Abstract
Over the past few decades, the world has witnessed considerable progress in women’s, children’s and adolescents’ health (WCAH) and the Sustainable Development Goals (SDGs). Yet deep inequities remain between and within countries. This scoping review aims to map financing interventions and measures to improve equity in WCAH in low- and middle-income countries (LMICs). This scoping review was conducted following Joanna Briggs Institute (JBI) guidance for conducting such reviews as well as the PRISMA Extension for Scoping Reviews (PRISMA-ScR) for reporting scoping reviews. We searched Medline, PubMed, EMBASE and the World Health Organization’s (WHO) Global Index Medicus, and relevant websites. The selection process was conducted in duplicate and independently. Out of 26 355 citations identified from electronic databases, relevant website searches and stakeholders’ consultations, 413 studies were included in the final review. Conditional cash transfers (CCTs) (22.3%), health insurance (21.4%), user fee exemptions (18.1%) and vouchers (16.9%) were the most reported financial interventions and measures. The majority were targeted at women (57%) and children (21%) with others targeting adolescents (2.7%) and newborns (0.7%). The findings highlighted that CCTs, voucher programs and various insurance schemes can improve the utilization of maternal and child health services for the poor and the disadvantaged, and improve mortality and morbidity rates. However, multiple implementation challenges impact the effectiveness of these programmes. Some studies suggested that financial interventions alone would not be sufficient to achieve equity in health coverage among those of a lower income and those residing in remote regions. This review provides evidence on financing interventions to address the health needs of the most vulnerable communities. It can be used to inform the design of equitable health financing policies and health system reform efforts that are essential to moving towards universal health coverage (UHC). By also unveiling the knowledge gaps, it can be used to inform future research on financing interventions and measures to improve equity when addressing WCAH in LMICs.
Background
Over the past few decades, and prior to the onset of the COVID-19 pandemic, the world witnessed considerable progress in WCAH and well-being and the SDGs. The number of maternal deaths worldwide decreased to 223 000 in 2020 from 342 000 in 2000 [1], and the mortality rate for children under-five years decreased by almost 50% between 2000 and 2021 [2]. Yet deep inequities remain between and within countries. For instance, although the global maternal mortality ratio is estimated to have fallen by 34% between 2000 and 2020, 94% of all maternal deaths occur in LMICs with the risk of stillbirth being 23 times higher in the most severely affected countries [3].
Inequities are also pronounced within countries where progress is not reaching every woman, adolescent and child, especially those in population groups facing multiple deprivations. These groups are often found in settings that are remote, rural, urban, conflict-affected or mobile. They are bearing the disproportionate burden of death and are being left furthest behind. For instance, two-thirds of zero-dose children (those who have not received a single dose of the DTP-containing vaccine, which protects against diphtheria, tetanus and polio) live below the poverty line and suffer nearly 50% of global deaths from vaccine-preventable diseases. Similarly, maternal mortality increase on average by 11% in conflict zones and by 28% in the worst hit conflicted affected areas [4]. Similarly, while significant reductions have been achieved in under-five mortality rates, progress on newborn mortality and stillbirths has fallen behind. It is estimated that 47% of under-five deaths occur during the neonatal period [5]. Factors such as age, gender, ethnicity, sexual orientation, migration status, socio-economic status and geographic location contribute to the important inequities across the continuum of sexual, reproductive, maternal, neonatal, child and adolescent health (SRMNCAH).
The COVID-19 pandemic has exacerbated these existing inequities and compounded the difficulties that women, children and adolescents face in accessing health and social services, negatively impacting SRMNCAH outcomes. For instance, recent estimates provided by the United Nations Population Fund indicate that across 115 LMICs, the pandemic disrupted contraceptive use for approximately 12 million women, causing nearly 1.4 million unintended pregnancies in 2020 [6]. Findings from a Lancet systematic review also indicate that maternal deaths and stillbirths increased during the pandemic, as did ruptured ectopic pregnancies and maternal depression. There seemed to be a considerable disparity between high-resource and low-resource settings [7]. In 2020, the number of children who missed out on receiving even a single vaccine shot increased by 3 million, from 10.6 million in 2019 to 13.7 million in 2020, in Gavi-supported countries. Zero-dose children and the communities they live in often face multiple deprivations and can be regarded as a marker of inequity [8]. For example, in Nepal, hospital deliveries decreased, most markedly among disadvantaged groups, including women in castes perceived as lower in status [9].
Furthermore, the socioeconomic consequences of the COVID-19 pandemic and the related restrictions that were imposed indicate that approximately 131 million more people were pushed into poverty in 2020, many of them women, children and adolescents from marginalized communities [10]; a finding which suggests that COVID-19 has reversed progress for the first time since 1999 [11]. Nevertheless, the prospect of recovery from the COVID-19 pandemic is emerging with the count of zero-dose children almost at pre-pandemic levels [12].
Certain populations are being more affected than others by the socioeconomic consequences of COVID-19. These include: women, children, and adolescents; those who are marginalized and excluded; who depend on the informal sector for income; who live in areas prone to fragility; who have insufficient access to social and health services; who lack social protection; who are denied access to health services due to discrimination; who have low levels of political influence; who have low incomes and limited opportunities to cope and adapt; and who have limited or no access to technologies [13].
Conflict, climate change, COVID-19 and the cost-of-living crisis, known as the four Cs, present many challenges to the health and welfare of women, children and adolescents [14]. In 2022, more than 100 million people were forcibly displaced from their homes due to armed conflict and violence with women and children bearing the greater share of this burden [15]. In addition to the direct maternal and newborn fatalities attributed to the conflicts, there are greater indirect consequences such as the collapse of the health systems, the diminished access to health services and the disruption to food supplies [15,16]. Exacerbating these challenges are the effects of climate change which causes floods, droughts and crop failure that endanger the livelihoods of the poorest and most vulnerable populations [17]. This global polycrisis has drastically increased the cost of living worldwide; global inflation rose from 4.7% in 2021 to 8.8% in 2022. This has jeopardized lower income households’ access to maternal and newborn health services [14]. The impact and extent of this multifaceted crisis varies among countries, presenting distinct yet interconnected and complex challenges that exacerbate pre-existing inequalities, particularly in LMICs with vulnerable health systems [14].
In light of these emerging findings, there is an urgent need to stimulate, coordinate and deliver financing strategies that are equity-enhancing and that target the most vulnerable communities. Such efforts should be supported by evidence-based strategies and interventions to improve equity in WCAH and well-being, especially among vulnerable populations living in specific situations, such as humanitarian and fragile contexts. The objective of this scoping review is to explore the depth and breadth of existing literature on financing interventions and measures to improve equity in WCAH in LMICs and to map out and summarize the evidence to support decision-making and advocacy across different stakeholders, including governments, civil society organizations (CSOs) and donors
Review questions
What are the financing interventions and measures employed by different stakeholders, including governments, CSOs and donors, to improve equity in WCAH in LMICs?
What is the available evidence on the effectiveness and implementation of financing interventions and measures to enhance equity for WCAH in LMICs?
Methods
Definitions
A scoping review is typically used to present “a broad overview of the evidence pertaining to a topic, irrespective of study quality, to examine areas that are emerging, to clarify key concepts and to identify gaps”. The updated JBI guidance for conducting scoping reviews was used [18] alongside the PRISMA Extension for Scoping Reviews (PRISMA-ScR) [19].
Financing for equity reflects on the need to “adapt, extend and scale up innovative and equity enhancing financing strategies that consider the differentiated reaches and impacts on vulnerable groups and populations, including women, children and adolescents in humanitarian and fragile settings” [20]).
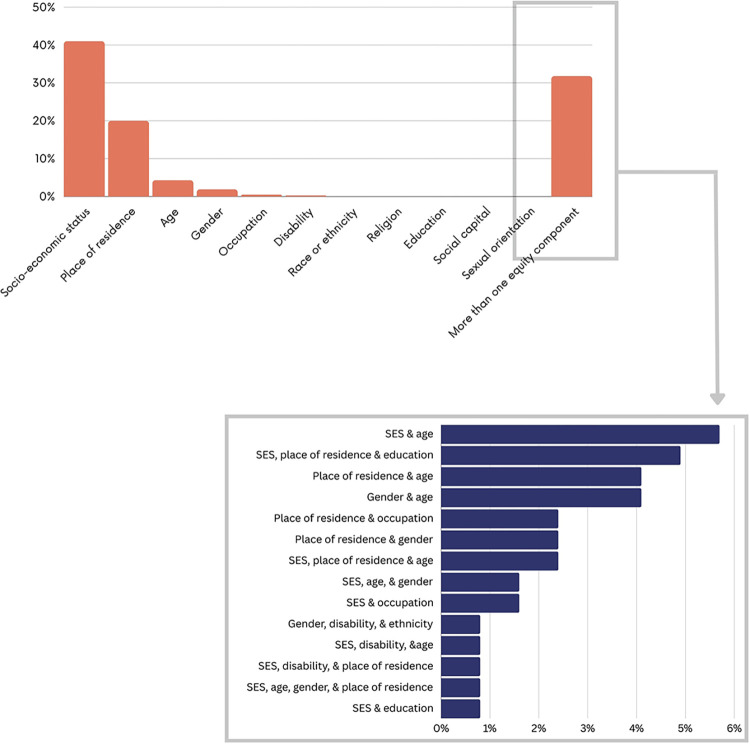
Equity in health can be defined as “the absence of disparities in health (and in its key social determinants) that are systematically associated with social advantage/disadvantage” [21]. This report used the guidance framework PROGRESS-Plus, which identifies components affecting health and healthcare equity including place of residence, race or ethnicity, occupation, gender, religion, education, social capital, socioeconomic status (SES), plus age, disability and sexual orientation.
Protocol and registration
The protocol was not registered as PROSPERO does not accept scoping review protocols. The protocol is available upon request from the corresponding author.
Eligibility criteria
Population of interest: The population of interest consisted of women, newborns or neonates, children and adolescents. The explicit use of terms to define each population were used as they had been categorized into different age groups across the different articles.
Intervention of interest: The report looked at financing interventions and measures employed by different stakeholders including government, international donors and CSOs that aim to improve equity in WCAH. It considered demand and supply-side financial interventions including user fee exemption policies, national health insurance plans, subsidization policies, health equity funds, pro-equity policies, performance-based financing (PBF), financial protection schemes for vulnerable women, children and adolescents and incentive programmes such as CCTs, unconditional cash transfers (UCTs) and voucher schemes. The search excluded financial interventions targeting the general population without addressing any equity component such as SES, place of residence, disability etc. It also excluded studies that assessed financial interventions as part of a multi-component intervention and did not separate the results.
Outcome of interest: Only studies that assessed health outcomes were included, for instance those looking at morbidity and mortality and health systems outcomes such as access to healthcare, healthcare utilization and quality of care.
Setting of interest: The search focused on LMICs including humanitarian and fragile settings (HFS) as per the World Bank Country and Lending Groups’ classification by income issued in July 2022 [22] (S1 Appendix).
Study design: The study included primary studies, narrative reviews, systematic reviews and technical reports. The eligibility criteria was restricted to articles and reports published since the year 2000.
Literature search
The following electronic databases were searched: Medline, PubMed, Emboss, the WHO’s Global Index Medicus. The websites of key actors in this space for technical reports were included, including Gavi, The Vaccine Alliance, the World Bank, the Global Financing Facility and UNHCR, The UN Refugee Agency. The search was conducted for studies published between January 2000 and June 2023. S2 Appendix provides the search strategies of the databases searched.
Both index terms and free text words for the three following concepts were used: health financing, women, children and adolescents, equity and setting (i.e. LMIC). The search strategy was co-developed and run by an information specialist who validated the information sources—for example, electronic databases and websites—the search and medical subject headings (Mesh) terms, the search techniques—for example, boolean operators and search filters—and the documentation of search strategies and results. The search was not limited to specific languages. Additionally, purposive outreach was conducted for a few key actors, such as WHO, Gavi, the Global Fund to Fight AIDS, Tuberculosis and Malaria and the World Bank, to identify additional documents.
Selection process
Title and abstract screening: Teams of two reviewers used the above eligibility criteria to screen titles and abstracts of identified citations in duplicate and independently for potential eligibility. The full text for citations judged as potentially eligible by at least one of the two reviewers were retrieved.
Full-text screening: Teams of two reviewers used the above eligibility criteria to screen the full texts in duplicate and independently for eligibility. The teams of two reviewers resolved any disagreement by discussion or with the help of a third reviewer. Standardized and pilot-tested screening forms were used.
To ensure the validity of the selection process, calibration exercises were conducted. This involved a random subset of 100 articles for reviewers to independently screen against the eligibility criteria. Reviewers then met to discuss the point of disagreement and revise the eligibility criteria and instructions to ensure clarity, minimize disagreements and avoid confusion.
Data extraction
One reviewer extracted data using standardized and pilot-tested forms and a senior reviewer validated these. The data extraction form was pilot tested to ensure the clarity and validity of the data extraction process.
The following information was extracted from each paper:
Last name of first author or name of institutions for reports
Year of publication
Study characteristics:
Type of publication
Type of study design or report
Language of publication
Authors’ information:
Country of affiliation of the contact author
Country of affiliation of first author
Source (Journal name or institution name)
Setting:
Country (ies) subject of the paper
Income level classification according to the World Bank list of economies issued in July 2022 (S1 Appendix)
HFS classification (S3 Appendix)
Financing intervention or measure
Type of intervention or measure
Target population (women, newborns, children or adolescents)
Equity component (PROGRESS Plus factor)
Outcomes assessed and key findings including effects/implementation of interventions and SRMNCAH/well-being/equity outcomes
Statements on funding and conflict of interest of authors
Risk of bias assessment
No risk of bias assessment was conducted, consistent with the JBI guidance manual.
Data analysis
A descriptive analysis of the general characteristics of the included papers, including study designs and settings, was conducted. A thematic analysis of the included studies was also done. These were categorized according to the intervention and outcomes assessed. Findings were further stratified according to variables such as country income group (LMIC level), HFS classification, population of interest and equity factor such as SES, migration etc.
Results
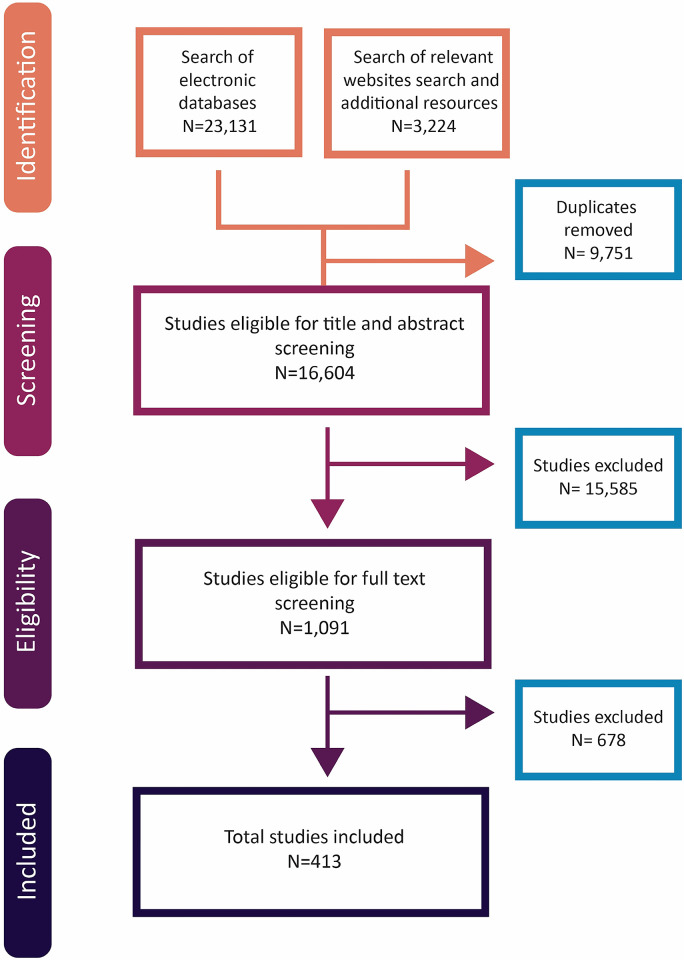
Fig 1 summarizes the selection process. Out of 26 355 citations identified from electronic databases, relevant website searches and stakeholders consultations, 413 studies were included in the final scoping review [23–435]. 678 full texts were excluded for the following reasons: not an intervention of interest (n = 260); did not address equity (n = 152); not a population of interest (n = 134); not a design of interest (n = 61); not an outcome of interest (n = 18); not a setting of interest (n = 16); duplicate (n = 14); full text not retrievable (n = 13); no separate data for the effects of the financing policy (n = 9); or not a time frame of interest (n = 1).
Fig 1. PRISMA flowchart.
Characteristics of included studies
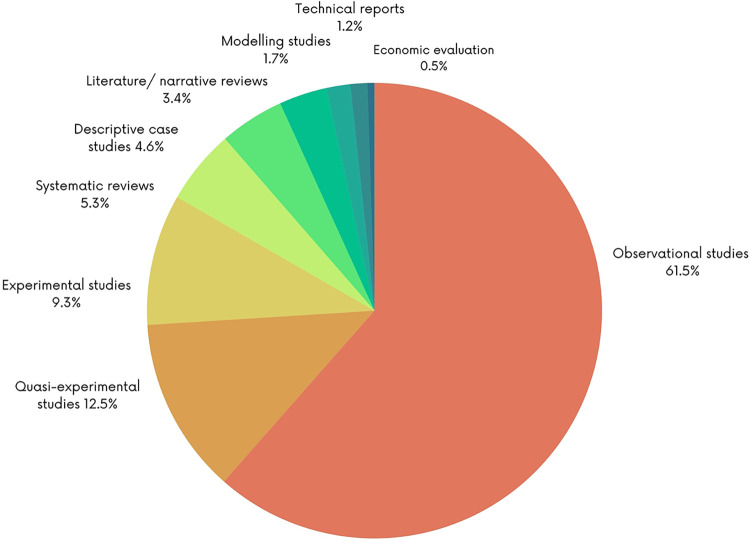
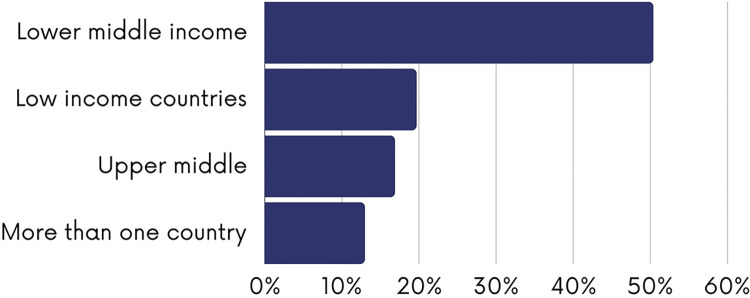
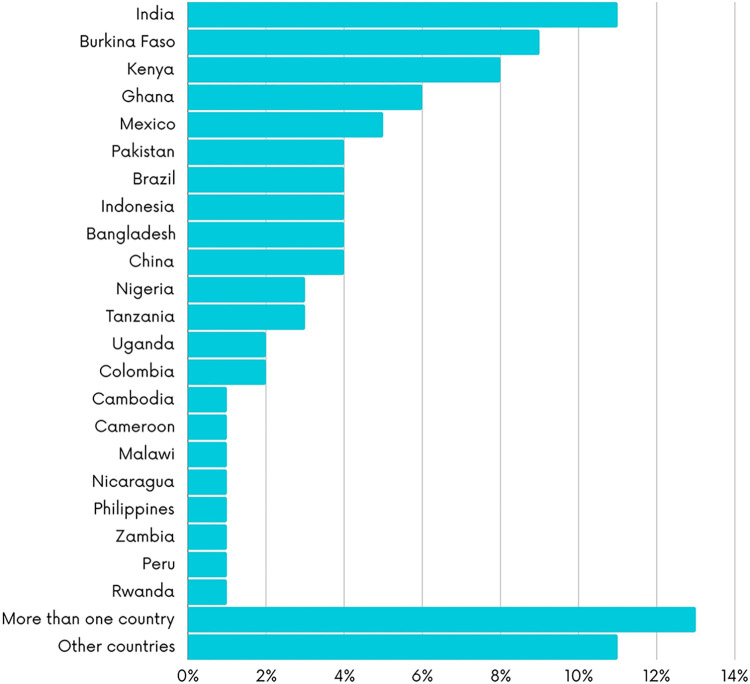
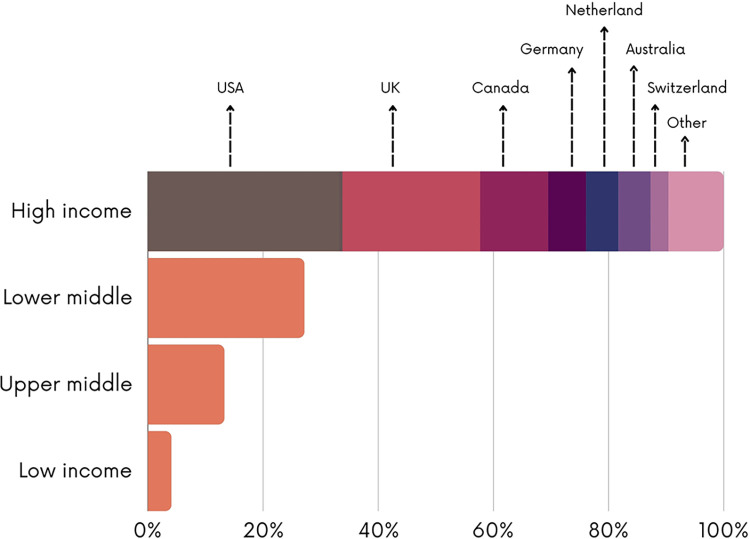
The figures below present the characteristics of the included studies. As shown in Fig 2, most of the studies employed observational study designs (n = 254; 61.5%), followed by quasi-experimental (n = 52; 12.5%) and experimental designs (n = 38; 9.3%). 22 systematic reviews on the topic were identified (5.3%). Most the studies were conducted in lower-middle income countries (n = 209; 50.6%) and low-income countries (n = 82; 19.7%) with fewer studies conducted in upper-middle income countries (n = 70; 13%) (Fig 3). Most of the studies were conducted in India (n = 40; 10.6%) or Burkina Faso (n = 35; 8.7%) (Fig 4). The first authors of included studies were mostly affiliated with institutions from high-income countries (n = 228; 55.2%) mainly the United States (n = 76; 33.2%), the United Kingdom (n = 56; 24.5%) and Canada (n = 27; 11.8%) while only 4.1% of studies had first authors affiliated with institutions from low-income countries (Fig 5).
Fig 2. Type of study design.
Fig 3. Classification of the country of the policy assessed.
Fig 4. Country subject of the papers.
Fig 5. Classification of the country of the institution to which the first author is affiliated.
