Abstract
Background
Techniques in endovascular therapy have evolved to offer a promising alternative to medical therapy alone for Type B aortic dissections (TBADs).
Aim
The aim of this meta-analysis was to compare mortality and overall complications between thoracic endovascular aortic repair (TEVAR) and best medical therapy (BMT) in patients with TBADs.
Methods
We included randomized control trials and prospective or retrospective cohort studies that compared TEVAR and BMT for the treatment of type B aortic dissection. Multiple electronic databases were searched.
Results
Thirty-two cohort studies including 150,836 patients were included. TEVAR was associated with a significantly lower 30-day mortality rate than BMT (RR = 0.79, CI = 0.63, 0.99, P = 0.04), notably in patients ≥ 65 years of age (RR = 0.78, CI = 0.64, 0.95, P = 0.01). The TEVAR group had a significantly prolonged hospital stay (MD = 3.42, CI = 1.69, 5.13, P = 0.0001) and ICU stay (MD = 3.18, CI = 1.48, 4.89, P = 0.0003) compared to the BMT. BMT was associated with increased stroke risk (RR = 1.52, CI = 1.29, 1.79, P < 0.00001). No statistically significant differences in late mortality (1, 3, and 5 years) or intervention-related factors (acute renal failure, spinal cord ischemia, myocardial infarction, respiratory failure, and sepsis) were noted between the groups.
Conclusion
Our meta-analysis revealed a significant association between the TEVAR group and a decreased mortality rate of TBAD compared to the medical treatment group, especially in patients aged 65 years or older. Further randomized controlled trials are needed to confirm our findings.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12893-024-02555-4.
Keywords: Thoracic endovascular aortic repair, Medical therapy, Type B aortic dissection
Introduction
Aortic dissection (AD) is a known component of acute aortic syndrome, in conjunction with intramural hematoma and a penetrating aortic ulcer. It develops when the intimal layer of the aorta tears, allowing blood to leak into the wall and creating a dissection plane along the medial layer. Uncontrolled hypertension and trauma are the frequent causes of dissection. Occasionally, an underlying connective tissue condition predisposes the patient to its pathogenesis [1].
The majority of the 43,000 to 47,000 aortic disease-related deaths that occur annually in the United States are linked to dissection [2]. Type B aortic dissection (TBAD) has a 30-day mortality rate of 10%–20%. When patients with ascending aortic dissection underwent surgery instead of medical care, mortality was dramatically reduced; however, this effect was not observed in patients with descending aortic dissection. For the past 50 years, treatment has been guided by the Stanford classification, which is based on this finding. As a result, type B dissections that are considered complicated, such as those with aortic rupture, neurologic sequelae, hypotension or shock, end-organ malperfusion, recurrent or refractory pain, early aortic dilation, hypertension resistant to medical treatment, or propagation of the dissection, have been saved for surgical intervention [3, 4].
Thoracic endovascular aortic repair (TEVAR) has been a successful alternative to surgery for acute complex TBAD since it was first emerged by DeBakey et al. [5] and Daily et al. [6] in the late 1960s and has a lower perioperative mortality rate. TEVAR's overall effectiveness of TEVAR in treating patients with acute, uncomplicated TBAD is still under discussion. Medical or conservative treatment is used for individuals with uncomplicated TBAD. This involves the management of hypertension and close monitoring [7]. The long-term outcomes of the best medical treatment (BMT) in patients with uncomplicated TBAD, however, tend to be less than desirable, with a recorded false-lumen expansion of 20% to 50% after 4 years and cumulative mortality of 30% to 50% at 5 years [8–10].
In terms of hospital mortality, TEVAR has shown high efficacy in reducing mortality rates, as reported by several studies [11–13]. In contrast, other studies found no significant difference between TEVAR and medical management (MM) in terms of mortality rate [14–16]. Therefore, we aimed to compare MM and TEVAR in the management of TBAD and to resolve these conflicting results.
Methods
Data sources and search strategy
A systematic search of Cochrane Library, PubMed, Scopus and Web of Science up to February 2023 was conducted for appropriate studies using the following search strategy “("Thoracic Endovascular Aortic Repair" OR "Endovascular Stent Grafting" OR "Fenestrated Endovascular Aneurysm Repair" OR "Branched Endovascular Aneurysm Repair" OR "Thoracic Endovascular Aneurysm Repair") AND ("Aortic Dissection" OR "Dissecting Aortic Aneurysm"). We included only articles published in English.
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed in this meta-analysis.
Study selection
Pre-defined PICOS criteria were followed to select relevant studies (P: acute or chronic type B aortic dissection patients; I: thoracic endovascular aortic repair; C: medical therapy; O: in-hospital mortality and adverse event outcomes). Studies were included in the meta-analysis if they were randomized control trials and prospective or retrospective cohorts that compared thoracic endovascular aortic repair (TEVAR) versus medical therapy for the treatment of acute or chronic type B aortic dissection. Case reports, case series and animal studies were excluded. Awe followed these criteria to perform title and abstract screening of the publications to assess their eligibility for inclusion. Studies that passed this initial screening were then evaluated in full text screening. Each stage involved a duplicate review of the publications, with any disagreements resolved through consensus or by a third reviewer.
Data extraction and assessment of study quality
Data extraction of the baseline characteristics and outcomes were done using a standardized method. Baseline characteristics that were extracted included study year, country, sample size, number of patients in each group, sex, age, length of hospital or ICU stay, extent of dissection at admission, baseline diseases, and baseline medications. Two authors performed title and abstract screening and two authors performed full-text screening. Five authors extracted the Data and another author examined data accuracy. We used The Newcastle Ottawa scale tool to assess quality of the observational studies.
Statistical analysis
Statistical analysis was performed using RevMan software (version 5.4). For continuous outcomes, such as length of hospital stay, the mean difference (MD) and the associated 95% confidence interval (CI) were used. For dichotomous outcomes, such as mortality, the risk ratio (RR) and its corresponding 95% CIs were used. The overall effect of the meta-analysis was estimated using a Z-test. If no heterogeneity was detected, a fixed effects model was used to present the results. If significant heterogeneity was present, a random effects model was applied. Heterogeneity was estimated using the chi-squared test.
Results
Literature search
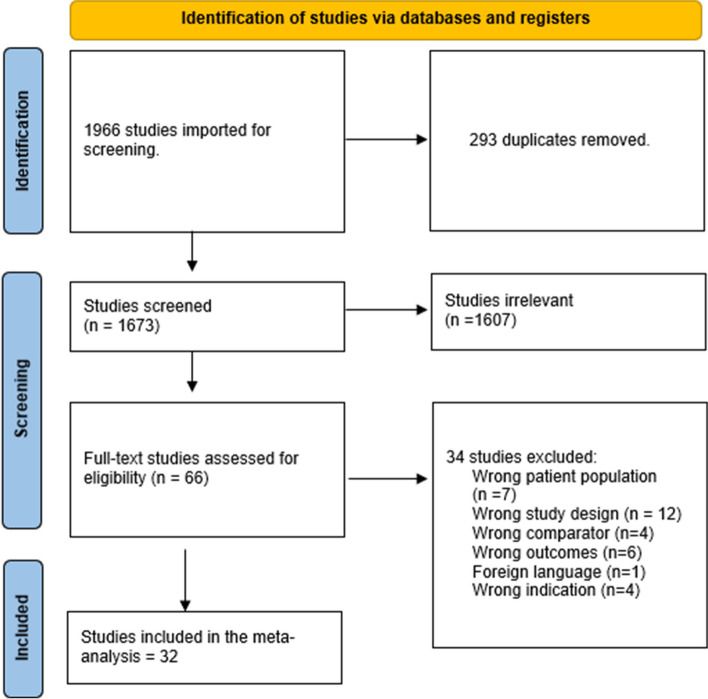
After conducting an extensive literature search, 1,966 studies were identified. Following the removal of duplicates, 1,673 studies were deemed eligible for title and abstract screening. Of these, 1,607 were found to be irrelevant, leaving 66 studies that were suitable for full-text screening. Ultimately, 32 studies [11, 17–47] were included in the meta-analysis after review of the full-text, (Fig. 1).
