Highlights
-
•
A mixed methods approach was applied through rigorous phases.
-
•
Five factors of structural social capital were extracted.
-
•
For cognitive social capital, factor analysis grouped 43 items into four subscales.
-
•
The maternal social capital assessment tool is valid and reliable.
-
•
The application of such a tool could allow us to decipher the influence of social capital on maternal health.
Keywords: Factor analysis, Maternal health, Social capital, Tool development, Validation
Abstract
Objective
To develop and validate a social capital assessment tool that considers the cultural and social realities of north-western Ethiopia.
Methods
A mixed-methods approach was applied through rigorous phases. Existing measurement approaches for social capital are reviewed. Additionally, a qualitative study was conducted for domain and item identification. The domains and their items were given to panel experts and rated for content validity. Cognitive interviews were conducted with mothers who gave birth in the previous year. For psychometric validation of the tool, 400 mothers who lived in South Gondar zone participated from January 2 to 27, 2023.
Results
Five factors of structural social capital were extracted. These include group participation, emotional, social, financial, and informational support. The content validity index of the scale was 0.88, indicating that 88% of the experts rated the items of the scale as relevant. The loading of the items ranged from 0.505 to 0.858, exceeding the threshold of 0.50. For cognitive social capital, factor analysis grouped 43 items into four subscales: trust in social networks, trust in institutions, trust in the health care system, and social cohesion. The loadings of the items ranged from 0.507 to 0.913. The internal consistency reliability of the scale was excellent, with a Cronbach’s alpha of 0.901.
Conclusion
The Maternal Social Capital Assessment Tool is a valid and reliable instrument for measuring social capital during pregnancy, childbirth, and the postpartum period. The application of such a tool could allow us to decipher the influence of social capital on maternal health.
1. Background
Since the 1980s, researchers including Bourdieu, Coleman, and Putnam have laid a foundation on the multifaceted concept of social capital. It stands for the ability of actors to secure benefits by virtue of membership in social networks or other social structures (Coleman, 1988, Bourdieu, 2011, Putnam, 2000). Community leaders value social capital as a valuable resource for community development and civic engagement laying the groundwork for identifying community strengths and weaknesses (Stout et al., 2011). Unlike physical capital, which depreciates with usage, social capital accumulates as it is used and shared by many people simultaneously (Putnam, 2000).
Social capital is a latent variable that cannot be directly measured. It considers both structural and cognitive dimensions. Structural social capital involves connectivity in social networks and organizations, including participation in voluntary associations, support within the community, and links to institutions. Cognitive social capital considers subjective characteristics such as attitudes and trust in social interactions, sense of belonging, and social cohesion (Agampodi et al., 2017, Islam et al., 2006).
Social capital can affect the health of pregnant women, mothers, and children. It promotes physical and mental well-being and reduces mild illnesses during pregnancy through psychosocial resources and health systems (Agampodi et al., 2017). In addition, domains of social capital such as social trust, a sense of belonging, and community participation have been positively associated with perceived physical and mental health outcomes (Kawachi et al., 2008). Contextual social capital and social support have also been identified as social determinants of the appropriate use of prenatal care (Leal et al., 2011).
Recently, researchers have become interested in examining the role of contextual factors such as social capital beyond individual factors (Derose and Varda, 2009). However, because social capital is highly integrated with social and cultural norms, the concept and context of social capital may vary across communities and societies. The use of consistent measurements over time raises trust in the validity of tools and enables current researchers to build on the work of past scholars (Kawachi et al., 2008, Engbers et al., 2017). There are instruments to measure social capital in English, Spanish, Vietnamese and Chinese (Mokkink et al., 2010, Terwee et al., 2007, De Silva et al., 2006). However, little is known about the psychometric properties of the instrument in Ethiopia, as social capital has its own forms and contexts. This study aimed to develop and validate a context-specific social capital assessment tool for northwest Ethiopia.
2. Methods
2.1. Study design and procedures
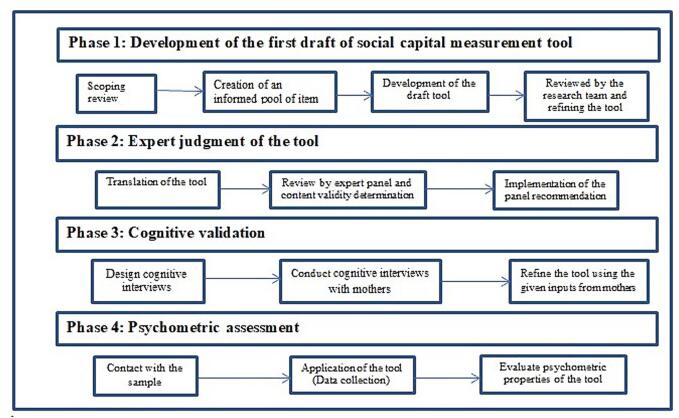
A mixed-methods approach was applied through rigorous phases. In the first phase, a scoping review was performed to map the existing measurement approaches of social capital. Additionally, a qualitative study was conducted for domain and item identification or generation. In the second phase, the domains and their items were given to panel experts (selected based on subject matter knowledge (social capital), research methodology and special training in tool development) to comment them. Then, we have incorporated all necessary comments. Language and subject matter experts translated the forward and backward translation processes. We also arranged meetings to reach consensus, and panel experts rated the content validity of the tool. In the third phase, for face validity, cognitive interviews were conducted with lay experts (mothers who gave birth in the last year). Finally, in the fourth phase, a survey for pilot testing, establishment of the structural validity, estimation of the internal consistency and psychometric property of the tool was assessed (Boateng et al., 2018) (Fig. 1).
Fig. 1.
Tool development and validation process in northwest Ethiopia, 2023.