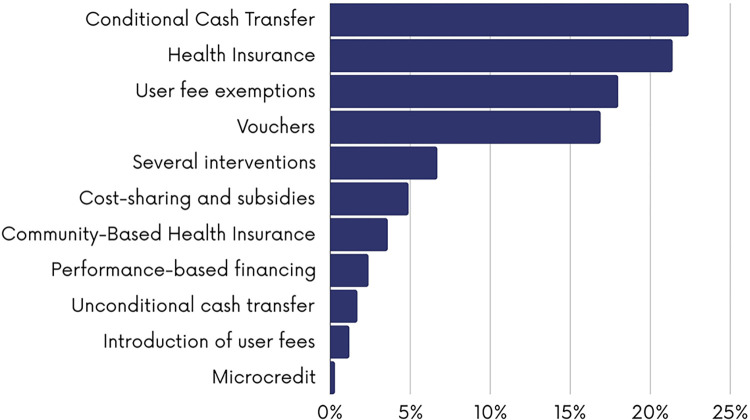
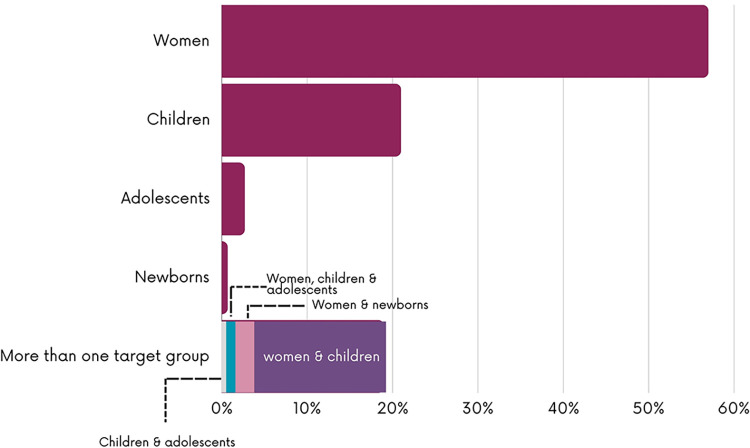
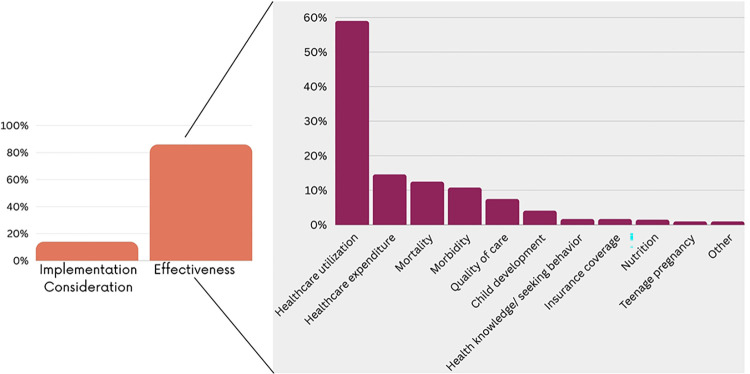
As shown in Fig 6, CCTs (n = 92; 22.3%), health insurance (n = 89; 21.4%), user fee exemptions (n = 75; 18.1%) and vouchers (n = 70; 16.9%) were the most reported financial interventions and measures. Some studies assessed several financial interventions whether implemented separately or as multi-component financial interventions (n = 28; 6.7%). Financial interventions or measures mainly targeted women (n = 236; 57.1%), children (n = 87; 21%) or both women and children (n = 62; 15%) with fewer targeting adolescents (n = 10; 2.7%) and newborns (n = 3; 0.7%) (Fig 7). As shown in Fig 8, the majority of the studies were evaluation studies (n = 354; n = 85.7%) with 59 studies addressing implementation considerations (14.2%). The outcome mostly assessed was the healthcare utilization (n = 245; 59.3%) followed by health expenditures (n = 61; 14.6%), mortality rates (n = 52; 12.6%) and morbidity (n = 44; 10.8%).
Fig 6. Financial mechanisms assessed.
Fig 7. Target population of the financial mechanism.
Fig 8. Type of assessment and outcomes measured.
Equity components
Fig 9 presents the equity components addressed in the included studies. Most of the studies assessed the impact of financial interventions on addressing inequities related to SES (n = 171; 41.4%) followed by place of residence (n = 82; 19.8%) and age (n = 17; 4.2%). Many studies addressed several equity components (n = 132, 31.9%) including SES and place of residence (n = 70; 53%), SES and ethnicity (n = 8; 6.1%), SES and age (n = 7; 5.3%), SES, place of residence and education (n = 7; 5.3%), SES and occupation (n = 2; 1.6%), gender, disability and ethnicity (n = 1; 0.8%). None of the included studies addressed sexual orientation, religion or social capital.
Fig 9. Equity components addressed.
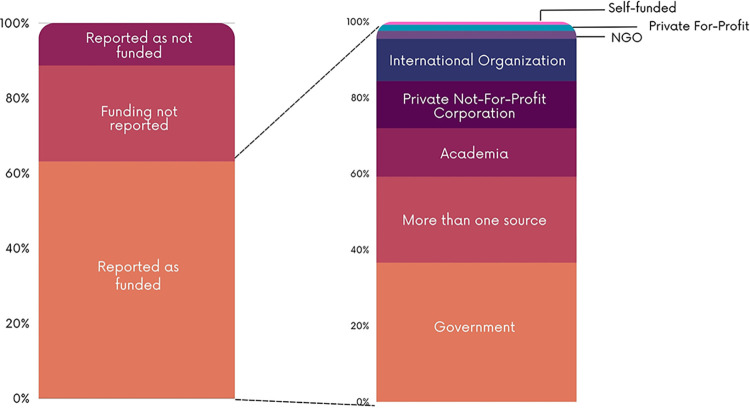
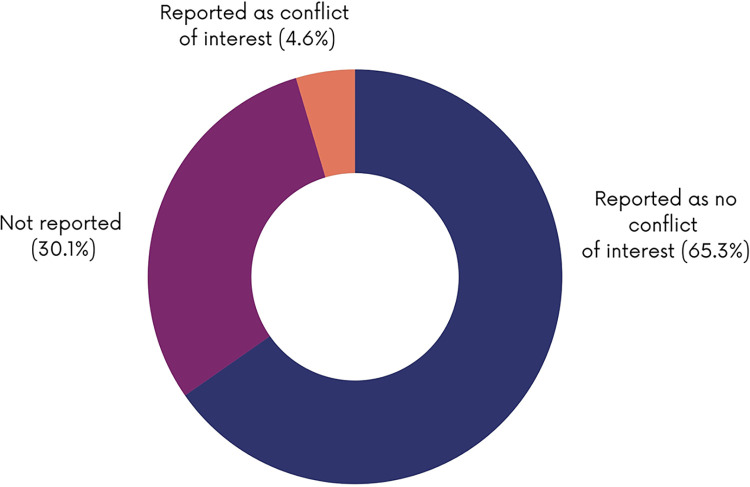
Funding and conflicts of interest characteristics of the included studies
As shown in Fig 10, most of the studies reported study funding (n = 261; 63.1%). Of the studies reported as funded, the funding sources were mainly governments (n = 96; 36.6%), academia (n = 31; 12.8%), private not-for-profit (n = 33; 12.4%) and international organizations (n = 30; 11.1%). Some studies reported being funded by multiple sources (n = 59; 22.6%). Almost a third of the papers (30.1%) did not report on conflict of interest of study authors (Fig 11).
Fig 10. Reporting of funding.
Fig 11. Reporting of conflict of interest.
Findings
The findings below are presented by financial interventions and corresponding outcomes. S1 to S11 Tables present the characteristics of the individual studies.
CCTs (n = 92)
CCTs have been introduced in many LMICs as a provision of monetary transfers to households on the condition that they comply with a set of requirements [46]. 92 studies evaluated the effectiveness of CCT programs on healthcare utilization, morbidity, mortality, child development, healthcare expenditure, quality of care and other outcomes including health knowledge, responsive caregiving, teenage pregnancy and nutrition as well as implementation considerations [23–109,407–411]. The majority of the studies assessed CCT programs in Latin America (n = 41), mainly Brazil (n = 17), and India (n = 24) assessing the Janani Suraksha Yojana (JSY) program.
Healthcare utilization (n = 48): 48 studies assessed the effect of CCT programs on healthcare utilization [23–27,29,30,32,33,35–37,39–43,45–50,59,62,63,71,78,81–87,89,90,94–97,100,101,105,107–109,408]. 40 studies found that CCT interventions can increase the utilization of maternal and child health services for the poor and the disadvantaged, including antenatal care visits [24–26,29,30,35,39,41–43,45,47,50,63,96,105,108], post-partum care [63,105], institutional delivery [23–26,29,33,36,37,47,78,82,84–87,89,94], caesarean sections [37,95], skilled birth attendance [26,45,94,96], contraceptive use among young women [90], child health check-ups [40–42,46,49,59,81] and immunization coverage [26,27,32,71,100,101]. One study reported that the CCT program encouraged adolescents to attend the clinic for assessments or HIV testing [109]. Although CCT was shown to increase access to institutional delivery, three studies revealed a disproportionate lower concentration of institutional deliveries in low-income populations in comparison to high-income populations [33,36,48]. One study revealed that CCT decreased rates of caesarean section deliveries, which is explained by a shift from the private sector [94]. Two studies suggested that CCT programs addressing both the supply and demand side of health services may increase the coverage of maternal and child health services [62,408]. Five studies found negative results on the impact of CCTs on immunization coverage [41,46,63,83,87]. One study reports the poor effect of CCTs on immunization coverage to be because of weak monitoring of conditionality [83]. One systematic review found mixed results on immunization coverage that might be due to the initial high rates of immunization [46] while another systematic review found insufficient evidence on the impact of CCTs on child health service utilization in sub-Saharan Africa [107].
Mortality (n = 20): 20 studies reported on the effect of CCT programmes on maternal and child mortality [23,24,26–30,32–34,73,85,87,88,91,94,99,103,409]. 13 studies and one systematic review revealed a positive impact of CCTs in reducing infant, child and maternal mortality rates for the poor and the disadvantaged [27–30,32,34,73,85,87,88,91,99,103,409,410]. Five studies reported a reduction in child mortality whereby the intervention led to a decrease in overall mortality from poverty-related causes, which included malnutrition and diarrhoea [24,27,34,73,91]. One study suggested an improvement in child mortality when CCTs are combined with improvements to adequate access to water, sanitation and solid waste collection [34]. Another study highlighted that although CCT programmes reduce maternal mortality, inequalities persisted whereby fewer death were observed in the richest divisions compared to the poorest division [33]. One study showed a positive impact on determinants of maternal mortality but suggested a small effect on maternal mortality due to implementation issues [25]. Three studies did not find any impact of CCTs on maternal or child mortality [23,26,94].
Morbidity (n = 16): 16 studies reported on the effects of CCT programmes on morbidity [32,46,55,56,64,66,79–82,85,91,98,102,107,411]. 10 studies found that CCT interventions can improve child health for vulnerable groups by reducing malnutrition and wasting [79,91,411], hospital admissions [27,91], illness and anemia rates [46,64,79,85], diarrhea and acute respiratory infections [32], psychosocial health [81] and incidences of dental caries [80]. One systematic review found insufficient evidence on the impact of CCTs on child health status in sub-Saharan Africa [107]. One study suggested that CCTs reduced HIV risks among young women [56]. Two studies reported a positive impact of CCTs on women’s health including a lower prevalence of being underweight or overweight [79] and lower current hypertension rates [55] while one study reported an increase in body mass index (BMI) and obesity risks among women [66]. Another study found no evidence that the CCTs led to a reduction in preventable delivery complications [82]. Two studies found no impact on mental health among youth [98,102], mainly among females, suggesting that conditions should not stereotype females [98].
Child development (n = 14): 14 studies addressed the effect of CCTs on child development [30,38,43,46,52,57,58,60,64,67,75,76,103,104]. 10 studies found that CCT interventions can improve child health by reducing the incidence of low birth weight [30,57,103,104], and improving height-for-age Z scores, length and stunting among children [38,43,46,58,64,75,76]. Four studies showed that CCTs did not significantly impact weight-for-age Z scores [43], height-for-age Z scores [67], BMI-for-age Z scores and stunting [52] and weight gain [60].
Other health outcomes (n = 9): Nine studies reported on the effect of CCTs on health knowledge and behavior [25,88], responsive care giving [43], teenage pregnancy [61,65], adult fertility [72] and nutrition [40,74,93]. One study showed an increase in demand for maternal and child health services within facilities among beneficiaries [88] while another study found no improvement in health knowledge among mothers [25]. Three studies reported on the effectiveness of CCT programmes on nutrition [40,74,93]. All studies suggested a positive impact of CCTs on nutrition determinants including an increase in dietary diversity and food consumption [40,93], especially in rural areas [40], and an increase in food per capita household consumption [74]. One study found that CCTs resulted in a positive change in key parenting practices, including children’s intake of protein-rich foods and care-seeking behavior [43] and a decrease in teen pregnancy and fertility [61,65] with no effect on adult fertility [72].
Health expenditures (n = 3): Three studies from India found that although CCTs can enhance financial access to maternal and child health services, it did not adequately protect beneficiaries from out-of-pocket expenditures [84,97,106].
Quality of care (n = 2): Two studies reported on the effect of CCTs on the quality of care and beneficiaries’ satisfaction [82,103]. CCT programmes significantly improved the quality of delivery care and satisfaction with care in one study [82]. One systematic review reported on two studies from Mexico suggesting that CCTs improved the quality of care but the measure of care was based on women’s recall [103].
Implementation considerations (n = 15): 15 studies reported on implementation considerations for CCT programmes [31,36,44,51,53,54,68–70,77,88,92,98,105,407]. Challenges to the implementation of CCT programmes included the complicated eligibility criteria, irregular cash transfers, insufficient entitlements, unclear payment procedures, the quality of care in public health facilities, insufficient healthcare personnel, infrastructure, medicine and equipment, increased workload and low literacy levels among beneficiaries [36,44,54,68,70,77,88,407]. The lack of awareness among beneficiaries about the CCT programme and the included services may have also hindered service uptake [36]. In India, the bribes imposed by providers incurred additional out-of-pocket expenditures for CCT beneficiaries [53]. The misuse and mismanagement of cash were also reported as a challenge [44,54,70]. In one study, beneficiaries proposed that CCT programmes may be unsustainable and expressed concern that young women may misuse or mismanage the transfers [54]. Another study reported that mothers’ in-laws forced their daughters-in-law to stay in their villages, not allowing them to go to the mother’s area at the time of delivery for the sake of securing the cash incentive, which is given only upon the condition of the women delivering in the local institution where she is registered [70]. To increase the effectiveness and acceptance of CCT programmes, studies suggested the need for adequate human resources, staff training systems, improving the access and quality of care, community engagement in the design and implementation of the programme, improvement in targeting, increasing awareness of the programme and removing any stereotype in conditions and extensive monitoring [31,36,51,69,77,92,98,105].
Health insurance (n = 89)
89 studies tackling various health insurance schemes including national health insurance, social health insurance and employment-based health insurance were included. These studies evaluated the effectiveness of these various health insurance schemes on healthcare utilization, healthcare expenditure, mortality, morbidity, quality of care and other outcomes including insurance coverage and nutrition as well as implementation considerations [327–404,406,412–421].
Healthcare utilization (n = 46): 37 studies reported that various health insurance schemes increased skilled birth attendants, facility-based deliveries, caesarean section deliveries, antenatal care utilization, children health consultations and vaccination coverage, utilization of health services among women with disabilities and use of family planning services [328,334,336,337,339,341,345,346,349–352,354,358,359,365,367,368,370,374,376,377,379,383–387,390,391,394–397,399,401,404,406,414,420]. 11 of these studies indicated that these favorable effects were mostly prominent among poor households [334,337,367,370,377,394,396,397], those residing in rural areas [346], individuals with disability [345] and indigenous women [390]. This suggests that insurance schemes led to more equitable access to health services among the impoverished and vulnerable populations. While three studies reported that although there has been a notable increase in the utilization of maternal health services due to the insurance schemes, this increase was not as significant among the extremely poor [349,415] and those residing in rural areas [376]. Five studies showed that insurance schemes had no effect on the use of family planning services [329,363], access to HIV testing during antenatal care visits [332], utilization of outpatient services in children [343] and facility-based deliveries [403].
Health expenditures (n = 21): 10 studies reported that enrollment in an insurance scheme reduced households’ out-of-pocket expenditures for maternal care [340,352], facility-based deliveries [337], inpatient care [330,348], child care [334,365], neonates critical care [375] and breast cancer treatment [382,401]. Five studies indicated that insurance schemes can protect poor households and migrant women from the financial burden of out-of-pocket health expenses [369,380,392,420], and can provide adequate health coverage for children with mental disorders [347]. Four studies showed that these schemes had no significant effect on reducing out-of-pocket payments sustained by poor households for maternal and child care [336,345,362,421]. As for the remaining two studies, they reported that the enrollment in insurance schemes caused women extra financial hardship due to their lack of awareness about their rights within the programme and mistrust in the scheme that drove them to private health providers [389] and that women from lower socioeconomic disadvantage had higher out-of-pocket health expenses than those from higher socioeconomic disadvantage [402].
Mortality rate (n = 15): 12 studies reported that national health insurance schemes reduced maternal, neonatal and infant mortality rates [327,341,351,358,371,375,378,379,382,385,393,394]. Three studies reported that insurance schemes had no significant positive effect on neonatal mortality rates [403], didn’t reduce inequality in maternal mortalities within the regions [388] and that one year all-cause mortality rates were notably higher in women enrolled in rural insurance schemes than those enrolled in an urban insurance scheme [381].
Morbidity (n = 10): All 10 studies reported a positive effect of the different types of health insurance schemes on treatment adherence in children with cancer [333,394], overall health status of women and children [355,356,398,400], preventing malnutrition and stunting in children [344,366,379] and reducing the incidence of influenza and diarrhea in children [375].
Other outcomes (n = 9): Five studies highlighted inequities in health coverage under several insurance schemes with women who are poorer, less educated, unemployed or residing in remote areas being less likely to be insured [335,353,357,412,413]. One study showed that a health insurance scheme implemented in Peru had increased health coverage among marginalized women and contributed to more equity in healthcare access [364]. Another study reported that enrollment in a public health insurance scheme in China didn’t improve the nutritional status of rural poor children [372]. A study conducted in Colombia showed that women living in low socioeconomic residential areas and who were affiliated to a subsidized health insurance scheme (versus contributive) experienced a reduced probability of cervical cancer survival compared to women living in high socioeconomic areas [419]. One study found higher cancer survival rates for insured versus uninsured children in Kenya [417].
Implementation considerations (n = 8): Eight studies reported on different barriers that hindered either women’s enrollment in insurance schemes or their access to healthcare despite their enrollment. The barriers included: the need to move to another city to get the treatment; the authorizations of the paying entities; the medication costs [331], the distance to facilities [418]; having unreliable sources of income [342]; having invalid insurance cards [353]; having a low educational level [360]; encountering high premiums [416] and the extra costs of care [336]. One study addressed facilitators to the enrollment of children from lower socioeconomic status in insurance schemes. These included: eliminating the remaining small yearly renewal fee’ organizing outreach initiatives to offer registration assistance to female guardians of children; and establishing additional administrative offices for the programme in remote areas [361]. Another study addressed the facilitators of enrollment of poor women residing in rural areas. These were educating the public on the importance of enrolling in a health insurance programme and offering initial free subscriptions to individuals with the lowest economic wealth status [391].
User fee exemption (n = 75)
User fee exemptions have been implemented in many LMICs to alleviate the substantial out-of-pocket payments and the resulting financial burden incurred by low-income households [113]. 69 studies evaluated the effectiveness of user fee exemption policies on healthcare utilization, healthcare expenditure, mortality, morbidity, quality of care and other outcomes including health-seeking behavior and teen pregnancy as well as implementation considerations [107–175,419–424].
Healthcare utilization (n = 43): 27 studies reported positive effects of these programmes on the use of facility-based delivery services [113,121,126,139,141,147,150,156,160,163,168,173,426], malaria prevention and treatment services for pregnant women and children [119,145,155,161], maternal and child consultations [122,132,133,136,142,158,164,177] and family planning and contraception services [167,170], leading to more equitable access among the poor and vulnerable populations. 16 studies indicated that user fee exemption programmes had minimal to no effect on increasing the utilization of maternal and sexual and reproductive health services among poor women or those living in rural areas [110–112,115,120,123,124,127–129,134,137,138,140,157,178].
Health expenditures (n = 17): Nine studies reported a positive effect of user fee exemption programmes on reducing out-of-pocket health expenditures and medical expenses among poor households [130,131,143,152,157,171,172,177,426]. While eight studies showed limited to no effect of these programmes on eliminating out-of-pocket health expenditures among impoverished households, this could be attributed to additional expenses not covered by the scheme such as transportation, medical supplies, medications and unofficial provider fees [116,150,154,159,165,175,176,425].
Mortality (n = 7): Four studies reported that despite the implementation of user fee exemption programmes there was no noticeable reduction in maternal, neonatal or under-five child mortality rates [119,126,139,168]. Three other studies reported that these programmes reduced maternal, neonatal and under-five child mortality rates due to the uptake of institutional deliveries and child health services [113,121,145].
Morbidity (n = 4): Three studies reported a positive effect of user fee exemption programmes on reducing wasting and stunting in children [162], on prompt treatment of sick newborns [166] and on improved screening for sexually transmitted infections (stir) in young women [175]. One study indicated that these programmes did not reduce illness in children [115].
Quality of care (n = 4): Three studies reported that user fee exemption programs had a positive effect on the quality of delivery and maternal care services [135,172] and on the quality of medical prescriptions with physicians reducing their use of antibiotics in for children by 62% [177]. One study indicated that the quality of maternal care provided under these programmes was perceived as poor by managers and health providers due to the increase in workload, delayed reimbursement of funds and stock-out of essential drugs and medical supplies [117].
Other outcomes (n = 2): Two studies reported that user fee exemption programs led to a decrease in teen pregnancies [169] and had a positive effect on health-seeking behaviors in children [149].
Implementation considerations (n = 15): Nine studies reported on several barriers to the implementation and uptake of user fee exemption policies. These included: a lack of infrastructure and human resources; sociocultural factors; limited awareness of the policy; out-of-pocket payments on drugs; transportation and lab tests; reduced quality of the services; and increased administrative workload [114,118,125,148,154,174,422,424,427]. Six studies reported on facilitators for the implementation of these policies. They included: residing near the facility; knowledge and awareness of the policy; residing in urban areas; having a good drug supply system in place; and having higher levels of education [144,146,151,153,156,423].
Vouchers (n = 70)
This financial intervention involves distributing vouchers of a predetermined value to patients, which they can redeem to receive services from providers who are then repaid by the insurance or government payor that issued the voucher. 70 studies that evaluated the effectiveness of voucher schemes on healthcare utilization, quality of care, health expenditures, mortality, morbidity, health knowledge and child development as well as implementation considerations were included in the scoping review [176–243,425,426].
Healthcare utilization (n = 56): All 56 studies reported on the positive effect of voucher schemes on the use of sexual and reproductive health services [179,180,183,189,196,197,204,205,210,213,218,225,231], contraceptive and family planning services [181,182,187,192,200,201,208,211,212,222,228,241,244,246,428], facility-based deliveries [186,190,193,199,209,214,223,224,227,229,232,233,238,242,245], skilled birth attended deliveries [191,230], antenatal care services [185,198,215,219,226,239], child immunization services [194,429] and the use of insecticide-treated nets for pregnant women and children [188,216,236]. Across the majority of these studies, the effect of the voucher scheme was notably pronounced among the poorest populations, fostering more equity in healthcare utilization with the exception of one study where a voucher program aiming at providing insecticide-treated nets for pregnant women reported coverage of only 18% among the poorest compared to 37% among the richest [188].
Quality of care (n = 10): Seven studies showed that voucher schemes helped to improve the comfort of the patients, thus increasing their satisfaction and improving the interpersonal skills of the healthcare workforce [193,203,210,221,231,240,246]. However, one study showed that vouchers increased the workload for public health facilities [224]. Two studies showed that the current evidence is inconclusive on the effect of voucher programs on the quality of care [180,181].
Health expenditures (n = 6): Four studies agreed that voucher schemes helped reduce the out-of-pocket expenditure on healthcare services endured by women and decreased the financial barrier to access to maternal and sexual health services. [185,195,200,229]. One study highlighted that an SMS money transfer system can successfully reimburse healthcare providers located in remote and rural areas [182]. One study showed that the effect of vouchers on low-income households’ health spending is more substantial when coupled with health equity funds [206].
Mortality (n = 3): Two studies reported that vouchers helped to reduce maternal and newborn mortality rates [197] as well as malaria-related under-five mortality rates in the context of an insecticide-treated net voucher [220]. However, one study showed that a voucher scheme implemented in Bangladesh did not improve stillbirths, neonatal or infant mortality rates [245].
