability and willingness among men who have sex with men (MSM) to use a tablet-based HIV risk assessment in a clinical setting. Springerplus, 2014. 3: p. 708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fredericksen RJ, et al. , Provider perceptions of the value of same-day, electronic patient-reported measures for use in clinical HIV care. AIDS Care, 2016: p. 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fredericksen RJ, et al. , Patient acceptability and usability of a self-administered electronic patient-reported outcome assessment in HIV care: relationship with health behaviors and outcomes. AIDS Care, 2021. 33(9): p. 1167–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Short D, et al. , Utility and Impact of the Implementation of Same-Day, Self-administered Electronic Patient-Reported Outcomes Assessments in Routine HIV Care in two North American Clinics. AIDS Behav, 2022. 26(7): p. 2409–2424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Miller DP Jr., et al. , Universal Screening in Primary Care Practices by Self-administered Tablet vs Nursing Staff. JAMA Netw Open, 2022. 5(3): p. e221480. [DOI] [PMC free article] [PubMed] [Google Scholar]