2.2. Phase one: Development of the first draft of social capital measurement tool
In the first phase, existing literature focusing on measurement approaches for social capital is reviewed. All studies conducted in LMICs that measured any aspect of social capital related to health and were published in English were identified. In the first category, the term related to ‘social capital’ such as ‘social support’, ‘social trust’, ‘social network’, ‘community network’, OR ‘social cohesion’; in the second category, the term ‘health’; in the third category, country terms such as Low- and middle- income countries (LMICs) regions were included. The lists of LMICs were identified from the recent World Bank classification (Fantom and Serajuddin, 2016). All synonym keywords and subject headings were combined with the “OR” Boolean operator. Finally, we combined all three categories using the Boolean operator “AND” to run the databases. Data were extracted from articles or reports using Microsoft Excel. The main information collected from each study contained the last name of the author(s), year of publication, dimensions, and components of social capital. Based on this review, we identified a pool of items that served as the foundation for a draft questionnaire. (Table 2, Table 3) In addition, we employed a qualitative study through in-depth interviews with key informants, and focus group discussions. A maximum variation purposive sampling technique was used to select 41 study participants (11 in-depth interviews and 4 FGDs comprising 7–8 participants) (Mengesha et al., 2023).
Table 2.
Summary of measurement tools of social capital among studies reviewed in low- and middle-income countries.
| Author, publication year | Tool’s name |
|---|---|
| Agampodi et al. (2019) | LMICs Social Capital Assessment Tool for Maternal Health (LSCAT-MH) |
| Harpham et al. (2002) | Adapted Social Capital Assessment Tool (A-SCAT) |
| Harpham et al. (2006) | |
| De Silva et al. (2006) | Short version of the Adapted Social Capital Assessment Tool (SA-SCAT) |
| Ashrafi et al. (2012) | Six item scale |
| Hurtado et al. (2011) | |
| Friche et al. (2013) | Neighborhood scale |
| Borges et al. (2010) | Integrated questionnaire on social capital (SCIQ) |
| de Souza and Grundy (2007) | |
| Mitchell and Bossert (2007) | |
| Wang et al. (2009) | Ten social capital items of trust and mistrust |
| Thuy and Berry (2013) | Australian community participation questionnaire (ACPQ) |
| Brune and Bossert (2009) | World Bank’s Social capital assessment tool (SCAT) |
| Pronyk et al. (2008) | |
| Looman and Farrag (2009) | 20-item Arabic social capital scale |
| Modie-Moroka (2009) | Perceived social capital scale |
| Moscardino et al. (2010) | |
| Moscardino et al. (2010) |
|
| |
| Wang et al. (2014) | Personal Social Capital Scale (PSCS-16 and PSCS-8) |
Table 3.
Socio-demographic characteristics of mothers participated in the survey (n = 400).
| Characteristics | Frequency (%) | |
|---|---|---|
| Residence | Urban | 277 (69.2) |
| Rural | 123 (30.8) | |
| Mean age (SD) | 30.62 (±12.17) | |
| Mean family size (SD) | 3.86 (±1.48) | |
| Marital status | Single | 29 (7.3) |
| Married | 361 (90.3) | |
| Divorced | 8 (2.0) | |
| Widowed | 2 (0.5) | |
| Religion | Orthodox | 318 (79.5) |
| Muslim | 75 (18.8) | |
| Protestant | 7 (1.8) | |
| Highest level of education | Unable to read and write | 78 (19.5) |
| Able to write and read without formal education | 76 (19.0) | |
| Primary education (Grade 1–8) | 84 (21.0) | |
| Secondary education (Grade 9–12) | 89 (22.3) | |
| College diploma and above (12+) | 73 (18.3) | |
| Occupation | Housewife | 179 (44.8) |
| Farmer | 69 (17.3) | |
| Merchant | 64 (16.0) | |
| Government employee | 55 (13.8) | |
| Others | 33 (8.5) | |
| Health facility type where mothers received service | District Hospital | 108 (27.0) |
| Health center | 236 (59.0) | |
| Health post | 56 (14.0) | |
SD: Standard deviation, others: Daily laborer and Student.
2.3. Phase two: Expert judgment of the tool
In the second phase, thirty-four experts participated as expert panels in the study to check the content validity, clarity, and relevance of each item in the draft questionnaire. Of these, 22 experts, including language experts, sociologists, social anthropologists, psychologists, and reproductive and child health experts, had one-day workshop that allowed them to evaluate the content validity of the questionnaire through their independent evaluations. The remaining 12 experts provided feedback via email and telephone. Each expert scored and commented on the modified items. Items that were regularly judged as omitted by experts were removed. At this stage, the second draft of the tool was produced.
The experts were requested to share their views on the relevance, adequacy, comprehensibility, and clarity of the proposed categories and items (Grant and Davis, 1997). The relevance of individual items was evaluated using a four-point scale, ranging from 1 = not relevant to 4 = very relevant, to determine whether items should be retained or rejected in the draft questionnaire.
2.4. Phase-three: Cognitive validation
Cognitive interviews were conducted to determine whether study participants could understand and answer each question by examining the question-and-answer process. Failure to understand questions from the respondent's point of view could lead to misinterpretations, falsified answers, missing responses, and offended respondents (Bowden et al., 2002).
2.5. Phase-four: Psychometric assessment
Mothers who visited the selected health facilities for their child immunization services were invited to participate in the psychometric assessment survey. The survey was conducted in four primary healthcare facilities in the South Gondar zone consisting of one district hospital, two health centers, and one health post. A systematic random sampling technique was used to select a total of 400 participants from January 2 to 27, 2023. First, the average monthly flow was estimated based on the last three-month child immunization services. The sampling interval was then determined by dividing the sample size calculated by the average monthly flow of mothers who were coming to the selected health facilities for their child immunization services. For the qualitative study, purposive sampling technique was used to address mothers’ perception of the perceived meaning of each question during the cognitive interviews.