Health knowledge (n = 3): Two studies concluded that voucher schemes enhanced the knowledge and awareness of voucher receivers on contraceptives and STIs [183,201]. One study, however, showed that a voucher scheme had no effect on enhancing adolescent girls’ knowledge about STIs [211].
Morbidity (n = 1): One systematic review reported that the impact of vouchers on the overall health status of women was inconclusive since improvements in health outcomes require more time to manifest and may not be apparent within the designated evaluation time [189].
Child development (n = 1): One study conducted within a refugee camp in Bangladesh showed that the substitution of food rations with electronic food vouchers was linked to enhanced linear growth among children aged between six years and 23 months [217].
Implementation considerations (n = 8): Eight studies explored facilitators to the implementation of voucher programmes. Facilitators included: designing a context-specific programme [213,235]; sensitizing the community [233]; and integrating vouchers within other programmes [207]. Four other studies identified barriers, including the complex eligibility procedures used in determining beneficiaries that might at times mean missing out the poorest beneficiaries, to the implementation of voucher schemes [234]. Other barriers included: a lack of knowledge among the target population about the services provided by the voucher program [237]; the significant amount of time required to achieve awareness and uptake of the program [184]; and the high cost of starting a mobile e-voucher program that requires software systems and staff training [243].
Studies assessing several interventions (n = 28)
28 studies addressed several financing interventions whether implemented separately or as part of a multi-component intervention. 19 studies, mainly literature reviews, assessed the use of different financing interventions including vouchers, user fee exemptions, cash transfers, the introduction of user fees, community healthcare plans, social protection schemes and insurance schemes that were either implemented in different countries or the same country but at different time periods or in different regions of the country [254–272]. The outcomes assessed were healthcare utilization [254–264,266,269,271], quality of care [254,258,259,264,268,269], healthcare expenditure [261,265,271], child development [267] and insurance coverage [256] as well as implementation considerations [255,257,268–270,272].
Five studies compared the effectiveness of CCT versus UCT interventions in Zimbabwe and other LMICs [247–249,431]. Four studies assessed the combination of different financing interventions to address health inequities [250–253]. A study conducted in Kenya found that the combination of a voucher and a CCT programme led to an increase in facility-based deliveries with 48% of the women using these schemes and subsequently delivering in a hospital or a clinic [250]. Another study assessing the use of a UCT programme paired with health insurance found that this combination increased the access of vulnerable households to healthcare services by reducing cost barriers [251]. The study evaluating the use of PBF in addition to user fee exemption found that despite the increase in facility-based deliveries due to these interventions, caesarean section rates remained alarmingly low (3%) and below the WHO recommendation [252].
Finally, according to a study assessing the combination of public insurance, a pay-for-performance scheme and a CCT program in Argentina, there was a significant decrease in the prevalence of stunting and underweight among children enrolled in these schemes [253]. However, stunting and obesity remained more common among rural populations [253]. One study assessing the effect of the a PBF program and a user fee removal policy on out-of-pocket expenditure found that user fee exemption can reduce out-of-pocket costs while there was no substantial effect of PBF [430].
Cost-sharing (n = 20)
Cost-sharing has been used by the public health sector in several LMICs to partially redeem the expenses associated with providing healthcare services [273]. 20 studies that evaluated the effectiveness of cost-sharing and subsidies on healthcare utilization, health expenditures, morbidity, quality of care, and mortality, as well as implementation considerations were included in this scoping review [273–291,432].
Healthcare utilization (n = 11): 11 studies reported a positive impact of cost-sharing and subsidies on healthcare utilization with an increase in institutional deliveries [275–278,281], use of child health services [283], skilled birth attendance rates [280,288], households’ use of different health services [273,284] and consumption of fortified packaged complementary food (FPCF) in children [282].
Health expenditures (n = 5): Four studies reported that cost-sharing schemes led to a reduction in poor households’ facility-based delivery and reproductive health medical expenses [281,285,291] as well as a reduction in the societal cost of micronutrient deficiencies in children [282]. One study reported that despite the implementation of a cost-sharing scheme in Kenya, spending on family planning and reproductive health remained disproportionately borne by households with an increase in out-of-pocket expenses from 10% in 2005–06 to 14% in 2009–10 [274].
Morbidity (n = 2): Two studies reported a positive effect of cost-sharing policies on morbidity in women and children by reducing incidence and prevalence of reproductive tract infections and reducing the number of disability-adjusted life years due to iodine deficiency, vitamin A deficiency and iron-deficiency anemia in children aged six to 23 months [279,282].
Quality of care (n = 2): Two studies reported a positive effect of subsidy policies on the quality of care provided to women delivering in hospitals [281,291].
Mortality (n = 2): One study found significant reductions in national under-five mortality following a targeted subsidization of case management of under-five malaria [432] while another study conducted in Burkina Faso reported a non-significant decrease in deaths per live births [275].
Implementation considerations (n = 5): Five studies reported on implementation considerations for the cost-sharing policies [286–290]. A subsidy program implemented in Peru to improve the follow-up of cervical cytology was highly accepted by lower-income women [290]. The interaction between health workers and women is an important factor in determining their use of facility-based deliveries in light of a subsidy policy [286]. Moreover, three studies addressed implementation gaps which included health workers taking advantage of the subsidy policy to overestimate the cost of deliveries and incur financial gains [288], inadequate enforcement and organizational capacity [289] and limited understanding of the power dynamics between individuals representing the health system and communities [287].
Community-based health insurance (CBHI) (n = 15)
CBHI is a form of health insurance that revolves around mutual assistance, solidarity and collective risk pooling. It offers flat rates to workers in the informal sector and rural communities [302]. 15 studies that evaluated the effectiveness of CBHI on healthcare utilization, health expenditures, morbidity, and mortality and implementation considerations were included in this scoping review [292–304,434,435].
Healthcare utilization (n = 9): Seven studies found a positive impact of CBHI on increasing the utilization of health services mainly when it came to institutional deliveries, antenatal and postnatal care, vaccinations among the poorest, and increasing the likelihood of mothers seeking healthcare services for child illnesses [292–294,297,300,302,303]. One systematic review found that the CBHI had a negative impact on the use of family planning and reproductive health services [296] and one study found no significant effects of CBHI on the utilization of maternal and child healthcare services [435].
Health expenditures (n = 5): Four studies reported that CBHI had a positive effect on reducing out-of-pocket expenditures at the point of service [293], providing substantial financial protection to households [300,304] and decreasing annual health expenditure [294]. One study reported that the high cost of transportation added to the cost of inpatient care was enough to prevent insured women with a low-income from being hospitalized [298].
Morbidity (n = 3): Two studies reported that household participation in a CBHI scheme was associated with a lower likelihood of stunting in offspring [299,302]. Another study reported that in terms of the distribution of stunting, children in the lowest socioeconomic welfare index had a higher prevalence of stunting and that there was no statistically significant association between CBHI participation and stunting [295].
Mortality (n = 2): One study conducted in Burkina Faso reported no significant difference in overall mortality rates between households enrolled and not enrolled in the CBHI scheme [292] while another study reported that the intervention was associated with lowering of the risk of mortality in children enrolled in health insurance when compared to those not enrolled [294].
Implementation considerations (n = 2): One study conducted in Cameroon reported that income was a barrier to women’s enrollment in health insurance schemes, which emphasizes the need for collaboration between health insurance programmes and governments in providing a financial safety net that will lessen the toll of illness on the underprivileged [301]. Another study suggested the need to increase women’s understanding of the CBHI system to develop their trust and enable recognition of its benefits [434].
PBF (n = 10)
PBF is a supply-side intervention that offers incentives to healthcare providers upon the achievement of a set of objectives [312]. 10 studies that evaluated the effectiveness of PBF on healthcare utilization, quality of care, morbidity, resource availability and implementation considerations were included in this scoping review [305–313,433].
Healthcare utilization (n = 6): Six studies found no significant impact of PBF on increasing the utilization of maternal and child health services for institutional deliveries, antenatal and postnatal care and vaccinations among the poorest [305,306,309–311,433]. One study found that the effect of PBF is greater when supplemented by maternal vouchers that eliminate user fees [310]. Another study found that combining PBF with equity interventions, such as systematic targeting and subsidizing health services, did not improve the utilization of maternal health services. The study suggested that financial incentives for providers might not be enough to improve equity as other non-financial barriers to access, including distance to catchment primary health facility, literacy, parity and religion, should be considered [311].
Quality of care (n = 4): Four studies reported contradictory results in regards to the effect of PBF on the quality of care. Two studies found positive effects of PBF on improving the quality of care, specifically in improving the quality of treatment received by children from lower-income backgrounds [306] and on the motivation of health providers in delivering care to lower-income women. One study conducted in Malawi showed that PBF had neither a positive nor a negative effect on the quality of the antenatal care services provided by healthcare providers [313]. Another study on PBF covering under-five curative care, child vaccination and growth monitoring visits in Burkina Faso showed no impact on the quality of care [305,306,312].
Morbidity (n = 2): Two studies conducted in Burundi [308] and Rwanda [306] reported no significant effectiveness of PBF in reducing morbidity such as fever, diarrhea and malnutrition in children [306,308].
Resource availability (n = 1): One study conducted in Cameroon showed that PBF is associated with a significant reduction in stock-outs of family planning medicines but not in stock-outs of antenatal care drugs, vaccines, integrated management of childhood illness drugs and labour and delivery drugs [307].
Implementation considerations (n = 1): One study reported that the effectiveness of any PBF scheme addressing inequity specific to maternal health depends on the different stakeholders’ sharing a common understanding of what poor and vulnerable means as well as on the prompt payment of incentives to healthcare facilities and providers [312].
UCTs (n = 7)
UCT programmes provide low-income and vulnerable populations with additional income without imposing any requirements on the recipients [320]. Seven studies that evaluated the effectiveness of UCTs on morbidity, healthcare utilization, health expenditures, nutritional status and child development were included in this scoping review [314–320].
Morbidity (n = 4): Two studies found a favorable effect of UCTs on the likelihood of having experienced any disease in children [320] and on the anthropometric measures in children [319]. Another two studies found no effects of UCT programmes on the prevalence of malnutrition, incidence of wasting or stunting in children [316,318].
Health expenditures (n = 2): One study conducted in Burkina Faso reported that the availability of UCTs supported families in spending more on healthcare to support children’s health [317]. One systematic review found that UCTs may help improve healthcare expenditures in LMICs [320].
Healthcare utilization (n = 2): One study noticed better access to maternal health services, specifically skilled attendance at birth, as a result of UCTs [315] while another study reported that UCTs had no effect on the utilization of health services among children and adults [320].
Nutrition (n = 2): Two studies mentioned that UCTs improved the quality of children’s diets and increased the food availability in the house [317] as well as households’ access to food [320].
Child development (n = 1): One study reported that a UCT programme had a preventive effect on children’s growth in Togo [314].
Introduction of user fees (n = 5)
Across many sub-Saharan African countries user fees are paid directly at the point-of-care as the introduction of fees generates revenue for health systems and may decrease the demand for unnecessary care [321,323]. Five studies that evaluated the effect of the introduction of user fees on healthcare utilization were included in this study [321–325].
Healthcare utilization (n = 5): Three studies reported that this policy decreased the utilization of inpatient care by women and children in the rural areas of Zambia [321], decreased the use of health services and presentation for care by women in Mali [323] and decreased the number of skilled birth deliveries and antenatal care in Malawi [325]. One study reported an increase in the use of cervical screening despite the introduction of a fee-for-service policy [322]. Another study reported that the increase in prices did not have any disproportionate effect on the use of family planning and reproductive health services among lower-income women [324].
Micro-credit (n = 2)
Microcredit extends loans to the impoverished without requiring collateral thereby including those who would o’t have been able to access credit otherwise [405]. One study reported that microcredit positively affected child mortality [405]. Another study highlighted that microcredit can complement health insurance in enhancing child health by increasing households’ affordability for out-of-pocket health expenditures, protecting them from the financial risks associated with health insurance plans and improving rural households’ access to insurance plans [326].
Equity considerations
The scoping review’s findings highlight that CCT and voucher programmes can improve the utilization of maternal and child health services as well as the health outcomes for the poor and the disadvantaged. However, multiple implementation challenges impact the effectiveness of these programmes such as the complex eligibility procedures, unsustainability and misuse of transfers. Other barriers included irregular cash transfers, unclear payment mechanisms, and cultural barriers [24]. An increased workload and the insufficient healthcare personnel and infrastructure can also limit the effectiveness of CCT and voucher programmes in providing access to high-quality care to vulnerable groups. The various insurance schemes were found to have positive effect on healthcare utilization, healthcare expenditures, mortality rates and morbidity especially among the vulnerable populations including the poor, those residing in rural areas and other vulnerable populations. Few studies suggested that inequities in health coverage persisted under these programmes and schemes among the lower-income, less educated and those residing in remote regions, implying that demand-side interventions alone are insufficient in achieving equity. This also could be attributed to the persistence of other financial barriers and a lack of awareness about the programmes.
Findings showed that combining demand-side interventions with supply-side interventions can have better effect on maternal and child health outcomes [33,408]. Although user fee exemption of healthcare was found to have a positive impact on increasing utilization for the lower-income, leading to more equity, its effect is limited due to other financial and non-financial barriers. PBF was also found to have a limited impact on increasing utilization of maternal and child health services among the poorest, suggesting that financial incentives for providers might not be enough to improve equity due to non-financial barriers to access at the demand side. Not enough evidence was identified to draw conclusions on the other financial interventions such as UCTs, the introduction of user fees and microcredit. Also, evidence on the effect of financial interventions on improving equity for those living with a disablity, those less educated and LGBTIQ+ community was insufficient to draw any conclusions.
Discussion
Principal findings and research gaps
This scoping review mapped the literature on financing interventions and measures aiming to improve equity for WCAH. This review can inform the agendas of funders and researchers working in the field of WCAH of potential knowledge gaps. The review highlighted the lack of studies assessing financial interventions targeting adolescents and newborns; the majority of the studies focused on women and children.
The review’s findings show that most of the included studies assessed CCTs, health insurance, vouchers and user fee exemptions while fewer studies addressed supply-side interventions such as PBF. The findings highlight that even when financial barriers are removed, inequities can persist due to other non-financial barriers to access including distance to catchment primary health facility, literacy, parity and religion. Financial interventions and measures are not enough unless coupled with other non-financial interventions that address barriers such as knowledge and geographical barriers. The findings suggest a strong synergy between the effects of supply-side and demand-side incentives. The engagement of concerned stakeholders is crucial for the successful implementation of financial interventions and design of financial interventions should be context-specific. Maintaining the sustainability of the effect and the quality of care while implementing financial interventions is crucial to achieving a positive impact on the target population. Successful implementations require adequate health system inputs, such as a capable, motivated and sufficient health workforce, and provision of reimbursements, supplies and equipment. The findings can inform the design of equitable health financing policies and health system reform efforts essential in moving toward UHC [436].
This review highlighted the scarcity of studies addressing the effect of financial interventions on addressing inequities related to education, age, disability and sexual orientation. The included studies mainly focused on financing mechanisms aiming to improve socioeconomics and place of residence disparities. This finding reflects a gap in evidence of financing mechanisms targeted at people living with a disability and LGBTIQ+ communities. Other reviews also focused on equity of health financing based on SES and place of residence but with a lesser focus on other equity components [437,438].
Most of the studies were conducted by authors affiliated with institutions based in high-income countries. This can be interpreted as a result of limited research capacity in low-income countries to conduct health policy and systems research. This finding corroborates other studies and reviews, highlighting the imbalance of research capacity between high-income and low-income countries [439–441]. This scoping review found that studies are mostly funded by governments, academic institutions, private not-for-profits and international organizations.
Strengths and limitations
To our knowledge, this scoping review is the first to map financing interventions and measures to improve equity in WCAH in LMICs. One strength of the review is that it followed JBI guidance for conducting scoping reviews [18] and the PRISMA-ScR for reporting scoping reviews [19]. One limitation is that the review aimed to include studies addressing at least one PROGRESS-plus equity component without due attention to the general pattern of inequity in low-income and LMICs where 91.9% of the global population living in extreme poverty, namely with less than US$ 2.15 per day, resides [442]. Another limitation is the fact that we did not search non-English databases although we did include non-English articles.
Implications on policy and research
The latest data on progress towards the SDGs shows that vulnerable populations are not doing well with WCAH outcome improvements. The COVID-19 pandemic and climate change, which impact the most vulnerable the hardest, including those living in conflict settings, pose challenges. These intersectional issues amplify the exclusion and marginalization of the most vulnerable. Dedicated policy efforts are required to redress the imbalance. This review provides evidence on different financing interventions that may be used to address the needs of the most vulnerable communities and improve equity. The review can be used to inform future research on financing interventions and measures to improve equity when addressing WCAH in LMICs by revealing current knowledge gaps.
Supporting information
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
The Partnership for Maternal, Newborn and Child Health (PMNCH) gratefully acknowledges the contributions of the many individuals and organizations who contributed to this report. PMNCH is the world’s largest alliance for women’s, children’s and adolescents’ health and well-being, with over 1400 partner organizations working together through 10 constituency groups. Its work is funded by a range of government and philanthropic donors. More information can be found on https://pmnch.who.int/.
Data Availability
All data underpinning the results of the scoping review are found within the paper and in the Supporting Information files.
Funding Statement
This work is funded by the Partnership for Maternal, Newborn and Child Health (PMNCH) at the World Health Organization (WHO). The Partnership for Maternal, Newborn and Child Health (PMNCH) has contributed to the development of this work, as part of its 2021–2025 strategy and related workplans. PMNCH is the world’s largest alliance for women’s, children’s and adolescents’ health and well-being, with over 1400 partner organizations working together through 10 constituency groups. Its work is funded by a range of government and philanthropic donors, which had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.World Health Organization. Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division: executive summary [Internet]. Geneva: World Health Organization; 2019. Available from: https://iris.who.int/handle/10665/327596. [Google Scholar]
- 2.Protect the progress: rise, refocus and recover. 2020 progress report on the Every Woman Every Child Global Strategy for Women’s, Children’s and Adolescents’ Health (2016–2030). Geneva: World Health Organization and the United Nations Children’s Fund (UNICEF); 2020. Licence: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- 3.Trends in maternal mortality 2000 to 2020: estimates by WHO, UNICEF, UNFPA, World Bank Group and UNDESA/Population Division. Geneva: World Health Organization; 2023. Licence: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- 4.Bendavid E, Boerma T, Akseer N, Langer A, Malembaka EB, Okiro EA, et al. The effects of armed conflict on the health of women and children. The Lancet. 2021;397(10273):522–32. doi: 10.1016/S0140-6736(21)00131-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sharrow D, Hug L, Lee S, Liu Y, You D, on behalf of the United Nations Inter-agency Group for Child Mortality Estimation (UN IGME). Levels & Trends in Child Mortality. Estimates developed by the UN Inter-agency Group for Child Mortality Estimation. Report 2021. [Internet]. Available from: file:///C:/Users/ss280/Downloads/UNICEF-IGME-2021-Child-Mortality-Report.pdf. [accessed 2022 May]. [Google Scholar]
- 6.New UNFPA data reveals that nearly 12 million women lost access to contraception due to disruptions caused by the pandemic, leading to 1.4 million unintended pregnancies [press release]. New York: UNFPA; 2021. Mar 11 [Internet]. Available from: https://www.unfpa.org/press/new-unfpa-data-reveals-nearly-12-million-women-lost-access-contraception-due-disruptions. [accessed 2022 May]. [Google Scholar]
- 7.Chmielewska B, Barratt I, Townsend R, Kalafat E, van der Meulen J, Gurol-Urganci I, et al. Effects of the COVID-19 pandemic on maternal and perinatal outcomes: a systematic review and meta-analysis. Lancet Glob Health. 2021;9(6):e759–e72. doi: 10.1016/S2214-109X(21)00079-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zero dose’ children: almost 14 million get no vaccines [Internet]. Interview: Gavi Deputy CEO Anuradha Gupta says ‘zero dose’ children account for disproportionate number of early deaths. 2022. Apr 28. Vaccines Work. Available from: https://www.gavi.org/vaccineswork/zero-dose-children-almost-14-million-get-no-vaccines. [accessed 2023 May] [Google Scholar]
- 9.Kc A, Gurung R, Kinney MV, Sunny AK, Moinuddin M, Basnet O, et al. Effect of the COVID-19 pandemic response on intrapartum care, stillbirth, and neonatal mortality outcomes in Nepal: a prospective observational study. The Lancet Global Health. 2020;8(10):e1273–e81. doi: 10.1016/S2214-109X(20)30345-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gopinath G. A Long, Uneven and Uncertain Ascent. IMF Blog Retrieved from: https://blogsimforg/2020/10/13/a-long-uneven-and-uncertain-ascent/ 2020.