Fig. 1.
PRISMA flow diagram
The overall quality of the included studies was found good in 23 studies, fair in one study, and poor in seven studies (Table 1).
The total number of included participants in the study was 150,836, 19,512 patients in TEVAR group, and 131,324 patients in medical treatment group, Table 2 shows other baseline data.
Outcomes
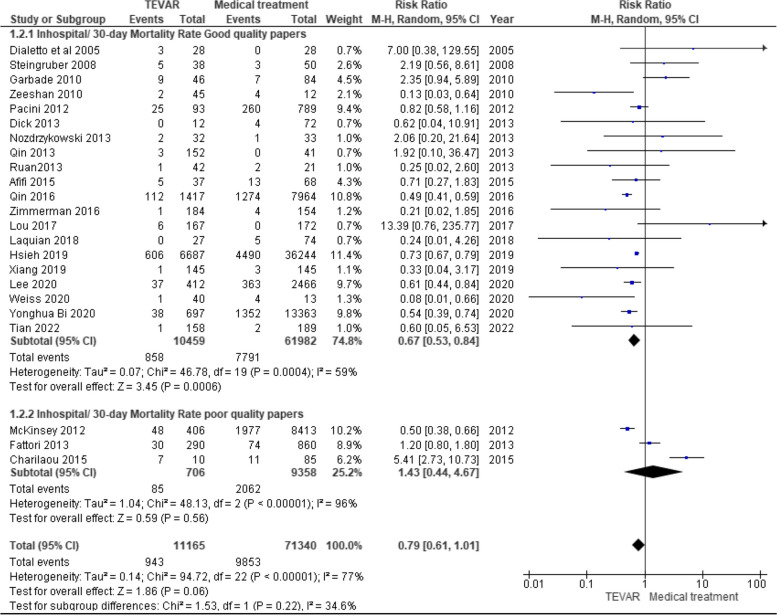
In hospital / 30-day Mortality Rate analysis
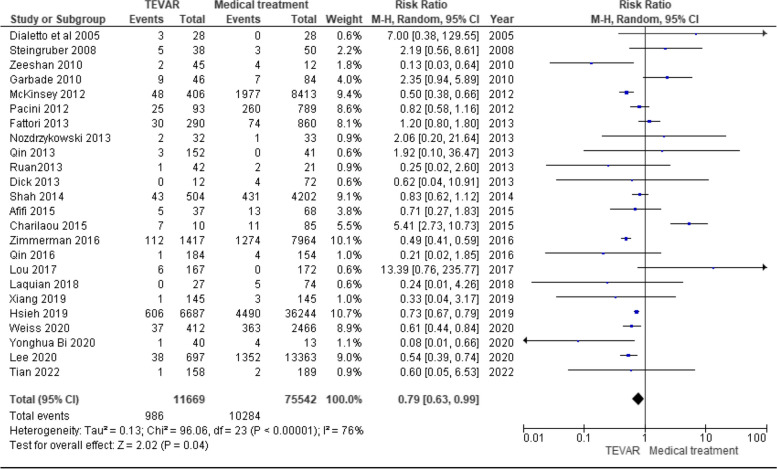
The overall effect estimate showed a statistically significant association between the TEVAR group and decreased hospital/ 30-day mortality rate compared with the medical treatment group (RR = 0.79, CI = 0.63, 0.99, P = 0.04). Significant heterogeneity was found among studies that wasn't resolved by the leave-one-out test (P < 0.00001, I2 = 76%), as shown in Fig. 2.
Fig. 2.
In hospital / 30-day Mortality Rate
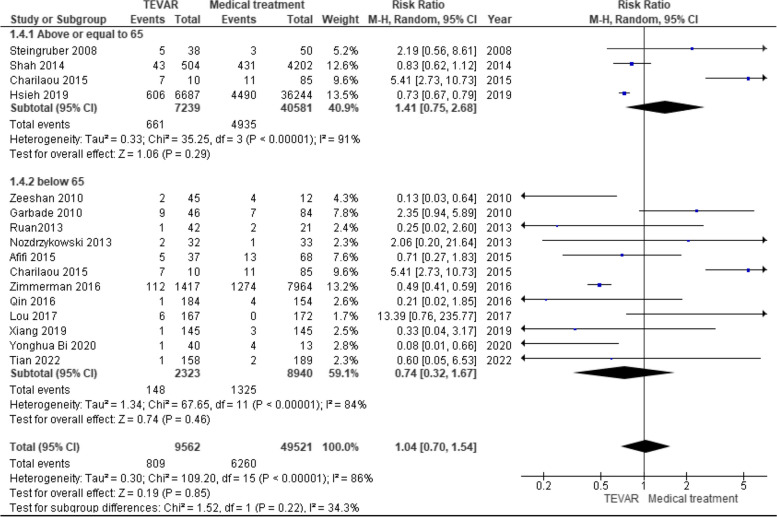
In hospital / 30-day Mortality Rate age subgroup analysis
More than or equal to 65 years old
The overall effect estimate showed no statistically significant difference between TEVAR and Medical treatment group in patients more than or equal to 65 years old (RR = 1.41, CI 0.75, 2.68, P = 0.29). Significant heterogeneity was found among the studies (P < 0.00001, I2 = 91%), Fig. 3. So, leave one out test was done by removing the study (Charilaou 2015) and the heterogeneity was solved (P = 0.21, I2 = 35%) and the overall effect estimate showed a statistically significant association between TEVAR group and decreased in hospital/ 30-day mortality rate in patients more than or equal to 65 years old (RR = 0.78, CI = 0.64, 0.95, P = 0.01).
Fig. 3.
In hospital / 30-day Mortality subgroup analysis according to age
Less than 65 years old
The overall effect estimate showed no statistically significant difference between the TEVAR and Medical treatment group in patients aged < 65 years (RR = 0.74, CI 0.32, 1.67, P = 0.46). Significant heterogeneity was found among studies that was not not resolved by the leave-one-out test (P < 0.00001, I2 = 84%), Fig. 3.
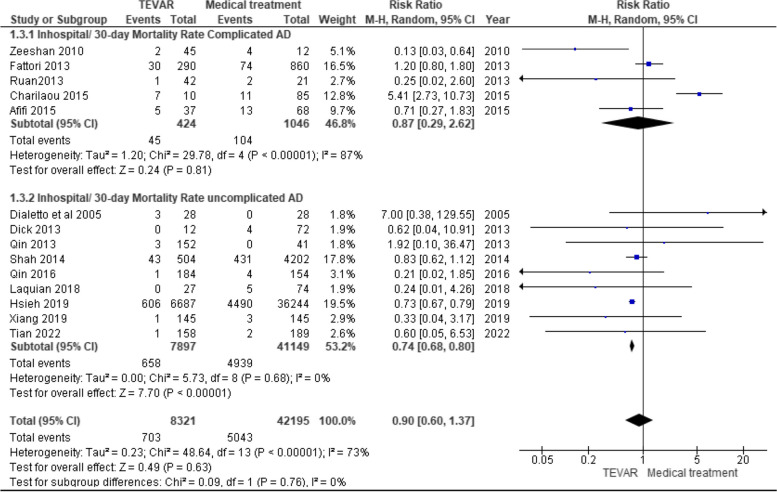
In hospital / 30-day Mortality Rate age subgroup analysis
Complicated AD
The overall effect estimate showed no statistically significant difference between the TEVAR and Medical treatment group in complicated AD patients (RR = 0.87, CI 0.29, 2.62, P = 0.81). Significant heterogeneity was found among studies that wasn't resolved by the leave-one-out test (P < 0.00001, I2 = 87%), as shown in Fig. 4.
