Abstract
Background
Cancer therapy is considered to cause accelerated ischemia. Ankle-Brachial Index (ABI) measurement is an inexpensive, simple, available test for the early diagnosis of peripheral artery disease (PAD); however, it is not performed routinely. We aimed to evaluate the role of routine ABI measurement for the diagnosis of PAD among patients diagnosed with cancer and whether it correlates with left ventricular (LV) dysfunction.
Methods
A retrospective, single-center study including patients diagnosed with cancer at Tel Aviv Sourasky Medical Center. The cohort included patients performing routine ABI and LV global longitudinal strain (GLS) echocardiography. The primary endpoint was the prevalence of PAD and whether it correlates with LV dysfunction, defined by LV GLS absolute value < 19%. The secondary composite endpoint evaluated the association between reduced ABI to LV dysfunction and all-cause mortality.
Results
Among 226 patients, PAD was diagnosed in 14 patients (6%). We revealed a positive correlation between ABI and LV GLS (r = 0.22, p < 0.01) with a reduced mean ABI score among patients with reduced LV GLS. A reduced mean ABI was observed among the positive composite endpoint group; however, it was not statistically significant (p = 0.35).
Conclusions
We report, for the first time to our knowledge, the routine use of ABI testing among patients diagnosed with cancer. ABI showed a significant correlation to LV GLS, implying a potential tool in the early diagnosis of atherosclerosis and cardiotoxicity. Considering its low cost and availability, future prospective trials are needed to integrate its role in routine assessment.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40959-024-00262-w.
Keywords: ABI, PAD, Atherosclerosis, LV GLS, LV dysfunction, Cardiotoxicity
Introduction
Cancer therapy, including chemotherapy, radiation, and biologic therapy, can lead to cardiac injury [1], primarily characterized by left ventricular (LV) dysfunction, and may manifest as transient subclinical damage or progress to full-blown heart failure (HF) [2]. To prevent cardiac injury, defined as cardiotoxicity, the search for early subclinical markers is emerging. Currently, the primary diagnostic tool for identifying cardiotoxicity relies on two-dimensional (2D) echocardiography, which predominantly assesses the left ventricular ejection fraction (LVEF) [3]. However, since a decline in LVEF becomes apparent only in the presence of substantial cardiac damage [4], the innovative 2D speckle tracking echocardiography (2D-STE), with a specific focus on LV global longitudinal strain (LV GLS), is considered the optimal tool for early detection of LV dysfunction in patients diagnosed with cancer [3, 5]. Recent studies have demonstrated that LV GLS measurements exhibit higher replicability [6] and greater sensitivity [7] than LVEF measurements. Furthermore, early alternations in LV GLS serve as a predictive indicator for the onset of cardiotoxicity [8, 9] and mortality [10]. While cancer therapy is considered cardiotoxic directly to the myocardium, causing LV dysfunction, it is also known to cause accelerated atherosclerosis and ischemia, mainly in the coronary arteries [11]. Recently, several studies revealed structural arterial remodeling, increased arterial stiffness, and endothelial dysfunction after anthracycline therapy [12]. While arterial stiffness is an independent risk factor for future cardiovascular (CV) diseases in the general population [13], limited data is available regarding its role in patients diagnosed with cancer. Furthermore, acknowledging that atherosclerosis is a poly-vascular disease, it has been reported that 25% of the patients diagnosed with coronary artery disease (CAD) had concomitant disease in other vascular beds, including cerebrovascular and peripheral arterial disease (PAD). While the estimated prevalence of PAD in the developed world is approximately 9–11% [14], the occurrence among females is lower, estimated at around 4% [15]. Additionally, PAD is often deemed underdiagnosed due to the absence of classic symptoms, such as peripheral claudication, in the majority of patients [16]. Ankle-Brachial Index (ABI) testing is an inexpensive, simple, available test for the early diagnosis of PAD [17]. However, it is not performed routinely, neither in the general population nor in patients diagnosed with cancer. While PAD has been associated with unfavorable prognosis in HF patients [18], its role as a marker for the early diagnosis of cardiotoxicity in patients diagnosed with cancer is still unknown.
Our study aimed to evaluate the role of routine ABI measurement for early diagnosis of PAD in patients diagnosed with cancer and further investigate its correlation with LV dysfunction, assessed by LV GLS.