- 11.Lakner C, Yonzan N, Gerszon M, Castaneda Aguilar A, Wu H. Updated estimates of the impact of COVID-19 on global poverty: Looking back at 2020 and the outlook for 2021 [Internet]. World Bank; 2021. Jan 11. Available from: https://blogs.worldbank.org/en/opendata/updated-estimates-impact-covid-19-global-poverty-looking-back-2020-and-outlook-2021. [accessed 2022 May]. [Google Scholar]
- 12.Immunization coverage [press release]. Geneva: World Health Organization; [Internet]. Available from: https://www.who.int/news-room/fact-sheets/detail/immunization-coverage. [accessed 2023 May]. [Google Scholar]
- 13.United Nations. A UN framework for the immediate socio-economic response to COVID-19 [Internet]. April 2020. Available from: https://unsdg.un.org/sites/default/files/2020-04/UN-framework-for-the-immediate-socio-economic-response-to-COVID-19.pdf. [accessed 2021 May]. [Google Scholar]
- 14.COVID-19, conflict, climate crises exacerbate setbacks for childhood and adolescent prospects, women’s rights [press release]. World Health Organization; 2022. Oct 18 [Internet]. Available from: https://www.who.int/news/item/18-10-2022-staggering-backsliding-across-women-s—children-s-and-adolescents—health-revealed-in-new-un-analysis. [accessed 2023 May]. [Google Scholar]
- 15.Born too soon: decade of action on preterm birth [Internet]. Geneva: World Health Organization; 2023. Licence: CC BY-NC-SA 3.0 IGO. Available from: https://creativecommons.org/licenses/by-nc-sa/3.0/igo/. [accessed 2022 May]. [Google Scholar]
- 16.Protect the promise: 2022 progress report on the Every Woman Every Child Global Strategy for Women’s, Children’s and Adolescents’ Health (2016–2030) [Internet]. Geneva: World Health Organization and the United Nations Children’s Fund (UNICEF); 2022. Licence: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- 17.Bjerde A. Rethinking Development in an Age of Crisis. 2023, World Bank Blogs: World Bank Blogs. [Google Scholar]
- 18.Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evidence Synthesis. 2020;18(10). doi: 10.11124/JBIES-20-00167 [DOI] [PubMed] [Google Scholar]
- 19.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Annals of Internal Medicine. 2018;169(7):467–73. doi: 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 20.PMNCH. PROTECTING THE PROGRESS FOR WOMEN, CHILDREN AND ADOLESCENTS IN THE COVID-19 CRISIS: more and better financing for improved equity. 2020. [Google Scholar]
- 21.Braveman P, Gruskin S. Defining equity in health. Journal of Epidemiology and Community Health. 2003;57(4):254. doi: 10.1136/jech.57.4.254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.The Work Bank. World Bank Country and Lending Groups. 2024; Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. [Google Scholar]
- 23.Randive B, Diwan V, De Costa A. India’s Conditional Cash Transfer Programme (the JSY) to Promote Institutional Birth: Is There an Association between Institutional Birth Proportion and Maternal Mortality? PLoS ONE. 2013;8(6). doi: 10.1371/journal.pone.0067452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lim SS, Dandona L, Hoisington JA, James SL, Hogan MC, Gakidou E. India’s Janani Suraksha Yojana, a conditional cash transfer programme to increase births in health facilities: an impact evaluation. The Lancet. 2010;375(9730):2009–23. doi: 10.1016/S0140-6736(10)60744-1 [DOI] [PubMed] [Google Scholar]
- 25.Kusuma D, Cohen J, McConnell M, Berman P. Can cash transfers improve determinants of maternal mortality? Evidence from the household and community programs in Indonesia. Social Science and Medicine. 2016;163:10–20. [DOI] [PubMed] [Google Scholar]
- 26.de Brauw A, Peterman A. Can conditional cash transfers improve maternal health care? Evidence from El Salvador’s Comunidades Solidarias Rurales program. Health Economics (United Kingdom). 2020;29(6):700–15. doi: 10.1002/hec.4012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rasella D, Aquino R, Santos CA, Paes-Sousa R, Barreto ML. Effect of a conditional cash transfer programme on childhood mortality: a nationwide analysis of Brazilian municipalities. Lancet. 2013;382(9886):57–64. doi: 10.1016/S0140-6736(13)60715-1 [DOI] [PubMed] [Google Scholar]
- 28.Shei A. Brazil’s conditional cash transfer program associated with declines in infant mortality rates. Health Affairs. 2013;32(7):1274–81. doi: 10.1377/hlthaff.2012.0827 [DOI] [PubMed] [Google Scholar]
- 29.Rasella D, Alves FJO, Reboucas P, de Jesus GS, Barreto ML, Campello T, et al. Long-term impact of a conditional cash transfer programme on maternal mortality: a nationwide analysis of Brazilian longitudinal data. BMC Medicine. 2021;19(1):127. doi: 10.1186/s12916-021-01994-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Glassman A, Duran D, Fleisher L, Singer D, Sturke R, Angeles G, et al. Impact of conditional cash transfers on maternal and newborn health. Journal of Health, Population and Nutrition. 2013;31(4 SUPPL.2):S48–S66. [PubMed] [Google Scholar]
- 31.Poirier MJP. Geographic targeting and normative frames: Revisiting the equity of conditional cash transfer program distribution in bolivia, colombia, ecuador, and peru. International Journal for Equity in Health. 2020;19(1). doi: 10.1186/s12939-020-01233-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cruz RCS, Moura LBA, Soares Neto JJ. Conditional cash transfers and the creation of equal opportunities of health for children in low and middle-income countries: a literature review. International Journal for Equity in Health. 2017;16(1):161. doi: 10.1186/s12939-017-0647-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Randive B, San Sebastian M, De Costa A, Lindholm L. Inequalities in institutional delivery uptake and maternal mortality reduction in the context of cash incentive program, Janani Suraksha Yojana: Results from nine states in India. Social Science and Medicine. 2014;123:1–6. doi: 10.1016/j.socscimed.2014.10.042 [DOI] [PubMed] [Google Scholar]
- 34.de Souza AA, Mingoti SA, Paes-Sousa R, Heller L. Combination of conditional cash transfer program and environmental health interventions reduces child mortality: an ecological study of Brazilian municipalities. BMC public health. 2021;21(1):627. doi: 10.1186/s12889-021-10649-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barber SL, Gertler PJ. Empowering women to obtain high quality care: evidence from an evaluation of Mexico’s conditional cash transfer programme. Health Policy & Planning. 2009;24(1):18–25. doi: 10.1093/heapol/czn039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lahariya C, Mishra A, Nandan D, Gautam P, Gupta S. Additional cash incentive within a conditional cash transfer scheme: a ’controlled before and during’ design evaluation study from India. Indian journal of public health. 2011;55(2):115–20. doi: 10.4103/0019-557X.85245 [DOI] [PubMed] [Google Scholar]
- 37.Barber SL. Mexico’s conditional cash transfer programme increases cesarean section rates among the rural poor. European journal of public health. 2010;20(4):383–8. doi: 10.1093/eurpub/ckp184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Paes-Sousa R, Santos LMP, Miazaki ÉS. Effects of a conditional cash transfer programme on child nutrition in Brazil. Bulletin of the World Health Organization. 2011;89:496–503. doi: 10.2471/BLT.10.084202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Triyana M, Shankar AH. The effects of a household conditional cash transfer programme on coverage and quality of antenatal care: a secondary analysis of Indonesia’s pilot programme. BMJ Open. 2017;7(10):e014348. doi: 10.1136/bmjopen-2016-014348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lopez-Arana S, Avendano M, van Lenthe FJ, Burdorf A. The impact of a conditional cash transfer programme on determinants of child health: evidence from Colombia. Public health nutrition. 2016;19(14):2629–42. doi: 10.1017/S1368980016000240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Morris SS, Flores R, Olinto P, Medina JM. Monetary incentives in primary health care and effects on use and coverage of preventive health care interventions in rural Honduras: cluster randomised trial. Lancet. 2004;364(9450):2030–7. doi: 10.1016/S0140-6736(04)17515-6 [DOI] [PubMed] [Google Scholar]
- 42.Owusu-Addo E, Cross R. The impact of conditional cash transfers on child health in low- and middle-income countries: a systematic review. International Journal of Public Health. 2014;59(4):609–18. doi: 10.1007/s00038-014-0570-x [DOI] [PubMed] [Google Scholar]
- 43.Kandpal E, Alderman H, Friedman J, Filmer D, Onishi J, Avalos J. A Conditional Cash Transfer Program in the Philippines Reduces Severe Stunting. Journal of Nutrition. 2016;146(9):1793–800. doi: 10.3945/jn.116.233684 [DOI] [PubMed] [Google Scholar]
- 44.Baba-Ari F, Eboreime EA, Hossain M. Conditional Cash Transfers for Maternal Health Interventions: Factors Influencing Uptake in North-Central Nigeria. International Journal of Health Policy & Management. 2018;7(10):934–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sosa-Rubi SG, Walker D, Servan E, Bautista-Arredondo S. Learning effect of a conditional cash transfer programme on poor rural women’s selection of delivery care in Mexico. Health Policy & Planning. 2011;26(6):496–507. doi: 10.1093/heapol/czq085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lagarde M, Haines A, Palmer N. The impact of conditional cash transfers on health outcomes and use of health services in low and middle income countries. Cochrane Database of Systematic Reviews. 2009(4). doi: 10.1002/14651858.CD008137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Edmond KM, Foshanji AI, Naziri M, Higgins-Steele A, Burke JM, Strobel N, et al. Conditional cash transfers to improve use of health facilities by mothers and newborns in conflict affected countries, a prospective population based intervention study from Afghanistan. BMC Pregnancy & Childbirth. 2019;19(1):193. doi: 10.1186/s12884-019-2327-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Thongkong N, van de Poel E, Roy SS, Rath S, Houweling TA. How equitable is the uptake of conditional cash transfers for maternity care in India? Evidence from the Janani Suraksha Yojana scheme in Odisha and Jharkhand. International Journal for Equity in Health. 2017;16(1):48. doi: 10.1186/s12939-017-0539-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Thomas R. Conditional cash transfers to improve education and health: an ex ante evaluation of Red de Proteccion Social, Nicaragua. Health Economics. 2012;21(10):1136–54. [DOI] [PubMed] [Google Scholar]
- 50.Njuguna J. Impact of a Conditional Cash Transfer Program Aimed at Promoting Maternal and Child Health Services in Kakamega County, Kenya. Journal of health care for the poor and underserved. 2019;30(1):329–38. doi: 10.1353/hpu.2019.0024 [DOI] [PubMed] [Google Scholar]
- 51.Sidney K, Tolhurst R, Jehan K, Diwan V, De Costa A. ’The money is important but all women anyway go to hospital for childbirth nowadays’—a qualitative exploration of why women participate in a conditional cash transfer program to promote institutional deliveries in Madhya Pradesh, India. BMC Pregnancy & Childbirth. 2016;16:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lopez-Arana S, Avendano M, Forde I, Van Lenthe FJ, Burdorf A. Conditional cash transfers and the double burden of malnutrition among children in Colombia: A quasi-experimental study. British Journal of Nutrition. 2016;115(10):1780–9. doi: 10.1017/S0007114516000714 [DOI] [PubMed] [Google Scholar]
- 53.Landrian A, Phillips BS, Singhal S, Mishra S, Kajal F, Sudhinaraset M. Do you need to pay for quality care? Associations between bribes and out-of-pocket expenditures on quality of care during childbirth in India. Health policy and planning. 2020;35(5):600–8. doi: 10.1093/heapol/czaa008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kennedy CE, Brahmbhatt H, Likindikoki S, Beckham SW, Mbwambo JK, Kerrigan D. Exploring the potential of a conditional cash transfer intervention to reduce HIV risk among young women in Iringa, Tanzania. AIDS Care—Psychological and Socio-Medical Aspects of AIDS/HIV. 2014;26(3):275–81. doi: 10.1080/09540121.2013.824539 [DOI] [PubMed] [Google Scholar]
- 55.Fernald LC, Gertler PJ, Hou X. Cash component of conditional cash transfer program is associated with higher body mass index and blood pressure in adults. Journal of Nutrition. 2008;138(11):2250–7. doi: 10.3945/jn.108.090506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pettifor A, MacPhail C, Selin A, Gómez-Olivé FX, Rosenberg M, Wagner RG, et al. HPTN 068: a randomized control trial of a conditional cash transfer to reduce HIV infection in young women in South Africa—study design and baseline results. AIDS and Behavior. 2016;20:1863–82. doi: 10.1007/s10461-015-1270-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Barber SL, Gertler PJ. The impact of Mexico’s conditional cash transfer programme, Oportunidades, on birthweight. Tropical Medicine & International Health. 2008;13(11):1405–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fernald LC, Gertler PJ, Neufeld LM. Role of cash in conditional cash transfer programmes for child health, growth, and development: an analysis of Mexico’s Oportunidades. Lancet. 2008;371(9615):828–37. doi: 10.1016/S0140-6736(08)60382-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fink G, Rockers PC. Financial Incentives, Targeting, and Utilization of Child Health Services: Experimental Evidence from Zambia. Health Economics (United Kingdom). 2017;26(10):1307–21. doi: 10.1002/hec.3404 [DOI] [PubMed] [Google Scholar]
- 60.Morris SS, Olinto P, Flores R, Nilson EA, Figueiro AC. Conditional cash transfers are associated with a small reduction in the rate of weight gain of preschool children in northeast Brazil. Journal of Nutrition. 2004;134(9):2336–41. doi: 10.1093/jn/134.9.2336 [DOI] [PubMed] [Google Scholar]
- 61.Baird S, Chirwa E, McIntosh C, Özler B. The short-term impacts of a schooling conditional cash transfer program on the sexual behavior of young women. Health Economics. 2010;19(SUPPL. 1):55–68. doi: 10.1002/hec.1569 [DOI] [PubMed] [Google Scholar]
- 62.Servan-Mori E, Cerecero-Garcia D, Heredia-Pi IB, Pineda-Antunez C, Sosa-Rubi SG, Nigenda G. Improving the effective maternal-child health care coverage through synergies between supply and demand-side interventions: evidence from Mexico. Journal of global health. 2019;9(2):020433. doi: 10.7189/jogh.09.020433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rahman MM, Pallikadavath S. How much do conditional cash transfers increase the utilization of maternal and child health care services? New evidence from Janani Suraksha Yojana in India. Economics & Human Biology. 2018;31:164–83. doi: 10.1016/j.ehb.2018.08.007 [DOI] [PubMed] [Google Scholar]
- 64.Gertler P. Do Conditional Cash Transfers Improve Child Health? Evidence from PROGRESA’s Control Randomized Experiment. American Economic Review. 2004;94(2):336–41. [DOI] [PubMed] [Google Scholar]
- 65.Olson Z, Clark RG, Reynolds SA. Can a conditional cash transfer reduce teen fertility? The case of Brazil’s Bolsa Familia. Journal of Health Economics. 2019;63:128–44. doi: 10.1016/j.jhealeco.2018.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Forde I, Chandola T, Garcia S, Marmot MG, Attanasio O. The impact of cash transfers to poor women in Colombia on BMI and obesity: Prospective cohort study. International Journal of Obesity. 2012;36(9):1209–14. doi: 10.1038/ijo.2011.234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fernald LC, Gertler PJ, Neufeld LM. 10-year effect of Oportunidades, Mexico’s conditional cash transfer programme, on child growth, cognition, language, and behaviour: a longitudinal follow-up study. The Lancet. 2009;374(9706):1997–2005. doi: 10.1016/S0140-6736(09)61676-7 [DOI] [PubMed] [Google Scholar]
- 68.Rao KD, Kachwaha S, Kaplan A, Bishai D. Not just money: what mothers value in conditional cash transfer programs in India. BMJ Global Health. 2020;5(10):10. doi: 10.1136/bmjgh-2020-003033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Skovdal M, Robertson L, Mushati P, Dumba L, Sherr L, Nyamukapa C, et al. Acceptability of conditions in a community-led cash transfer programme for orphaned and vulnerable children in Zimbabwe. Health policy and planning. 2014;29(7):809–17. doi: 10.1093/heapol/czt060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gopichandran V, Chetlapalli SK. Conditional cash transfer to promote institutional deliveries in India: Toward a sustainable ethical model to achieve MDG 5A. Public Health Ethics. 2012;5(2):173–80. [Google Scholar]
- 71.Barham T, Maluccio JA. Eradicating diseases: The effect of conditional cash transfers on vaccination coverage in rural Nicaragua. Journal of Health Economics. 2009;28(3):611–21. doi: 10.1016/j.jhealeco.2008.12.010 [DOI] [PubMed] [Google Scholar]
- 72.Stecklov G, Winters P, Todd J, Regalia F. Unintended effects of poverty programmes on childbearing in less developed countries: Experimental evidence from Latin America. Population Studies. 2007;61(2):125–40. doi: 10.1080/00324720701300396 [DOI] [PubMed] [Google Scholar]
- 73.Neves JA, Vasconcelos FAG, Machado ML, Recine E, Garcia GS, Medeiros MAT. The Brazilian cash transfer program (Bolsa Familia): A tool for reducing inequalities and achieving social rights in Brazil. Global Public Health. 2020:1–17. [DOI] [PubMed] [Google Scholar]
- 74.Kilburn K, Hughes JP, MacPhail C, Wagner RG, Gomez-Olive FX, Kahn K, et al. Cash Transfers, Young Women’s Economic Well-Being, and HIV Risk: Evidence from HPTN 068. AIDS & Behavior. 2019;23(5):1178–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Andersen CT, Reynolds SA, Behrman JR, Crookston BT, Dearden KA, Escobal J, et al. Participation in the Juntos Conditional Cash Transfer Program in Peru Is Associated with Changes in Child Anthropometric Status but Not Language Development or School Achievement. Journal of Nutrition. 2015;145(10):2396–405. doi: 10.3945/jn.115.213546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Leroy JL, Garcia-Guerra A, Garcia R, Dominguez C, Rivera J, Neufeld LM. The Oportunidades program increases the linear growth of children enrolled at young ages in urban Mexico. Journal of Nutrition. 2008;138(4):793–8. doi: 10.1093/jn/138.4.793 [DOI] [PubMed] [Google Scholar]
- 77.Gupta A, Fledderjohann J, Reddy H, Raman VR, Stuckler D, Vellakkal S. Barriers and prospects of India’s conditional cash transfer program to promote institutional delivery care: a qualitative analysis of the supply-side perspectives. BMC Health Services Research. 2018;18(1):40. doi: 10.1186/s12913-018-2849-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sidney K, Diwan V, El-Khatib Z, De Costa A. India’s JSY cash transfer program for maternal health: Who participates and who doesn’t—a report from Ujjain district. Reproductive Health. 2012:2. doi: 10.1186/1742-4755-9-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Perez-Lu JE, Carcamo C, Nandi A, Kaufman JS. Health effects of ’Juntos’, a conditional cash transfer programme in Peru. Maternal & Child Nutrition. 2017;13(3):07. doi: 10.1111/mcn.12348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Calvasina P O’Campo P, Pontes MM, Oliveira JB, Vieira-Meyer A. The association of the Bolsa Familia Program with children’s oral health in Brazil. BMC Public Health. 2018;18(1):1186. doi: 10.1186/s12889-018-6084-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Shei A, Costa F, Reis MG, Ko AI. The impact of Brazil’s Bolsa Familia conditional cash transfer program on children’s health care utilization and health outcomes. BMC International Health & Human Rights. 2014;14:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Okeke EN, Wagner Z, Abubakar IS. Maternal Cash Transfers Led To Increases In Facility Deliveries And Improved Quality Of Delivery Care In Nigeria. Health Affairs. 2020;39(6):1051–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Andrade MV, Chein F, de Souza LR, Puig-Junoy J. Income transfer policies and the impacts on the immunization of children: The Bolsa Família Program. Cadernos de Saude Publica. 2012;28(7):1347–58. [DOI] [PubMed] [Google Scholar]
- 84.Gopalan SS, Durairaj V. Addressing maternal healthcare through demand side financial incentives: experience of Janani Suraksha Yojana program in India. BMC Health Services Research. 2012;12:319. doi: 10.1186/1472-6963-12-319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Owusu-Addo E. Perceived impact of Ghana’s conditional cash transfer on child health. Health Promotion International. 2016;31(1):33–43. doi: 10.1093/heapro/dau069 [DOI] [PubMed] [Google Scholar]
- 86.Witvorapong N, Foshanji AI. The impact of a conditional cash transfer program on the utilization of non-targeted services: Evidence from Afghanistan. Social Science & Medicine. 2016;152:87–95. doi: 10.1016/j.socscimed.2016.01.043 [DOI] [PubMed] [Google Scholar]
- 87.Adato M, Bassett L. Social protection to support vulnerable children and families: the potential of cash transfers to protect education, health and nutrition. AIDS Care. 2009;21 Suppl 1:60–75. doi: 10.1080/09540120903112351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Oduenyi C, Ordu V, Okoli U. Perspectives of beneficiaries, health service providers, and community members on a maternal and child health conditional cash transfer pilot programme in Nigeria. International Journal of Health Planning & Management. 2019;34(2):e1054–e73. doi: 10.1002/hpm.2741 [DOI] [PubMed] [Google Scholar]
- 89.Thomas D, Sarangi BL, Garg A, Ahuja A, Meherda P, Karthikeyan SR, et al. Closing the health and nutrition gap in Odisha, India: A case study of how transforming the health system is achieving greater equity. Social Science and Medicine. 2015;145:154–62. doi: 10.1016/j.socscimed.2015.06.010 [DOI] [PubMed] [Google Scholar]
- 90.Darney B, Weaver M, Sosa-Rubi S, Walker D, Gakidou E. Oportunidades conditional cash transfer program: Impact on adolescent pregnancy in rural Mexico. Contraception. 2012;86(3):292. [Google Scholar]
- 91.Moncayo AL, Granizo G, Grijalva MJ, Rasella D. Strong effect of Ecuador’s conditional cash transfer program on childhood mortality from poverty-related diseases: a nationwide analysis. BMC public health. 2019;19(1):1132. doi: 10.1186/s12889-019-7457-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Vellakkal S, Reddy H, Gupta A, Chandran A, Fledderjohann J, Stuckler D. A qualitative study of factors impacting accessing of institutional delivery care in the context of India’s cash incentive program. Soc Sci Med. 2017;178:55–65. doi: 10.1016/j.socscimed.2017.01.059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kusuma D, McConnell M, Berman P, Cohen J. The impact of household and community cash transfers on children’s food consumption in Indonesia. Preventive Medicine. 2017;100:152–8. doi: 10.1016/j.ypmed.2017.04.020 [DOI] [PubMed] [Google Scholar]
- 94.Powell-Jackson T, Mazumdar S, Mills A. Financial incentives in health: New evidence from India’s Janani Suraksha Yojana. Journal of Health Economics. 2015;43:154–69. doi: 10.1016/j.jhealeco.2015.07.001 [DOI] [PubMed] [Google Scholar]
- 95.Bogg L, Diwan V, Vora KS, DeCosta A. Impact of Alternative Maternal Demand-Side Financial Support Programs in India on the Caesarean Section Rates: Indications of Supplier-Induced Demand. Matern Child Health J. 2016;20(1):11–5. doi: 10.1007/s10995-015-1810-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Anderson I, Axelson H, Tan BK. The other crisis: the economics and financing of maternal, newborn and child health in Asia. Health policy and planning. 2011;26(4):288–97. doi: 10.1093/heapol/czq067 [DOI] [PubMed] [Google Scholar]
- 97.Rout SK, Mahapatra S. Has the public health system provided adequate financial risk protection for child birth conditions–evidences from an Eastern Indian state. International journal of health policy and management. 2019;8(3):145 doi: 10.15171/ijhpm.2018.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Prencipe L, Houweling TA, van Lenthe FJ, Palermo T. Do conditional cash transfers improve mental health? Evidence from Tanzania’s governmental social protection program. Journal of Adolescent Health. 2021;69(5):797–805. doi: 10.1016/j.jadohealth.2021.04.033 [DOI] [PubMed] [Google Scholar]
- 99.Ramos D, da Silva NB, Ichihara MY, Fiaccone RL, Almeida D, Sena S, et al. Conditional cash transfer program and child mortality: A cross-sectional analysis nested within the 100 Million Brazilian Cohort. PLoS medicine. 2021;18(9):e1003509. doi: 10.1371/journal.pmed.1003509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.de Souza EL, de Rossi Ferreira VL, Waldman EA, Sato APS. Effect of a conditional cash transfer programme on infant up-to-date and timely vaccination. J Epidemiol Community Health. 2022;76(7):685–93. doi: 10.1136/jech-2021-217964 [DOI] [PubMed] [Google Scholar]
