Abstract
Objective
Many unscheduled return visits to the emergency department (ED) stem from insufficient access to outpatient follow‐up. We piloted an emergency medicine‐staffed, on‐demand, virtual after care clinic (VACC) as an alternative for discharged ED patients.
Methods
Prospective cohort study of discharged ED patients who scheduled VACC appointments within 72 hours of index ED visit. We performed descriptive analyses and compared risks of ED return at 72 hours and 30 days between patients who did/did not attend their appointment.
Results
From March to December 2022, 309 patients scheduled VACC appointments and 210 (68%) attended them. Patients who scheduled appointments were young (median 37 years), non‐Hispanic white (80%), females (75%) with a primary care physicians (PCP) (90%), and commercial insurance (72%). Most VACC visits reinforced ED testing and/or treatment (64%) or adjusted medications (26%). VACC attendees were less likely to return to the ED within 72 h (3.3% vs. 13.1%; risk difference 9.3% [95% confidence interval, CI 2.7%‒19.8%]) and 30 days (16.2% vs. 30.3%; risk difference 14.1% [95% CI 3.8%‒24.4%]) compared to those who scheduled but did not attend a VACC appointment. VACC attendance was associated with lower odds of 72‐h (adjusted odds ratio [aOR] 0.0; 95% CI 0.0‒0.4) and 30‐day (aOR 0.4; 95% CI 0.2‒0.7) return ED visits.
Conclusions
In this pilot study, younger, white, female, commercially insured patients with a PCP preferentially scheduled VACC appointments. Among patients who scheduled VACC appointments, those who attended their appointments were less likely to return to the ED within 72 hours and 30 days than those who did not.
Keywords: aftercare, emergency service, return visits, telehealth, telemedicine
1. INTRODUCTION
1.1. Background
More than one quarter of patients who are discharged from the emergency department (ED) return to the ED within the following month. 1 , 2 Often referred to as “bounce‐back” ED visits, over half of these unscheduled returns occur within 48 hours of discharge. 3 The underlying causes for return ED visits appear to be heterogeneous. 4 , 5 The occurrence of an early return ED visit, especially those requiring hospitalization, 6 raises reasonable questions about diagnostic, treatment, or communication failures during the index ED encounter, 4 , 7 , 8 , 9 prompting some to suggest return visit rates as a metric for quality ED care. 4 , 5 , 10 , 11 However, many factors outside of ED clinician purview influence patient decisions to return to the ED. Progression or recurrence of disease 12 , 13 may appropriately lead a patient to return to the ED, which often constitutes compliance with ED discharge instructions. Qualitative analyses also suggest that many return ED visits are motivated by unaddressed patient concerns over persistent symptoms and lack of timely access to outpatient follow‐up. 7 , 8 , 9 , 14
1.2. Importance
Irrespective of the root causes of ED return visits, they constitute potentially inefficient uses of scarce healthcare resources. EDs are already overburdened with patients 15 and the ED is well‐recognized as a comparatively expensive location to deliver non‐emergency healthcare. 16 In order to support patients with ongoing concerns following ED discharge when outpatient follow‐up could not be rapidly obtained, we piloted an emergency medicine clinician‐operated, on‐demand, virtual after care clinic (VACC) service. VACC visits offered an opportunity for urgent follow‐up to address ongoing patient concerns and optimize treatment, with an underlying goal of preventing avoidable return ED visits.
1.3. Goals of this investigation
This pilot analysis had two primary aims: (1) characterize individuals who scheduled and attended VACC appointments, and (2) estimate the association between VACC attendance and return ED visits among those who scheduled appointments.
