Abstract
Assessing the acceptance of the monkeypox vaccine is crucial for the success of vaccination programs, yet the prevalence reports remain inconclusive. The aim of this study was to determine the global prevalence of monkeypox vaccine acceptance and identify its associated factors. A meta-analysis was conducted with a comprehensive search strategy on the following databases, including Scopus, Embase, and PubMed, for articles published up to April 5, 2024. This study utilizes a single-arm meta-analysis to calculate the pooled prevalence of monkeypox vaccine acceptance. A Z-test was employed to identify factors associated with the vaccine acceptance. Our study analyzed 51 articles encompassing 98,746 participants, revealing an overall monkeypox vaccine acceptance rate of 65%. Notably, the highest acceptance rates were observed among men who have sex with men (MSMs), while healthcare workers (HCWs) showed the lowest acceptance rates. Additionally, our findings indicated an increased acceptance in individuals with educational attainment beyond a bachelor’s degree, a history of COVID-19 and influenza vaccination, homosexual orientation, and HIV-positive status. Conversely, lower acceptance risk was associated with those with educational attainment below a bachelor’s degree, heterosexual orientation, and bisexual orientation. In conclusion, our current study has determined the rate of monkeypox vaccine acceptance and identified its associated factors. These findings offer valuable insights as the foundation for targeted policies to manage and increase acceptance rates.
Keywords: Monkeypox, vaccine, acceptance, predictors, prevalence
Introduction
Monkeypox vaccination has become a global priority since the potential monkeypox outbreak that was reported in 2022 [1]. Efforts have primarily focused on ensuring the safety and efficacy of available monkeypox vaccines, such as JYNNEOS®, ACAM2000, and the modified smallpox vaccine, as well as increasing vaccination coverage among high-risk populations [2]. Implementing vaccination programs is crucial for effectively managing and preventing monkeypox infections. This urgency is evidenced by the successful control of infections such as
polio, measles, mumps, and rubella through vaccination initiatives. Additionally, vaccination programs have been shown to improve global health outcomes and economic conditions [3,4]. However, the potential ineffectiveness of any vaccination initiatives needs to be evaluated. A study highlighted obstacles to successful vaccination programs, including rejection, high distribution cost, limited availability of healthcare services, and impractical scheduling for immunization appointments [5]. Among these factors, vaccine rejection is deemed one of the most significant [6]. Individuals who refuse vaccination often spread misinformation and potentially influencing others to do the same. Therefore, assessing vaccine acceptance is crucial for the successful delivery of vaccination programs worldwide [7].
Evaluating vaccine acceptance is important, particularly for novel vaccines or potential vaccine options [6,7]. This occurrence has been reported in instances of Ebola [8], malaria [9], and dengue [10]. Factors influencing vaccine acceptance are multifaceted, including insufficient knowledge about disease prevention and socioeconomic circumstances [11]. This situation poses a challenge for achieving comprehensive vaccine uptake. Furthermore, the governments, which function as the ultimate regulatory bodies of countries, appear to lack specialized interventions to proactively address vaccine acceptance in immunization initiatives. Notably, interim advice regarding vaccination against monkeypox emphasizes primary recommendations such as surveillance, contact tracing, information campaigns, robust pharmacovigilance, and exposure assessment [12]. However, there is a lack of information on how to assess monkeypox vaccination acceptance. The acceptance rate is crucial to evaluate, given that regardless of how well-designed a vaccination program may be, its effectiveness hinges on population acceptance of the vaccine. Several studies have attempted to assess the acceptance level of the monkeypox vaccine. Nevertheless, the findings have been inconclusive, demonstrating variability in acceptance rates [13-16]. Moreover, no study has assessed the cumulative factors contributing to monkeypox vaccine acceptance. Therefore, the aim of this meta-analysis was to estimate the global prevalence and potential influencing factors of monkeypox vaccination acceptance. The findings of this study could serve as a reference for formulating regulations regarding monkeypox vaccination.
Methods
Study design
Between March and April 2024, a comprehensive meta-analysis on monkeypox vaccine acceptance was conducted, including articles from Scopus, Embase, and PubMed. Relevant data were extracted from each article to determine a cumulative effect estimate employing a meticulous approach. Adherence to the guidelines outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist ensured rigor and consistency in the protocol [17]. The PRISMA checklist for this study is available in Supplementary Table 1. The study was registered with the International Prospective Register of Systematic Reviews (PROSPERO) database under the identification number CRD42024534065.
Eligibility criteria
Before the study inclusion in our analysis, potential articles underwent assessment for eligibility criteria. Inclusion criteria comprised epidemiological studies focusing on the prevalence and associated factors related to monkeypox vaccine acceptance with complete data for calculating cumulative prevalence and effect estimates. Meanwhile, exclusion criteria are the irrelevant articles based on their title and abstract, duplications, or those falling into categories such as reviews, commentaries, or editorials. Additionally, articles were excluded if they exhibited poor quality, as determined by the assessment conducted using the Newcastle-Ottawa Scale (NOS).
Quality assessment
The assessment of article quality in this study employed the NOS method. This assessment evaluates three aspects: sample selection, comparability, and results. Scores on the NOS assessment range from 0 to 9 points, where scores of 1–3 indicate poor-quality articles, 4–6 indicate articles of moderate quality, and 7–9 indicate articles of high quality [18]. The assessment process was conducted by three different authors (OR, LNH, and KC), and in cases of divergent assessments, discussions with a senior author (JKF) were held to reach a consensus. The outcomes of the NOS assessment in this study are presented in Supplementary Table 2.
Search strategy
The search strategy utilized three databases: PubMed, Embase, and Scopus for articles published up to April 5, 2024. English-written articles were included, and the search keywords comprised variations of “vaccine” OR “vaccination” OR “immunization” AND “monkeypox” OR “MPOX” AND “acceptance” OR “willingness to vaccinate” OR “intention to vaccinate” OR “hesitancy” OR “rejection”. These keywords were adapted to the medical subject heading (MeSH). Supplementary articles were sought by reviewing the citation lists of related articles. The article search and screening process was conducted by six independent authors, ensuring comprehensive coverage and thoroughness.
Data extraction
Information retrieval from each article included several key data points: first author’s name, year of publication, study location, study design, sample size, mean age, male-to-female ratio, study duration, survey methodology, population source, NOS assessment, the prevalence of monkeypox vaccine acceptance, and factors associated with the vaccine acceptance. The data extraction process was done by four different authors (AR, TDS, DA, and EF) to ensure accuracy and comprehensiveness. In cases of discrepancies or overlapping data, discussions were held with a senior researcher (JKF) to reconcile differences and ensure the integrity of the extracted information.
Covariates
The primary outcome of this study is the prevalence of monkeypox vaccine acceptance, defined as the willingness or intention of individuals to receive a monkeypox vaccine. Data regarding the prevalence of monkeypox vaccine acceptance were presented as numbers and percentages. Furthermore, subgroup analyses were conducted on various demographics, including the general population, medical students, healthcare workers (HCWs), and men who have sex with men (MSMs). These subgroup categories were determined following an exhaustive search for available data. Meanwhile, the predictor covariates encompassed a range of factors, including age, gender, marital status, level of education, occupational status, socioeconomic status, urbanicity, knowledge of monkeypox, sexual orientation, history of chronic disease, HIV positivity, history of sexually transmitted diseases (STDs), history of monkeypox, and history of vaccination, including coronavirus disease of 2019 (COVID-19) vaccination, influenza vaccination, and smallpox vaccination. The selection of predictor covariates was based on the data availability that was determined through a thorough search conducted by four authors (TDS, DA, EF, and DD). Discussions were performed with a senior researcher in discrepancies or overlapping data to ensure consistency and accuracy.