- 101.von Haaren P, Klonner S. Lessons learned? Intended and unintended effects of India’s second‐generation maternal cash transfer scheme. Health Economics. 2021;30(10):2468–86. doi: 10.1002/hec.4390 [DOI] [PubMed] [Google Scholar]
- 102.Ziebold C, Paula CS, Santos IS, Barros FC, Munhoz TN, Lund C, et al. Conditional cash transfers and adolescent mental health in Brazil: Evidence from the 2004 Pelotas Birth Cohort. Journal of Global Health. 2021;11. doi: 10.7189/jogh.11.04066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Leroy JL, Koch B, Roy S, Gilligan D, Ruel M. Social assistance programs and birth outcomes: a systematic review and assessment of nutrition and health pathways. The Journal of Nutrition. 2021;151(12):3841–55. doi: 10.1093/jn/nxab292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Lucas ADP, de Oliveira Ferreira M, Lucas TDP, Salari P. The intergenerational relationship between conditional cash transfers and newborn health. BMC public health. 2022;22(1):201. doi: 10.1186/s12889-022-12565-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Godha D, Hotchkiss DR. A decade of conditional cash transfer programs for reproductive health in India: How did equality fare? BMC Public Health. 2022;22(1):394. doi: 10.1186/s12889-022-12563-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Goli S, Pradhan J, Reja T. The unending burden of high out-of-pocket expenditure on institutional deliveries in India. Public Health. 2021;193:43–7. doi: 10.1016/j.puhe.2021.01.029 [DOI] [PubMed] [Google Scholar]
- 107.Onwuchekwa C, Verdonck K, Marchal B. Systematic review on the impact of conditional cash transfers on child health service utilisation and child health in sub-Saharan Africa. Frontiers in public health. 2021;9:643621. doi: 10.3389/fpubh.2021.643621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Jacobs W, Downey LE. Impact of conditional cash transfer programmes on antenatal care service uptake in low and middle-income countries: a systematic review. BMJ open. 2022;12(11):e064673. doi: 10.1136/bmjopen-2022-064673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Khoza N, Stadler J, MacPhail C, Chikandiwa A, Brahmbhatt H, Delany-Moretlwe S. Cash transfer interventions for sexual health: meanings and experiences of adolescent males and females in inner-city Johannesburg. BMC Public Health. 2018;18(1):120. doi: 10.1186/s12889-018-5027-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ajayi AI, Akpan W. Who benefits from free institutional delivery? evidence from a cross sectional survey of North Central and Southwestern Nigeria. BMC health services research. 2017;17(1):620. doi: 10.1186/s12913-017-2560-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Dennis ML, Benova L, Goodman C, Barasa E, Abuya T, Campbell OMR. Examining user fee reductions in public primary healthcare facilities in Kenya, 1997–2012: Effects on the use and content of antenatal care. International Journal for Equity in Health. 2020;19(1). doi: 10.1186/s12939-020-1150-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Amoako Johnson F. A geospatial analysis of the impacts of maternity care fee payment policies on the uptake of skilled birth care in Ghana. BMC pregnancy and childbirth. 2016;16(1):1–13. doi: 10.1186/s12884-016-0833-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Lamichhane P, Sharma A, Mahal A. Impact evaluation of free delivery care on maternal health service utilisation and neonatal health in Nepal. Health policy and planning. 2017;32(10):1427–36. doi: 10.1093/heapol/czx124 [DOI] [PubMed] [Google Scholar]
- 114.Shrestha G, Paudel P, Shrestha PR, Jnawali SP, Jha D, Ojha TR, Lamichhane B. Free Newborn Care Services: A New Initiative in Nepal. Journal of Nepal Health Research Council. 2018;16(3):340–4. [PubMed] [Google Scholar]
- 115.Zombré D, De Allegri M, Platt RW, Ridde V, Zinszer K. An evaluation of healthcare use and child morbidity 4 years after user fee removal in rural Burkina Faso. Maternal and child health journal. 2019;23:777–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Kruk ME, Mbaruku G, Rockers PC, Galea S. User fee exemptions are not enough: out‐of‐pocket payments for ‘free’delivery services in rural Tanzania. Tropical medicine & international health. 2008;13(12):1442–51. [DOI] [PubMed] [Google Scholar]
- 117.Ansu-Mensah M, Danquah FI, Bawontuo V, Ansu-Mensah P, Mohammed T, Udoh RH, Kuupiel D. Quality of care in the free maternal healthcare era in sub-Saharan Africa: a scoping review of providers’ and managers’ perceptions. BMC Pregnancy and Childbirth. 2021;21:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Dalinjong PA, Wang AY, Homer CSE. The implementation of the free maternal health policy in rural Northern Ghana: synthesised results and lessons learnt. BMC Research Notes. 2018;11(1):341. doi: 10.1186/s13104-018-3452-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Nkwenti HE, Ngowe MN, Fokam P, Fonyuy JN, Atanga SN, Nkfusai NC, et al. The effect of subsidized malaria treatment among under-five children in the Buea Health District, Cameroon. The Pan African Medical Journal. 2019;33. doi: 10.11604/pamj.2019.33.152.16832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Obare F, Abuya T, Matanda D, Bellows B. Assessing the community-level impact of a decade of user fee policy shifts on health facility deliveries in Kenya, 2003–2014. International journal for equity in health. 2018;17(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Ravit M, Audibert M, Ridde V, De Loenzien M, Schantz C, Dumont A. Removing user fees to improve access to caesarean delivery: a quasi-experimental evaluation in western Africa. BMJ global health. 2018;3(1):e000558. doi: 10.1136/bmjgh-2017-000558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Garchitorena A, Miller AC, Cordier LF, Ramananjato R, Rabeza VR, Murray M, et al. In Madagascar, use of health care services increased when fees were removed: lessons for universal health coverage. Health affairs. 2017;36(8):1443–51. doi: 10.1377/hlthaff.2016.1419 [DOI] [PubMed] [Google Scholar]
- 123.Fournier P, Dumont A, Tourigny C, Philibert A, Coulibaly A, Traore M. The free caesareans policy in low-income settings: an interrupted time series analysis in Mali (2003–2012). PLoS One. 2014;9(8):e105130. doi: 10.1371/journal.pone.0105130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ajayi AI. Inequalities in access to birth by caesarean section in the context of user fee exemption for maternal health services in southwest and north central Nigeria. International health. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Witter S, Arhinful DK, Kusi A, Zakariah-Akoto S. The Experience of Ghana in Implementing a User Fee Exemption Policy to Provide Free Delivery Care. Reproductive Health Matters. 2007;15(30):61–71. doi: 10.1016/S0968-8080(07)30325-X [DOI] [PubMed] [Google Scholar]
- 126.Hatt LE, Makinen M, Madhavan S, Conlon CM. Effects of user fee exemptions on the provision and use of maternal health services: a review of literature. Journal of health, population, and nutrition. 2013;31(4 Suppl 2):S67. [PubMed] [Google Scholar]
- 127.Ganle JK, Parker M, Fitzpatrick R, Otupiri E. Inequities in accessibility to and utilisation of maternal health services in Ghana after user-fee exemption: a descriptive study. International journal for equity in health. 2014;13(1):1–19. doi: 10.1186/s12939-014-0089-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Brault MA, Ngure K, Haley CA, Kabaka S, Sergon K, Desta T, et al. The introduction of new policies and strategies to reduce inequities and improve child health in Kenya: a country case study on progress in child survival, 2000–2013. PLoS One. 2017;12(8):e0181777. doi: 10.1371/journal.pone.0181777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.El-Khoury M, Hatt L, Gandaho T. User fee exemptions and equity in access to caesarean sections: An analysis of patient survey data in Mali. International Journal for Equity in Health. 2012;11(1). doi: 10.1186/1475-9276-11-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Tripathi N, Saini SK, Prinja S. Impact of Janani Shishu Suraksha Karyakram on out-of-pocket expenditure among urban slum dwellers in northern India. Indian Pediatrics. 2014;51:475–7. doi: 10.1007/s13312-014-0430-z [DOI] [PubMed] [Google Scholar]
- 131.Abdou Illou MM, Haddad S, Agier I, Ridde V. The elimination of healthcare user fees for children under five substantially alleviates the burden on household expenses in Burkina Faso. BMC health services research. 2015;15:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Witter S, Brikci N, Harris T, Williams R, Keen S, Mujica A, et al. The free healthcare initiative in Sierra Leone: evaluating a health system reform, 2010‐2015. The International journal of health planning and management. 2018;33(2):434–48. doi: 10.1002/hpm.2484 [DOI] [PubMed] [Google Scholar]
- 133.Parmar D, Banerjee A. How do supply-and demand-side interventions influence equity in healthcare utilisation? Evidence from maternal healthcare in Senegal. Social Science & Medicine. 2019;241:112582. doi: 10.1016/j.socscimed.2019.112582 [DOI] [PubMed] [Google Scholar]
- 134.Ferry GA, Dickson SR, Mbaruku G, Freedman LP, Kruk ME. Equity of inpatient health care in rural Tanzania: A population- and facility-based survey. International Journal for Equity in Health. 2012;11(1). doi: 10.1186/1475-9276-11-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Philibert A, Ridde V, Bado A, Fournier P. No effect of user fee exemption on perceived quality of delivery care in Burkina Faso: a case-control study. BMC health services research. 2014;14(1):1–8. doi: 10.1186/1472-6963-14-120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Zombré D, De Allegri M, Ridde V. Immediate and sustained effects of user fee exemption on healthcare utilization among children under five in Burkina Faso: a controlled interrupted time-series analysis. Social Science & Medicine. 2017;179:27–35. doi: 10.1016/j.socscimed.2017.02.027 [DOI] [PubMed] [Google Scholar]
- 137.Chama-Chiliba CM, Koch SF. An assessment of the effect of user fee policy reform on facility-based deliveries in rural Zambia. BMC Research Notes. 2016;9(1):504. doi: 10.1186/s13104-016-2316-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Edu BC, Agan TU, Monjok E, Makowiecka K. Effect of free maternal health care program on health-seeking behavior of women during pregnancy, intra-partum and postpartum periods in Cross River State of Nigeria: A mixed method study. Macedonian Journal of Medical Sciences. 2017;5(3):370–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Lang’at E, Mwanri L, Temmerman M. Effects of implementing free maternity service policy in Kenya: an interrupted time series analysis. BMC health services research. 2019;19(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Wilkinson D, Gouws E, Sach M, Karim SSA. Effect of removing user fees on attendance for curative and preventive primary health care services in rural South Africa. Bulletin of the World Health organization. 2001;79(7):665–71. [PMC free article] [PubMed] [Google Scholar]
- 141.Leone T, Cetorelli V, Neal S, Matthews Z. Financial accessibility and user fee reforms for maternal healthcare in five sub-Saharan countries: a quasi-experimental analysis. BMJ open. 2016;6(1):e009692. doi: 10.1136/bmjopen-2015-009692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Ridde V, Haddad S, Heinmüller R. Improving equity by removing healthcare fees for children in Burkina Faso. J Epidemiol Community Health. 2013;67(9):751–7. doi: 10.1136/jech-2012-202080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Ridde V, Agier I, Jahn A, Mueller O, Tiendrebéogo J, Yé M, et al. The impact of user fee removal policies on household out-of-pocket spending: evidence against the inverse equity hypothesis from a population based study in Burkina Faso. The European Journal of Health Economics. 2015;16:55–64. doi: 10.1007/s10198-013-0553-5 [DOI] [PubMed] [Google Scholar]
- 144.Owiti A, Oyugi J, Essink D. Utilization of Kenya’s free maternal health services among women living in Kibera slums: a cross-sectional study. Pan African medical journal. 2018;30(1). doi: 10.11604/pamj.2018.30.86.15151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Ponsar F, Van Herp M, Zachariah R, Gerard S, Philips M, Jouquet G. Abolishing user fees for children and pregnant women trebled uptake of malaria-related interventions in Kangaba, Mali. Health policy and planning. 2011;26(suppl_2):ii72–ii83. doi: 10.1093/heapol/czr068 [DOI] [PubMed] [Google Scholar]
- 146.Ridde V, Diarra A. A process evaluation of user fees abolition for pregnant women and children under five years in two districts in Niger (West Africa). BMC Health Services Research. 2009;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Dzakpasu S, Soremekun S, Manu A, Ten Asbroek G, Tawiah C, Hurt L, et al. Impact of free delivery care on health facility delivery and insurance coverage in Ghana’s Brong Ahafo Region. PloS one. 2012;7(11):e49430. doi: 10.1371/journal.pone.0049430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Dalinjong PA, Wang AY, Homer CSE. Are health facilities well equipped to provide basic quality childbirth services under the free maternal health policy? Findings from rural Northern Ghana. BMC Health Services Research. 2018;18(1):959. doi: 10.1186/s12913-018-3787-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Ansah EK, Narh-Bana S, Asiamah S, Dzordzordzi V, Biantey K, Dickson K, et al. Effect of removing direct payment for health care on utilisation and health outcomes in Ghanaian children: a randomised controlled trial. PLoS medicine. 2009;6(1):e1000007. doi: 10.1371/journal.pmed.1000007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Nagpal S, Masaki E, Pambudi ES, Jacobs B. Financial protection and equity of access to health services with the free maternal and child health initiative in Lao PDR. Health Policy and Planning. 2019;34(Supplement_1):i14–i25. doi: 10.1093/heapol/czz077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Asante-Sarpong H, Owusu AY, Saravanan S, Appiah E, Abu M. Determinants of use of supervised delivery care under Ghana’s fee exemption policy for maternal healthcare: the case of the Central Region. BMC pregnancy and childbirth. 2016;16:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Ameur AB, Ridde V, Bado AR, Ingabire M-G, Queuille L. User fee exemptions and excessive household spending for normal delivery in Burkina Faso: the need for careful implementation. BMC health services research. 2012;12(1):1–10. doi: 10.1186/1472-6963-12-412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.De Allegri M, Ridde V, Louis VR, Sarker M, Tiendrebéogo J, Yé M, et al. Determinants of utilisation of maternal care services after the reduction of user fees: a case study from rural Burkina Faso. Health policy. 2011;99(3):210–8. doi: 10.1016/j.healthpol.2010.10.010 [DOI] [PubMed] [Google Scholar]
- 154.Ganle JK, Mahama MS, Maya E, Manu A, Torpey K, Adanu R. Understanding factors influencing home delivery in the context of user‐fee abolition in Northern Ghana: Evidence from 2014 DHS. The International journal of health planning and management. 2019;34(2):727–43. doi: 10.1002/hpm.2731 [DOI] [PubMed] [Google Scholar]
- 155.Watson SI, Wroe EB, Dunbar EL, Mukherjee J, Squire SB, Nazimera L, et al. The impact of user fees on health services utilization and infectious disease diagnoses in Neno District, Malawi: a longitudinal, quasi-experimental study. BMC health services research. 2016;16:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.McKinnon B, Harper S, Kaufman JS. Who benefits from removing user fees for facility-based delivery services? Evidence on socioeconomic differences from Ghana, Senegal and Sierra Leone. Social science & medicine. 2015;135:117–23. doi: 10.1016/j.socscimed.2015.05.003 [DOI] [PubMed] [Google Scholar]
- 157.Witter S, Boukhalfa C, Cresswell JA, Daou Z, Filippi V, Ganaba R, et al. Cost and impact of policies to remove and reduce fees for obstetric care in Benin, Burkina Faso, Mali and Morocco. International journal for equity in health. 2016;15(1):1–19. doi: 10.1186/s12939-016-0412-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Manthalu G, Yi D, Farrar S, Nkhoma D. The effect of user fee exemption on the utilization of maternal health care at mission health facilities in Malawi. Health policy and planning. 2016;31(9):1184–92. doi: 10.1093/heapol/czw050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Eze P, Ezenduka C, Obikeze E, Ogbuabor D, Arize I, Ezenwaka U, et al. Examining the distribution of benefits of a free Maternal and Child Health programme in Enugu State, Nigeria: a benefit incidence analysis. Tropical Medicine & International Health. 2020;25(12):1522–33. doi: 10.1111/tmi.13486 [DOI] [PubMed] [Google Scholar]
- 160.Nguyen HT, Zombre D, Ridde V, De Allegri M. The impact of reducing and eliminating user fees on facility-based delivery: a controlled interrupted time series in Burkina Faso. Health Policy & Planning. 2018;33(8):948–56. doi: 10.1093/heapol/czy077 [DOI] [PubMed] [Google Scholar]
- 161.Ruhago GM, Mujinja PG, Norheim OF. Equity implications of coverage and use of insecticide treated nets distributed for free or with co-payment in two districts in Tanzania: A cross-sectional comparative household survey. International journal for equity in health. 2011;10(1):1–8. doi: 10.1186/1475-9276-10-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Zombré DY, De Allegri M, Ridde V, Zinszer K. User fees removal and community-based management of undernutrition in Burkina Faso: what effects on children’s nutritional status? Public Health Nutrition. 2021;24(12):3768–79. doi: 10.1017/S1368980021000732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Penfold S, Harrison E, Bell J, Fitzmaurice A. Evaluation of the delivery fee exemption policy in Ghana: population estimates of changes in delivery service utilization in two regions. Ghana medical journal. 2007;41(3):100. [PMC free article] [PubMed] [Google Scholar]
- 164.Samadoulougou S, Negatou M, Ngawisiri C, Ridde V, Kirakoya-Samadoulougou F. Effect of the free healthcare policy on socioeconomic inequalities in care seeking for fever in children under five years in Burkina Faso: a population-based surveys analysis. International Journal for Equity in Health. 2022;21(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Sunny AK, Basnet O, Acharya A, Poudel P, Malqvist M, Kc A. Impact of free newborn care service package on out of pocket expenditure‐evidence from a multicentric study in Nepal. BMC Health Services Research. 2021;21:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Paudel P, Subedi KU, Karmacharya SB, Shrestha S, Shrestha AK, Subedi P, et al. Utilization and Effectiveness of Free Newborn Care Service Package in Inpatient Care of Sick Newborns–A Time For its Revision to Ensure Sustainability: Evidences From a Tertiary Level Public Hospital in Nepal. Journal of Nepal Paediatric Society. 2021;41(3):439–46. [Google Scholar]
- 167.Karra M, Maggio D, Guo M, Ngwira B, Canning D. The causal effect of a family planning intervention on women’s contraceptive use and birth spacing. Proceedings of the National Academy of Sciences. 2022;119(22):e2200279119. doi: 10.1073/pnas.2200279119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Lagarde M, Lepine A, Chansa C. The long-term effects of free care on birth outcomes: Evidence from a national policy reform in Zambia. SSM-Population Health. 2022;17:101051. doi: 10.1016/j.ssmph.2022.101051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Muchiri S. Impact of Free/Subsidized Secondary School Education on the Likelihood of Teenage Motherhood. Demography. 2021;58(4):1401–21. doi: 10.1215/00703370-9357498 [DOI] [PubMed] [Google Scholar]
- 170.Beaujoin C, Bila A, Bicaba F, Plouffe V, Bicaba A, Druetz T. Women’s decision-making power in a context of free reproductive healthcare and family planning in rural Burkina Faso. BMC Women’s Health. 2021;21:1–11. doi: 10.1186/s12905-020-01152-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Gunarathne SP, Wickramasinghe ND, Agampodi TC, Prasanna IR, Agampodi SB. How costly is the first prenatal clinic visit? Analysis of out-of-pocket expenditure in rural Sri Lanka-a country with free maternal health care. BMC Health Services Research. 2021;21(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Ochieng BM, Kaseje M, Kaseje DCO, Oria K, Magadi M. Perspectives of stakeholders of the free maternity services for mothers in western Kenya: lessons for universal health coverage. BMC Health Services Research. 2022;22(1):226. doi: 10.1186/s12913-022-07632-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Orangi S, Kairu A, Malla L, Ondera J, Mbuthia B, Ravishankar N, et al. Impact of free maternity policies in Kenya: an interrupted time-series analysis. BMJ Global Health. 2021;6(6):e003649. doi: 10.1136/bmjgh-2020-003649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Orangi S, Kairu A, Ondera J, Mbuthia B, Koduah A, Oyugi B, et al. Examining the implementation of the Linda Mama free maternity program in Kenya. The International Journal of Health Planning and Management. 2021;36(6):2277–96. doi: 10.1002/hpm.3298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Oyugi B, Kendall S, Peckham S. Effects of free maternal policies on quality and cost of care and outcomes: an integrative review. Primary health care research & development. 2021;22:e43. doi: 10.1017/S1463423621000529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Meda IB, Baguiya A, Ridde V, Ouédraogo HG, Dumont A, Kouanda S. Out-of-pocket payments in the context of a free maternal health care policy in Burkina Faso: a national cross-sectional survey. Health Economics Review. 2019;9:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Ridde V, Queuille L, Atchessi N, Samb O, Heinmüller R, Haddad S. The evaluation of an experiment in healthcare user fees exemption for vulnerable groups in Burkina Faso. Field Actions Science Reports The journal of field actions. 2013(Special Issue 8). [Google Scholar]
- 178.Ravit M, Audibert M, Ridde V, De Loenzien M, Schantz C, Dumont A. Do free caesarean section policies increase inequalities in Benin and Mali? International journal for equity in health. 2018;17:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Mehboob G, Shaikh BT. EXPERIENCE OF VOUCHERS FOR REPRODUCTIVE HEALTH SERVICES IN DEVELOPING COUNTRIES: MAKING A CASE FOR PAKISTAN THROUGH A SYSTEMATIC REVIEW. Journal of Ayub Medical College, Abbottabad: JAMC. 2015;27(3):695–701. [PubMed] [Google Scholar]
- 180.Bellows NM, Bellows BW, Warren C. Systematic Review: The use of vouchers for reproductive health services in developing countries: Systematic review. Tropical Medicine and International Health. 2011;16(1):84–96. doi: 10.1111/j.1365-3156.2010.02667.x [DOI] [PubMed] [Google Scholar]
- 181.Eva G, Quinn A, Ngo TD. Vouchers for family planning and sexual and reproductive health services: a review of voucher programs involving Marie Stopes International among 11 Asian and African countries. International Journal of Gynaecology & Obstetrics. 2015;130 Suppl 3:E15–20. [DOI] [PubMed] [Google Scholar]
- 182.Corby N. Using mobile finance to reimburse sexual and reproductive health vouchers in Madagascar. London: Marie Stopes International. 2011. [Google Scholar]
- 183.Meuwissen LE, Gorter AC, Knottnerus AJ. Impact of accessible sexual and reproductive health care on poor and underserved adolescents in Managua, Nicaragua: a quasi-experimental intervention study. Journal of Adolescent Health. 2006;38(1):56. e1-. e9. doi: 10.1016/j.jadohealth.2005.01.009 [DOI] [PubMed] [Google Scholar]
- 184.Mushi AK, Armstrong Schellenberg JRM, Mponda H, Lengeler C. Targeted subsidy for malaria control with treated nets using a discount voucher system in Tanzania. Health Policy and Planning. 2003;18(2):163–71. doi: 10.1093/heapol/czg021 [DOI] [PubMed] [Google Scholar]
- 185.Nguyen HT, Hatt L, Islam M, Sloan NL, Chowdhury J, Schmidt JO, et al. Encouraging maternal health service utilization: an evaluation of the Bangladesh voucher program. Social Science & Medicine. 2012;74(7):989–96. doi: 10.1016/j.socscimed.2011.11.030 [DOI] [PubMed] [Google Scholar]
- 186.Dennis ML, Abuya T, Campbell OMR, Benova L, Baschieri A, Quartagno M, et al. Evaluating the impact of a maternal health voucher programme on service use before and after the introduction of free maternity services in Kenya: a quasi-experimental study. BMJ Global Health. 2018;3(2):e000726. doi: 10.1136/bmjgh-2018-000726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Meuwissen LE, Gorter AC, Segura Z, Kester AD, Knottnerus JA. Uncovering and responding to needs for sexual and reproductive health care among poor urban female adolescents in Nicaragua. Tropical Medicine & International Health. 2006;11(12):1858–67. doi: 10.1111/j.1365-3156.2006.01741.x [DOI] [PubMed] [Google Scholar]
