Abstract
The extensive history of pandemics has spanned many centuries, profoundly impacting societies, economies, and public health, and thereby shaping the course of history in various ways. Advances in medicine, science, and public health practices have played a pivotal role in mitigating the effects of pandemics over time. This review explores the scientific landscape of contemporary pandemics, examining their diverse and complex nature. It goes beyond the biological aspects of pandemics to consider socioeconomic, environmental, and technological factors. Through a scientific lens, this study aims to understand the complexities of pandemics and contribute to the expanding knowledge base that helps humanity strengthen its defenses against global health threats. By elucidating the enigmas of pandemics, the study hopes to foster a more resilient and prepared global health environment. Highlighting the importance of a multidisciplinary, cross-disciplinary, and transdisciplinary approach, this exploration emphasizes the critical need to integrate biological, socioeconomic, environmental, and technological domains to develop more robust defenses against these global health challenges.
Keywords: Collaboration, Interdisciplinary, Multiagency, Pandemics
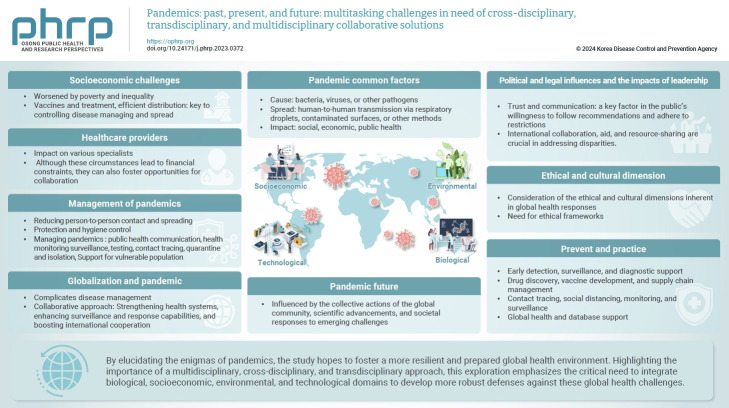
Graphical abstract
Introduction
Pandemics represent a significant global health challenge, punctuating human history with indelible marks on societies and reshaping the trajectory of public health. From the Spanish flu of 1918 to the more recent coronavirus disease 2019 (COVID-19) pandemic, these events are characterized by the widespread and sustained transmission of infectious agents, causing pervasive illness and societal disruption. They underscore the vulnerability of human populations to infectious diseases [1–3]. These historical events serve as stark reminders of the diverse and profound impacts that pandemics have on societies, economies, and cultures across centuries [3].
At the core of pandemics lies the science of infectious diseases, which involves a complex interplay among pathogens, hosts, and the environment. It is crucial to understand the modes of transmission, the role of reservoirs, and the factors that influence the evolution of virulence. Zoonotic spillover events, in which pathogens jump from animals to humans, are key drivers in the emergence of novel infectious diseases. Moreover, the globalized nature of our interconnected world, enhanced by international travel and trade, plays a critical role in the rapid spread of these agents across borders [1,3]. Although there has been progress in understanding the biological mechanisms and immediate responses to pandemics, a significant gap remains in addressing their broader socioeconomic, environmental, technological, and ethical impacts. These factors have the potential to either effectively manage or mismanage a pandemic, as will be discussed in the following sections [4].
The Social, and Psychological Impacts of Pandemics
The socioeconomic and psychological impacts of pandemics are profound, altering human behaviors, exacerbating mental health challenges, and inducing significant shifts in societal norms [5,6]. For example, sleep disorders are conditions with both psychological and socioeconomic repercussions. In their study, Checa-Ros et al. [7] identified 4 distinct patterns of melatonin production and excretion among children with sleep disorders. A few years later, Choudhry et al. [8] reported that insomnia significantly affected patients who had recovered from COVID-19, necessitating consultation and treatment to mitigate long-term consequences. Melatonin, which is synthesized by the pineal gland, is known for its anti-inflammatory, antioxidant, and immunomodulatory activities. Its antiviral properties, cost-effectiveness, minimal side effects, and particularly its ability to enhance humoral immunity by suppressing inflammatory products and boosting the immune system—especially when activity is low or suppressed—make it a potential adjuvant in the treatment of COVID-19. Molina-Carballo et al. [9] demonstrated its effectiveness as a therapeutic alternative for treating COVID-19 infection in a systematic review conducted in 2022. Although further clinical trials are recommended, these studies illustrate how the psychosocial impacts of the pandemic can be linked to its socioeconomic burden and broader effects on public health. They also highlight how scientific and technological advancements targeting specific conditions may contribute to innovative solutions in pandemic management.
Climate and Environmental Changes
Climate hazards impact the spread of infectious diseases through various direct and indirect mechanisms. These mechanisms include gradual increases in temperature, environmental changes that facilitate the proliferation of disease vectors such as mosquitoes, rodents, and ticks, and sudden extreme events such as floods. Floods can lead to the contamination of drinking water sources and the displacement of humans and animals, both of which can carry and transmit pathogens. The growing threat of climate change and environmental degradation introduces additional complexity, potentially hastening the emergence of new infectious diseases [10,11]. This interconnection underscores the urgent need for an environmentally conscious approach to pandemic preparedness and response.
Technology, Innovation, and Pandemic Prevention
Innovative treatments and preventive measures play a crucial role in managing pandemics. The 2022 systematic review by Molina-Carballo et al. [9] highlights the protective effects of melatonin administration against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and its potential inclusion in treatment protocols as an innovative approach. Furthermore, technological advancements, especially in artificial intelligence (AI) and big data, are revolutionizing our ability to track, predict, and manage pandemic scenarios, providing essential support to vulnerable populations [12–14].
Ambient intelligence represents an emerging concept where information technology is employed to establish networks of interconnected devices and services. These networks dynamically collaborate to assist individuals in various activities. A recent study focusing on security-enhanced ambient assisted living that supports school activities during hospitalization illustrates how this technology can help mitigate the broader socioeconomic impacts of pandemics [15]. By facilitating educational activities and addressing ethical concerns, while also enhancing the ability to provide care under diverse conditions, such technologies ensure that vulnerable populations receive the necessary support during health crises [12,15].
Ethical Aspects of Pandemics
Ethical considerations are paramount during pandemics. Balancing public health measures with individual freedoms, ethically allocating scarce medical resources, and addressing global health inequities present challenges that require thoughtful and humane responses [16,17]. Understanding these dimensions has profound implications for societal resilience and sustainability.
The interplay between these factors and pandemics is crucial for devising holistic strategies, yet it is often underexplored in current literature [4]. This study aims to address gaps in pandemic preparedness by comprehensively exploring various dimensions, enhancing global health systems, supporting sustainable development goals (SDGs), and improving our ability to manage future pandemics [5,11,17]. A multidisciplinary approach is essential, integrating insights from virology, public health, technology, economics, and social sciences [4,11,12,17] to better predict, prevent, and respond to global health threats in an informed and sustainable manner. This review covers pandemics biological, socioeconomic, environmental, and technological aspects, emphasizing the need for a multidisciplinary approach to strengthen defenses against global health threats [18–20].
Materials and Methods
This narrative literature review was conducted to provide a comprehensive understanding of the evolution of pathogens, societal responses, and the natural interplay between infectious agents and human populations [21]. Traditional academic and clinical training typically prepares clinicians and researchers for one-on-one interactions with patients. However, the broader public health challenges presented by pandemic care require decision-makers to adopt a multidisciplinary, cross-disciplinary, and transdisciplinary approach to population-based issues, which is often unfamiliar to most.
Search Strategy
We meticulously crafted a systematic search strategy to explore the pandemic’s socioeconomic, technological, and environmental dimensions. Using major databases such as PubMed, Scopus, and Web of Science, we employed predefined keywords either in isolation or in combination. Furthermore, we implemented “practical action research” to analyze the outcomes and simultaneously investigate emerging insights during our analysis [22]. This approach provided a blend of operational and critical reflection through action research, utilizing a spiral of “planning-acting-observing-reflecting.” It allowed us to contextualize the existing pandemic response, question why certain gaps exist, and explore potential improvement strategies based on practical performances.
To ensure a comprehensive review, we also examined the reference lists of identified studies to uncover any potentially overlooked works, thereby minimizing the risk of missing relevant literature. The selection criteria were designed to capture the most recent and pertinent insights into pandemic research, with a focus on studies that offered novel perspectives on the socioeconomic, technological, or environmental aspects of pandemics. This thorough and targeted approach to the literature review facilitated the collection of a diverse and robust body of evidence, which served as the cornerstone of our analysis.
Keywords
The following keywords were used alone or in combination: pandemics, infectious diseases, public health responses, and societal impact. Each keyword was isolated during database searches to reduce the number of hits.
Search Strings
The search strings used for all databases were: pandemics (AND) infectious (AND) diseases (AND) public (AND) health (AND) responses (AND) societal (AND) impacts.
Inclusion and Exclusion Criteria
The inclusion criteria encompassed peer-reviewed studies published in English, without any time limitations, focusing on the epidemiology, public health responses, and social implications of pandemics. Studies that did not directly address these themes or lacked empirical data were excluded.
Data Analysis and Extraction
Data extraction concentrated on the objectives, methodologies, key findings, and conclusions of each study. This information underwent qualitative analysis to identify common themes, trends, and divergences within the literature. The quality of each study was evaluated based on its methodology, potential biases, and the reliability of its findings.
Data Selection
Studies were selected through a review of their titles and abstracts. Two authors independently assessed all the compiled documents, striving to reach a consensus. When disagreements arose regarding the inclusion of a study, a third author was consulted to make the final decision. The findings were thematically organized and summarized under relevant subheadings [23], offering a structured overview of the current understanding of pandemics.