2. METHODS
2.1. Study design and setting
This is a prospective, observational cohort study of patients who scheduled a VACC appointment after discharge from any of 10 (three urban/suburban and seven rural) EDs in a single health system with a total annual ED volume approaching 400,000 patients. The study cohort consisted of consecutive adult patients who scheduled a VACC appointment for any reason during its pilot phase (between March 1 and December 31, 2022). For patients with more than one VACC visit, only the first was included in the analytic cohort. A quality improvement log tracked all patients who scheduled appointments and captured basic information about VACC visits. The Corewell Health IRB approved this study as secondary analysis of a quality improvement project with waiver of informed consent.
The Bottom Line
This pilot study evaluated the use and impact of an emergency medicine clinician‐run virtual after care clinic (VACC) for patients discharged from the emergency department (ED). We found that the clinic was used primarily by younger, white, female, commercially insured patients from urban EDs who already had a primary care physician. The main service provided during VACC appointments was reinforcement of the existing discharge plan. Patients who attended their VACC appointment were less likely to return to the ED within 30 days compared to those who scheduled but did not attend their appointment.
2.2. Virtual after care clinic
We developed the VACC to support ED patients following discharge and prevent unnecessary return ED visits. All adult patients discharged from participating EDs received standardized written information about VACC in their printed discharge instructions. Although there was no specific recruitment strategy, ED clinicians at all sites were aware of the VACC as an option for patients who required close follow‐up. Discharge instructions emphasized preferential follow‐up with a patient's own primary care clinicians (PCC), but also offered VACC contact information as an alternative if patients sought follow‐up more urgently than was available through their PCP. The electronic health record (Epic) online patient portal allowed patients to self‐schedule 15‐min appointments from four to eight daily available slots between 08:00 and 21:00 on weekdays during the first 72 h following ED discharge. Experienced emergency medicine clinicians (MD, DO, PA‐C, or NP) conducted VACC appointments using the Epic video conferencing platform and documented encounters in the patient's medical record as a telehealth visit.
2.3. Measurements and outcomes
We performed a descriptive analysis of the demographics, health insurance status, PCP assignment, and ED visit characteristics (location, chief complaint, triage acuity, and diagnostic impression at discharge) of patients who made VACC appointments and compared them to other contemporaneous discharged adult ED patients. We also compared individuals who kept VACC appointments to those who scheduled appointments but did not attend. Quality improvement nurses classified the primary service delivered as reinforcement of ED testing/treatment, adjustment to medication(s), referral to a specialist, ordering additional diagnostic testing, or “other” after reviewing the VACC clinician note. Manual review of the electronic medical records also identified return ED visits for all patients who scheduled an appointment. A regional electronic health information exchange afforded access to records for ED visits and hospitalizations at all three regional health systems. The primary outcome was any return ED visit within 72 h of the index ED visit. Secondary outcomes included return ED visits within 30 days of the index visit, as well as hospitalization at any point within 72 h and 30 days.
2.4. Statistical analysis
Using Stata (StataCorp), we performed a descriptive analysis of subjects who scheduled VACC appointments. We used chi square tests to compare clinical features between subjects who scheduled VACC appointments and all other adult ED discharges, as well as between those who did and did not attend VACC appointments. Multiple variable logistic regression estimated the association between VACC attendance (vs non‐attendance) and outcomes, adjusting for available clinically relevant covariates (age, sex, race, insurance type, rural [vs urban] ED, weekend [vs. weekday] ED visit, substantial ED utilization [greater than six ED visits in the prior 12 months], and triage acuity level). Finally, post hoc exploratory analysis quantified the risk of return ED visit by VACC attendance and index chief complaint as categorized by the primary relevant organ system.
3. RESULTS
3.1. Characteristics of study subjects
Over a 9‐month period between March and December 2022, there were 181,654 adult ED patients discharged from the 10 included EDs. Of these, 309 (0.2%) scheduled a VACC appointment and 210/309 (68.0%) attended their appointment (Figure 1), filling 22% of available VACC appointment slots. Table 1 shows overall subject characteristics. Compared to all adult ED discharges, the VACC appointment cohort was more likely to be young, female, commercially insured, and evaluated on a weekend in an urban ED. Nearly, all patients who scheduled a VACC appointment had a PCP. Patients who attended their VACC appointment had similar characteristics to those who did not attend. During appointments, clinicians most frequently reinforced the ED plan (64%) or adjusted medications (26%). Additional actions included ordering further testing or specialty referral (6%) and providing a work note (3%). Two patients were referred to the ED by the VACC clinician for further testing and/or treatment.
