Key Points
Question
Is active visual art therapy associated with patient health outcomes?
Findings
In this meta-analysis including 50 studies with 217 outcomes and 2766 individuals, evidence was markedly heterogeneous regarding outcomes, population, and study quality. Based on the available evidence, active visual art therapy was associated with an improvement in 18% of the patient outcomes.
Meaning
The findings of this study suggest that, given its association with patient outcomes, visual art therapy may be considered a valuable addition to standard medical care.
Abstract
Importance
Art therapy has a long-standing tradition in patient treatment. As scientific interest in its use has recently grown, a comprehensive assessment of active visual art therapy is crucial to understanding its potential benefits.
Objective
To assess the association of active visual art therapy with health outcomes across patient groups and comparators.
Data Sources
The systematic literature search included the Cochrane Library, Embase, MEDLINE, CINAHL, ERIC, American Psychological Association PsycArticles, American Psychological Association PsycInfo, PSYNDEX, the German Clinical Trials Register, and ClinicalTrials.gov. No filters regarding language were applied. The search covered all dates before March 2021. Data analysis was conducted from April 24 to September 8, 2023.
Study Selection
Randomized clinical trials with any type of patient population comparing the intervention with any control not using active visual art therapy were included. Two researchers independently screened the abstracts and full texts.
Data Extraction and Synthesis
Data extraction followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines, and study quality was evaluated using the Cochrane Risk of Bias tool. Data were synthesized using narrative summaries, forest plots, and random effects meta-analyses.
Main Outcome and Measures
In line with the protocol, all outcome measures of the included studies were extracted.
Results
The search identified 3104 records, of which 356 outcomes of 69 studies were included, with a total of approximately 4200 participants, aged 4 to 96 years, in the review. The meta-analyses included 50 studies and 217 outcomes of 2766 participants. Treatment indications included mental, neurological, and other somatic disorders, and prevention. Most outcome measures focused on depression, anxiety, self-esteem, social adjustment, and quality of life. Art therapy was associated with an improvement in 18% of the 217 outcomes compared with the controls (1%), while 81% showed no improvement. The standardized mean difference in the change from baseline of the meta-analyses of 0.38 (95% CI, 0.26-0.51) and posttest analysis of 0.19 (95% CI, 0.12-0.26) also indicated an improvement of outcomes associated with art therapy. Overall study quality was low.
Conclusions and Relevance
In this systematic review and meta-analysis of randomized clinical trials, visual art therapy was associated with therapeutic benefits for some outcomes, although most studies were of low quality. Further good-quality studies are needed to provide additional insights for its best possible integration into routine care.
This systematic review and meta-analysis examines the use of visual art therapy in the prevention and treatment of mental health disorders.
Introduction
The use of art therapy is widespread across many countries and disciplines,1 especially in the areas of mental health,2 rehabilitation, pain management, holistic cancer treatment, and care of older individuals. Various versions of art therapy are used in a wide variety of settings, including hospitals,3 schools,4 prisons,5 or nursing homes.6 Despite its popularity, to our knowledge, the use of art therapy was never systematically documented, which impedes the estimation of the number of global recipients. The lack of documentation and scarcity of large studies might be the reason why art therapy is not always routinely funded and integrated into standard care. Our study contributes to closing this gap.
A report from the World Health Organization has summarized the existing evidence on art and health in a scoping review, triangulating different study designs, patient groups, and indications.7 After including more than 900 publications in the review, the authors concluded that the arts have a great potential to enhance and maintain good health. While this extensive report has provided many useful insights into the benefits of art therapy and has further established the role art can play in gaining and maintaining health, the review has been criticized for the absence of a systematic literature search and a quality screening of the individual studies.8
We set out to conduct what is, to our knowledge, the first systematic review and meta-analysis of all existing randomized and controlled art therapy evidence in a single report that also takes quality of the included studies into account. We therefore believe that it may be a helpful addition to the World Health Organization report and other existing literature. To provide an overview of the complex evidence base, we aimed to gather all currently available studies on the effectiveness of art therapy. Since the overall study quality and methods are very diverse, we decided to focus on randomized clinical trials (RCTs), which are considered the standard for evaluating interventions and limit some of the bias associated with other study designs.9
With this systematic review and meta-analysis, we aimed to gather all available evidence regarding the effectiveness of active visual art therapy (AVAT). Since we are particularly interested in enhancing the well-being of patients, we decided to focus on the application of AVAT both to alleviate current symptoms and as a preventive measure.
Methods
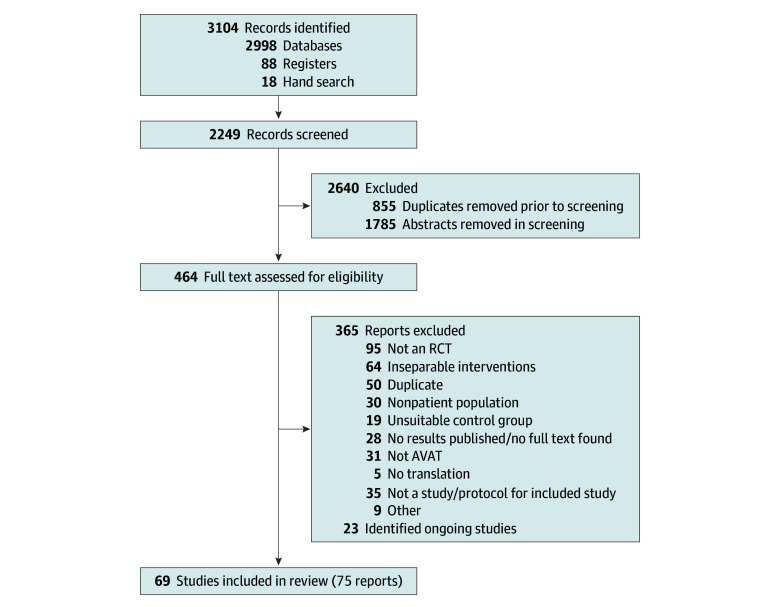
The protocol for this systematic review and meta-analysis has been registered with PROSPERO (CRD42021233272), and details of the methods have been published.10 We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guideline,11 and the Cochrane handbook.12 The literature search flow diagram is shown in Figure 1.