Results
The initial search yielded the following 26 results from PubMed, 16 from Scopus, and 30 from Web of Science. Given the “action research” design of our study, we adopted a dynamic approach that allowed for the continuous incorporation of new studies, thus increasing the total number of papers included. Although this strategy was time-consuming, it enabled us to address immediate issues by practically exploring published solutions. This approach was particularly effective in evaluating existing systems and implementing new changes.
Of the 72 studies retrieved from the search, 22 were duplicates, 31 were irrelevant, and 5 were excluded for other reasons. Additional studies were identified and included after reviewing the reference lists of the papers initially selected or as deemed necessary upon further reading. The compiled studies were evaluated for eligibility, and examined in detail. All papers that met the inclusion criteria were utilized (see the reference section). Finally, the content from the included articles was organized into various categories reflecting their differences and similarities.
Pandemics’ Etiology and Impacts: From Past to Present
Pandemics have had profound impacts on societies, economies, and public health throughout the centuries. Advances in medicine and public health practices have helped to mitigate their effects. Table 1 summarizes the major pandemics in history [2,20–33].
Table 1.
A brief overview of some major pandemics throughout history
| Name | Time | Comment |
|---|---|---|
| Antonine Plague [25] | 165–180 AD | Believed to be caused by either smallpox or measles, this pandemic affected the Roman Empire during the reign of Marcus Aurelius. |
| Justinian Plague [26] | 541–542 AD | This pandemic, possibly caused by the Yersinia pestis bacterium (which also causes the bubonic plague), affected the Byzantine Empire and contributed to the decline of the Eastern Roman Empire. |
| The Black Death [27] | 1347–1351 | One of the most devastating pandemics in human history, the Black Death was caused by the Yersinia pestis bacterium. It swept through Europe, Asia, and North Africa, leading to the death of millions of people. |
| Third cholera pandemic [28] | 1852–1860 | Cholera, caused by the Vibrio cholerae bacterium, spread from India to Asia, Europe, North America, and Africa, causing significant mortality and social disruption. |
| Spanish flu [29] | 1918–1919 | The H1N1 influenza A virus caused the Spanish flu, which infected about one-third of the world’s population and resulted in an estimated 50 million deaths worldwide. It was unique for its high mortality among young, healthy adults. |
| Asian flu [30] | 1957–1958 | The H2N2 influenza A virus caused the Asian flu, which originated in East Asia and spreading globally. It resulted in an estimated 1–2 million deaths worldwide. |
| HIV/AIDS pandemic [31] | 1981–present | The HIV causes AIDS. This pandemic has had a profound impact globally, with millions of people infected and millions of deaths since it was first identified in the early 1980s. |
| H1N1 influenza pandemic [32] | 2009–2010 | The H1N1 influenza A virus, also known as swine flu, spread globally and resulted in an estimated 151,700–575,400 deaths. |
| COVID-19 pandemic [33] | 2019–present | The coronavirus SARS-CoV-2, which causes COVID-19, was first identified in Wuhan, China, in late 2019. The virus quickly spread worldwide, leading to widespread illness, social and economic disruptions, and significant loss of life. |
HIV, human immunodeficiency virus; AIDS, acquired immunodeficiency syndrome; COVID-19, coronavirus disease 2019; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Despite their unique characteristics, pandemics share several common factors: they are typically caused by bacteria, viruses, or other pathogens and often spread through human-to-human transmission via respiratory droplets, contaminated surfaces, or other methods. The rapid spread of infectious diseases is facilitated by global travel, connectivity, and trade, which pose significant challenges to containment efforts [25–33]. Additionally, the high population density in urban areas, characterized by crowded living conditions and close contact, further accelerates the transmission of diseases [2,25–33]. Novel or highly mutative infectious agents often encounter populations that lack pre-existing immunity, thereby increasing susceptibility and facilitating the spread of the disease. Previous research suggests that certain cultural groups may temporarily experience either advantages or disadvantages in disease outcomes [2,18,19,34].
Delays in detecting and responding to new pathogens have historically facilitated widespread transmission. The capacity and resilience of healthcare systems play a crucial role in effective disease management and control. Understanding these common factors is essential for developing public health strategies and preparedness to mitigate future pandemics. Global cooperation, early detection, rapid response, and investment in healthcare infrastructure are vital for effective pandemic responses [4,6,20].
Socioeconomic Challenges
Socioeconomic factors such as poverty, limited or inadequate access to healthcare, and societal inequalities can exacerbate the effects of pandemics. Vulnerable populations are often disproportionately impacted. The availability of vaccines and effective treatments plays a significant role in shaping the trajectory of a pandemic. The development, production, and distribution of vaccines and treatments are essential for controlling the spread of infectious diseases [2,4,19,27,35–37].
Healthcare providers
While the immediate focus during a pandemic is typically on the relevant infectious diseases, its impact spreads widely, significantly affecting various other medical specialties, healthcare staff, their productivity, and the availability of financial resources [38]. Although these circumstances lead to financial constraints, they can also foster opportunities for collaboration [4,5,20,33,35].
Specialist care
Infectious disease specialists and epidemiologists are at the forefront of managing and controlling the spread of diseases. They provide patient care and implement public health measures. Public health experts engage in surveillance activities and communicate with the public to prevent further transmission. Pediatric infectious disease specialists focus on the specific needs of children, including how the disease presents, potential complications, and vaccination strategies tailored for pediatric populations. Rheumatologists and immunologists modify treatments for particularly vulnerable patients. Neurologists address neurological complications, whereas respiratory specialists manage conditions such as acute respiratory distress syndrome and pneumonia. Cardiologists may encounter an increase in cardiovascular complications, and disruptions in cancer care are also possible. Primary care physicians triage patients and address non-pandemic-related health issues, while dentists enforce infection control protocols. Psychiatrists provide support for individuals dealing with increased stress and mental health challenges during pandemics [37–41]. Pandemics can cause a significant increase in the number of critically ill patients, which places immense pressure on critical care and emergency medicine services. Intensive care units may face a higher demand for ventilators, medical staff, and specialized equipment. Although there is a decrease in trauma care admissions, the pattern and quality of care generally remain unchanged [42].
Socioeconomic impacts on healthcare
This interconnected network of experts and specialists could provide an opportunity to enhance high-quality care and alleviate financial burdens if structured collaboratively [43,44]. Understanding the broad socioeconomic impacts of pandemics is essential for comprehensive pandemic preparedness and response. Pandemics test the frontline specialties that directly handle infectious agents and impose extraordinary demands on the entire healthcare ecosystem, underscoring the importance of a holistic approach to managing global health crises with sufficient human and financial resources.
Nevertheless, pandemics can also drive innovation and lead to unique solutions by utilizing a multiagency workforce to establish new response units and transform financial losses into successful projects. A recent study from Thailand exemplifies this. A home isolation care center was created, employing a team with diverse specialties and backgrounds to diagnose, treat, and provide daily care to around 6,000 COVID-19 patients, demonstrating the effectiveness of a flexible surge capacity concept [43,44]. Healthcare administrators play a pivotal role in managing resources during a pandemic. This includes distributing medical supplies, coordinating staff, and overseeing the overall operation of healthcare facilities. Their actions underscore the necessity for flexibility within the healthcare system [44].
Medical research and education
During a pandemic, the focus of medical research often shifts to prioritize understanding the infectious agent, developing treatments and vaccines, and investigating the long-term health effects of the disease. Concurrently, medical education programs may experience disruptions, including alterations in clinical rotations, the implementation of virtual learning, and adjustments to the training schedules of medical students, residents, and fellows [45–47].
Management of pandemics
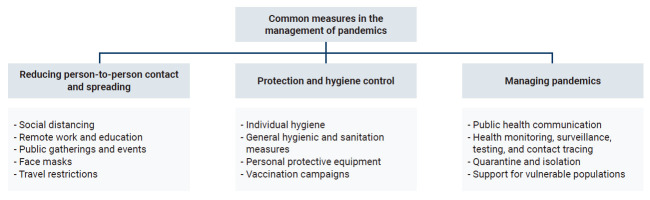
Various measures have been implemented worldwide to control the spread of infectious diseases, including pandemics such as COVID-19. Public health authorities and governments often recommend these measures to mitigate the disease’s impact. Although the specific strategies may differ depending on the pathogen's nature, Figure 1 illustrates some common measures, which include several subgroups [2,4,5,18,36,48–52].
Figure 1.
Common measures in the management of pandemics.
Public and individual approaches
The primary approach focuses on minimizing person-to-person contact and the associated risks of transmission by encouraging individuals to maintain physical distance, particularly in crowded areas [48,49]. This includes implementing strategies such as reducing the capacity of public spaces, ensuring spacing on public transportation, and promoting remote and online work options to decrease the number of people in workplaces and educational settings. Additionally, large gatherings, events, and festivals are either limited or prohibited to mitigate the risk of virus spread. When gatherings do occur, it is crucial to implement protocols that ensure they are conducted safely [50,51]. Moreover, the use of face masks is recommended or mandated in public settings, especially where maintaining physical distance is difficult [52]. Further measures include implementing travel restrictions, such as border closures, quarantine requirements for travelers, and limitations on both international and domestic travel [3,4,53–55].
Promoting regular and thorough handwashing with soap and water for at least 20 seconds, along with the use of hand sanitizers containing at least 60% alcohol when soap and water are unavailable, are key measures for individual protection. Additionally, implementing enhanced cleaning and sanitation protocols in public spaces, transportation systems, and high-touch surfaces addresses environmental safety [51,56]. Ensuring the availability and proper use of personal protective equipment, such as masks, gloves, and gowns, in healthcare settings and other high-risk environments, is crucial for combining protective measures at home and work, in addition to vaccination [51,52]. Vaccination campaigns aimed at achieving widespread immunity are essential for reducing the severity of illnesses in the population. Individuals should be encouraged to receive recommended vaccinations to prevent other infectious diseases [52-54].