FIGURE 1.
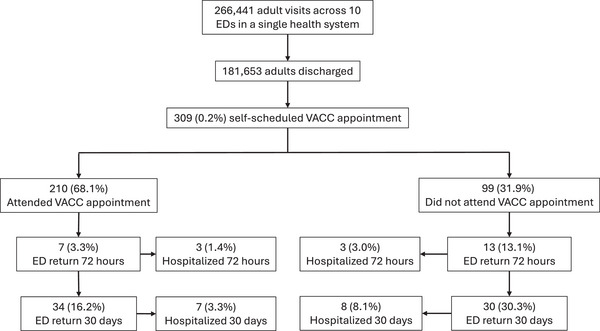
Study cohort and primary outcomes. ED, emergency department; VACC, virtual after care clinic.
TABLE 1.
Characteristics of emergency department (ED) discharges and patients who scheduled and attended a virtual after care clinic (VACC) appointment.
| Adult ED discharges without VACC appointment, N = 181,345 (%) | Adult ED discharges with a VACC appointment, N = 309 (%) | p‐value | Attended VACC, n = 210 (%) | Did not attend VACC, n = 99 (%) | p‐value | |
|---|---|---|---|---|---|---|
| Age category (years) | <0.001 | 0.630 | ||||
| 18‒29 | 45,439 (25.1) | 85 (27.5) | 59 (28.1) | 26 (26.3) | ||
| 30‒39 | 33,656 (18.6) | 89 (28.8) | 60 (28.6) | 29 (29.3) | ||
| 40‒49 | 25,793 (14.2) | 51 (16.5) | 35 (16.7) | 16 (16.2) | ||
| 50‒64 | 36,296 (20.0) | 60 (19.4) | 43 (20.5) | 17 (17.2) | ||
| 65 or greater | 40,161 (22.2) | 24 (7.8) | 13 (6.2) | 11 (11.1) | ||
| Female | 104,772 (57.8) | 233 (75.4) | <0.001 | 158 (75.2) | 75 (75.8) | 0.921 |
| Insurance | <0.001 | 0.365 | ||||
| Public | 95,065 (52.4) | 80 (25.8) | 50 (23.8) | 30 (30.3) | ||
| Commercial | 65,459 (36.1) | 222 (71.8) | 156 (74.3) | 66 (66.7) | ||
| None | 20,821 (11.5) | 7 (2.3) | 4 (1.9) | 3 (3) | ||
| Rural (vs. suburban or urban) | 80,571 (44.4) | 99 (32.0) | <0.001 | 70 (33.3) | 29 (29.3) | 0.478 |
| Weekend ED visit | 48,384 (26.6) | 101 (32.7) | 0.017 | 71 (33.8) | 30 (30.3) | 0.540 |
| Low triage acuity (level 4‒5) | 47,558 (26.2) | 63 (20.4) | 0.028 | 43 (20.5) | 20 (20.2) | 0.955 |
| Race/ethnicity | Not available | 0.384 | ||||
| Non‐Hispanic White | 248 (80.3) | 170 (80.9) | 78 (78.8) | |||
| Non‐Hispanic Black | 25 (8.1) | 14 (6.7) | 11 (11.1) | |||
| Hispanic | 23 (7.4) | 18 (8.6) | 5 (5.1) | |||
| Other/missing | 13 (4.2) | 8 (3.8) | 5 (5.1) | |||
| PCP | Not available | 278 (90.0) | 188 (89.5) | 90 (90.9) | 0.705 |
Abbreviation: PCP, primary care physician.