Fig. 4.
In hospital / 30-day Mortality subgroup analysis according to complicated or uncomplicated AD
Uncomplicated AD
The overall effect estimate showed a statistically significant association between the TEVAR group and decreased hospital/ 30-day mortality rate in uncomplicated AD patients compared to the medical treatment group (RR = 0.74, CI = 0.68, 0.80, P < 0.00001). No significant heterogeneity was found among the studies (P = 0.68, I2 = 0%), as shown in Fig. 4.
In hospital / 30-day Mortality Rate study quality subgroup analysis
Good quality
The overall effect estimate showed a statistically significant association between the TEVAR group and decreased hospital/ 30-day mortality rate compared to the medical treatment group in good-quality studies (RR = 0.67, CI 0.53, 0.84, P = 0.0006). Significant heterogeneity was found among the studies (P = 0.0004, I2 = 59%), Fig. 5. We performed leave-one-out test by removing the study (Qin 2016) and the heterogeneity was solved (P = 0.02, I2 = 45%), and the overall effect estimate showed a statistically significant association between AD type B patients who were treated with TEVAR and decreased hospital/ 30-day mortality rate in good quality studies (RR = 0.71, CI = 0.55, 0.91, P = 0.006).
Fig. 5.
In hospital / 30-day Mortality subgroup analysis according to quality
Poor quality
The overall effect estimate showed no statistically significant difference between the TEVAR group and medical treatment group in poor quality studies (RR = 1.43, CI 0.44, 4.67, P = 0.56). Significant heterogeneity was found among studies that wasn't resolved by the leave-one-out test (P < 0.00001, I2 = 96%), Fig. 5.
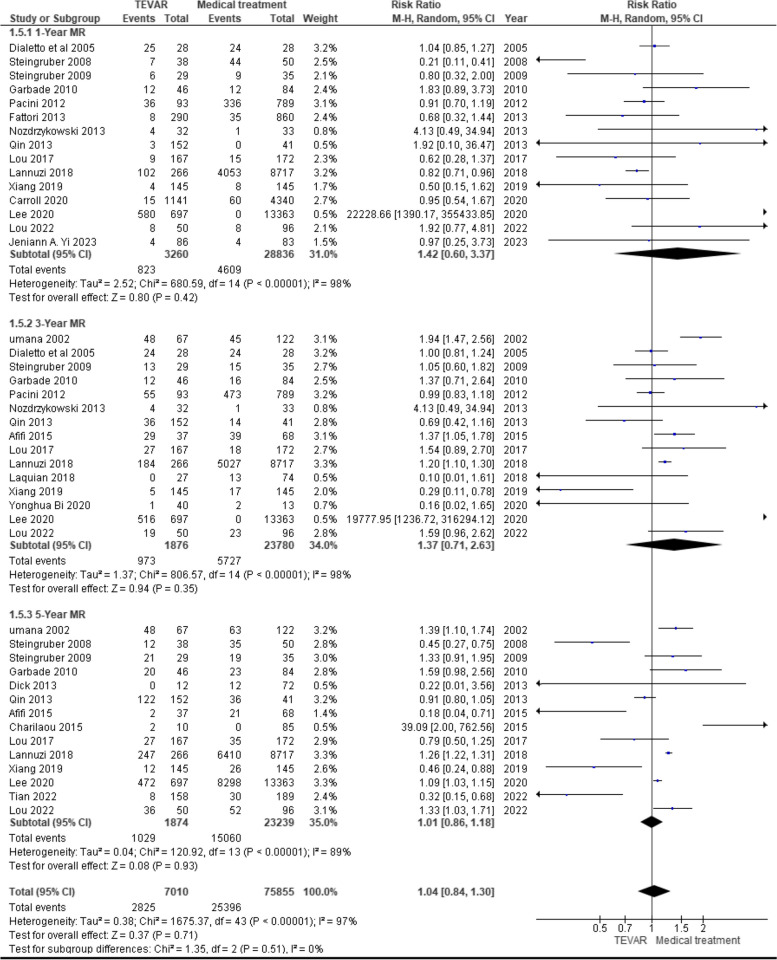
Late mortality rate (MR) analysis
1 year mortality rate (MR)
The overall effect estimate showed no statistically significant difference between the TEVAR group and medical treatment group (RR = 1.42, CI = 0.60, 3.37, P = 0.42). Significant heterogeneity was found among studies that was not resolved by the leave-one-out test (P < 0.00001, I2 = 98%), Fig. 6.
Fig. 6.
Late mortality rate analysis
3 year mortality rate (MR)
The overall effect estimate showed no statistically significant difference between the TEVAR group and medical treatment group (RR = 1.37, CI = 0.71, 2.63, P = 0.35). Significant heterogeneity was found among studies that was not resolved by the leave-one-out test (P < 0.00001, I2 = 98%), Fig. 6.
5 year mortality rate (MR)
The overall effect estimate showed no statistically significant difference between the TEVAR group and medical treatment group (RR = 1.01, CI = 0.86, 1.18, P = 0.93). Significant heterogeneity was found among studies that was not resolved by the leave-one-out test (P < 0.00001, I2 = 89%), Fig. 6.
Length of hospital stay analysis
The overall effect estimate showed a statistically significant association between the TEVAR group and an increased length of hospital stay compared to the medical treatment group (RR = 3.42, CI = 1.69, 5.13, P = 0.0001). Significant heterogeneity was found among studies that was not resolved by the leave-one-out test (P < 0.00001, I2 = 96%), Fig. 7.
Fig. 7.
Length of hospital stay analysis
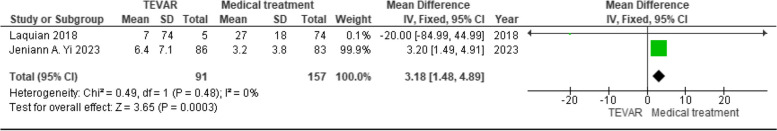
Length of ICU stay analysis
The overall effect estimate showed a statistically significant association between the TEVAR group and an increased length of ICU stay compared to the medical treatment group (RR = 3.18, CI = 1.48, 4.89, P = 0.0003). No significant heterogeneity was found between the two studies (P = 0.48, I2 = 0%), Fig. 8.
Fig. 8.
Length of ICU stay analysis
Development of Retrograde A dissection analysis
The overall effect estimate showed no statistically significant difference between the TEVAR group and medical treatment group (RR = 0.87, CI = 0.68, 1.11, P = 0.27). No significant heterogeneity was found between the two studies (P = 0.08, I2 = 37%), as shown in Fig. 9.
Fig. 9.
Retrograde type A dissection analysis
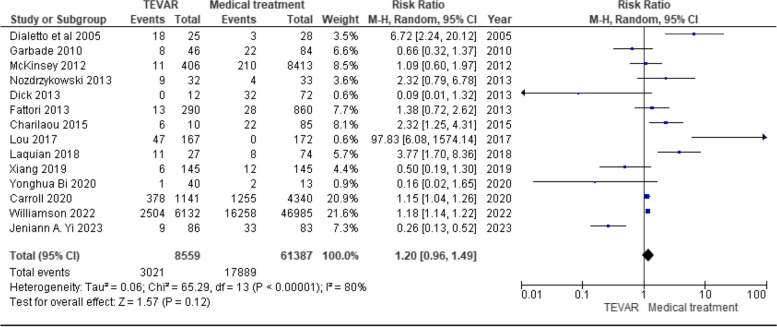
Reintervention / dissection related admission analysis
The overall effect estimate showed no statistically significant difference between the TEVAR group and medical treatment group (RR = 1.20, CI = 0.96, 1.49, P = 0.12). Significant heterogeneity was found among studies that was not resolved by the leave-one-out test (P < 0.00001, I2 = 80%), Fig. 10.