Public communication and information
Public and individual measures are costly and require a motivated and informed public. A Japanese study found that vaccine efficacy, lifetime immunity, and fear of the pandemic positively influenced the public's willingness to use a vaccine. Conversely, the high cost of vaccines and potential side effects and toxicity negatively impacted their acceptance [52,55]. Managing the pandemic partly relies on clear and transparent communication about the pathogen, preventive measures, and the evolving situation. It is imperative to disseminate accurate information through various channels to combat misinformation and to conduct widespread testing to identify and isolate infected individuals.
Health monitoring systems and robust contact tracing are essential tools for identifying and alerting people to emerging hot spots and potential exposures to the virus. Technologies such as mobile apps have proven effective for both health monitoring and contact tracing. Quarantine measures are implemented for individuals who have either been exposed to the virus or have traveled from areas deemed high-risk. Those who test positive are isolated to prevent the virus from spreading further [2,23,53,54]. These strategies are often used in tandem and can be adapted based on the changing circumstances, scientific insights, and recommendations from public health experts. Individuals and communities must stay informed and follow the guidelines issued by public health authorities to help curb the spread of infectious diseases. Additionally, support and resources must be made available to vulnerable groups, including the elderly, those with pre-existing health conditions, and individuals experiencing economic difficulties.
The use of social media
Social media has been tested as a tool for communication and information to raise public awareness and track infected individuals during recent pandemics. These platforms play a vital role in shaping public sentiment and significantly influence behavior during public health emergencies [55]. Generally, public behavior and acceptance of rules and recommendations hinge on a trustworthy relationship with authorities and governments. Establishing such a relationship well before a pandemic is crucial to ensure the full implementation of all measures [56].
The inevitable public-politic-professional triangle
The successful management of a pandemic relies on a robust relationship among professionals, authorities, and the public. Research conducted during the recent COVID-19 pandemic has revealed a dynamic shift in public reactions over time [55]. Initially, there was a strong sense of unity, which later shifted to attributing the ongoing crisis to specific causes. As the pandemic continued, doubts about the efficacy of stringent precautionary measures grew, compounded by concerns over economic hardships and mental health issues. This progression led to increased worries about social vulnerabilities, prompting public scrutiny and criticism of government restrictions amid feelings of anxiety and confusion. Effective public health communication about COVID-19 should emphasize transparency and tackle issues related to health equity and social justice. Adopting this strategy can cultivate a sense of both individual and collective responsibility essential for protecting the public against the pandemic [53].
Another study revealed a significant trend of healthcare avoidance among the general population, particularly during the COVID-19 outbreak, indicating an underutilization of healthcare services. However, the findings also highlighted disparities in healthcare avoidance among various societal groups, with specific demographic characteristics disproportionately affected [54]. These studies provide insights into the socioeconomic patterns of healthcare utilization during emerging infectious disease outbreaks, thereby assisting public health emergency management in developing strategies to improve healthcare system preparedness, supported by more accurate financial estimations.
Globalization and pandemic
Globalization, which is characterized by increased connectivity and interdependence among countries, has both spurred advancements and introduced distinct challenges in public health, particularly in the context of pandemics. Table 2 outlines various ways in which globalization can affect the dynamics of infectious disease transmission [4,5,57,58].
Table 2.
Positive and negative aspects of globalization in pandemics
| Positive aspect | Negative aspect | |
|---|---|---|
| Increased travel and connectivity | Globalization has facilitated increased travel and connectivity, enabling the exchange of goods, ideas, and cultures. This has contributed to economic growth, cultural exchange, and scientific collaboration. | The increased movement of people also means that infectious agents can spread more rapidly across borders. An individual infected with a pathogen in one part of the world can travel to another, potentially introducing and spreading the disease in new regions. |
| Global trade and supply chain | Global trade and supply chains have led to economic development, increased access to diverse goods and services, and promoted the transfer of technology. | Disruptions in supply chains can impact the availability of essential medical supplies, medications, and equipment during a pandemic, posing challenges for healthcare systems. |
| Urbanization and population density | Globalization has been associated with urbanization and the concentration of populations in urban centers, leading to economic opportunities and improved living standards. | High population density in urban areas can promote the rapid spread of infectious diseases, especially in the absence of effective public health measures. |
| Environmental changes | Globalization has contributed to advancements in technology, science, and environmental conservation. | Activities associated with globalization, such as deforestation, habitat destruction, and climate change, can alter ecosystems and increase the risk of disease spillover from animals to humans, leading to the emergence of novel pathogens. |
| Information exchange and awareness | Globalization has enabled rapid information exchange, scientific collaboration, and the dissemination of health-related information. | Misinformation can also spread quickly, influencing public perceptions and responses during a pandemic. |
| International cooperation in healthcare | Globalization has facilitated international cooperation in healthcare, research, and the development of medical technologies. | Challenges in international coordination and cooperation may arise during a pandemic, affecting the equitable distribution of resources and access to medical interventions. |
Globalization has accelerated economic growth and cultural exchange but also presents significant public health challenges. Addressing these challenges requires leveraging the strengths of global connectivity for international healthcare cooperation and rapid information exchange, to manage infectious diseases. It is essential to mitigate the negative consequences of globalization, including environmental degradation and rapid urbanization, which fuels new pathogens. While globalization brings benefits, it also complicates disease management, necessitating coordinated global health efforts. Strengthening health systems, enhancing surveillance and response capabilities, and boosting international cooperation are crucial to counter pandemics in our interconnected world [48,57,58].
The response to the COVID-19 pandemic varied significantly across countries, influenced by several factors including healthcare infrastructure, governance, and public adherence to health measures [57]. Assessing how effectively a country managed COVID-19 pandemic involves considering a range of factors such as testing capacity, healthcare infrastructure, public health measures, governance, and public compliance. The success of pandemic management is also shaped by the evolving nature of the virus and the effectiveness of the response strategies. It is important to recognize that opinions on the success of a country’s response can differ, and the situation continues to evolve [57,58]. Despite this, some countries have been frequently recognized for their efficient handling of the COVID-19 pandemic. Table 3 lists these countries along with their response measures, illustrating the variety of strategies different countries have implemented to manage the pandemic [56–65].
Table 3.
The countries that have been most frequently cited for their effective management of the COVID-19 pandemic
| Country | Measures | Summary |
|---|---|---|
| New Zealand [61] | Swift and strict measures: New Zealand implemented strict lockdown measures early in the pandemic, closing its borders and implementing a nationwide lockdown. The government’s approach focused on eliminating the virus rather than merely containing it. | Command and control, safety, communication |
| Effective communication: Clear and consistent communication from Prime Minister Jacinda Ardern and health officials helped build public trust and compliance with health measures. | ||
| Isolation and quarantine: The country implemented effective isolation and quarantine measures for incoming travelers. | ||
| Taiwan [62] | Early action and surveillance: Taiwan took early and aggressive measures to control the spread of the virus, including comprehensive testing, contact tracing, and quarantine measures. | Command and control, safety, communication |
| Experience from SARS: Taiwan’s experience with the SARS epidemic in 2003 contributed to a well-prepared and responsive healthcare system. | ||
| Technology and data integration: The use of technology for contact tracing and integrating data from various sources facilitated a targeted and efficient response. | ||
| Australia [63] | Stringent border controls: Australia implemented strict border controls and quarantine measures for international arrivals. | Command and control, safety, communication, collaboration |
| Effective testing and contact tracing: Australia had a robust testing and contact tracing system, contributing to the early detection and containment of outbreaks. | ||
| Regional collaboration: Collaboration between different states and territories in Australia allowed for coordinated responses. | ||
| Vietnam [64] | Proactive measures: Vietnam implemented proactive measures, including widespread testing, contact tracing, and quarantine for affected individuals. | Command and control, safety, communication, collaboration |
| Effective communication: Clear communication from the government and public health authorities contributed to public understanding and compliance. | ||
| Community engagement: Vietnam emphasized community engagement and mobilization in its response efforts. | ||
| Republic of Korea [65] | Mass testing and contact tracing: Republic of Korea implemented widespread testing, extensive contact tracing, and technology-driven solutions to identify and isolate cases. | Command and control, safety, communication |
| Transparent communication: Transparent communication, including the use of mobile apps for real-time information, helped keep the public informed. | ||
| Experience from previous outbreaks: Previous experiences with outbreaks like MERS influenced the country’s preparedness and response strategies. |
COVID-19, coronavirus disease 2019; SARS, severe acute respiratory syndrome; MERS, Middle East respiratory syndrome.
Common threads in these successful responses include early and decisive action, effective use of technology, transparent communication, and strong community engagement. These elements were instrumental in controlling case numbers and minimizing the overall impact on public health, the economy, and societal well-being [59–65]. Recognizing the dynamic nature of pandemics, the factors contributing to success or challenges can evolve over time. Moreover, the success of a country’s response should not be judged solely by the number of cases but also by the overall impact on public health, economic stability, and societal resilience. Public health experts continue to analyze and learn from various countries’ responses to better inform future pandemic preparedness and response efforts.
Global interconnectedness necessitates a collaborative approach to address global health threats. To manage pandemics effectively, it is essential to strengthen international health systems, enhance surveillance and response capabilities, and foster global cooperation. However, political and legal issues at both national and international levels may impede such collaborative efforts.
Political and legal influences and the impacts of leadership
It has become increasingly evident that leadership, especially political leadership, plays a crucial role in managing emergencies and pandemics [4,57,66]. A key factor in the public’s willingness to follow recommendations and adhere to restrictions is the level of trust between the population and their political leaders [66–71]. Information and communication technology has facilitated the faster dissemination of news than ever before. Consequently, accurate and timely communication and information sharing from political leaders are invaluable.