2.6. Data analysis
In phase one, the item pool was developed inductively, based on qualitative data gathered from focus group discussions and individual women interviews, and deductively, through a review of literature and existing scales related to the identified domains (Mengesha et al., 2023, Mengesha et al., 2021).
In phase two, the content validity index (CVI) was computed. A team of experts evaluated the items using four-point scale to determine whether the items constituted the domain for content relevance, representativeness, and technical quality. The CVI for each scale item is the proportion of experts who rated the item as 3 or 4 on a 4-point scale. The CVI for the entire scale was 0.88. It was computed using the average of all the CVI scores of the items. The summary CVI is the proportion of experts whose endorsement is required to establish content validity beyond the 0.05 level of significance (DeVon et al., 2007) (Additional file 1).
In the third phase, five mothers coming to Felege Hiwot Comprehensive Specialized Hospital for vaccination of their children and pregnant women were asked to respond to the question posed during their prenatal visits. They were also asked to explain their perceptions and thoughts regarding the answers to each question. Finally, we compared the intended and perceived meanings, and checked the acceptability of the items in the draft questionnaire.
Finally, in the fourth phase, the responses to the questionnaires by the study participants were coded and analyzed using the Statistical Package for Social Science (SPSS), and confirmatory factor analysis (CFA) was conducted using SPSS Analysis of Moment Structure (AMOS) version 23 software package (Blunch, 2012) and JASP (Jeffreys’s Amazing Statistics Program) version 0.16.4 software (Faulkenberry et al., 2020). Descriptive statistics and exploratory factor analysis (EFA) were used to determine the psychometric characteristics of the tool, including item responses, internal consistency, and validity.
The important tests carried out by the EFA were the Kaiser–Meyer–Olkin (KMO) Measure of Sampling Adequacy and Bartlett’s Test of Sphericity. The closer the value of KMO to 1, the better the pattern of correlation. However, the cutoff value for KMO must be >0.5, as recommended by Kaiser and Rice (1974). In addition, CFA was employed to test how well a pre-specified measurement theory composed of measured variables and factors fits reality, as captured by data. We assessed the goodness-of-fit of the CFA model using several diagnostic measures, including the chi-square test (χ2), root mean square error of approximation (RMSEA), goodness of fit (GFI), comparative fit index (CFI), Tucker-Lewis index (TLI), relative non-centrality index, and incremental fit index (IFI).
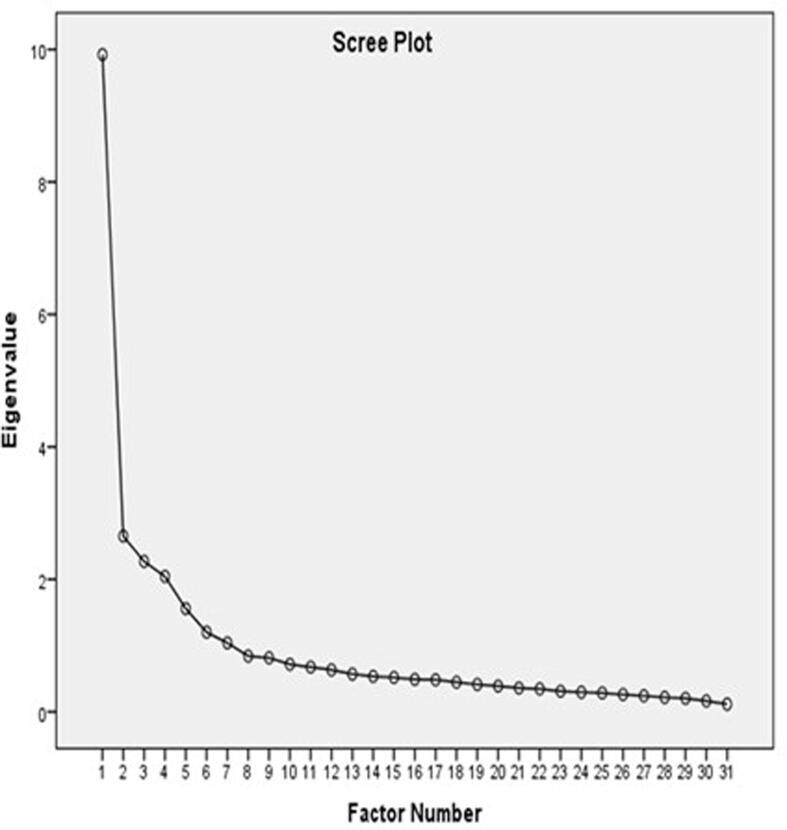
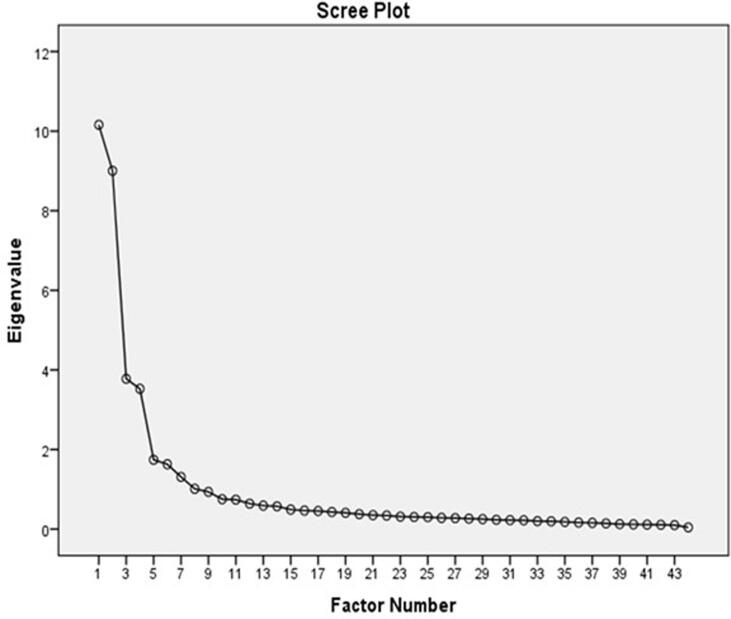
Exploratory factor analysis was employed to determine the optimum number of under social capital factors that could explain the order and structure of the scale’s items. Variables under the structural and cognitive social capital subscales were included separately in the analysis. The Promax rotation method is also employed. The scree plot showed the pattern of eigenvalues of the extracted factors greater than 1.0, against the number of factors in their order of extraction, and the shape of the resulting curve was used to evaluate the cut-off point. A confirmatory factor analysis confirmed the proposed theoretical model. The results implied that the fit of the model was acceptable.