3.2. Main results
Return visits are summarized in Table 2. Overall return visit rates for those who scheduled VACC appointments were similar among those who scheduled appointments with the VACC clinic returned to the ED and were hospitalized at similar rates to the overall ED population. Patients who attended their VACC appointment were less likely to return to the ED within 72 hours (3.3 vs. 13.1%; risk difference 9.8% [95% confidence interval, CI 2.7%‒19.8%]) and 30 days (16.2% vs. 30.3%; risk difference 14.1% [95% CI 3.8%‒24.4%]) compared to those who did not attend. Return visits with hospitalization were also modestly lower for VACC attendees than non‐attendees at 72 hours (risk difference 1.6% [95% CI −2.1% to 5.3%]) and at 30 days (5.8% [95% CI −1.1% to 10.7%]); however, neither difference reached statistical significance. Of the 13 return ED visits within 72 hours of discharge among VACC non‐attenders, six (46%) occurred during or before their VACC appointment time. Of the 20 return visits in the VACC cohort that occurred within 72 hours, 14 (70%) were to the same hospital and six (29%) sought care elsewhere.
TABLE 2.
Comparison of return emergency department (ED) visits and hospitalizations among full ED population, patients who attended a virtual after care clinic (VACC) appointment, and those who scheduled but did not attend.
| Outcome | Adult ED discharges without VACC appointment, n = 181,345 (%) | Adult ED discharges with a VACC appointment, n = 309 (%) | p‐value | Attended VACC, n = 211 (%) | Did not attend VACC, n = 99 (%) |
Difference in proportions (95% confidence interval) |
|---|---|---|---|---|---|---|
| Return to ED within 72 h | 11,543 (6.4%) | 20 (6.5) | 0.939 | 7 (3.3) | 13 (13.1) | 9.8% (2.7%‒19.8%) |
| Return to ED within 30 days | 36,868 (20.3) | 64 (20.7) | 0.868 | 34 (16.2) | 30 (30.3) | 14.1% (3.8%‒24.4%) |
| Admission within 72 h | 2783 (1.5) | 6 (1.9) | 0.561 | 3 (1.4) | 3 (3.0) | 1.6% (−2.1% to 5.3%) |
| Admission within 30 days | 9680 (5.3) | 15 (4.9) | 0.705 | 7 (3.3) | 8 (8.1) | 4.7% (−1.1% to 10.6%) |
Table 3 shows results of the multiple variable regression modeling. Adjusting for age, sex, race, insurance type, rural ED (vs. urban/suburban), weekend ED visit (vs. weekday), and burden of prior ED use, attendance at the VACC appointment was associated with lower odds of return ED visit at both 72 h (odds ratio [OR] 0.1; 95% CI 0.0‒0.4) and 30 days (OR 0.4; 95% CI 0.2‒0.7). Point estimates suggest that VACC attendance might also influence the odds of hospitalization at 72 h (OR 0.5; 95% CI 0.1‒2.8) and 30 days (OR 0.4; 95% CI 0.1‒1.2); however, these results did not reach statistical significance.
TABLE 3.
Output from multivariable regression models of return emergency department (ED) visits among 309 scheduled appointments at the virtual after care clinic (VACC).
| Outcome | Unadjusted OR (95% CI) given VACC attendance | p‐value |
Adjusted a OR (95% CI) given VACC attendance |
p‐value |
|---|---|---|---|---|
| Return to ED within 72 h | 0.2 (0.1‒0.6) | 0.002 | 0.1 (0.0‒0.4) | 0.001 |
| Return to ED within 30 days | 0.4 (0.3‒0.8) | 0.005 | 0.4 (0.2‒0.7) | 0.003 |
| Admission within 72 h | 0.5 (0.1‒2.3) | 0.352 | 0.5 (0.1‒2.8) | 0.366 |
| Admission within 30 days | 0.4 (0.1‒1.1) | 0.079 | 0.4 (0.1‒1.2) | 0.099 |
Note: ORs represent the relative odds of a patient returning to the ED among those who scheduled and attended versus those who scheduled but did not attend a VACC appointment.
