Abstract
The prevalence of human immunodeficiency virus (HIV) among adolescents is on the rise due to a lack of comprehensive knowledge, leading to suboptimal attitudes and behaviors, which emphasizes the critical need for targeted interventions. The aim of this review study was to evaluate the effectiveness of educational interventions for HIV prevention among adolescents by assessing their impact on knowledge, attitude, and behavior. A systematic review of seven databases: PubMed, Science Direct, Cochrane, JSTOR, Embase, Scopus, and EBSCO were identified, and 14 eligible randomized controlled trials published until June 2023 were included. Two independent authors assessed quality appraisal using the Risk of Bias 2.0. Outcomes were measured using the standard mean difference (SMD) with random effects model and a 95% confidence interval. Subgroup analyses and meta-regression were performed to explore heterogeneity. The results showed significant improvements in participants’ knowledge (SMD: 1.13, 95%CI: 0.78–1.49), behavior intentions (SMD: 1.22, 95%CI: 0.37–2.07), and attitude (SMD: 0.48, 95%CI: 0.02–0.95) after receiving HIV prevention education programs. Interventions grounded in theoretical principles and incorporating technology, group settings, and audio-visual aids were found to be effective in enhancing knowledge of HIV prevention and promoting behavioral intentions. Peer-led education positively impacted both knowledge and attitude. Moreover, excluding parents from these programs was identified as a crucial factor in improving adolescents’ knowledge of HIV prevention. In conclusion, educational programs focused on HIV effectively enhance adolescents’ knowledge, attitudes, and behavioral intentions among adolescents. Professionals planning interventions should consider these impactful components in designing comprehensive strategies.
Keywords: Attitude, behavioral, educational programs, HIV, knowledge
Introduction
Human immunodeficiency virus (HIV) and acquired immune deficiency syndrome (AIDS) are infectious diseases that pose significant challenges for healthcare professionals around the world in terms of prevention, management, and eradication among specific populations and high-risk groups [1]. HIV and AIDS can be transmitted through several body fluids, including blood, semen, pre-ejaculate fluid, vaginal fluid, anal fluid, and breast milk [2,3]. The rapid transmission of HIV has led to a significant annual rise in HIV cases [4]. The incidence of HIV infection among adolescents has risen over the past five years, with a prevalence rate of 35% or 480,000 cases among individuals aged 10–24 years, and 140,000 cases in those aged 10–19 years [5]. This high prevalence can be attributed to a lack of comprehensive knowledge, leading to poor attitudes and behaviors in avoiding HIV and AIDS in this age group [6]. Hence, devising an intervention specifically targeting HIV prevention in adolescents is crucial.
Attitudes toward HIV and AIDS prevention in adolescents reflect their positive outlook to engage in preventative measures against HIV/AIDS [7]. HIV/AIDS prevention behavior refers to an individual’s capacity to engage in actions such as abstaining from sexual relations, avoiding multiple sexual partners, using condoms, and refraining from using injectable drugs [8-10]. Those two variables (attitude and behavior) are the protective variables that influence adolescents’ decision-making regarding the enactment of behavior [3]. Enhancing these protective factors is essential to mitigate the risk of HIV and AIDS among adolescent by improving their knowledge, attitudes, and behaviors about prevention [11].
One of the prevention programs is the Determined, Resilient, Empowered, AIDS-free, Mentored, and Safe (DREAMS) program, which focuses on implementing various interventions for HIV and AIDS prevention among young women at high risk in sub-Saharan Africa through a comprehensive approach [12]. It includes HIV prevention education, mentorship for empowerment, the creation of safe spaces for open discussions, behavioral interventions promoting safe practices, and community engagement to address social norms. The program’s primary objective is to reduce new HIV infections by addressing the social, economic, and health factors contributing to vulnerability, empowering young women with the knowledge and skills to protect themselves and lead healthy lives. Numerous intervention programs designed to enhance adolescents’ understanding of HIV prevention have been implemented in community and school settings, involving educational and counseling initiatives facilitated by peers, instructors, and parents [13]. However, the existing investigations, employing both randomized control trials (RCTs) [14] and non-randomized control trial design [15], pose challenges in reaching definitive results [16,17]. Combining research with an RCT design to increase the sample size may offer advantageous outcomes [18] and yield more accurate outcomes [19].
The aim of this meta-analysis was to address a crucial research gap in existing systematic reviews and meta-analyses that have focused on different aspects of HIV prevention, such as knowledge enhancement, attitude, and behavior modifications, or the efficacy of educational interventions among adolescents [20-28]. There remains a scarcity of synthesized evidence that collectively examines the holistic outcomes of educational programs specifically targeting adolescents. The identified studies have primarily focused on either knowledge enhancement [25,29-33], attitude and behavior modifications [21,22,28,34], or the efficacy of educational interventions [21,32,35,36] among adolescents.
Adolescence is a period of significant and quick transformations in physical, mental, and intellectual capacities, making it crucial for the development of knowledge, attitudes, beliefs, and healthy behavior, including HIV and AIDS prevention [37]. To create an educational program tailored for adolescents, various elements like the content, delivery method, information source, setting, and format of the educational material should be adaptable to the specific needs and circumstances. Previous meta-analyses by Mirzazadeh et al. [13] and Kim et al. [38], have not clarified which specific program aspects and characteristics are linked to successful HIV prevention in terms of adolescent knowledge, behavior, and attitudes. The complex nature of the factors that influence behavior change also contributes to the lack of data on efficacy. Long-term and thorough tactics, as indicated by the research of Lonczak et al. [39], involving the active participation of peers, teachers, and parents have proven more effective than interventions solely focused on sexual education within schools [40-42]. Therefore, it is imperative to perform an analysis of the essential elements in developing an appropriate educational program to prevent HIV among adolescents.
This aim of this meta-analysis was to provide a comprehensive understanding of the overall impact of educational programs on adolescents’ knowledge, attitude, and behavior regarding HIV prevention by enhancing the comparability of study findings, assess the effectiveness of educational programs on HIV prevention knowledge and behavior among adolescents, and identify the key components of successful programs in preventing HIV among this age group. The synthesis is intended to offer valuable insights into the complex nature of HIV prevention efforts, potentially guiding the development of more efficient and focused interventions.
Methods
The present study offered a systematic review and meta-analysis of RCTs. The research procedure has been prospectively registered in the International Prospective Register of Systematic Reviews (PROSPERO), CRD42023406705. This study adhered to the guidelines set forth by Preferred Reporting Items for Systematic Reviews and Meta-Analysis 2020 (PRISMA 2020).
Search strategy
Three independent authors (DR, MHH, and MAM) conducted article searches autonomously. A comprehensive literature search was conducted using various combinations of keywords, such as ‘HIV’ OR ‘AIDS’ AND ‘prevention’ AND ‘education’ OR ‘knowledge’ OR ‘attitudes’ OR ‘behavior’ OR ‘practice’ AND ‘adolescents’ OR ‘teenager’ AND ‘randomized controlled trials’ OR ‘randomized controlled study’. Systematic searches were conducted in seven databases: PubMed, ScienceDirect, Cochrane, JSTOR, Embase, Scopus, and EBSCO, covering the period from January 1, 2010, to June 23, 2023. For a comprehensive literature search, the authors utilized Medical Subject Headings (MeSH) terms to ensure the retrieval of relevant and high-quality articles.
Eligibility criteria
The researchers determined the following criteria for the included studies: (1) the study involved adolescents between the ages of 10 to 19 based on studies by Sawyer et al. [43] and Word Health Organization (WHO) [44]; (2) all included studies followed an RCT design and published in the English language; (3) the intervention implemented was an educational program focused on HIV prevention aimed at enhancing HIV knowledge, attitudes, and behavioral intentions in both individuals and groups, including peers, family, and teachers, with the goal of transforming them into support networks for adolescents; (4) the intervention program described in the evaluation was implemented by a team comprising peers, teachers, social workers, and professional healthcare providers, including school nurses, health promotion specialists, psychologists, and psychiatrists, through in-person sessions in schools or communities, as well as online platforms using technology such as the web, Android applications, game therapy, and audiovisual aids such as videos, animations, and photos; and (5) the effectiveness of these programs was assessed by measuring the participants’ HIV knowledge, attitude, and behavioral intentions using a validated questionnaire. The researchers excluded papers that did not have protocol designs, irrelevant studies, duplicates, no full-text access, failure to meet the study purpose, unreported sample sizes, or unreported outcomes of interventions (no effect size estimated presented and no HIV knowledge).
Data screening and extraction
The removal of duplicate articles was automated by Endnote, with any remaining duplications manually eliminated by the researcher. Three researchers (DR, AS, and WW) initially reviewed the titles and abstracts using identical inclusion and exclusion criteria. Subsequently, the articles that satisfied the inclusion criteria, as determined by the title and abstract, were further screened by examining the complete text. Discussions were conducted with the third author (MHH) when discrepancies arose between the three writers throughout the screening process.