2.7. Ethical considerations
Ethical clearance was obtained from the Institutional Review Board of the College of Medicine and Health Sciences, Bahir Dar University, Ref No. CMHS/IRB/331/2021. Support letters were also obtained from the Amhara Public Health Institute and Woreda Health Offices. To maintain the confidentiality of the study participants, no personal identifiers were asked. Verbal consent was obtained from all participants based on the knowledge that the study was not likely to be harmful and all study participants were over the age of 18 years. Privacy and confidentiality were maintained throughout the data collection, analysis and presentation.
3. Results
3.1. Development of the first draft questionnaire
In the first phase, the qualitative study identified five themes and 13 sub-themes that could be input for the development of the tool. The themes identified were social networking, social norms, social support, and community cohesion. In addition, a scoping review of the measurement of social capital in LMICs was conducted, which served as a basis for establishing the contents of the items and drafting the questionnaire.
3.2. Social capital dimensions
Findings from this review show that the concept of social capital has multiple dimensions. In this review, 12 studies assessed both structural and cognitive social capital, whereas the other three studies examined only cognitive social capital. In addition, four studies measured the bonding and bridging dimensions (Table 1).
Table 1.
Dimensions and components of social capital among studies reviewed in low- and middle-income countries.
| Author, publication year | Dimensions | Components of social capital | |
|---|---|---|---|
| Harpham et al. (2002) | Structural social capital |
|
|
| Harpham et al. (2006) |
|
|
|
| De Silva et al. (2006) |
|
|
|
| Ashrafi et al. (2012) |
|
|
|
| Hurtado et al. (2011) |
|
|
|
| Friche et al. (2013) |
|
|
|
| Borges et al. (2010) |
|
|
|
| Thuy and Berry (2013) |
|
|
|
| Brune and Bossert (2009) |
|
|
|
| Mitchell and Bossert (2007) |
|
|
|
| Looman and Farrag (2009) | |||
| Pronyk et al. (2008) | |||
| Harpham et al. (2002) | Cognitive social capital |
|
|
| Harpham et al. (2006) |
|
|
|
| De Silva et al. (2006) |
|
|
|
| Ashrafi et al. (2012) |
|
|
|
| Hurtado et al. (2011) |
|
|
|
| Friche et al. (2013) |
|
|
|
| Borges et al. (2010) |
|
|
|
| Thuy and Berry (2013) |
|
|
|
| Brune and Bossert (2009) |
|
||
| Mitchell and Bossert (2007) |
|
||
| Looman and Farrag (2009) |
|
||
| Pronyk et al. (2008) | |||
| de Souza and Grundy (2007) | |||
| Wang et al. (2009) | |||
| Modie-Moroka (2009) | |||
| Moscardino et al. (2010) | |||
| Agampodi et al. (2019) | Structural bonding | Informal social networks | |
| Agampodi et al. (2019) | Cognitive bonding | Domestic and neighborhood cohesion | |
| Agampodi et al. (2019) | Structural bridging | Social participation | |
| Ashrafi et al. (2012) | Bonding |
|
|
| Borges et al. (2010) |
|
||
| Agampodi et al. (2019) | |||
| Wang et al. (2014) | |||
| Ashrafi et al. (2012) | Bridging |
|
|
| Borges et al. (2010) |
|
||
| Agampodi et al. (2019) |
|
||
| Wang et al. (2014) |
|
||
3.3. Measurement tools for social capital
Related to the measurement of social capital, 18 studies conducted in LMICs that used 14 different measurement tools were reviewed. The instruments used to measure social capital vary in their content.
The items listed in the instrument were too extended and time-consuming to complete. As a result, a short form of the Adapted Social Capital Assessment Tool (SA-SCAT) with 12 items, the Personal Social Capital Scale (PSCS-16) with 16 items, and the PSCS-8 with eight items was developed and used in a multi-country large-scale survey study (De Silva et al., 2006, Wang et al., 2014, Chen et al., 2009). Another study also used SA-SCAT with a nine-item instrument derived for assessing personally owned social capital. Although the original instrument, SCAT, was developed by a team from the World Bank (Krishna and Shrader, 2000), the items used to assess group membership in the SA-SCAT have its limitations. The study participants experienced difficulties in answering culture-specific questions as ‘trade union’, ‘community association’, and ‘credit/funeral associations. The SA-SCAT tool does not measure emotional, economic, and instrumental sources of support separately (De Silva et al., 2006, Chen et al., 2009) (Table 2).