Fig. 10.
Reintervension / dissection related admission analysis
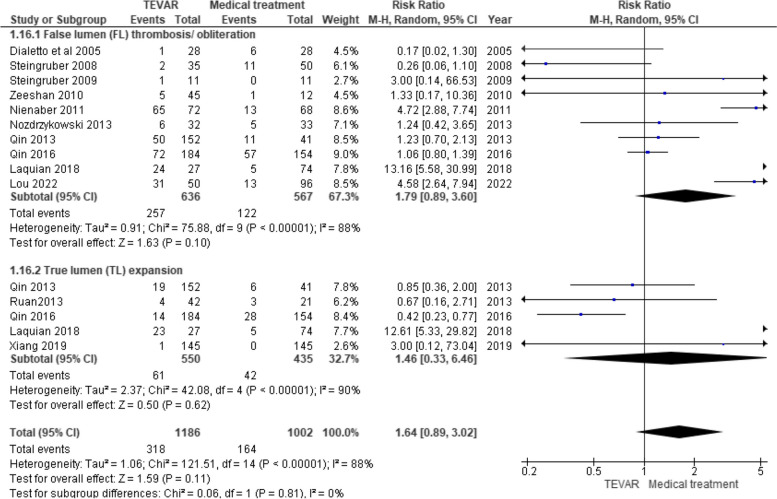
Aortic remodeling analysis
False lumen (FL) obliteration / thrombosis analysis
The overall effect estimate showed no statistically significant difference between the TEVAR group and medical treatment group (RR = 1.79, CI = 0.89, 3.60, P = 0.10). Significant heterogeneity was found among studies that was not resolved by the leave-one-out test (P < 0.00001, I2 = 88%), Fig. 11.
Fig. 11.
Aortic remodeling analysis
True lumen (TL) expansion analysis
The overall effect estimate showed no statistically significant difference between the TEVAR group and medical treatment group (RR = 1.46, CI = 0.33, 6.46, P = 0.62). Significant heterogeneity was found (P < 0.00001, I2 = 90%), Fig. 11. Therefore, we performed a leave-one-out test by removing the study (Laquian 2018) and the heterogeneity was resolved (P = 0.40, I2 = 0%), and the overall effect estimate showed a statistically significant association between the TEVAR group and decreased true lumen expansion (RR = 0.56, CI = 0.36, 0.89, P = 0.01).
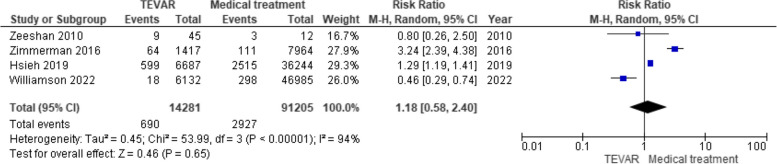
Respiratory failure analysis
The overall effect estimate showed no statistically significant difference between the TEVAR group and medical treatment group (RR = 1.18, CI = 0.58, 2.40, P = 0.65). Significant heterogeneity was found among studies that was not resolved by the leave-one-out test (P < 0.00001, I2 = 94%), Fig. 12.
Fig. 12.
Respiratory failure analysis
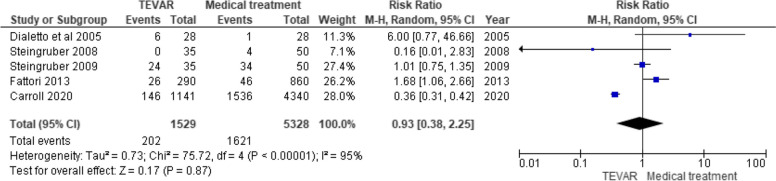
Extension or dilatation of dissection / new dissection analysis
The overall effect estimate showed no statistically significant difference between the TEVAR group and medical treatment group (RR = 0.93, CI = 0.38, 2.25, P = 0.87). Significant heterogeneity was found among studies that was not resolved by the leave-one-out test (P < 0.00001, I2 = 95%), Fig. 13.
Fig. 13.
Extension or dilatation of dissection / new dissection
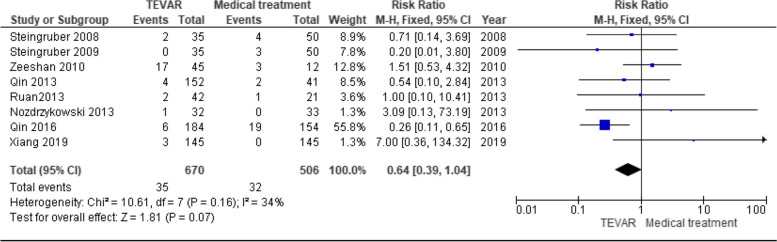
Aortic rupture analysis
The overall effect estimate showed no statistically significant difference between the TEVAR group and medical treatment group (RR = 0.64, CI = 0.39, 1.04, P = 0.07). No significant heterogeneity was found between the two studies (P = 0.16, I2 = 34%), Fig. 14.
Fig. 14.
Aortic rupture
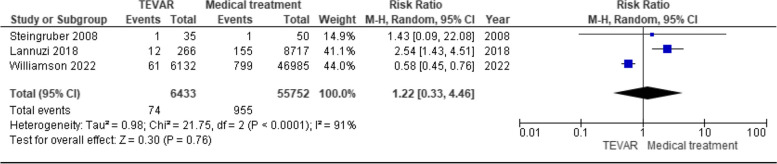
Sepsis
The overall effect estimate showed no statistically significant difference between the TEVAR group and medical treatment group (RR = 1.22, CI = 0.33, 4.46, P = 0.76). Significant heterogeneity among the studies was found (P < 0.0001, I2 = 91%), Fig. 15. Therefore, we performed leave-one-out test by removing the study (Williamson 2022) and the heterogeneity was resolved (P = 0.69, I2 = 0%), and the overall effect estimate showed a statistically significant association between TEVAR and increased incidence of sepsis (RR = 2.48, CI = 1.41, 4.35, P = 0.002).
Fig. 15.
Sepsis analysis
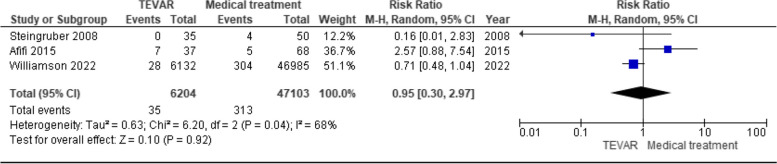
Chest pain
The overall effect estimate showed no statistically significant difference between the TEVAR group and medical treatment group (RR = 0.95, CI = 0.30, 2.97, P = 0.92). Significant heterogeneity was found among the studies (P = 0.04, I2 = 68%), Fig. 16. Therefore, we performed leave -one- out test by removing the study (Afifi 2015) and the heterogeneity was resolved (P = 0.31, I2 = 2%), and the overall effect estimate showed no statistically significant difference between the TEVAR group and the medical treatment group (RR = 0.68, CI = 0.42, 1.10, P = 0.11).
Fig. 16.
