SUMMARY
Clostridioides difficile (C. difficile) is a Gram-positive, spore-forming anaerobic bacterium emerged as a leading cause of diarrhea globally. CDI’s (Clostridioides difficile infection) impact on healthcare systems is concerning due to high treatment cost and increased hospitalisation time. The incidence of CDI has been influenced by hypervirulent strains such as the 027 ribotype, responsible for significant outbreaks in North America and Europe. CDI’s epidemiology has evolved, showing increased community-acquired cases alongside traditional hospital-acquired infections. Mortality rates remain high, with recurrent infections further elevating the risk. Transmission of C. difficile primarily occurs via spores, which survive in healthcare settings and play a pivotal role in transmission. Not only health workers, but also the food chain could have a significant impact on the transmission of infection, although no confirmed foodborne cases have been documented. Pathogenicity of C. difficile involves spore germination and toxin production. Toxins A and B can cause cellular damage and inflammatory responses in the host, leading to colitis. Clinical picture can range from mild diarrhea to fulminant colitis with toxic megacolon, and bowel perforation.
Risk factors for CDI include antibiotic exposure, advanced age, hospitalization, and use of proton pump inhibitors. Patients who experience abdominal surgery or patients with inflammatory bowel disease (IBD) are particularly susceptible due to their compromised gut microbiota. Management of CDI has evolved, with fidaxomicin emerging as a superior treatment option over vancomycin for initial and recurrent infections due to its reduction of recurrence rate. Faecal microbiota transplantation (FMT) is effective for recurrent CDI, restoring gut eubiosis. Bezlotoxumab, a monoclonal antibody against C. difficile toxin B, has shown promise in reducing recurrence rates. Severe cases of CDI may require surgical intervention, particularly in instances of toxic megacolon or bowel perforation. In conclusion, CDI remains a significant clinical entity. Further research are needed to improve patients’ outcome and reduce the burden on healthcare systems.
Keywords: Clostridioides difficile, bezlotoxumab, fidaxomicin
INTRODUCTION
Clostridioides difficile is a Gram-positive, spore-forming anaerobic bacterium that has emerged as a leading cause of nosocomial diarrhoea, with a concerning increase in community-onset cases in recent years. According to the ECDC, the European incidence of CDI exceeds 120,000 cases per year, making it one of the major economic burdens on healthcare systems, due to the high treatment costs and prolonged hospital stay [1]. The European report by COMBACTE-CDI survey documented a median CDI incidence rate of 4.1 cases per 10.000 bed-days [2]. Interestingly, community acquired CDI (CA-CDI) have increased in the last decades, reflecting important changes in epidemiology and risk factors. However, recent Italian data reported a relevant missed CA-CDI diagnosis rate, probably resulting from younger patients with no previous antibiotic exposure or history of hospitalisation [3]. An Italian surveillance study showed a lower-than-expected incidence of CDI (0.96 cases/10000 patient daysbed), reflecting disease under-estimation [4].
Concurrently, recent 20 years have seen the spread of epidemic strains, such as the hypervirulent 027 ribotype, which was responsible for an outbreak in the US and UK [5].
Latest guidelines have highlighted some changes in the therapeutic approach of CDI [6, 7]. Clostridioides difficile illness can be considered a subject of primary interest in terms of epidemiological changes, burden of disease and therapeutic options, remaining both a central topic in scientific debate and a concern in clinical practice.
Given this background knowledge, our narrative review aims to give an overview of C. difficile epidemiological and pathogenetic features, together with current updates on therapeutical approach.
METHODS
We performed a narrative review on Clostridioides difficile using PubMed electronic databases. Keywords were: “Clostridioides difficile”, “CDI”, “colitis”, “epidemiology”, “strains”, “risk factors”, “pathogenesis”, “toxins”, “dysbiosis”, and “therapy” including “FMT”. The search string used was “(Clostridioides difficile) AND (colitis) OR (epidemiology) OR (risk factors) OR (pathogenesis) OR (toxins) OR (dysbiosis) OR (therapy) OR (FMT)”. According to this criterion, all original and review articles were considered. Further studies were collected by screening the reference lists of selected articles for any relevant sources not retrieved in the initial search. Finally, 96 articles were considered pertinent and were thus selected for inclusion.
EPIDEMIOLOGY AND BURDEN OF DISEASE
By the first years of 2000s, an increased incidence of CDI in Canada, US and Europe was noticed [8]. Since then, several studies attempted to investigate the mechanisms underlying these epidemiological changes. Innovative molecular biology techniques allowed us to amplify the 16S–23S intergenic spacer regions of C. difficile, in order to identify a new epidemic strain of C. difficile defined as BI/NAP/PCR ribotype 027, an hypervirulent strain responsible for several outbreaks in the US [9]. This strain is characterised by fluoroquinolones resistance and a higher MIC90 to metronidazole when compared with non-027 isolates [10]. Between 2004–2006 an outbreak of C. difficile 027/BI/NAP1 presented in the UK with a documented rising incidence from 25.9% to 41.3% [11]. Moreover, an Italian study reported a significant increase in RT027 incidence up to 64% between 2009 and 2012 [12]. Outbreaks of 027-like ribotypes have been described all over Europe. Between 2016 and 2019, RT181 was identified as the most frequent and virulent ribotype in Greece, found in approximately 70% of hospitals. Despite the similarities, RT181 appears to have a lower virulence than RT027. Furthermore, while RT027 is associated with cases of both CA-CDI and HACDI, RT181 has only been observed in nosocomial outbreaks [13, 14].
An Italian study conducted from 2015 to 2018 also showed that strains ST-378, ST-379 (belonging to clade 1) and ST-37, ST-11 (belonging to clades 4 and 5) were mostly isolated in patients with CDI, while ST-5 and ST-380 were isolated only in outpatients [15].
Recent data reported a marked high raise in CDI incidence in American hospitals, with an incidence in US up to 8.3 CDI cases per 10000 patient-days [16].
COVID-19 pandemic significantly impacted on CDI epidemiology, although the available data are quite heterogeneous. According to an US analysis conducted nationwide in 2020, 4920 cases of CDI were found among a total of 1,045,125 patients with COVID-19. Furthermore, CDI was independently associated with higher mortality-rates [17]. Other data from the National Healthcare Safety Network, later confirmed by Italian and Mexican studies, showed an overall reduction in hospital acquired-CDI (HA-CDI) in 2020 compared to 2019 [18–21. Improved infection prevention and control practices, increased emphasis on hand hygiene and the use of personal protective equipment might have had a positive impact on HAIs rates during the COVID-19 pandemic.
On the other hand, further studies conducted in America and Europe reported a rise of CDI cases, especially in the early months of the pandemic. This may be explained by the limited resources available at the beginning of the COVID-19 pandemic, when small ward spaces, small staff and lack of personal protective equipment could have limited infection prevention and control practices [22].
Mortality rates related to CDI are still high, ranging from 11% to 18%, with substantial risk of complications even after 12 months from hospital admission [23, 24]. The estimated death per year due to CDI amounts to 29,000 and 1,800 deaths in the USA and UK, respectively [25, 26]. This adds up to the large economic impact related to hospital management of CDI. A recent study conducted in Germany revealed that healthcare resource usage and associated costs were consistently higher in CDI patients compared to non-CDI patients [23]. The incremental cost per patient was € 4,101 in CDI patients, increasing to € 13,291 in case of ≥3 recurrences [23]. An American study published in 2022 revealed how CDI-associated deaths were almost 10 times higher for patients with recurrent CDI than primary CDI (25.4% versus 2.7%), with higher hospitalisation rates and higher healthcare costs [27].
