RESUME
Introduction: La prise en charge de l’hypertension pulmonaire (HTP) ne peut se concevoir que dans un centre spécialisé. L’objectif de la présente étude était de rapporter l’expérience d’un service de réanimation tunisien en matière d’exploration hémodynamique invasive de l’HTP et de décrire les décisions thérapeutiques qui en découlent. Méthodes: Il s’agissait d’une étude descriptive rétrospective incluant tous les patients admis au service de réanimation médicale de l’hôpital Abderrahmen Mami pour un cathétérisme cardiaque droit, entre 2005 et 2019, dans le cadre de l’exploration de l’HTP. Les caractéristiques des patients, l’innocuité de la procédure et les décisions thérapeutiques qui en découlent ont ensuite été rapportées.Résultats: Quarante patients ont été admis pour une évaluation hémodynamique. Le cathétérisme cardiaque droit a confirmé l’HTP chez 31 patients et l’exploration a été complétée par un test de vasoréactivité au NO. L’âge moyen était de 41,3±15 ans, le genre-ratio H/F de 1,06. L’HTP a été classée en : groupe 1 (n=13), groupe 2 (n=14), groupe 4 (n=2) et groupe 5 (n=2). Le test de vasoréactivité au NO était positif dans 50% des HTP post-capillaires et dans 28% des HTP pré-capillaires. La décision thérapeutique suite au test de réversibilité était : prescription d’inhibiteurs calciques (n=5), d’un vasodilatateur pulmonaire spécifique (n=10), l’opérabilité (n=6), la transplantation coeur-poumon (n=3) et l’abstention thérapeutique (n=7). Deux complications mineures ont été rapportées.Conclusion: Le service de réanimation médicale de l’hôpital Abderrahmen Mami dispose d’une équipe expérimentée en matière d’investigations hémodynamiques, en dépit du faible nombre annuel de cathétérisme cardiaque droit. Le test de réactivité au NO est un outil indispensable qui permet de prendre des décisions importantes au cours de la gestion de l’HTP.
ABSTRACT
INTRODUCTION: Pulmonary hypertension (PH) management can only be conceived in a specialized center. We aimed to report the experience of a Tunisian ICU about PH invasive hemodynamic exploration and to describe consequent therapeutic decisions. METHODS: Retrospective descriptive study including all patients admitted to the medical ICU of Abderrahmen Mami Hospital for right heart catheterization (RHC), between 2005 and 2019 as part of the investigation of PH. Patients' characteristics, procedure safety and arising therapeutic decisions were then reported. RESULTS: Forty patients were admitted for hemodynamic evaluation. RHC confirmed PH in 31 patients and exploration was then completed with NO reactivity test. Mean age was 41.3±15 years, gender ratio M/F was 1.06. PH was classified into: group 1 (n=13), group 2 (n=14), group 4 (n=2) and group 5 (n=2). NO vasoreactivity test was positive in 50% of post-capillary PH and in 28% of pre-capillary PH. The therapeutic decision following the reversibility test was: prescription of calcium channel blockers (n=5), a specific pulmonary vasodilator (n=10), operability (n=6), heart-lung transplant (n=3) and therapeutic abstention (n=7). Two minor complications were reported. CONCLUSION: The medical ICU in Abderrahmen Mami Hospital represents an experienced team in hemodynamic investigations despite low annual RHC number. NO reactivity test is an indispensable tool that enables important decisions during PH management.
introduction
Pulmonary arterial hypertension (PAH) is a rare pulmonary vascular disease, with an estimated worldwide prevalence of 1% in adults [1] .
It is a serious condition, which can be life-threatening and functionally challenging for patients in the short and long term.
From a pathophysiological point of view, PAH etiologies are multiple and it can complicate the majority of cardiovascular and respiratory diseases [2] .
As a result, its management can only be conceived within the framework of a specialized reference center.
In this regard, several recommendations have been made regarding the criteria that should be met by a PH reference center [2].