Chest pain analysis
Discussion
Our meta-analysis compared TEVAR and medical treatment in TBAD treatment and revealed a significant association between the TEVAR group and decreased in-hospital or 30-day mortality rate compared with the medical treatment group. Further subgroup analysis of in-hospital or 30-day mortality rates was performed according to age, which was divided into two subgroups: (more than or equal to 65 years old) and (less than 65 years old). Complications were divided into two subgroups: (complicated) and (uncomplicated). Study quality was divided into two subgroups: (good quality) and (poor quality). In age subgroups, there was a significant association between TEVAR group and decreased in-hospital or 30-day mortality rate in patients more than or equal to 65 years old; however, there was no significant difference between TEVAR and Medical treatment group in patients less than 65 years old. Similarly, in the complication subgroups, there was no significant difference between the TEVAR and Medical treatment groups in patients with complicated TBAD; however, there was a significant association between the TEVAR group and decreased in-hospital or 30-day mortality rate in patients with uncomplicated TBAD compared with the medical treatment group. Similarly, in the study quality subgroups, there was a significant association between the TEVAR group and decreased in-hospital or 30-day mortality rates in good-quality studies; however, there was no significant difference between TEVAR and Medical treatment groups in poor-quality studies. In contrast, we found no significant difference between the TEVAR and Medical treatment groups in the late mortality rate at 1,3, and 5 years. In addition, the TEVAR group was associated with an increased length of hospital stay and ICU stay compared with the medical treatment group. However, no significant difference was observed between the TEVAR and Medical treatment groups in other complications, such as acute renal failure, paralysis or spinal cord ischemia, myocardial infarction, development of Retrograde A dissection, respiratory failure, extension or dilatation of dissection or new dissection, aortic rupture, sepsis, and chest pain. Further analysis of true lumen (TL) expansion was performed, and a significant association between the TEVAR group and decreased true lumen expansion compared with the medical treatment group was found; however, no difference in FL obliteration or thrombosis was found between the TEVAR and medical treatment groups in False lumen (FL) obliteration or thrombosis. We found no difference between the two groups in terms of reintervention or dissection-related admission rates.
Historically, medical treatment rather than surgical techniques have been used to treat TBADs [9, 10]. The benefits of TEVAR include stabilizing the dissected aorta, causing aortic remodeling processes, and encouraging false lumen thrombosis [48]. A thrombosed false lumen is associated with better survival and fewer late adverse TBAD events [49]. The efficacy of TEVAR in dissected aortic remodeling in the acute phase can be explained by the advantageous mechanical characteristics of the dissection flap (pliable and dynamic). Aortic endograft coverage of the primary intimal tear stops antegrade FL flow, which depressurizes the FL. FL thromboses, contracts, and in a considerable portion of patients is eliminated as a result, allowing the true lumen (TL) to enlarge. [14] According to the hypothesis of Lou et al. [14], enhanced FL thrombosis or obliteration will result in a reduced need for distal aortic re-intervention, reduced FL aneurysm formation, and improved long-term survival. Therefore, preemptive TEVAR has additionally been carried out in patients with acute, uncomplicated TBAD in an effort to lower late mortality [15, 49–51]. TEVAR's overall effectiveness of TEVAR in treating patients with acute, uncomplicated TBAD is still under discussion. Medical or conservative treatment is used for individuals with uncomplicated TBAD. However, the long-term outcomes tend to be less than desirable. Additionally, it frequently requires many antihypertensive drugs to achieve blood pressure and heart rate targets in outpatients, and this treatment is ineffective in younger and obese patients [52]. Sustainable medical management is further complicated by lack of access to care, particularly for low-income families. Our meta-analysis found that TEVAR was associated with better results and reduced mortality in uncomplicated TBAD; however, no difference was found between TEVAR and medical treatment in managing complicated TBAD.
Our results are also consistent with those of Qin et al. [15], who reported that TEVAR was linked to a reduction in aortic-related adverse events and a lower mortality compared to BMT for uncomplicated type B aortic dissection. The early mortality rates were 0.5% with TEVAR and 2.6% with BMT. The early adverse event rates in their study were 10.3% in the TEVAR group and 4.5% in the BMT group, but the difference was not statistically significant. Although TEVAR was associated with more frequent early events, it was not a major complication of MM. Aortic rupture (32.2%) and aortic enlargement (47.5%) were the main causes of late adverse events in the MM group. In line with earlier studies [53], in patients with uncomplicated TBAD treated with only medical therapy, aortic enlargement was associated with aortic rupture and was therefore a significant late adverse event. Fattori et al. [49] reported similar in-hospital mortality rates for TEVAR and MM in patients with complicated TBAD. Additionally, a similar one-year mortality was observed in both groups. According to the 5-year Kaplan–Meier estimates, aortic growth or new aneurysm was the most frequent adverse event during follow-up, occurring in 73.3% of patients receiving medicinal therapy and in 62.7% of patients receiving TEVAR. However, Kaplan–Meier survival estimates reported that patients who underwent TEVAR had a decreased death rate at 5 years.
Zeeshan et al. [13] found an association between TEVAR and lower in-hospital or 30-day mortality than MM in managing complicated TBAD. The TEVAR group demonstrated markedly improved survival at 1, 3, and 5 years. Patients who underwent TEVAR had a 79% 5-year survival rate. This is in line with recent research published by Khoynezhad et al. [54], which showed a 78% 5-year survival rate and is consistent with a larger series that accessed the International Registry of Acute Aortic Dissection (IRAD) database [55, 56].
The potential benefit of TEVAR in aortic remodeling accounts for the lower mortality and higher survival rates. In the majority of patients who underwent TEVAR, the false lumen in the thoracic aorta at the endograft level was completely thrombosed and obliterated. In spite of complete remodeling in the proximal thoracic aorta, the majority of patients continue to have a patent false lumen in the distal thoracic and abdominal aortas. Interestingly, the Investigation of STEnt grafts in Aortic Dissection (INSTEAD) trial also showed positive aortic remodeling with TEVAR, similar to Zeeshan findings, despite being a study assessing the efficacy of TEVAR in uncomplicated type B aortic dissection [57]. However, in most cases, medical treatment alone did not cause any false lumen shrinkage or thrombus formation. When compared to individuals treated with conventional treatment, larger trials using IRAD have shown that patients treated with TEVAR have a lower 5-year mortality rate [49]. According to Lee et al. [11], the TEVAR and MM groups had in-hospital mortality rates of 5.45% and 10.12%, respectively, and 30-day mortality rates of 8.18% and 12.51%, respectively. The TEVAR group had a 1-year survival rate of 83.2%. The acute phase for patients with type TBAD undergoing surgical treatment has a significant risk of morbidity and mortality due to catastrophic situations such as aortic rupture or impending rupture. Older age was the most significant predictor of in-hospital mortality across all treatment groups, including the entire population. Naturally, age can affect a patient’s general health or underlying disorders, which can affect treatment. Other risk factors associated with in-hospital mortality include female sex, hypertension, and chronic kidney disease. According to Lou et al. [17], there was no significant difference in mortality rates between the TEVAR and MM groups, with both groups showing a 0% in-hospital mortality rate. The mean age of the MM group (58.6 years) was slightly higher than that of the TEVAR group (54.4 years); however, this difference was not significant (p = 0.055). The MM group also had a significantly higher proportion of males compared to the TEVAR group (p = 0.005). However, there were no statistically significant differences between the groups in terms of comorbidities, such as hypertension, diabetes, end-stage renal disease, history of stroke, and chronic obstructive pulmonary disease. The TEVAR group did, however, show a trend towards improved survival at 1 and 3 years, but there was no difference in overall survival [14] TEVAR group had a 91% five-year survival, but with MM, it was 82% [14]. Additionally, Complete false lumen (FL) thrombosis was observed in 72.1% of patients with TEVAR and 20.0% with MM, which provided superior aortic remodeling to MM in TBAD, resulting in increased long-term survival [17]. Likewise, Xiang et al. [58] reported that 30-day mortality, stroke, acute renal failure, and retrograde type A dissection rates between the TEVAR and BMT groups were not significantly different, but the early adverse event rates were significantly higher in the TEVAR group than in the BMT group. Although TEVAR was associated with higher complications in the early stage, patients in the TEVAR group had lower late aortic and lower risk of late death than those with MM in uncomplicated acute TBAD.