The researchers developed a systematic table for extracting the data, which was created based on the papers that were included. The variables that were retrieved comprised the following: (1) research characteristics, such as the authors, year, and country in which the research was conducted, the number of participants in both the experimental and control groups, and the average age of the respondents; (2) components of intervention including theoretical framework, intervention type, setting, content, format, intervention provider, and duration of intervention; and (3) outcomes including the results which were the acquisition of knowledge and the utilization of measurement instruments.
Quality assessment
Two authors (DR and MAM) assessed the methodological rigor of the study using the Cochrane risk of bias tool for randomized controlled trials (RoB 2.0). Five domains were evaluated including the randomization method, variation of intended interventions, missing result data, outcome measurements, selection of reported outcomes, and overall bias. Every element was categorized as having a low risk of bias, a high risk of bias, or a presence of some concern [45– 47]. Discrepancies in the authors’ conclusions were resolved by engaging in a discussion with a third and fourth reviewer (MHH and AS) until a consensus was achieved.
Data analysis
The meta-analysis was conducted using the Comprehensive Meta Analysis version 2.0 (CMA) software [48]. The mean, standard deviation (SD), and sample size of each group were utilized to calculate the standardized mean difference (SMD) and the 95% confidence interval (CI). These values were subsequently employed to generate aggregated effect estimates. Random effects model was employed to synthesize the effects of educational programs on HIV prevention. To explore the possible factors contributing to heterogeneity, moderator analyses were performed on the estimates of participant or intervention characteristics related to knowledge, behavior, and attitude. Subgroup analyses were generated by merging trials and comparing their impacts. Additionally, meta-regressions were conducted to assess the influence of continuous variables on outcomes, that is the duration of the intervention.
Publication bias was assessed by utilizing the Begg and Mazumdar’s rank correlation test [49] and the Duval and Tweedie’s trim-and-fill method [50,51]. Publication bias was detected using a modified Begg’s rank adjustment test with a p-value of 0.05. Furthermore, a sensitivity analysis was performed to assess the resilience of our findings.
Results
Search results
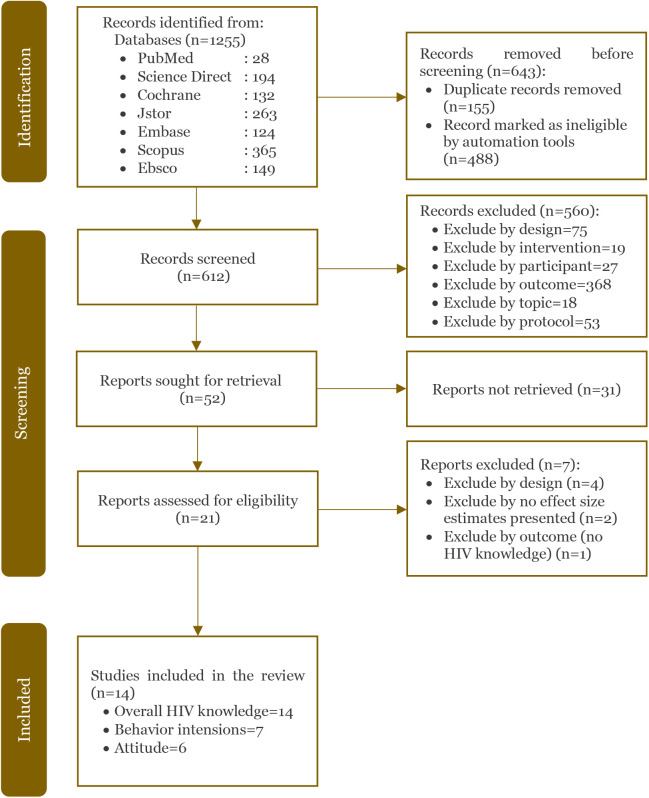
A total of 1255 studies were retrieved from seven databases. Following the elimination of duplicate entries and papers that did not match our inclusion criteria, the complete texts of 612 publications were thoroughly examined and 598 were excluded for reasons listed in Figure 1. Fourteen full-text papers representing 14 specific studies were finally included in this meta-analysis.
Figure 1.
PRISMA flow diagram
Study characteristics
The majority of the studies (n=6) were conducted in the United States. The research sample comprised of 8,045 individuals, with respondents’ average age ranging from 12.9 to 17 years. Several studies utilized various theories to develop educational programs, including a combination of social cognitive theory, reasoned action theory, and plan behavior theory [52], rational emotive behavior therapy (REBT) [53], the theory of planned behavior [54], interactive learning theory [55], a combination of social cognitive theory and the theory of planned behavior [56], and a combination of social cognitive theory and the theory of reasoned action [57].
The included studies exhibit diverse characteristics in terms of delivering educational programs. Various combinations of curriculum and skill based were used [52,58,59]. Some of these interventions were technology-based [53,55,60–63], while other interventions relied solely on a curriculum-based course without incorporating other types of interventions [54,56,57,64,65]. The educational programs were implemented in schools (n=7) and communities (n=7) with the utilization of group-based approaches (n=10). Intervention providers encompassed a range of professionals, including facilitators, nurses, peer educators, professional health promotion specialists, social workers, teachers, and therapists. Most of these studies did not include parental involvement and lacked the utilization of educational media to deliver educational programs (n=10). Furthermore, the instructional programs varied in length, ranging from a minimum of 2 days to a maximum of 4 months (Table 1).
Table 1.
Characteristics of included studies
| Author (year, country) | Participant | Theory | Type of intervention | Setting | Content of intervention | Format | Conducted by | Duration | Outcomes measures | Measurement tools |
|---|---|---|---|---|---|---|---|---|---|---|
| Bauman et al. [52] (2021, United States) | n=397 I=200 C=197 Mean age=13.4 | Social cognitive theory, theory of reasoned action and theory of plan behavior | Curriculum- based Skill-based | Group-based School | Sexual risk behavior Social cognitions Gender norms, relationships, and resilience | Lecture | Facilitator | 14 weeks (11 sessions and 3-week internship) | HIV knowledge Behavioral intentions | 18-items [66] CAPS Sexual behavior [67] |
| Ezegbe et al. [53] (2018, Nigeria) | n=80 I=40 C=40 Mean age= 14.63- 14.93 |
Rationale emotive behavior therapy (REBT) |
Technology- based: digital storytelling |
Group-based School | Signs, symptoms, and stages Mode of transmission Preventive measures |
Lecture Audiovisual |
- | Twice per week over 8 weeks |
HIV knowledge |
HIV Knowledge Questionnaire (HIV-KQ-18) |
| Farahani et al. [54] (2020, Iran) |
n=578 I=289 C=289 Mean age=14.1 |
Theory planned behavior | Curriculum- based | Group-based School | HIV virus HIV prevention HIV transmission Risky behaviors |
Lecture Brainstorming Workshop | Professional health promotion | 6 phases, 2 hours each phase over 10 months | HIV knowledge Attitude Behavioral intentions |
Structure questionnaire |
| Fiellin et al. [55] (2017, United States) |
n=333 Mean age=12.9 |
Interactive learning theory | Technology- based | Individual- based Community |
Sexual risk behaviors and knowledge Attitudes intentions | Video games | - | 75 minutes twice/week over 6 weeks | HIV knowledge Attitude Behavioral intentions |
Sexual health knowledge |
| Kaufman et al. [56] (2014, United States) |
n=635 I=314 C=321 Mean age: 12.98 |
Social cognitive theory and theory of planned behavior |
Curriculum- based | Group-based School |
Knowledge structures Outcome expectancies Efficacy expectancies | Lecture | Social worker | 12 months (30 hours) |
HIV knowledge |
Structured questionnaire National survey |
| Kennedy et al. [57] (2018, Liberia) |
n=704 I=353 C=351 Mean age=16.03 |
Social cognitive theory and theory of reasoned action |