Figure 1. Flowchart of the Study Selection Process for the Systematic Review of AVAT.
The number of included studies and reports is not identical, because some articles published outcomes in separate reports, while others reported more than 1 study. AVAT indicates active visual art therapy; RCT, randomized clinical trial.
Eligibility Criteria
Study Design, Intervention, and Control Group
We defined AVAT as any type of artistic activity in which patients would actively manipulate materials with their hands, such as drawing, painting, ceramic sculpting, any form of arts and crafts, and sand painting. Not included were all forms of music therapy, dance therapy, literature-based therapy, and therapy based on performing arts. To keep the diverse range of art therapies as comparable as possible, we also excluded all digital interventions.
As per our predefined search criteria, we only included RCTs in which one group used AVAT and the other group used anything other than AVAT (including no intervention, treatment as usual, attention control, or a non-AVAT intervention). Studies that used art as a diagnostic tool but not as an intervention were excluded.
Participants
We included all patient groups and groups receiving targeted preventive art therapy. Reasons for exclusion were induced moods (eg, artificial anxiety induction in healthy intervention groups), studies on healthy college students, or educational classroom settings with no clear preventive or curative target.
Outcomes
We included all RCT outcomes in our review. To identify the range of conditions and issues addressed by art therapy, we extracted all scales and measures from the studies included in our review and assigned them to broader categories.
If a study had more than 1 method of measuring the same end point, we only included 1 measure for this end point, selected either based on popularity of the measure or interpretability of the score. Studies with an attrition of more than 50% were excluded from the analysis.
Search Strategy
To create a conclusive overview, we did not apply any language filters or date of publication limits. The search consisted of 3 elements, which were combined.10 The first element referred to the art, the second element referred to the therapeutic use of the art, and the third consisted of an adapted RCT filter.13,14 The search strategy was adapted according to the functionality of the individual databases, and the literature search syntax was peer reviewed by 2 of us (R.J. and A.B.) according to the Peer Review of Electronic Search Strategies guideline.15
Following the Cochrane recommendations, we searched the Cochrane library, MEDLINE, and Embase (through Ovid). In addition, we searched CINAHL, ERIC, American Psychological Association PsycArticles, American Psychological Association PsycInfo, PSYNDEX (all through EBSCOHost), the German Clinical Trials Register, and ClinicalTrials.gov. At the time of our search, the World Health Organization International Clinical Trials Registry Platform was not accessible. We also conducted a hand search of the Journal of Creative Arts Therapies. All systematic searches were conducted March 8 and 9, 2021.
Study Selection
The study selection followed a 2-step process, aided by Covidence software16; first, all titles and abstracts were screened, and second, relevant studies were identified through thorough review of the full text. Both steps were done independently: the title and abstract screening (R.J., W.A.G., and A.B.) and the full text screening (R.J. and W.A.G.). All disagreements were resolved by a subsequent discussion.
The references of identified reviews were screened for studies that we might have missed. Any protocols for planned studies we found were matched to the published study for later bias evaluation and added to the list of ongoing studies.
Data Extraction and Categorization
Information on the intervention (materials used, frequency, duration, and therapist training), control group, participants (age, sex, and indication), study characteristics (country of study and study arms), outcome (group size, scale description, and preintervention and postintervention data), data regarding possible bias, and other information were extracted by 1 of us (R.J. or C.K.) using a data extraction form (eAppendix in Supplement 1).
For better comparability, we tagged the outcomes across all studies with outcome tags, which we aggregated in a second step into 6 broader categories. A similar approach was used for the recorded treatment indications. Furthermore, we categorized the included study populations into 3 age groups according to the patients’ median, mean, or range of age, depending on how the data were reported. If participants spanned more than 1 age category, we labeled that study in accordance with the greatest numbers of its members. We defined children and adolescents as a study population younger than 18 years, adults as individuals aged between 18 and 65 years, and older adults as those older than 65 years.
If there were multiple control groups that could not be combined due to missing data (eg, combined SDs), we extracted the less-specific control group (eg, treatment as usual) to ensure greater compatibility across studies. If there were multiple follow-up measures of an outcome, we only considered the first measurement after the intervention had stopped to ensure comparability.
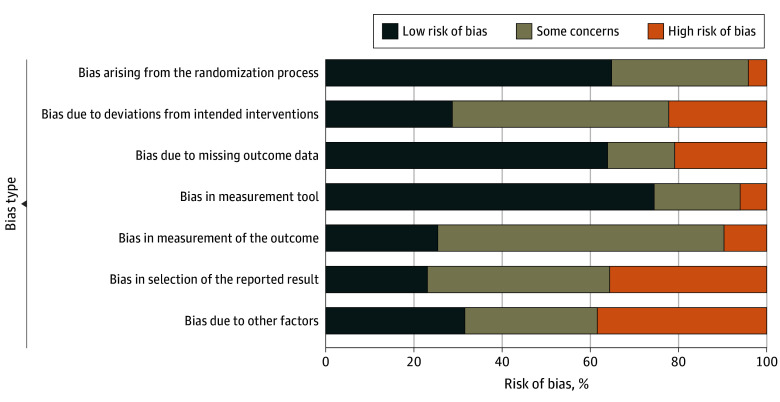
Bias Evaluation
Bias evaluation was performed by 1 of us (R.J. or C.K.) using an adapted version of the Cochrane risk-of-bias tool for randomized trials.17,18 The evaluated domains of bias were the randomization process, deviations from intended interventions, missing outcome data, measurement tool used, measurement of the outcome, selection of the reported result, and other factors.
Statistical Analysis
We performed random-effects meta-analyses, with standardized mean difference (SMD) as pooled-effect size and 2-sided 95% CIs. Outcomes with sufficient data are displayed in forest plots. To be displayed, each study outcome had to report at least the number of participants in the study and the mean (SD) of the outcome for the control and intervention groups separately, measured after the intervention. Likert scales with 5 or more levels, as well as scales with counts, were treated as continuous data for the analysis.
We summarized outcomes reported as either change from baseline or posttest separately, following standard practice. If both were reported, we used change from baseline. Change from baseline represents the change of variables after the AVAT treatment compared with a baseline level determined before the intervention, whereas posttest measures are observations after the intervention. Given the heterogeneity of the outcomes, we applied a random-effects model for the meta-analyses. We planned to perform a meta-regression including patient age, publication date, intervention duration, therapist qualification, treatment setting, type of AVAT, and country.