Other changes in epidemiology concern the recent emergence of clusters of CA-CDI. CA-CDI is defined when the onset of symptoms is in the community setting, or within 48 hours after admission to a health-care facility [28, 29]. A population-based study exploring risk factors for CACDI revealed that community-acquired patients were more likely to be younger, females and with a lower comorbidity score than hospital-acquired patients [29]. Moreover, patients with CA-CDI were more likely to be antibiotic naïve, less likely to be on gastric acid suppressing therapy, and less likely to have cancer [29].
TRANSMISSION
C. difficile requires the spore formation for its survival. Spore is a metabolically inert bacterial form, which provides resistance to oxygen, UV, desiccation and heat.
Sporulation is ruled by master regulator Spo0A and the subsequent sigma factor cascade, which allows an asymmetric separation of the cell, bringing to the formation of the spore [9]. Once ingested, spores survive the acid gastric environment and reach the duodenum, where the interaction with bile acids allows germination into toxin-producing bacteria and colonisation of the large intestine [25]. Hospital-outbreaks are the most common sources of transmission via the oral-faecal route, even though the relationship between antibiotic exposure, spore exposure and symptom onset often remain unknown. Health-care workers play a pivotal role in C. difficile transmission, stressing how hand hygiene programmes need to be pursued to limit CDI outbreaks [30]. In parallel, it is also crucial to enforce infection control measures in case of hospital outbreaks. Besides hand hygiene with water and soap, isolation procedures for infected patients in single rooms or with cohort isolation, should be applied. Correct hygiene of high-touch surfaces, and all shared equipment prior to use with another patient, including toilets, wheelchairs and gurneys, should be guaranteed to prevent spore’s contamination and CDI intra-hospital diffusion [31].
Besides HA-CDI, several studies focussed on C. difficile diffusion through the food chain. Although there are no confirmed cases of any foodborne disease caused by C. difficile, its occurrence in livestock and foods suggests that contaminated food products with spores could be a vehicle to spread CDI [32–36]. Studies confirmed that detection of similar C. difficile strains and spores in food is present in meat retails, vegetables and seafood [32]. PCR ribotype analysis confirmed that RT 017, 027, 078, were concurrently identified in both CA-and HA-outbreaks but also in foods and live-stocks [33–36].
Interestingly, an analysis of C. difficile-ribotype distribution and a culture investigation among retail potatoes crops were performed in 2018, showing a C. difficile positivity rate above 10% in 9/12 countries. The most frequently identified ribotypes (014/020, 078/126, 010 and 023) were the same as those found in human, animal and environmental samples [37].
PATHOGENICITY
As aforementioned, sporulation and germination can be included amongst the pathogenic factors of C. difficile [38]. Besides from spores’ germination, different molecules are involved in the pathogenic pathways of CDI. The slpA gene encodes for a particular group of adhesines, which are surface layer proteins (SLPs) of C. difficile that differs from SLPs of several other bacteria. Interestingly, it was proven that chemical removal of SPLs results in a missing adherence of C. difficile to human Henrietta Lacks cells (HeLa) [39].
The group of SLPs also includes cell wall proteins (CWPs), a cluster of highly immunogenic proteins implicated in CDI pathogenesis. Amongst them, Cwp22 seems to be involved in toxin production, sporulation, bacteria motility and cell viability. Studies revealed that Cwp22 inactivation resulted in an increased cell permeability and autolysis, with an impaired cellular adherence in vitro and a decreased cytotoxicity [25, 40]. CD283 is another relevant C. difficile surface protein, whose over-expression increase biofilm formation on abiotic surface [25, 41].
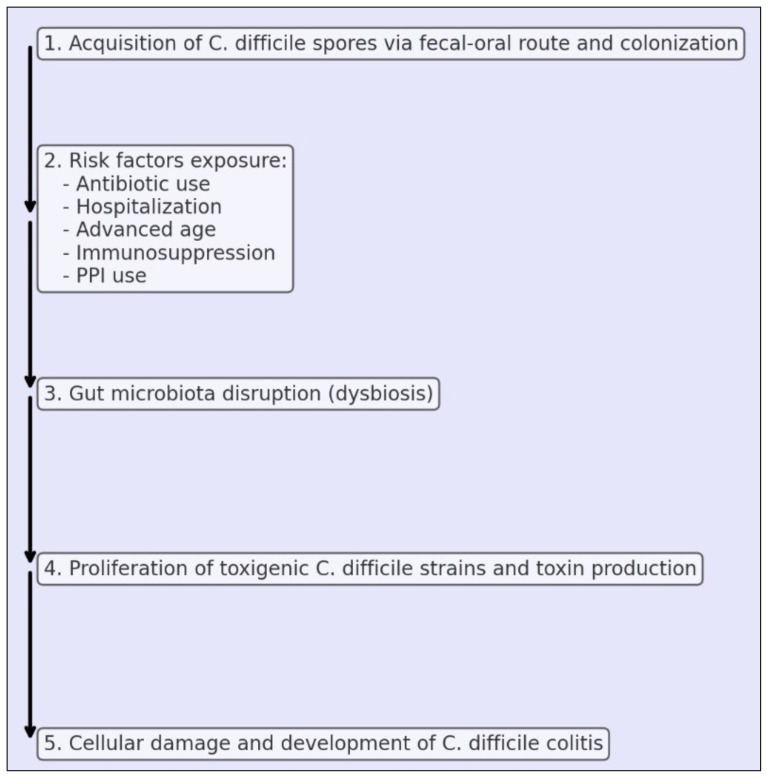
Toxin production is the major virulence factor in CDI pathogenesis. Toxin A and toxin B are encoded by a group of genes implicated in toxin expression and secretion (TcdR, TcdE, TcdL, TcdC). Toxin A/B mechanism concerns glycosylation of host GTP-ases, whose inactivation leads to changes in the actin cytoskeletal structure, cytokines secretion, cell cycle arrest and cell death [42]. All these factors can lead to CDI pathogenesis under favourable conditions. Patient’s risk factors can lead to a gut microbiota alteration, defined as dysbiosis, which favours the proliferation of toxigenic strains of C. difficile and sporulation and subsequent toxin production. Toxins trigger an inflammatory response with fluid secretion and tissue damage, then causing diarrhoea [43] (Figure 1).
Figure 1.
Pathogenesis of C. difficile colitis.
Moreover, C. difficile strains exhibit intrinsic resistance to different classes of antibiotics. RT001 ribotype is intrinsically resistant to fluoroquinolones, ceftriaxone, and erythromycin, while RT00 express resistance to fluoroquinolones and clindamycin. Notably, RT027 is known to be intrinsically resistant to fluoroquinolones [42].
Therefore, broad-spectrum antibiotics contribute to gut microbiota, promoting intestinal colonisation by C. difficile, reducing its clearance and finally increasing the risk of infection and recurrence [25]. Moreover, since conventional therapies with oral vancomycin and metronidazole contribute to alteration of the gut microbiota, the use of these drugs may increase the risk of reinfection. The introduction of fidaxomicin, a non-absorbable antibiotic that is less toxic to intestinal commensal bacteria, appears to play a role in reduction of CDI recurrence [44].
RISK FACTORS
CDI features multiple risk factors that contribute to its development. Antibiotic exposure is primarily linked to CDI, due to the disruption of gut microbiota, then creating a favourable environment for C. difficile proliferation and toxin production [45].