Methods
Study population
We conducted a retrospective, single-center, observational study at Tel Aviv Sourasky Medical Center, a tertiary cancer center in Israel. The study was approved by the local ethics Tel Aviv Sourasky committee (Identifier: 0228–16-TLV). ABI measurement is not performed routinely in our cardio-oncology clinic. Still, it was performed as part of a grant given to us by Bayer Israel Ltd to identify PAD in patients with ischemic heart disease (IHD). To assess potential benefits, we incorporated routine ABI measurement as a key exploratory process over three months. The cohort included adult patients who performed routine ABI and LV GLS assessments within one month. Exclusion criteria included age < 18 years, absence of ABI or LV GLS assessment, or an interval greater than one month between the two tests.
Data collection
Baseline medical history, treatment, cancer type, and cancer therapy were reviewed via electronic medical charts. Cardiac risk factors included diabetes mellitus (DM), hypertension (HTN), hyperlipidemia, and chronic kidney disease (CKD), as defined by the 2022 ESC guidelines [19], and were diagnosed by the treating physician and updated in the medical chart. CV diseases were determined by the treating cardio-oncologist (M.L.P).
ABI measurement, using the MESI (ABPIMDACFFSL) device, was performed routinely as part of the cardio-oncology clinic evaluation for an explarotory period of three months. ABI score < 0.9 was considered diagnostic for PAD, according to the accepted literature [20].
Echocardiography
Three standard apical views (4-chamber, 2-chamber, and apical long-axis) were recorded using a General Electric system, model Vivid S70 echocardiogram, and performed by the same vendor, technician and interpreting cardiologist to prevent inter-vendor variability. Images were acquired using a high frame rate (> 50 frames/s) and stored digitally for offline analysis. LV GLS was measured using STE software and tracking within an approximately 5 mm wide region of interest. A mid-systolic frame was used to initialize LV boundaries, automatically tracked throughout the cardiac cycle. Manual corrections were performed to optimize boundary tracking as needed. Optimization of images for endocardial visualization through adjustment of gain, compress, and time-gain compensation controls was done before acquisition.
Study endpoints
Our primary endpoint was to evaluate the prevalence of PAD among patients diagnosed with cancer and whether there is a correlation between reduced ABI and LV dysfunction, defined by LV GLS absolute value < 19%, as accepted by the literature [3].
Our secondary composite endpoint evaluated whether reduced ABI is associated with the development of LV dysfunction (defined as relative LV GLS decrease of 15% or absolute LVEF decrease of 10% between consecutive follow-up visits) [3] and all-cause mortality.
Statistical analysis
Categorical variables were expressed as frequency and percentages. The distribution of continuous variables was assessed using a histogram and Q-Q plot. Normally distributed continuous variables were described using mean and standard deviation (SD), and non-normally distributed continuous variables using median and interquartile range (IQR). A Chi-square test was used to evaluate the association between categorical variables. Continuous variables were compared using the independent sample t-test or the Mann–Whitney U test, depending on the distribution. The correlation between continuous variables was evaluated using Spearman's correlation coefficient. The relationship between ABI and LV GLS was assessed as two continuous variables using Pearson’s correlation. The difference in ABI values between visits was assessed using a mixed-effects model with Tukey’s test for multiple comparisons. A 2-tailed p-value of < 0.05 was considered significant for all analyses. All analyses were performed using the SPSS software V.29 (SPSS Inc., Chicago, IL).
Results
From November 2020 to January 2021, 226 patients diagnosed with cancer who had performed ABI and LV GLS assessments were included. Baseline clinical characteristics are summarized in Tables 1, 2, 3, 4. Our cohort’s mean age was 64 ± 14 years, with a female predominantly (67%). The most prevalent cancer diagnosis was Breast (44%), followed by Multiple Myeloma (12%). The primary cancer therapy administered included doxorubicin (47%), cyclophosphamide (48%), paclitaxel (37%), and radiation (27%).
Table 1.
Baseline characteristics
| Demographics Characteristics | N = 226 |
|---|---|
| Age, years, mean (SD) | 64 (14) |
| Female (sex, assigned at birth), n (%) | 153 (67) |
| Height, Cm, mean (SD) | 166 (8) (N = 155) |
| Weight, Kg, mean (SD) | 69.65 (14.91) (N = 195) |
| BMI, Kg/m2, mean (SD) | 25.44 (4.59) (N = 155) |
n Number, SD Standard deviation
Table 2.