4. Psychometric assessment
4.1. Socio-demographic characteristics
A total of 400 mothers who came for their child immunization service participated, with a response rate of 91 %. Of these, 90.3 % were married at a mean age and standard deviation (SD) of 30.62 (±12.17) years. The majority of mothers (59 %) received services from a health center (Table 3).
4.2. Exploratory factor analysis
In total, 107 items were included in the structural social capital subscale. Of these, five factors with 31 items were extracted. These include group participation, emotional, social, financial, and informational support. The loading of the items ranged from 0.505 to 0.858, above the threshold value of 0.50 (Hair, 2011). 73 items were eliminated because of low loading (<0.40) and cross loading. The KMO for the items with structural social capital was 0.897. In addition, the Bartlett's test of sphericity was significant (P < 0.001). The KMO for the items under cognitive social capital was 0.899 and the Bartlett's test of sphericity was significant (P < 0.001). These results indicated that the data were appropriate for factor analysis (Additional file 3 and Table 5).
For cognitive social capital, a four-factor solution with 43 items was extracted. These included trust in social networks, institutions, health systems, and social cohesion. The loadings of the items ranged from 0.507 to 0.913. Out of the 80 items included in the analysis, 37 were eliminated due to low loading and cross-loading. (Additional file 4 and Table 6).
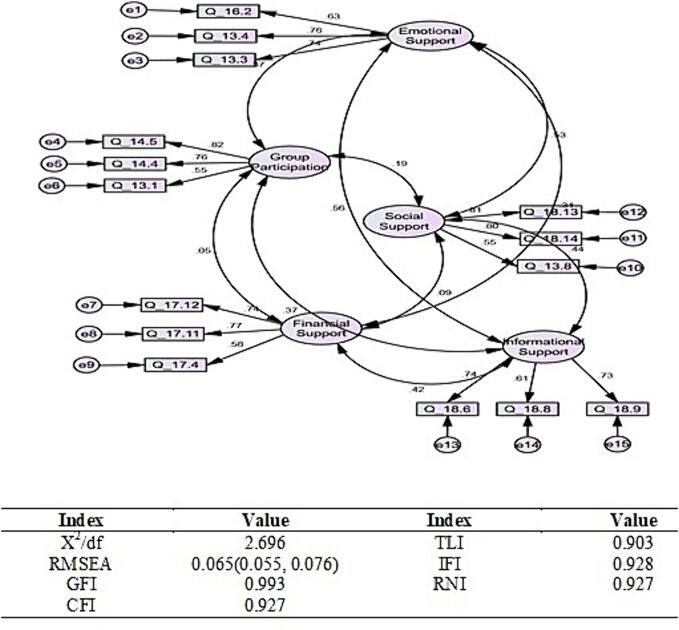
4.3. Confirmatory factor analysis
The EFA results showed five factors for structural social capital and four factors for cognitive social capital, while the CFA results further supported the factor structure. The five factors confirmed under structural social capital were emotional support, group participation, social support, financial support, and informational support; the items were included in each factor (Fig. 2).
Fig. 2.
Confirmatory factor analysis of structural social capital in northwest Ethiopia, 2023.
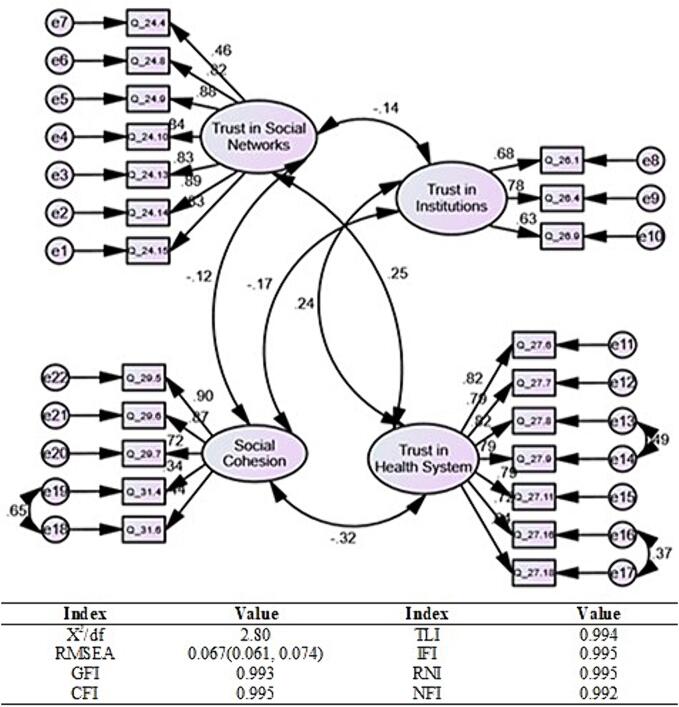
The four factors confirmed under cognitive social capital were trust in social networks, trust in institutions, trust in the health system, and social cohesion; the items were included in each factor (Fig. 3). In general, 37 items (15 for structural social capital and 22 for cognitive social capital) were confirmed in the CFA (Additional file 2).
Fig. 3.
Confirmatory factor analysis of cognitive social capital in northwest Ethiopia, 2023.
5. Discussion
The objective of this study was to develop and validate a culturally appropriate measure of maternal social capital in north-western Ethiopia. A reliable and valid instrument was developed to assess mothers' social capital. The most important dimensions are structural and cognitive social capital. The following section interprets the properties of the newly developed and validated social capital assessment instrument, including evidence of its content validity, factor analysis results, and data reliability. In addition, the results are discussed in light of previous literature and the limitations of the present study, implications for future research are identified, and applications of the new scale are discussed.