Curriculum- based | Group-based Community | HIV/AIDS- knowledge, Peer norms Sexual attitudes Sexual behaviors |
Lecture | - | 6 months | HIV/AIDS knowledge |
HIV-related knowledge scale |
| Khezri et al. [64] (2019, Iran) |
n=60 I=30 C=30 Mean age=6–18 |
- | Curriculum- based | Group-based Community | Intensity, sensitivity, prevalence, and transmission High-risk actions HIV/AIDS prevention Wrong beliefs HIV/AIDS treatment |
Lecture Movie Photos | - | 2 days | HIV knowledge Attitude |
Knowledge questionnaire about HIV and AIDS Attitude questionnaire about HIV and AIDS |
| Khosravi et al. [65] (2018, Iran) |
n=61 I=30 C=31 Mean age=14.9 |
- | Curriculum- based | Group-based Community | The nature of the disease Mode of transmission, prevention methods Free of charge HIV/AIDS services Communicate and teach their friends |
Lecture Brochures | Trained peers’ educator | 4 weeks | HIV knowledge Attitude Behavioral intentions |
Behavioral surveillance surveys |
| Lescano et al. [59] (2020, United States) |
n=227 I=117 C=110 Mean age I=43.43 (7.18) C=43.86 (6.98) |
- | Curriculum- based Skill-based |
Group-based Community | HIV prevention High-risk behavior Communication about sex and risk behavior Decision-making procedures |
Lecture Discussion Parent involvement: + |
Health professional | 7 hours | HIV knowledge |
HIV knowledge questionnaire and self-efficacy for HIV prevention |
| Marsch et al. [60] (2015, United States) |
n=141 I=69 C=72 Mean age=12.9 |
- | Technology- based | Individual- based Community |
Drug and sex- related factors Youth living with HIV and Hepatitis C Disease coping Managing stigma Disclosing serostatus Healthy style |
Web-based | - | 2 weeks | HIV knowledge Behavioral intentions |
HIV, hepatitis, and STI knowledge test Behavioral intentions scale |
| Mathews et al. [58] (2016, South Africa) |
n=3034 I=1515 C=1519 Mean age=13.7 |
Reason action theory and I-Change theoretical model |
Curriculum- based Skill-based |
Group-based School | Educational program School health service School safety program |
Lecture-based | School nurse | 21 weeks 1– 1.5 hours per week |
HIV knowledge Attitude Behavioral intentions |
Structure questionnaire |
| Nelson et al. [61] (2021, United States) |
n=154 I=77 C=77 Mean age=14–17 |
- | Technology- based | Individual- based Community |
Male anatomy HIV/STIs prevention information General sexual health information Pornography literacy skills |
Games Animation video Infographic | - | 18 weeks | HIV knowledge |
HIV Knowledge Questionnaire (HIV-KQ-18) STD Knowledge Questionnaire (STD-KQ) Validated questionnaire |
| Ofoegbu et al. [62] (2020, Nigeria) |
n=98 I=49 C=49 Mean age=20.43 (0.89) |
Technology- based | Group-based School | Signs, symptoms, and stages Mode of transmission Preventive measures |
Lecture (Audiovisual storytelling) Counselling | Therapist | 16 sessions 8 weeks | HIV knowledge |
HIV-KQ-18 | |
| Peskin et al. [63] (2019, United States) |
n=1543 I=804 C=739 Mean age=13 |
Theory planned behavior | Technology- based | Individual and group- based School |
Friendship qualities Dating Sexual behavior |
Lecture Discussion Parent involvement: + |
Teachers | 24 lessons over 4 months |
HIV knowledge Attitude Behavioral intentions |
Validated questionnaire |
AIDS: acquired immunodeficiency syndrome; C: comparison; CAPS: condom attitude and practice scale; HIV: human immunodeficiency virus; I: intervention; n: total number; STIs: sexually transmitted infections; STD-KQ: sexually transmitted disease-knowledge questionnaire
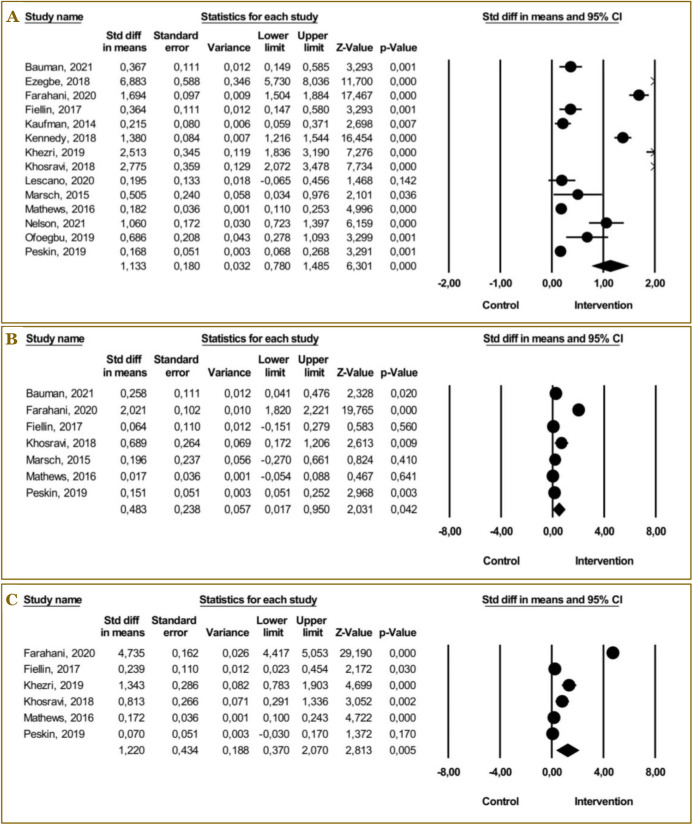
Effectiveness of educational programs on knowledge, behavior, and attitude
The study findings indicated that adolescents who underwent an educational program exhibited significantly higher knowledge scores compared to those who did not receive such a program (SMD: 1.13, 95%CI: 0.78–1.49, p<0.001). Additionally, the I2 value of 97.8 (p<0.001) suggested a high level of heterogeneity among the analyzed studies.
The educational program led to a substantial improvement in behavioral intention among adolescents who received therapy (SMD: 0.48, 95%CI: 0.02–0.95, p<0.05), compared to those in the control group. The analysis revealed a significant level of heterogeneity among the included studies, as indicated by an I2 value of 98.30 and a p<0.001.
The analysis revealed that adolescents who underwent an educational program showed a significant increase in their attitude score toward HIV prevention compared to those who did not undergo the program (SMD: 1.22, 95%CI: 0.37–2.07, p<0.001). The I2 value of 93.4 (p<0.001) indicated a high level of heterogeneity among the studies. Fourteen studies were combined to explore the effects of educational programs (Table 2). Three separate figures depicting the overall effect of educational programs on knowledge (A), behavioral intention (B), and attitude (C) are included in Figure 2.
Table 2.
Effectiveness of educational programs about HIV prevention on knowledge, behavioral intention, and attitude
| Outcome | Number of studies | Standardized mean difference (95%CI) | Heterogeneity | |
|---|---|---|---|---|
| I 2 | p-value | |||
| Knowledge about HIV | 14 | 1.13 (0.78–1.49) *** | 97.80 | <0.001 |
| Behavioral intention | 7 | 0.48 (0.02–0.95) * | 98.30 | <0.001 |
| Attitude | 6 | 1.22 (0.37–2.07) ** | 93.40 | <0.001 |
Statistically significant at p<0.05
Statistically significant at p<0.01
Statistically significant at p<0.001
Figure 2.
The overall effect of educational programs about HIV prevention on knowledge (A), behavioral intention (B), and attitude (C).
Subgroup analysis and meta-regression
The subgroup analysis revealed that theory-based educational programs, technology-based interventions, and group-based education were significantly associated with an increase in knowledge scores regarding HIV prevention (SMD: 1.24, 95%CI: 0.55, 1.92, p<0.001; SMD: 1.69, 95%CI: 0.17–1.75, p<0.001; SMD: 1.64, 95%CI: 0.18–1.10, p<0.00, respectively). The analysis findings also indicated that the implementation of peer educators, exclusion of parental involvement, and utilization of audio-visuals are beneficial strategies for enhancing knowledge of HIV prevention (SMD: 2.51, 95%CI: 1.84 3.19, p<0.001; SMD: 1.35, 95%CI: 0.91–1.8, p<0.001; SMD: 6.88, 95%CI: 5.73–8.04, p<0.001, respectively).
From the analysis, we found that the use of theory and technology, as well as a combination of individual and group modes, led to an increase in behavioral intention (SMD: 0.21, 95%CI: 0.16–0.26, p<0.001; SMD: 1.14, 95%CI: 0.05–1.23, p<0.001; SMD: 0.15, 95%CI: -0.05–0.25, p<0.01, respectively). Adolescent behavior was considerably improved by educational programs offered by experts in health promotion through the use of brochures with an extended intervention duration (SMD: 2.02, 95%CI: 1.82–2.22, p<0.001; SMD: 0.69, 95%CI: 0.17–1.21, p<0.001). The intervention’s impact was also supported by a positive regression coefficient (B: 0.04, p<0.08) (Table 3).
Table 3.