Cephalosporins are typically associated with CDI, especially third-and fourth-generation molecules [46]. Beta-lactams/beta-lactamase inhibitor combinations are also linked to an increased risk for CDI, due to a greater dysbiosis caused by beta-lactamase inhibitors [47]. Duration of antibiotic exposure has also a significant impact, as reported in a work by Brown et al. where 10- and 14-day courses of antibiotic therapy were significantly associated with increased risk of CDI when compared to 7-day courses (respectively 12% and 27%) [48]. Hospitalization represents another critical risk factor due to the increased likelihood of exposure to C. difficile in healthcare settings, paired with higher prevalence of susceptible populations in this environment [49]. Advanced age is strongly associated with CDI. Elderly patients often have weakened immune systems, co-morbidities, experience frequent hospitalizations with high antibiotics exposure, which all relate to an increased risk for CDI [50]. Furthermore, older age is typically linked to an increased risk of recurrent diseases [51], also due to changes in gut’s inter-species diversity, with less protection against pathogenic bacteria [52]. Moreover, when considering the gender distribution, women typically have an increased risk of CDI [53]. Abdominal surgery is a relevant risk factor for CDI. Recent data report a considerable CDI incidence after abdominal surgery, of which laparoscopic colorectal surgery appears to be the procedure with the highest risk of CDI occurrence [54].
Historically, proton pump inhibitors (PPIs) have been linked to a higher risk of CDI. PPIs reduce gastric acidity, potentially leading to an alteration of the gut microbiome and so creating an environment more conducive to C. difficile colonization and toxin production. A meta-analysis by Trifan et al. found that PPIs use was associated with a 65% increased risk of CDI [55]. More recently, Meta et al. highlighted the linkage between PPIs and recurrent CDI, showing that patients treated with PPIs were 64% more likely to develop recurrent CDI [56]. This association underscores the importance of cautious PPI use, particularly in patients with other risk factors, and suggests that healthcare providers should strongly evaluate the actual indication of PPI therapy in this category of patients for de-prescribing. Chronic kidney disease (CKD) has been also identified as a significant risk factor for CDI, as reported in a study by Thonprayoon et al. [57]. Patients with CKD often have a compromised immune system and frequently require antibiotic treatments, further disrupting their gut microbiota and enhancing the risk of CDI. Moreover, a systematic review focusing on CDI risk factors in American patients reported how CKD was a relevant risk factor for primary CDI and recurrent CDI [58]. This data emphasizes the need for vigilant infection control and appropriate antibiotic stewardship in this vulnerable population. Obese patients are predisposed to CDI as well due to less diversity of gut microbiota. Obesity is also associated with chronic inflammation and impaired immune responses, which can lead to increased susceptibility to infections. There are few data in literature showing how obesity is linked to a significantly increased risk of CDI compared to patients with normal body mass index [59]. On the contrary, a study by Malick et al. did not found association between obesity and death among patients with CDI [60]. Patients with chronic inflammatory bowel disease (IBD) present anatomic-functional alterations that promote the onset of CDI. In addition, biological drugs used for IBD treatment favours the occurrence of CDI [61]. Lastly, a relevant risk factor for CDI development are previous episodes of CDI, with recurrence rates progressively more frequent after subsequent infections, highlighting the difficulty to achieve a complete eradication of the infection [62]. Intervening on risk factors appears to be crucial in combating CDI. STOPP/START criteria (Screening Tool of Older Person’s Prescriptions/Screening Tool to Alert doctors to Right Treatment) collect a number of indications to identify relevant prescribing problems related to potentially inappropriate drugs and potential prescription omissions [63]. When applied to CDI, START criteria promote the use of probiotics in combination with antibiotics to prevent C. difficile diarrhoea, especially in non-immunocompromised or severely debilitated patients.
CLINICAL PICTURE
CDI occurs with a broad spectrum of clinical manifestations, ranging from mild diarrhoea to severe, life-threatening conditions. The severity of CDI is typically classified into mild, moderate, severe, and fulminant/severe-complicated colitis. Mild CDI is characterized by watery diarrhoea without relevant systemic symptom, while moderate CDI is often associated with moderate abdominal pain, fever and leucocytosis [64]. Patients with severe colitis exhibit more relevant symptoms such as profuse diarrhoea, severe abdominal pain, significant leucocytosis, hypoalbuminemia and increased serum creatinine levels [65]. The most severe form of colitis is fulminant CDI, with patients experiencing severe abdominal distension, ileus and profound systemic and life-threatening toxicity with signs of shock [66]. Fulminant CDI is often characterised by the onset of toxic megacolon and gut perforation. Prevalence of toxic megacolon ranges between 0.4% and 3% among cases of CDI, with higher rates occurring in patients older than 80 years. It is a serious complication which prompts rapid surgical evaluation, defined by the radiological finding of the diameter of the transverse colon >6 cm, with loss of haustration [67]. Recent guidelines by European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and Infectious Diseases Society of America (IDSA) have proposed a classification of CDI into non-severe, severe and severely complicated (i.e., fulminant) colitis [6, 7]. Although they differ slightly in some clinical and laboratory criteria, the cornerstones in the diagnosis of severe colitis are a white blood cell count >15000 cells/ml and an increased creatinine level (> 1.5 mg/dl for IDSA and >50% baseline according to ESCMID’s guidelines). Notably, ESCMID also includes additional radiological supporting factors such as imaging evidence of distention of the large intestine, pericolic fat stranding or colonic wall thickening. Fulminant or severe-complicated colitis is characterized in both cases by the presence of signs of haemodynamic impairment (hypotension, septic shock), ileus or radiological evidence of megacolon. Again, ESCMID also includes signs of severity such as increased serum lactates, intestinal perforation or any fulminant course of disease (i.e. rapid deterioration of the patient). Besides a clinical severity classification, a distinction is made between first episode and recurrent CDI. Recurrent CDI is defined as a return of diarrhoea and a positive stool test for C. difficile toxins or nucleic acid amplification test within two to eight weeks after completing treatment for the initial infection [45]. Approximately 15%–25% of patients with an initial CDI episode will develop a first recurrence, with a growing risk of recurrence up to 60% after the second recurrences as the number of CDI episodes increases [67]. Given the pivotal role of CDI recurrences in the clinical management of patients, early intervention with optimal therapy is crucial.