The analysis was conducted from April 24 to September 8, 2023, using RStudio, version 4.3.0 (R Foundation for Statistical Computing).19 Specifically, we used the package meta to calculate the meta-analysis and create the forest plots for all outcomes with sufficient and adequate outcome data.19,20 We chose Hedges g as the effect size and used the package’s default random-effects model DerSimonian-Laird. For the creation of the risk-of-bias plot (Figure 2), we used the packages robvis21 and ggplot2.22
Figure 2. Bias as Assessed by the Adapted Cochrane Risk of Bias Tool for Randomized Trials for Outcomes of Studies Included in the Analysis.
Results
Results of Literature Search
Our search yielded 1368 results in the Cochrane library: 1223 through Ovid, 407 through EBSCOhost, 78 from Clinicaltrials.gov, and 10 from the German Clinical Trials Register. A further 18 studies were added after reference screening during the literature-screening stage. Of the resulting 3104 reports, 855 were duplicates and were removed using EndNote.23 The full study selection process can be seen in Figure 1.11 We translated all non-English and non-German records (including French, Chinese, Korean, and Turkish articles) during the screening process using Google Translate24 and DeepL Translator.25 There were 5 reports that could not be translated due to their format and resulting technical limitations (2 Persian, 2 Hebrew, and 1 Korean), and were thus excluded.
Included Studies
We identified 75 reports of 69 studies that were eligible for this review3,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98 (eTable 1 in Supplement 1). Some publications reported the results of 2 studies in 1 article (eg, Gussak et al46), whereas the results of other studies were reported in several publications (eg, Öster et al,70,71,72 Svensk et al,75 and Thyme et al76). When there were multiple reports of the same study, we included all outcome measures that were not duplicates. The article title and a brief description of the study population, intervention, and control group are presented in the eTable 1 in Supplement 1 , while a more-detailed description of the characteristics of the included studies, including age of participants, country of publication, scale of the outcome, total hours of intervention, level of bias, and characteristics of intervention and control groups, are displayed in the eTable in Supplement 2.
Characteristics of Included Studies
Age of Study Population
Overall, most studies included an adult population (n = 31), followed by children and adolescents (n = 17) and older adults (n = 17); approximately 4200 participants were included. The age range was 4 to 96 years. Four studies examined the effect of AVAT on children together with their parents.
Countries
We included studies from 21 known countries; 1 study did not specify its location. Most studies were conducted in the US (23), followed by the UK (5), Iran (5), and Sweden (4). Japan, Israel, Germany, and China each contributed 3 trials. Furthermore, 2 studies were conducted in each of the following countries: the Netherlands, Turkey, Taiwan, South Korea, India, and France, and 1 study each was carried out in Iraq, Italy, Brazil, Russia, Tanzania, Australia, and Indonesia.
Comparators
The included control groups were very diverse and subsequently classified into 6 categories. These control categories were treatment as usual (25), other (17), attention control (10), no intervention (10), waiting list control (5), and not specified (2).
Included Interventions
The included studies used a wide variety of art therapy interventions, which we clustered into the 7 following categories according to the materials used: drawing/sketching (48), painting (43), arts and crafts (23), sculpting (17), not specified (12), coloring-in/mandala (7), and other (7). Most interventions fell into 2 or more of the categories. Most AVAT interventions (49) included a therapeutic element, 17 did not, and for the remaining 3 it was unclear.
Ongoing Studies
We identified 23 study descriptions of ongoing research projects that fulfilled our criteria of AVAT. An overview of these studies can be found in eTable 2 in Supplement 1.
Treatment Indications for AVAT
Most studies investigated AVAT received by patients with mental health problems (37 studies), followed by patients with neurologic symptoms (13 studies), art therapy as prevention (10 studies), or for patients with other somatic challenges (9 studies).
Outcomes Treated With AVAT
We identified 356 end point measures of 48 different outcome categories in the studies. Most outcome measures focused on depression, anxiety, self-esteem, social adjustment, and quality of life. Most frequently, AVAT was used to alleviate psychiatric symptoms (86 measures), improve psychological well-being (77), reduce social and behavioral problems (63), and improve cognitive function (16) or other somatic symptoms (eg, pain, asthma exacerbations, and hand function) (17). Seven measures (eg, treatment satisfaction or intervention costs) fit in none of those categories.
Of the identified 69 studies with 356 end point measures, we included 50 studies with 217 end point measures in the meta-analysis. Reasons for omitting end points included missing posttest means or SDs (96), a participant dropout rate of more than 50% (9), an ordinal (2) or dichotomous (2) outcome, and other reasons, such as measures of subscales when there was a total score of the instrument provided (30).
Association of AVAT and Health Outcomes
A total of 217 outcomes of 50 studies from 53 publications, including data from 2766 patients were included in 2 meta-analyses4,26,27,28,30,31,33,35,36,37,38,39,41,42,44,45,46,47,48,50,51,52,53,55,56,57,59,60,61,62,63,64,66,67,69,71,73,75,76,79,80,81,82,83,84,86,90,91,92,96,97,98,99 (eTable 1 in Supplement 1). Of the total 217 outcomes, 18% favored AVAT, 1% favored the control group, and 81% showed no effect.
We created forest plots as a visual representation of the results (eFigure 1 and eFigure 2 in Supplement 1). These meta-analyses are explorative and thus nonconfirmatory. In the change from baseline random-effects meta-analysis, AVAT was associated with more positive health outcomes than the control groups (SMD, 0.38; 95% CI, 0.26-0.51). Results should be interpreted with caution due to substantial heterogeneity (I2 = 71%; τ2 = 0.23; P < .001).
The posttest random-effects meta-analysis also favored outcomes of disorders treated with AVAT over the control groups (SMD, 0.19; 95% CI, 0.12-0.26). Heterogeneity was substantial (I2 = 53%; τ2 = 0.08; P < .001).