Subgroup analysis and meta-regression of educational programs about HIV prevention on knowledge, behavioral intention, and attitude
| Variables | Knowledge about HIV | Behavioral intention | Attitude | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | SMD (95%CI) | p-value | n | SMD (95%CI) | p-value | n | SMD (95%CI) | p-value | |
| Theory-based intervention | 14 | <0.001 | 7 | 0.013 | 6 | 0.712 | |||
| Yes | 6 | 1.24 (0.55–1.92) *** | 5 | 0.21 (0.16–0.26) *** | 4 | 1.29 (0.24–2.34) * | |||
| No | 8 | 1.07 (0.62–1.52)*** | 2 | 0.42 (0.07–0.76) | 2 | 1.07 (0.55–1.59)*** | |||
| Type of intervention | 14 | <0.001 | 7 | <0.001 | 6 | 0.268 | |||
| Curriculum-based | 5 | 1.66 (0.89–2.43)*** | 3 | 0.91 (-0.60–2.42) | 3 | 2.30 (-0.43–5.03) | |||
| Curriculum-based + skill-based | 3 | 0.21 (0.12–0.31)*** | 1 | 0.26 (0.04–0.48)* | 1 | 0.17 (0.10–0.24)*** | |||
| Technology based | 6 | 1.69 (0.17–1.75)*** | 3 | 1.14 (0.05–1.23) ** | 2 | 0.13 (-0.03–0.28) | |||
| Setting | 14 | 0.969 | 7 | 0.360 | 6 | 0.093 | |||
| School | 7 | 1.05 (0.59–1.51)*** | 4 | 0.61 (-0.05–1.27) | 4 | 1.57 (0.42–2.72)** | |||
| Community | 7 | 1.19 (0.64–1.75)*** | 3 | 0.26 (-0.09–0.61) | 2 | 0.48 (-0.08–1.03) | |||
| Mode | 14 | <0.001 | 7 | 0.002 | 6 | 0.158 | |||
| Group-based | 10 | 1.64 (0.18–1.10)** | 4 | 0.75 (-0.27–1.76) | 4 | 1.77(-0.70–4.23) | |||
| Individual-based | 3 | 1.47 (0.96–1.98)*** | 2 | 0.09 (-0.11–0.28) | 1 | 0.24 (0.02–0.45)* | |||
| Combination | 1 | 0.17 (0.07–0.27)** | 1 | 0.15 (0.05–0.25)** | 1 | 0.07 (-0.03–0.17) | |||
| Provider | 8 | <0.001 | 4 | <0.001 | 4 | <0.001 | |||
| Facilitator | 1 | 0.37 (0.15–0.59)** | 1 | 0.23 (0.04–0.48)* | - | ||||
| Nurse | 1 | 0.18 (0.11–0.25)*** | 1 | 0.02 (-0.05–0.09) | 1 | 0.17 (0.10–0.24)*** | |||
| Peer educator | 1 | 2.51 (1.84–3.19)*** | - | - | 1 | 1.34 (0.78–1.90)*** | |||
| Professional health promotion | 2 | 0.95 (-0.52–2.42) | 1 | 2.02 (1.82–2.22)*** | 1 | 4.74 (4.42–5.05)*** | |||
| Social worker | 1 | 0.22 (0.06–0.37)** | - | - | - | - | |||
| Teacher | 1 | 0.17 (0.07–0.27)** | 1 | 0.15 (0.01–0.25)** | 1 | 0.07 (-0.03–0.17) | |||
| Therapist | 1 | 0.69 (0.28–1.09)** | - | - | - | ||||
| Parent involvement | 14 | <0.001 | 7 | 0.271 | 6 | 0.072 | |||
| Yes | 2 | 0.17 (0.08–0.27)*** | 1 | 0.15 (0.05–0.25)** | 1 | 0.07 (-0.03–0.17) | |||
| No | 12 | 1.35 (0.91–1.80)*** | 6 | 0.54 (-0.15–1.23) | 5 | 1.46 (-0.05–2.97) | |||
| Promotion tools | 14 | <0.001 | 7 | 0.002 | 6 | 0.368 | |||
| Animation + infographic | 1 | 1.06 (0.72–1.40)*** | - | - | |||||
| Audiovisual | 1 | 6.88 (5.73–8.04)*** | - | - | |||||
| Brochure | 1 | 2.78 (2.07–3.48)*** | 1 | 0.69 (0.17–1.21)** | 1 | 0.81 (0.29–1.34)** | |||
| Movie + photo | 1 | 2.51 (0.12–1.84)*** | - | 1 | 1.34 (0.78–1.90)*** | ||||
| None used | 10 | 0.58 (0.24–0.91)** | 6 | 0.45 (-0.05–0.96) | 4 | 1.28 (0.24–2.34)** | |||
| Duration | 14 | β=0.02 | 0.206 | 7 | β=0.04 | 0.008 | 6 | β=0.09 | 0.004 |
| Age | 11 | β=-0.01 | 0.507 | 7 | β=0.54 | 0.173 | 5 | β=0.62 | 0.532 |
B: coefficient beta; CI: confident interval; n: number of studies; SMD: standardized mean difference
Statistically significant at p<0.05
Statistically significant at p<0.01
Statistically significant at p<0.001
The study’s findings also indicated that longer educational sessions offered by health promotion professionals considerably enhanced adolescents’ attitudes toward HIV prevention (SMD: 4.74, 95%CI: 4.42–5.05, p<0.001). The regression analysis further supported this, showing a positive relationship between session length and improved attitudes (B: 0.09, p<0.04). The subgroup analysis and meta-regression of the included studies are depicted in Table 3.
Risk of bias among included studies
Following the evaluation of the studies that were included, it was determined that six studies had low chance of bias, six studies had certain concerns, and one study had a significant risk of bias (Table 4). The majority of studies expressed issues in the domains of randomization procedure (n=5), deviation from intended intervention (n=2), n domain, and assessment of the outcome (n=1).
Table 4.
Risk of bias among included studies
| Study | D1 | D2 | D3 | D4 | D5 | Overall |
|---|---|---|---|---|---|---|
| Bauman et al. 2021 [52] United States |
⊖ | ⊕ | ⊕ | ⊕ | ⊕ | ⊖ |
| Ezegbe et al. 2018 [53] Nigeria |
⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ |
| Farahani et al. 2020 [54] Iran |
⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ |
| Fiellin et al. 2017 [55] United States |
⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ |
| Kaufman et al. 2014 [56] United States |
⊖ | ⊕ | ⊕ | ⊕ | ⊕ | ⊖ |
| Kennedy et al. 2018 [57] Liberia |
⊕ | ⊖ | ⊕ | ⊕ | ⊕ | ⊖ |
| Khezri et al. 2019 [64] Iran | ⊖ | ⊕ | ⊕ | ⊕ | ⊕ | ⊖ |
| Khosravi et al. 2018 [65] Iran |
⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ |
| Lescano et al. 2020 [59] United States |
⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ |
| Marsch et al. 2015 [60] United States |
⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ |
| Mathews et al. 2016 [58] South Africa |
⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ |
| Nelson et al. 2021 [61] United States |
⊕ | ⊖ | ⊕ | ⊕ | ⊕ | ⊖ |
| Ofoegbu et al. 2020 [62] Nigeria |
⊖ | ⊕ | ⊕ | ⊖ | ⊕ | ⊗ |
| Peskin et al. 2019 [63] United States |
⊖ | ⊕ | ⊕ | ⊕ | ⊕ | ⊖ |
D1: randomization process; D2: deviation from intended intervention; D3: missing outcome data; D4: measurement of the outcome; D5: selection of the reported result
Judgement:
⊗ High
⊖ Some
⊕ Low
Publication bias
Begg and Mazumdar’s rank correlation test was employed using Kendall’s tau statistics with a continuity adjustment to evaluate the presence of publication bias. Kendall’s statistic for knowledge was determined to be 0.27, with a corresponding z-score of 0.75 and a p-value of 0.45. The results of our analysis showed that Kendall’s statistics for behavioral intention and attitude were 0.00, z=0.00, p=1.00, and -0.50, z=1.02, p=0.31, respectively. These findings indicate that there was no substantial bias concerning these variables.
Sensitivity analysis
No outliers were identified in the sensitivity analysis when the study with the greatest effect size on knowledge, behavioral intention, and attitude was excluded. Significant SMD values were obtained for knowledge (SMD: 1.10, 95%CI: 0.77–1.46, p<0.001), behavioral intention (SMD: 0.48, 95%CI: 0.02, 0.95; p<0.05), and attitude (SMD: 1.02, 95%CI: 0.34, 2.05; p<0.001); these values suggest that the findings were robust.
Discussion
To the best of our knowledge, this is the first systematic review and meta-analysis to assess the effectiveness of educational programs in enhancing knowledge, attitude, and behavior intentions regarding HIV/AIDS prevention among adolescents. Our findings indicate that these programs significantly improve knowledge, behavior, and attitude toward HIV/AIDS prevention. This improvement is in line with the studies from Iran [30] and India [68]. Moreover, the study by Angrist et al. [69] in Botswana showed that educational programs have the potential to enhance HIV knowledge by providing accurate information through interactive and participatory methods such as games, videos, discussions, and group activities [70,71]. These programs also foster self-confidence, self-awareness, and healthy lifestyle skills among adolescents [72]. Therefore, it is imperative to consistently implement and incorporate educational initiatives focused on HIV prevention into the school curricula [73,74].
Behavioral intentions are also positively influenced by educational programs, aligning with findings by Moeini et al. [75]. These programs aim to enhance positive behavioral intention by modifying and developing individual protection factors, such as self-efficacy and attitude intention, as well as sociocultural protection factors, such as communication and peer teaching [76-78]. Enhancing protection factors in school settings can be achieved through the implementation of novel learning and training approaches that are centered on curriculum, group dynamics, and technology [28,79,80]. It is crucial for health workers in educational institutions to incorporate this information into their programs to enhance behavioral intentions toward HIV prevention.