Statistical analysis
In presenting the data, the rate of acceptance of the monkeypox vaccine was depicted as n (%). Egger’s test and funnel plot analysis were employed to assess publication bias. A p-value above 0.05 and a symmetrical distribution in the funnel plot indicate the absence of publication bias. In cases where potential publication bias was identified, adjustment was made using the Trim-Fill method [19]. Heterogeneity was evaluated using I-squared and p-heterogeneity statistics. Heterogeneity was considered significant if the I-squared exceeded 50% or the p-heterogeneity was less than 0.10. Random-effects models were utilized for heterogeneous data, while fixed-effects models were applied in the absence of heterogeneity [20]. The cumulative prevalence of monkeypox vaccine acceptance was determined through single-arm meta-analysis with dichotomous data presented as event rates. Mantel–Haenszel tests were conducted for dichotomous variables, and inverse variance methods were used for continuous variables to assess the potential influence of predictor variables on monkeypox vaccine acceptance. A p-value less than 0.05 indicated a significant contribution. Effect estimates for continuous variables were presented as mean±SD, while odds ratios (OR) were used for dichotomous variables, outlined in a forest plot [21]. The analysis was performed using the R package (RStudio version 4.1.1, MA, US).
Results
Article selection
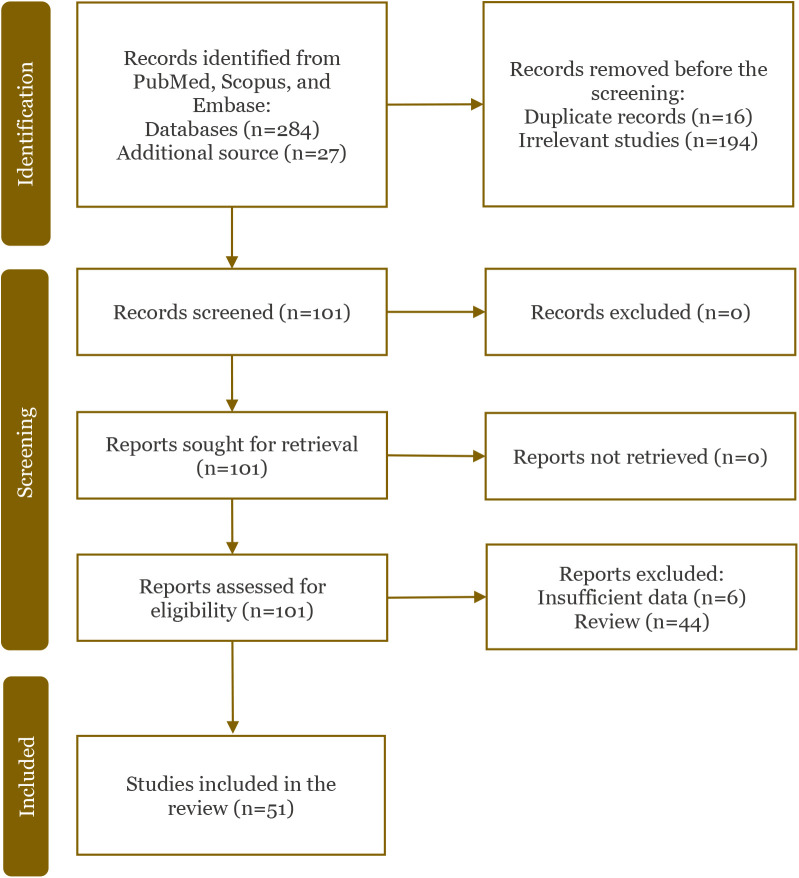
The initial article selection process yielded 284 articles from the Scopus, Embase, and PubMed databases, with an additional 27 articles identified from the citation lists of related articles. In the first exclusion phase, 16 articles were removed as repetitive, while 194 articles were excluded as they were deemed unrelated to the topic. Subsequently, 101 articles underwent full-text evaluation. In the second exclusion phase, 44 review articles and six articles with insufficient information were excluded. Ultimately, the final sample included in the study comprised 51 articles [22-72]. The article selection process in our study is illustrated in Figure 1. Baseline characteristics of the articles included in our analysis are presented in Table 1.
Figure 1.
A flowchart of article selection.
Table 1.
Baseline characteristics of included studies
| Author | Region | Sample size | Age (mean±SD or range) | Gender (male/female) % | Study period | Survey type | Population | NOS |
|---|---|---|---|---|---|---|---|---|
| Abd-Elhafeez et al. 2023 [22] | Mixed | 11919 | 21.7±2.2 | 45.6/54.4 | NA | Online | MS | 6 |
| Ahmed et al. (a) 2023 [23] | Iraq | 510 | 18–57 | 54.3/45.7 | Jul 22 | NA | GP | 7 |
| Ahmed et al. (b) 2023 [24] | Iraq | 637 | 21–51 | 49.9/50.1 | Nov 22-Jan 23 | Online | HCW | 7 |
| Alarif et al. 2023 [25] | Saudi Arabia | 743 | 25–56 | 49.1/50.9 | Sep-Nov 22 | Online | HCW | 7 |
| Andersen et al. 2024 [26] | US | 373 | 43–62 | 73.9/24.2 | Aug 22-Jan 23 | Online | GP | 6 |
| Araoz-Salinas et al. 2023 [27] | Peru | 373 | 31.0±9.0 | 85.0/6.2 | Nov 22-Jan 23 | Online and Offline | MSM | 7 |
| Bates et al. 2022 [28] | US | 182 | 26–75 | 57.4/35.0 | Sep 22 | Online | HCW | 6 |
| Caycho-Rodríguez et al. 2023 [29] | Peru | 472 | 28.1±9.7 | 39.4/60.6 | Dec 22 | Online | GP | 6 |
| Chen et al. 2023 [30] | China | 154 | 22.0±12.0 | 96.1/3.9 | Aug 22 | Online | GP | 6 |
| Crosato et al. 2024 [31] | Italy | 144 | 30–60 | 96.5/2.8 | Aug-Oct 22 | Offline | GP | 7 |
| Curtis et al. 2023 [32] | US | 317 | 29.9±4.8 | 81.3/14.7 | Dec-21 | Offline | GP | 6 |
| Dong et al. 2023 [33] | China | 512 | 30.0±26.4 | 50.7/49.3 | Sept-Oct 22 | Online | GP | 7 |
| Dukers-Muijrers et al. 2023 [34] | Netherland | 1856 | 42.0±31.0 | NA | Jul-22 | Online | MSM | 6 |
| Filardo et al. 2023 [35] | US | 273 | 35–57 | 27.0/71.0 | Oct-Nov 22 | Offline | GP | 7 |
| Fu et al. 2023 [36] | China | 577 | 32.0±28.0 | NA | Aug-Sept 22 | Online | MSM | 7 |
| Ghazy et al. 2023 [37] | Egypt | 605 | 30.0±6.8 | 60.8/39.2 | Nov-Dec 22 | Online | GP | 7 |
| Harapan et al. (a) 2020 [38] | Indonesia | 407 | NA | 31.4/68.6 | Jul 19 | Online | HCW | 7 |
| Harapan et al. (b) 2020 [39] | Indonesia | 407 | NA | 31.4/68.6 | Jul 19 | Online | HCW | 7 |