DIAGNOSIS
C. difficile diagnostics should be performed in patients with diarrhoea, defined as the occurrence of ≥ 3 unformed stool evacuations within 24 hours, while formed stool samples should not be tested for CDI [45]. There are various tests available, each with a different target for detecting the presence of C. difficile. Glutamate dehydrogenase (GDH) test is typically used as an initial screening test. GDH is an enzyme expressed by all strains of C. difficile, therefore it does not distinguish between the presence of toxigenic and non-toxigenic strains [68]. The sensitivity of the glutamate dehydrogenase test is 96%, with a high negative predictive value ranging from 98.4% to 100% [68]. Detection of C. difficile toxins A and B is a key diagnostic test for CDI diagnosis, given the toxins’ central role in the pathogenesis of the disease. Although cytotoxicity neutralization assay and toxigenic culture represent the reference diagnostic methods, they are no longer used in clinical practice due to their lack of resource efficiency [69]. Enzyme immunoassays (EIAs) for toxins A and B are currently the main toxins detection test due to their rapid turnaround and simplicity. A stool sample is collected from the patient, then incubated with specific antibodies that bind to toxin A and B. If toxins are present, a change in colour made by a specific substrate indicates a positive result, which is later measured using a spectrophotometer providing quantitative or qualitative results. The entire process is typically completed in a few hours, yielding results rapidly [69]. However, the sensitivity of toxin EIAs can range from 60% to 80%, mainly due to the lability of the toxin in the faecal sample, and potentially leading to false-negative results. Interestingly, a better sensitivity is described for the new ultrasensitive toxin assays, with overall higher accuracy than multistep algorithms, but they are not yet commercially available [70]. Moreover, repeating the toxin test after treatment is not recommended, as toxins can be detected on stools even 6 weeks after treatment and resolution of diarrhoea. Nucleic acid amplification tests (NAATs) consist of a variety of molecular tests which use polymerase chain reaction, loop-mediated isothermal amplification, helicase dependent amplification assay, and microarray technologies for detecting a variety of toxigenic C. difficile gene targets [68]. NAATs tests show high sensitivity (up to 95%) and high negative predictive value for diagnosis of C. difficile infection. On the other hand, these tests also detect asymptomatic carriers of toxigenic C. difficile strains, so the correct stool sample collection is crucial. To enhance CDI diagnostics, the recent European and American guidelines recommend a multi-step diagnostic algorithm. ESCMID guidelines propose a two-step algorithm consisting of a sensitive screening method (NAATs or GDH test) followed, in case of a positive result, by an EIA for toxin A/B [6]. An alternative is the concomitant screening of both GDH and toxin A/B EIA, considering samples with a GDH-positive test but negative toxin A/B test as samples with CDI or C. difficile carriage. In these cases, NAATs can be performed. IDSA guidelines propose the same approach, with the exception that NAATs alone can be considered diagnostic in setting of appropriate stool sample selection [7]. Further supporting this approach, a systematic review by Kraft et al. sustains the use of diagnostic algorithms that use NAAT alone or in combination with GDH or GDH plus toxin EIA [71].
The use of radiology and endoscopy plays a complementary role in the diagnosis of CDI, particularly in assessing complications and severe cases. Abdominal X-rays are often used first to assess the extent of colonic distention and to check for perforations. CT scans provide detailed images of the colon, revealing the extent of inflammation and complications such as abscesses, perforation or megacolon [72]. CT findings of CDI typically include colonic wall thickening, “accordion” or “target” signs, and pericolonic stranding. Endoscopy, particularly flexible sigmoidoscopy or colonoscopy is not routinely performed, due to the high risk of perforation and bleeding, especially in cases of fulminant CDI [72]. On the other hand, it could be a helpful tool when the suspicion is high and stool tests are negative, or when other diseases must be ruled out, especially in patient with persistent symptoms after an adequate treatment. Endoscopy reveals the typical colic manifestation of CDI, which is pseudomembranous colitis (PMC). PMC is characterized by the presence of pseudomembranes, which are 2 cm mucosal yellow/white lesions irregularly distributed in the colon. However, pseudomembranes are present in about 40–60% of CDI cases and could be found also in other bacterial infections and non-infectious diseases [73, 74].
THERAPY
Treatment strategies of CDI have evolved significantly. In the past, metronidazole has been the main therapy choice for a first mild CDI episode. Oral vancomycin gradually replaced metronidazole, due to multiple evidence supporting its superiority in the treatment of both severe and mild/moderate CDI [75,76]. Vancomycin is poorly absorbed from the gastrointestinal tract when administered orally, ensuring high colon concentrations while minimizing systemic absorption and thus reducing the risk of systemic side effects [45]. Both ESCMID and IDSA guidelines had recommended vancomycin as the first line in the treatment of mild and severe CDI [45]. However, recent guidelines suggested fidaxomicin over vancomycin for both the first episode and up to the second recurrence of CDI, with vancomycin being acceptable for a first episode only if other agents are unavailable [6, 7]. Fidaxomicin was introduced into clinical practice following its FDA approval in 2011. It is a macrocyclic antibiotic with high stool concentration and a narrow spectrum of activity, primarily targeting C. difficile, therefore probably causing less gut microbiome dysbiosis when compared to vancomycin [77]. Two randomized controlled trials showed the non-inferiority of fidaxomicin over vancomycin for clinical cure of mild and severe CDI, with a significantly lower recurrence rate [78,79]. Moreover, a subgroup analysis population from both studies highlighted how recurrence within 28 days occurred in 35.5% of patients from the vancomycin group and 19.7% in the fidaxomicin group [80]. Also, patients with CDI treated with fidaxomicin experienced less colonisation and overgrowth of VRE and Candida species [81].
For both vancomycin and fidaxomicin, the standard duration of therapy for mild/severe CDI is 10 days, at a dosage of 125 mg vancomycin every 6 hours and 200 mg fidaxomicin every 12 hours, respectively. Interestingly, the updated guidelines introduce the extended-pulsed fidaxomicin regimen consisting of 200 mg 12 hourly for 5 days followed by 200 mg every other day for 20 days. Evidence comes from the EXTEND trial, in which extended-pulsed fidaxomicin was superior to standard-dose vancomycin for sustained cure of CDI, reporting also the lowest recurrence rates observed in a randomized clinical trial of antibiotic treatment for CDI [82]. Considering different durations of therapy, an insight can be found in this recent observational study including patients with CDI treated with a short course of vancomycin (5–7 days) and fidaxomicin (5 days), compared to standard 10-days regimen. Interestingly, shortened treatment regimens were shown to be effective, with lower recurrence rate [83].
There is still no standardised therapeutic strategy in the treatment of fulminant severe-complicated CDI. While IDSA recommends higher-dose vancomycin (500 mg 6 hourly) in association with IV metronidazole, ESCMID consider the use of fidaxomicin and suggest the addition of IV tigecycline, avoiding IV metronidazole [6, 7]. Interestingly, evidence supporting the combination of high-dose vancomycin, and IV metronidazole are scarce.
Early data about the effectiveness of dual therapy came from an American study conducted in 2015 reporting a lower mortality in patients treated with vancomycin and IV metronidazole combination [84]. More recently, a retrospective study by Wang et al. showed no association between dual therapy and improved outcomes compared with vancomycin alone in patients with fulminant and non-fulminant CDI [85]. Interestingly, a recent Italian meta-analysis examining data from three retrospective studies revealed a mild, not statistically significant difference in mortality between the dual therapy group and the monotherapy group [86]. Considering the lack of solid evidence, RCT comparing the efficacy of the combination regimen versus vancomycin alone in patients with fulminant or severe-complicated CDI are currently needed. Interestingly, despite the ESCMID indication, there is no current data on the efficacy of fidaxomicin in severe life-threatening disease.
Faecal microbiota transplantation (FMT) has emerged in the past years as a pivotal therapeutic option for the treatment of recurrent CDI [87]. Were it not for organizational issues, FMT could possibly become a first line treatment due its efficacy and tolerability. FMT procedure consists of a stool infusion from a healthy donor into the gastrointestinal tract of the patient with CDI, in order to restore gut eubiosis and suppress the overgrowth of C. difficile. Studies have shown the FMT effectiveness for treating recurrent and refractory C. difficile infection while some evidence is emerging on the potential benefits of FMT for treating initial episodes of CDI [88–90]. A study by Popa et al. showed how in 25 patients with primary CDI (19 with a severe and 6 with a non-severe form) the FMT success rate was 94.7% [91]. Stronger evidence is provided by a Danish randomized trial comparing the efficacy of FMT with placebo after a 10-days course of oral vancomycin at standard dosing in patients with first or second CDI episode. Interestingly, FMT was highly effective and superior to the standard of care including vancomycin alone in achieving sustained resolution from C. difficile [92].