Baseline cancer characteristics
| Cancer type, n (%) | Cancer therapy, n (%) | ||
|---|---|---|---|
| Doxorubicin | 106 (47) | ||
| Breast cancer | 99 (44) | Cyclophosphamide | 109 (48) |
| Multiple Myeloma | 28 (12) | Docetaxel | 14 (6) |
| Lymphoma | 20 (9) | Carboplatin | 30 (13) |
| Lung cancer | 7 (3) | Trastuzumab | 34 (15) |
| Prostate cancer | 7 (3) | Pertuzumab | 28 (12) |
| Colorectal cancer | 8 (4) | Paclitaxel | 84 (37) |
| Osteosarcoma | 14 (6) | Flourouracil | 14 (6) |
| Leukemia | 3 (1) | Bevacizumab | 8 (4) |
| Other | 35 (15) | Radiation | 60 (27) |
n Number, SD Standard deviation
Table 3.
Baseline medical characteristics
| Medical History, n (%) | |
| Hypertension | 94 (42) |
| Diabetes Meletus | 40 (18) |
| Hyperlipidemia | 65 (29) |
| Ischemic Heart disease | 45 (20) |
| Congestive heart failure | 42 (19) |
| Atrial fibrillation | 26 (11) |
| Cerebrovascular accident | 10 (4) |
| Cardiac Specific Medications, n (%) | |
| Beta blocker | 70 (31) |
| Statin | 70 (31) |
| RAASi | 36 (16) |
| Furosemide | 26 (12) |
| MRA | 16 (7) |
| Aspirin | 47 (21) |
n Number, SD Standard deviation, RAASi Renin–angiotensin–aldosterone system inhibitors, MRA Aldosterone receptor antagonist
Table 4.
Baseline echocardiography characteristics
| Echocardiographic Baseline measurements, mean (SD) | |
|---|---|
| Ejection fraction, % | 57 (6) |
| GLS, % | 19 (4) |
| LVEDD, cm | 4.74 (0.67) |
| LVESD, cm | 2.92 (0.67) |
| IVS, cm | 1.16 (0.33) |
| E/A ratio | 0.80 (0.25) |
| Deceleration time, ms | 237 (86) |
| E' medial, m/s | 5.95 (1.72) |
| E' lateral, m/s | 7.75 (2.53) |
| E/e medial | 11.22 (3.28) |
| E/e lateral | 8.94 (3.12) |
| E/e average | 10.16 (3.16) |
| LA volume, ml | 72.38 (34.45) |
| LA volume index, ml/m2 | 16.96 (22.13) |
| TAPSE, cm | 2.26 (0.69) |
| SPAP, mmHg | 34 (8) |
| Diastolic function | |
| Normal | 104 (46) |
| Grade 1 dysfunction | 85 (38) |
| Grade 2 dysfunction | 30 (13) |
| Grade 3 dysfunction | 2 (1) |
SD Standard deviation, GLS Global Longitudinal Strain, LA left atrial, LVEDD Left ventricular end-diastolic dimension, LVESD Left ventricular end-systolic dimension, cm centimeter, IVS Interventricular septum, ms milliseconds, ml milliliter, TASPE Tricuspid annular plane systolic excursion, SPAP systolic pulmonary arterial pressure, mmHg millimetre of mercury
Cardiac risk factors were relatively common, as expected, among this elderly population and included HTN (42%), hyperlipidemia (29%), and DM (18%). Overall, 20% and 4% of the patients had a baseline diagnosis of IHD and cerebrovascular accident (CVA), respectively. A total of 16%, 31%, 31%, and 21% of the patients were treated with Renin–angiotensin–aldosterone system (RAASi), beta-blockers (BB), statins, and aspirin, respectively.
Baseline LVEF was 57 ± 6%, and absolute LV GLS was 19 ± 4%. Diastolic dysfunction grade 1 and 2 was observed in 38% and 13% of the patients, respectively. Diastolic parameters included mean e’ lateral 7.75 ± 2.53m/s, mean E/e’ lateral 8.94 ± 3.12, mean left atrial volume index (LAVI) 16.96 ± 22.13ml/m2, and mean systolic pulmonary artery pressure (SPAP) 34 ± 8mmHg (Table 4).
The mean ABI score was 1.10 ± 0.4, and PAD was diagnosed in 14 patients (6%). Four patients presented with ABI 0.5. Due to the small number, we do not believe it affects the final results. Using the same ABI methodology, we evaluated the prevalence of PAD among a non-cancer population in our clinic. We found a prevalence of 21 (9%) patients, with no significant differences in PAD prevalence and mean ABI following adjustment to age and sex.