Furthermore, our review revealed that educational programs positively impact adolescents’ attitudes toward HIV prevention. This finding were consistent with the study by Thammaraksa et al. [81] in Thailand. The programs address misconceptions and promote positive behavior by offering accurate information, addressing personal beliefs and values, fostering a supportive school and peer environment, and promoting positive social norms [82]. Hence, educational programs can significantly enhance health behavior, as they are integrated into a holistic strategy that tackles several aspects influencing attitudes and behavior [35].
The effectiveness of educational programs is rooted in theoretical frameworks. A study by Siuki et al. [83] also used theoretical frameworks in the development of therapies. The educational programs often incorporated theories of health promotion, including the theory of reasoned action [84], social cognitive theory [85], the theory of planned action [86][87], REBT [88,89], and interactive learning theory [90]. These theories enhance knowledge and behavioral intention by emphasizing observational learning, the conviction that HIV/AIDS prevention behavior is secure, socially acceptable, and socially anticipated, and the ability to exert control and actively participate in HIV prevention behavior [91]. The educational program that implemented activities through the dissemination of information and the demonstration of behavior aimed to shape attitudes by influencing individuals’ perceptions of behavior and its outcomes. Additionally, it promotes healthier behavior by fostering positive intentions and perceived control over behavior [92]. Thus, incorporating these theoretical frameworks is crucial for developing interventions that effectively enhance HIV-related knowledge, attitudes, and behavior among adolescents in the context of HIV prevention [36,93].
Technology-based educational programs are particularly effective in increasing knowledge and behavior regarding HIV prevention, as demonstrated in a study conducted in KwaZulu-Natal, South Africa [94]. Adolescents exhibit a high acceptance of technology-based solutions due to their familiarity and proficiency with digital systems. These programs offer adaptability, accessibility, user-friendliness, and opportunities for peer connections and interaction, which facilitate optimal learning [95,96]. Furthermore, it is imperative to involve adolescents in the development of health-related technology applications as they have already benefited from digital technology [97]. Technology enables adolescents to engage in optimal learning at any time [98,99]. Therefore, when developing educational programs for adolescents, technology is the most effective tool.
Group-based educational programs are more effective than individual approaches in enhancing knowledge of HIV prevention. The programs promote interactive learning, exchange of experiences, and critical thinking [100], which are essential for a deeper comprehension of knowledge, attitudes, and behavior related to HIV/AIDS prevention [101]. Moreover, educational programs incorporating group discussions can foster critical thinking and encourage problem-solving skills from diverse perspectives among adolescents. Additionally, engaging in group study can offer social support and motivate individuals to modify their behavior [102]. Consequently, delivering HIV prevention education in a group setting is important.
Peer educators also play a crucial role in improving adolescents’ comprehension and disposition toward HIV prevention. This study is supported by the study conducted by Joorbonyan et al. [103] in Ramsar, Iran. Adolescents are more likely to engage with and trust information delivered by their peers, as peer educators are often more relatable and relevant to their experiences [104]. Information obtained from peers is often considered more credible and reliable [105]. Peer educators enhance their trustworthiness among adolescents by customizing the curriculum to be more relevant and applicable to the experiences of their peers [106]. Peer-led learning experiences provide robust emotional, informational, and material support, fostering a sense of community and mutual assistance, which can enhance the retention of knowledge [72]. Therefore, incorporating peer educators into HIV prevention programs is essential for effectively reaching and influencing adolescents.
Contrary to the findings of Jones et al. [107] and Okigbo et al. [108], our review suggests that parental participation may not have a significant positive impact on adolescents’ knowledge and behavior in HIV prevention. This phenomenon could be due to societal taboos surrounding sexual matters and HIV prevention, which might cause discomfort among adolescents during discussions related to these topics [109]. According to a study by Tolli [110], adolescents are more likely to share knowledge with their peers due to their shared origins, hobbies, and language usage. These similarities facilitate the exchange of information and helps develop good life skills. Therefore, while parental involvement is important, it should be approached with sensitivity and appropriate knowledge.
The utilization of animation, infographics, audio-visual materials, and brochures as educational tools has proven effective in enhancing adolescents’ knowledge and promoting behaviors related to HIV prevention. Research by Jeihooni et al. [80] in Fasa, Iran, demonstrates that these tools foster emotional connections, enabling youngsters to comprehend and retain educational messages. Educational content is presented in various formats, such as animation, infographics, audio-visual material, brochures, modules, and web-based or Android applications, captures attention, encourages interactivity, and effectively communicates complex messages [111,112]. To effectively engage the adolescent audience, it is crucial to create HIV teaching materials in formats such as animation, infographics, audio-visual materials, brochures, modules, and web-based or Android applications [113]. These tools offer a sense of ease and confidentiality for adolescents, who might feel ashamed or fearful about expressing their curiosity about this subject [114-116]. However, traditional teaching methods, such as lectures and presentations, remain effective due to their adaptability to adolescents’ learning preferences [117].
This study demonstrated that an increase in intervention duration has a positive correlation with the changes in adolescents’ attitudes and behaviors regarding HIV prevention, align with the findings of Siuki et al. [83]. Altering attitudes and behaviors is a sustained process influenced by various factors, including cultural, social, psychological, and adolescent behavioral aspects [118,119]. Ongoing educational efforts are necessary to foster substantial shifts in attitudes among adolescents toward HIV/AIDS prevention and to instill the necessary values and standards for engaging in preventative behaviors [120,121]. To facilitate the comprehension of potential hazards, repercussions, and suitable preventive measures, substantial behavioral modifications among adolescents necessitate ongoing engagement, participation, and interaction throughout any educational programming [23,122,123]. Longer-term interventions can effectively influence adolescents’ attitudes and behaviors regarding HIV prevention through the implementation of a comprehensive strategy, ongoing education, and consistent support. However, the efficacy of these interventions may depend on various variables, including the program’s content, delivery method, and the target population.
This review has several strengths. First, it employs Cochrane RoB 2.0 for systematic reviews and other risk assessment tools to avoid bias. Second, the study identified specific program aspects and characteristics that effectively increase knowledge, behavior, and attitudes in HIV prevention among adolescents. Third, because this meta-analysis focused on adolescents or students rather than active adults, the findings are valuable to professionals who focus on adolescents, particularly concerning health education strategies.
This study also has limitations. There was considerable heterogeneity among the included studies, which was addressed through subgroup analysis and meta-regression. Additionally, the individual studies showed an elevated risk of bias due to factors such as randomization procedures, deviation from the intervention, and outcome measurement. Future RCTs should provide comprehensive information regarding the randomization procedure to enhance the reliability of findings.
Conclusion
This meta-analysis suggests that educational programs can effectively improve knowledge, behavioral intention, and attitude in preventing HIV among adolescents. Studies with theory-based, curriculum-based, group-based models, providers in the form of peer educators, no parent involvement, and promotion tools with audio visuals in educational programs are more effective. These findings provide evidence that it is more effective to increase adolescents’ knowledge when they are in a group. Simultaneously, educational programs with peer educators trained in group-based are more effective. When creating educational programs, healthcare professionals must consider the factors that significantly influence knowledge, behavior, and attitude in preventing HIV.
Acknowledgments
The authors would like to thank the Center for Education Financial Services of the Ministry of Education, Culture, Research, and Technology of the Republic of Indonesia in collaboration with the Educational Fund Management Institution (Lembaga Pengelola Dana Pendidikan, LPDP) of the Ministry of Finance for offering doctoral scholarships to the first author through the Indonesian Education Scholarship (Beasiswa Pendidikan Indonesia, BPI); Universitas Indonesia and Universitas Pembangunan Nasional Veteran Jakarta for their academic support.
Ethics approval
Not required.
Competing interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
This study was funded by the Indonesian Education Scholarship (BPI) for the Postgraduate Program, provided by the Center for Education Financial Services of the Ministry of Education, Culture, Research, and Technology of the Republic of Indonesia in collaboration with the Educational Fund Management Institution (LPDP) of the Ministry of Finance. The recipient: Diah Ratnawati.
Underlying data
Derived data supporting the findings of this study are available from the corresponding author on request.
How to cite
Ratnawati D, Huda MH, Mukminin MA, et al. Meta-analysis of the effectiveness of educational programs about HIV prevention on knowledge, attitude, and behavior among adolescents. Narra J 2024; 4 (2): e870 - http://doi.org/10.52225/narra.v4i2.870.