| Hong et al. 2023 [40] | China | 1032 | 27.9±7.9 | NA | Aug-Sept 22 | Online | MSM | 7 |
| Huang et al. 2024 [41] | China | 1093 | 18–25 | NA | Sept-Nov 22 | Online | MSM | 7 |
| Islam et al. 2023 [42] | Lebanon | 260 | 24.4±8.4 | 24.1/75.9 | Sep 22 | Online | GP | 7 |
| Jamaleddine et al. 2023 [43] | Lebanon | 493 | 36–54 | NA | Jul-Aug 22 | Online | GP | 7 |
| Jongen et al. 2024 [44] | Netherland | 492 | 18–68 | NA | Jun-Aug 22 | Online | MSM | 7 |
| Karapinar et al. 2023 [45] | Turkey | 707 | 22.5±3.5 | 45.7/54.3 | Oct 22 | Online | MSM | 7 |
| Kumar et al. 2022 [46] | Malaysia | 946 | NA | 32.8/67.2 | Jul-Aug 22 | Online | MS | 7 |
| Lin et al. 2022 [47] | Malaysia | 229 | 18–40 | 29.7/70.3 | Jun-Sept 2022 | Online | MS | 7 |
| Lounis et al. 2023 [48] | Algeria | 111 | 20–30 | 14.3/85.7 | Dec 22 | Online | HCW | 7 |
| Lounis et al. 2024 [49] | Algeria | 196 | 24.6±2.9 | NA | Sep 22 | Online | MS | 7 |
| Luo et al. 2024 [50] | China | 2493 | NA | 50.3/49.7 | Jan 23 | Online | MSM | 6 |
| Mahameed et al. 2023 [51] | Jordan | 485 | 18–66 | NA | Jul 22 | Online | GP | 7 |
| Paparini et al. 2023 [52] | Sweden | 1932 | 30–47 | NA | Jul-Aug 22 | Online | MSM | 7 |
| Peptan et al. 2022 [53] | Czech Republic | 1376 | 46.1±12.0 | 9.7/88.9 | Sep 22 | Online | GP | 6 |
| Ren et al. 2023 [54] | Czech Republic | 2293 | NA | 5.6/94.4 | Oct 22 | Online | HCW | 6 |
| Reyes-Urueña et al. 2022 [55] | Sweden | 32902 | 42.9±10.0 | 35.0/65.0 | May 22 | Online | MSM | 6 |
| Riad et al. 2022 [56] | Czech Republic | 341 | 18–59 | 41.3/58.7 | Aug-Sept 22 | Online | HCW | 7 |
| Riad et al. 2023 [57] | Czech Republic | 144 | 26–38 | 65.3/34.7 | Aug 22 | Online | HCW | 6 |
| Riccò et al. 2022 [58] | Italy | 163 | 37.0±7.0 | 34.5/40.4 | Jul-Aug 22 | Online | HCW | 7 |
| Sahin et al. 2022 [59] | Turkey | 283 | NA | 42.0/58.0 | May-Jun 22 | Online | HCW | 7 |
| Salim et al. 2022 [60] | Indonesia | 75 | 36.0±14.0 | NA | Jul 22 | Online | MS | 6 |
| Scarinci et al. 2023 [61] | Italy | 204 | NA | 28.6/71.4 | Apr-Aug 22 | Online | HCW | 7 |
| Temsah et al. 2022 [62] | Saudi Arabia | 1546 | 18–49 | NA | Aug 22 | Offline | GP | 6 |
| Torres et al. 2023 [63] | Brazil | 6236 | NA | NA | Jul 22 | Online | MSM | 6 |
| Tran et al. 2023 [64] | Vietnam | 842 | 18–50 | 37.4/62.2 | Aug-Sept 22 | Online | GP | 7 |
| Turpin et al. 2023 [65] | US | 24 | 18–55 | 48.0/51.0 | Jul 22 | Online | MSM | 6 |
| Wang et al. 2022 [66] | Netherland | 394 | 16–26 | 44.0/43.8 | Aug-Sept 23 | Online | MSM | 7 |
| Wang et al. 2023 [67] | China | 2135 | 18–36 | NA | Jul-Aug 23 | Online | GP | 7 |
| Winters et al. 2022 [68] | US | 856 | 25–40 | NA | Jul 22 | Online | GP | 6 |
| Yang et al. 2024 [69] | China | 7311 | 18–59 | NA | Jul 22 | Online | MS | 6 |
| Zheng et al. 2022 [70] | China | 3340 | NA | NA | May-Aug 22 | Online | MSM | 7 |
| Zheng et al. 2023 [71] | China | 7196 | NA | NA | Jul 22 | Online | MSM | 6 |
| Zucman et al. 2022 [72] | France | 155 | 34.3±8.2 | NA | Aug-Sept 22 | Online | MSM | 7 |
GP: general population; HCW: healthcare worker; MS: medical students; MSM: men who have sex with men; NA: not available; NOS: Newcastle–Ottawa scale; SD: standard deviation
The rate of acceptance for the monkeypox vaccine
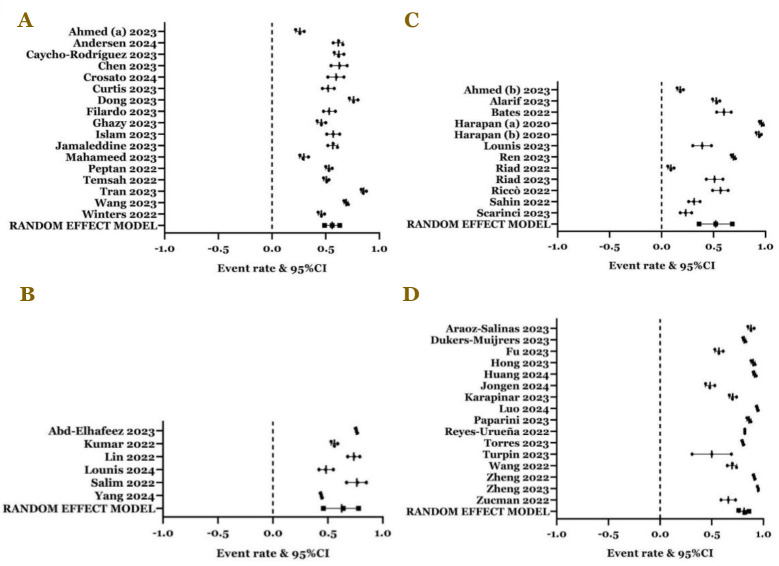
In our study, 65% of participants showed a willingness to accept monkeypox vaccination (event rate=0.65; 95%CI: 0.59, 0.71; p<0.0001; p-Egger: 0.0581; p-Heterogeneity<0.0001) (Figure 2). Subgroup analysis results based on demographic populations were as follows: in the general population, the prevalence of monkeypox vaccination acceptance was 56% (event rate=0.56; 95%CI: 0.49, 0.63; p=0.0890; p-Egger= 0.8556; p-Heterogeneity<0.0001) (Figure 3A). Among medical students, the prevalence of monkeypox vaccination acceptance was 64% (event rate=0.64; 95%CI: 0.46, 0.78; p=0.1360; p-Egger=0.9291; p-Heterogeneity<0.0001) (Figure 3B). Within the HCW population, the prevalence of monkeypox vaccination acceptance was 52% (event rate=0.52; 95%CI: 0.36, 0.68; p=0.7890; p-Egger=0.4068; p-Heterogeneity<0.0001) (Figure 3C). Among MSMs, the prevalence of monkeypox vaccination acceptance was notably high at 82% (event rate=0.82; 95%CI: 0.76, 0.86; p<0.0001; p-Egger=0.9294; p-Heterogeneity<0.0001) (Figure 3D).
Figure 2.