Subgroups
We conducted some explorative subgroup analyses. We divided the data by age groups and found, based on visual inspection of the forest plot, the outcomes of children improved slightly more on average than the other 2 age groups. When looking at the control groups, we could see that this seemed to be especially true when comparing AVAT with no intervention or treatment as usual (posttest) and waiting list (change from baseline) comparison groups, and that interventions with a therapeutic element might lead to a slightly more favorable total result.
Meta-Regression
We calculated a meta-regression with the 9 moderators we predefined in the protocol. The meta-regression yielded inconclusive results due to the large number and variety of included factors.
Risk of Bias Assessment
Bias in the measurement of the outcome, selective reporting bias, and other sources of bias were the most common causes for bias in the measurement of the outcomes. While many studies displayed low bias in multiple categories, all studies had at least 1 source of unclear or high bias. The eTable in Supplement 2 provides a detailed list of all assessed bias, including for missing outcome data. The funnel plots indicate a slight publishing bias (eFigure 3 and eFigure 4 in Supplement 1).
Discussion
Overall, AVAT was associated with an improvement of health outcomes, especially in the area of mental health or when treating somatic conditions that may be associated with impaired mental health. This aligns with our practical observations made in clinical settings, where AVAT seems to be frequently associated with the management of mental health issues.
Multiple factors are of special relevance when discussing the results of this review. One of these factors involves the properties of the AVAT interventions. While it was exceeding the scope of this review to separate the effects of the different art types from each other to estimate outcomes, the presence or absence of a therapeutic element seems to be of particular relevance to the intervention. This observation aligns with the principles of patient-centered care, emphasizing the critical role of therapeutic engagement in the healing process.
A notable observation is the regional difference in AVAT research, with more studies conducted in the US and UK, possibly indicating differences in AVAT use. This may hint at the possible influence of structural and political factors shaping research priorities. With the benefits of AVAT, these findings underscore the need to promote equitable health care access by extending the benefits of AVAT to diverse populations, regardless of regional boundaries.
To further the quality of art therapy research and thereby lay the foundation for a future integration into standard care, it might be beneficial to establish guidelines that enhance research consistency and comparability. These guidelines should include standards for reporting AVAT and control interventions, thereby facilitating the future synthesis of treatment effects. Furthermore, the guidelines should incorporate a framework on suitable control interventions to avoid methodologic flaws. Such improvements would not only increase the research quality of the field but also provide a better foundation for evidence-based clinical decision-making.
Limitations
This study has limitations. While this meta-analysis exclusively focused on RCTs, a triangulation of different methods is valuable when studying a complex and multifaceted intervention such as art therapy. Furthermore, the heterogeneity of the control groups posed unique challenges when examining AVAT. Several studies had to be excluded because the control group’s engagement included AVAT and therefore could not serve as a valid comparator. But even the remaining control interventions often contained therapy elements, such as psychotherapy, pharmaceuticals, and therapy dog encounters. Some complex treatment-as-usual interventions may have contained elements of AVAT. These potentially very effective control interventions might dilute the true effects of AVAT interventions in our data and have probably contributed to the observed heterogeneity. The observed association of AVAT and improved health outcomes in our data, despite these strong comparators, attests to the potential of AVAT.
Conclusions
In this systematic review and meta-analysis, we found an overall benefit associated with AVAT interventions with the potential to improve various patient outcomes, particularly in the area of mental health. Those positive tendencies might even increase in magnitude with improving study quality. To reach that goal, international collaboration and harmonization of research methods are important.
eAppendix. Data Extraction Form
eTable 1. Characteristics of the Included Studies, Including the Short ID, Title, a Brief Description of the Study Population, Intervention and Control Group
eTable 2. Ongoing or Recently Published Studies That Investigate the Effectiveness of AVAT
eFigure 1. Forest Plot of the Effects of AVAT for Studies Presenting Results as Change From Baseline
eFigure 2. Forest Plot of the Effects of AVAT for Studies Presenting Results as Post-test
eFigure 3. Funnel Plot for Change From Baseline Outcomes
eReferences
eTable. Detailed Description of Study Characteristics
Data Sharing Statement
References
- 1.Sajnani N, Fietje N. The Jameel Arts & Health Lab in collaboration with the WHO-Lancet global series on the health benefits of the arts. Lancet. 2023;402(10414):1732-1734. doi: 10.1016/S0140-6736(23)01959-1 [DOI] [PubMed] [Google Scholar]
- 2.Haeyen S, van Hooren S, van der Veld WM, Hutschemaekers G. Promoting mental health versus reducing mental illness in art therapy with patients with personality disorders: a quantitative study. Arts Psychother. 2018;58:11-16. doi: 10.1016/j.aip.2017.12.009 [DOI] [Google Scholar]