References
- 1.Jones J, Sullivan PS, Curran JW. Progress in the HIV epidemic: Identifying goals and measuring success. PLoS Med 2019;16(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mayer KH, Pizer HF. HIV prevention: A comprehensive approach. London: Academic Press; 2009. [Google Scholar]
- 3.Sinulingga E, Waluyo A.. The role of the church members and nurses in improving self-awareness to prevent HIV. J Public Health Res 2021;10():69–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rudgard WE, Saminathen MG, Orkin M, et al. Protective factors for adolescent sexual risk behaviours and experiences linked to HIV infection in South Africa: A three-wave longitudinal analysis of caregiving, education, food security, and social protection. BMC Public Health 2023;23(1):1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.UNAIDS. Global HIV & AIDS statistics - Fact sheet 2023. 2023. Available from: https://www.unaids.org/en/resources/fact-sheet. Accessed: 21 February 2023.
- 6.Wongkongdech R, Chanthamath S, Wongkongdech A.. Knowledge, attitude and prevention behavior related to HIV/AIDS among students of a college in Lao-PDR: A cross-sectional study. F1000Research 2020;9:181. [Google Scholar]
- 7.Richard AK, Roland YK, Christian YK, et al. Knowledge, attitudes, and practices of HIV-positive adolescents related to HIV/AIDS prevention in Abidjan (Côte d’Ivoire). Int J Pediatr 2020;2020:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gong J, Saxena V, Mathur A, et al. HIV risk and prevention behaviours, intentions, perceptions and knowledge among youth in Goa, India. Int J STD AIDS 2010;21(6):392–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bastami F, Mostafavi F, Hassanzadeh A.. Effect of educational intervention on knowledge, perceived benefits, barriers and self-efficacy regarding AIDS preventive behaviors among drug addicts. J Educ Health Promot 2015;4:90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nigussie T, Mamo Y, Qanche Q, et al. HIV preventive behaviors and associated factors among gold mining eorkers in Dima District, Southwest Ethiopia, 2019: Community-based cross-sectional study. BioMed Res Int 2021;2021:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Somefun OD, Odimegwu C.. The protective role of family structure for adolescent development in Sub-Saharan Africa. PLoS One 2018;13(10):e0206197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agathis NT, Annor FB, Coomer R, et al. HIV prevention program eligibility among adolescent girls and young women — Namibia, 2019. MMWR Morb Mortal Wkly Rep 2021;70(45):1570–1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mirzazadeh A, Biggs MA, Viitanen A, et al. Do school-based programs prevent HIV and other sexually transmitted infections in adolescents? A systematic review and meta-analysis. Prev Sci 2018;19(4):490–506. [DOI] [PubMed] [Google Scholar]
- 14.Spoth R, Redmond C, Shin C, et al. PROSPER delivery of universal preventive interventions with young adolescents: Long-term effects on emerging adult substance misuse and associated risk behaviors. Psychol Med 2017;47(13):2246–2259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hill KG, Bailey JA, Hawkins JD, et al. The onset of STI diagnosis through age 30: Results from the Seattle social development project intervention. Prev Sci 2014;15(S1):19–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McCorkle R, Dowd M, Ercolano E, et al. Effects of a nursing intervention on quality of life outcomes in post-surgical women with gynecological cancers. Psychooncology 2009;18(1):62–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Raphaelis S, Kobleder A, Mayer H, et al. Effectiveness, structure, and content of nurse counseling in gynecologic oncology: A systematic review. BMC Nurs 2017;16(1):1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deaton A, Cartwright N.. Understanding and misunderstanding randomized controlled trials. Soc Sci Med 2018;210(1997):2–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gopalakrishnan S, Ganeshkumar P.. Systematic reviews and meta-analysis: Understanding the best evidence in primary healthcare. J Fam Med Prim Care 2013;2(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Amaugo LG, Papadopoulos C, Ochieng BMN, et al. The effectiveness of HIV/AIDS school-based sexual health education programmes in Nigeria: A systematic review. Health Educ Res 2014;29(4):633–648. [DOI] [PubMed] [Google Scholar]
- 21.Fauk NK, Kristanti E, Ratu M, et al. Effectiveness of school-based, Peer-led sexual health interventions in increasing STIS/HIV knowledge amongst adolescents: A systematic review. AcademiaEdu 2017;7(12):221–233. [Google Scholar]
- 22.Faust L, Yaya S.. The effect of HIV educational interventions on HIV-related knowledge, condom use, and HIV incidence in sub-Saharan Africa: A systematic review and meta-analysis. BMC Public Health 2018;18(1):1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fonner VA, Armstrong KS, Kennedy CE, et al. School based sex education and HIV prevention in lowand middle-income countries: A systematic review and meta-analysis. PLoS ONE 2014;9(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ibrahim S, Sidani S.. Community based HIV prevention intervention in developing countries: A systematic review. Adv Nurs 2014;2014:1–11. [Google Scholar]
- 25.Latifi A, Merghati-Khoei E, Shojaeizadeh D, et al. Theory-based interventions in STIs/HIV prevention: A systematic review of the literature in Iran. Med J Islam Repub Iran 2017;31(1):869–876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mumtaz GR, Hilmi N, Majed EZ, et al. Characterising HIV/AIDS knowledge and attitudes in the Middle East and North Africa: Systematic review and data synthesis. Glob Public Health 2020;15(2):275–298. [DOI] [PubMed] [Google Scholar]
- 27.Napierala Mavedzenge SM, Doyle AM, Ross DA. HIV prevention in young people in sub-Saharan Africa: A systematic review. J Adolesc Health 2011;49(6):568–586. [DOI] [PubMed] [Google Scholar]
- 28.Sani AS, Abraham C, Denford S, et al. School-based sexual health education interventions to prevent STI/HIV in sub-Saharan Africa: A systematic review and meta-analysis. BMC Public Health 2016;16(1):1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dadipoor S, Shahsavari S, Ghaffari M, et al. Iranian school students’ awareness of and attitude towards HIV/AIDS: A systematic review. Int J Adolesc Youth 2020;25(1):240–250. [Google Scholar]
- 30.Honarvar B, Jalalpour AH, Shaygani F, et al. Knowledge, attitudes, threat perception, and practices toward HIV/AIDS among youths in Iran: A health belief model-based systematic review. Shiraz E-Med J 2022;23(6):1–12. [Google Scholar]
- 31.Mwale M, Muula AS. Systematic review: A review of adolescent behavior change interventions [BCI] and their effectiveness in HIV and AIDS prevention in sub-Saharan Africa. BMC Public Health 2017;17(1):718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Protogerou C, Johnson BT. Factors underlying the success of behavioral HIV-prevention interventions for adolescents: A meta-review. AIDS Behav 2014;18(10):1847–1863. [DOI] [PubMed] [Google Scholar]
- 33.Samkange-Zeeb FN, Spallek L, Zeeb H.. Awareness and knowledge of sexually transmitted diseases (STDs) among school-going adolescents in Europe: A systematic review of published literature. BMC Public Health 2011;11(1):727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Medley A, Kennedy C, O’reilly K, et al. Effectiveness of peer education interventions for HIV prevention in developing countries: A systematic review and meta-analysis. AIDS Educ Prev 2009;21(3):181–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mohamadkhani Shahri L, Simbar M, Bagherinia M, et al. Effects of model-based educational interventions on promoting AIDS preventive behaviors in Iranian adolescents: A systematic review. J Pediatr Rev 2022;10(3):203–216. [Google Scholar]
- 36.Morales A, Espada JP, Orgilés M, et al. Interventions to reduce risk for sexually transmitted infections in adolescents: A meta-analysis of trials, 2008–2016. PLoS ONE 2018;13(6):e0199421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nugrahawati REPC, Hernayanti MR, Purnamaningrum YE, et al. Factors related to adolescent behavior towards HIV/AIDS prevention. Kesmas Natl Public Health J 2019;13(4):197. [Google Scholar]
- 38.Kim EJ, Park B, Kim SK, et al. A meta-analysis of the effects of comprehensive sexuality education programs on children and adolescents. Healthcare 2023;11(18):2511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lonczak HS, Abbott RD, Hawkins JD, et al. Effects of the Seattle social development project on sexual behavior, pregnancy, birth, and sexually transmitted disease outcomes by age 21 years. Arch Pediatr Adolesc Med 2002;156(5):438–447. [DOI] [PubMed] [Google Scholar]
- 40.Kirby D. The impact of schools and school programs upon adolescent sexual behavior. J Sex Res 2002;39(1):27–33. [DOI] [PubMed] [Google Scholar]
- 41.Oringanje C, Meremikwu MM, Eko H, et al. Interventions for preventing unintended pregnancies among adolescents. Cochrane Database Syst Rev 2016;2016(2):7–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lameiras-Fernández M, Martínez-Román R, Carrera-Fernández MV, et al. Sex education in the spotlight: What is working? Systematic review. Int J Environ Res Public Health 2021;18(5):2555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sawyer SM, Azzopardi PS, Wickremarathne D, et al. The age of adolescence. Lancet Child Adolesc Health 2018;2(3):223–228. [DOI] [PubMed] [Google Scholar]
- 44.World Health Organization/WHO. Adolescent health 2023. Available from: https://www.who.int/health-topics/adolescent-health/#tab=tab_1. Accessed: 11 March 2023.