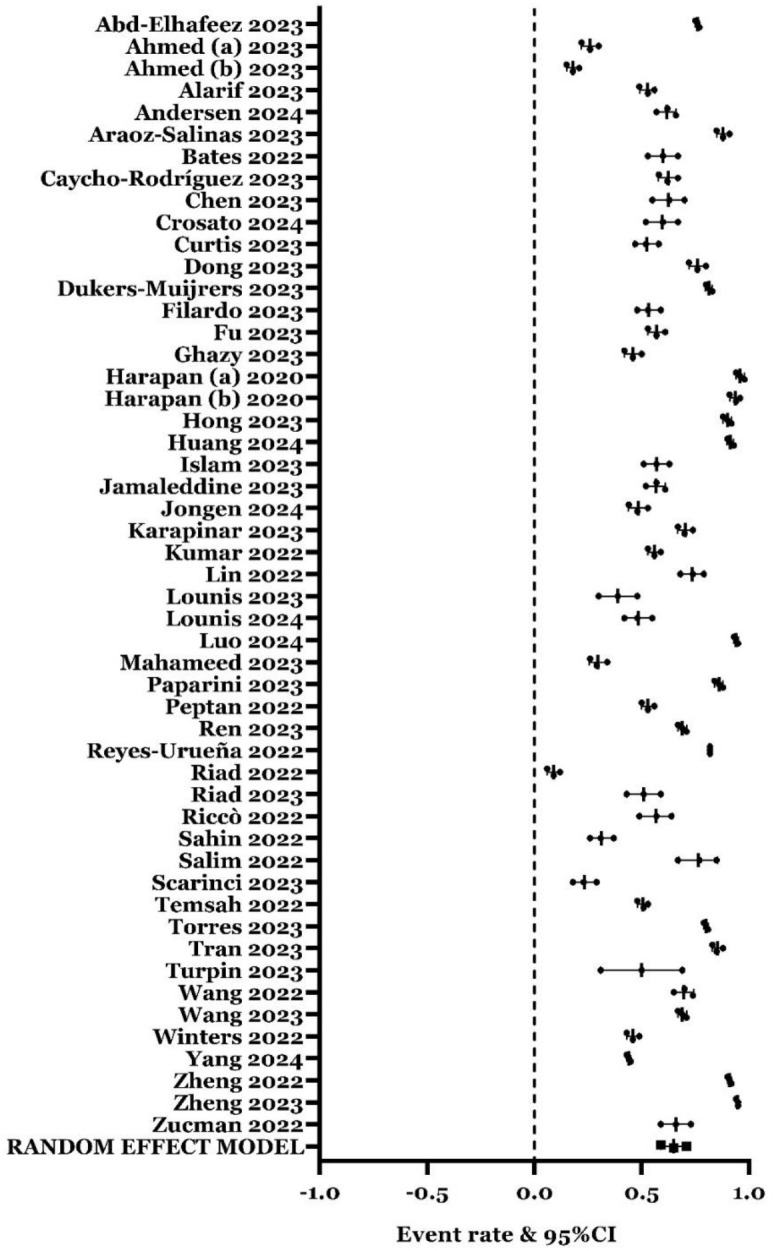
The prevalence of monkeypox vaccination acceptance in all populations (event rate: 0.65; 95%CI: 0.59–0.71; p<0.0001; p-Egger=0.0581; p-Heterogeneity<0.0001).
Figure 3.
The prevalence of monkeypox vaccination acceptance in (A) general population (event rate: 0.56; 95%CI: 0.49, 0.63; p=0.0890; p-Egger: 0.8556; p-Heterogeneity<0.0001); (B) medical students (event rate: 0.64; 95%CI: 0.46, 0.78; p=0.1360; p-Egger=0.9291; p- Heterogeneity<0.0001); (C) healthcare workers (event rate: 0.52; 95%CI: 0.36, 0.68; p=0.7890; p-Egger=0.4068; p-Heterogeneity<0.0001); and (D) men who have sex with men (event rate: 0.82; 95%CI: 0.76, 0.86; p<0.0001; p-Egger=0.9294; p-Heterogeneity<0.0001).
Determinants related to the acceptance of monkeypox vaccination
Among all the covariates analyzed, the result indicated that only educational attainment (Figure 4A), history of vaccination (Figure 4B and 4C), HIV positivity, and sexual orientation, including bisexual (Figure 5A), heterosexual (Figure 5B), and homosexual orientation (Figure 5C) contributed to the acceptance of monkeypox vaccination. Regarding educational attainment, individuals with a Bachelor of Science (BSc) degree or higher had a 1.36 times higher risk of accepting the monkeypox vaccine compared to those with educational attainment below BSc level (OR=1.36; 95%CI: 1.11, 1.66; p=0.0030; p-Egger=0.0687; p-Heterogeneity<0.0001). Furthermore, concerning the history of vaccination, our findings suggested that individuals with a history of COVID-19 (OR=2.48; 95%CI: 1.50, 4.07; p<0.0001; p-Egger=0.4259; p-Heterogeneity=0.0010) and influenza vaccination (OR=1.46; 95%CI: 1.09, 1.95; p=0.0120; p-Egger=0.2308; p-Heterogeneity=0.2660) had an elevated risk of accepting monkeypox vaccination. In terms of sexual orientation, homosexual individuals exhibited a higher likelihood of accepting monkeypox vaccination (OR=1.27; 95%CI: 1.10, 1.47; p=0.0010; p-Egger=0.6958; p-Heterogeneity=0.5670) than heterosexual group, while individuals identifying as bisexual (OR=0.84; 95%CI: 0.72, 0.99; p=0.0350; p-Egger=0.0110; p-Heterogeneity=0.5000) and heterosexual (OR=0.76; 95%CI: 0.59, 0.97; p=0.0260; p-Egger=0.7406; p-Heterogeneity=0.6830) exhibited the opposite effect compared to homosexuals. Additionally, this study indicated that individuals living with HIV had an increased risk of accepting monkeypox vaccination (OR=1.43; 95%CI: 1.16, 1.77; p=0.0010; p-Egger=0.3304; p-Heterogeneity=0.0750). The outcomes of the analysis concerning factors linked to the acceptance of monkeypox vaccination are depicted in Table 2.
Figure 4.
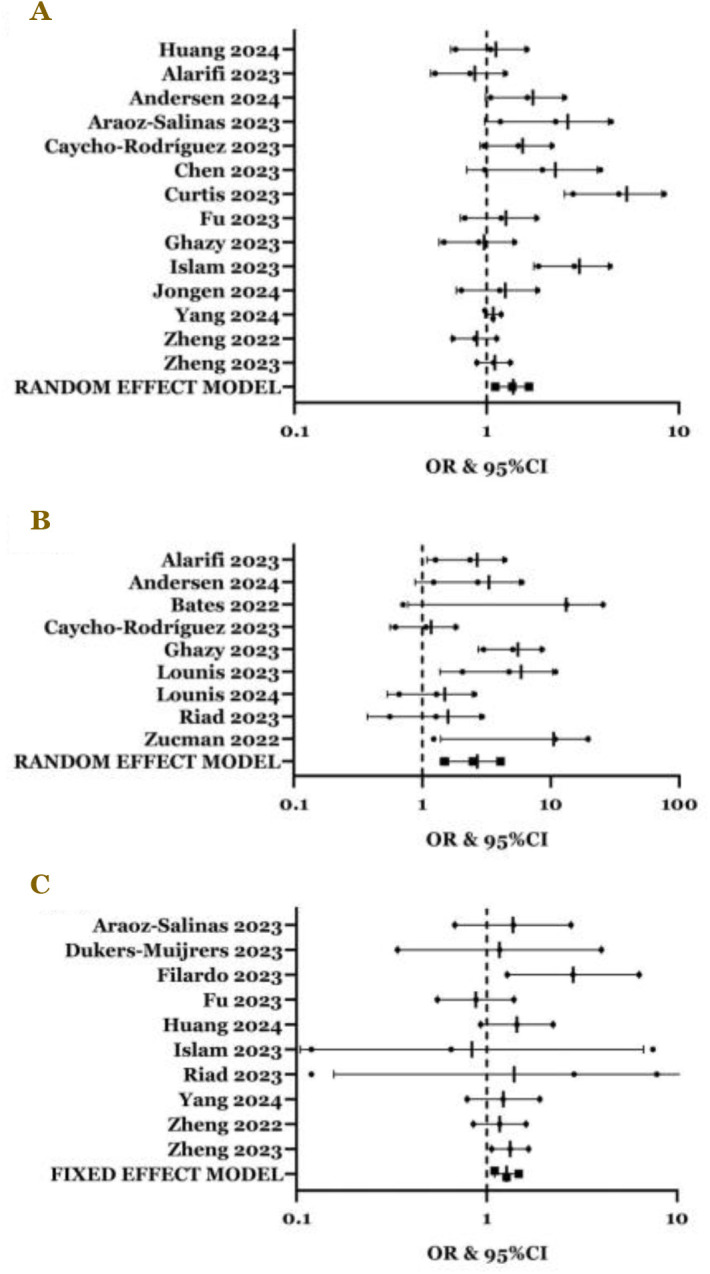
Individuals with (A) education levels of BSc or higher (OR=1.36; 95%CI: 1.11, 1.66; p=0.0030; p-Egger=0.0687; p-Heterogeneity<0.0001); (B) had a history of COVID-19 vaccination (OR=2.48; 95%CI: 1.50, 4.07; p<0.0001; p-Egger=0.4259; p-Heterogeneity=0.0010); and (C) had a history of influenza vaccination had a higher acceptance rate of monkeypox vaccination (OR=1.39; 95%CI: 1.10, 1.76; p=0.0060; p-Egger=0.2308; p-Heterogeneity=0.2660).