- 188.Marchant T, Schellenberg D, Nathan R, Armstrong-Schellenberg J, Mponda H, Jones C, et al. Assessment of a national voucher scheme to deliver insecticide-treated mosquito nets to pregnant women. CMAJ. 2010;182(2):152–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Brody CM, Bellows N, Campbell M, Potts M. The impact of vouchers on the use and quality of health care in developing countries: A systematic review. Global Public Health. 2013;8(4):363–88. doi: 10.1080/17441692.2012.759254 [DOI] [PubMed] [Google Scholar]
- 190.Agha S. Impact of a maternal health voucher scheme on institutional delivery among low income women in Pakistan. Reproductive Health. 2011;8(1). doi: 10.1186/1742-4755-8-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Ahmed S, Khan MM. Is demand-side financing equity enhancing? Lessons from a maternal health voucher scheme in Bangladesh. Social Science and Medicine. 2011;72(10):1704–10. doi: 10.1016/j.socscimed.2011.03.031 [DOI] [PubMed] [Google Scholar]
- 192.Eva G, Shah S, Quinn A, Ngo T. Are our voucher programmes working? Evaluating our methods and results in six countries. 2015. [Google Scholar]
- 193.Pilasant S, Kulpeng W, Werayingyong P, Tritasavit N, Yamabhai I, Teerawattananon Y, et al. Maternal and child health voucher scheme in Myanmar: a review of early stage implementation. BMC Health Services Research. 2016;16(1):600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Chandir S, Khan AJ, Hussain H, Usman HR, Khowaja S, Halsey NA, et al. Effect of food coupon incentives on timely completion of DTP immunization series in children from a low-income area in Karachi, Pakistan: A longitudinal intervention study. Vaccine. 2010;28(19):3473–8. doi: 10.1016/j.vaccine.2010.02.061 [DOI] [PubMed] [Google Scholar]
- 195.Bellows B, Mackay A, Dingle A, Tuyiragize R, Nnyombi W, Dasgupta A. Increasing Contraceptive Access for Hard-to-Reach Populations With Vouchers and Social Franchising in Uganda. Global health, science and practice. 2017;5(3):446–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Grainger C, Gorter A, Okal J, Bellows B. Lessons from sexual and reproductive health voucher program design and function: A comprehensive review. International Journal for Equity in Health. 2014;13(1). doi: 10.1186/1475-9276-13-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Njuki R, Abuya T, Kimani J, Kanya L, Korongo A, Mukanya C, et al. Does a voucher program improve reproductive health service delivery and access in Kenya? BMC health services research. 2015;15:206. doi: 10.1186/s12913-015-0860-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Mia MN, Mahmood SS, Iqbal M, Bhuiya A, Pallikadavath S, Stones W. The Bangladesh Maternal Health Voucher Scheme: impact on completeness of antenatal care provision. Journal of biosocial science. 2021:1–8. doi: 10.1017/S0021932020000784 [DOI] [PubMed] [Google Scholar]
- 199.Obare F, Warren C, Abuya T, Askew I, Bellows B. Assessing the population-level impact of vouchers on access to health facility delivery for women in Kenya. Social Science and Medicine. 2014;102:183–9. doi: 10.1016/j.socscimed.2013.12.007 [DOI] [PubMed] [Google Scholar]
- 200.Obare F, Warren C, Kanya L, Abuya T, Bellows B. Community-level effect of the reproductive health vouchers program on out-of-pocket spending on family planning and safe motherhood services in Kenya. BMC health services research. 2015;15:343. doi: 10.1186/s12913-015-1000-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Ali M, Azmat SK, Hamza HB, Rahman MM, Hameed W. Are family planning vouchers effective in increasing use, improving equity and reaching the underserved? An evaluation of a voucher program in Pakistan. BMC health services research. 2019;19(1):200. doi: 10.1186/s12913-019-4027-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Warren CE, Abuya T, Kanya L, Obare F, Njuki R, Temmerman M, et al. A cross sectional comparison of postnatal care quality in facilities participating in a maternal health voucher program versus non-voucher facilities in Kenya. BMC Pregnancy and Childbirth. 2015;15(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Meuwissen LE, Gorter AC, Kester AD, Knottnerus JA. Does a competitive voucher program for adolescents improve the quality of reproductive health care? A simulated patient study in Nicaragua. BMC Public Health. 2006;6:204. doi: 10.1186/1471-2458-6-204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Bajracharya A, Veasnakiry L, Rathavy T, Bellows B. Increasing Uptake of Long-Acting Reversible Contraceptives in Cambodia Through a Voucher Program: Evidence From a Difference-in-Differences Analysis. Global health, science and practice. 2016;4:S109–S21. doi: 10.9745/GHSP-D-16-00083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Van de Poel E, Flores G, Ir P, O’Donnell O, Van Doorslaer E. Can vouchers deliver? An evaluation of subsidies for maternal health care in Cambodia. Bulletin of the World Health Organization. 2014;92(5):331–9. doi: 10.2471/BLT.13.129122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Ensor T, Chhun C, Kimsun T, McPake B, Edoka I. Impact of health financing policies in Cambodia: A 20 year experience. Social Science and Medicine. 2017;177:118–26. doi: 10.1016/j.socscimed.2017.01.034 [DOI] [PubMed] [Google Scholar]
- 207.Okal J, Kanya L, Obare F, Njuki R, Abuya T, Bange T, et al. An assessment of opportunities and challenges for public sector involvement in the maternal health voucher program in Uganda. Health Research Policy and Systems. 2013;11(1). doi: 10.1186/1478-4505-11-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Bellows B, Bulaya C, Inambwae S, Lissner CL, Ali M, Bajracharya A. Family Planning Vouchers in Low and Middle Income Countries: A Systematic Review. Studies in family planning. 2016;47(4):357–70. doi: 10.1111/sifp.12006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Keya KT, Bellows B, Rob U, Warren C. Improving Access to Delivery Care and Reducing the Equity Gap Through Voucher Program in Bangladesh: Evidence From Difference-in-Differences Analysis. International quarterly of community health education. 2018;38(2):137–45. doi: 10.1177/0272684X17749568 [DOI] [PubMed] [Google Scholar]
- 210.Prata N, Graff M, Graves A, Potts M. Avoidable maternal deaths: Three ways to help now. Global Public Health. 2009;4(6):575–87. doi: 10.1080/17441690802184894 [DOI] [PubMed] [Google Scholar]
- 211.Meuwissen LE, Gorter AC, Knottnerus JA. Perceived quality of reproductive care for girls in a competitive voucher programme. A quasi-experimental intervention study, Managua, Nicaragua. International Journal for Quality in Health Care. 2006;18(1):35–42. doi: 10.1093/intqhc/mzi073 [DOI] [PubMed] [Google Scholar]
- 212.Boddam-Whetham L, Gul X, Al-Kobati E, Gorter AC. Vouchers in Fragile States: Reducing Barriers to Long-Acting Reversible Contraception in Yemen and Pakistan. Global health, science and practice. 2016;4:S94–S108. doi: 10.9745/GHSP-D-15-00308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Brody CD, Freccero J, Brindis CD, Bellows B. Redeeming qualities: Exploring factors that affect women’s use of reproductive health vouchers in Cambodia. BMC International Health and Human Rights. 2013;13(1). doi: 10.1186/1472-698X-13-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Obare F, Warren C, Njuki R, Abuya T, Sunday J, Askew I, et al. Community-level impact of the reproductive health vouchers programme on service utilization in Kenya. Health policy and planning. 2013;28(2):165–75. doi: 10.1093/heapol/czs033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Mahmood SS, Amos M, Hoque S, Mia MN, Chowdhury AH, Hanifi SMA, et al. Does healthcare voucher provision improve utilisation in the continuum of maternal care for poor pregnant women? Experience from Bangladesh. Global health action. 2019;12(1):1701324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Macedo de Oliveira A, Wolkon A, Krishnamurthy R, Erskine M, Crenshaw DP, Roberts J, et al. Ownership and usage of insecticide-treated bed nets after free distribution via a voucher system in two provinces of Mozambique. Malaria Journal. 2010;9:222. doi: 10.1186/1475-2875-9-222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Hoddinott J, Dorosh P, Filipski M, Rosenbach G, Tiburcio E. Food transfers, electronic food vouchers and child nutritional status among Rohingya children living in Bangladesh. PLoS ONE. 2020;15(4). doi: 10.1371/journal.pone.0230457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Rahman M, Rob U, Noor F, Bellows B. Out-of-pocket expenses for maternity care in rural Bangladesh: A public-private comparison. International Quarterly of Community Health Education. 2012;33(2):143–57. doi: 10.2190/IQ.33.2.d [DOI] [PubMed] [Google Scholar]
- 219.Kihara AB, Harries AD, Bissell K, Kizito W, Van Den Berg R, Mueke S, et al. Antenatal care and pregnancy outcomes in a safe motherhood health voucher system in rural Kenya, 2007–2013. Public Health in Action. 2015;5(1):23–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Kramer K, Mandike R, Nathan R, Mohamed A, Lynch M, Brown N, et al. Effectiveness and equity of the Tanzania National Voucher Scheme for mosquito nets over 10 years of implementation. Malaria Journal. 2017;16(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Watt C, Abuya T, Warren CE, Obare F, Kanya L, Bellows B. Can reproductive health voucher programs improve quality of postnatal care? A quasi-experimental evaluation of Kenya ’ s Safe Motherhood voucher scheme. PLoS ONE. 2015;10(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Atukunda EC, Mugyenyi GR, Obua C, Atuhumuza EB, Lukyamuzi EJ, Kaida A, et al. Provision of family planning vouchers and early initiation of postpartum contraceptive use among women living with HIV in southwestern Uganda: A randomized controlled trial. PLoS Medicine. 2019;16(6). doi: 10.1371/journal.pmed.1002832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Amendah DD, Mutua MK, Kyobutungi C, Buliva E, Bellows B. Reproductive health voucher program and facility based delivery in informal settlements in Nairobi: A longitudinal analysis. PLoS ONE. 2013;8(11). doi: 10.1371/journal.pone.0080582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Schmidt JO, Ensor T, Hossain A, Khan S. Vouchers as demand side financing instruments for health care: a review of the Bangladesh maternal voucher scheme. Health Policy. 2010;96(2):98–107. doi: 10.1016/j.healthpol.2010.01.008 [DOI] [PubMed] [Google Scholar]
- 225.Bellows BW, Conlon CM, Higgs ES, Townsend JW, Nahed MG, Cavanaugh K, et al. A taxonomy and results from a comprehensive review of 28 maternal health voucher programmes. Journal of Health, Population and Nutrition. 2013;31(4 SUPPL.2):S106–S28. [PubMed] [Google Scholar]
- 226.Rob U, Rahman M, Bellows B. Using vouchers to increase access to maternal healthcare in Bangladesh. International Quarterly of Community Health Education. 2009;30(4):293–309. doi: 10.2190/IQ.30.4.b [DOI] [PubMed] [Google Scholar]
- 227.Janisch CP, Albrecht M, Wolfschuetz A, Kundu F, Klein S. Vouchers for health: A demand side output-based aid approach to reproductive health services in Kenya. Global Public Health. 2010;5(6):578–94. doi: 10.1080/17441690903436573 [DOI] [PubMed] [Google Scholar]
- 228.Ali M, Azmat SK, Hamza HB, Rahman MM. Assessing effectiveness of multipurpose voucher scheme to enhance contraceptive choices, equity, and child immunization coverage: Results of an interventional study from Pakistan. Journal of Multidisciplinary Healthcare. 2020;13:1061–74. doi: 10.2147/JMDH.S245900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Ir P, Horemans D, Souk N, Damme Wv. Using targeted vouchers and health equity funds to improve access to skilled birth attendants for poor women: a case study in three rural health districts in Cambodia. BMC Pregnancy and Childbirth. 2010;10(1):(7 January 2010). doi: 10.1186/1471-2393-10-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Bellows B, Kyobutungi C, Mutua MK, Warren C, Ezeh A. Increase in facility-based deliveries associated with a maternal health voucher programme in informal settlements in Nairobi, Kenya. Health policy and planning. 2013;28(2):134–42. doi: 10.1093/heapol/czs030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Njuki R, Obare F, Warren C, Abuya T, Okal J, Mukuna W, et al. Community experiences and perceptions of reproductive health vouchers in Kenya. BMC Public Health. 2013;13:660. doi: 10.1186/1471-2458-13-660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Kanya L, Obare F, Warren C, Abuya T, Askew I, Bellows B. Safe motherhood voucher programme coverage of health facility deliveries among poor women in South-western Uganda. Health policy and planning. 2014;29:i4–i11. doi: 10.1093/heapol/czt079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.De Brouwere V, Richard F, Witter S. Access to maternal and perinatal health services: Successful and less successful examples of improving access to safe delivery and care of the newborn. Tropical Medicine and International Health. 2009;14:16–7. [DOI] [PubMed] [Google Scholar]
- 234.Chersich MF, Luchters S, Blaauw D, Scorgie F, Kern E, Van Den Heever A, et al. Safeguarding maternal and child health in South Africa by starting the child support grant before birth: Design lessons from pregnancy support programmes in 27 countries. South African Medical Journal. 2016;106(12):1192–210. doi: 10.7196/SAMJ.2016.v106.i12.12011 [DOI] [PubMed] [Google Scholar]
- 235.Bakyono R, Tapsoba LDG, Lépine A, Berthé A, Ilboudo PG, Diallo CO, et al. Contraceptive use by married women or concubines living in rural areas in Burkina Faso: a qualitative study of free voucher use. The Pan African medical journal. 2020;37:72-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Marchant T, Hanson K, Nathan R, Mponda H, Bruce J, Jones C, et al. Timing of delivery of malaria preventive interventions in pregnancy: results from the Tanzania national voucher programme. Journal of Epidemiology & Community Health. 2011;65(1):78–82. doi: 10.1136/jech.2008.085449 [DOI] [PubMed] [Google Scholar]
- 237.Njuki R, Okal J, Warren CE, Obare F, Abuya T, Kanya L, et al. Exploring the effectiveness of the output-based aid voucher program to increase uptake of gender-based violence recovery services in Kenya: A qualitative evaluation. BMC Public Health. 2012;12:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Massavon W, Wilunda C, Nannini M, Agaro C, Amandi S, Orech JB, et al. Community perceptions on demand-side incentives to promote institutional delivery in Oyam district, Uganda: a qualitative study. BMJ open. 2019;9(9):e026851. doi: 10.1136/bmjopen-2018-026851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Obare F, Okwero P, Villegas L, Mills S, Bellows B. Increased Coverage of Maternal Health Services among the Poor in Western Uganda in an Output-Based Aid Voucher Scheme. 2016. [Google Scholar]
- 240.Azmat SK, Mustafa G, Hameed W, Asghar J, Ahmed A, Shaikh BT. Social franchising and vouchers to promote long-term methods of family planning in rural Pakistan: a qualitative stocktaking with stakeholders. JPMA The Journal of the Pakistan Medical Association. 2013;63(4 Suppl 3):S46–53. [PubMed] [Google Scholar]
- 241.Azmat SK, Shaikh BT, Hameed W, Mustafa G, Hussain W, Asghar J, et al. Impact of social franchising on contraceptive use when complemented by vouchers: a quasi-experimental study in rural Pakistan. PLoS ONE [Electronic Resource]. 2013;8(9):e74260. doi: 10.1371/journal.pone.0074260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Malik MA, Rohm LR, van Baal P, van Doorslaer EvD. Improving maternal and child health in Pakistan: a programme evaluation using a difference in difference analysis. BMJ global health. 2021;6(12):e006453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Lee S, Adam A-j. Designing a logic model for mobile maternal health e-voucher programs in low-and middle-income countries: an interpretive review. International journal of environmental research and public health. 2022;19(1):295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Azmat SK, Temmerman M, Ali M. Accessibility and uptake of modern contraceptive methods in Pakistan-a critical view on what works? JPMA The Journal of the Pakistan Medical Association. 2021;71(11):S20–S32. [PubMed] [Google Scholar]
- 245.Nandi A, Charters TJ, Quamruzzaman A, Strumpf EC, Kaufman JS, Heymann J, et al. Health care services use, stillbirth, and neonatal and infant survival following implementation of the Maternal Health Voucher Scheme in Bangladesh: A difference-in-differences analysis of Bangladesh Demographic and Health Survey data, 2000 to 2016. PLoS Medicine. 2022;19(8):e1004022. doi: 10.1371/journal.pmed.1004022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Ali M, Farron M, Azmat SK, Hameed W. The logistics of voucher management: The underreported component in family planning voucher discussions. Journal of Multidisciplinary Healthcare. 2018;11:683–90. doi: 10.2147/JMDH.S155205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Robertson L, Mushati P, Eaton JW, Dumba L, Mavise G, Makoni J, et al. Effects of unconditional and conditional cash transfers on child health and development in Zimbabwe: a cluster-randomised trial. The Lancet. 2013;381(9874):1283–92. doi: 10.1016/S0140-6736(12)62168-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Crea TM, Reynolds AD, Sinha A, Eaton JW, Robertson LA, Mushati P, et al. Effects of cash transfers on Children’s health and social protection in Sub-Saharan Africa: differences in outcomes based on orphan status and household assets. BMC public health. 2015;15:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.de Walque D, Fernald L, Gertler P, Hidrobo M. Cash transfers and child and adolescent development. Child and Adolescent Health and Development 3rd edition. 2017. [PubMed] [Google Scholar]
- 250.Grépin KA, Habyarimana J, Jack W. Cash on delivery: results of a randomized experiment to promote maternal health care in Kenya. Journal of health economics. 2019;65:15–30. doi: 10.1016/j.jhealeco.2018.12.001 [DOI] [PubMed] [Google Scholar]
- 251.Barrington C, Peterman A, Akaligaung AJ, Palermo T, de Milliano M, Aborigo RA. ‘Poverty can break a home’: Exploring mechanisms linking cash plus programming and intimate partner violence in Ghana. Social Science & Medicine. 2022;292:114521. doi: 10.1016/j.socscimed.2021.114521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Ravit M, Lohmann J, Dumont A, Kabore C, Koulidiati JL, De Allegri M. How a supply‐side intervention can help to increase caesarean section rates in Burkina Faso facilities—Evidence from an interrupted time‐series analysis using routine health data. Tropical Medicine & International Health. 2023;28(2):136–43. doi: 10.1111/tmi.13840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Nuñez PA, Fernández-Slezak D, Farall A, Szretter ME, Salomón OD, Valeggia CR. Impact of universal health coverage on child growth and nutrition in Argentina. American journal of public health. 2016;106(4):720–6. doi: 10.2105/AJPH.2016.303056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Dennis ML, Benova L, Abuya T, Quartagno M, Bellows B, Campbell OMR. Initiation and continuity of maternal healthcare: examining the role of vouchers and user-fee removal on maternal health service use in Kenya. Health policy and planning. 2019;34(2):120–31. doi: 10.1093/heapol/czz004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Wang WJ, Temsah G, Mallick L. Health insurance coverage and its impact on maternal health care utilization in low- and middle-income countries. DHS Analytical Studies. 2014(No.45):xii + 66 pp. [Google Scholar]
- 256.Wang W, Temsah G, Mallick L. The impact of health insurance on maternal health care utilization: evidence from Ghana, Indonesia and Rwanda. Health policy and planning. 2017;32(3):366–75. doi: 10.1093/heapol/czw135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Witter S, Govender V, Ravindran TKS, Yates R. Minding the gaps: health financing, universal health coverage and gender. Health policy and planning. 2017;32(5):v4–v12. doi: 10.1093/heapol/czx063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Brals D, Nelissen H, van der List M, Faye C, Juma C, Elbers C, et al. Impact of the community healthcare plan and the free maternity services programme on maternal and child healthcare utilisation in rural Kenya: a dairy farmer population-based study. African Health Sciences. 2019;19(3):2600–14. doi: 10.4314/ahs.v19i3.36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Borghi J, Ensor T, Somanathan A, Lissner C, Mills A. Mobilising financial resources for maternal health. Lancet. 2006;368(9545):1457–65. doi: 10.1016/S0140-6736(06)69383-5 [DOI] [PubMed] [Google Scholar]
- 260.Vora KS, Koblinsky SA, Koblinsky MA. Predictors of maternal health services utilization by poor, rural women: a comparative study in Indian States of Gujarat and Tamil Nadu. Journal of Health, Population and Nutrition. 2015;33(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Prinja S, Bahuguna P, Gupta R, Sharma A, Rana SK, Kumar R. Coverage and financial risk protection for institutional delivery: how universal is provision of maternal health care in India? PloS one. 2015;10(9):e0137315. doi: 10.1371/journal.pone.0137315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Hunter BM, Harrison S, Portela A, Bick D. The effects of cash transfers and vouchers on the use and quality of maternity care services: a systematic review. PloS one. 2017;12(3):e0173068. doi: 10.1371/journal.pone.0173068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Johnson FA, Frempong-Ainguah F, Padmadas SS. Two decades of maternity care fee exemption policies in Ghana: have they benefited the poor? Health policy and planning. 2016;31(1):46–55. doi: 10.1093/heapol/czv017 [DOI] [PubMed] [Google Scholar]
- 264.Morgan L, Stanton ME, Higgs ES, Balster RL, Bellows BW, Brandes N, et al. Financial incentives and maternal health: Where do we go from here? Journal of Health, Population and Nutrition. 2013;31(4 SUPPL.2):S8–S22. [PubMed] [Google Scholar]
- 265.Das S, Sundaramoorthy L, Bhatnagar T. Out-of-pocket expenditure for delivery at home and public health facilities in the context of conditional cash transfer and free delivery care programs: An analytical cross-sectional study in South 24 Parganas district, West Bengal, India, 2017. Clinical Epidemiology and Global Health. 2020;8(4):1395–401. [Google Scholar]
- 266.Richard F, Witter S, de Brouwere V. Innovative approaches to reducing financial barriers to obstetric care in low-income countries. American journal of public health. 2010;100(10):1845–52. doi: 10.2105/AJPH.2009.179689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Gopalan SS, Mutasa R, Friedman J, Das A. Health sector demand-side financial incentives in low-and middle-income countries: a systematic review on demand-and supply-side effects. Social Science & Medicine. 2014;100:72–83. doi: 10.1016/j.socscimed.2013.10.030 [DOI] [PubMed] [Google Scholar]
- 268.Hunter BM, Murray SF. Demand-side financing for maternal and newborn health: what do we know about factors that affect implementation of cash transfers and voucher programmes? BMC pregnancy and childbirth. 2017;17:1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Jehan K, Sidney K, Smith H, de Costa A. Improving access to maternity services: An overview of cash transfer and voucher schemes in South Asia. Reproductive Health Matters. 2012;20(39):142–54. doi: 10.1016/S0968-8080(12)39609-2 [DOI] [PubMed] [Google Scholar]
- 270.Montagu D, Graff M. Equity and financing for sexual and reproductive health service delivery: current innovations. BMJ Sexual & Reproductive Health. 2009;35(3):145–9. doi: 10.1783/147118909788708165 [DOI] [PubMed] [Google Scholar]
- 271.Ahmed S, Hasan MZ, Ali N, Ahmed MW, Haq E, Shabnam S, et al. Effectiveness of health voucher scheme and micro-health insurance scheme to support the poor and extreme poor in selected urban areas of Bangladesh: An assessment using a mixed-method approach. Plos one. 2021;16(11):e0256067. doi: 10.1371/journal.pone.0256067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Kabia E, Mbau R, Muraya KW, Morgan R, Molyneux S, Barasa E. How do gender and disability influence the ability of the poor to benefit from pro-poor health financing policies in Kenya? An intersectional analysis. International journal for equity in health. 2018;17:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Burnham GM, Pariyo G, Galiwango E, Wabwire-Mangen F. Discontinuation of cost sharing in Uganda. Bulletin of the World Health Organization. 2004;82(3):187–95. [PMC free article] [PubMed] [Google Scholar]
- 274.Sidze EM, Pradhan J, Beekink E, Maina TM, Maina BW. Reproductive health financing in Kenya: An analysis of national commitments, donor assistance, and the resources tracking process. Reproductive Health Matters. 2013;21(42):139–50. doi: 10.1016/S0968-8080(13)42738-6 [DOI] [PubMed] [Google Scholar]