In Tunisia, there is no reference center of PAH management yet, nor national register gathering PAH patients’ data.
Since descriptive statistics in biomedical research are of vital importance [3], reporting a description of this rare condition is useful.
Through the experience of the medical ICU of a pulmonology hospital in Tunisia, we aimed to describe our invasive hemodynamic exploration activity; then we proposed to study the challenges encountered in the process of acquiring competence in order to make Abderrahmen Mami hospital a reference center in the management of PAH.
methods
Setting:
The Abderrahmen Mami Hospital of pulmonology is a teaching center located in the governorate of Ariana, in northern Tunisia.
It is a university hospital specialized in pulmonary and thoracic pathologies (formerly known as the hospital of pneumo-phtysiology), with a capacity of 320 beds, comprising different services: 7 pulmonology departments with different sub-specialties (pediatrics, allergology, multi-resistant tuberculosis, interventional endoscopy, oncology...), interventional cardiology, thoracic surgery, cardiovascular surgery, surgical anesthesia-intensive care, medical imaging, microbiology, biochemistry, anatomopathology, occupational medicine, medical carcinology, radiotherapy, and medical ICU.
The medical ICU department is 22-bed ward with a respiratory valence.
It also carries out invasive hemodynamic explorations at the request of other departments of the hospital as well as other hospitals or private specialists all over the country.
Study design:
We conducted a retrospective descriptive study from 2005 until 2019, including all patients diagnosed with PAH in pulmonology or cardiology departments and admitted to the ICU for right heart catheterization (RHC) and NO vasoreactivity test.
Exclusion criteria were: unconfirmed PAH with the RHC, failure of RHC and suspected right atrial thrombosis.
We aimed to describe hemodynamic profile of PAH among these patients.
Procedure:
Approval for transfer to the ICU is given only after checking the contraindications of the RHC.
For patients receiving oral anticoagulants, overlap with heparin is carried out upstream (in the department of origin) to minimize the duration of admission to the ICU.
The patient is admitted to the ICU after verification of his medical file: a transthoracic echography (TTE) performed by an experienced cardiologist showing an elevated PAPs, and possible contraindications, notably haemostasis disorders.
After explaining the procedure to the patient, the RHC is performed by inserting a Swan Ganz probe via direct puncture of the right jugular vein after local anesthesia (Figure 1).
Figure 1. Puncture of the right jugular vein .

puncture of the right jugular vein after local anesthesia (Figure 1).
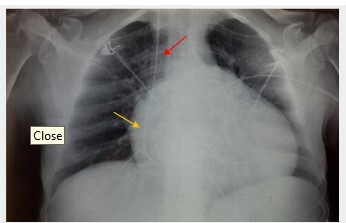
The correct positioning of the catheter is guided by the appearance of the curves obtained on the scope (Figure 2) and confirmed by a chest X-ray (Figure 3)
Figure 2. Wedge PAOP indicating catheter positioning in the pulmonary artery .
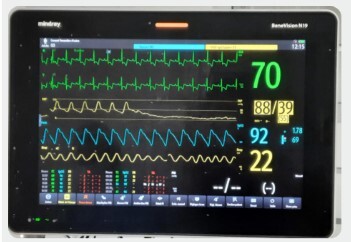
Figure 3. Chest X-ray imaging showing Swan Ganz introduced through right jugular vein (red arrow) with distal tip positioned in the right pulmonary artery (yellow arrow) .
An initial haemodynamic assessment is carried out with measurement of cardiac output, PAP, PAPO, pulmonary and systemic resistances.
If the PAP value is really pathological, the vasoreactivity test is started.
Vasoreactivity test is performed with inhaled Nitrogen Monoxide (NO).
NO administration was performed under noninvasive ventilation.
The starting dose was 5ppm and was progressively augmented towards 20ppm
Measures were performed each 5ppm.