Figure 5.
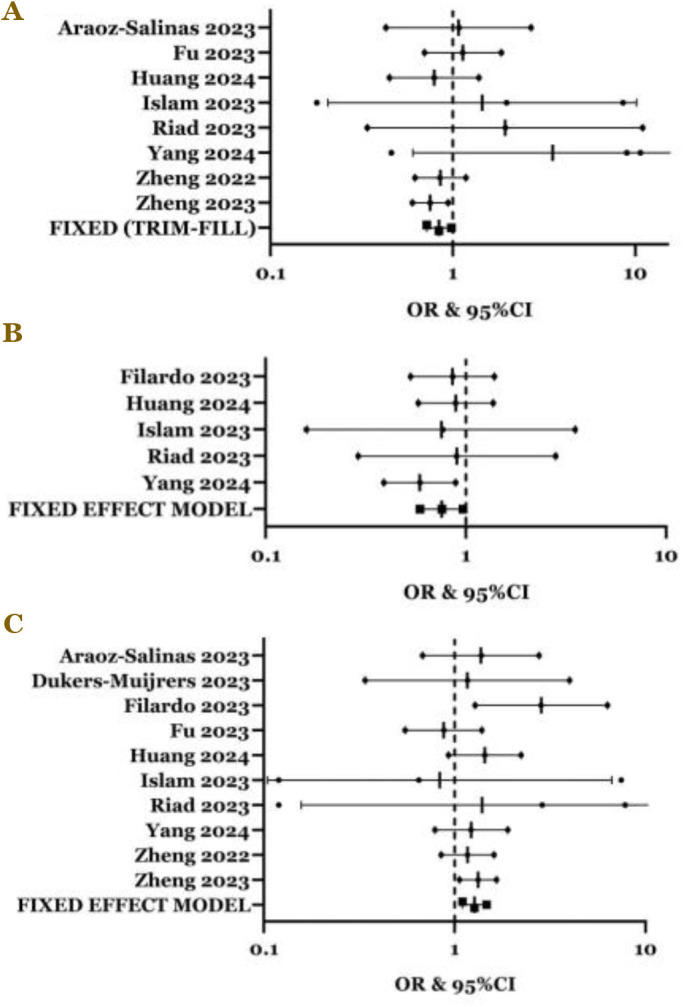
The acceptance of monkeypox vaccination among individuals with (A) bisexual orientation (OR=0.84; 95%CI: 0.72, 0.99; p=0.0350; p-Egger’s=0.0110; p-Heterogeneity=0.5000); (B) heterosexual (OR=0.76; 95%CI: 0.59, 0.97; p=0.0260; p-Egger=0.7406; p-Heterogeneity=0.6830), and (C) homosexual (OR=1.27; 95%CI: 1.10, 1.47; p=0.0010; p-Egger=0.6958; p-Heterogeneity=0.5670).
Table 2.
The potential factors associated with the acceptance of monkeypox vaccination
| Covariates | Acceptance/total (%) | Number of studies | Mean difference*/odds ratio | 95% confidence interval | p-Egger | p-Heterogeneity | p-value |
|---|---|---|---|---|---|---|---|
| Age (years), mean±SD | 36.90±9.64 | 10 | 0.52* | -1.24–2.28 | 0.0423 | <0.0001 | 0.5630 |
| Gender | |||||||
| Male | 4198/7991 (52.53) | 20 | 1.20 | 0.97–1.48 | 0.3674 | <0.0001 | 0.0910 |
| Female | 4208/8175 (51.47) | 20 | 0.84 | 0.68–1.03 | 0.3674 | <0.0001 | 0.0910 |
| Marital status | |||||||
| Married | 1366/2057 (66.41) | 8 | 0.82 | 0.62–1.09 | 0.6400 | 0.0010 | 0.1700 |
| Single | 6945/8222 (84.47) | 8 | 1.22 | 0.92–1.61 | 0.6400 | 0.0010 | 0.1700 |
| Educational attainment | |||||||
| <BSc | 6803/9436 (72.10) | 14 | 0.74 | 0.60–0.90 | 0.0687 | <0.0001 | 0.0030 |
| ≥BSc | 9136/13212 (69.15) | 14 | 1.36 | 1.11–1.66 | 0.0687 | <0.0001 | 0.0030 |
| Employment | |||||||
| Not working | 563/932 (60.41) | 7 | 0.84 | 0.27–2.66 | 0.1432 | <0.0001 | 0.7690 |
| Working | 5010/6450 (77.67) | 7 | 1.19 | 0.38–3.75 | 0.1432 | <0.0001 | 0.7690 |
| Socioeconomic status | |||||||
| Low income | 2195/3142 (69.86) | 7 | 1.03 | 0.72–1.48 | 0.2537 | <0.0001 | 0.8570 |
| Middle income | 1624/2168 (74.91) | 7 | 0.88 | 0.77–1.01 | 0.7162 | 0.1180 | 0.0740 |
| High income | 958/1273 (75.26) | 7 | 1.04 | 0.62 – 1.74 | 0.4024 | <0.0001 | 0.8910 |
| Urbanicity | |||||||
| Urban | 6780/11294 (60.03) | 10 | 1.21 | 0.91–1.61 | 0.4015 | <0.0001 | 0.1980 |
| Rural | 1592/3242 (49.11) | 10 | 0.83 | 0.62–1.10 | 0.4015 | <0.0001 | 0.1980 |
| Good knowledge of monkeypox | 2081/2859 (72.79) | 9 | 1.23 | 0.80–1.90 | 0.6176 | <0.0001 | 0.3410 |
| Sexual orientation | |||||||
| Bisexual | 2285/2508 (91.11) | 8 | 0.84 | 0.72–0.99 | 0.0110 | 0.5000 | 0.0350 |
| Heterosexual | 3913/8314 (47.07) | 5 | 0.76 | 0.59–0.97 | 0.7406 | 0.6830 | 0.0260 |
| Homosexual | 9672/10694 (90.44) | 10 | 1.27 | 1.10–1.47 | 0.6958 | 0.5670 | 0.0010 |
| History of chronic disease(s) | 942/1135 (83.00) | 7 | 1.20 | 0.84–1.71 | 0.0973 | 0.0730 | 0.3180 |
| HIV positivity | 4610/5197 (88.71) | 7 | 1.43 | 1.16–1.77 | 0.3304 | 0.0750 | 0.0010 |
| History of STDs | 7044/8130 (86.64) | 8 | 1.25 | 0.86–1.80 | 0.0823 | <0.0001 | 0.2430 |
| History of monkeypox | 311/371 (83.83) | 4 | 1.34 | 0.82–2.20 | 0.2305 | 0.0630 | 0.2430 |
| History of vaccination | |||||||
| COVID-19 vaccination | 1398/2400 (58.25) | 9 | 2.48 | 1.50–4.07 | 0.4259 | 0.0010 | <0.0001 |
| Influenza vaccination | 722/1272 (56.76) | 6 | 1.39 | 1.10–1.76 | 0.2308 | 0.2660 | 0.0060 |
| Smallpox vaccination | 676/994 (68.01) | 6 | 0.88 | 0.61–1.27 | 0.1297 | 0.0080 | 0.4990 |
BSc: Bachelor of Science; STD: sexually transmitted disease
Heterogeneity and potential publication bias
The results of the Q-test indicated the heterogeneity in the overall monkeypox vaccine acceptance prevalence and its subgroup analysis. The heterogeneity data were presented using a random effect model. In this study, the heterogeneity was negligible in the middle-income variable, sexual orientation, and influenza vaccination, with the data presented in a fixed effect model. Furthermore, Egger’s test and funnel plot analyses (see Underlying data) revealed potential publication bias in the age and bisexual orientation variables. Consequently, data interpretation was adjusted using the trim-fill method.