- 275.Meda IB, Dumont A, Kouanda S, Ridde V. Impact of fee subsidy policy on perinatal health in a low-resource setting: A quasi-experimental study. PLoS ONE [Electronic Resource]. 2018;13(11):e0206978. doi: 10.1371/journal.pone.0206978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Fan X, Xu Y, Stewart M, Zhou Z, Dang S, Wang D, et al. Effect of China’s maternal health policy on improving rural hospital delivery: Evidence from two cross-sectional surveys. Scientific reports. 2018;8(1):12326. doi: 10.1038/s41598-018-29830-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.De Allegri M, Ridde V, Louis VR, Sarker M, Tiendrebeogo J, Ye M, et al. The impact of targeted subsidies for facility-based delivery on access to care and equity—evidence from a population-based study in rural Burkina Faso. Journal of Public Health Policy. 2012;33(4):439–53. doi: 10.1057/jphp.2012.27 [DOI] [PubMed] [Google Scholar]
- 278.Mohanty SK, Mishra RS, Mishra S, Sen S. Understanding equity of institutional delivery in public health centre by level of care in India: an assessment using benefit incidence analysis. International Journal for Equity in Health. 2020;19(1). doi: 10.1186/s12939-020-01331-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Garg R, Goyal S, Gupta S. India moves towards menstrual hygiene: subsidized sanitary napkins for rural adolescent girls—issues and challenges. Maternal and child health journal. 2012;16:767–74. doi: 10.1007/s10995-011-0798-5 [DOI] [PubMed] [Google Scholar]
- 280.Langlois EV, Karp I, Serme JDD, Bicaba A. Effect of a policy to reduce user fees on the rate of skilled birth attendance across socioeconomic strata in Burkina Faso. Health Policy and Planning. 2016;31(4):462–71. doi: 10.1093/heapol/czv088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Ganaba R, Ilboudo PG, Cresswell JA, Yaogo M, Diallo CO, Richard F, et al. The obstetric care subsidy policy in Burkina Faso: what are the effects after five years of implementation? Findings of a complex evaluation. BMC Pregnancy and Childbirth. 2016;16:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Wieser S, Brunner B, Tzogiou C, Plessow R, Zimmermann MB, Farebrother J, et al. Reducing micronutrient deficiencies in Pakistani children: are subsidies on fortified complementary foods cost-effective? Public health nutrition. 2018;21(15):2893–906. doi: 10.1017/S1368980018001660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Somanathan A. the impact of price subsidies on child health care use evaluation of the indonesian healthcard: World Bank Publications; 2008. [Google Scholar]
- 284.Coronini-Cronberg S, Laohasiriwong W, Gericke CA. Health care utilisation under the 30-Baht Scheme among the urban poor in Mitrapap slum, Khon Kaen, Thailand: a cross-sectional study. International journal for equity in health. 2007;6(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Ridde V, Kouanda S, Bado A, Bado N, Haddad S. Reducing the medical cost of deliveries in Burkina Faso is good for everyone, including the poor. PloS one. 2012;7(3):e33082. doi: 10.1371/journal.pone.0033082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.De Allegri M, Tiendrebéogo J, Müller O, Yé M, Jahn A, Ridde V. Understanding home delivery in a context of user fee reduction: a cross-sectional mixed methods study in rural Burkina Faso. BMC pregnancy and childbirth. 2015;15(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Belaid L, Ridde V. An implementation evaluation of a policy aiming to improve financial access to maternal health care in Djibo district, Burkina Faso. BMC pregnancy and childbirth. 2012;12(1):1–12. doi: 10.1186/1471-2393-12-143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Ridde V, Richard F, Bicaba A, Queuille L, Conombo G. The national subsidy for deliveries and emergency obstetric care in Burkina Faso. Health policy and planning. 2011;26(suppl_2):ii30–ii40. doi: 10.1093/heapol/czr060 [DOI] [PubMed] [Google Scholar]
- 289.Ridde V, Kouanda S, Yameogo M, Kadio K, Bado A. Why do women pay more than they should? A mixed methods study of the implementation gap in a policy to subsidize the costs of deliveries in Burkina Faso. Evaluation and program planning. 2013;36(1):145–52. doi: 10.1016/j.evalprogplan.2012.09.005 [DOI] [PubMed] [Google Scholar]
- 290.Ferris DG, Chen J, Isaac A, Braithwaite E, Beideck E, Mikail N, et al. Reimbursement Incentives to Improve Adherence to Follow-Up of Cervical Cancer Cytology Screening Results in Peru. Journal of Lower Genital Tract Disease. 2019;23(2):116–23. doi: 10.1097/LGT.0000000000000459 [DOI] [PubMed] [Google Scholar]
- 291.Bhat R, Mavalankar DV, Singh PV, Singh N. Maternal healthcare financing: Gujarat’s Chiranjeevi Scheme and its beneficiaries. Journal of health, population, and nutrition. 2009;27(2):249. doi: 10.3329/jhpn.v27i2.3367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Hounton S, Byass P, Kouyate B. Assessing effectiveness of a community based health insurance in rural Burkina Faso. BMC health services research. 2012;12:363. doi: 10.1186/1472-6963-12-363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Smith KV, Sulzbach S. Community-based health insurance and access to maternal health services: Evidence from three West African countries. Social Science and Medicine. 2008;66(12):2460–73. doi: 10.1016/j.socscimed.2008.01.044 [DOI] [PubMed] [Google Scholar]
- 294.Schoeps A, Lietz H, Sié A, Savadogo G, Allegri Md, Müller O, et al. Health insurance and child mortality in rural Burkina Faso. Global Health Action. 2015;8:27327. doi: 10.3402/gha.v8.27327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Nshakira-Rukundo E, Mussa EC, Gerber N, Braun Jv. Impact of community-based health insurance on child health outcomes: evidence on stunting from rural Uganda. ZEF-Discussion Papers on Development Policy. 2019(No.269):39 pp. [DOI] [PubMed] [Google Scholar]
- 296.Karra M, Canning D, Hu J, Ali M, Lissner C. Community-Based Financing of Family Planning in Developing Countries: A Systematic Review. Studies in family planning. 2016;47(4):325–39. doi: 10.1111/sifp.12000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Divya P, Allegri Md Savadogo G, Sauerborn R Do community-based health insurance schemes fulfil the promise of equity? A study from Burkina Faso. Health Policy and Planning. 2014;29(1):76–84. doi: 10.1093/heapol/czs136 [DOI] [PubMed] [Google Scholar]
- 298.Kent Ranson M, Sinha T, Chatterjee M, Acharya A, Bhavsar A, Morris SS, et al. Making health insurance work for the poor: Learning from the Self-Employed Women’s Association’s (SEWA) community-based health insurance scheme in India. Social Science and Medicine. 2006;62(3):707–20. doi: 10.1016/j.socscimed.2005.06.037 [DOI] [PubMed] [Google Scholar]
- 299.Lu C, Mejia-Guevara I, Hill K, Farmer P, Subramanian SV, Binagwaho A. Community-Based Health Financing and Child Stunting in Rural Rwanda. American Journal of Public Health. 2016;106(1):49–55. doi: 10.2105/AJPH.2015.302913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Sinha T, Ranson MK, Chatterjee M, Acharya A, Mills AJ. Barriers to accessing benefits in a community-based insurance scheme: Lessons learnt from SEWA Insurance, Gujarat. Health Policy and Planning. 2006;21(2):132–42. doi: 10.1093/heapol/czj010 [DOI] [PubMed] [Google Scholar]
- 301.Oraro T, Ngube N, Atohmbom GY, Srivastava S, Wyss K. The influence of gender and household headship on voluntary health insurance: the case of North-West Cameroon. Health Policy and Planning. 2018;33(2):163–70. doi: 10.1093/heapol/czx152 [DOI] [PubMed] [Google Scholar]
- 302.Nshakira-Rukundo E, Mussa EC, Gerber N, von Braun J. Impact of voluntary community-based health insurance on child stunting: Evidence from rural Uganda. Social Science & Medicine. 2020;245:112738. doi: 10.1016/j.socscimed.2019.112738 [DOI] [PubMed] [Google Scholar]
- 303.Simieneh MM, Yitayal M, Gelagay AA. Effect of community-based health insurance on healthcare-seeking behavior for childhood illnesses among rural mothers in Aneded District, East Gojjam Zone, Amhara Region, Northwest Ethiopia. Risk Management and Healthcare Policy. 2021:1659–68. doi: 10.2147/RMHP.S298658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Koch R, Nkurunziza T, Rudolfson N, Nkurunziza J, Bakorimana L, Irasubiza H, et al. Does community-based health insurance protect women from financial catastrophe after cesarean section? A prospective study from a rural hospital in Rwanda. BMC Health Services Research. 2022;22(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Koulidiati JL, De Allegri M, Lohmann J, Hillebrecht M, Kiendrebeogo JA, Hamadou S, et al. Impact of Performance-Based Financing on effective coverage for curative child health services in Burkina Faso: Evidence from a quasi-experimental design. Tropical Medicine and International Health. 2021. doi: 10.1111/tmi.13596 [DOI] [PubMed] [Google Scholar]
- 306.Skiles MP, Curtis SL, Basinga P, Angeles G, Thirumurthy H. The effect of performance-based financing on illness, care-seeking and treatment among children: an impact evaluation in Rwanda. BMC health services research. 2015;15:375. doi: 10.1186/s12913-015-1033-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Sieleunou I, De Allegri M, Roland Enok Bonong P, Ouédraogo S, Ridde V. Does performance‐based financing curb stock‐outs of essential medicines? Results from a randomised controlled trial in Cameroon. Tropical Medicine & International Health. 2020;25(8):944–61. doi: 10.1111/tmi.13447 [DOI] [PubMed] [Google Scholar]
- 308.Korachais C, Nkurunziza S, Nimpagaritse M, Meessen B. Impact of the extension of a performance-based financing scheme to nutrition services in Burundi on malnutrition prevention and management among children below five: A cluster-randomized control trial. PLoS ONE [Electronic Resource]. 2020;15(9):e0239036. doi: 10.1371/journal.pone.0239036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Lannes L, Meessen B, Soucat A, Basinga P. Can performance-based financing help reaching the poor with maternal and child health services? The experience of rural Rwanda. International Journal of Health Planning and Management. 2016;31(3):309–48. doi: 10.1002/hpm.2297 [DOI] [PubMed] [Google Scholar]
- 310.Van de Poel E, Flores G, Ir P, O’Donnell O. Impact of Performance-Based Financing in a Low-Resource Setting: A Decade of Experience in Cambodia. Health Economics. 2016;25(6):688–705. doi: 10.1002/hec.3219 [DOI] [PubMed] [Google Scholar]
- 311.Mwase T, Lohmann J, Hamadou S, Brenner S, Somda SMA, Hien H, et al. Can Combining Performance-Based Financing With Equity Measures Result in Greater Equity in Utilization of Maternal Care Services? Evidence From Burkina Faso. International journal of health policy and management. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Nkangu M, Little J, Asahngwa C, Deonandan R, Pongou R, Adams O, et al. Examining the Implementation of the Performance-Based Financing Equity Strategy in Improving Access and Utilization of Maternal Health Services in Cameroon: A Qualitative Study. International Journal of Environmental Research and Public Health [Internet]. 2022; 19(21). doi: 10.3390/ijerph192114132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Brenner S, Favaretti C, Lohmann J, Chinkhumba J, Muula AS, De Allegri M. Implementation of a performance-based financing scheme in Malawi and resulting externalities on the quality of care of non-incentivized services. BMC pregnancy and childbirth. 2021;21(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Briaux J, Martin-Prevel Y, Carles S, Fortin S, Kameli Y, Adubra L, et al. Evaluation of an unconditional cash transfer program targeting children’s first-1,000–days linear growth in rural Togo: A cluster-randomized controlled trial. PLoS Medicine. 2020;17(11). doi: 10.1371/journal.pmed.1003388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Handa S, Peterman A, Seidenfeld D, Tembo G. Income Transfers and Maternal Health: Evidence from a National Randomized Social Cash Transfer Program in Zambia. Health Economics (United Kingdom). 2016;25(2):225–36. doi: 10.1002/hec.3136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Sibson VL, Grijalva-Eternod CS, Noura G, Lewis J, Kladstrup K, Haghparast-Bidgoli H, et al. Findings from a cluster randomised trial of unconditional cash transfers in Niger. Maternal & child nutrition. 2018;14(4):e12615–e. doi: 10.1111/mcn.12615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Tonguet-Papucci A, Houngbe F, Lompo P, Yameogo WME, Huneau J-F, Ait Aissa M, et al. Beneficiaries’ perceptions and reported use of unconditional cash transfers intended to prevent acute malnutrition in children in poor rural communities in Burkina Faso: qualitative results from the MAM’Out randomized controlled trial. BMC Public Health. 2017;17(1):527. doi: 10.1186/s12889-017-4453-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Houngbe F, Tonguet-Papucci A, Altare C, Ait-Aissa M, Huneau JF, Huybregts L, et al. Unconditional Cash Transfers Do Not Prevent Children’s Undernutrition in the Moderate Acute Malnutrition Out (MAM’Out) Cluster-Randomized Controlled Trial in Rural Burkina Faso. J Nutr. 2017;147(7):1410–7. doi: 10.3945/jn.117.247858 [DOI] [PubMed] [Google Scholar]
- 319.Grellety E, Babakazo P, Bangana A, Mwamba G, Lezama I, Zagre NM, et al. Effects of unconditional cash transfers on the outcome of treatment for severe acute malnutrition (SAM): a cluster-randomised trial in the Democratic Republic of the Congo. BMC Medicine. 2017;15(1):87. doi: 10.1186/s12916-017-0848-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Pega F, Pabayo R, Benny C, Lee E-Y, Lhachimi SK, Liu SY. Unconditional cash transfers for reducing poverty and vulnerabilities: effect on use of health services and health outcomes in low‐and middle‐income countries. Cochrane Database of Systematic Reviews. 2022(3). doi: 10.1002/14651858.CD011135.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Malama C, Chen Q, De Vogli R, Birbeck GL. User fees impact access to healthcare for female children in rural Zambia. Journal of Tropical Pediatrics. 2002;48(6):371–2. doi: 10.1093/tropej/48.6.371 [DOI] [PubMed] [Google Scholar]
- 322.Degregorio G, Manga S, Kiyang E, Manjuh F, Bradford L, Cholli P, et al. Implementing a fee-for-service cervical cancer screening and treatment program in Cameroon: Challenges and opportunities. Oncologist. 2017;22(7):850–9. doi: 10.1634/theoncologist.2016-0383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Johnson A, Goss A, Beckerman J, Castro A. Hidden costs: The direct and indirect impact of user fees on access to malaria treatment and primary care in Mali. Social Science and Medicine. 2012;75(10):1786–92. doi: 10.1016/j.socscimed.2012.07.015 [DOI] [PubMed] [Google Scholar]
- 324.Bratt JH, Weaver MA, Foreit J, De Vargas T, Janowitz B. The impact of price changes on demand for family planning and reproductive health services in Ecuador. Health Policy and Planning. 2002;17(3):281–7. doi: 10.1093/heapol/17.3.281 [DOI] [PubMed] [Google Scholar]
- 325.Pot H, de Kok BC, Finyiza G. When things fall apart: local responses to the reintroduction of user-fees for maternal health services in rural Malawi. Reproductive Health Matters. 2018;26(54):126–36. doi: 10.1080/09688080.2018.1535688 [DOI] [PubMed] [Google Scholar]
- 326.You J. Lending to Parents and Insuring Children: Is There a Role for Microcredit in Complementing Health Insurance in Rural China? Health Economics (United Kingdom). 2016;25(5):543–58. [DOI] [PubMed] [Google Scholar]
- 327.Chen Y, Jin GZ. Does health insurance coverage lead to better health and educational outcomes? Evidence from rural China. Journal of Health Economics. 2012;31(1):1–14. doi: 10.1016/j.jhealeco.2011.11.001 [DOI] [PubMed] [Google Scholar]
- 328.Perez-Cuevas R, Doubova SV, Flores-Hernandez S, Munoz-Hernandez O. Utilization of healthcare services among children members of Medical Insurance for a New Generation. Salud Publica de Mexico. 2012;54 Suppl 1:S28–41. doi: 10.1590/s0036-36342012000700005 [DOI] [PubMed] [Google Scholar]
- 329.Mozumdar A, Aruldas K, Jain A, Reichenbach L. Understanding the use of India’s National Health Insurance Scheme for family planning and reproductive health services in Uttar Pradesh. The International journal of health planning and management. 2018;33(4):823–35. doi: 10.1002/hpm.2531 [DOI] [PubMed] [Google Scholar]
- 330.Wagner N, Quimbo S, Shimkhada R, Peabody J. Does health insurance coverage or improved quality protect better against out-of-pocket payments? Experimental evidence from the Philippines. Social Science and Medicine. 2018;204:51–8. doi: 10.1016/j.socscimed.2018.03.024 [DOI] [PubMed] [Google Scholar]
- 331.Velasquez-De Charry LC, Carrasquilla G, Roca-Garavito S. [Equity in access to treatment for breast cancer in Colombia]. Salud Publica de Mexico. 2009;51 Suppl 2:s246–53. [DOI] [PubMed] [Google Scholar]
- 332.Ettenger A, Barnighausen T, Castro A. Health insurance for the poor decreases access to HIV testing in antenatal care: evidence of an unintended effect of health insurance reform in Colombia. Health Policy & Planning. 2014;29(3):352–8. doi: 10.1093/heapol/czt021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Ganguly S, Kinsey S, Bakhshi S. Childhood cancer in India. Cancer Epidemiology. 2021;71(Pt B):101679. doi: 10.1016/j.canep.2020.101679 [DOI] [PubMed] [Google Scholar]
- 334.Yip W, Berman P. Targeted health insurance in a low income country and its impact on access and equity in access: Egypt’s school health insurance. Health Economics. 2001;10(3):207–20. doi: 10.1002/hec.589 [DOI] [PubMed] [Google Scholar]
- 335.Zhou M, Zhao S, Zhao Z. Gender differences in health insurance coverage in China. International Journal for Equity in Health. 2021;20(1). doi: 10.1186/s12939-021-01383-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Palmer M, Mitra S, Mont D, Groce N. The impact of health insurance for children under age 6 in Vietnam: A regression discontinuity approach. Social Science and Medicine. 2015;145:217–26. doi: 10.1016/j.socscimed.2014.08.012 [DOI] [PubMed] [Google Scholar]
- 337.Long Q, Zhang T, Xu L, Tang S, Hemminki E. Utilisation of maternal health care in western rural China under a new rural health insurance system (New Co-operative Medical System). Tropical Medicine and International Health. 2010;15(10):1210–7. doi: 10.1111/j.1365-3156.2010.02602.x [DOI] [PubMed] [Google Scholar]
- 338.Sanogo NA, Fantaye AW, Yaya S. Beyond coverage: a qualitative study exploring the perceived impact of Gabon’s health insurance plan on access to and quality of prenatal care. BMC Health Services Research. 2020;20(1):483. doi: 10.1186/s12913-020-05310-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Blanchet NJ, Fink G, Osei-Akoto I. The effect of Ghana’s National Health Insurance Scheme on health care utilisation. Ghana medical journal. 2012;46(2):76–84. [PMC free article] [PubMed] [Google Scholar]
- 340.Quayyum Z, Nadjib M, Ensor T, Sucahya PK. Expenditure on obstetric care and the protective effect of insurance on the poor: lessons from two Indonesian districts. Health Policy & Planning. 2010;25(3):237–47. doi: 10.1093/heapol/czp060 [DOI] [PubMed] [Google Scholar]
- 341.Agbadi P, Okyere J, Lomotey A, Duah HO, Seidu AA, Ahinkorah BO. Socioeconomic and demographic correlates of nonenrolment onto the national health insurance scheme among children in Ghana: Insight from the 2017/18 Multiple Indicator Cluster Survey. Preventive Medicine Reports. 2021;22. doi: 10.1016/j.pmedr.2021.101385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Dixon J, Luginaah IN, Mkandawire P. Gendered inequalities within Ghana’s National Health Insurance Scheme: are poor women being penalized with a late renewal policy? Journal of health care for the poor and underserved. 2014;25(3):1005–20. doi: 10.1353/hpu.2014.0122 [DOI] [PubMed] [Google Scholar]
- 343.Zhu JM, Zhu Y, Liu R. Health insurance of rural/township schoolchildren in Pinggu, Beijing: Coverage rate, determinants, disparities, and sustainability. International Journal for Equity in Health. 2008;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Quimbo SA, Peabody JW, Shimkhada R, Florentino J, Solon O. Evidence of a causal link between health outcomes, insurance coverage, and a policy to expand access: Experimental data from children in the Philippines. Health Economics. 2011;20(5):620–30. doi: 10.1002/hec.1621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.van Hees SGM O’Fallon T, Hofker M Dekker M, Polack S, Banks LM, et al. Leaving no one behind? Social inclusion of health insurance in low- and middle-income countries: a systematic review. International Journal for Equity in Health. 2019;18(1):134. doi: 10.1186/s12939-019-1040-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Parmar D, Banerjee A. Impact of an employment guarantee scheme on utilisation of maternal healthcare services: Results from a natural experiment in India. Social Science and Medicine. 2019;222:285–93. doi: 10.1016/j.socscimed.2019.01.028 [DOI] [PubMed] [Google Scholar]
- 347.Sivakumar T, James JW, Basavarajappa C. Health insurance schemes for children and adolescents with psychiatric disability. Journal of Indian Association for Child and Adolescent Mental Health. 2017;13(1):1–9. [Google Scholar]
- 348.Mendhe HG, Rohit D, Daneshwar S, Makade KG. Universal Health Insurance coverage and utilization among women in urban slum of Rajnandgaon, Chhattisgarh. Journal of Family Medicine and Primary Care. 2021;10(3):1313–9. doi: 10.4103/jfmpc.jfmpc_2226_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Islam MT, Igarashi I, Kawabuchi K. The impact of gonoshasthaya kendra’s micro health insurance plan on antenatal care among poor women in rural bangladesh. BioScience Trends. 2012;6(4):165–75. doi: 10.5582/bst.2012.v6.4.165 [DOI] [PubMed] [Google Scholar]
- 350.Servan-Mori E, Wirtz V, Avila-Burgos L, Heredia-Pi I. Antenatal Care Among Poor Women in Mexico in the Context of Universal Health Coverage. Maternal and child health journal. 2015;19(10):2314–22. doi: 10.1007/s10995-015-1751-9 [DOI] [PubMed] [Google Scholar]
- 351.Comfort AB, Peterson LA, Hatt LE. Effect of health insurance on the use and provision of maternal health services and maternal and neonatal health outcomes: A systematic review. Journal of Health, Population and Nutrition. 2013;31(4 SUPPL.2):S81–S105. [PubMed] [Google Scholar]
- 352.Mohanty SK, Kastor A. Out-of-pocket expenditure and catastrophic health spending on maternal care in public and private health centres in India: a comparative study of pre and post national health mission period. Health Economics Review. 2017;7(1). doi: 10.1186/s13561-017-0167-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353.Akazili J, Welaga P, Bawah A, Achana FS, Oduro A, Awoonor-Williams JK, et al. Is Ghana’s pro-poor health insurance scheme really for the poor? Evidence from Northern Ghana. BMC health services research. 2014;14:637. doi: 10.1186/s12913-014-0637-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354.Bonfrer I, Breebaart L, De Poel EV. The effects of Ghana’s national health insurance scheme on maternal and infant health care utilization. PLoS ONE. 2016;11(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Jafree SR, Zakar R, Ahsan H, Mustafa M, Fischer F. Impact of microfinance health interventions on health-related outcomes among female informal workers in Pakistan: A retrospective quasi-experimental study. BMJ Open. 2021;11(1). doi: 10.1136/bmjopen-2020-043544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Pérez-Cuevas R, Chertorivski S, Cortés-Gallo G, Rodríguez-Ortega E, Caballero F, Muñoz-Hernández O. Lessons learned from the first evaluation of the Medical Insurance for a New Generation: Bridging research and policy. Salud Publica de Mexico. 2012;54(SUPPL.1):S90–S7. doi: 10.1590/s0036-36342012000700012 [DOI] [PubMed] [Google Scholar]
- 357.Ahinkorah BO. Ecological zone and health insurance coverage among adolescent girls in Ghana: analysis of the 2017 maternal health survey. Journal of Public Health (Germany). 2020. [Google Scholar]
- 358.Ibrahim A, Maya ET, Donkor E, Agyepong IA, Adanu RM. Perinatal mortality among infants born during health user-fees (Cash & Carry) and the national health insurance scheme (NHIS) eras in Ghana: a cross-sectional study. BMC Pregnancy & Childbirth. 2016;16(1):385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Nasution SK, Mahendradhata Y, Trisnantoro L. Can a National Health Insurance Policy Increase Equity in the Utilization of Skilled Birth Attendants in Indonesia? A Secondary Analysis of the 2012 to 2016 National Socio-Economic Survey of Indonesia. Asia-Pacific journal of public health. 2020;32(1):19–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Kuwawenaruwa A, Mtei G, Baraka J, Tani K. The effects of MCH insurance cards on improving equity in access and use of maternal and child health care services in Tanzania: a mixed methods analysis. Journal of health, population, and nutrition. 2016;35(1):37. doi: 10.1186/s41043-016-0075-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Williams GA, Parmar D, Dkhimi F, Asante F, Arhinful D, Mladovsky P. Equitable access to health insurance for socially excluded children? The case of the National Health Insurance Scheme (NHIS) in Ghana. Social Science and Medicine. 2017;186:10–9. doi: 10.1016/j.socscimed.2017.05.023 [DOI] [PubMed] [Google Scholar]