At the end of all haemodynamic measurements, patients with confirmed PH were classified according to the 2015 ESC/ERS classification [2].
Statistical study:
Statistical analysis was carried out with the SPSS version 23 statistical analysis software.
Quantitative variables were expressed as mean ± standard deviation or median (IQR) if their distribution did not follow a normal distribution.
Qualitative variables were expressed as numbers (frequencies and percentages).
Ethical considerations:
This was a retrospective review of patient records referred for haemodynamic testing as part of their management.
Patient data were anonymized.
Such studies do not require prior approval of the ethics committee in our institution.
The authors declare that they have no conflicts of interest.
results
During the study period, 40 patients were admitted to the ICU for RHC and NO reversibility testing, with an average of 2.66 patients per year.
Transferring wards were as follow: Cardiology (55 %), Pulmonology (25 %), cardiovascular surgery (15 %), Internal medicine (2.5%) and ICU (2.5 %).
RHC was performed for all patients, and then 9 were excluded: mPAP value at RHC was normal and reversibility test was therefore not performed (n=7); catheter insertion failure: pulmonary valve stenosis (n=1) and catheter coiling in the right ventricle due to ecstatic right cavities(n=1).
Figure 4. Inclusion flowchart .
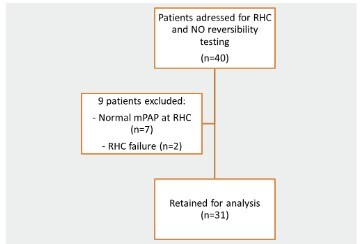
Included patients (n=31) were divided into 16 men (52%)and 15 women (48%), making a gender-ratio M/F of 1.06; with an average age of 41.5±15 years [19 - 76].
All of them had dyspnea at baseline, with mMRC stage classification of 1 (n=4; 13%), 2 (n=6; 19%), 3 (n=17; 55%) and 4 (n=4; 13%).
The history and baseline status of the patients were detailed in Table 1.
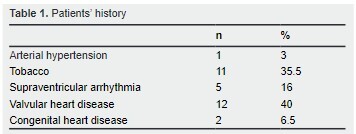
Valvular heart diseases were: mitral stenosis (n=3), aortic stenosis (n=1), mitral regurgitation (n=1), combined and multiple valve disease (n=7).
Congenital heart diseases were ventricular septal defect (n=2).
On admission, median SAPS II score was 13 IQR [6.5 - 18] and median APACHE II score was 3 IQR [1 - 4.5].
Clinical signs of right heart failure were present in 14 patients (45%).
All patients had undergone TTE prior to admission to ICU, showing high PAPs in all cases.
The mean PAPs on TTE were 87 ± 18.5 [55 - 140] mmHg.
RHC was performed in all cases via the right jugular vein(n=31), followed by NO reactivity testing.
The whole procedure was completely safe in 29 patients.
Complications were recorded in 2 cases: pneumothorax complicating jugular puncture (n=1) and hypotension requiring dobutamine after NO introduction (n=1).
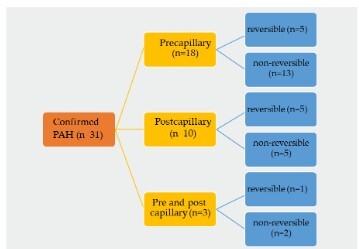
In the light of haemodynamic findings and anamnestic features, PH was confirmed in 31 patients and classified as follows: (Figure 5).
Figure 5. Patients’ classification according to ESC guidelines .
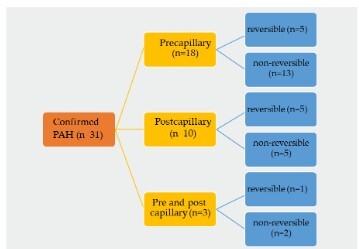
The reversibility of PAH according to the haemodynamic profile was illustrated in figure 6. The percentage of reversibility was 50% in the group of patients with postcapillary PAH and 28% in those with pre-capillary PAH.