Discussion
Our study found that the global prevalence of monkeypox vaccination acceptance was 65%. Sub-group analysis revealed that the highest prevalence of monkeypox vaccination acceptance was among MSMs (82%), followed by medical students (64%), and the general population (56%). Conversely, HCWs exhibited the lowest prevalence of monkeypox vaccine acceptance (52%). Our findings showed a higher rate of monkeypox vaccine acceptance compared to the last meta-analyses, with acceptance rates ranging between 56%–61% [13-16]. Furthermore, our study offers several advantages over the previous meta-analysis. First, our sample size was larger population, including 51 articles with 98,746 participants, compared to the previous study, which encompassed 10–30 articles with 8,045–81,792 participants [13-16]. Second, prior studies lacked adequate statistical testing methods, as they uniformly applied random effect models despite significant heterogeneity ranging from 0% to 80% [15]. The choice between random or fixed effect models should have been aligned with the level of heterogeneity to avoid biases in the results [20]. Third, some references had been omitted in previous studies [13], as a reference, is crucial for ensuring the replicability of meta-analysis procedures. Fourth, previous studies only reported overall prevalence rates [13-16], and this study also identified contributing factors to monkeypox vaccination acceptance.
Our study also revealed that educational attainment of at least a BSc degree, history of COVID-19 vaccination, and influenza vaccination were associated with increased acceptance of the monkeypox vaccine. However, the underlying reasons for our study’s findings remain difficult to explain. It should be noted that educational attainment of at least a BSc degree indicated that individuals likely had good knowledge of health behaviors [73]. However, this did not align with our results, as we failed to demonstrate a clear role of knowledge about monkeypox in the monkeypox vaccine acceptance. This complexity is difficult to explain. It is important to understand that knowledge and applying health awareness behaviors do not always align. Having good knowledge of a disease does not necessarily equate to adopting good health behaviors. Good knowledge alone, without awareness behaviors, may not be adequate in triggering acceptance of the monkeypox vaccine [74]. This condition may explain our findings that individuals with a good awareness of disease prevention, such as those who had received influenza and COVID-19 vaccinations, showed increased acceptance of the monkeypox vaccine. This study revealed that although the majority of study participants demonstrated adequate understanding, the vaccine acceptance rate was relatively lower [75]. Another study also emphasized the crucial role of awareness in increasing vaccine acceptance [76]. This explanation may correspond to our findings that individuals with a history of COVID-19 and influenza vaccination and those with the educational attainment of at least a BSc degree showed a favorable response to monkeypox vaccine acceptance.
Furthermore, we found that individuals with homosexual orientation and those who were HIV-positive exhibited higher acceptance of monkeypox vaccination, while individuals identified as heterosexual or bisexual demonstrated lower acceptance. In the case of HIV patients, it is widely acknowledged that a significant portion of them engage in behaviors associated with homosexuality [77]. Hence, this correlation could provide insight into the idea that both HIV-positive status and homosexual behavior played contributory roles in the heightened acceptance of monkeypox vaccination. Several factors explain this increased acceptance within these demographic groups. First, due to their sexual behaviors and close contact with multiple partners, they are deemed a high-risk demographic for monkeypox infection [16]. Second, their heightened awareness of the threat posed by monkeypox and the critical importance of vaccination was evident through their increased concern regarding outbreaks and their expressed intentions to receive the vaccine [78]. Third, within the homosexual community, there is a noticeable sense of solidarity and collective responsibility toward safeguarding both individual health and the broader community from the possible consequences of the illness [55]. This collective mindset likely fostered acceptance and uptake of the monkeypox vaccine among the populations.
This study has several implications. First, it contributed to understanding the prevalence of monkeypox vaccine acceptance across various demographics, enabling the identification of the groups that are more inclined to accept the vaccine and those who require focused education and outreach efforts. These findings are crucial in shaping more effective vaccination campaigns and public health policies, supporting monkeypox vaccination initiatives [79]. Second, our study identified the determinants of vaccine acceptance, including educational level, vaccination history, HIV status, and sexual orientation. This knowledge could guide targeted interventions to strengthen vaccine acceptance within specific populations [80]. Third, by comparing vaccine acceptance rates among diverse groups such as the general population, MSMs, medical students, and HCWs, we could identify disparities in acceptance and tailor public health interventions accordingly. Fourth, understanding the prevalence of vaccine acceptance could help the vaccine distribution strategies and potentially prioritize vaccination for high-risk groups or implement focused outreach to enhance acceptance in specific populations [79]. In summary, our investigation into the global prevalence and associated factors of monkeypox vaccine acceptance is pivotal for guiding public health policies and strategies to mitigate the spread of the disease.
There are some limitations to this study. First, although this meta-analysis serves as a methodological approach to calculate the crude effect of relevant factors and establish evidence, evaluating the impact of potential confounding variables proved challenging. Factors such as government regulations, sources of information on monkeypox vaccination, and environmental influences were not included in this study, necessitating a cautious interpretation of our findings. Second, this study involved a multinational population, where the understanding of disease prevention may have varied among individuals with similar socioeconomic and educational backgrounds in different regions. Third, the proportion of selected articles varied across regions, potentially influencing the final results. Fourth, in determining contributing factors, this study included diverse populations such as HCWs, the general population, medical students, and MSMs, which may have yet to fully represent all groups at risk of monkeypox infection. Fifth, our study lacked longitudinal data on vaccine acceptance, inhibiting our ability to discern changes over time and assess the impact of public health interventions.
Conclusion
This meta-analysis found that the global acceptance rate for monkeypox vaccination was estimated to be 65%. Additionally, our findings revealed that the acceptance of monkeypox vaccine was influenced by several factors, including educational attainment, history of vaccination, HIV status, and sexual orientation.
Acknowledgments
We thank to Indonesia Endowment Fund for Education Agency (Lembaga Pengelola Dana Pendidikan/LPDP).
Ethics approval
Not required.
Competing interests
All the authors declare that there are no conflicts of interest.
Funding
This study received no external funding.
Underlying data
Supplementary data can be accessed through this link: https://doi.org/10.6084/m9.figshare.25598916.
How to cite
Indiastari D, Fajar JK, Tamara F, et al. Global prevalence and determinants associated with the acceptance of monkeypox vaccination. Narra J 2024; 4 (2): e866 - http://doi.org/10.52225/narra.v4i2.866.
References
- 1.Hraib M, Jouni S, Albitar MM, et al. The outbreak of monkeypox 2022: An overview. Ann Med Surg (Lond) 2022;79(1):104069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reina J, Iglesias C.. Vaccines against monkeypox. Med Clin (Engl Ed) 2023;160(7):305–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Greenwood B. The contribution of vaccination to global health: Past, present and future. Philos Trans R Soc Lond B Biol Sci 2014;369(1645):20130433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salo H, Kilpi T.. National vaccination program - a success story of public health and economy. Duodecim 2017;133(10):977–983. [PubMed] [Google Scholar]
- 5.Anderson EL. Recommended solutions to the barriers to immunization in children and adults. Mo Med 2014;111(4):344–348. [PMC free article] [PubMed] [Google Scholar]
- 6.Shen SC, Dubey V.. Addressing vaccine hesitancy: Clinical guidance for primary care physicians working with parents. Can Fam Physician 2019;65(3):175–181 [PMC free article] [PubMed] [Google Scholar]
- 7.Fajar JK, Sallam M, Soegiarto G, et al. Global prevalence and potential influencing factors of COVID-19 vaccination hesitancy: A meta-analysis. Vaccines (Basel) 2022;10(8):1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mesch GS, Schwirian KP. Vaccination hesitancy: Fear, trust, and exposure expectancy of an Ebola outbreak. Heliyon 2019;5(7):e02016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aide P, Bassat Q, Alonso PL. Towards an effective malaria vaccine. Arch Dis Child 2007;92(6):476–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fatima K, Syed NI. Dengvaxia controversy: Impact on vaccine hesitancy. J Glob Health 2018;8(2):010312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schmid P, Rauber D, Betsch C, et al. Barriers of influenza vaccination intention and behavior - a systematic review of influenza vaccine hesitancy, 2005–2016. PLoS One 2017;12(1):e0170550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization. Vaccines and immunization for monkeypox: Interim guidance, 16 November 2022. Available from: https://www.who.int/publications/i/item/WHO-MPX-Immunization. Accessed: 10 April 2024.