- 3.Brady C, Moss H, Kelly BD. A fuller picture: evaluating an art therapy programme in a multidisciplinary mental health service. Med Humanit. 2017;43(1):30-34. doi: 10.1136/medhum-2016-011040 [DOI] [PubMed] [Google Scholar]
- 4.Yan H, Chen J, Huang J. School bullying among left-behind children: the efficacy of art therapy on reducing bullying victimization. Front Psychiatry. 2019;10:40. doi: 10.3389/fpsyt.2019.00040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gussak D. The effectiveness of art therapy in reducing depression in prison populations. Int J Offender Ther Comp Criminol. 2007;51(4):444-460. doi: 10.1177/0306624X06294137 [DOI] [PubMed] [Google Scholar]
- 6.Jeppson TA, Nudo CA, Mayer JF. Painting for a purpose: a visual arts program as a method to promote engagement, communication, cognition, and quality of life for individuals with dementia. Am J Speech Lang Pathol. 2022;31(4):1687-1701. doi: 10.1044/2022_AJSLP-21-00300 [DOI] [PubMed] [Google Scholar]
- 7.Fancourt D, Finn S. What Is the Evidence on the Role of the Arts in Improving Health and Well-Being? A Scoping Review. World Health Organization Regional Office for Europe; 2019. [PubMed] [Google Scholar]
- 8.Clift S, Fancourt D, Finn S. What is the evidence on the role of the arts in improving health and well-being? a scoping review. Nordic J Arts Culture Health. 2020;2(1):77-83. doi: 10.18261/issn.2535-7913-2020-01-08 [DOI] [Google Scholar]
- 9.Hariton E, Locascio JJ. Randomised controlled trials—the gold standard for effectiveness research: study design, randomised controlled trials. BJOG. 2018;125(13):1716-1716. doi: 10.1111/1471-0528.15199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Joschko R, Roll S, Willich SN, Berghöfer A. The effect of active visual art therapy on health outcomes: protocol of a systematic review of randomised controlled trials. Syst Rev. 2022;11(1):96. doi: 10.1186/s13643-022-01976-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89. doi: 10.1186/s13643-021-01626-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Higgins JPT, Thomas J, Chandler J, et al. , eds. Cochrane Handbook for Systematic Reviews of Interventions, version 6.1. September 2020. Accessed August 9, 2024. www.training.cochrane.org/handbook
- 13.Wong SS, Wilczynski NL, Haynes RB. Developing optimal search strategies for detecting clinically sound treatment studies in EMBASE. J Med Libr Assoc. 2006;94(1):41-47. [PMC free article] [PubMed] [Google Scholar]
- 14.Lefebvre C, Glanville J, Briscoe S, et al. Searching for and selecting studies. In: Higgins JPT, Thomas J, Chandler J, et al, eds. Cochrane Handbook for Systematic Reviews of Interventions version 6.1. 2020. Accessed August 9, 2024. www.training.cochrane.org/handbook
- 15.McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40-46. doi: 10.1016/j.jclinepi.2016.01.021 [DOI] [PubMed] [Google Scholar]
- 16.Veritas Health Innovation . Covidence systematic review software. Accessed August 9, 2024. www.covidence.org
- 17.Higgins JPT, Savović J, Page MJ, Elbers RG, Sterne JAC. 8.2 Overview of RoB 2. In: Higgins JPT, Thomas J, Chandler J, et al. , eds. Cochrane Handbook for Systematic Reviews of Interventions, version 6.1. September 2020. 6.1 ed. Cochrane, 2020. Accessed August 9, 2024. www.training.cochrane.org/handbook [Google Scholar]
- 18.Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:4898. doi: 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 19.R Foundation for Statistical Computing . R: a language and environment for statistical computing, version 4.3.0. 2023. Accessed August 9, 2024. https://www.R-project.org
- 20.Schwarzer G, Carpenter JR, Rücker G. Meta-Analysis With R. Switzerland Springer; 2015. doi: 10.1007/978-3-319-21416-0 [DOI] [Google Scholar]
- 21.McGuinness LA, Higgins JPT. Risk-of-bias visualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. 2021;12(1):55-61. doi: 10.1002/jrsm.1411 [DOI] [PubMed] [Google Scholar]
- 22.Wickham H. ggplot2: Elegant Graphics for Data Analysis. 1st ed. Springer; 2019. [Google Scholar]
- 23.Clarivate. EndNote. version, EndNote X9. 2013. Accessed August 9, 2024. https://endnote.com/
- 24.Google L. GoogletTranslate. 2006. Accessed August 1, 2022. http://translate.google.com
- 25.Kutylowski J. DeepL Translator. DeepL SE. 2017. Accessed August 1, 2022. https://www.deepl.com/de/translator
- 26.Abbing A, Baars EW, de Sonneville L, Ponstein AS, Swaab H. The effectiveness of art therapy for anxiety in adult women: a randomized controlled trial. Front Psychol. 2019;10(May):1203-1203. doi: 10.3389/fpsyg.2019.01203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abbing A, de Sonneville L, Baars E, Bourne D, Swaab H. Anxiety reduction through art therapy in women: exploring stress regulation and executive functioning as underlying neurocognitive mechanisms. PLoS One. 2019;14(12):e0225200. doi: 10.1371/journal.pone.0225200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abdulah DM, Abdulla BMO. Effectiveness of group art therapy on quality of life in paediatric patients with cancer: a randomized controlled trial. Complement Ther Med. 2018;41:180-185. doi: 10.1016/j.ctim.2018.09.020 [DOI] [PubMed] [Google Scholar]
- 29.Barfarazi H, Pourghaznein T, Mohajer S, Mazlom SR, Asgharinekah SM. Evaluating the effect of painting therapy on happiness in the elderly. Evidence Based Care J. 2018;8(3):17-26. [Google Scholar]
- 30.Bazargan Y, Pakdaman S. The effectiveness of art therapy in reducing internalizing and externalizing problems of female adolescents. Arch Iran Med. 2016;19(1):51-56. [PubMed] [Google Scholar]
- 31.Beebe A, Gelfand EW, Bender B. A randomized trial to test the effectiveness of art therapy for children with asthma. J Allergy Clin Immunol. 2010;126(2):263-266, 266.e1. doi: 10.1016/j.jaci.2010.03.019 [DOI] [PubMed] [Google Scholar]