In addition, political leadership should respect scientific leadership as the frontline in combating emergencies and pandemics. It is essential to receive updated and accurate information from international authorities like the World Health Organization (WHO). Additionally, implementing coherent response strategies, restoring and extending a second line of preventive measures, maintaining a united front, and embracing the One Health concept, along with providing financial support for prevention and response at various levels, are all crucial [71–74]. The legal definition of pandemics, such as COVID-19, has become a topic of national discussion in several countries. Such changes may lead to stricter regulations concerning the diagnosis, treatment, and follow-up of the disease, as well as the implementation of preventive measures [48,73].
The impacts of national institutional infrastructure vary between high-income countries (HICs) and low and middle-income countries (LMICs), covering economic, social, political, and technological dimensions. It is crucial to recognize that these terms are generalizations that may oversimplify the intricate realities of individual countries. Furthermore, the classification of countries into the “LMIC” or “HIC” categories is determined by various criteria, including gross domestic product per capita, infrastructure, education, healthcare, and other indicators. Table 4 illustrates some of the differences between these nations [57,60,70,74,75].
Table 4.
Differences in status in selected areas between high-income and low- and middle-income countries
| Status | High-income countries | Low- and middle-income countries |
|---|---|---|
| Economic | Generally, have high-income economies with well-established industries, advanced technology, and diverse service sectors. Examples include the United States, Germany, Japan, and Australia. | Tend to have lower-income economies, with a focus on agriculture, manufacturing, and resource extraction. They may have emerging industries and face challenges related to economic development. Examples include India, Nigeria, and Bangladesh. |
| Infrastructure | Typically, have advanced and well-maintained infrastructure, including modern transportation systems, reliable energy networks, and widespread access to technology. | Often face challenges in infrastructure development, with issues such as inadequate transportation, limited access to electricity, and less widespread technology adoption. |
| Education and healthcare | Generally, have well-established and accessible education and healthcare systems. There is often a higher literacy rate, and life expectancy tends to be longer. | May face challenges in providing universal access to quality education and healthcare. Issues such as limited resources, inadequate infrastructure, and health disparities can be more pronounced. |
| Political stability | Tend to have stable political systems with established democratic institutions, the rule of law, and low levels of political violence. | Political stability can vary widely, and some nations may experience political instability, governance challenges, and conflicts. |
| Technology and innovation | Are often at the forefront of technological innovation, with advanced research and development capabilities and a high level of technology adoption. | May face challenges in adopting and developing advanced technologies, although there can be pockets of innovation and efforts to bridge the technological gap. |
| Income inequality | Often have social safety nets and policies aimed at addressing disparities, despite the existence of income inequality. | Income inequality can be more pronounced, with limited resources and challenges in implementing effective social welfare programs. |
| Access to basic services | Generally, provide widespread access to basic services such as clean water, sanitation, and electricity. | May face challenges in ensuring universal access to these basic services, contributing to issues related to public health and quality of life. |
It is important to approach these distinctions with nuance, acknowledging that countries exist on a spectrum influenced by governance, historical context, and cultural factors. Many countries are actively striving to transition from developing to developed status through various economic and social initiatives. These differences profoundly impact their capacity to manage pandemics, affecting healthcare infrastructure, governance, resource accessibility, and overall response capacity [74,75]. Table 5 summarizes some of the ways these differences influence pandemic management.
Table 5.
Differences in management between high-income and low- and middle-income countries
| High-income countries | Low- and middle-income countries | |
|---|---|---|
| Healthcare infrastructure | Typically, have more robust and well-established healthcare systems with advanced medical facilities, a higher number of healthcare professionals, and better access to medical equipment and supplies. | May face challenges with limited healthcare infrastructure, fewer healthcare professionals, and inadequate medical resources. This can impact the capacity to diagnose, treat, and manage the spread of infectious diseases. |
| Access to testing and diagnostics | Often have better access to diagnostic tools, testing facilities, and a more extensive network for mass testing. This facilitates early detection and containment efforts. | May experience delays in testing due to limited resources, leading to challenges in identifying and isolating cases promptly. |
| Public health response | Generally, have more sophisticated public health systems, which can facilitate coordinated responses, contact tracing, and the implementation of public health measures. | May face challenges in coordinating an effective public health response, including issues related to communication, resource allocation, and the implementation of widespread testing and contact tracing. |
| Economic impact and social support | Often have the financial means to implement economic stimulus packages and social support programs, helping individuals and businesses cope with the economic fallout of a pandemic. | May struggle to provide adequate economic support, leading to increased vulnerability among populations that rely on daily wages and have limited access to social safety nets. |
| Vaccine access and distribution | Typically, have greater resources to invest in developing vaccines, obtaining vaccine supplies, and implementing vaccination campaigns swiftly. | May face challenges in accessing vaccines, obtaining sufficient doses, and distributing them efficiently to the population due to financial constraints and logistical challenges. |
| Information technology and communication | Often have more advanced information technology infrastructure, facilitating communication, data collection, and the dissemination of accurate information during a pandemic. | May encounter difficulties in widespread communication, data collection, and information dissemination, leading to challenges in managing public perceptions and behaviors. |
| Logistical challenges | Generally, have better logistical capabilities to manage the distribution of medical supplies, establish testing centers, and implement quarantine measures. | May face challenges in logistics, including transportation, storage, and distribution of medical resources, which can impact the effectiveness of response efforts. |
| Population density and living conditions | Often have lower population density and better living conditions, enabling more effective implementation of social distancing measures. | May have higher population density, crowded living conditions, and challenges in implementing social distancing, leading to a higher risk of disease spread. |
International collaboration, aid, and resource-sharing are crucial in addressing disparities. Strengthening healthcare infrastructure, public health systems, and ensuring equitable access to resources and vaccines can improve global pandemic management [4]. Supporting LMIC nations in building resilience requires a comprehensive approach, including socioeconomic, health, and governance systems [44,49,67]. Investment should focus on critical infrastructure like transportation, energy, water, and sanitation as well as enhancing digital infrastructure, healthcare facilities, and education. Emphasizing literacy, workforce development, and health education empowers communities, while educational programs on disaster preparedness and updated pandemic response plans are crucial.
Strengthening governance is crucial for effective decision-making, combating corruption, and enhancing transparency. Establishing robust social safety nets and targeted programs to reduce poverty and inequality are crucial for supporting vulnerable populations. Community involving in decision-making promotes initiatives tailored to local needs and encourages economic diversification [43,44]. Encouraging the growth of small and medium-sized enterprises, facilitating access to finance, and implementing strategies for adapting to climate change are key to building resilience. International collaboration provides critical financial aid, technical expertise, and knowledge sharing. Emphasizing research, development, and technological advancements is vital. Building resilience requires long-term commitment from governments, communities, and the international community to address vulnerabilities and develop adaptive systems.
Ethical and cultural dimensions of the pandemic
Addressing the multifaceted challenges posed by pandemics requires consideration of the ethical and cultural dimensions inherent in global health responses [76]. The pandemic’s global reach has highlighted significant inequities in healthcare access, emphasizing the urgent need for ethical frameworks that prioritize fairness and equitable distribution of resources and treatments across diverse populations [77]. Furthermore, the cultural sensitivity of public health measures is of paramount importance.
Strategies must be adaptable to the diverse cultural contexts in which they are implemented, respecting local customs, beliefs, and practices [78]. This approach not only ensures the effectiveness of these measures but also fosters trust and cooperation among communities, which are essential for the successful management and mitigation of pandemics. Engaging local leaders and stakeholders during the planning and implementation phases of public health initiatives can provide invaluable insights into culturally appropriate practices, thereby enhancing the acceptability of and adherence to interventions designed to curb the spread of disease [79]. Moving forward, integrating ethical considerations and cultural competence into pandemic preparedness and response strategies will help address current disparities and strengthen the resilience of health systems to face future global health crises.
How to prevent subsequent pandemics?
Preventing subsequent pandemics requires a multifaceted and coordinated approach that involves various sectors such as public health, research, policy, technology, and global cooperation. Figure 2 illustrates the available preventive strategies and measures that could help prevent future pandemics [4,5,80–87].
Figure 2.
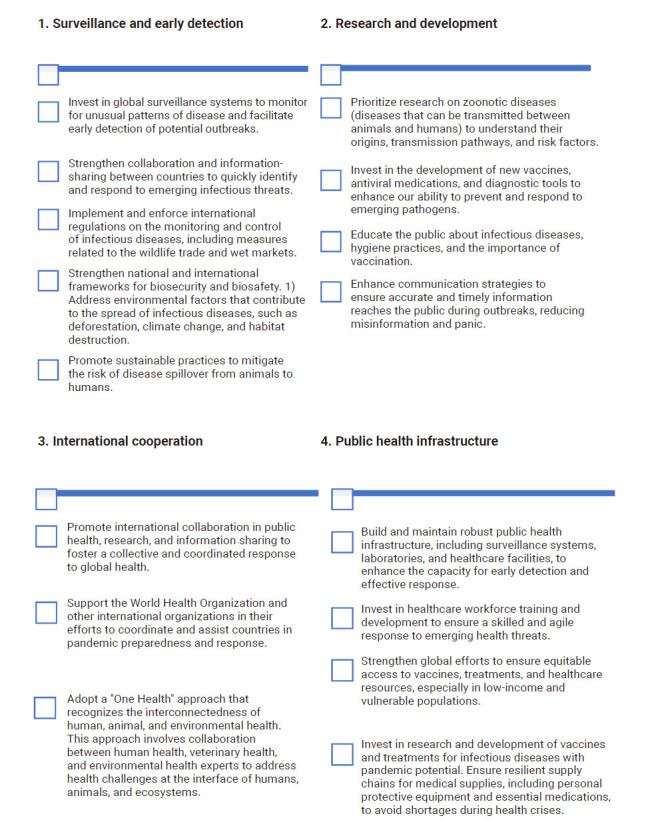
Pillars in the prevention of pandemics.