The content validity index (CVI) of the entire scale was 0.88, which means that 88 % of the experts rated the items of the scale as very or fairly relevant. Most of the questions were rated as relevant, but the wording was criticized. Therefore, the content of the instrument is valid, as a CVI score of 0.78 and above is considered acceptable content validity (Polit et al., 2007). Agreement indices are the only component in determining content validity and should not be used as the sole basis for rejecting or modifying items (Halek et al., 2017).
During the development and validation of the instrument, several changes were made to the maternal social capital assessment instrument, including a reduction in the number of items from 187 to 37. This significant reduction in the number of items is the result of the elimination of items related to EFA and CFA. As a result of the EFA, 111 items (74 and 37 for structural and cognitive social capital, respectively) were eliminated, leaving 76 items. In addition, 39 items were eliminated during the CFA, leaving 37 items in the final version of the social capital scale. The newly developed maternal social capital assessment tool is a relatively short instrument with good reliability, as indicated by its high internal consistency. The number of items also varied for previous social capital assessment instruments, including the SCAT (Brune and Bossert, 2009), A-SCAT (Harpham et al., 2006), SA-SCAT (De Silva et al., 2006), and LSCAT-MH (Agampodi et al., 2019). These tools emerged with the advent of heterogeneous definitions of social capital in many fields (Portes, 1998, Putnam et al., 1992). However, none of these scales have been validated in the Ethiopian context.
Regarding the structural social capital subscale, five factors were extracted: group participation, emotional support, social support, financial support, and information support. Using the root mean square error of approximation (RMSEA) as an indicator of the goodness of fit of the factor solution, a five-factor solution yielded an RMSEA of 0.065. Additionally, for cognitive social capital, a four-factor solution with 43 items yielded an RMSEA of 0.067. These were trust in social networks, trust in institutions, trust in the healthcare system, and social cohesion. According to Browne and Cudeck, the RMSEA is 0.0 for a perfect fit, between 0.0 and 0.05 for a close fit, between 0.05 and 0.10 for a good fit, and above 0.10 for a poor fit (Browne and Cudeck, 1992). Therefore, both the five and four-factor solutions fell within a good fit range.
5.1. Strength and limitation of the study
This study describes the development of an instrument to measure the social capital related to maternal health in Ethiopia. The tool development process was comprehensive and included a review study, in-depth qualitative research, and content and psychometric validations. The new social capital assessment instrument has adequate reliability, face, content, and cross-cultural validity. In addition, the instrument was developed in collaboration with experts, such as psychologists, sociologists, social anthropologists, and reproductive health and child health experts, who are involved in practice and research on social capital and maternal health.
Regarding the limitations of this study, many of the questions in the tool were Likert scales, in which respondents reported their subjective assessments. In addition, those who had poor social participation might have underreported community activities and social harmony.
5.2. Implications of this study
Considering these limitations, this study serves as a platform for other researchers and stakeholders involved in the study of social capital to improve maternal health. The application of such an instrument to different cultural contexts could also allow us to decipher the influence of sociocultural aspects on social capital and maternal health. Such research has the potential to influence practice through the development of policies that improve public attitudes toward indigenous social networks. In addition, future research should be conducted in different regions of Ethiopia and to explore the application of this tool in populations with greater diversity in terms of culture, socioeconomic status, age, education, marital status, and social networks.
6. Conclusion
In the present study, a reliable and valid instrument was developed to assess mothers' social capital in north-western Ethiopia. To ensure external validity, future research should validate this instrument in diverse populations. It is also necessary to examine both the predictors and outcomes of social capital.
7. Consent for publication
Not applicable.
Funding
This research was supported by the Amhara Public Health Institute and the Bahir Dar University.
CRediT authorship contribution statement
Endalkachew Worku Mengesha: Writing – review & editing, Writing – original draft, Validation, Software, Methodology, Investigation, Formal analysis, Data curation. Gizachew A. Tessema: Writing – review & editing, Validation, Supervision, Methodology, Formal analysis, Data curation. Yibeltal Assefa: Writing – review & editing, Validation, Supervision, Methodology, Formal analysis, Data curation. Getu Degu Alene: Validation, Supervision, Formal analysis, Data curation, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors would like to acknowledge the support of Amhara Public Health Institute, and Bahir Dar University for providing support in data collection. Our profound gratitude goes to panel of experts, women, and managers and to all study respondents who gave their time and opinions so generously.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2024.102869.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Supplementary Fig. 1.
The scree plot of structural social capital in northwest Ethiopia, 2023.
Supplementary Fig. 2.
The scree plot of cognitive social capital in northwest Ethiopia, 2023.
Content validity check list evaluated by experts in northwest Ethiopia, 2023.
Validated social capital assessment tool in northwest Ethiopia, 2023.
Items, factors and loadings of the extracted structural social capital tool in northwest Ethiopia, 2023.
Factors and loadings of the extracted cognitive social capital tool in northwest Ethiopia, 2023.
Data availability
The original contributions presented in the study are included in the article/additional files. Further inquiries can be directed to the corresponding author.