- 32.Beh-Pajooh A, Abdollahi A, Hosseinian S. The effectiveness of painting therapy program for the treatment of externalizing behaviors in children with intellectual disability. Vulnerable Child Youth Stud. 2018;13(3):221-227. doi: 10.1080/17450128.2018.1428779 [DOI] [Google Scholar]
- 33.Blomdahl C, Guregård S, Rusner M, Wijk H. A manual-based phenomenological art therapy for individuals diagnosed with moderate to severe depression (PATd): a randomized controlled study. Psychiatr Rehabil J. 2018;41(3):169-182. doi: 10.1037/prj0000300 [DOI] [PubMed] [Google Scholar]
- 34.Borchers KK. Do gains made in group art therapy persist? A study with aftercare patients. Am J Art Ther. 1985;23(3):89-91. [PubMed] [Google Scholar]
- 35.Bozzatello P, Bellino S, De Marzi G, et al. Effectiveness of psychosocial treatments on symptoms and functional domains in schizophrenia spectrum disorders: a prospective study in a real-world setting. Disabil Rehabil. 2019;41(23):2799-2806. doi: 10.1080/09638288.2018.1480666 [DOI] [PubMed] [Google Scholar]
- 36.Broome ME, Maikler V, Kelber S, Bailey P, Lea G. An intervention to increase coping and reduce health care utilization for school-age children and adolescents with sickle cell disease. J Natl Black Nurses Assoc. 2001;12(2):6-14. [PubMed] [Google Scholar]
- 37.Çetinkaya F, Aşiret G, Direk F, Özkanlı N. The effect of ceramic painting on the life satisfaction and cognitive status of older adults residing in a nursing home. Top Geriatr Rehabil. 2019;35:108-112. doi: 10.1097/TGR.0000000000000208 [DOI] [Google Scholar]
- 38.Ching-Teng Y, Ya-Ping Y, Yu-Chia C. Positive effects of art therapy on depression and self-esteem of older adults in nursing homes. Soc Work Health Care. 2019;58(3):324-338. doi: 10.1080/00981389.2018.1564108 [DOI] [PubMed] [Google Scholar]
- 39.Choi H. Jung D-J, Jeon Y-H, Kim MJ. The effects of combining art psychotherapy with pharmacotherapy in treating major depressive disorder: randomized control study. Arts Psychother. 2020;70:101689. doi: 10.1016/j.aip.2020.101689 [DOI] [Google Scholar]
- 40.Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 41.Ciasca EC, Ferreira RC, Santana CLA, et al. Art therapy as an adjuvant treatment for depression in elderly women: a randomized controlled trial. Braz J Psychiatry. 2018;40(3):256-263. doi: 10.1590/1516-4446-2017-2250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Crawford MJ, Killaspy H, Barnes TR, et al. ; MATISSE project team . Group art therapy as an adjunctive treatment for people with schizophrenia: multicentre pragmatic randomised trial. BMJ. 2012;344:e846. doi: 10.1136/bmj.e846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Decker KP, Deaver SP, Abbey V, Campbell M, Turpin C. Quantitatively improved treatment outcomes for combat-associated PTSD with adjunctive art therapy: randomized controlled trial. Art Ther (Alex). 2019;35(4):184-194. doi: 10.1080/07421656.2018.1540822 [DOI] [Google Scholar]
- 44.Ellis-Hill C, Thomas S, Gracey F, et al. HeART of Stroke: randomised controlled, parallel-arm, feasibility study of a community-based arts and health intervention plus usual care compared with usual care to increase psychological well-being in people following a stroke. BMJ Open. 2019;9(3):e021098. doi: 10.1136/bmjopen-2017-021098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gussak D. Effects of art therapy with prison inmates: a follow-up study. Arts Psychother. 2006;33(3):188-198. doi: 10.1016/j.aip.2005.11.003 [DOI] [Google Scholar]
- 46.Gussak D. The effects of art therapy on male and female inmates: advancing the research base. Arts Psychother. 2009;36(1):5-12. doi: 10.1016/j.aip.2008.10.002 [DOI] [Google Scholar]
- 47.Haeyen S, van Hooren S, van der Veld W, Hutschemaekers G. Efficacy of art therapy in individuals with personality disorders cluster B/C: a randomized controlled trial. J Pers Disord. 2018;32(4):527-542. doi: 10.1521/pedi_2017_31_312 [DOI] [PubMed] [Google Scholar]
- 48.Hattori H, Hattori C, Hokao C, Mizushima K, Mase T. Controlled study on the cognitive and psychological effect of coloring and drawing in mild Alzheimer’s disease patients. Geriatr Gerontol Int. 2011;11(4):431-437. doi: 10.1111/j.1447-0594.2011.00698.x [DOI] [PubMed] [Google Scholar]
- 49.Hill KE, Lineweaver TT. Improving the short-term affect of grieving children through art. Art Ther (Alex). 2016;33(2):91-98. doi: 10.1080/07421656.2016.1166414 [DOI] [Google Scholar]
- 50.Hsiao CY, Chen SL, Hsiao YS, Huang HY, Yeh SH. Effects of art and reminiscence therapy on agitated behaviors among older adults with dementia. J Nurs Res. 2020;28(4):e100. doi: 10.1097/jnr.0000000000000373 [DOI] [PubMed] [Google Scholar]
- 51.Ilali ES, Mokhtary F, Mousavinasab N, Tirgari AH. Impact of art-based life review on depression symptoms among older adults. Art Ther (Alex). 2018;35(3):148-155. doi: 10.1080/07421656.2018.1531276 [DOI] [Google Scholar]
- 52.Jouybari L, Abbariki E, Jebeli M, et al. Comparison of the effect of narrative writing and art therapy on maternal stress in neonatal intensive care settings. J Matern Fetal Neonatal Med. 2020;33(4):664-670. doi: 10.1080/14767058.2018.1499719 [DOI] [PubMed] [Google Scholar]
- 53.Leurent B, Killaspy H, Osborn DP, et al. Moderating factors for the effectiveness of group art therapy for schizophrenia: secondary analysis of data from the MATISSE randomised controlled trial. Soc Psychiatry Psychiatr Epidemiol. 2014;49(11):1703-1710. doi: 10.1007/s00127-014-0876-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Katz C, Barnetz Z, Hershkowitz I. The effect of drawing on children’s experiences of investigations following alleged child abuse. Child Abuse Negl. 2014;38(5):858-867. doi: 10.1016/j.chiabu.2014.01.003 [DOI] [PubMed] [Google Scholar]