- 362.Wang Q, Liu H, Lu ZX, Luo Q, Liu JA. Role of the new rural cooperative medical system in alleviating catastrophic medical payments for hypertension, stroke and coronary heart disease in poor rural areas of China. BMC Public Health. 2014;14(1):1–10. doi: 10.1186/1471-2458-14-907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363.Kuwawenaruwa A, Ramsey K, Binyaruka P, Baraka J, Manzi F, Borghi J. Implementation and effectiveness of free health insurance for the poor pregnant women in Tanzania: A mixed methods evaluation. Social Science & Medicine. 2019;225:17–25. doi: 10.1016/j.socscimed.2019.02.005 [DOI] [PubMed] [Google Scholar]
- 364.Ramos Rosas E, Winkler V, Brenner S, De Allegri M. Identifying the determinants of health insurance coverage among Peruvian women of reproductive age: an assessment based on the national Peruvian demographic survey of 2017. International Journal for Equity in Health. 2020;19(1):195. doi: 10.1186/s12939-020-01310-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 365.Muñoz-Hernández O, Chertorivski-Woldenberg S, Cortés-Gallo G, Pérez-Cuevas R. The Medical Insurance for a New Generation: a viable answer for the health needs of Mexican children. salud pública de méxico. 2012;54:s3–s10. doi: 10.1590/s0036-36342012000700002 [DOI] [PubMed] [Google Scholar]
- 366.Peng X, Conley D. The implication of health insurance for child development and maternal nutrition: evidence from China. European Journal of Health Economics. 2016;17(5):521–34. doi: 10.1007/s10198-015-0696-7 [DOI] [PubMed] [Google Scholar]
- 367.Brooks MI, Thabrany H, Fox MP, Wirtz VJ, Feeley FG, Sabin LL. Health facility and skilled birth deliveries among poor women with Jamkesmas health insurance in Indonesia: a mixed-methods study. BMC health services research. 2017;17:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 368.Saavedra-Avendaño B, Darney BG, Reyes-Morales H, Serván-Mori E. Does public health insurance improve health care? The case of prenatal care for adolescents in Mexico. Salud Publica de Mexico. 2016;58(5):561–8. [DOI] [PubMed] [Google Scholar]
- 369.Lattof SR. Health insurance and care-seeking behaviours of female migrants in Accra, Ghana. Health policy and planning. 2018;33(4):505–15. doi: 10.1093/heapol/czy012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370.Chen G, Liu GG, Xu F. The impact of the urban resident basic medical insurance on health services utilisation in China. Pharmacoeconomics. 2014;32:277–92. doi: 10.1007/s40273-013-0097-7 [DOI] [PubMed] [Google Scholar]
- 371.Castro-Ríos A, Reyes-Morales H, Pelcastre-Villafuerte BE, Rendón-Macías ME, Fajardo-Gutiérrez A. Socioeconomic inequalities in survival of children with acute lymphoblastic leukemia insured by social security in Mexico: a study of the 2007–2009 cohorts. International Journal for Equity in Health. 2019;18:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 372.Fan H, Yan Q, Liu S, Cai J, Coyte PC. Childhood nutrition in rural China: what impact does public health insurance have? Value in Health. 2021;24(3):317–24. doi: 10.1016/j.jval.2020.06.017 [DOI] [PubMed] [Google Scholar]
- 373.Liabsuetrakul T, Oumudee N. Effect of health insurance on delivery care utilization and perceived delays and barriers among southern Thai women. BMC Public Health. 2011;11(1):1–9. doi: 10.1186/1471-2458-11-510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 374.Renaudin P, Prual A, Vangeenderhuysen C, Abdelkader MO, Vall MOM, El Joud DO. Ensuring financial access to emergency obstetric care: three years of experience with Obstetric Risk Insurance in Nouakchott, Mauritania. International Journal of Gynecology & Obstetrics. 2007;99(2):183–90. doi: 10.1016/j.ijgo.2007.07.006 [DOI] [PubMed] [Google Scholar]
- 375.Celhay P, Martinez S, Muñoz M, Perez M, Perez-Cuevas R. Long-term effects of public health insurance on the health of children in Mexico: a retrospective study. Lancet Glob Health. 2019; 7 (10): e1448–57. doi: 10.1016/S2214-109X(19)30326-2 [DOI] [PubMed] [Google Scholar]
- 376.Gardezi NuZ. Public health insurance and birth outcomes: evidence from Punjab, Pakistan. Health Policy and Planning. 2021;36(1):1–13. doi: 10.1093/heapol/czaa115 [DOI] [PubMed] [Google Scholar]
- 377.Gouda HN, Hodge A, Bermejo R III, Zeck W, Jimenez-Soto E. The impact of healthcare insurance on the utilisation of facility-based delivery for childbirth in the Philippines. PLoS One. 2016;11(12):e0167268. doi: 10.1371/journal.pone.0167268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378.Kesuma ZM, Chongsuvivatwong V. Comparison of satisfaction with maternal health-care services using different health insurance schemes in aceh province, Indonesia. Indian journal of public health. 2016;60(3):195. doi: 10.4103/0019-557X.189013 [DOI] [PubMed] [Google Scholar]
- 379.Boutayeb W, Lamlili M, Maamri A, Ben El Mostafa S, Boutayeb A. Actions on social determinants and interventions in primary health to improve mother and child health and health equity in Morocco. International journal for equity in health. 2016;15:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 380.Habib SS, Zaidi S. Exploring willingness to pay for health insurance and preferences for a benefits package from the perspective of women from low-income households of Karachi, Pakistan. BMC Health Services Research. 2021;21(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 381.Gu H-Q, Yang X, Rao Z-Z, Wang C-J, Zhao X-Q, Wang Y-L, et al. Disparities in outcomes associated with rural-urban insurance status in China among inpatient women with stroke: a registry-based cohort study. Annals of Translational Medicine. 2019;7(18). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382.Xie Y, Valdimarsdóttir UA, Wang C, Zhong X, Gou Q, Zheng H, et al. Public health insurance and cancer‐specific mortality risk among patients with breast cancer: a prospective cohort study in China. International Journal of Cancer. 2021;148(1):28–37. doi: 10.1002/ijc.33183 [DOI] [PubMed] [Google Scholar]
- 383.Barua P, Narattharaksa K. The impact of the stateless health insurance scheme on inpatient service utilization of stateless children at the four selected district hospitals in Tak Province, Thailand. The International Journal of Health Planning and Management. 2020;35(1):e12–e27. [DOI] [PubMed] [Google Scholar]
- 384.Aizawa T. The impact of health insurance on out-of-pocket expenditure on delivery in Indonesia. Health Care for Women International. 2019;40(12):1374–95. doi: 10.1080/07399332.2019.1578778 [DOI] [PubMed] [Google Scholar]
- 385.Houweling TA, Arroyave I, Burdorf A, Avendano M. Health insurance coverage, neonatal mortality and caesarean section deliveries: an analysis of vital registration data in Colombia. J Epidemiol Community Health. 2017;71(5):505–12. doi: 10.1136/jech-2016-207499 [DOI] [PubMed] [Google Scholar]
- 386.Anindya K, Lee JT, McPake B, Wilopo SA, Millett C, Carvalho N. Impact of Indonesia’s national health insurance scheme on inequality in access to maternal health services: A propensity score matched analysis. Journal of global health. 2020;10(1). doi: 10.7189/jogh.10.010429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 387.Kesuma ZM, Chongsuvivatwong V. Utilization of the Local Government Health Insurance Scheme (JKA) for maternal health services among women living in underdeveloped areas of Aceh Province, Indonesia. Asia Pacific Journal of Public Health. 2015;27(3):348–59. doi: 10.1177/1010539514524818 [DOI] [PubMed] [Google Scholar]
- 388.Rivillas JC, Devia-Rodriguez R, Ingabire M-G. Measuring socioeconomic and health financing inequality in maternal mortality in Colombia: a mixed methods approach. International Journal for Equity in Health. 2020;19:1–12. doi: 10.1186/s12939-020-01219-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 389.RamPrakash R, Lingam L. Why is women’s utilization of a publicly funded health insurance low?: a qualitative study in Tamil Nadu, India. BMC Public Health. 2021;21(1):1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 390.Serván-Mori E, Orozco-Núñez E, Heredia-Pi I, Armenta-Paulino N, Wirtz VJ, Meneses-Navarro S, et al. Public health insurance and ethnic disparities in maternal health care: the case of vulnerable Mexican women over the last 25 years. Health Policy and Planning. 2021;36(10):1671–80. doi: 10.1093/heapol/czab119 [DOI] [PubMed] [Google Scholar]
- 391.Solanke BL. Do the determinants of institutional delivery among childbearing women differ by health insurance enrolment? Findings from a population‐based study in Nigeria. The International Journal of Health Planning and Management. 2021;36(3):668–88. doi: 10.1002/hpm.3112 [DOI] [PubMed] [Google Scholar]
- 392.Tschirhart N, Jiraporncharoen W, Thongkhamcharoen R, Yoonut K, Ottersen T, Angkurawaranon C. Including undocumented migrants in universal health coverage: a maternal health case study from the Thailand-Myanmar border. BMC Health Services Research. 2021;21(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Imo CK, Wet-Billings D, Isiugo-Abanihe UC. The impact of maternal health insurance coverage and adequate healthcare services utilisation on the risk of under-five mortality in Nigeria: a cross-sectional study. Archives of Public Health. 2022;80(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 394.Indraswari BW, Kelling E, Vassileva SM, Sitaresmi MN, Danardono D, Mulatsih S, et al. Impact of universal health coverage on childhood cancer outcomes in Indonesia. Pediatric Blood & Cancer. 2021;68(9):e29186. doi: 10.1002/pbc.29186 [DOI] [PubMed] [Google Scholar]
- 395.Kofinti RE, Asmah EE, Ameyaw EK. Comparative study of the effect of National Health Insurance Scheme on use of delivery and antenatal care services between rural and urban women in Ghana. Health Economics Review. 2022;12(1):13. doi: 10.1186/s13561-022-00357-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396.Liyanto E, Nuryana D, Cahyani RA, Utomo B, Magnani R. How well are Indonesia’s urban poor being provided access to quality reproductive health services? Plos one. 2022;17(4):e0265843. doi: 10.1371/journal.pone.0265843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 397.Marthias T, McPake B, Carvalho N, Millett C, Anindya K, Saputri NS, et al. Associations between Indonesia’s national health insurance, effective coverage in maternal health and neonatal mortality: a multilevel interrupted time-series analysis 2000–2017. J Epidemiol Community Health. 2022;76(12):999–1010. doi: 10.1136/jech-2021-217213 [DOI] [PubMed] [Google Scholar]
- 398.Aziz N, Liu T, Yang S, Zukiewicz-Sobczak W. Causal relationship between health insurance and overall health status of children: Insights from Pakistan. Frontiers in Public Health. 2022;10. doi: 10.3389/fpubh.2022.934007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 399.Bolarinwa OA, Babalola TO, Adebayo OA, Ajayi KV. Health insurance coverage and modern contraceptive use among sexually active women in Nigeria: Further analysis of 2018 Nigeria Demographic Health Survey. Contraception and Reproductive Medicine. 2022;7(1):22. doi: 10.1186/s40834-022-00187-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 400.Chen H, Xing J, Yang X, Zhan K. Heterogeneous Effects of Health Insurance on Rural Children’s Health in China: A Causal Machine Learning Approach. International Journal of Environmental Research and Public Health. 2021;18(18):9616. doi: 10.3390/ijerph18189616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 401.Diao Y, Lin M, Xu K, Huang J, Wu X, Li M, et al. Impact of public health insurance coverage of novel anticancer medication on medical expenditure and patient affordability in a provincial medical centre of China: a propensity score-matching analysis with the quasi-experimental design. BMJ open. 2022;12(2):e054713. doi: 10.1136/bmjopen-2021-054713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 402.Ekholuenetale M, Barrow A. Inequalities in out-of-pocket health expenditure among women of reproductive age: after-effects of national health insurance scheme initiation in Ghana. Journal of the Egyptian Public Health Association. 2021;96:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 403.Philibert A, Ravit M, Ridde V, Dossa I, Bonnet E, Bedecarrats F, et al. Maternal and neonatal health impact of obstetrical risk insurance scheme in Mauritania: a quasi experimental before-and-after study. Health policy and planning. 2017;32(3):405–17. doi: 10.1093/heapol/czw142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 404.Kuwawenaruwa A, Mtei G, Baraka J, Tani K. Implementing demand side targeting mechanisms for maternal and child health-experiences from national health insurance fund program in Rungwe District, Tanzania. Globalization and health. 2016;12(1):1–12. doi: 10.1186/s12992-016-0180-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 405.Adams AM, Rabbani A, Ahmed S, Mahmood SS, Al-Sabir A, Rashid SF, et al. Bangladesh: Innovation for Universal Health Coverage 4: Explaining equity gains in child survival in Bangladesh: Scale, speed, and selectivity in health and development. Lancet. 2013;382:2027–37. [DOI] [PubMed] [Google Scholar]
- 406.Paredes KP. Inequality in the use of maternal and child health services in the Philippines: do pro-poor health policies result in more equitable use of services? International Journal for Equity in Health. 2016;15(1):181. doi: 10.1186/s12939-016-0473-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 407.Bustos M, Lau LL, Kirkpatrick SI, Dubin JA, Manguerra H, Dodd W. Examining the Association Between Household Enrollment in the Pantawid Pamilyang Pilipino Program (4Ps) and Wasting and Stunting Status Among Children Experiencing Poverty in the Philippines: A Cross-Sectional Study. Asia-Pacific journal of public health. 2023;35(6–7):420–8. doi: 10.1177/10105395231189570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 408.Palmer T, Batura N, Skordis J, Stirrup O, Vanhuyse F, Copas A, et al. Economic evaluation of a conditional cash transfer to retain women in the continuum of care during pregnancy, birth and the postnatal period in Kenya. PLOS Global Public Health. 2022;2(3):e0000128. doi: 10.1371/journal.pgph.0000128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 409.Alves FJO, Ramos D, Paixao ES, Falcao IR, de Cassia Ribeiro-Silva R, Fiaccone R, et al. Association of Conditional Cash Transfers With Maternal Mortality Using the 100 Million Brazilian Cohort. JAMA Network Open. 2023;6(2):e230070. doi: 10.1001/jamanetworkopen.2023.0070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 410.Cavalcanti DM, Ordoñez JA, Aransiola T, Almeida C, Perdomo Díaz JF, Zuluaga Mayorga D, et al. Evaluation and Forecasting Analysis of the Association of Conditional Cash Transfer with Child Mortality in Latin America, 2000–2030. JAMA Network Open. 2023;6(7):E2323489. doi: 10.1001/jamanetworkopen.2023.23489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 411.Patwardhan V. The impact of the Mamata conditional cash transfer program on child nutrition in Odisha, India. Health Economics (United Kingdom). 2023;32(9):2127–46. doi: 10.1002/hec.4720 [DOI] [PubMed] [Google Scholar]
- 412.Zhang X, Anser MK, Ahuru RR, Zhang Z, Peng MYP, Osabohien R, et al. Do Predictors of Health Facility Delivery Among Reproductive-Age Women Differ by Health Insurance Enrollment? A Multi-Level Analysis of Nigeria’s Data. Frontiers in public health. 2022;10:797272. doi: 10.3389/fpubh.2022.797272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 413.Tsala Dimbuene Z, Muanza Nzuzi R, Nzita Kikhela PD. Poverty, education and health insurance coverage among women of reproductive ages in the Democratic Republic of the Congo: a cross-sectional and multilevel analysis. BMJ Open. 2022;12(12):e064834. doi: 10.1136/bmjopen-2022-064834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 414.Ramos Rosas E, Winkler V, Huicho L, Blas MM, Brenner S, De Allegri M. Comprehensive Health Insurance and access to maternal healthcare services among Peruvian women: a cross-sectional study using the 2021 national demographic survey. BMC Pregnancy and Childbirth. 2023;23(1). doi: 10.1186/s12884-023-06086-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 415.Lee JT, McPake B, Putri LP, Anindya K, Puspandari DA, Marthias T. The effect of health insurance and socioeconomic status on women’s choice in birth attendant and place of delivery across regions in Indonesia: a multinomial logit analysis. BMJ Global Health. 2023;8(1):01. doi: 10.1136/bmjgh-2021-007758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 416.Nasir MH, Anser MK, Ahuru RR, Osabohien R, Ebiaku KC, Abbas S. A comparative study of the effect of health insurance on women’s use of health facility delivery: Evidence from demographic health survey in Benin Republic. African journal of reproductive health. 2022;26(6):104–15. doi: 10.29063/ajrh2022/v26i6.12 [DOI] [PubMed] [Google Scholar]
- 417.Langat S, Njuguna F, Olbara G, Martijn H, Sieben C, Haverkort M, et al. Influence of health-insurance on treatment outcome of childhood cancer in Western Kenya. Supportive Care in Cancer. 2023;31(8). doi: 10.1007/s00520-023-07913-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 418.Latif D, Ahmed H. Distance and health facility choice: Evidence from a health micro insurance program in Punjab, Pakistan. The International journal of health planning and management. 2022;37(6):3172–91. doi: 10.1002/hpm.3547 [DOI] [PubMed] [Google Scholar]
- 419.Chayo I, Uribe Perez CJ, De Vries E, Pinheiro PS. The impact of health insurance affiliation and socioeconomic status on cervical cancer survival in Bucaramanga, Colombia. Cancer Epidemiology. 2023;85:102375. doi: 10.1016/j.canep.2023.102375 [DOI] [PubMed] [Google Scholar]
- 420.de Groot R., et al., The impact of digital health insurance for low-income women in Kenya. 2023. [Google Scholar]
- 421.Garg S, Tripathi N, Bebarta KK. Does government health insurance protect households from out of pocket expenditure and distress financing for caesarean and non-caesarean institutional deliveries in India? Findings from the national family health survey (2019–21). BMC research notes. 2023;16(1):85. doi: 10.1186/s13104-023-06335-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 422.Ajayi AI, Ahinkorah BO, Seidu AA. "I don’t like to be seen by a male provider": health workers’ strike, economic, and sociocultural reasons for home birth in settings with free maternal healthcare in Nigeria. International Health. 2023;15(4):435–44. doi: 10.1093/inthealth/ihac064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 423.Browne L, Cooper S, Tiendrebeogo C, Bicaba F, Bila A, Bicaba A, et al. Using experience to create evidence: a mixed methods process evaluation of the new free family planning policy in Burkina Faso. Reproductive Health. 2022;19(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 424.Furechi O. Awareness and utilization of free maternal healthcare services among women in Mt. Elgon Sub-County, Kenya. 2023. [Google Scholar]
- 425.Gunarathna SP, Wickramasinghe ND, Agampodi TC, Prasanna IR, Agampodi SB. Out-of-Pocket Expenditure for Antenatal Care Amid Free Health Care Provision: Evidence From a Large Pregnancy Cohort in Rural Sri Lanka. Global health, science and practice. 2023;11(5). doi: 10.9745/GHSP-D-22-00410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 426.Ilboudo PG, Siri A. Effects of the free healthcare policy on maternal and child health in Burkina Faso: a nationwide evaluation using interrupted time-series analysis. Health Economics Review. 2023;13(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 427.Nzalie RNT, Palle JN, Nsagha DS. User fee exemption and malaria treatment-seeking for children under five in a Cameroonian health district: a cross-sectional study. Malaria Journal. 2023;22(1):124. doi: 10.1186/s12936-023-04509-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 428.Azmat SK, Ali M, Rahman MM. Assessing the sustainability of two independent voucher-based family planning programs in Pakistan: a 24-months post-intervention evaluation. Contraception and Reproductive Medicine. 2023;8(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 429.Sultana N, Hossain A, Das H, Pallikadavath S, Koeryaman M, Rahman M, et al. Is the maternal health voucher scheme associated with increasing routine immunization coverage? Experience from Bangladesh. Frontiers in Public Health. 2023;11:963162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 430.Aye TT, Nguyen HT, Brenner S, Robyn PJ, Tapsoba LDG, Lohmann J, et al. To What Extent Do Free Healthcare Policies and Performance-Based Financing Reduce Out-of-Pocket Expenditures for Outpatient services? Evidence From a Quasi-experimental Study in Burkina Faso. International journal of health policy and management. 2023;12:6767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 431.Richterman A, Millien C, Bair EF, Jerome G, Suffrin JCD, Behrman JR, et al. The effects of cash transfers on adult and child mortality in low- and middle-income countries. Nature. 2023;618(7965):575–82. doi: 10.1038/s41586-023-06116-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 432.Dasgupta RR, Mao W, Ogbuoji O. Addressing child health inequity through case management of under-five malaria in Nigeria: an extended cost-effectiveness analysis. Malaria Journal. 2022;21(1). doi: 10.1186/s12936-022-04113-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 433.Anselmi L, Ohrnberger J, Fichera E, Nhassengo P, Fernandes QF, Chicumbe S. The impact of performance-based financing within local health systems: Evidence from Mozambique. Health Economics (United Kingdom). 2023;32(7):1525–49. doi: 10.1002/hec.4677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 434.Handebo S, Demie TG, Woldeamanuel BT, Biratu TD, Gessese GT. Enrollment of reproductive age women in community-based health insurance: An evidence from 2019 Mini Ethiopian Demographic and Health Survey. Front Public Health. 2023;11:1067773. doi: 10.3389/fpubh.2023.1067773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 435.Mussa EC, Palermo T, Angeles G, Kibur M, Otchere F. Impact of community-based health insurance on health services utilisation among vulnerable households in Amhara region, Ethiopia. BMC Health Serv Res. 2023;23(1):55. doi: 10.1186/s12913-023-09024-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 436.Kutzin J. Health financing for universal coverage and health system performance: concepts and implications for policy. Bull World Health Organ. 2013;91(8):602–11. doi: 10.2471/BLT.12.113985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 437.Rostampour M, Nosratnejad S. A Systematic Review of Equity in Healthcare Financing in Low- and Middle-Income Countries. Value Health Reg Issues. 2020;21:133–40. doi: 10.1016/j.vhri.2019.10.001 [DOI] [PubMed] [Google Scholar]
- 438.Asante A, Price J, Hayen A, Jan S, Wiseman V. Equity in Health Care Financing in Low- and Middle-Income Countries: A Systematic Review of Evidence from Studies Using Benefit and Financing Incidence Analyses. PloS one. 2016;11(4):e0152866–e. doi: 10.1371/journal.pone.0152866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 439.Iyer AR. Authorship trends in The Lancet Global Health. The Lancet Global Health. 2018;6(2):e142. doi: 10.1016/S2214-109X(17)30497-7 [DOI] [PubMed] [Google Scholar]
- 440.Bou-Karroum L, El-Harakeh A, Kassamany I, Ismail H, El Arnaout N, Charide R, et al. Health care workers in conflict and post-conflict settings: Systematic mapping of the evidence. PLOS ONE. 2020;15(5):e0233757. doi: 10.1371/journal.pone.0233757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 441.Bowsher G, Papamichail A, El Achi N, Ekzayez A, Roberts B, Sullivan R, et al. A narrative review of health research capacity strengthening in low and middle-income countries: lessons for conflict-affected areas. Global Health. 2019;15(1):23. doi: 10.1186/s12992-019-0465-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 442.López-Calva LF. Where are we today in the fight against global poverty? Five messages for the future [Internet]. Expert Group Meeting on SDG 1; 2024. May 7. World Bank Group; [accessed 2024 May]. Available from: https://sdgs.un.org/sites/default/files/2024-05/2024%20May%207%20-%20EGM%20SDG1%20-%20LFLC%20-%20V3_0.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All data underpinning the results of the scoping review are found within the paper and in the Supporting Information files.