- 45.Higgins JPT, Altman DG, Gøtzsche PC, et al. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ Online 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Higgins J, Sterne J, Savović J, et al. Revised cochrane risk of bias tool for randomized trials (RoB 2.0). Cochrane Database Syst Rev 2016;1(10):1–52. [Google Scholar]
- 47.Sterne JAC, Savović J, Page MJ, et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. The BMJ 2019;366:1–8. [DOI] [PubMed] [Google Scholar]
- 48.Borenstein M. Comprehensive meta-analysis software. In: Egger M, Higgins JPT, Smith GD, editors. Systematic reviews in health research: Meta-analysis in context. Third Edition. Ltd: John Wiley and Sons; 2022:535–548. [Google Scholar]
- 49.Begg CB, Mazumdar M.. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50(4):1088–1011. [PubMed] [Google Scholar]
- 50.Duval S, Tweedie R.. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000;56(2):455–463. [DOI] [PubMed] [Google Scholar]
- 51.Shi L, Lin L.. The trim-and-fill method for publication bias: Practical guidelines and recommendations based on a large database of meta-analyses. Medicine (Baltimore) 2019;98(23):e15987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bauman LJ, Watnick D, Silver EJ, et al. Reducing HIV/STI risk among adolescents aged 12 to 14 years: A randomized controlled trial of Project Prepared. Prev Sci 2021;22(8):1023–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ezegbe B, Eseadi C, Ede MO, et al. Efficacy of rational emotive digital storytelling intervention on knowledge and risk perception of HIV/AIDS among schoolchildren in Nigeria. Medicine (Baltimore) 2018;97(47):e12910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Farahani FK, Darabi F, Yaseri M.. The effect of theory-based HIV/AIDS educational program on preventive behaviors among female adolescents in Tehran: A randomized controlled trial. J Reprod Infertil 2020;21(3):194–206. [PMC free article] [PubMed] [Google Scholar]
- 55.Fiellin LE, Hieftje KD, Pendergrass TM, et al. Video game intervention for sexual risk reduction in minority adolescents: Randomized controlled trial. J Med Internet Res 2017;19(9):e314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kaufman CE, Whitesell NR, Keane EM, et al. Effectiveness of circle of life, an HIV-preventive intervention for American Indian middle school youths: A group randomized trial in a Northern Plains tribe. Am J Public Health 2014;104(6):e106–e112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kennedy SB, Atwood K, Harris AO, et al. Preliminary impacts of an HIV-prevention program targeting out-of-school youth in postconflict Liberia. Glob Pediatr Health 2018;5:2333794X18754452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mathews C, Eggers SM, Townsend L, et al. Effects of PREPARE, a multi-component, school-based HIV and intimate partner violence (IPV) prevention programme on adolescent sexual risk behaviour and IPV: Cluster randomised controlled trial. AIDS Behav 2016;20(9):1821–1840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lescano CM, Castillo HL, Calcano E, et al. Latino STYLE: Preliminary findings from an HIV prevention RCT among Latino youth. J Pediatr Psychol 2020;45(4):411–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Marsch LA, Guarino H, Grabinski MJ, et al. Comparative effectiveness of web-based vs. educator-delivered HIV Prevention for adolescent substance users: A randomized, controlled trial. J Subst Abuse Treat 2015;59:30–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nelson KM, Perry NS, Stout CD, et al. The young men and media study: A pilot randomized controlled trial of a community-informed, online HIV prevention intervention for 14-17-year-old sexual minority males. AIDS Behav 2021;26(2):569–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ofoegbu TO, Otu MS, Christopher I, et al. Impact of an educational digital storytelling intervention on HIV risk perception among Nigerian adolescents. J Int Med Res 2020;48(1):300060519854635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Peskin MF, Coyle KK, Anderson PM, et al. Replication of It’s Your Game…Keep It Real! in Southeast Texas. J Prim Prev 2019;40(3):297–323. [DOI] [PubMed] [Google Scholar]
- 64.Khezri M, Farokhzadian J, Nematollahi M, et al. HIV/AIDS prevention education: An effective tool for enhancing street children’s knowledge and attitude. A randomized controlled trial. Child Youth Serv Rev 2019;104:104351. [Google Scholar]
- 65.Khosravi N, Kolifarhood G, Shoghli A, et al. Effectiveness of peer education approach on improving HIV/AIDS related healthy behaviors among immigrant street children: A randomized controlled trial. Clin Epidemiol Glob Health 2018;6(3):115–121. [Google Scholar]
- 66.Volpe EM, Nelson LE, Kraus RA, et al. Adaptation and refinement of the HIV knowledge questionnaire for use with adolescent girls. J Assoc Nurses AIDS Care 2007;18(5):57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Dilorio C, Resnicow K, McCarty F, et al. Keepin’ It R.E.A.L.! Results of a mother-adolescent HIV prevention program. Nurs Res 2006;55(1):43–51. [DOI] [PubMed] [Google Scholar]
- 68.Bhagavathula AS, Clark CCT, Sharma R, et al. Knowledge and attitude towards HIV/AIDS in India: A systematic review and meta-analysis of 47 studies from 2010-2020. Health Promot Perspect 2021;11(2):148–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Angrist N, Matshaba M, Gabaitiri L, et al. Revealing a safer sex option to reduce HIV risk : A cluster-randomized trial in Botswana. BMC Public Health 2019;19(610):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Thongnopakun S, Pumpaibool T, Somrongthong R.. The effects of an educational program on knowledge, attitudes and intentions regarding condom and emergency contraceptive pill use among Thai female university students. J Health Res 2018;32(4):270–278. [Google Scholar]
- 71.Lys CL, Logie CH, Okumu M.. Pilot testing Fostering Open eXpression among Youth (FOXY), an arts-based HIV/STI prevention approach for adolescent women in the Northwest Territories, Canada. Int J STD AIDS 2018;29(10):980–986. [DOI] [PubMed] [Google Scholar]
- 72.Saul J, Bachman G, Allen S, et al. The DREAMS core package of interventions: A comprehensive approach to preventing HIV among adolescent girls and young women. PLOS ONE 2018;13(12):e0208167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mensch BS, Grant MJ, Soler-Hampejsek E, et al. Does schooling protect sexual health? The association between three measures of education and STIs among adolescents in Malawi. Popul Stud 2020;74(2):241–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Isworo TA, Susanto T, Rokhmah D.. Dating behaviour and its associated factors among female adolescents in Indonesia: A school-based survey. J Keperawatan Soedirman 2020;15(3). [Google Scholar]
- 75.Moeini B, Hazavehei SMM, Zareban I, et al. Effectiveness of an educational program based on the theory of planned behavior for improving safe sexual behaviors intention among addicted males: A quasi experimental study. Int J High Risk Behav Addict 2017;6(2). [Google Scholar]
- 76.Timol F, Vawda MY, Bhana A, et al. Addressing adolescents’ risk and protective factors related to risky behaviours: Findings from a school-based peer-education evaluation in the Western Cape. SAHARA-J J Soc Asp HIVAIDS 2016;13(1):197–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Abbaspour A, Jalili Z, Shojaeizadeh D.. Study the effect of education based on the theory of planned behavior in the prevention of AIDS among addicts. Iran J Health Educ Health Promot 2021;9(2):201–211. [Google Scholar]
- 78.Xu T, Tomokawa S, Gregorio ER, et al. School-based interventions to promote adolescent health: A systematic review in low- and middle-income countries of WHO Western Pacific Region. PLOS ONE 2020;15(3):e0230046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Vaughn LM, Whetstone C, Boards A, et al. Partnering with insiders: A review of peer models across community-engaged research, education and social care. Health Soc Care Community 2018;26(6):769–786. [DOI] [PubMed] [Google Scholar]
- 80.Jeihooni AK, Moradi A, Yari A, et al. The effect of educational intervention based on theory of planned behavior on mothers’ skills in sexual care of children. BMC Public Health 2022;22(1):1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Thammaraksa P, Powwattana A, Lagampan S, et al. Effects of school-based participation program to prevent multiple risk behaviors in Thai male adolescents. Pac Rim Int J Nurs Res 2019;23(3):228–242. [Google Scholar]
- 82.Lestari WAE, Indarwati R, Krisnana I, et al. A model of self-regulation in preventing risk sexual behavior among adolescents. Int J Public Health Sci IJPHS 2023;12(3):989. [Google Scholar]
- 83.Siuki HA, Peyman N, Vahedian-Shahroodi M, et al. Health education intervention on HIV/AIDS prevention behaviors among health volunteers in healthcare centers: An applying the theory of planned behavior. J Soc Serv Res 2019;45(4):582–588. [Google Scholar]