- 55.Khedekar S, Shimpi AP, Shyam A, Sancheti P. Use of art as therapeutic intervention for enhancement of hand function in patients with rheumatoid arthritis: a pilot study. Indian J Rheumatol. 2017;12(2). doi: 10.4103/0973-3698.199130 [DOI] [Google Scholar]
- 56.Kim SK. A randomized, controlled study of the effects of art therapy on older Korean-Americans’ healthy aging. Arts Psychother. 2013;40(1):158-164. doi: 10.1016/j.aip.2012.11.002 [DOI] [Google Scholar]
- 57.Kline JA, VanRyzin K, Davis JC, et al. Randomized trial of therapy dogs versus deliberative coloring (art therapy) to reduce stress in emergency medicine providers. Acad Emerg Med. 2020;27(4):266-275. doi: 10.1111/acem.13939 [DOI] [PubMed] [Google Scholar]
- 58.Kopytin A, Lebedev A. Humor, self-attitude, emotions, and cognitions in group art therapy with war veterans. Art Ther (Alex). 2013;30(1):20-29. doi: 10.1080/07421656.2013.757758 [DOI] [Google Scholar]
- 59.Lalingkar RA, Yadav TS, Gijare SS. Effect of recreational therapy on attention and depression in school children with learning difficulties. Indian J Public Health Res Dev. 2020;11(3):573-578. [Google Scholar]
- 60.Laurer M, van der Vennet R. Effect of art production on negative mood and anxiety for adults in treatment for substance abuse. Art Ther (Alex). 2015;32(4):177-183. doi: 10.1080/07421656.2015.1092731 [DOI] [Google Scholar]
- 61.Lawson LM, Williams P, Glennon C, et al. Effect of art making on cancer-related symptoms of blood and marrow transplantation recipients. Oncol Nurs Forum. 2012;39(4):E353-E360. doi: 10.1188/12.ONF.E353-E360 [DOI] [PubMed] [Google Scholar]
- 62.Liu C. Examining the effectiveness of solution-focused art therapy (SF-AT) for sleep problems of children with traumatic experience [dissertation], ProQuest Information & Learning; 2018. [Google Scholar]
- 63.Lock J, Fitzpatrick KK, Agras WS, Weinbach N, Jo B. Feasibility study combining art therapy or cognitive remediation therapy with family-based treatment for adolescent anorexia nervosa. Eur Eat Disord Rev. 2018;26(1):62-68. doi: 10.1002/erv.2571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Masika GM, Yu DSF, Li PWC. Can visual art therapy be implemented with illiterate older adults with mild cognitive impairment? a pilot mixed-method randomized controlled Trial. J Geriatr Psychiatry Neurol. 2021;34(1):76-86. doi: 10.1177/0891988720901789 [DOI] [PubMed] [Google Scholar]
- 65.McCaffrey R. The effect of healing gardens and art therapy on older adults with mild to moderate depression. Holist Nurs Pract. 2007;21(2):79-84. doi: 10.1097/01.HNP.0000262022.80044.06 [DOI] [PubMed] [Google Scholar]
- 66.Montag C, Haase L, Seidel D, et al. A pilot RCT of psychodynamic group art therapy for patients in acute psychotic episodes: feasibility, impact on symptoms and mentalising capacity. PLoS One. 2014;9(11):e112348. doi: 10.1371/journal.pone.0112348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Morris JH, Kelly C, Joice S, et al. Art participation for psychosocial wellbeing during stroke rehabilitation: a feasibility randomised controlled trial. Disabil Rehabil. 2019;41(1):9-18. doi: 10.1080/09638288.2017.1370499 [DOI] [PubMed] [Google Scholar]
- 68.Narme P, Tonini A, Khatir F, Schiaratura L, Clément S, Samson S. [Non pharmacological treatment for Alzheimer’s disease: comparison between musical and non-musical interventions]. Geriatr Psychol Neuropsychiatr Vieil. 2012;10(2):215-224. doi: 10.1684/pnv.2012.0343 [DOI] [PubMed] [Google Scholar]
- 69.Omizo MM, Omizo SA. Art activities to improve self-esteem among Native Hawaiian children. J Humanist Educ Dev. 1989;27(4):167-176. doi: 10.1002/j.2164-4683.1989.tb00173.x [DOI] [Google Scholar]
- 70.Öster I, Magnusson E, Thyme KE, Lindh J, Astrom S. Art therapy for women with breast cancer: the therapeutic consequences of boundary strengthening. Arts Psychother. 2007;34:277-288. doi: 10.1016/j.aip.2007.04.003 [DOI] [Google Scholar]
- 71.Öster I, Svensk AC, Magnusson E, et al. Art therapy improves coping resources: a randomized, controlled study among women with breast cancer. Palliat Support Care. 2006;4(1):57-64. doi: 10.1017/S147895150606007X [DOI] [PubMed] [Google Scholar]
- 72.Öster I, Tavelin B, Thyme K, et al. Art therapy during radiotherapy—a five-year follow-up study with women diagnosed with breast cancer. Arts Psychother. 2014;41(1):36-40. doi: 10.1016/j.aip.2013.10.003 [DOI] [Google Scholar]
- 73.Pongan E, Tillmann B, Leveque Y, et al. ; LACMé Group . Can musical or painting interventions improve chronic pain, mood, quality of life, and cognition in patients with mild Alzheimer’s disease? evidence from a randomized controlled trial. J Alzheimers Dis. 2017;60(2):663-677. doi: 10.3233/JAD-170410 [DOI] [PubMed] [Google Scholar]
- 74.Qin Y. Effect of music therapy intervention on physical functions and mental health of patients with ankylosing spondylitis. Psychiatr Danub. 2020;32(3-4):403-410. doi: 10.24869/psyd.2020.403 [DOI] [PubMed] [Google Scholar]
- 75.Svensk AC, Öster I, Thyme KE, et al. Art therapy improves experienced quality of life among women undergoing treatment for breast cancer: a randomized controlled study. Eur J Cancer Care (Engl). 2009;18(1):69-77. doi: 10.1111/j.1365-2354.2008.00952.x [DOI] [PubMed] [Google Scholar]
- 76.Thyme KE, Sundin EC, Wiberg B, Öster I, Aström S, Lindh J. Individual brief art therapy can be helpful for women with breast cancer: a randomized controlled clinical study. Palliat Support Care. 2009;7(1):87-95. doi: 10.1017/S147895150900011X [DOI] [PubMed] [Google Scholar]
- 77.Agbaria Q. Acquiring social and cognitive skills in an intervention for Arab parents of children with intellectual developmental disability accompanied by behavioral conditions. Child Fam Soc Work. 2020;25(S1):73-82. doi: 10.1111/cfs.12715 [DOI] [Google Scholar]