Preventing pandemics necessitates a sustained and collaborative effort on a global scale. Governments, international organizations, researchers, healthcare professionals, and the public each play essential roles in establishing a resilient and effective system for preventing, detecting, and responding to emerging infectious threats. Technological advancements have been pivotal in enhancing response strategies during recent pandemics. AI, data analytics, and digital health tools have become critical assets, significantly aiding in the management and prevention of pandemics by improving surveillance, early detection, response, research, and the ability to learn from past pandemics [88,89]. Below are some ways in which AI can be utilized in the context of pandemic management [81–83].
Early detection, surveillance, and diagnostic support
AI algorithms can analyze data from diverse sources, including social media, healthcare records, and environmental monitoring systems, to identify patterns and predict potential outbreaks before they become widespread [82]. These models are capable of forecasting the spread of infectious diseases, thereby assisting public health authorities in allocating resources and implementing targeted interventions effectively. Additionally, AI can simulate disease spread and model various scenarios, aiding policymakers in making well-informed decisions regarding interventions and resource distribution [85]. Machine learning algorithms utilize data from medical imaging, laboratory tests, and clinical symptoms to facilitate rapid and accurate diagnoses of infectious diseases. Furthermore, AI-powered chatbots can deliver real-time information, respond to inquiries, and provide preliminary screening for individuals concerned about their symptoms, thereby alleviating the pressure on healthcare hotlines.
Drug discovery, vaccine development, and supply chain management
AI can analyze existing drugs and identify potential candidates for repurposing to treat new or emerging diseases, thereby accelerating the drug development process. AI algorithms can also assist in the design of vaccines by predicting potential antigen structures and optimizing vaccine formulations [83,88]. Additionally, AI can optimize supply chain management by forecasting the demand for medical supplies and ensuring the timely production and distribution of essential resources, such as ventilators, masks, and vaccines.
Contact tracing, social distancing, monitoring, and surveillance
AI-powered contact tracing applications can identify and notify individuals potentially exposed to an infectious disease, facilitating targeted interventions and quarantine measures. AI technologies, including computer vision and machine learning, can monitor adherence to social distancing guidelines in public spaces. AI-powered telemedicine platforms and remote monitoring systems allow healthcare professionals to assess and monitor patients remotely, thereby reducing the risk of transmission in healthcare settings [80,90]. AI technologies can also analyze data from wildlife surveillance systems to monitor and predict potential disease spillover events. Additionally, AI can analyze environmental data to understand how factors like climate change and habitat destruction may contribute to the emergence of infectious diseases.
Public communication and education
AI-powered chatbots can distribute accurate information, analyze frequently asked questions, and guide the public, thereby helping to combat misinformation. AI can also analyze social media and news articles to assess public sentiment and address concerns in real time. AI systems must be designed with strong security measures to protect sensitive health data and to ensure compliance with privacy regulations [89]. Although AI presents significant opportunities in managing pandemics, it is vital to consider ethical issues, data privacy concerns, and to ensure that AI technologies are seamlessly integrated into existing public health frameworks to enhance collaboration and effectiveness. The development and deployment of AI tools must be carried out with transparency, accountability, and a commitment to addressing potential biases in the algorithms.
These technologies bolster current efforts to manage pandemics and provide important insights for future preparedness plans [91]. By incorporating these technological tools into public health strategies, we can improve global capabilities for predicting, preventing, and responding to pandemic threats.
How to implement scientific knowledge in practice?
Understanding the economic impacts of pandemics can guide policymakers in designing economic systems that are more resilient and capable of withstanding future health crises. Similarly, recognizing the role of environmental degradation in the emergence of pandemics underscores the importance of implementing sustainable practices and policies to prevent future outbreaks. Technologically, the critical role of digital health technologies and big data analytics in enhancing pandemic surveillance and response has been highlighted. Collectively, these transdisciplinary insights contribute to the global agenda of sustainable development by promoting health equity, enhancing preparedness, and fostering innovation in public health strategies.
Transdisciplinary teaching and cooperation extend beyond merely teaching across disciplines. They necessitate interdisciplinary collaboration to forge a cohesive relationship aimed at solving complex problems. This approach demands innovation, cooperation, and intentionality [92]. It should begin at the medical and public health school levels, incorporating major curriculum changes that are integrated with the foundational curriculum. Such contributions are essential for building a more resilient society, better prepared to manage future pandemics, and directly supporting several SDGs, including Good Health and Well-Being (SDG 3), Sustainable Cities and Communities (SDG 11), and Climate Action (SDG 13) [11,17].
Global health database support
Creating data dashboard to track and analyze pandemic dynamics facilitates faster decision-making and improved forecasts. Handling these datasets requires a multidisciplinary team of experts [40,84]. Raw data often collected indirectly by various organizations and nations, necessitates different expertise levels for accurate interpretation.
A practical approach involves establishing central units to store, interpret, and utilize data scientifically. These units would continuously upgrade collection methodsand monitor key information to enhance the management of the pandemic and improve national health outcomes” [40,84]. Organizations like the Centers for Disease Control may monitor regions, critically assess pandemic planning, prevention, and management, and share vital information globally to prepare for future outbreaks [40].
This type of international or inter-organizational relationship requires an intelligence system capable of real-time analysis of critical and dynamic data, including the essential components of surge capacity: staff, stuff, space, and systems. Additionally, the demographics of daily confirmed cases and other relevant information contribute to creating an adaptive and predictive system. This system provides clear insights into the changes and dynamics of the pandemic, continuously offering a basis for decision-making, preemptive deployment of control measures, and forecasting. As a result, time, resources, and lives are effectively saved, and adjustments are made to accommodate the impacts of cultural differences, habits, and patterns of social and population mobility [40,84–86].
Nevertheless, such a system faces challenges including data privacy concerns, legal discrepancies across different jurisdictions, and political obstacles. These issues highlight the need for a robust framework managed by international organizations such as the WHO and the United Nations (UN). Moreover, collaboration at international, national, and regional levels is essential. As data are collected and analyzed locally and regionally, it is imperative to facilitate the transfer of this information to an international platform. Here, authorities like the WHO and the UN could oversee the ongoing influx of data, which is crucial for global decision-making. Even at the local level, interpreting data and understanding its implications necessitates a collaborative effort involving multiple agencies [48,68].
The Future of Pandemics
Predicting the future of pandemics is inherently uncertain, yet certain trends can be anticipated based on existing knowledge and ongoing advancements in science, technology, and global health [62–69]. The risk of new infectious agents, such as viruses and bacteria, crossing from animals to humans (zoonotic spillover) continues to be a significant concern. Factors including habitat destruction, wildlife trade, and climate change may contribute to these spillover events. Enhanced awareness and insights gained from recent pandemics, such as COVID-19, could enhance global preparedness and response mechanisms.
Understanding the impact of environmental changes and climate-related factors on the emergence and spread of infectious diseases is likely to receive increased attention. Strategies aimed at mitigating the environmental drivers of pandemics may become crucial to global health initiatives. Strengthened global governance structures and greater international cooperation in public health could prove indispensable. Collaborative efforts may be prioritized to address gaps in pandemic preparedness and response [2,18,40,61].
International collaboration and coordination in detecting and managing outbreaks are likely to become more robust. Enhanced surveillance systems and early warning mechanisms, which include the use of AI and big data analytics, could enable quicker detection of potential outbreaks, facilitating more rapid response efforts. The increasing integration of technology, such as telemedicine, remote monitoring, and digital contact tracing, is expected to become more prevalent in pandemic management. These technologies can assist in early detection, healthcare delivery, and public health interventions. A continued shift toward a “One Health” approach, recognizing the interconnectedness of human, animal, and environmental health, may inform strategies for preventing and managing pandemics [73,86].
Ongoing advancements in vaccine technologies, such as mRNA vaccines, may accelerate the development and deployment of vaccines against new infectious agents. Rapid vaccine development platforms could potentially shorten the timeline for vaccine availability. Efforts to ensure equitable access to vaccines and medical resources globally may become a focal point. Initiatives to address vaccine distribution disparities and increase vaccine production capacity in developing countries could play a crucial role. Building community resilience and promoting active participation in the pandemic response could be emphasized, and empowering communities with information and resources can contribute to more effective local responses [2,18,36,80].
War and disease have significantly shaped military history, yet they continue to be overlooked in countries such as the United States [88]. The combined impact of war and pandemics could potentially lead to more fatalities than a nuclear war, adding to the already severe consequences of conflict [93]. During the Vietnam War, few realized that the bubonic and pneumonic plagues, including their bubonic-septicemic and septicemic variants, were rampant. In many regions, the ongoing conflict halted not only hostilities but also vital commerce and access to medical services [94]. Throughout the peak years of the Vietnam War from 1964 to 1972, the majority of the world’s plague cases were of the bubonic type (Figure 3).
Figure 3.
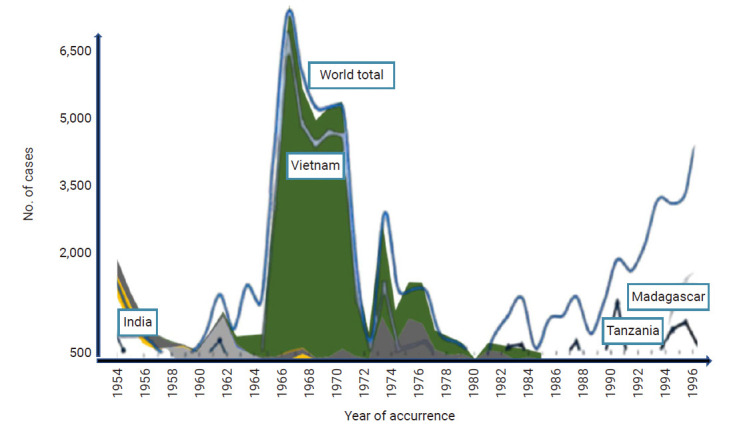
The impact of plague in Vietnam, combined with a chart from the World Health Organization. Reproduced from Plague cases reported in Asia to the World Health Organizations for the period 1954–1986. Other peaks in India, Tanzania, and Madagascar are also visible. Available from: https://timelines.issarice.com/wiki/Timeline_of_plague.