References
- Agampodi T.C., Rheinländer T., Agampodi S.B., Glozier N., Siribaddana S. Social capital and health during pregnancy; an in-depth exploration from rural Sri Lanka. Reprod. Health. 2017;14(1):1–19. doi: 10.1186/s12978-017-0349-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agampodi T.C., Agampodi S.B., Glozier N., Lelwala T., Sirisena K., Siribaddana S. Development and validation of the Social Capital Assessment Tool in pregnancy for Maternal Health in Low and middle income countries (LSCAT-MH) BMJ Open. 2019;9(7):e027781. doi: 10.1136/bmjopen-2018-027781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashrafi E., Montazeri A., Mousavi M., Vaez-Mahdavi M., Asadi-Lari M. Influence of sociodemographic features and general health on social capital: findings from a large population-based survey in Tehran, Iran (Urban-HEART) Public Health. 2012;126(9):796–803. doi: 10.1016/j.puhe.2012.06.013. [DOI] [PubMed] [Google Scholar]
- Blunch N. Sage; 2012. Introduction to Structural Equation Modeling Using IBM SPSS Statistics and AMOS. [Google Scholar]
- Boateng G.O., Neilands T.B., Frongillo E.A., Melgar-Quiñonez H.R., Young S.L. Best practices for developing and validating scales for health, social, and behavioral research: a primer. Front. Public Health. 2018;6:149. doi: 10.3389/fpubh.2018.00149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges C.M., Campos A.C.V., Vargas A.D., Ferreira E.F., Kawachi I. Social capital and self-rated health among adolescents in Brazil: an exploratory study. BMC. Res. Notes. 2010;3(1):1–6. doi: 10.1186/1756-0500-3-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourdieu, P., 1986. The forms of capital. Cultural theory: An anthology 1, 81–93.
- Bowden A., Fox-Rushby J., Nyandieka L., Wanjau J. Methods for pre-testing and piloting survey questions: illustrations from the KENQOL survey of health-related quality of life. Health Policy Plan. 2002;17(3):322–330. doi: 10.1093/heapol/17.3.322. [DOI] [PubMed] [Google Scholar]
- Browne M.W., Cudeck R. Alternative ways of assessing model fit. Soc. Methods Res. 1992;21(2):230–258. [Google Scholar]
- Brune N.E., Bossert T. Building social capital in post-conflict communities: evidence from Nicaragua. Soc. Sci. Med. 2009;68(5):885–893. doi: 10.1016/j.socscimed.2008.12.024. [DOI] [PubMed] [Google Scholar]
- Chen X., Stanton B., Gong J., Fang X., Li X. Personal Social Capital Scale: an instrument for health and behavioral research. Health Educ. Res. 2009;24(2):306–317. doi: 10.1093/her/cyn020. [DOI] [PubMed] [Google Scholar]
- Coleman J.S. Social capital in the creation of human capital. Am. J. Soc. 1988;94:S95–S120. [Google Scholar]
- De Silva M.J., Harpham T., Tuan T., Bartolini R., Penny M.E., Huttly S.R. Psychometric and cognitive validation of a social capital measurement tool in Peru and Vietnam. Soc. Sci. Med. 2006;62(4):941–953. doi: 10.1016/j.socscimed.2005.06.050. [DOI] [PubMed] [Google Scholar]
- de Souza E.M., Grundy E. Intergenerational interaction, social capital and health: results from a randomised controlled trial in Brazil. Soc. Sci. Med. 2007;65(7):1397–1409. doi: 10.1016/j.socscimed.2007.05.022. [DOI] [PubMed] [Google Scholar]
- Derose K.P., Varda D.M. Social capital and health care access: a systematic review. Med. Care Res. Rev.: MCRR. 2009;66(3):272. doi: 10.1177/1077558708330428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeVon H.A., Block M.E., Moyle-Wright P., Ernst D.M., Hayden S.J., Lazzara D.J., et al. A psychometric toolbox for testing validity and reliability. J. Nurs. Scholarsh. 2007;39(2):155–164. doi: 10.1111/j.1547-5069.2007.00161.x. [DOI] [PubMed] [Google Scholar]
- Engbers T.A., Thompson M.F., Slaper T.F. Theory and measurement in social capital research. Soc. Indic. Res. 2017;132(2):537–558. [Google Scholar]
- Fantom, N.J., Serajuddin, U., 2016. The World Bank's classification of countries by income. World Bank Policy Research Working Paper. 2016(7528).
- Faulkenberry T.J., Ly A., Wagenmakers E.-J. Bayesian inference in numerical cognition: a tutorial using JASP. J. Numer. Cogn. 2020;6(2):231–259. [Google Scholar]
- Friche, A., Diez-Roux, A., César, C., Xavier, C., Proietti, F., Caiaffa, W., 2013. Assessing the psychometric and ecometric properties of neighborhood scales in developing countries: Saúde em Beagá Study, Belo Horizonte, Brazil, 2008-2009. J. Urban Health 90(2). [DOI] [PMC free article] [PubMed]
- Grant J.S., Davis L.L. Selection and use of content experts for instrument development. Res. Nurs. Health. 1997;20(3):269–274. doi: 10.1002/(sici)1098-240x(199706)20:3<269::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- Hair J.F. Multivariate data analysis: an overview. Int. Encycl. Stat. Sci. 2011:904–907. [Google Scholar]
- Halek M., Holle D., Bartholomeyczik S. Development and evaluation of the content validity, practicability and feasibility of the Innovative dementia-oriented Assessment system for challenging behaviour in residents with dementia. BMC Health Serv. Res. 2017;17:1–26. doi: 10.1186/s12913-017-2469-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harpham T., Grant E., Thomas E. Measuring social capital within health surveys: key issues. Health Policy Plan. 2002;17(1):106–111. doi: 10.1093/heapol/17.1.106. [DOI] [PubMed] [Google Scholar]
- Harpham T., De Silva M.J., Tuan T. Maternal social capital and child health in Vietnam. J. Epidemiol. Commun. Health. 2006;60(10):865–871. doi: 10.1136/jech.2005.044883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurtado D., Kawachi I., Sudarsky J. Social capital and self-rated health in Colombia: the good, the bad and the ugly. Soc. Sci. Med. 2011;72(4):584–590. doi: 10.1016/j.socscimed.2010.11.023. [DOI] [PubMed] [Google Scholar]