Figure 6. Reversibility according to PAH type .
At the end of the exploration, the reactivity test allowed a therapeutic decision to be made of: Calcium channel blockers (n= 5), Specific pulmonary vasodilators (n= 10), Operability of heart disease (n= 6), To propose for heartlung transplantation proposition (n= 3), and Therapeutic abstention (n= 7).
discussion
To the best of our knowledge, this is the first cases series of PAH hemodynamic exploration in Tunisia.
Mainly, this study shows that requests for RHC most often come from cardiology departments, and that hemodynamic exploration often enables mandatory decisions to be taken.
Investigated patients for PAH were young with an average age of 41.5 years, without any gender predominance.
These results are similar to the data reported in an Egyptian series, where a mean age of 43.9±13.69 years was reported.
Nevertheless, a female predominance of 72.7%, as well as in the Giessen registry in Germany and the ASPIRE registry in the United Kingdom, 58.94% and 62% respectively, was mostly reported (4-6 ).
In the present study, the patients had quite disabling dyspnea at the time of exploration. It was mostly class 3 according to mMRC/NYHA.
As in the Egyptian series, dyspnea was grade III in 60.6%, grade II in 28.7% and grade IV in 10.7%.
These data are similar to those found in the ASPIRE and Giessen registries, with grade III dyspnea in 65% of cases.
In contrast, grade IV dyspnea was reported in 16% and 22% of cases respectively in both registries 5, 6 .
According to the ESC/ERS 2015 classification [2], group 2 PAH secondary to left heart disease was predominant with 14 patients (45%), followed by group 1 PH with 13 patients (42%), of which 11 were idiopathic (36%)
Two patients had group 4 post-embolic PH (6.5%).
In the same Egyptian series, the most frequent group was group 1 PH (57.5%), followed by group 4 post-embolic PH (22.7%), then group 3 (18.3%).
PH in group 2 was the least frequent group with 15%.
The authors explained these results by the fact that these patients were usually diagnosed and managed by cardiologists and were not referred to the study center 4.
At the time of the first hemodynamic investigation, pulmonary vasoreactivity tests should be performed, in order to better classify PAH and determine the subsequent therapeutic strategy or decide on operability in case of heart disease [7].
In our series, the percentage of reversibility was 50% in the group of patients with post- capillary PAH and 28% in those with pre-capillary PAH.
Based on the reactivity test, five patients were put on calcium channel blockers and 10 patients on specific pulmonary vasodilators.
Cardiac surgery was possible in 6 cases and heart-lung transplantation was proposed in 3 cases
RHC can be a difficult procedure in patients with PH and requires expertise, attention to detail and meticulous data collection 7
In patients with PAH, RHC has been associated with serious, life-threatening complications.
In a multicenter study evaluating adverse events of RHC in PAH patients, including experienced centers in Europe and the United States 8, out of 7218 investigations performed, the total number of serious adverse events was 76 (1.1%), with four deaths and a procedure-related mortality of 0.055%..
Furthermore, the most frequent complications were related to venous access, followed by arrhythmias and hypotensive episodes related to vasoreactivity testing.
The majority of complications was mild to moderate and resolved spontaneously or after appropriate intervention ( 8 ).
In our series, complications were recorded in 2 cases.
The jugular puncture was complicated with a pneumothorax in 1 case and the use of NO was complicated with hypotension requiring dobutamine in 1 other case.
In order to obtain accurate and reproducible information and to minimize the risks associated with the procedure, RHC should be limited to specialized centers and operators with training and expertise in hemodynamic exploration and PH ( 8 ).
Although the number of investigated patients was low (2.66/year), ICU team was enough trained and the procedure was safe.
In reality, the number of test requests we receive far exceeds this figure.
There are 2 main obstacles often encountered to explain this low number.
First, there is no area specifically dedicated to PAH exploration, so we have to occupy an ICU bed to do it.