- 78.Ramirez K, Haen C, Cruz RF. Investigating impact: the effects of school-based art therapy on adolescent boys living in poverty. Arts Psychother. 2020;71:101710. doi: 10.1016/j.aip.2020.101710 [DOI] [Google Scholar]
- 79.Rao D, Nainis N, Williams L, Langner D, Eisin A, Paice J. Art therapy for relief of symptoms associated with HIV/AIDS. AIDS Care. 2009;21(1):64-69. doi: 10.1080/09540120802068795 [DOI] [PubMed] [Google Scholar]
- 80.Regev D, Guttmann J. The psychological benefits of artwork: the case of children with learning disorders. Arts Psychother. 2005;32(4):302-312. doi: 10.1016/j.aip.2005.02.001 [DOI] [Google Scholar]
- 81.Richardson P, Jones K, Evans C, Stevens P, Rowe A. Exploratory RCT of art therapy as an adjunctive treatment in schizophrenia. J Ment Health. 2009;16(4):483-491. doi: 10.1080/09638230701483111 [DOI] [Google Scholar]
- 82.Robinson EM, Baker R, Hossain MM. Randomized trial evaluating the effectiveness of coloring on decreasing anxiety among parents in a pediatric surgical waiting area. J Pediatr Nurs. 2018;41:80-83. doi: 10.1016/j.pedn.2018.02.001 [DOI] [PubMed] [Google Scholar]
- 83.Rosal ML. Comparative group art therapy research to evaluate changes in locus of control in behavior disordered children. Arts Psychother. 1993;20(3):231-241. doi: 10.1016/0197-4556(93)90018-W [DOI] [Google Scholar]
- 84.Roswiyani R, Hiew CH, Witteman CLM, Satiadarma MP, Spijker J. Art activities and qigong exercise for the well-being of older adults in nursing homes in Indonesia: a randomized controlled trial. Aging Ment Health. 2020;24(10):1569-1578. doi: 10.1080/13607863.2019.1617239 [DOI] [PubMed] [Google Scholar]
- 85.Rusted J, Sheppard L, Waller D. A multi-centre randomized control group trial on the use of art therapy for older people with dementia. Group Analysis. 2006;39(4):517-536. doi: 10.1177/0533316406071447 [DOI] [Google Scholar]
- 86.Schrade C, Tronsky L, Kaiser DH. Physiological effects of mandala making in adults with intellectual disability. Arts Psychother. 2011;38(2):109-113. doi: 10.1016/j.aip.2011.01.002 [DOI] [Google Scholar]
- 87.Schreier H, Ladakakos C, Morabito D, Chapman L, Knudson MM. Posttraumatic stress symptoms in children after mild to moderate pediatric trauma: a longitudinal examination of symptom prevalence, correlates, and parent-child symptom reporting. J Trauma. 2005;58(2):353-363. doi: 10.1097/01.TA.0000152537.15672.B7 [DOI] [PubMed] [Google Scholar]
- 88.Siegel J, Iida H, Rachlin K, Yount G. Expressive arts therapy with hospitalized children: a pilot study of co-creating healing sock creatures. J Pediatr Nurs. 2016;31(1):92-98. doi: 10.1016/j.pedn.2015.08.006 [DOI] [PubMed] [Google Scholar]
- 89.Sommer F, Obenaus K, Engelmann U. Creative-dynamic image synthesis: a useful addition to the treatment options for impotence. Int J Impot Res. 2001;13(5):268-274. doi: 10.1038/sj.ijir.3900729 [DOI] [PubMed] [Google Scholar]
- 90.Sterz C, Heimes S, Blessing T, Flachenecker P. Creative arts therapy improves quality of life in MS—results of a randomized controlled trial during inpatient rehabilitation. Neurol Rehab. 2013;19(3):176-182. [Google Scholar]
- 91.Sukru F, Ozturk M, Kilic O, Guneytepe S, Ucok A. The impact of a six-month interpersonal group psychotherapy on functionality of patients with schizophrenia in a community mental health center. Alpha Psychiatry. 2018;19:59-67. [Google Scholar]
- 92.Thyme KE, Sundin EC, Stahlberg G, Lindstrom B, Eklof H, Wiberg B. The outcome of short-term psychodynamic art therapy compared to short-term psychodynamic verbal therapy for depressed women. Psychoanal Psychother. 2007;21(3):250-264. doi: 10.1080/02668730701535610 [DOI] [Google Scholar]
- 93.Tibbetts TJ, Stone B. Short-term art therapy with seriously emotionally disturbed adolescents. Arts Psychother. 1990;17(2):139-146. doi: 10.1016/0197-4556(90)90024-K [DOI] [Google Scholar]
- 94.Wahlbeck H, Kvist LJ, Landgren K. Art therapy and counseling for fear of childbirth: a randomized controlled trial. Art Ther (Alex). 2020;37(3):123-130. doi: 10.1080/07421656.2020.1721399 [DOI] [Google Scholar]
- 95.Wu CJ, Lee SY. After the intervention: an evaluation and analysis of visual art therapy in the treatment of PTSD. Int J Clin Exp Med. 2020;13(10):7646-7653. [Google Scholar]
- 96.Yamada T, Kawamata H, Kobayashi N, Kielhofner G, Taylor RR. A randomised clinical trial of a wellness programme for healthy older people. Br J Occup Ther. 2010;73(11):540-548. doi: 10.4276/030802210X12892992239314 [DOI] [Google Scholar]
- 97.Yount G, Rachlin K, Siegel J. Expressive arts therapy for hospitalized children: a pilot study measuring cortisol levels. Pediatr Rep. 2013;5(2):28-30. doi: 10.4081/pr.2013.e7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Yu YZ, Ming CY, Yue M, Li JH, Ling L. House–tree–person drawing therapy as an intervention for prisoners’ prerelease anxiety. Soc Behav Personal. 2016;44(6):987-1004. doi: 10.2224/sbp.2016.44.6.987 [DOI] [Google Scholar]
- 99.Rajendran N, Mitra TP, Shahrestani S, Coggins A. randomized controlled trial of adult therapeutic coloring for the management of significant anxiety in the emergency department. Acad Emerg Med. 2020;27(2):92-99. doi: 10.1111/acem.13838 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Data Extraction Form
eTable 1. Characteristics of the Included Studies, Including the Short ID, Title, a Brief Description of the Study Population, Intervention and Control Group
eTable 2. Ongoing or Recently Published Studies That Investigate the Effectiveness of AVAT
eFigure 1. Forest Plot of the Effects of AVAT for Studies Presenting Results as Change From Baseline
eFigure 2. Forest Plot of the Effects of AVAT for Studies Presenting Results as Post-test
eFigure 3. Funnel Plot for Change From Baseline Outcomes
eReferences
eTable. Detailed Description of Study Characteristics
Data Sharing Statement