Notably, FMT could play a relevant role in treating fulminant disease. In 2021 a systematic review on FMT efficacy in refractory severe or fulminant CDI was performed [93]. 209 patients from 10 studies where analysed, revealing that FMT could be effective in treating fulminant CDI but requires multiple treatments and additional anti-CDI antibiotics to achieve resolution. However, considering the limits of the procedure, stronger evidence with randomized trials is needed to better assess the therapeutic role of FMT in these patients.
Other molecules besides antibiotics also have their place in the therapeutic management of CDI. Bezlotoxumab is a new drug approved by the FDA in 2016 and included in the latest guidelines for the treatment of CDI recurrences alongside standard antibiotic treatment [6, 7]. Bezlotoxumab is a monoclonal antibody specifically targeting C. difficile toxin B. MODIFY I and MODIFY II trials demonstrated that bezlotoxumab significantly reduced the rate of CDI recurrence within 12 weeks of treatment compared to placebo [94].
According to IDSA recommendations, patients with a primary CDI and risk factors for CDI recurrences could be treated with betlozoxumab in addition to standard-of-care therapy in settings where logistics are not an issue while bezlotoxumab is only considered in the management of patients with CDI starting from the second recurrence onwards according to the ESCMID indications. Interestingly, given the data from post-hoc analyses of the MODIFY studies, bezlotoxumab was effective in reducing the rate of relapse even in patients with primary CDI infection [6, 7, 95]. Therefore, considering the limitations of high costs and the need for intravenous therapy, further studies would be necessary to promote bezlotoxumab as a possible therapeutic choice in patients at high risk of relapse.
Going beyond medical therapy, patients with severe-complicated or fulminant forms of CDI may require surgical treatment. Undoubtedly, an urgent surgical assessment could be necessary for patients with signs of megacolon, colonic perforation, acute abdomen, septic shock or organ failure. When comparing IDSA and ESCMID guidelines, IDSA suggest surgical treatment for patient with fulminant CDI with high WBC count, while ESCMID consider surgical evaluation for clinically deteriorating patients not responding to CDI therapy [6, 7]. Timing for surgical evaluation is crucial. Data from a Canadian study reported a survival benefit in patients treated with emergency colectomy with lactate levels ≥5 mmol/L and WBC lower than 20 × 109/L, suggesting the importance of early surgical evaluation in at-risk patients prior to severe clinical deterioration [96].
CONCLUSIONS
C. difficile infection remains a major clinical entity of growing scientific importance. The incremental risk of recurrence characteristic of this pathogen is the cornerstone on which treatment choices must be strengthened to improve patient outcomes and reduce healthcare costs. Furthermore, intervening and addressing the risk factors for CDI in both hospital and out-of-hospital settings may be the key to reducing the spread of the disease and the exposure of patients at high risk of CDI recurrence. Overall, the management of CDI has evolved significantly, with advances in both pharmacological treatments and innovative therapies. Further studies will be needed to investigate the therapeutic landscape to best optimise the management of CDI.
REFERENCES
- 1.European Centre for Disease Prevention and Control. European Surveillance of Clostridioides (Clostridium) Difficile Infections. Surveillance Protocol Version 2.4. ECDC; 2019. Dec, [DOI] [Google Scholar]
- 2.Viprey VF, Granata G, Vendrik KEW, et al. COMBACTE-CDI Consortium. European Survey on the Current Surveillance Practices, Management Guidelines, Treatment Pathways and Heterogeneity of Testing of Clostridioides difficile, 2018–2019: Results from The Combatting Bacterial Resistance in Europe CDI (COMBACTE-CDI) J Hosp Infect. 2023;131:213–220. doi: 10.1016/j.jhin.2022.11.011. [DOI] [PubMed] [Google Scholar]
- 3.Granata G, Cataldo MA, D’arezzo S, et al. Clostridium difficile infection underdiagnosis in Italy: do we know the true magnitude of the problem? A prospective cohort study. Int J Infect Dis. 2018;73:35–40. [Google Scholar]
- 4.Bertolino L, Patauner F, Gagliardi M, et al. Diagnostic and infection control strategies for Clostridioides difficile infections in a setting of high antimicrobial resistance prevalence. Infez Med. 2021;29(1):70–78. [PubMed] [Google Scholar]
- 5.He M, Miyajima F, Roberts P, Ellison L, et al. Emergence and global spread of epidemic Healthcare-Associated Clostridium difficile. Nat Genet. 2013;45(1):109–113. doi: 10.1038/Ng.2478. doi: 10.1038/Ng.2478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Van Prehn J, Reigadas E, Vogelzang EH, et al. Guideline Committee of the European Study Group on Clostridioides difficile. European Society of Clinical Microbiology and Infectious Diseases: 2021 update on the treatment guidance document for Clostridioides difficile infection in adults. Clin Microbiol Infect. 2021;27(Suppl 2):S1–S21. doi: 10.1016/j.cmi.2021.09.038. [DOI] [PubMed] [Google Scholar]
- 7.Johnson S, Lavergne V, Skinner AM, et al. Clinical Practice Guideline by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA): 2021 focused update guidelines on management of Clostridioides difficile infection in adults. Clin Infect Dis. 2021;73(5):e1029–e1044. doi: 10.1093/cid/ciab549. [DOI] [PubMed] [Google Scholar]
- 8.Pépin J, Valiquette L, Alary ME, et al. Clostridium difficile-Associated Diarrhea in a Region of Quebec from 1991 to 2003: A Changing Pattern of Disease Severity. CMAJ. 2004;171(5):466–472. doi: 10.1503/cmaj.1041104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McDonald LC, Killgore GE, Thompson A, et al. An epidemic, toxin gene-variant strain of Clostridium difficile. N Engl J Med. 2005;353(23):2433–2441. doi: 10.1056/NEJMoa051590. [DOI] [PubMed] [Google Scholar]
- 10.Jones AM, Kuijper EJ, Wilcox MH. Clostridium difficile: A European Perspective. J Infect. 2013;66(2):115–128. doi: 10.1016/j.jinf.2012.10.019. [DOI] [PubMed] [Google Scholar]
- 11.Brazier JS, Raybould R, Patel B, et al. HPA Regional microbiology network. distribution and antimicrobial susceptibility patterns of Clostridium difficile PCR ribotypes in English hospitals, 2007–08. Euro Surveill. 2008;13(41):19000. doi: 10.2807/ese.13.41.19000-en. [DOI] [PubMed] [Google Scholar]
- 12.Aschbacher R, Indra A, Wiedermann CJ, et al. Predominance of Clostridium difficile 027 during a five-year period in Bolzano, Northern Italy. Infez Med. 2017;25(1):13–20. [PubMed] [Google Scholar]
- 13.Kachrimanidou M, Metallidis S, Tsachouridou O, et al. Predominance of Clostridioides difficile PCR Ribotype 181 in Northern Greece, 2016–2019. Anaerobe. 2022;76:102601. doi: 10.1016/j.anaerobe.2022.102601. [DOI] [PubMed] [Google Scholar]