This is not always possible due to the high demand for critically ill patients.
Second, Swan Ganz catheters are both costly and not consistently available.
Thus, this low annual number of explored patients represents one of our hospital’s shortcomings in becoming a PAH reference center
In this respect, several recommendations have been made concerning the definition of a center of expertise in the management of PAH.
According to the 2015 ESC/ERS recommendations ( 2 )
the aim of an expert referral center is to receive new referrals and undertake assessment and investigation of all causes of PAH, regularly manage appropriate patients with specific drug therapies for PAH, work closely with other healthcare providers to achieve the best outcomes for patients, and undertake audit, research and teaching activities
Thus, according to the same recommendations, the ideal number of patients seen by an adult center each year should be at least 200, at least half of whom have a definitive diagnosis of PAH ( 2 ).
The facilities and skills required for an expert reference center according to the same recommendations can be provided 2 , 9 - 14 .
Thus, it is recommended that expert centers provide care by a multidisciplinary team which should, at a minimum, include: 2 experienced consultant physicians (usually in cardiology and respiratory medicine) with a special interest in PAH, participating in a dedicated PH outpatient clinic for outpatients, inpatients and a multidisciplinary team meeting 2 .
These centers should also have: a clinical nurse specialist, a radiologist with expertise in pulmonary hypertension imaging, a cardiologist or doctor with expertise in echocardiography, a cardiologist or doctor with expertise in RHC and vasoreactivity testing, access to psychological and social support and an on-call activity with adequate expertise [ 2 ].
The condition of multidisciplinarity is well met by Abderrahmen Mami hospital, which is a multidisciplinary university structure, with a research vocation, that concentrates doctors with expertise in the management of thoracic pathologies, notably pneumologists, cardiologists and radiologists.
Multidisciplinary meetings already exist in Abderrahmen Mami hospital; they are regular and weekly for cancerous pathologies and diffuse infiltrating pneumonia management.
If necessary, difficult cases in any specialty are open to debate with local experts.
Therefore, even though there is currently no dedicated PAH consultation meeting, its implementation will not be a problem due to the established culture of multidisciplinary management.
Our study has several limits.
Mainly, it is the low sample size, although the reasons have already been discussed above.
Then, since the medical ICU only provides hemodynamic exploration, we don’t dispose of follow-up data for these patients, especially as no national or local PAH register exists.
conclusion
All the scientific and academic societies agree on the fact that the management of PAH can only be conceived within the framework of an expert center of reference, in order to guarantee a better management as well as a rationalization of the resources.
The medical ICU ward of Abderrahmen Mami Ariana has an experienced team in hemodynamic explorations.
However, the acquisition of expertise remains mainly slowed down not only by the low number of patients taken in charge, but also by the nonavailability of the whole therapeutic arsenal necessary.
However, some determinants of a center of expertise exist,in particular the presence of specialist practitioners in resuscitation, cardiology, thoracic imaging, pulmonology and surgery.
The acquisition of expertise cannot be conceived on the scale of a department, but of an entire hospital with the sharing of the various material resources available, to reduce costs while guaranteeing quality care according to international recommendations.