Abbreviations: CI, confidence interval; OR, odds ratio.
Adjusted for age, sex, race, insurance type, rural ED (vs. urban), weekend ED visit (vs. weekday), prior ED use (>6 visits during prior 12 months vs. less), and triage acuity.
Table 4 shows the distribution of index ED visit chief complaints organized by organ system for patients who scheduled VACC appointments, along with VACC attendance and return ED visits. Gastrointestinal complaints (ie, vomiting, diarrhea, or abdominal pain), musculoskeletal complaints (ie, fracture, back pain), and cardiovascular complaints (ie, chest pain, palpitations, near syncope) were the three most common concerns. Post hoc exploratory comparison of ED return by organ system suggests that cardiovascular and neurologic chief complaints may be especially influenced by attending the VACC appointment.
TABLE 4.
Virtual after care clinic (VACC) clinic scheduling, attendance, and return emergency department (ED) visits within 72 h by organ system of complaint/diagnosis.
| System | Count | Show (%) | Return overall (%) | ED return if show (%) | ED return if no show (%) |
|---|---|---|---|---|---|
| GI | 45 | 31 (68.9) | 3 (6.7) | 1 (3.2) | 2 (14.3) |
| Musculoskeletal | 44 | 28 (63.6) | 1 (2.3) | 0 (0) | 1 (6.3) |
| CV | 41 | 29 (70.7) | 3 (7.3) | 0 (0) | 3 (25) |
| Pulmonary | 30 | 22 (73.3) | 3 (10) | 2 (9.1) | 1 (12.5) |
| Systemic | 27 | 15 (55.6) | 0 (0) | 0 (0) | 0 (0) |
| Neuro | 26 | 17 (65.4) | 2 (7.7) | 0 (0) | 2 (22.2) |
| Renal/urinary | 24 | 18 (75) | 2 (8.3) | 1 (5.6) | 1 (16.7) |
| Soft tissue | 21 | 15 (71.4) | 1 (4.8) | 0 | 1 (16.7) |
| Genital | 14 | 7 (50) | 1 (7.1) | 0 (0) | 1 (14.3) |
| ENT | 13 | 10 (76.9) | 1 (7.7) | 1 (10.0) | 0 (0) |
| Psychiatric | 12 | 8 (66.7) | 3 (25) | 2 (25.0) | 1 (25.0) |
| Endocrine | 4 | 4 (100) | 0 (0) | 0 (0) | ‒ |
| Eyes | 3 | 3 (100) | 0 (0) | 0 (0) | ‒ |
| Allergy | 3 | 2 (66.7) | 0 (0) | 0 (0) | 0 (0) |
| OB | 1 | 0 (0) | 0 (0) | ‒ | 0 (0) |
| Missing | 1 | 1 (100) | 0 (0) | 0 (0) | ‒ |
Abbreviations: CV, cardiovascular; ENT, ear, nose, and throat; GI, gastrointestinal; Neuro, neurologic; OB, obstetrical.
4. LIMITATIONS
This observational study has several important limitations. First, it is not possible to infer a causal link between VACC attendance and reduced risk of return ED visits from this observational analysis. Second, VACC patients were younger and likely had more access to digital resources than the overall ED population, raising questions about generalizability. Third, patients self‐selected to both schedule and attend VACC appointments, which could confound the associations between attendance and return visits if sicker patients are more likely to miss VACC appointments and to return to the ED. Despite our attempts to control for confounding factors, our dataset contained a relatively limited number of covariates and lacked data to fully characterize patient concerns, the content of ED care during the index and return visits, and the ultimate reasons patients sought care in any setting. Fourth, there is potential for reverse causality among non‐attenders if patients returned to the ED prior to their VACC appointment, but we observed this in only six of 99 (6%) non‐attenders. It is unknown if any of these return visits could have been avoided by VACC attendance, but four out of the six were discharged again following their ED evaluation. Finally, it should be emphasized that associations between individual complaints and return ED visits are derived from very small sample sizes and thus should be considered hypothesis‐generating rather than definitive findings.