It is important to note that the future of pandemics will be influenced by the collective actions of the global community, scientific advancements, and societal responses to emerging challenges. Preparedness, adaptability, and a commitment to addressing the root causes of infectious diseases are crucial in determining the trajectory of pandemics in the coming years [95–97].
Recommendations
Based on this comprehensive review, we recommend some steps for the future management of pandemics based on different aspects of pandemic preparedness, response, and the role of technology and collaboration in these efforts. Table 6 shows these recommendations as major themes and their associated subcategories.
Table 6.
Recommendations for the management of future pandemics
| Major theme | Category | Subcategory | Measure |
|---|---|---|---|
| A. Interdisciplinary strategies for pandemic preparedness | 1. Strengthening surveillance and early warning systems | Advanced technology | Utilize AI and big data analytics to improve disease detection and prediction. |
| Promote international data sharing and collaboration for robust early warning mechanisms. | |||
| 2. Promoting interdisciplinary collaboration | Collaborative efforts | Encourage collaboration among virologists, public health experts, technologists, economists, and social scientists. | |
| Establish interdisciplinary task forces to oversee pandemic preparedness and response efforts, ensuring a coordinated approach. | |||
| B. Improving global health infrastructure | 1. Equitable access and healthcare logistics | Infrastructure improvements | Improve global health infrastructure, particularly in low- and middle-income countries. |
| Invest in healthcare logistics for efficient distribution of medical supplies and vaccines. | |||
| 2. “One Health” approach | Integrated health strategies | Implement a “One Health” approach that integrates human, animal, and environmental health to address zoonotic spillovers. | |
| C. Rapid vaccine development and distribution | 1. Funding and global agreements | Vaccine development | Fund rapid vaccine development platforms. |
| Create global agreements to ensure fair vaccine distribution, especially to vulnerable populations. | |||
| D. Building community resilience | 1. Education and resources | Local empowerment | Build community resilience through education and resources to empower local responses. |
| Foster global cooperation and governance to streamline international pandemic response efforts. | |||
| E. Technological advancements in pandemic response | 1. Role of AI and big data analytics | Data processing and decision-making | Use AI to analyze vast amounts of data from social media, health records, and environmental sensors to identify early warning signals of potential outbreaks. |
| Utilize big data analytics to predict disease spread and allocate resources by creating predictive models from multiple data sources. | |||
| 2. Improving diagnostic capabilities | AI-driven tools | Deploy machine learning algorithms to analyze medical images and test results with high accuracy, providing faster diagnoses compared to traditional methods. Rapid diagnostic capabilities are crucial for the timely identification of cases to prevent further spread. | |
| 3. Telemedicine and digital health tools | Healthcare delivery | Provide remote consultations through telemedicine platforms, reducing the risk of virus transmission. | |
| Use AI-powered digital contact tracing applications to identify and notify individuals exposed to infectious diseases, enabling timely quarantine and isolation measures. | |||
| F. Ensuring data privacy and security | 1. Protecting health information | Privacy frameworks | Establish robust frameworks to protect sensitive health information and ensure compliance with privacy regulations. |
| Invest in training and resources to integrate AI and big data analytics into existing public health infrastructures, building the necessary technical expertise. |
AI, artificial intelligence.
Conclusion
In the era of globalization, the interconnectedness of our world has yielded significant benefits, including economic growth and enhanced scientific collaboration. However, it has also presented unique challenges, especially in the rapid spread of infectious diseases, as vividly demonstrated by the COVID-19 pandemic. This review has explored the complexities of pandemics beyond their immediate health implications, examining their socioeconomic, environmental, and technological aspects. Our findings highlight the urgent need for robust pandemic preparedness and response mechanisms that go beyond traditional healthcare infrastructure to address broader socioeconomic and environmental vulnerabilities.
Reflecting on the objectives outlined in the introduction, our review addresses a significant gap in the literature by offering a comprehensive analysis of pandemics from multidisciplinary, cross-disciplinary, and transdisciplinary perspectives. The insights gained from this study enhance the growing body of knowledge that is crucial for strengthening global health defenses against pandemics. Importantly, our research emphasizes the importance of interdisciplinary collaboration and cross-sectoral partnerships in developing effective and inclusive strategies for pandemic response. These efforts are essential not only for the immediate management of pandemics but also for advancing the broader goals of sustainable development, which include promoting health equity, resilience, and environmental stewardship.
Our exploration highlights the necessity of an integrated approach to pandemic management, emphasizing effective surveillance, early detection, and coordinated international efforts alongside technological innovations like AI and telemedicine. These technologies enhance monitoring and response capabilities and promote equitable healthcare access, reducing disparities effecting marginalized communities, aligning SDG 3, SDG 11, and SDG 13.
Building on this alignment, our study advocates for a holistic approach, integrating health, environmental sustainability, and social equity to enhancesocietal resilience against future pandemics. Drawing lessons from past pandemics, including COVID-19, we gain valuable insights for improved preparation and response. By fostering collaboration, innovation, and sustainability, we can minimize future pandemics impacts, safeguard global well-being and advance toward a more resilient and equitable world.
HIGHLIGHTS
• Despite the profound historical impacts of pandemics on societies, economies, and public health, new pandemics are met with similar unpreparedness and confusion.
• Exploring the socioeconomic, environmental, and technological dimensions of contemporary pandemics is necessary to understand them comprehensively.
• Cross-disciplinary, transdisciplinary, and multidisciplinary approaches are necessary to integrate various perspectives to strengthen defenses against global health threats.
Footnotes
Ethics Approval
Not applicable.
Conflicts of Interest
The authors have no conflicts of interest to declare.
Funding
None.
Availability of Data
The datasets are not publicly available but are available from the corresponding author upon reasonable request.
Authors’ Contributions
Conceptualization: AKM; Data curation: all authors; Formal analysis: all authors; Investigation: all authors; Methodology: AKM; Project administration: AKM; Resources: all authors; Supervision: FMB, KG; Validation: all authors; Visualization: all authors; Writing–original draft: AKM; Writing–review & editing: all authors. All authors read and approved the final manuscript.
References
- 1.Grennan D. What is a pandemic? JAMA. 2019;321:910. doi: 10.1001/jama.2019.0700. [DOI] [PubMed] [Google Scholar]
- 2.Morens DM, Daszak P, Markel H, et al. Pandemic COVID-19 joins history’s pandemic legion. mBio. 2020;11:e00812–20. doi: 10.1128/mBio.00812-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morens DM, Folkers GK, Fauci AS. What is a pandemic? J Infect Dis. 2009;200:1018–21. doi: 10.1086/644537. [DOI] [PubMed] [Google Scholar]
- 4.Khorram-Manesh A, Goniewicz K, Burkle FM. Unleashing the global potential of public health: a framework for future pandemic response. J Infect Public Health. 2024;17:82–95. doi: 10.1016/j.jiph.2023.10.038. [DOI] [PubMed] [Google Scholar]
- 5.Goniewicz K, Khorram-Manesh A, Burkle FM, et al. The European Union’s post-pandemic strategies for public health, economic recovery, and social resilience. Glob Transit. 2023;5:201–9. [Google Scholar]
- 6.Bavel JJ, Baicker K, Boggio PS, et al. Using social and behavioural science to support COVID-19 pandemic response. Nat Hum Behav. 2020;4:460–71. doi: 10.1038/s41562-020-0884-z. [DOI] [PubMed] [Google Scholar]
- 7.Checa-Ros A, Munoz-Hoyos A, Molina-Carballo A, et al. Analysis of different melatonin secretion patterns in children with sleep disorders: melatonin secretion patterns in children. J Child Neurol. 2017;32:1000–8. doi: 10.1177/0883073817726680. [DOI] [PubMed] [Google Scholar]
- 8.Choudhry AA, Shahzeen F, Choudhry SA, et al. Impact of COVID-19 infection on quality of sleep. Cureus. 2021;13:e18182. doi: 10.7759/cureus.18182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Molina-Carballo A, Palacios-Lopez R, Jerez-Calero A, et al. Protective effect of melatonin administration against SARS-CoV-2 infection: a systematic review. Curr Issues Mol Biol. 2021;44:31–45. doi: 10.3390/cimb44010003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Briggs A. In: Healthcare access: new threats, new approaches. Emel Önal A, editor. IntechOpen; 2023. Climate change, conflict, and contagion: emerging threats to global public health; pp. 21–52. [Google Scholar]
- 11.Khorram-Manesh A. Global transition, global risks, and the UN’s sustainable development goals: a call for peace, justice, and political stability. Glob Transit. 2023;5:90–7. [Google Scholar]