References
- Hoeper MM, Humbert M, Souza R, Idrees M, Kawut SM, Sliwa-Hahnle K, et al. A global view of pulmonary hypertension. Lancet Respir Med. 2016;4:306–322. doi: 10.1016/S2213-2600(15)00543-3. [DOI] [PubMed] [Google Scholar]
- Galiè N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, et al. ESC Scientific Document Group. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT) Eur Heart J. 2016;37:67–119. doi: 10.1093/eurheartj/ehv317. [DOI] [PubMed] [Google Scholar]
- Ben Abdelaziz A, Ben Hassine D, Chebil D, Nouira S, Ben Abdelaziz A, Melki S, Barhoumi T, Ben Salem K. Descriptive Statistics in Health Sciences. Tunis Med. 2021 DéCembre;99(12):1117–1125. English. [PMC free article] [PubMed] [Google Scholar]
- Elshazly M, Mostafa AI, Ibrahim A, Sabry IM. Assessing the spectrum of pulmonary hypertension identified at an Egyptian expert referral center. Egypt J Bronchol. 2021;15:48. [Google Scholar]
- Hurdman J, Condliffe R, Elliot CA, Davies C, Hill C, Wild JM, Capener D, et al. ASPIRE registry: Assessing the spectrum of pulmonary hypertension identified at a referral centre. Eur Respir J. 2012;39:945–955. doi: 10.1183/09031936.00078411. [DOI] [PubMed] [Google Scholar]
- Gall H, Felix JF, Schneck FK, Milger K, Sommer N, Voswinckel R, et al. The Giessen Pulmonary Hypertension Registry: Survival in pulmonary hypertension subgroups. J Heart Lung Transplant. 2017;36:957–967. doi: 10.1016/j.healun.2017.02.016. [DOI] [PubMed] [Google Scholar]
- D’Alto M, Dimopoulos K, Coghlan JG, Kovacs G, Rosenkranz S, Naeije R. Right Heart Catheterization for the Diagnosis of Pulmonary Hypertension: Controversies and Practical Issues. Heart Fail Clin. 2018;14:467–477. doi: 10.1016/j.hfc.2018.03.011. [DOI] [PubMed] [Google Scholar]
- Hoeper MM, Lee SH, Voswinckel R, Palazzini M, Jais X, Marinelli A, et al. Complications of right heart catheterization procedures in patients with pulmonary hypertension in experienced centers. J Am Coll Cardiol. 2006;48:2546–2552. doi: 10.1016/j.jacc.2006.07.061. [DOI] [PubMed] [Google Scholar]
- British Cardiac Society Guidelines and Medical Practice Committee, and approved by the British Thoracic Society and the British Society of Rheumatology Recommendations on the management of pulmonary hypertension in clinical practice. Heart. 2001;86(Suppl 1):I1–I13. [PMC free article] [PubMed] [Google Scholar]
- National Pulmonary Hypertension Centres of the UK and Ireland Consensus statement on the management of pulmonary hypertension in clinical practice in the UK and Ireland. Thorax. 2008;63(Suppl 2):ii1–ii41. doi: 10.1136/thx.2007.090480. [DOI] [PubMed] [Google Scholar]
- Barberà JA, Escribano P, Morales P, Gómez MA, Oribe M, Martínez A, et al. Estándares asistenciales en hipertensión pulmonar. Documento de consenso elaborado por la Sociedad Española de Neumología y Cirugía Torácica (SEPAR) y la Sociedad Española de Cardiología (SEC) [Standards of care in pulmonary hypertension. Consensus statement of the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR) and the Spanish Society of Cardiology (SEC)]. Rev Esp Cardiol. 2008;61:170–184. Spanish. [PubMed] [Google Scholar]
- Armstrong I, Rochnia N, Harries C, Bundock S, Yorke J. The trajectory to diagnosis with pulmonary arterial hypertension: a qualitative study. BMJ Open. 2012;2:e000806. doi: 10.1136/bmjopen-2011-000806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghofrani HA, Distler O, Gerhardt F, Gorenflo M, Grünig E, Haefeli WE, et al. Treatment of pulmonary arterial hypertension (PAH): updated Recommendations of the Cologne Consensus Conference 2011. Int J Cardiol. 2011;154(Suppl 1):S20–S33. doi: 10.1016/S0167-5273(11)70490-9. [DOI] [PubMed] [Google Scholar]
- Vachiéry JL, Gaine S. Challenges in the diagnosis and treatment of pulmonary arterial hypertension. Eur Respir Rev. 2012;21:313–320. doi: 10.1183/09059180.00005412. [DOI] [PMC free article] [PubMed] [Google Scholar]