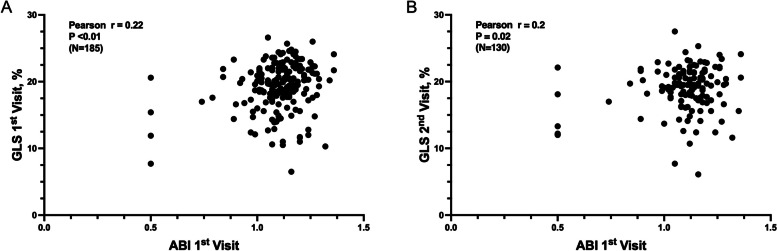
Evaluating the correlation between ABI and LV GLS at 1st visit, we revealed a Pearson correlation coefficient (r) of 0.22, indicating a positive (p < 0.01) linear relationship between the two variables. Furthermore, we assessed the correlation of ABI at 1st visit with LV GLS at 2nd visit, finding a Pearson correlation coefficient (r) of 0.2 with p = 0.02 (Fig. 1).
Fig. 1.
A and B ABI and LV GLS correlation. A Correlation between ABI at visit 1 and LV GLS at visit 1 B Correlation between ABI at visit 1 and LV GLS at visit 2
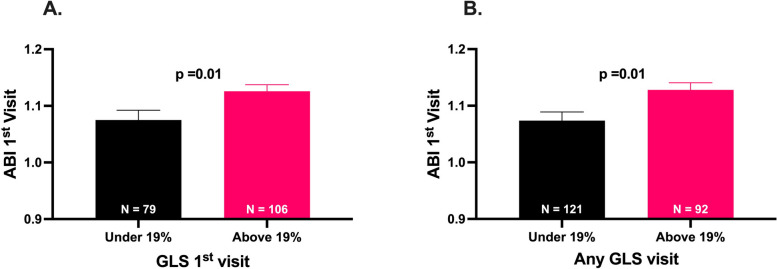
Investigating the potential relationship between reduced ABI and cardiac damage, defined by LV GLS < 19%, we found a reduced mean ABI score at 1st visit in patients presented with LV GLS < 19% at the 1st visit (1.08 ± 0.15 vs. 1.13 ± 0.12, p = 0.01) (Fig. 2A), or in any following visit (1.07 ± 0.16 vs. 1.13 ± 0.12, p < 0.01) (Fig. 2B).
Fig. 2.
A and B Mean ABI and LV GLS < 19%. A Mean ABI according to LV GLS under and above 19% at visit 1 (B) Mean ABI according to LV GLS under and above 19% at any visit during follow-up visits
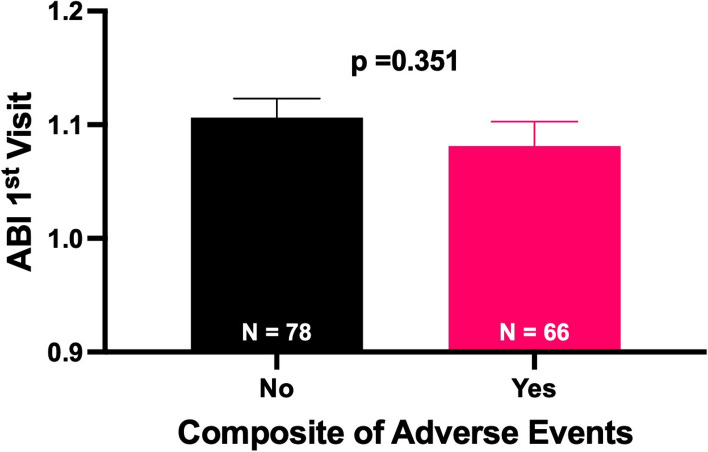
During a median follow-up of 7 [IQR 2–11] months, a total of 66 (29%) patients presented with the secondary composite endpoints; among them, 27 (12%) patients died, and 42 (19%) patients developed LV dysfunction (Table 5). Evaluating the association between reduced ABI and the development of secondary composite endpoints, we found that a reduced mean ABI was observed among the positive composite endpoint group (1.08 ± 0.17 vs. 1.11 ± 0.14); however, it was not statistically significant (p = 0.35) (Fig. 3).
Table 5.
Secondary Endpoint
| N = 226 | |
|---|---|
| Total LV Dysfunction, n (%) | 42 (19) |
| 10% absolute reduction in LV Ejection Fraction, n (%) | 19 (8) |
| 15% relative reduction in LV GLS, n (%) | 23 (10) |
| All-cause mortality, n (%) | 27 (12) |
n Number, LV Left ventricular, GLS Global longitudinal starin
Fig. 3.