Despite these inherent limitations to a pilot study, these data suggest that there may be real value in a post‐discharge, ED‐operated telehealth clinic. Further investigation is needed to delineate the drivers of ED use that the VACC is best suited to address and identify ED patients who stand to benefit from VACC appointments. Ultimately, a randomized clinical trial should determine the impact of a VACC appointment and evaluate the cost‐effectiveness of this approach.
5. DISCUSSION
Unscheduled return visits to the ED are common, 4 , 5 costly, 16 , 17 and may reflect failures of initial ED diagnosis, treatment, or communication or a lack of urgently available outpatient services to meet the needs of patients following discharge. 14 , 18 Hospital readmission reduction programs targeting improved transitions of care for hospital discharges have demonstrated some success in preventing unnecessary hospital readmissions, 19 suggesting similar models may be of benefit for ED discharges. Yet existing studies of telephone follow‐up and care coordination programs intended to improve transitions of care following ED discharge have not translated into reduced return ED visits. 20 This pilot study demonstrates the feasibility of an alternative model: an on‐demand virtual after care clinic staffed by emergency medicine clinicians.
During the pilot phase of this project, a very small percentage of patients discharged from the ED scheduled appointments at the VACC. We suspect that patients were largely unaware of the clinic since there was no consistent mechanism to encourage its use beyond patients’ own initiative in reading their discharge instructions and scheduling an appointment. Furthermore, the VACC clinic had substantial unfilled capacity. Nevertheless, the demographics of patients who did schedule appointments had interesting features that differed from the overall ED population. VACC appointments were most often scheduled by young, urban patients with commercial insurance and a PCP whose index ED visit occurred on a weekend. This group of patients is likely to have superior health literacy and financial resources compared to the general ED population. Furthermore, since nearly all VACC patients were already assigned to a PCP, it appears that lack of available appointments rather than lack of access to primary care motivated the decision to schedule a VACC appointment. Another surprising difference was the marked imbalance in VACC scheduling by sex. More than three quarters of VACC appointments were scheduled by females, a phenomenon that has been described for utilization of telehealth services in other settings. 21 , 22 , 23 Nevertheless, there was some diversity among patients scheduled appointments. One fourth of VACC patients were over the age of 50 years, one‐fourth were publicly insured, and one third were from rural settings. Moreover, there were no differences in VACC attendance by any demographic or clinical characteristic. These findings illustrate the potential for the VACC model to serve more medically vulnerable patients.
The goal of the VACC was to provide additional support to patients discharged from the ED to avoid unnecessary return ED visits. Compared to those who scheduled but did not attend a VACC appointment, VACC attendees were much less likely to return to the ED as far out as 30 days from their index ED visit. Furthermore, given the similar rates of ED return visits with hospitalization for VACC attenders and non‐attenders, we hypothesize that short‐term telehealth follow‐up sufficiently addressed patient concerns to curb some avoidable return ED visits. This finding stands in contrast to most care transition interventions previously studied. 20 Of note, two VACC patients were sent back to the ED and subsequently hospitalized, demonstrative value of these appointments in averting further delays in care for serious issues.
This pilot study is unable to define the precise mechanisms by which the VACC prevented return ED visits, but it is noteworthy that additional testing or medication changes occurred during a minority of visits. In fact, the most common function of VACC clinicians was to reinforce the content of the index ED visit, typically by reviewing and explaining test results and reassuring patients that continued outpatient follow‐up was still appropriate. Taken together, these findings support those from qualitative studies that suggest inadequate ED communication, lack of timely PCP access, and patient concerns about ongoing symptoms are key drivers of ED return visits, 7 , 8 , 9 all of which are potentially remedied by additional support services such as the VACC.