- 14.Kachrimanidou M, Baktash A, Metallidis S, et al. An Outbreak of Clostridioides difficile Infections Due to a 027-like PCR Ribotype 181 in a rehabilitation centre: epidemiological and microbiological characteristics. Anaerobe. 2020;65:102252. doi: 10.1016/j.anaerobe.2020.102252. [DOI] [PubMed] [Google Scholar]
- 15.Mancini A, La Vigna G, Puciarelli S, et al. A Threeyear study entailing molecular characterization and epidemiology of Clostridium difficile in an Italian Tertiary Care Hospital. Infez Med. 2018;26(3):204–209. [PubMed] [Google Scholar]
- 16.Marra AR, Perencevich EN, Nelson RE, et al. Incidence and outcomes associated with Clostridium difficile infections: a systematic review and meta-analysis. JAMA Netw Open. 2020;3(1):e1917597. doi: 10.1001/jamanetworkopen.2019.17597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Deda X, Elfert K, Gandhi M, et al. Clostridioides difficile infection in COVID-19 hospitalized patients: a nationwide analysis. Gastroenterol Res. 2023;16(4):234–239. doi: 10.14740/gr1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weiner-Lastinger LM, Pattabiraman V, Konnor RY, et al. The impact of Coronavirus Disease 2019 (COVID-19) on healthcare-associated infections in 2020: a summary of data reported to the national healthcare safety network. Infect Control Hosp Epidemiol. 2022;43(1):12–25. doi: 10.1017/ice.2021.362. [DOI] [PubMed] [Google Scholar]
- 19.Baker MA, Sands KE, Huang SS, et al. CDC Prevention Epicenters program. the impact of Coronavirus Disease 2019 (COVID-19) on Healthcare-Associated Infections. Clin Infect Dis. 2022;74(10):1748–1754. doi: 10.1093/cid/ciab688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ochoa-Hein E, Rajme-López S, Rodríguez-Aldama JC, et al. Substantial reduction of healthcare facility-onset Clostridioides difficile Infection (HO-CDI) rates after conversion of a hospital for exclusive treatment of COVID-19 patients. Am J Infect Control. 2021;49(7):966–968. doi: 10.1016/j.ajic.2020.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bentivegna E, Alessio G, Spuntarelli V, et al. Impact of COVID-19 prevention measures on risk of health care-associated Clostridium difficile infection. Am J Infect Control. 2021;49(5):640–642. doi: 10.1016/j.ajic.2020.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spigaglia P. Clostridioides difficile Infection (CDI) during the COVID-19 Pandemic. Anaerobe. 2022;74:102518. doi: 10.1016/j.anaerobe.2022.102518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Antunes A, Tricotel A, Wilk A, et al. Estimating excess mortality and economic burden of Clostridioides difficile infections and recurrences during 2015–2019: The RECUR Germany Study. BMC Infect Dis. 2024;24(1):548. doi: 10.1186/s12879-024-09422-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Enoch DA, Murray-Thomas T, Adomakoh N, et al. Risk of complications and mortality following recurrent and non-recurrent Clostridioides difficile infection: a retrospective observational database study in England. J Hosp Infect. 2020;106(4):793–803. doi: 10.1016/j.jhin.2020.09.025. [DOI] [PubMed] [Google Scholar]
- 25.Buddle JE, Fagan RP. Pathogenicity and virulence of Clostridioides difficile. Virulence. 2023;14(1):2150452. doi: 10.1080/21505594.2022.2150452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lessa FC, Mu Y, Bamberg WM, et al. Burden of Clostridium difficile infection in the United States. N Engl J Med. 2015;372(9):825–834. doi: 10.1056/NEJMoa1408913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Feuerstadt P, Nelson WW, Drozd EM, et al. Mortality, health care use, and costs of Clostridioides difficile infections in older adults. J Am Med Dir Assoc. 2022;23(10):1721–1728. doi: 10.1016/j.jamda.2022.01.075. [DOI] [PubMed] [Google Scholar]
- 28.McDonald LC, Coignard B, Dubberke E, et al. Ad Hoc Clostridium difficile Surveillance Working Group. Recommendations for Surveillance of Clostridium difficile-Associated Disease. Infect Control Hosp Epidemiol. 2007;28(2):140–145. doi: 10.1086/511798. [DOI] [PubMed] [Google Scholar]
- 29.Khanna S, Pardi DS, Aronson SL, et al. The Epidemiology of community-acquired Clostridium difficile infection: a population-based study. Am J Gastroenterol. 2012;107(1):89–95. doi: 10.1038/ajg.2011.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Martin JS, Monaghan TM, Wilcox MH. Clostridium difficile infection: epidemiology, diagnosis and understanding transmission. Nat Rev Gastroenterol Hepatol. 2016;13(4):206–216. doi: 10.1038/nrgastro.2016.25. [DOI] [PubMed] [Google Scholar]
- 31.Candel-Pérez C, Ros-Berruezo G, Martínez-Graciá C. A Review of Clostridioides [Clostridium] difficile occurrence through the food chain. Food Microbiol. 2019;77:118–129. doi: 10.1016/j.fm.2018.08.012. [DOI] [PubMed] [Google Scholar]
- 32.Goorhuis A, Debast SB, van Leengoed LA, et al. Clostridium difficile PCR Ribotype 078: an emerging strain in humans and in pigs? J Clin Microbiol. 2008;46(3):1157. doi: 10.1128/JCM.01536-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Janezic S, Zidaric V, Pardon B, et al. International Clostridium difficile animal strain collection and large diversity of animal associated strains. BMC Microbiol. 2014;14:173. doi: 10.1186/1471-2180-14-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Keel K, Brazier JS, Post KW, et al. Prevalence of PCR Ribotypes among Clostridium difficile isolates from pigs, calves, and other species. J Clin Microbiol. 2007;45(6):1963–1964. doi: 10.1128/JCM.00224-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weese JS, Avery BP, Rousseau J, et al. Detection and Enumeration of Clostridium difficile spores in retail beef and pork. Appl Environ Microbiol. 2009;75(15):5009–5011. doi: 10.1128/AEM.00480-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tkalec V, Viprey V, Davis G, et al. COMBACTE-CDI Consortium. Clostridioides difficile positivity rate and pcr ribotype distribution on retail potatoes in 12 European Countries, January to June 2018. Euro Surveill. 2022;27(15):2100417. doi: 10.2807/1560-7917.ES.2022.27.15.2100417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Czepiel J, Dróżdż M, Pituch H, et al. Clostridium difficile infection: review. Eur J Clin Microbiol Infect Dis. 2019;38(7):1211–1222. doi: 10.1007/s10096-019-03539-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Calabi E, Calabi F, Phillips AD, et al. Binding of Clostridium difficile surface layer proteins to gastrointestinal tissues. Infect Immun. 2002;70(10):5770–5778. doi: 10.1128/IAI.70.10.5770-5778.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhu D, Bullock J, He Y, et al. Cwp22, a Novel peptidoglycan cross-linking enzyme, plays pleiotropic roles in Clostridioides difficile. Environ Microbiol. 2019;21(8):3076–3090. doi: 10.1111/1462-2920.14706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Arato V, Gasperini G, Giusti F, et al. Dual role of the colonization factor CD2831 in Clostridium difficile pathogenesis. Sci Rep. 2019;9(1):5554. doi: 10.1038/s41598-019-42000-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Di Bella S, Sanson G, Monticelli J, et al. Clostridioides difficile infection: history, epidemiology, risk factors, prevention, clinical manifestations, treatment, and future options. Clin Microbiol Rev. 2024;37(2):e0013523. doi: 10.1128/cmr.00135-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Abt MC, McKenney PT, Pamer EG. Clostridium difficile colitis: pathogenesis and host defence. Nat Rev Microbiol. 2016;14(10):609–620. doi: 10.1038/nrmicro.2016.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McDonald LC, Gerding DN, Johnson S, et al. Clinical Practice Guidelines for Clostridium difficile Infection in Adults and Children: 2017 Update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA) Clin Infect Dis. 2018;66(7):E1–E48. doi: 10.1093/cid/cix1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ebrahim-Saraie HS, Heidari H, Amanati A, et al. A multicenter-based study on epidemiology, antibiotic susceptibility and risk factors of toxigenic Clostridium difficile in hospitalized patients in Southwestern Iran. Infez Med. 2018;26(4):308–315. [PubMed] [Google Scholar]