Future implications
Our study revealed a significant association between the TEVAR group and decreased mortality rate compared to the medical treatment group, mainly in patients aged 65 years and older and patients with uncomplicated TBAD. Randomized controlled trials are warranted to confirm our results and further assess the efficacy of TEVAR for complicated and non-complicated TBAD.
Strengths and limitations
The overall quality of most of the studies included in our analysis was good. The large sample size is an additional strength, as 150,836 patients were included in our study. Additionally, a high number of studies [32] were included in our analysis. Patients categorized under MM in the original primary studies were included because they lacked procedure codes indicating treatment with TEVAR. This suggests a potential bias owing to the likelihood that these patients may have died before receiving any form of treatment. The main limitation was that all of the included studies were observational rather than randomized controlled trials. Therefore, randomized controlled trials are needed to confirm our results and further evaluate the role of TEVAR in TBAD.
Conclusion
Our study revealed a significant association between the TEVAR group and decreased mortality rate compared with the medical treatment group, mainly in patients aged 65 years and older and patients with uncomplicated TBAD. Randomized controlled trials are warranted to confirm our results and further assess the efficacy of TEVAR in complicated and non-complicated TBAD in terms of the incidence of mortality.
Supplementary Information
Acknowledgements
None
Authors’ contributions
Idea validation: Karam R. Motawea. -Supervision: Karam R. Motawea, Samah S. Rouzan, Rowan H. Elhalag. -Concept: Karam R. Motawea, Mohammed Najdat Seijari, Amr Farwati, Amine Rakab. -Design: Karam R. Motawea, Mohammed Najdat Seijari, Amr Farwati, Amine Rakab. -Search strategy: Karam R. Motawea, Samah S. Rouzan, Rowan H. Elhalag. -Screening: Abdelrhamam M. Abdelwahab, Hussam Al Hennawi, Salem Elshenawy. -Data Extraction: Mai Saad Mohamed, Pensée Chébl, Mohamed Salem Madian, Mostafa Elsayed Elsayed Hewalla, Abdelrhamam M. Abdelwahab. -Quality assessment: Abdelrhamam M. Abdelwahab, Salem Elshenawy, Sarya Swed, Wael Hafez. -Data Analysis: Rowan H. Elhalag, Bisher Sawaf, Samer Kaspo, Naim Battikh. -Manuscript writing: Karam R. Motawea, Samah S. Rouzan, Rowan H. Elhalag, Mai Saad Mohamed, Pensée Chébl, Mohamed Salem Madian, Mostafa Elsayed Elsayed Hewalla, Sarya Swed, Wael Hafez. -Final Revision: Karam R. Motawea, Bisher Sawaf, Samer Kaspo, Naim Battikh.
Funding
None.
Availability of data materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
Not Applicable.
Consent for publication
Not Applicable.
Competing of interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tang JH, Lo ZJ, Wong J, Hong Q, Yong E, Chandrasekar S, et al. Effect of thoracic endovascular aortic repair on aortic remodeling in patients with type B aortic dissection in an Asian population. Ann Vasc Surg. 2020;69:352–9. 10.1016/j.avsg.2020.05.058 [DOI] [PubMed] [Google Scholar]
- 2.de Grubb MCM, Kilbourne B, Kilbourne K, Langston M, Gittner L, Zoorob RJ, et al. Socioeconomic, environmental, and geographic factors and US lung cancer mortality, 1999‐2009. Family Medicine and Community Health. 2017;5(1):3–12.
- 3.Nauta FJ, Trimarchi S, Kamman AV, Moll FL, Van Herwaarden JA, Patel HJ, et al. Update in the management of type B aortic dissection. Vasc Med. 2016;21(3):251–63. 10.1177/1358863X16642318 [DOI] [PubMed] [Google Scholar]
- 4.Williamson AJ, Sankary S, Kuchta KM, Gaines S, Morcos O, Lind B, Pocivavsek L, Dua A, Lee CJ. Contemporary Unplanned Readmission Trends Following Management of Type B Aortic Dissection. Vasc Specialist Int. 2022;38:16. 10.5758/vsi.220007. [DOI] [PMC free article] [PubMed]
- 5.De Bakey ME, Henly WS, Cooley DA, Morris GC Jr, CrawfordBeall ES AC Jr, et al. Surgical management of dissecting aneurysms of the aorta. J Thorac Cardiovasc Surg. 1965;49(1):130–49. 10.1016/S0022-5223(19)33323-9 [DOI] [PubMed] [Google Scholar]
- 6.Daily PO. Management of acute aortic dissections. Ann Thorac Surg. 1970;10:237–47. 10.1016/S0003-4975(10)65594-4 [DOI] [PubMed] [Google Scholar]
- 7.Estrera AL, Miller CC, Goodrick J, Porat EE, Achouh PE, Dhareshwar J, et al. Update on outcomes of acute type B aortic dissection. Ann Thorac Surg. 2007;83(2):S842–5. 10.1016/j.athoracsur.2006.10.081 [DOI] [PubMed] [Google Scholar]
- 8.Akin I, Kische S, Ince H, Nienaber C, Surgery E. Indication, timing and results of endovascular treatment of type B dissection. Eur J Vasc Endovasc Surg. 2009;37(3):289–96. 10.1016/j.ejvs.2008.12.004 [DOI] [PubMed] [Google Scholar]
- 9.Trimarchi S, Tolenaar J, Tsai T, Froehlich J, Pegorer M, Upchurch G, et al. Influence of clinical presentation on the outcome of acute B aortic dissection: evidences from IRAD. J Cardiovasc Surg (Torino). 2012;53(2):161–8. [PubMed] [Google Scholar]
- 10.Tsai TT, Trimarchi S, Nienaber C. Acute aortic dissection: perspectives from the International Registry of Acute Aortic Dissection (IRAD). Eur J Vasc Endovasc Surg. 2009;37(2):149–59. 10.1016/j.ejvs.2008.11.032 [DOI] [PubMed] [Google Scholar]
- 11.Lee JH, Cho Y, Cho YH, Kang H, Lim TH, Jang HJ, et al. Incidence and mortality rates of thoracic aortic dissection in Korea-inferred from the nationwide health insurance claims. J Korean Med Sci. 2020;35(40):e360. 10.3346/jkms.2020.35.e360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weiss S, Rojas RL, Habermann EB, Moriarty JP, Borah BJ, DeMartino RR. Impact of patient factors and procedure on readmission after aortic dissection admission in the states of Florida and New York. J Vasc Surg. 2020;72(4):1277–87. 10.1016/j.jvs.2020.01.046 [DOI] [PubMed] [Google Scholar]