- 13.Mektebi A, Elsaid M, Yadav T, et al. Mpox vaccine acceptance among healthcare workers: A systematic review and meta-analysis. BMC Public Health 2024;24(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leon-Figueroa DA, Barboza JJ, Valladares-Garrido MJ, et al. Prevalence of intentions to receive monkeypox vaccine. A systematic review and meta-analysis. BMC Public Health 2024;24(1):35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moawad MH, Taha AM, Nguyen D, et al. Attitudes towards receiving monkeypox vaccination: A systematic review and meta-analysis. Vaccines (Basel) 2023;11(12):1840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ulloque-Badaracco JR, Alarcon-Braga EA, Hernandez-Bustamante EA, et al. Acceptance towards monkeypox vaccination: A systematic review and meta-analysis. Pathogens 2022;11(11):1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021;372(1):n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25(9):603–605. [DOI] [PubMed] [Google Scholar]
- 19.Fajar JK. Approaches for identifying and managing publication bias in meta-analysis. Deka in Medicine 2024;1(1):e865. [Google Scholar]
- 20.Ruppar T. Meta-analysis: How to quantify and explain heterogeneity? Eur J Cardiovasc Nurs 2020;19(7):646–652. [DOI] [PubMed] [Google Scholar]
- 21.Lee CH, Cook S, Lee JS, et al. Comparison of two meta-analysis methods: Inverse-variance-weighted average and weighted sum of Z-scores. Genomics Inform 2016;14(4):173–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abd ElHafeez S, Gebreal A, Khalil MA, et al. Assessing disparities in medical students’ knowledge and attitude about monkeypox: A cross-sectional study of 27 countries across three continents. Front Public Health 2023;11(1):1192542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ahmed SK, Abdulqadir SO, Omar RM, et al. Knowledge, attitude and worry in the Kurdistan region of Iraq during the mpox (monkeypox) outbreak in 2022: An online cross-sectional study. Vaccines (Basel) 2023;11(3):610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ahmed SK, Abdulqadir SO, Omar RM, et al. Knowledge, attitudes, and willingness of healthcare workers in Iraq’s Kurdistan region to vaccinate against human monkeypox: A nationwide cross-sectional study. Vaccines (Basel) 2023;11(12):1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alarifi AM, Alshahrani NZ, Sah R.. Are Saudi healthcare workers willing to receive the monkeypox virus vaccine? Evidence from a descriptive-baseline survey. Trop Med Infect Dis 2023;8(8):396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Andersen EW, Kulie P, Castel AD, et al. Mpox awareness, risk reduction, and vaccine acceptance among people with HIV in Washington, DC. Pathogens 2024;13(2):124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Araoz-Salinas JM, Ortiz-Saavedra B, Ponce-Rosas L, et al. Perceptions and intention to get vaccinated against mpox among the LGBTIQ+ community during the 2022 outbreak: A cross-sectional study in Peru. Vaccines (Basel) 2023;11(5):1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bates BR, Grijalva MJ. Knowledge, attitudes, and practices towards monkeypox during the 2022 outbreak: An online cross-sectional survey among clinicians in Ohio, USA. J Infect Public Health 2022;15(12):1459–1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Caycho-Rodriguez T, Valencia PD, Ventura-Leon J, et al. Intention to receive the monkeypox vaccine and its psychological and sociodemographic predictors: A cross-sectional survey in the general population of Peru. Psicol Reflex Crit 2023;36(1):39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen Y, Li Y, Fu L, et al. Knowledge of human mpox (monkeypox) and attitude towards mpox vaccination among male sex workers in china: A cross-sectional study. Vaccines (Basel) 2023;11(2):285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Crosato V, Formenti B, Gulletta M, et al. Perception and awareness about monkeypox and vaccination acceptance in an at-risk population in Brescia, Italy: An investigative survey. AIDS Behav 2024;10(1):s10461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Curtis MG, Davoudpour S, Rodriguez-Ortiz AE, et al. Predictors of Mpox vaccine uptake among sexual and gender minority young adults living in Illinois: Unvaccinated vs. double vs. single dose vaccine recipients. Vaccine 2023;41(27):4002–4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dong C, Yu Z, Zhao Y, et al. Knowledge and vaccination intention of monkeypox in China’s general population: A cross-sectional online survey. Travel Med Infect Dis 2023;52(1):102533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dukers-Muijrers N, Evers Y, Widdershoven V, et al. Mpox vaccination willingness, determinants, and communication needs in gay, bisexual, and other men who have sex with men, in the context of limited vaccine availability in the Netherlands (Dutch mpox-survey). Front Public Health 2022;10(1):1058807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Filardo TD, Prasad N, Waddell CJ, et al. Mpox vaccine acceptability among people experiencing homelessness in San Francisco - October-November 2022. Vaccine 2023;41(39):5673–5677. [DOI] [PubMed] [Google Scholar]
- 36.Fu L, Sun Y, Li Y, et al. Perception of and vaccine readiness towards mpox among men who have sex with men living with HIV in China: A cross-sectional study. Vaccines (Basel) 2023;11(3):528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ghazy RM, Yazbek S, Gebreal A, et al. Monkeypox vaccine acceptance among Ghanaians: A call for action. Vaccines (Basel) 2023;11(2):240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Harapan H, Wagner AL, Yufika A, et al. Acceptance and willingness to pay for a hypothetical vaccine against monkeypox viral infection among frontline physicians: A cross-sectional study in Indonesia. Vaccine 2020;38(43):6800–6806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Harapan H, Setiawan AM, Yufika A, et al. Physicians’ willingness to be vaccinated with a smallpox vaccine to prevent monkeypox viral infection: A cross-sectional study in Indonesia. Clin Epidemiol Glob Health 2020;8(4):1259–1263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hong J, Pan B, Jiang HJ, et al. The willingness of Chinese healthcare workers to receive monkeypox vaccine and its independent predictors: A cross-sectional survey. J Med Virol 2023;95(1):e28294. [DOI] [PubMed] [Google Scholar]
- 41.Huang X, Lin Z, Qin J, et al. Willingness to accept monkeypox vaccine and its correlates among men who have sex with men in Southern China: A web-based online cross-sectional study. Front Public Health 2024;12(1):1289918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Islam MR, Haque MA, Ahamed B, et al. Assessment of vaccine perception and vaccination intention of mpox infection among the adult males in Bangladesh: A cross-sectional study findings. PLoS One 2023;18(6):e0286322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jamaleddine Y, El Ezz AA, Mahmoud M, et al. Knowledge and attitude towards monkeypox among the Lebanese population and their attitude towards vaccination. J Prev Med Hyg 2023;64(1):E13–E26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jongen VW, Groot Bruinderink ML, Boyd A, et al. What determines mpox vaccination uptake? Assessing the effect of intent-to-vaccinate versus other determinants among men who have sex with men. Vaccine 2024;42(2):186–193. [DOI] [PubMed] [Google Scholar]
- 45.Karapinar A, Akdağ D, Gökengin D.. Awareness and acceptability of monkeypox vaccine in men who have sex with men. Turk J Med Sci 2023;53(5):1136–1143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kumar N, Ahmed F, Raza MS, et al. Monkeypox cross-sectional survey of knowledge, attitudes, practices, and willingness to vaccinate among university students in Pakistan. Vaccines (Basel) 2022;11(1):97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lin GSS, Tan WW, Chan DZK, et al. Monkeypox awareness, knowledge, and attitude among undergraduate preclinical and clinical students at a Malaysian dental school: An emerging outbreak during the COVID-19 era. Asian Pacific Journal of Tropical Medicine 2022;15(10):461–467. [Google Scholar]