- 45.Pultz NJ, Donskey CJ. Effect of antibiotic treatment on growth of and toxin production by Clostridium difficile in the cecal contents of mice. Antimicrob Agents Chemother. 2005;49(8):3529–3532. doi: 10.1128/AAC.49.8.3529-3532.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brown KA, Langford B, Schwartz KL, et al. Antibiotic prescribing choices and their comparative C. difficile infection risks: a longitudinal case-cohort study. Clin Infect Dis. 2021;72(5):836–844. doi: 10.1093/cid/ciaa124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Banaei N, Anikst V, Schroeder LF. Burden of Clostridium difficile infection in the United States. N Engl J Med. 2015;372(24):2368–2369. doi: 10.1056/NEJMc1505190. [DOI] [PubMed] [Google Scholar]
- 48.Guh AY, Mu Y, Winston LG, et al. Trends in U.S. Burden of Clostridioides difficile infection and outcomes. N Engl J Med. 2020;382(14):1320–1330. doi: 10.1056/NEJMoa1910215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Di Bella S, Capone A, Musso M, et al. Clostridium difficile infection in the elderly. Infez Med. 2013;21(2):93–102. [PubMed] [Google Scholar]
- 50.Arboleya S, Watkins C, Stanton C, Ross RP. Gut Bifidobacteria populations in human health and aging. Front Microbiol. 2016;7:1204. doi: 10.3389/Fmicb.2016.01204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Feuerstadt P, Theriault N, Tillotson G. The Burden of CDI in the United States: A Multifactorial Challenge. BMC Infect Dis. 2023;23:132. doi: 10.1186/S12879-023-08096-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fazl Alizadeh R, Li S, Sullivan B, et al. Surgical outcome in laparoscopic abdominal surgical operations with Clostridium difficile infection. Am Surg. 2022;88(10):2519–2524. doi: 10.1177/00031348221103644. [DOI] [PubMed] [Google Scholar]
- 53.Tariq R, Singh S, Gupta A, et al. Association of gastric acid suppression with recurrent Clostridium difficile infection: a systematic review and meta-analysis. JAMA Intern Med. 2017;177(6):784–791. doi: 10.1001/Jamainternmed.2017.0212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mehta P, Nahass RG, Brunetti L. Acid suppression medications during hospitalization as a risk factor for recurrence of Clostridioides difficile infection: systematic review and meta-analysis. Clin Infect Dis. 2021;73(1):e62–e68. doi: 10.1093/cid/ciaa545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Phatharacharukul P, Thongprayoon C, Cheungpasitporn W, et al. The risks of incident and recurrent Clostridium difficile-associated diarrhea in chronic kidney disease and end-stage kidney disease patients: a systematic review and meta-analysis. Dig Dis Sci. 2015;60(10):2913–2922. doi: 10.1007/S10620-015-3714-9. [DOI] [PubMed] [Google Scholar]
- 56.Eeuwijk J, Ferreira G, Yarzabal JP, Robert-Du Ry van Beest Holle M. A systematic literature review on risk factors for and timing of Clostridioides difficile infection in the United States. Infect Dis Ther. 2024;13(2):273–298. doi: 10.1007/S40121-024-00919-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Anderson DJ, Rojas LF, Watson S, et al. Identification of novel risk factors for community-acquired Clostridium difficile infection using spatial statistics and geographic information system analyses. PLoS One. 2017;12(5) doi: 10.1371/journal.pone.0176285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Malick A, Wang Y, Axelrad J, et al. Obesity Is not associated with adverse outcomes among hospitalized patients with Clostridioides difficile Infection. Gut Pathog. 2022;14(1):7. doi: 10.1186/s13099-022-00479-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dalal RS, Allegretti JR. Diagnosis and Management of Clostridioides difficile Infection in patients with inflammatory bowel disease. Curr Opin Gastroenterol. 2021;37(4):336–343. doi: 10.1097/MOG.0000000000000739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Smits WK, Lyras D, Lacy DB, et al. Clostridium difficile infection. Nat Rev Dis Primers. 2016;2:16020. doi: 10.1038/nrdp.2016.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.O’Mahony D, Cherubini A, Guiteras AR, et al. STOPP/START criteria for potentially inappropriate prescribing in older people: version 3. Eur Geriatr Med. 2023;14(4):625–632. doi: 10.1007/s41999-023-00777-y. Erratum in: Eur Geriatr Med 2023; 14(4)633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bagdasarian N, Rao K, Malani PN. Diagnosis and treatment of Clostridium difficile in adults: a systematic review. JAMA. 2015;313(4):398–408. doi: 10.1001/jama.2014.17103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Vickers RJ, Tillotson GS, Nathan R, et al. CoDIFy study group. efficacy and safety of ridinilazole compared with vancomycin for the treatment of clostridium difficile infection: a phase 2, randomised, double-blind, active-controlled, non-inferiority study. Lancet Infect Dis. 2017;17(7):735–744. doi: 10.1016/S1473-3099(17)30235-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kelly CP, LaMont JT. Clostridium difficile - more difficult than ever. N Engl J Med. 2008;359(18):1932–1940. doi: 10.1056/NEJMra0707500. [DOI] [PubMed] [Google Scholar]
- 65.McFarland LV, Elmer GW, Surawicz CM. Breaking the Cycle: Treatment Strategies for 163 Cases of Recurrent Clostridium Difficile Disease. Am J Gastroenterol. 2002;97(8):1769–1775. doi: 10.1111/j.1572-0241.2002.05839.x. [DOI] [PubMed] [Google Scholar]
- 66.Guery B, Galperine T, Barbut F. Clostridioides difficile: diagnosis and treatments. BMJ (Clinical Research Ed) 2019;366:L4609. doi: 10.1136/bmj.l4609. https://Doi.Org/10.1136/Bmj.L4609 . [DOI] [PubMed] [Google Scholar]
- 67.Kelly CR, Fischer M, Allegretti JR, et al. ACG Clinical Guidelines: prevention, diagnosis, and treatment of Clostridioides difficile infections. Am J Gastroenterol. 2021;2021;116(6):1124–1147. doi: 10.14309/ajg.0000000000001278. Doi.Org/10.14309/Ajg.0000000000001278 . [DOI] [PubMed] [Google Scholar]