- 13.Zeeshan A, Woo EY, Bavaria JE, Fairman RM, Desai ND, Pochettino A, et al. Thoracic endovascular aortic repair for acute complicated type B aortic dissection: superiority relative to conventional open surgical and medical therapy. Elsevier; 2010. p. S109-S15. [DOI] [PubMed]
- 14.Lou X, Chen EP, Duwayri YM, Jordan WD, Keeling WB, Leshnower BG. Early results of thoracic endovascular aortic repair for the management of acute uncomplicated type B aortic dissection. Semin Thorac Cardiovasc Surg. 2023 Summer;35(2):289–97. 10.1053/j.semtcvs.2021.12.014. [DOI] [PubMed]
- 15.Qin Y-L, Wang F, Li T-X, Ding W, Deng G, Xie B, et al. Endovascular repair compared with medical management of patients with uncomplicated type B acute aortic dissection. J Am Coll Cardiol. 2016;67(24):2835–42. 10.1016/j.jacc.2016.03.578 [DOI] [PubMed] [Google Scholar]
- 16.Shah TR, Rockman CB, Adelman MA, Maldonado TS, Veith FJ, Mussa FF. Nationwide comparative impact of thoracic endovascular aortic repair of acute uncomplicated type B Aortic Dissections. Vasc Endovascular Surg. 2014;48(3):230–3. 10.1177/1538574413518122 [DOI] [PubMed] [Google Scholar]
- 17.Afifi RO, Sandhu HK, Leake SS, Boutrous ML, Kumar V 3rd, Azizzadeh A, et al. Outcomes of patients with acute Type B (DeBakey III) Aortic Dissection: A 13-Year. Single-Center Exper Circulation. 2015;132(8):748–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bi Y, Yi M, Han X, Ren J. Clinical outcomes and quality of life in patients with acute and subacute type B aortic dissection after thoracic endovascular aortic repair. J Int Med Res. 2020;48(8):300060520945506. 10.1177/0300060520945506. [DOI] [PMC free article] [PubMed]
- 19.Carroll BJ, Schermerhorn M, Kennedy KF, Swerdlow N, Soriano KM, Yeh RW, et al. Readmissions after acute type B aortic dissection. J Vasc Surg. 2020;72(1):73–83e2. [DOI] [PubMed]
- 20.Charilaou P, Ziganshin BA, Peterss S, Rajbanshi BG, Rajakaruna C, Zaza KJ, et al. Current Experience With Acute Type B Aortic Dissection: Validity of the Complication-Specific Approach in the Present Era. Ann Thorac Surg. 2016;101(3):936–43. 10.1016/j.athoracsur.2015.08.074 [DOI] [PubMed] [Google Scholar]
- 21.Chemelli-Steingruber I, Chemelli A, Strasak A, Hugl B, Hiemetzberger R, Jaschke W, et al. Endovascular repair or medical treatment of acute type B aortic dissection? A comparison. Eur J Radiol. 2010;73(1):175–80. 10.1016/j.ejrad.2008.09.031 [DOI] [PubMed] [Google Scholar]
- 22.Chemelli-Steingruber IE, Chemelli A, Strasak A, Hugl B, Hiemetzberger R, Czermak BV. Evaluation of volumetric measurements in patients with acute type B aortic dissection–thoracic endovascular aortic repair (TEVAR) vs conservative. J Vasc Surg. 2009;49(1):20–8. 10.1016/j.jvs.2008.08.062 [DOI] [PubMed] [Google Scholar]
- 23.Dialetto G, Covino FE, Scognamiglio G, Manduca S, Della Corte A, Giannolo B, et al. Treatment of type B aortic dissection: endoluminal repair or conventional medical therapy? Eur J Cardiothorac Surg. 2005;27(5):826–30. 10.1016/j.ejcts.2005.02.002 [DOI] [PubMed] [Google Scholar]
- 24.Dick F, Hirzel C, Immer FF, Hinder D, Dai-Do D, Carrel T, et al. Quality of life after acute type B dissection in the era of thoracic endovascular aortic repair. Vasa. 2010;39(3):219–28. 10.1024/0301-1526/a000033 [DOI] [PubMed] [Google Scholar]
- 25.Fattori R, Montgomery D, Lovato L, Kische S, Di Eusanio M, Ince H, et al. Survival after endovascular therapy in patients with type B aortic dissection: a report from the International Registry of Acute Aortic Dissection (IRAD). JACC Cardiovasc Interv. 2013;6(8):876–82. 10.1016/j.jcin.2013.05.003 [DOI] [PubMed] [Google Scholar]
- 26.Garbade J, Jenniches M, Borger MA, Barten MJ, Scheinert D, Gutberlet M, et al. Outcome of patients suffering from acute type B aortic dissection: a retrospective single-centre analysis of 135 consecutive patients. Eur J Cardiothorac Surg. 2010;38(3):285–92. 10.1016/j.ejcts.2010.02.038 [DOI] [PubMed] [Google Scholar]
- 27.Hsieh RW, Hsu TC, Lee M, Hsu WT, Chen ST, Huang AH, et al. Comparison of type B dissection by open, endovascular, and medical treatments. J Vasc Surg. 2019;70(6):1792–800 e3. [DOI] [PubMed]
- 28.Iannuzzi JC, Stapleton SM, Bababekov YJ, Chang D, Lancaster RT, Conrad MF, et al. Favorable impact of thoracic endovascular aortic repair on survival of patients with acute uncomplicated type B aortic dissection. J Vasc Surg. 2018;68(6):1649–55. 10.1016/j.jvs.2018.04.034 [DOI] [PubMed] [Google Scholar]
- 29.Laquian L, Scali ST, Beaver TM, Kubilis P, Beck AW, Giles K, et al. Outcomes of thoracic endovascular aortic repair for acute type B dissection in patients with intractable pain or refractory hypertension. J Endovasc Ther. 2018;25(2):220–9. 10.1177/1526602818759339 [DOI] [PubMed] [Google Scholar]
- 30.Lou X, Chen EP, Duwayri YM, Jordan WD, Keeling WB, Leshnower BG. Early results of thoracic endovascular aortic repair for the management of acute uncomplicated type B aortic dissection. Semin Thorac Cardiovasc Surg. 2023;35(2):289–97. [DOI] [PubMed]
- 31.Lou X, Chen EP, Duwayri YM, Veeraswamy RK, Jordan WD Jr, Zehner CA, et al. The impact of thoracic endovascular aortic repair on long-term survival in type B aortic dissection. Ann Thorac Surg. 2018;105(1):31–8. 10.1016/j.athoracsur.2017.06.016 [DOI] [PubMed] [Google Scholar]
- 32.McKinsey JF, Kim I-K, Sosunov E, Moskowitz A, Egorova NJJoVS. Thoracic aortic dissection and thoracoabdominal acute type B aortic dissections have superior survival when treated with thoracic endovascular aneurysm repair and open surgery compared to medical therapy: outcomes from the National Medicare Database. J Vasc Surg. 2012;56(3):886.