- Islam M.K., Merlo J., Kawachi I., Lindström M., Gerdtham U.-G. Social capital and health: does egalitarianism matter? A literature review. Int. J. Equity Health. 2006;5(1):1–28. doi: 10.1186/1475-9276-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser H.F., Rice J. Little jiffy, mark IV. Educ. Psychol. Meas. 1974;34(1):111–117. [Google Scholar]
- Kawachi I., Subramanian S.V., Kim D. Springer; 2008. Social capital and health. Social capital and health. pp. 1–26. [Google Scholar]
- Krishna A., Shrader E. Cross-cultural measures of social capital: a tool and results from India and Panama. Soc. Cap. Initiat. Working Paper. 2000;21:1–118. [Google Scholar]
- Leal M.C., Pereira A.P.E., Lamarca G.A., Vettore M.V. The relationship between social capital, social support and the adequate use of prenatal care. Cad. Saude Publ. 2011;27(suppl 2):s237–s253. doi: 10.1590/s0102-311x2011001400011. [DOI] [PubMed] [Google Scholar]
- Looman W.S., Farrag S. Psychometric properties and cross-cultural equivalence of the Arabic Social Capital Scale: Instrument development study. Int. J. Nurs. Stud. 2009;46(1):45–54. doi: 10.1016/j.ijnurstu.2008.07.010. [DOI] [PubMed] [Google Scholar]
- Mengesha E.W., Alene G.D., Amare D., Assefa Y., Tessema G.A. Social capital and maternal and child health services uptake in low- and middle-income countries: mixed methods systematic review. BMC Health Serv. Res. 2021;21(1):1142. doi: 10.1186/s12913-021-07129-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mengesha E.W., Tessema G.A., Assefa Y., Alene G.D. Social capital and its role to improve maternal and child health services in Northwest Ethiopia: a qualitative study. PLoS One. 2023;18(4):e0284592. doi: 10.1371/journal.pone.0284592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell A.D., Bossert T.J. Measuring dimensions of social capital: evidence from surveys in poor communities in Nicaragua. Soc. Sci. Med. 2007;64(1):50–63. doi: 10.1016/j.socscimed.2006.08.021. [DOI] [PubMed] [Google Scholar]
- Modie-Moroka T. Does level of social capital predict perceived health in a community?—a study of adult residents of low-income areas of Francistown, Botswana. J. Health Popul. Nutr. 2009;27(4):462. doi: 10.3329/jhpn.v27i4.3390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokkink L.B., Terwee C.B., Knol D.L., Stratford P.W., Alonso J., Patrick D.L., et al. The COSMIN checklist for evaluating the methodological quality of studies on measurement properties: a clarification of its content. BMC Med. Res. Method. 2010;10(1):1–8. doi: 10.1186/1471-2288-10-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moscardino U., Scrimin S., Capello F., Altoè G. Social support, sense of community, collectivistic values, and depressive symptoms in adolescent survivors of the 2004 Beslan terrorist attack. Soc. Sci. Med. 2010;70(1):27–34. doi: 10.1016/j.socscimed.2009.09.035. [DOI] [PubMed] [Google Scholar]
- Polit D.F., Beck C.T., Owen S.V. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res. Nurs. Health. 2007;30(4):459–467. doi: 10.1002/nur.20199. [DOI] [PubMed] [Google Scholar]
- Portes A. Social capital: Its origins and applications in modern sociology. Annu. Rev. Sociol. 1998;24(1):1–24. [Google Scholar]
- Pronyk P.M., Harpham T., Morison L.A., Hargreaves J.R., Kim J.C., Phetla G., et al. Is social capital associated with HIV risk in rural South Africa? Soc. Sci. Med. 2008;66(9):1999–2010. doi: 10.1016/j.socscimed.2008.01.023. [DOI] [PubMed] [Google Scholar]
- Putnam R.D. Springer; 2000. Bowling alone: America’s declining social capital. Culture and politics; pp. 223–234. [Google Scholar]
- Putnam R.D., Leonardi R., Nanetti R.Y. Princeton University Press; 1992. Making Democracy work: Civic Traditions in Modern Italy. [Google Scholar]
- Stout M., Harms J., Knapp T., Vess L. measuring social capital and building community in the ozarks. Contexts. 2011;10(1):20–25. [Google Scholar]
- Terwee C.B., Bot S.D., de Boer M.R., van der Windt D.A., Knol D.L., Dekker J., et al. Quality criteria were proposed for measurement properties of health status questionnaires. J. Clin. Epidemiol. 2007;60(1):34–42. doi: 10.1016/j.jclinepi.2006.03.012. [DOI] [PubMed] [Google Scholar]
- Thuy N.T.M., Berry H.L. Social capital and mental health among mothers in Vietnam who have children with disabilities. Glob. Health Action. 2013;6(1):18886. doi: 10.3402/gha.v6i0.18886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang P., Chen X., Gong J., Jacques-Tiura A.J. Reliability and validity of the personal social capital scale 16 and personal social capital scale 8: two short instruments for survey studies. Soc. Indic. Res. 2014;119(2):1133–1148. [Google Scholar]
- Wang H., Schlesinger M., Wang H., Hsiao W.C. The flip-side of social capital: the distinctive influences of trust and mistrust on health in rural China. Soc. Sci. Med. 2009;68(1):133–142. doi: 10.1016/j.socscimed.2008.09.038. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Content validity check list evaluated by experts in northwest Ethiopia, 2023.
Validated social capital assessment tool in northwest Ethiopia, 2023.
Items, factors and loadings of the extracted structural social capital tool in northwest Ethiopia, 2023.
Factors and loadings of the extracted cognitive social capital tool in northwest Ethiopia, 2023.
Data Availability Statement
The original contributions presented in the study are included in the article/additional files. Further inquiries can be directed to the corresponding author.