- 12.AlKnawy B, Kozlakidis Z, Tarkoma S, et al. Digital public health leadership in the global fight for health security. BMJ Glob Health. 2023;8:e011454. doi: 10.1136/bmjgh-2022-011454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhu B, Nosaka N, Kanamaru S, et al. Rapid and sensitive SARS-CoV-2 detection using a homogeneous fluorescent immunosensor Quenchbody with crowding agents. Analyst. 2022;147:4971–9. doi: 10.1039/d2an01051h. [DOI] [PubMed] [Google Scholar]
- 14.Kumar A, Gupta PK, Srivastava A. A review of modern technologies for tackling COVID-19 pandemic. Diabetes Metab Syndr. 2020;14:569–73. doi: 10.1016/j.dsx.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anton P, Munoz A, Mana A, et al. Security-enhanced ambient assisted living supporting school activities during hospitalisation. J Ambient Intell Human Comput. 2012;3:177–92. [Google Scholar]
- 16.Smith MJ, Ahmad A, Arawi T, et al. Top five ethical lessons of COVID-19 that the world must learn. Wellcome Open Res. 2021;6:17. doi: 10.12688/wellcomeopenres.16568.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yeoh K, Wu Y, Chakraborty S, et al. Global health system resilience during encounters with stressors: lessons learnt from cancer services during the COVID-19 pandemic. Clin Oncol (R Coll Radiol) 2023;35:e289–300. doi: 10.1016/j.clon.2023.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jowell A, Barry M. COVID-19: a matter of planetary, not only national health. Am J Trop Med Hyg. 2020;103:31–2. doi: 10.4269/ajtmh.20-0419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Madhav N, Oppenheim B, Gallivan M, et al. In: Disease control priorities: improving health and reducing poverty. 3rd ed. Jamison DT, Gelband H, Horton S, et al., editors. The International Bank for Reconstruction and Development/The World Bank; 2017. Pandemics: risks, impacts, and mitigation; pp. e11–13. [PubMed] [Google Scholar]
- 20.Nunes MC, Thommes E, Frohlich H, et al. Redefining pandemic preparedness: multidisciplinary insights from the CERP modelling workshop in infectious diseases, workshop report. Infect Dis Model. 2024;9:501–18. doi: 10.1016/j.idm.2024.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sukhera J. Narrative reviews in medical education: key steps for researchers. J Grad Med Educ. 2022;14:418–9. doi: 10.4300/JGME-D-22-00481.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.George T. Scribbr; 2024. What is action research?: definition and examples [Internet] [cited 2024 Jun 5]. Available from: https://www.scribbr.com/methodology/action-research/ [Google Scholar]
- 23.Stemler S. An overview of content analysis. Pract Asses Res Eval. 2000;7:17. [Google Scholar]
- 24.Daszak P. Anatomy of a pandemic. Lancet. 2012;380:1883–4. doi: 10.1016/S0140-6736(12)61887-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fears JR. The plague under Marcus Aurelius and the decline and fall of the Roman Empire. Infect Dis Clin North Am. 2004;18:65–77. doi: 10.1016/S0891-5520(03)00089-8. [DOI] [PubMed] [Google Scholar]
- 26.Barbieri R, Signoli M, Cheve D, et al. Yersinia pestis: the natural history of plague. Clin Microbiol Rev. 2020;34:e00044–19. doi: 10.1128/CMR.00044-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Glatter KA, Finkelman P. History of the plague: an ancient pandemic for the age of COVID-19. Am J Med. 2021;134:176–81. doi: 10.1016/j.amjmed.2020.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Evans RJ. Epidemics and revolutions: cholera in nineteenth-century Europe. Past Present. 1988;120:123–46. doi: 10.1093/past/120.1.123. [DOI] [PubMed] [Google Scholar]
- 29.Tomes N. “Destroyer and teacher”: managing the masses during the 1918-1919 influenza pandemic. Public Health Rep. 2010;125(Suppl 3):48–62. doi: 10.1177/00333549101250S308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Honigsbaum M. Revisiting the 1957 and 1968 influenza pandemics. Lancet. 2020;395:1824–6. doi: 10.1016/S0140-6736(20)31201-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bekker LG, Beyrer C, Mgodi N, et al. HIV infection. Nat Rev Dis Primers. 2023;9:42. doi: 10.1038/s41572-023-00452-3. [DOI] [PubMed] [Google Scholar]
- 32.Girard MP, Tam JS, Assossou OM, et al. The 2009 A (H1N1) influenza virus pandemic: a review. Vaccine. 2010;28:4895–902. doi: 10.1016/j.vaccine.2010.05.031. [DOI] [PubMed] [Google Scholar]
- 33.Msemburi W, Karlinsky A, Knutson V, et al. The WHO estimates of excess mortality associated with the COVID-19 pandemic. Nature. 2023;613:130–7. doi: 10.1038/s41586-022-05522-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mayer JD, Schintler LA, Bledsoe S. Culture, freedom, and the spread of COVID‐19: do some societies and political systems have national anti‐bodies? World Med Health Policy. 2020;12:498–511. [Google Scholar]
- 35.Sandmann FG, Davies NG, Vassall A, et al. The potential health and economic value of SARS-CoV-2 vaccination alongside physical distancing in the UK: a transmission model-based future scenario analysis and economic evaluation. Lancet Infect Dis. 2021;21:962–74. doi: 10.1016/S1473-3099(21)00079-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Coccia M. Sources, diffusion and prediction in COVID-19 pandemic: lessons learned to face next health emergency. AIMS Public Health. 2023;10:145–68. doi: 10.3934/publichealth.2023012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yousif MG, Hashim K, Rawaf S. Post COVID-19 effect on medical staff and doctors’ productivity analysed by machine learning. Baghdad Sci J. 2023;20(4 (SI)):1507. [Google Scholar]
- 38.Doleman G, De Leo A, Bloxsome D. The impact of pandemics on healthcare providers' workloads: a scoping review. J Adv Nurs. 2023;79:4434–54. doi: 10.1111/jan.15690. [DOI] [PubMed] [Google Scholar]
- 39.Schepers M, Schmidtmann I, Zahn D, et al. Medical appointments and provision of medical care during the COVID-19 pandemic in Mainz, Germany. PLoS One. 2023;18:e0280292. doi: 10.1371/journal.pone.0280292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Romiti GF, Bencivenga L, Villani R, et al. The impact of COVID-19 pandemic on well-being of Italian physicians: a report from the Italian Society of Internal Medicine (SIMI) national survey. Intern Emerg Med. 2023;18:53–65. doi: 10.1007/s11739-022-03108-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ferrara F, Zovi A, Masi M, et al. Long COVID could become a widespread post-pandemic disease?: a debate on the organs most affected. Naunyn Schmiedebergs Arch Pharmacol. 2023;396:1583–9. doi: 10.1007/s00210-023-02417-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Saxon L, Fazio TN, Gumm K, et al. Quality of care was not compromised during the COVID-19 pandemic at a level 1 trauma centre. ANZ J Surg. 2022;92:172–9. doi: 10.1111/ans.17154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Phattharapornjaroen P, Carlstrom E, Sivarak O, et al. Community-based response to the COVID-19 pandemic: case study of a home isolation centre using flexible surge capacity. Public Health. 2022;211:29–36. doi: 10.1016/j.puhe.2022.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Khorram-Manesh A. Flexible surge capacity: public health, public education, and disaster management. Health Promot Perspect. 2020;10:175–9. doi: 10.34172/hpp.2020.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Willey JM, Olvet DM, Bird JB, et al. Pandemics past and present: a guided inquiry approach. J Med Educ Curric Dev. 2020;7:2382120520976957. doi: 10.1177/2382120520976957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Althwanay A, Ahsan F, Oliveri F, et al. Medical education, pre- and post-pandemic era: a review article. Cureus. 2020;12:e10775. doi: 10.7759/cureus.10775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sultan MA, Carlstrom E, Sorensen JL, et al. Incorporating simulation exercises using collaborative tools into disaster and emergency medicine curriculum: a pilot survey among Saudi Arabian professionals. J Contin Crisis Manag. 2023;31:905–12. [Google Scholar]
- 48.Khorram-Manesh A, Dulebenets MA, Goniewicz K. Implementing public health strategies: the need for educational initiatives: a systematic review. Int J Environ Res Public Health. 2021;18:5888. doi: 10.3390/ijerph18115888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Talic S, Shah S, Wild H, et al. Effectiveness of public health measures in reducing the incidence of COVID-19, SARS-CoV-2 transmission, and COVID-19 mortality: systematic review and meta-analysis. BMJ. 2021;375:e068302. doi: 10.1136/bmj-2021-068302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hu CY, Tang YW, Su QM, et al. Public health measures during the COVID-19 pandemic reduce the spread of other respiratory infectious diseases. Front Public Health. 2021;9:771638. doi: 10.3389/fpubh.2021.771638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.World Health Organization (WHO) (CH) United Nations Children's Fund (UNICEF) . WHO; 2020. Water, sanitation, hygiene and waste management for COVID-19: technical brief, 3 March 2020 [Internet] [cited 2024 Jun 5]. Available from: https://iris.who.int/handle/10665/331305. [Google Scholar]
- 52.Igarashi A, Nakano Y, Yoneyama-Hirozane M. Public preferences and willingness to accept a hypothetical vaccine to prevent a pandemic in Japan: a conjoint analysis. Expert Rev Vaccines. 2022;21:241–8. doi: 10.1080/14760584.2022.2016402. [DOI] [PubMed] [Google Scholar]
- 53.Ligo VA, Chang CM, Yi H. Contested solidarity and vulnerability in social media-based public responses to COVID-19 policies of mobility restrictions in Singapore: a qualitative analysis of temporal evolution. BMC Public Health. 2021;21:2232. doi: 10.1186/s12889-021-12316-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lee M, You M. Avoidance of healthcare utilization in South Korea during the coronavirus disease 2019 (COVID-19) pandemic. Int J Environ Res Public Health. 2021;18:4363. doi: 10.3390/ijerph18084363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dai J, Lyu F, Yu L, et al. Temporal and emotional variations in people’s perceptions of mass epidemic infectious disease after the COVID-19 pandemic using influenza A as an example: topic modeling and sentiment analysis based on Weibo data. J Med Internet Res. 2023;25:e49300. doi: 10.2196/49300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Van Scoy LJ, Miller EL, Snyder B, et al. Knowledge, perceptions, and preferred information sources related to COVID-19 among central Pennsylvania adults early in the pandemic: a mixed methods cross-sectional survey. Ann Fam Med. 2021;19:293–301. doi: 10.1370/afm.2674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Khorram-Manesh A, Carlstrom E, Hertelendy AJ, et al. Does the prosperity of a country play a role in COVID-19 outcomes? Disaster Med Public Health Prep. 2022;16:177–86. doi: 10.1017/dmp.2020.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Antras P, Redding SJ, Rossi-Hansberg E. Globalization and pandemics. Am Econ Rev. 2023;113:939–81. [Google Scholar]