Mean ABI according to Secondary Composite endpoints
Discussion
We performed a pivotal retrospective analysis of patients diagnosed with cancer and routinely performed ABI measurements. We found a 6% prevalence of PAD among our cohort and a close interaction between atherosclerosis and LV dysfunction, defined by reduced LV GLS.
As a response to the call to action expressed by both the American and European Cardio‐Oncology Guidelines [21], for the early diagnosis of cardiotoxicity, LV GLS emerged as the primary parameter for early subclinical LV dysfunction assessment among patients treated with cancer therapy [22]. However, since LV GLS assessment requires knowledge, practice, and technology and comes at a relatively high cost, it is still not widely available and is not performed routinely in all centers. Moreover, while LV dysfunction has been the main focus of cardiotoxicity in recent years, lately, there has been increasing awareness of accelerated ischemia among patients diagnosed with cancer [11]. While several studies revealed structural arterial remodeling, increased arterial stiffness, and endothelial dysfunction in patients treated with anthracycline therapy [12], data, among other therapies, is limited, and there are no recommendations for routine assessment for atherosclerosis among this population [19]. Acknowledging that atherosclerosis is a poly-vascular disease, it is reported that 61% of patients diagnosed with PAD had concomitant disease in other vascular beds [14]. Therefore, we attempted to assess, for the first time to our knowledge, the role of routine ABI measurement as a novel screening tool for the early diagnosis of atherosclerosis and LV dysfunction among patients diagnosed with cancer. Our reasoning behind this decision leaned on previous literature suggesting that an ABI measurement is reliable [17] in establishing the diagnosis of PAD, specifically in primary care clinics. We believe a simple, relatively available diagnostic tool can help determine susceptible patients who will benefit from earlier cardioprotective therapy.
We found a prevalence of 6% of PAD among our cohort population, which is relatively high compared to the general population, considering that most of our cohort is females. Our efforts yielded a statistically significant association between ABI score and LV GLS values at the same evaluation time. Furthermore, this correlation persisted in the follow-up visit, showing that a lower ABI score at baseline may indicate future cardiac toxicity manifested by a reduced LV GLS.
Longitudinally oriented myocardial fibers evaluated by LV GLS are located in the sub-endocardial space, the area most susceptible to ischemia, and thus, measurements of longitudinal motion and deformation are the most sensitive markers of pathology [23, 24]. Past studies have shown that LV GLS may have a role in assessing coronary artery disease [25] and myocardial ischemia [26, 27]. Our study supports those findings by implying a positive association between PAD and reduced LV GLS.
While patients developing a secondary composite endpoint presented with a lower baseline ABI score, it did not reach statistical significance.
Our study has several limitations. First, it is a single-center study, and thus, the generalization of our results is limited. However, since Tel Aviv Sourasky is a tertiary referral cancer center in Israel, the study population includes a variety of ethnic origins from all over the country. Second, this is a retrospective study. Therefore, our results are subject to the effects of potential confounders inherent to the nature of such studies. Third, it is important to note that using computerized patient charts from the Population Registry Bureau did not provide information on the cause of death. Consequently, we were unable to assess CV mortality. Fourth, our study included all patients evaluated in the cardio-oncology clinic. Therefore, our cohort is heterogenic and diverse, including different types of cancer and cancer therapy at a different time point of therapy. Due to the small number of patients in each group, we could not assess each cancer type or therapy separately; however, we believe that showing the positive correlation of ABI in this real-world heterogeneous population is an advantage. Fifth, we acknowledge that our cohort has a high prevalence of baseline risk factors for atherosclerosis and baseline IHD. Those risk factors are known to increase the risk for both PAD development as well as cardiotoxicity. Due to the low number of patients in each group, we could not perform a multivariable regression assessment. However, we aimed to assess the role of ABI measurement as an additional early marker for cardiotoxicity and LV dysfunction, regardless of baseline chronic diseases. Six, while other imaging, such as angiography and computed tomography, can show the extent and degree of atherosclerosis and be more accurate, they are other invasive or have higher cost and lower availability. ABI is a simple, low-cost, and available test and is considered a reliable tool for diagnosing PAD by the ACC/AHA [26]. Last, we are aware that due to the low number of PAD cases, we cannot reliably assess its correlation to LV dysfunction and all-cause mortality, and a larger prospective trial with a more extended follow-up period is needed.
In conclusion, we report for the first time the routine use of ABI measurement among patients diagnosed with cancer. PAD was relatively high among this population, and the ABI score showed a significant correlation to LV GLS assessment, suggesting a potential tool in the early diagnosis of atherosclerosis and cardiotoxicity. Considering its low cost and high availability, future prospective trials are needed to further evaluate its role as an additional tool for early diagnosis of cardiotoxicity.