- 68.Sandlund J, Davies K, Wilcox MH. Ultrasensitive Clostridioides difficile toxin testing for higher diagnostic accuracy. J Clin Microbiol. 2020;58(6):e01913–19. doi: 10.1128/JCM.01913-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kraft CS, Parrott JS, Cornish NE, et al. A Laboratory medicine best practices systematic review and meta-analysis of nucleic acid amplification tests (NAATs) and algorithms including NAATs for the diagnosis of Clostridioides (Clostridium) difficile in adults. Clin Microbiol Rev. 2019;32(3) doi: 10.1128/CMR.00032-18. Erratum in: Clin Microbiol Rev. 2019; 32(4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ramachandran I, Sinha R, Rodgers P. Pseudomembranous colitis revisited: spectrum of imaging findings. Clin Radiol. 2006;61:535–544. doi: 10.1016/j.crad.2006.03.009. [DOI] [PubMed] [Google Scholar]
- 71.Hookman P, Barkin JS. Clostridium difficile associated infection, diarrhea and colitis. World J Gastroenterol. 2009;15:1554–1580. doi: 10.3748/wjg.15.1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sylva D, Villa P, García C, et al. Pseudomembranous colitis from cytomegalovirus infection. Lancet Gastroenterol Hepatol. 2017;2:384. doi: 10.1016/S2468-1253(17)30044-4. [DOI] [PubMed] [Google Scholar]
- 73.Zar FA, Bakkanagari SR, Moorthi KM, et al. A comparison of vancomycin and metronidazole for the treatment of Clostridium difficile-associated diarrhea, stratified by disease severity. Clin Infect Dis. 2007;45:302–307. doi: 10.1086/519265. [DOI] [PubMed] [Google Scholar]
- 74.Johnson S, Louie TJ, Gerding DN, et al. Polymer alternative for CDI treatment (PACT) investigators. vancomycin, metronidazole, or tolevamer for Clostridium difficile infection: results from two multinational, randomized, controlled trials. Clin Infect Dis. 2014;59:345–354. doi: 10.1093/cid/ciu313. [DOI] [PubMed] [Google Scholar]
- 75.Oksi J, Anttila VJ, Mattila E. Treatment of Clostridioides (Clostridium) difficile infection. Ann Med. 2020;52(1–2):12–20. doi: 10.1080/07853890.2019.1701703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Louie TJ, Miller MA, Mullane KM, et al. OPT-80-003 Clinical study group. fidaxomicin versus vancomycin for Clostridium difficile infection. N Engl J Med. 2011;364:422–431. doi: 10.1056/NEJMoa0910812. [DOI] [PubMed] [Google Scholar]
- 77.Cornely OA, Crook DW, Esposito R, et al. Fidaxomicin versus vancomycin for infection with Clostridium difficile in europe, canada, and the usa: a double-blind, non-inferiority, randomised controlled trial. Lancet Infect Dis. 2012;12:281–289. doi: 10.1016/S1473-3099(11)70374-7. [DOI] [PubMed] [Google Scholar]
- 78.Cornely OA, Miller MA, Louie TJ, et al. Treatment of first recurrence of Clostridium difficile infection: fidaxomicin versus vancomycin. Clin Infect Dis. 2012;55(Suppl 2):S154–161. doi: 10.1093/cid/cis462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Nerandzic MM, Mullane K, Miller MA, et al. Reduced acquisition and overgrowth of vancomycin-resistant enterococci and candida species in patients treated with fidaxomicin versus vancomycin for Clostridium difficile infection. Clin Infect Dis. 2012;55(Suppl 2):S121–126. doi: 10.1093/cid/cis440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Guery B, Menichetti F, Anttila VJ, et al. EXTEND clinical study group. extended-pulsed fidaxomicin versus vancomycin for Clostridium difficile infection in patients 60 years and older. Lancet Infect Dis. 2018;18(3):296–307. doi: 10.1016/S1473-3099(17)30751-X. [DOI] [PubMed] [Google Scholar]
- 81.Duricek M, Halmova K, Krutova M, et al. Is shorter also better in the treatment of Clostridioides difficile infection? J Antimicrob Chemother. 2024;79(6):1413–1417. doi: 10.1093/jac/dkae119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Rokas KE, Johnson JW, Beardsley JR, et al. The addition of intravenous metronidazole to oral vancomycin is associated with improved mortality in critically ill patients with Clostridium difficile infection. Clin Infect Dis. 2015;61(6):934–941. doi: 10.1093/cid/civ409. [DOI] [PubMed] [Google Scholar]
- 83.Wang Y, Schluger A, Li J, et al. Does Addition of Intravenous Metronidazole to Oral Vancomycin Improve Outcomes in Clostridioides difficile Infection? Clin Infect Dis. 2020;71(9):2414–2420. doi: 10.1093/cid/ciz1115. [DOI] [PubMed] [Google Scholar]
- 84.Pipitone G, Granata G, Sartelli M, et al. On the use of intravenous metronidazole for severe and complicated Clostridioides difficile infection: a review and meta-analysis. Infez Med. 2024;32(1):20–24. doi: 10.53854/liim-3201-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kelly CR, Fischer M, Allegretti JR, et al. ACG Clinical guidelines: prevention, diagnosis, and treatment of Clostridioides difficile infections. Am J Gastroenterol. 2021;116(6):1124–1147. doi: 10.14309/ajg.0000000000001278. [DOI] [PubMed] [Google Scholar]
- 86.Van Nood E, Vrieze A, Nieuwdorp M, et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med. 2013;368(5):407–415. doi: 10.1056/NEJMoa1205037. [DOI] [PubMed] [Google Scholar]
- 87.Cammarota G, Masucci L, Ianiro G, et al. Randomised Clinical Trial: faecal microbiota transplantation by colonoscopy vs. vancomycin for the treatment of recurrent Clostridium difficile infection. Aliment Pharmacol Ther. 2015;41(9):835–843. doi: 10.1111/apt.13144. [DOI] [PubMed] [Google Scholar]
- 88.Quraishi MN, Widlak M, Bhala N, et al. Systematic review with meta-analysis: the efficacy of faecal microbiota transplantation for the treatment of recurrent and refractory Clostridium difficile infection. Aliment Pharmacol Ther. 2017;46(5):479–493. doi: 10.1111/apt.14201. [DOI] [PubMed] [Google Scholar]
- 89.Popa D, Neamtu B, Mihalache M, et al. Fecal microbiota transplant in severe and non-severe Clostridioides difficile infection: is there a role of FMT in primary severe CDI? J Clin Med. 2021;10(24):5822. doi: 10.3390/jcm10245822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Baunwall SMD, Andreasen SE, Hansen MM, et al. Faecal microbiota transplantation for first or second Clostridioides difficile infection (EarlyFMT): a randomised, double-blind, placebo-controlled trial. Lancet Gastroenterol Hepatol. 2022;7(12):1083–1091. doi: 10.1016/S2468-1253(22)00276-X. [DOI] [PubMed] [Google Scholar]
- 91.Song YN, Yang DY, Veldhuyzen van Zanten S, et al. Fecal microbiota transplantation for severe or fulminant Clostridioides difficile infection: systematic review and meta-analysis. J Can Assoc Gastroenterol. 2021;5(1):e1–e11. doi: 10.1093/jcag/gwab023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wilcox MH, Gerding DN, Poxton IR, et al. MODIFY I and MODIFY II Investigators. Bezlotoxumab for prevention of recurrent Clostridium difficile infection. N Engl J Med. 2017;376(4):305–317. doi: 10.1056/NEJMoa1602615. [DOI] [PubMed] [Google Scholar]
- 93.Granata G, Schiavone F, Pipitone G. Bezlotoxumab in patients with a primary Clostridioides difficile infection: a literature review. Antibiotics. 2022;11(11):1495. doi: 10.3390/antibiotics11111495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Lamontagne F, Labbé AC, Haeck O, et al. Impact of emergency colectomy on survival of patients with fulminant Clostridium difficile colitis during an epidemic caused by a hypervirulent strain. Ann Surg. 2007;245(2):267–272. doi: 10.1097/01.sla.0000236628.79550.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]