- 33.Nienaber CA. Influence and critique of the INSTEAD Trial (TEVAR versus medical treatment for uncomplicated type B aortic dissection). Semin Vasc Surg. 2011;24(3):167–71. 10.1053/j.semvascsurg.2011.10.003 [DOI] [PubMed] [Google Scholar]
- 34.Nozdrzykowski M, Etz CD, Luehr M, Garbade J, Misfeld M, Borger MA, et al. Optimal treatment for patients with chronic Stanford type B aortic dissection: endovascularly, surgically or both? Eur J Cardiothorac Surg. 2013;44(3):e165–74; discussion e74. [DOI] [PubMed]
- 35.Pacini D, Di Marco L, Fortuna D, Belotti LM, Gabbieri D, Zussa C, et al. Acute aortic dissection: epidemiology and outcomes. Int J Cardiol. 2013;167(6):2806–12. 10.1016/j.ijcard.2012.07.008 [DOI] [PubMed] [Google Scholar]
- 36.Qin YL, Deng G, Li TX, Wang W, Teng GJ. Treatment of acute type-B aortic dissection: thoracic endovascular aortic repair or medical management alone? JACC Cardiovasc Interv. 2013;6(2):185–91. 10.1016/j.jcin.2012.11.004 [DOI] [PubMed] [Google Scholar]
- 37.Qin YL, Wang F, Li TX, Ding W, Deng G, Xie B, et al. Endovascular repair compared with medical management of patients with uncomplicated type B acute aortic dissection. J Am Coll Cardiol. 2016;67(24):2835–42. 10.1016/j.jacc.2016.03.578 [DOI] [PubMed] [Google Scholar]
- 38.Ruan ZB, Zhu L, Chen GC, Yin YG. Early and long-term effect of thoracic endovascular aortic repair for Stanford B aortic dissection. Thorac Cardiovasc Surg. 2015;63(2):120–5. [DOI] [PubMed] [Google Scholar]
- 39.Shah TR, Rockman CB, Adelman MA, Maldonado TS, Veith FJ, Mussa FF. Nationwide comparative impact of thoracic endovascular aortic repair of acute uncomplicated type B aortic dissections. Vasc Endovascular Surg. 2014;48(3):230–3. 10.1177/1538574413518122 [DOI] [PubMed] [Google Scholar]
- 40.Tian C, Shu C, Luo M, Fang K, Zhang Y. Survival and aortic remodeling outcomes in patients with type B aortic intramural hematoma in the endovascular era: An observational cohort study. J Vasc Surg. 2022;76(1):70–8. 10.1016/j.jvs.2022.01.143 [DOI] [PubMed] [Google Scholar]
- 41.Umaña JP, Miller DC, Mitchell RS. What is the best treatment for patients with acute type B aortic dissections—medical, surgical, or endovascular stent-grafting? Ann Thorac Surg. 2002;74(5):S1840–3. 10.1016/S0003-4975(02)04140-1 [DOI] [PubMed] [Google Scholar]
- 42.Weiss S, Rojas RL, Habermann EB, Moriarty JP, Borah BJ, DeMartino RR. Impact of patient factors and procedure on readmission after aortic dissection admission in the states of Florida and New York. J Vasc Surg. 2020;72(4):1277–87. 10.1016/j.jvs.2020.01.046 [DOI] [PubMed] [Google Scholar]
- 43.Williamson AJ, Sankary S, Kuchta KM, Gaines S, Morcos O, Lind B, et al. Contemporary unplanned readmission trends following management of Type B aortic dissection. Vasc Specialist Int. 2022;38:16. 10.5758/vsi.220007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xiang D, Kan X, Liang H, Xiong B, Liang B, Wang L, et al. Comparison of mid-term outcomes of endovascular repair and medical management in patients with acute uncomplicated type B aortic dissection. J Thorac Cardiovasc Surg. 2021;162(1):26–36 e1. [DOI] [PubMed]
- 45.Yi JA, Gupta R, Tat Q, Potter HA, Han SM, Fleischman F, et al. Readmission after early thoracic endovascular aortic repair versus medical management of acute type B aortic dissection. J Vasc Surg. 2023;77(5):1387–93. 10.1016/j.jvs.2022.12.064 [DOI] [PubMed] [Google Scholar]
- 46.Zeeshan A, Woo EY, Bavaria JE, Fairman RM, Desai ND, Pochettino A, et al. Thoracic endovascular aortic repair for acute complicated type B aortic dissection: superiority relative to conventional open surgical and medical therapy. J Thorac Cardiovasc Surg. 2010;140(6 Suppl):S109-15 (discussion S42-S46). 10.1016/j.jtcvs.2010.06.024 [DOI] [PubMed] [Google Scholar]
- 47.Zimmerman KP, Oderich G, Pochettino A, Hanson KT, Habermann EB, Bower TC, et al. Improving mortality trends for hospitalization of aortic dissection in the National Inpatient Sample. J Vasc Surg. 2016;64(3):606-15 e1. 10.1016/j.jvs.2016.03.427 [DOI] [PubMed] [Google Scholar]
- 48.Erbel R, Aboyans V, Boileau C, Bossone E, Di Bartolomeo R, Eggebrecht H, et al. 2014 ESC guidelines on the diagnosis and treatment of aortic diseases. Kardiol Pol. 2014;72(12):1169–252. 10.5603/KP.2014.0225 [DOI] [PubMed] [Google Scholar]
- 49.Fattori R, Montgomery D, Lovato L, Kische S, DiEusanio M, Ince H, et al. Survival after endovascular therapy in patients with type B aortic dissection: a report from the International Registry of Acute Aortic Dissection (IRAD). JACC Cardiovasc Interv. 2013;6(8):876–82. 10.1016/j.jcin.2013.05.003 [DOI] [PubMed] [Google Scholar]
- 50.Nienaber CA, Rousseau H, Eggebrecht H, Kische S, Fattori R, Rehders TC, et al. Randomized comparison of strategies for type B aortic dissection: the INvestigation of STEnt Grafts in Aortic Dissection (INSTEAD) trial. Circulation. 2009;120(25):2519–28. 10.1161/CIRCULATIONAHA.109.886408 [DOI] [PubMed] [Google Scholar]
- 51.Qin Y-L, Deng G, Li T-X, Wang W, Teng G. Treatment of acute type-B aortic dissection: thoracic endovascular aortic repair or medical management alone? JACC Cardiovasc Interv. 2013;6(2):185–91. 10.1016/j.jcin.2012.11.004 [DOI] [PubMed] [Google Scholar]
- 52.Eggebrecht H, Schmermund A, Von Birgelen C, Naber C, Bartel T, Wenzel R, et al. Resistant hypertension in patients with chronic aortic dissection. J Hum Hypertens. 2005;19(3):227–31. 10.1038/sj.jhh.1001800 [DOI] [PubMed] [Google Scholar]
- 53.Hagan PG, Nienaber CA, Isselbacher EM, Bruckman D, Karavite DJ, Russman PL, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease JAMA. 2000;283(7):897–903. [DOI] [PubMed]
- 54.Khoynezhad A, Donayre CE, Omari BO, Kopchok GE, WalotI,WhiteRAJTJoT, et al. Midterm results of endovascular treatment of complicated acute type B aortic dissection. J Thorac Cardiovasc Surg. 2009;138(3):625–31. 10.1016/j.jtcvs.2009.04.044 [DOI] [PubMed] [Google Scholar]
- 55.Fattori R, Tsai TT, Myrmel T, Evangelista A, Cooper JV, Trimarchi S, et al. Complicated acute type B dissection: is surgery still the best option? A report from the International Registry of Acute Aortic Dissection. JACC Cardiovasc Interv. 2008;1(4):395–402. 10.1016/j.jcin.2008.04.009 [DOI] [PubMed] [Google Scholar]
- 56.Trimarchi S, Nienaber CA, Rampoldi V, Myrmel T, Suzuki T, Bossone E, et al. Role and results of surgery in acute type B aortic dissection: insights from the International Registry of Acute Aortic Dissection (IRAD). Circulation. 2006;114(1_supplement):I-357-I-64. [DOI] [PubMed]
- 57.Nienaber C, Rousseau H, Eggebrecht H. Randomized comparison of strategies for type B aortic dissection: the INvestigation of STEent Grafts in Aortic Dissection (INSTEAD) trial. Circulation. 2010;51(5):1321–2. [DOI] [PubMed]
- 58.Xiang D, Kan X, Liang H, Xiong B, Liang B, Wang L, et al. Comparison of mid-term outcomes of endovascular repair and medical management in patients with acute uncomplicated type B aortic dissection. J Thorac Cardiovasc Surg. 2021;162(1):26–36. e1. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.