Supplementary Information
Acknowledgements
This paper was conducted as part of the Hebrew University in Jerusalem MD program requirements.
Abbreviations
- ABI
Ankle-Brachial Index
- LV
Left Ventricle
- GLS
Global Longitudinal Strain
- PAD
Peripheral Artery Disease
- DM
Diabetes Mellitus
- HTN
Hypertension
- CKD
Chronic Kidney Disease
- IHD
Ischemic Heart Disease
- RAASi
Renin-Angiotensin-Aldosterone System Inhibitors
- BB
Beta Blockers
- CAD
Coronary Artery Disease
- SPAP
Systolic Pulmonary Artery Pressure
- LVEF
Left Ventricular Ejection Fraction
- 2D
Two-dimensional
- STE
Speckle Tracking Echocardiography
- ESC
European Society of Cardiology
- CV
Cardiovascular
- IQR
Interquartile Range
- SD
Standard Deviation
- BMI
Body Mass Index
Authors’ contributions
N.G wrote the main manuscript text, R.Y.B performed the statistics, M.S and S.K collected the data, O.H, Y.T, S.B and M.L.P performed the analysis and interpretation of data and reviewed the paper.
Funding
Dr. Michal Laufer-Perl received a research grant from Bayer Israel Ltd to.
perform ABI test during 2020–2022.
Availability of data and materials
Data cannot be shared for ethical/privacy reasons.
Data Availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
The study was approved by the Tel Aviv Sourasky Medical Center.
Helsinki Regulatory Ethics Committee (Identifier: TLV-0228–16(. Due to the retrospective.
Nature of the trial, the Ethics Committee waved the requirement for consent.
Consent of publication
Not applicable.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Angsutararux P, Luanpitpong S, Issaragrisil S. Chemotherapy-Induced Cardiotoxicity: Overview of the Roles of Oxidative Stress. Oxid Med Cell Longev. 2015;2015:1–13. 10.1155/2015/795602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Armenian SH, Lacchetti C, Barac A, Carver J, Constine LS, Denduluri N, Dent S, Douglas PS, Durand JB, Ewer M, Fabian C, Hudson M, Jessup M, Jones LW, Ky B, Mayer EL, Moslehi J, Oeffinger K, Ray K, Ruddy K, Lenihan D. Prevention and monitoring of cardiac dysfunction in survivors of adult cancers: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. 2017;35(8):893–911. 10.1200/JCO.2016.70.5400 [DOI] [PubMed] [Google Scholar]
- 3.Plana JC, Galderisi M, Barac A, Ewer MS, Ky B, Scherrer-Crosbie M, Ganame J, Sebag IA, Agler DA, Badano LP, Banchs J, Cardinale D, Carver J, Cerqueira M, DeCara JM, Edvardsen T, Flamm SD, Force T, Griffin BP, Jerusalem G, Lancellotti P. Expert consensus for multimodality imaging evaluation of adult patients during and after cancer therapy: a report from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovas Imaging. 2014;15(10):1063–93. 10.1093/ehjci/jeu192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eidem BW. Identification of anthracycline cardiotoxicity: left ventricular ejection fraction is not enough. J Am Soc Echocardiogr. 2008;21(12):1290–2. 10.1016/j.echo.2008.10.008 [DOI] [PubMed] [Google Scholar]
- 5.Santoro C, Arpino G, Esposito R, Lembo M, Paciolla I, Cardalesi C, de Simone G, Trimarco B, De Placido S, Galderisi M. 2D and 3D strain for detection of subclinical anthracycline cardiotoxicity in breast cancer patients: a balance with feasibility. European Heart Journal - Cardiovascular Imaging. 2017;18(8):930–6. 10.1093/ehjci/jex033 [DOI] [PubMed] [Google Scholar]