AUTHOR CONTRIBUTIONS
Study design, data analysis and interpretation, and manuscript preparation and revision: John Adam Oostema. Data collection and interpretation and manuscript revision: Todd Chassee. Study design, data interpretation, and manuscript revision: John Throop. Study design, data collection and interpretation, and manuscript revision: Christopher Port. Study design, data interpretation, and manuscript revision: John Deveau. Study design, data collection and interpretation, and manuscript revision: Stephanie Mullenix. Study design, data analysis and interpretation, and manuscript preparation and revision: Joshua C. Reynolds.
CONFLICT OF INTEREST STATEMENT
The authors report no financial conflicts of interest related to this project.
FUNDING INFORMATION
The authors received no specific funding for this work.
Biography
John Adam Oostema is an associate professor in the Department of Emergency Medicine at Michigan State University College of Medicine in Grand Rapids, Michigan, USA.
Oostema JA, Mullennix S, Chassee T, et al. Extending emergency care beyond discharge: Piloting a virtual after care clinic. JACEP Open. 2024;5:e13302. 10.1002/emp2.13302
Supervising Editor: Adam Landman, MD, MS
REFERENCES
- 1. Shy BD, Loo GT, Lowry T, et al. Bouncing back elsewhere: multilevel analysis of return visits to the same or a different hospital after initial emergency department presentation. Ann Emerg Med. 2018;71:555‐563.e551. doi: 10.1016/j.annemergmed.2017.08.023 [DOI] [PubMed] [Google Scholar]
- 2. Michelson KA, Lyons TW, Bachur RG, Monuteaux MC, Finkelstein JA. Timing and location of emergency department revisits. Pediatrics. 2018;141:e20174087. doi: 10.1542/peds.2017-4087 [DOI] [PubMed] [Google Scholar]
- 3. Rising KL, Victor TW, Hollander JE, Carr BG. Patient returns to the emergency department: the time‐to‐return curve. Acad Emerg Med. 2014;21:864‐871. doi: 10.1111/acem.12442 [DOI] [PubMed] [Google Scholar]
- 4. Hutchinson CL, McCloughen A, Curtis K. Incidence, characteristics and outcomes of patients that return to Emergency Departments. An integrative review. Australas Emerg Care. 2019;22:47‐68. doi: 10.1016/j.auec.2018.12.003 [DOI] [PubMed] [Google Scholar]
- 5. Trivedy CR, Cooke MW. Unscheduled return visits (URV) in adults to the emergency department (ED): a rapid evidence assessment policy review. Emerg Med J. 2015;32:324‐329. doi: 10.1136/emermed-2013-202719 [DOI] [PubMed] [Google Scholar]
- 6. Shy BD, Shapiro JS, Shearer PL, et al. A conceptual framework for improved analyses of 72‐hour return cases. Am J Emerg Med. 2015;33:104‐107. doi: 10.1016/j.ajem.2014.08.005 [DOI] [PubMed] [Google Scholar]
- 7. Hutchinson C, Curtis K, McCloughen A. Patients' experiences and reasons for unplanned return visits to the emergency department: a qualitative study. J Adv Nurs. 2023;79:2597‐2609. doi: 10.1111/jan.15617 [DOI] [PubMed] [Google Scholar]
- 8. Proud ME, Howard PK. Why do patients return to the emergency department? Adv Emerg Nurs J. 2016;38:83‐88. [DOI] [PubMed] [Google Scholar]
- 9. Rising KL, Padrez KA, O'Brien M, Hollander JE, Carr BG, Shea JA. Return visits to the emergency department: the patient perspective. Ann Emerg Med. 2015;65:377‐386. doi: 10.1016/j.annemergmed.2014.07.015 [DOI] [PubMed] [Google Scholar]