- 84.Jemmott LS, Jemmott JB, Ngwane Z, et al. “Let Us Protect Our Future” a culturally congruent evidenced-based HIV/STD risk-reduction intervention for young South African adolescents. Health Educ Res 2014;29(1):166–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Li X, Zhang L, Mao R, et al. Effect of social cognitive theory-based HIV education prevention program among high school students in Nanjing, China. Health Educ Res 2011;26(3):419–431. [DOI] [PubMed] [Google Scholar]
- 86.Visser M. Rethinking HIV-prevention for school-going young people based on current behaviour patterns. SAHARA-J J Soc Asp HIVAIDS 2017;14(1):64–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Jemmott JB, O’Leary A, Jemmott LS, et al. Effect of a behavioral intervention on perpetrating and experiencing forced sex among South African adolescents. JAMA Netw Open 2018;1(4):e181213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Onyechi KCN, Eseadi C, Okere AU, et al. Effects of Rational-emotive health education program on HIV risk perceptions among in-school adolescents in Nigeria. Medicine (Baltimore) 2016;95(29):e3967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Musindo O, Jafry S, Nyamiobo J, et al. Mental health and psychosocial interventions integrating sexual and reproductive rights and health, and HIV care and prevention for adolescents and young people (10-24 years) in sub-Saharan Africa: a systematic scoping review. eClinicalMedicine 2023;57:101835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Harper GW, Muthigani A, Neubauer LC, et al. The development and evaluation of a national school-based HIV prevention intervention for primary school children in Kenya. J HIV AIDS 2018;4(1):1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ashrafi E, Kasmaei P, Mehrabian F, et al. The effect of educational program based on the theory of planned behavior on HIV prevention skills. HIV AIDS Rev 2020;19(3):180–186. [Google Scholar]
- 92.Speizer IS, Xiong K, Mandal M, et al. HIV-Related Knowledge, Attitudes, and Behaviors among Grade 10 Girls and Boys in Mpumalanga and KwaZulu-Natal: Cross-Sectional Results. Open AIDS J 2020;14(1):75–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mpeta KN, Moroke ND, Gabaitiri L.. Explicating factors that explain condom use intention among in-school adolescents in Botswana: A structural equation modelling approach. Sahara J 2021;18(1):156–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chamane N, Ebenezer Ogunsakin R, Mashamba-Thompson TP. The effect of a mobile-learning curriculum on improving compliance to quality management guidelines for HIV rapid testing services in rural primary healthcare clinics, KwaZulu-Natal, South Africa: a quasi-experimental study. BMC Health Serv Res 2022;22(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Visser M, Kotze M, van Rensburg MJ. An mHealth HIV prevention programme for youth: lessons learned from the iloveLife.mobi programme in South Africa. AIDS Care - Psychol Socio-Med Asp AIDSHIV 2020;32 Suppl 2:148–154. [DOI] [PubMed] [Google Scholar]
- 96.Sharma A, Mwamba C, Ng’andu M, et al. Pilot implementation of a user-driven, web-based application designed to improve sexual health knowledge and communication among young Zambians: Mixed methods study. J Med Internet Res 2022;24(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Crowley T, Petinger C, van Wyk B.. Effectiveness, acceptability, and feasibility of technology-enabled health interventions for adolescents living with HIV in low- and middle-income countries: A systematic review protocol. PLoS ONE 2023;18(2):e0281894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Hou SI. Evaluating online courses via course-related competencies – A mixed-methods quasi-experiment evaluation study of an HIV prevention webcourses among college students. J Scholarsh Teach Learn 2020;20(1):22–39. [Google Scholar]
- 99.Calisane NNP, Yosep I, Lindayani L, et al. The effect of mobile application on HIV preventive behavior among adolescent in Indonesia. Malays J Med Health Sci 2022;18 Suppl 17:197–202. [Google Scholar]
- 100.Rohrbach LA, Donatello RA, Moulton BD, et al. Effectiveness evaluation of It’s Your Game: Keep It Real, a middle school HIV/sexually transmitted infection/pregnancy prevention program. J Adolesc Health 2019;64(3):382–389. [DOI] [PubMed] [Google Scholar]
- 101.Kemigisha E, Bruce K, Ivanova O, et al. Evaluation of a school based comprehensive sexuality education program among very young adolescents in rural Uganda. BMC Public Health 2019;19(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Kemigisha E, Ivanova O, Ruzaaza GN, et al. Process evaluation of a comprehensive sexuality education intervention in primary schools in South Western Uganda. Sex Reprod Healthc 2019;21:51–59. [DOI] [PubMed] [Google Scholar]
- 103.Joorbonyan H, Ghaffari M, Rakhshanderou S.. Peer-led theoretically Desinged HIV/AIDS prevention intervention among students: A case of health belief model. BMC Public Health 2022;22(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Mahat G, Scoloveno MA. Effectiveness of adolescent peer education programs on reducing HIV/STI risk: An Integrated review. Res Theory Nurs Pract 2018;32(2):168–198. [DOI] [PubMed] [Google Scholar]
- 105.Wolf K, Africa A.. ‘Now that I’m pregnant, I’m no longer an example’: peer educator experiences of an HIV prevention programme in Cape Town, South Africa. Sex Educ 2017;17(4):425–439. [Google Scholar]
- 106.Menna T, Ali A, Worku A.. Effects of peer education intervention on HIV/AIDS related sexual behaviors of secondary school students in Addis Ababa, Ethiopia: A quasi-experimental study. Reprod Health 2015;12(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Jones V, Modeste N, Hopp Marshak H, et al. The Effect of HIV/AIDS education on adolescents in Trinidad and Tobago. ISRN Infect Dis 2013;2013:1–8. [Google Scholar]
- 108.Okigbo CC, Kabiru CW, Mumah JN, et al. Influence of parental factors on adolescents’ transition to first sexual intercourse in Nairobi, Kenya: A longitudinal study. Reprod Health 2015;12(1):73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Tolli M V. Effectiveness of peer education interventions for HIV prevention, adolescent pregnancy prevention and sexual health promotion for young people: A systematic review of European studies. Health Educ Res 2012;27(5):904–913. [DOI] [PubMed] [Google Scholar]
- 110.Mkandawire IN, Iipinge SN. An exploratory study of parent-adolescent communication on sexual issues and HIV prevention, at Otjomuise Clinic, Namibia. J Community Public Health Nurs 2018;04(01):1–7. [Google Scholar]
- 111.Shabiralyani G, Hasan KS, Hamad N, et al. Impact of visual aids in enhancing the learning process case research: District Dera Ghazi Khan. J Educ Pract 2015;6(19):226–233. [Google Scholar]
- 112.Cardillo N. Visual aids supporting the learning of children in our classrooms. In: Geng G, Smith P, Black P, editors. The Challenge of Teaching. Singapore: Springer Singapore; 2017. 145–150. [Google Scholar]
- 113.Chory A, Nyandiko W, Beigon W, et al. Perspectives of education sector stakeholders on a teacher training module to reduce HIV/AIDS stigma in Western Kenya. BMC Public Health 2021;21(1):1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Harris JM. Knowledge, behavior, and attitudes of college students regarding HIV/AIDS. Available from: https://fisherpub.sjf.edu/education_etd/430/. Accessed: 5 April 2023.
- 115.Radovic A, Badawy SM. Technology use for adolescent health and wellness. Pediatrics 2020;145 Suppl 2:S186–S194. [DOI] [PubMed] [Google Scholar]
- 116.Rashedi RN, Bonnet K, Schulte RJ, et al. Opportunities and challenges in developing technology-based social skills interventions for adolescents with autism spectrum disorder: A qualitative analysis of parent perspectives. J Autism Dev Disord 2022;52(10):4321–4336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Chokprajakchad M, Phuphaibul R, Sieving RE. Sexual health interventions among early adolescents: An integrative review. J Health Res 2018;32(6):467–477. [Google Scholar]
- 118.Tung WC, Lu M, Rull R, et al. Pilot test results of a video-based HIV intervention for Chinese college students in the United States. J Public Health Emerg 2017;1:84–84. [Google Scholar]
- 119.Fernandez MI, Harper GW, Hightow-Weidman LB, et al. Research priorities to end the adolescent HIV epidemic in the United States: Viewpoint. JMIR Res Protoc 2021;10(1):e22279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Pillay K, Gardner M, Gould A, et al. Long term effect of primary health care training on HIV testing: A quasi-experimental evaluation of the Sexual Health in Practice (SHIP) intervention. PLOS ONE 2018;13(8):e0199891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Jadgal MS, Heshmati H, Keshavarz M, et al. Effect of theory of planned behavior-based educational intervention on HIV/AIDS preventive behaviors among male barbers. HIV AIDS Rev 2023;22(1):77–83. [Google Scholar]
- 122.Kinsler J. Evaluation of a school-based intervention for HIV/AIDS prevention among Belizean adolescents. Health Educ Res 2004;19(6):730–738. [DOI] [PubMed] [Google Scholar]
- 123.Mash R, Mash RJ. A quasi-experimental evaluation of an HIV prevention programme by peer education in the Anglican Church of the Western Cape, South Africa. BMJ Open 2012;2(2):e000638. [DOI] [PMC free article] [PubMed] [Google Scholar]