- 48.Lounis M, Bencherit D, Abdelhadi S.. Knowledge and awareness of Algerian healthcare workers about human monkeypox and their attitude toward its vaccination: An online cross-sectional survey. Vacunas 2023;24(2):122–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lounis M, Hamimes A, Dahmani A.. Assessment of monkeypox (mpox) knowledge and vaccination intention among health and life sciences students in Algeria: A cross-sectional study. Infect Dis Rep 2024;16(2):170–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Luo S, Jiao K, Zhang Y, et al. Behavioral intention of receiving monkeypox vaccination and undergoing monkeypox testing and the associated factors among young men who have sex with men in China: Large cross-sectional study. JMIR Public Health Surveill 2024;10(1):e47165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mahameed H, Al-Mahzoum K, AlRaie LA, et al. Previous vaccination history and psychological factors as significant predictors of willingness to receive mpox vaccination and a favorable attitude towards compulsory vaccination. Vaccines (Basel) 2023;11(5):897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Paparini S, Whitacre R, Smuk M, et al. Public understanding and awareness of and response to monkeypox virus outbreak: A cross-sectional survey of the most affected communities in the United Kingdom during the 2022 public health emergency. HIV Med 2023;24(5):544–557. [DOI] [PubMed] [Google Scholar]
- 53.Peptan C, Baleanu VD, Marcau FC. Study on the vaccination of the population of Romania against monkeypox in terms of medical security. Vaccines (Basel) 2022;10(11):1834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ren F, Miao J, Liu J, et al. Willingness to receive and recommend hypothetical mpox vaccination and associated factors in Chinese adults: A community-based survey in Shenzhen, China. Public Health 2023;225(1):267–276. [DOI] [PubMed] [Google Scholar]
- 55.Reyes-Uruena J, D’Ambrosio A, Croci R, et al. High monkeypox vaccine acceptance among male users of smartphone-based online gay-dating apps in Europe, 30 July to 12 August 2022. Euro Surveill 2022;27(42):2200757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Riad A, Drobov A, Rozmarinova J, et al. Monkeypox knowledge and vaccine hesitancy of Czech healthcare workers: A health belief model (hbm)-based study. Vaccines (Basel) 2022;10(12):2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Riad A, Rybakova N, Dubatouka N, et al. Belarusian healthcare professionals’ views on monkeypox and vaccine hesitancy. Vaccines (Basel) 2023;11(8):1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ricco M, Ferraro P, Camisa V, et al. When a neglected tropical disease goes global: Knowledge, attitudes and practices of Italian physicians towards monkeypox, preliminary results. Trop Med Infect Dis 2022;7(7):135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sahin TK, Erul E, Aksun MS, et al. Knowledge and attitudes of Turkish physicians towards human monkeypox disease and related vaccination: A cross-sectional study. Vaccines (Basel) 2022;11(1):19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Salim NA, Septadina IS, Permata M.. Knowledge, attitude, and perception of anticipating 2022 global human monkeypox infection among internal medicine residents at Palembang Indonesia: An online survey. Jurnal Kedokteran dan Kesehatan: Publikasi Ilmiah Fakultas Kedokteran Universitas Sriwijaya 2022;9(3):253–262. [Google Scholar]
- 61.Scarinci S, Padovan M, Cosci B, et al. Evaluation of smallpox vaccination coverage and attitude towards monkeypox vaccination among healthcare workers in an Italian university hospital. Vaccines (Basel) 2023;11(12):1741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Temsah MH, Aljamaan F, Alenezi S, et al. Monkeypox caused less worry than COVID-19 among the general population during the first month of the WHO monkeypox alert: Experience from Saudi Arabia. Travel Med Infect Dis 2022;49(1):102426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Torres TS, Silva MST, Coutinho C, et al. Evaluation of mpox knowledge, stigma, and willingness to vaccinate for mpox: Cross-sectional web-based survey among sexual and gender minorities. JMIR Public Health Surveill 2023;9(1):e46489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tran BX, Anh Do L, Hoang TP, et al. Crucial choices in a global health crisis: Revealing the demand and willingness to pay for a hypothetical monkeypox vaccine - the PREVENT study. J Glob Health 2023;13(1):04033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Turpin RE, Mandell CJ, Camp AD, et al. Monkeypox-related stigma and vaccine challenges as a barrier to HIV pre-exposure prophylaxis among black sexual minority men. Int J Environ Res Public Health 2023;20(14):6324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wang B, Peng X, Li Y, et al. Perceptions, precautions, and vaccine acceptance related to monkeypox in the public in China: A cross-sectional survey. J Infect Public Health 2023;16(2):163–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wang H, d’Abreu de Paulo KJI, Gultzow T, et al. Monkeypox self-diagnosis abilities, determinants of vaccination and self-isolation intention after diagnosis among MSM, the Netherlands, July 2022. Euro Surveill 2022;27(33):2200603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Winters M, Malik AA, Omer SB. Attitudes towards monkeypox vaccination and predictors of vaccination intentions among the US general public. PLoS One 2022;17(12):e0278622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Yang X, Yang X, Jiang W, et al. A cross-sectional investigation of factors influencing mpox vaccine hesitancy for students in Southwest China. Hum Vaccin Immunother 2024;20(1):2309704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zheng M, Qin C, Qian X, et al. Knowledge and vaccination acceptance toward the human monkeypox among men who have sex with men in China. Front Public Health 2022;10(1):997637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zheng M, Du M, Yang G, et al. Lower rate of mpox vaccination hesitancy and medical consultation among Chinese men who have sex with men living with HIV in comparison with those living without HIV: A national observational study. Hum Vaccin Immunother 2023;19(3):2290788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zucman D, Fourn E, Touche P, et al. Monkeypox vaccine hesitancy in French men having sex with men with prep or living with HIV in France. Vaccines (Basel) 2022;10(10):1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ping R, Oshio T.. Education level as a predictor of the onset of health problems among China’s middle-aged population: Cox regression analysis. Front Public Health 2023;11(1):1187336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Rincon Uribe FA, Godinho RCS, Machado MAS, et al. Health knowledge, health behaviors and attitudes during pandemic emergencies: A systematic review. PLoS One 2021;16(9):e0256731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Taneja P, Marya CM, Kashyap P, et al. Knowledge and acceptance of the COVID-19 vaccine for COVID-19 disease prevention among the Indian population: A mixed-method study. Vaccines (Basel) 2022;10(10):1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Asres F, Umeta B.. COVID-19 vaccines: Awareness, attitude and acceptance among undergraduate university students. J Pharm Policy Pract 2022;15(1):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Evans MG, Cloete A, Zungu N, et al. HIV risk among men who have sex with men, women who have sex with women, lesbian, gay, bisexual and transgender populations in South Africa: A mini-review. Open AIDS J 2016;10(1):49–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Aquino YSJ, Cabrera N, Salisi J, et al. Monkeypox and the legacy of prejudice in targeted public health campaigns. BMJ Glob Health 2022;7(10):e010630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chakraborty S, Mohapatra RK, Chandran D, et al. Monkeypox vaccines and vaccination strategies: Current knowledge and advances. An update - correspondence. Int J Surg 2022;105(1):106869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Petersen E, Zumla A, Hui DS, et al. Vaccination for monkeypox prevention in persons with high-risk sexual behaviours to control on-going outbreak of monkeypox virus clade 3. Int J Infect Dis 2022;122(1):569–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Supplementary data can be accessed through this link: https://doi.org/10.6084/m9.figshare.25598916.