- 10. Sørup CM, Jacobsen P, Forberg JL. Evaluation of emergency department performance—a systematic review on recommended performance and quality‐in‐care measures. Scand J Trauma Resusc Emerg Med. 2013;21:62. doi: 10.1186/1757-7241-21-62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Calder L, Pozgay A, Riff S, et al. Adverse events in patients with return emergency department visits. BMJ Qual Saf. 2015;24:142‐148. doi: 10.1136/bmjqs-2014-003194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. van Loon‐van Gaalen M, Voshol IE, van der Linden MC, Gussekloo J, van der Mast RC. Frequencies and reasons for unplanned emergency department return visits by older adults: a cohort study. BMC Geriatr. 2023;23:309. doi: 10.1186/s12877-023-04021-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wu CL, Wang FT, Chiang YC, et al. Unplanned emergency department revisits within 72 hours to a secondary teaching referral hospital in Taiwan. J Emerg Med. 2010;38:512‐517. doi: 10.1016/j.jemermed.2008.03.039 [DOI] [PubMed] [Google Scholar]
- 14. Lin MP, Burke RC, Orav EJ, Friend TH, Burke LG. Ambulatory follow‐up and outcomes among medicare beneficiaries after emergency department discharge. JAMA Netw Open. 2020;3:e2019878. doi: 10.1001/jamanetworkopen.2020.19878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kelen GD, Wolfe R, D'Onofrio G, et al. Emergency department crowding: the canary in the health care system. Catalyst Non‐Issue Content. 2021;2. doi:10.1056/CAT.21.0217 [Google Scholar]
- 16. Weinick RM, Burns RM, Mehrotra A. Many emergency department visits could be managed at urgent care centers and retail clinics. Health Aff. 2010;29:1630‐1636. doi: 10.1377/hlthaff.2009.0748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Duseja R, Bardach NS, Lin GA, et al. Revisit rates and associated costs after an emergency department encounter: a multistate analysis. Ann Intern Med. 2015;162:750‐756. doi: 10.7326/m14-1616 [DOI] [PubMed] [Google Scholar]
- 18. Moskovitz JB, Ginsberg Z. Emergency department bouncebacks: is lack of primary care access the primary cause? J Emerg Med. 2015;49:70‐77.e74. doi: 10.1016/j.jemermed.2014.12.030 [DOI] [PubMed] [Google Scholar]
- 19. Braet A, Weltens C, Sermeus W. Effectiveness of discharge interventions from hospital to home on hospital readmissions: a systematic review. JBI Database System Rev Implement Rep. 2016;14:106‐173. 10.11124/jbisrir-2016-2381 [DOI] [PubMed] [Google Scholar]
- 20. Aghajafari F, Sayed S, Emami N, Lang E, Abraham J. Optimizing emergency department care transitions to outpatient settings: a systematic review and meta‐analysis. Am J Emerg Med. 2020;38:2667‐2680. doi: 10.1016/j.ajem.2020.07.043 [DOI] [PubMed] [Google Scholar]
- 21. Drake C, Lian T, Cameron B, Medynskaya K, Bosworth HB, Shah K. Understanding telemedicine's “new normal”: variations in telemedicine use by specialty line and patient demographics. Telemed J E Health. 2022;28:51‐59. doi: 10.1089/tmj.2021.0041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Khatana SAM, Yang L, Eberly LA, Julien HM, Adusumalli S, Groeneveld PW. Predictors of telemedicine use during the COVID‐19 pandemic in the United States—an analysis of a national electronic medical record database. PLoS One. 2022;17:e0269535. doi: 10.1371/journal.pone.0269535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Luo J, Tong L, Crotty BH, et al. Telemedicine adoption during the COVID‐19 pandemic: gaps and inequalities. Appl Clin Inform. 2021;12:836‐844. doi: 10.1055/s-0041-1733848 [DOI] [PMC free article] [PubMed] [Google Scholar]