- 59.Bilinski A, Thompson K, Emanuel E. COVID-19 and excess all-cause mortality in the US and 20 comparison countries, June 2021-March 2022. JAMA. 2023;329:92–4. doi: 10.1001/jama.2022.21795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Worldometer (CH) Worldometer; 2024. COVID-19 coronavirus pandemic [Internet] [cited 2024 Jun 5]. Available from: https://www.worldometers.info/coronavirus/ [Google Scholar]
- 61.Ministry of Health (NZ) Ministry of Health; 2024. COVID-19 (novel coronavirus) [Internet] [cited 2024 Jun 5]. Available from: https://www.health.govt.nz/our-work/diseases-and-conditions/covid-19-novel-coronavirus. [Google Scholar]
- 62.Taiwan Centers for Disease Control (TW) Taiwan Centers for Disease Control; 2024. Coronavirus disease 2019 (COVID-19) [Internet] [cited 2024 Jun 5]. Available from: https://www.cdc.gov.tw/en/Disease/SubIndex/ [Google Scholar]
- 63.Australian Government, Department of Health and Aged Care (AU) Australian Government, Department of Health and Aged Care; 2023. Coronavirus (COVID-19) pandemic: find information about the 2019 to 2023 COVID-19 pandemic [Internet] [cited 2024 Jun 5]. Available from: https://www.health.gov.au/health-alerts/covid-19. [Google Scholar]
- 64.World Health Organization (WHO) (CH) WHO; 2021. COVID-19 in Viet Nam [Internet] [cited 2024 Jun 5]. Available from: https://www.who.int/vietnam/emergencies/covid-19-in-vietnam. [Google Scholar]
- 65.Lim S, Sohn M. How to cope with emerging viral diseases: lessons from South Korea’s strategy for COVID-19, and collateral damage to cardiometabolic health. Lancet Reg Health West Pac. 2023;30:100581. doi: 10.1016/j.lanwpc.2022.100581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Papadimos TJ, Soghoian SE, Nanayakkara P, et al. COVID-19 blind spots: a consensus statement on the importance of competent political leadership and the need for public health cognizance. J Glob Infect Dis. 2020;12:167–90. doi: 10.4103/jgid.jgid_397_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hall PA, Sheeran P, Fong GT, et al. Biobehavioral aspects of the COVID-19 pandemic: a review. Psychosom Med. 2021;83:309–21. doi: 10.1097/PSY.0000000000000932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ohmagari N. Social implications of a change in the legal classification of COVID-19: the need for pandemic prevention, preparedness, and healthcare system strengthening. Glob Health Med. 2023;5:75–7. doi: 10.35772/ghm.2023.01018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Haberer JE, van der Straten A, Safren SA, et al. Individual health behaviours to combat the COVID-19 pandemic: lessons from HIV socio-behavioural science. J Int AIDS Soc. 2021;24:e25771. doi: 10.1002/jia2.25771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.World Health Organization (WHO) (CH) WHO; 2024. WHO COVID-19 dashboard [Internet] [cited 2024 Jun 5]. Available from: https://data.who.int/dashboards/covid19/cases?n=c. [Google Scholar]
- 71.Baker MG, Durrheim D, Hsu LY, et al. COVID-19 and other pandemics require a coherent response strategy. Lancet. 2023;401:265–6. doi: 10.1016/S0140-6736(22)02489-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Whitty CJ, Smith G, McBride M, et al. Restoring and extending secondary prevention. BMJ. 2023;380:201. doi: 10.1136/bmj.p201. [DOI] [PubMed] [Google Scholar]
- 73.Lefrancois T, Malvy D, Atlani-Duault L, et al. After 2 years of the COVID-19 pandemic, translating One Health into action is urgent. Lancet. 2023;401:789–94. doi: 10.1016/S0140-6736(22)01840-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Global Burden of Disease 2021 Health Financing Collaborator Network Global investments in pandemic preparedness and COVID-19: development assistance and domestic spending on health between 1990 and 2026. Lancet Glob Health. 2023;11:e385–413. doi: 10.1016/S2214-109X(23)00007-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Roelen K, Ackley C, Boyce P, et al. COVID-19 in LMICs: the need to place stigma front and centre to its response. Eur J Dev Res. 2020;32:1592–612. doi: 10.1057/s41287-020-00316-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bennett B, Carney T. Law, ethics and pandemic preparedness: the importance of cross-jurisdictional and cross-cultural perspectives. Aust N Z J Public Health. 2010;34:106–12. doi: 10.1111/j.1753-6405.2010.00492.x. [DOI] [PubMed] [Google Scholar]
- 77.Johnson SB, Lucivero F, Zimmermann BM, et al. Ethical reasoning during a pandemic: results of a five country European study. AJOB Empir Bioeth. 2022;13:67–78. doi: 10.1080/23294515.2022.2040645. [DOI] [PubMed] [Google Scholar]
- 78.Sanchez-Bautista C, Reyes Gomez L, Mojica Gomez LC, et al. Teaching experiences in contexts of conflict and cultural diversity during the COVID-19 pandemic: the case of a public school in Bogota. Educ Confl Rev. 2023;4:73–80. [Google Scholar]
- 79.Goniewicz K, Burkle FM, Hall TF, et al. Global public health leadership: the vital element in managing global health crises. J Glob Health. 2022;12:03003. doi: 10.7189/jogh.12.03003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Donelle L, Comer L, Hiebert B, et al. Use of digital technologies for public health surveillance during the COVID-19 pandemic: a scoping review. Digit Health. 2023;9:20552076231173220. doi: 10.1177/20552076231173220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Leslie D. Tackling COVID-19 through responsible AI innovation: five steps in the right direction. Harvard Data Sci Rev. 2020;10:1–73. [Google Scholar]
- 82.MacIntyre CR, Chen X, Kunasekaran M, et al. Artificial intelligence in public health: the potential of epidemic early warning systems. J Int Med Res. 2023;51:3000605231159335. doi: 10.1177/03000605231159335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kumar A, Mani V, Jain V, et al. Managing healthcare supply chain through artificial intelligence (AI): a study of critical success factors. Comput Ind Eng. 2023;175:108815. doi: 10.1016/j.cie.2022.108815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Burkle FM, Bradt DA, Ryan BJ. Global public health database support to population-based management of pandemics and global public health crises, part I: the concept. Prehosp Disaster Med. 2021;36:95–104. doi: 10.1017/S1049023X20001351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Barouki R, Kogevinas M, Audouze K, et al. The COVID-19 pandemic and global environmental change: emerging research needs. Environ Int. 2021;146:106272. doi: 10.1016/j.envint.2020.106272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kinsella CM, Santos PD, Postigo-Hidalgo I, et al. Preparedness needs research: how fundamental science and international collaboration accelerated the response to COVID-19. PLoS Pathog. 2020;16:e1008902. doi: 10.1371/journal.ppat.1008902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Spirtas M, Webber S. Rand; 2022. The future and past of war and disease [Internet] [cited 2024 Jun 5]. Available from: https://www.rand.org/pubs/commentary/2022/01/the-future-and-past-of-war-and-disease.html. [Google Scholar]
- 88.Hatamlah H, Allan M, Abu-AlSondos I, et al. The role of artificial intelligence in supply chain analytics during the pandemic. Uncertain Supply Chain Manag. 2023;11:1175–86. [Google Scholar]
- 89.El-Haddadeh R, Fadlalla A, Hindi NM. Is there a place for responsible artificial intelligence in pandemics?: a tale of two countries. Inform Sys Front. 2023;25:2221–37. doi: 10.1007/s10796-021-10140-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Mehraeen E, SeyedAlinaghi S, Heydari M, et al. Telemedicine technologies and applications in the era of COVID-19 pandemic: a systematic review. Health Informatics J. 2023;29:14604582231167431. doi: 10.1177/14604582231167431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Johinke R, Cummings R, Di Lauro F. Reclaiming the technology of higher education for teaching digital writing in a post: pandemic world. J Uni Teach Learn Pract. 2023;20:1. [Google Scholar]
- 92.Hirsch A. Northern Illinois University, Center for Innovative Teaching and Learning; 2020. Transdisciplinary and interdisciplinary approaches [Internet] [cited 2024 Jun 5]. Available from: https://citl.news.niu.edu/2020/11/17/transdisciplinary-interdisciplinary/ [Google Scholar]
- 93.Carta MG, Orru G, Barberini L. War and pandemic: a negative synergism could amplify the catastrophe. J Public Health Res. 2022;11:3016. doi: 10.4081/jphr.2022.3016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Burkle FM. Plague as seen in South Vietnamese children: a chronicle of observations and treatment under adverse conditions. Clin Pediatr (Phila) 1973;12:291–8. doi: 10.1177/000992287301200512. [DOI] [PubMed] [Google Scholar]
- 95.Patterson GE, McIntyre KM, Clough HE, et al. Societal impacts of pandemics: comparing COVID-19 with history to focus our response. Front Public Health. 2021;9:630449. doi: 10.3389/fpubh.2021.630449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Alami H, Lehoux P, Fleet R, et al. How can health systems better prepare for the next pandemic?: lessons learned from the management of COVID-19 in Quebec (Canada) Front Public Health. 2021;9:671833. doi: 10.3389/fpubh.2021.671833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Destoumieux-Garzon D, Matthies-Wiesler F, Bierne N, et al. Getting out of crises: environmental, social-ecological and evolutionary research is needed to avoid future risks of pandemics. Environ Int. 2022;158:106915. doi: 10.1016/j.envint.2021.106915. [DOI] [PMC free article] [PubMed] [Google Scholar]