- 6.Karlsen S, Dahlslett T, Grenne B, Sjøli B, Smiseth O, Edvardsen T, Brunvand H. Global longitudinal strain is a more reproducible measure of left ventricular function than ejection fraction regardless of echocardiographic training. Cardiovasc Ultrasound. 2019;17(1):18. 10.1186/s12947-019-0168-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krishnasamy R, Isbel NM, Hawley CM, Pascoe EM, Burrage M, Leano R, Haluska BA, Marwick TH, Stanton T. Left Ventricular Global Longitudinal Strain (GLS) Is a Superior Predictor of All-Cause and Cardiovascular Mortality When Compared to Ejection Fraction in Advanced Chronic Kidney Disease. PLoS ONE. 2015;10(5): e0127044. 10.1371/journal.pone.0127044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arciniegas Calle MC, Sandhu NP, Xia H, Cha SS, Pellikka PA, Ye Z, Herrmann J, Villarraga HR. Two-dimensional speckle tracking echocardiography predicts early subclinical cardiotoxicity associated with anthracycline-trastuzumab chemotherapy in patients with breast cancer. BMC Cancer. 2018;18(1):1037. 10.1186/s12885-018-4935-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laufer-Perl M, Derakhshesh M, Milwidsky A, Mor L, Ravid D, Amrami N, Sherez J, Keren G, Topilsky Y, Arbel Y. Usefulness of Global Longitudinal Strain for Early Identification of Subclinical Left Ventricular Dysfunction in Patients With Active Cancer. Am J Cardiol. 2018;122(10):1784–9. 10.1016/j.amjcard.2018.08.019 [DOI] [PubMed] [Google Scholar]
- 10.Laufer-Perl M, Arnold JH, Mor L, Amrami N, Derakhshesh M, Moshkovits Y, Sadeh B, Arbel Y, Topilsky Y, Rozenbaum Z. The association of reduced global longitudinal strain with cancer therapy-related cardiac dysfunction among patients receiving cancer therapy. Clin Res Cardiol. 2020;109(2):255–62. 10.1007/s00392-019-01508-9 [DOI] [PubMed] [Google Scholar]
- 11.Chang HM, Moudgil R, Scarabelli T, Okwuosa TM, Yeh ETH. Cardiovascular Complications of Cancer Therapy: Best Practices in Diagnosis, Prevention, and Management: Part 1. J Am Coll Cardiol. 2017;70(20):2536–51. 10.1016/j.jacc.2017.09.1096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mozos I, Borzak G, Caraba A, Mihaescu R. Arterial stiffness in hematologic malignancies. Onco Targets Ther. 2017;10:1381–8. 10.2147/OTT.S126852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Novo S, Carità P, Corrado E, Muratori I, Pernice C, Tantillo R, Novo G. Preclinical carotid atherosclerosis enhances the global cardiovascular risk and increases the rate of cerebro- and cardiovascular events in a five-year follow-up. Atherosclerosis. 2010;211(1):287–90. 10.1016/j.atherosclerosis.2010.01.019 [DOI] [PubMed] [Google Scholar]
- 14.Bhatt DL, Steg PG, Ohman EM, Hirsch AT, Ikeda Y, Mas JL, Goto S, Liau CS, Richard AJ, Röther J, Wilson PW, REACH Registry Investigators. International prevalence, recognition, and treatment of cardiovascular risk factors in outpatients with atherothrombosis. JAMA. 2006;295(2):180–9. 10.1001/jama.295.2.180 [DOI] [PubMed] [Google Scholar]
- 15.Gonçalves-Martins G, Gil-Sala D, Tello-Díaz C, Tenezaca-Sari X, Marrero C, Puig T, Gayarre R, Fité J, Bellmunt-Montoya S. Prevalence of Peripheral Arterial Disease and Associated Vascular Risk Factors in 65-Years-Old People of Northern Barcelona. J Clin Med. 2021;10(19):4467. 10.3390/jcm10194467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hirsch AT, Criqui MH, Treat-Jacobson D, Regensteiner JG, Creager MA, Olin JW, Krook SH, Hunninghake DB, Comerota AJ, Walsh ME, McDermott MM, Hiatt WR. Peripheral arterial disease detection, awareness, and treatment in primary care. JAMA. 2001;286(11):1317–24. 10.1001/jama.286.11.1317 [DOI] [PubMed] [Google Scholar]
- 17.Ichihashi S, Desormais I, Hashimoto T, Magne J, Kichikawa K, Aboyans V. Accuracy and Reliability of the Ankle Brachial Index Measurement Using a Multicuff Oscillometric Device Versus the Doppler Method. European journal of vascular and endovascular surgery: the official journal of the European Society for Vascular Surgery. 2020;60(3):462–8. 10.1016/j.ejvs.2020.06.013 [DOI] [PubMed] [Google Scholar]
- 18.Wei B, Qian C, Fang Q, Wang Y. The Prognostic Value of Peripheral Artery Disease in Heart Failure: Insights from a Meta-analysis. Heart Lung Circ. 2016;25(12):1195–202. 10.1016/j.hlc.2016.04.002 [DOI] [PubMed] [Google Scholar]
- 19.Lyon AR, Lopez-Fernandez T, Couch LS, Asteggiano R, Aznar MC, Bergler-Klein J, Boriani G, Cardinale D, Cordoba R, Cosyns B, Cutter DJ, de Azambuja E, de Boer RA, Dent SF, Farmakis D, Gevaert SA, Gorog DA, Herrmann J, Lenihan D, Moslehi J, ESC Scientific Document Group. 2022 ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS) Developed by the task force on cardio-oncology of the European Society of Cardiology (ESC). Eur Heart J Cardiovasc Imaging. 2022;43(41):4229–361. [DOI] [PubMed] [Google Scholar]
- 20.Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, Hiratzka LF, Murphy WR, Olin JW, Puschett JB, Rosenfield KA, Sacks D, Stanley JC, Taylor LM Jr, White CJ, White J, White RA, Antman EM, Smith SC Jr, Adams CD, ... Vascular Disease Foundation. ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation. 2006;113(11):e463–e654. [DOI] [PubMed]
- 21.Alexandre J, Cautela J, Ederhy S, Damaj GL, Salem JE, Barlesi F, Farnault L, Charbonnier A, Mirabel M, Champiat S, Cohen-Solal A, Cohen A, Dolladille C, Thuny F. Cardiovascular Toxicity Related to Cancer Treatment: A Pragmatic Approach to the American and European Cardio-Oncology Guidelines. J Am Heart Assoc. 2020;9(18): e018403. 10.1161/JAHA.120.018403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oikonomou EK, Kokkinidis DG, Kampaktsis PN, Amir EA, Marwick TH, Gupta D, Thavendiranathan P. Assessment of Prognostic Value of Left Ventricular Global Longitudinal Strain for Early Prediction of Chemotherapy-Induced Cardiotoxicity: A Systematic Review and Meta-analysis. JAMA cardiology. 2019;4(10):1007–18. 10.1001/jamacardio.2019.2952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoffmann S, Jensen JS, Iversen AZ, Sogaard P, Galatius S, Olsen NT, Bech J, Fritz-Hansen T, Biering-Sorensen T, Badskjaer J, Pietersen A, Mogelvang R. Tissue Doppler echocardiography improves the diagnosis of coronary artery stenosis in stable angina pectoris. Eur Heart J Cardiovasc Imaging. 2012;13(9):724–9. 10.1093/ehjci/jes001 [DOI] [PubMed] [Google Scholar]
- 24.Hoffmann S, Mogelvang R, Sogaard P, Iversen AZ, Hvelplund A, Schaadt BK, Fritz-Hansen T, Galatius S, Risum N, Biering-Sørensen T, Jensen JS. Tissue Doppler echocardiography reveals impaired cardiac function in patients with reversible ischaemia. European journal of echocardiography : the journal of the Working Group on Echocardiography of the European Society of Cardiology. 2011;12(8):628–34. 10.1093/ejechocard/jer094 [DOI] [PubMed] [Google Scholar]
- 25.Biering-Sørensen T, Hoffmann S, Mogelvang R, Zeeberg Iversen A, Galatius S, Fritz-Hansen T, Bech J, Jensen JS. Myocardial strain analysis by 2-dimensional speckle tracking echocardiography improves diagnostics of coronary artery stenosis in stable angina pectoris. Circ Cardiovasc Imaging. 2014;7(1):58–65. 10.1161/CIRCIMAGING.113.000989 [DOI] [PubMed] [Google Scholar]
- 26.Elimelech C, Zornitzki L, Konigstein M, Rozenbaum Z, Arnold JH, Havakuk O, Revivo M, Flint N, Khoury S, Topilsky Y, Banai S, Laufer-Perl M. Baseline Left Ventricle Longitudinal Strain as a Predictor for Clinical Improvement Following Coronary Sinus Reducer Implantation. Am J Cardiol. 2023;204:77–83. 10.1016/j.amjcard.2023.07.026 [DOI] [PubMed] [Google Scholar]
- 27.Laufer-Perl M, Arnold JH, Moshkovits Y, Havakuk O, Shmilovich H, Chausovsky G, Sivan A, Szekely Y, Arbel Y, Banai S, Topilsky Y, Rozenbaum Z. Evaluating the role of left ventricle global longitudinal strain in myocardial perfusion defect assessment. Int J Cardiovasc Imaging. 2022;38(2):289–96. 10.1007/s10554-021-02399-6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data cannot be shared for ethical/privacy reasons.
No datasets were generated or analysed during the current study.