Abstract
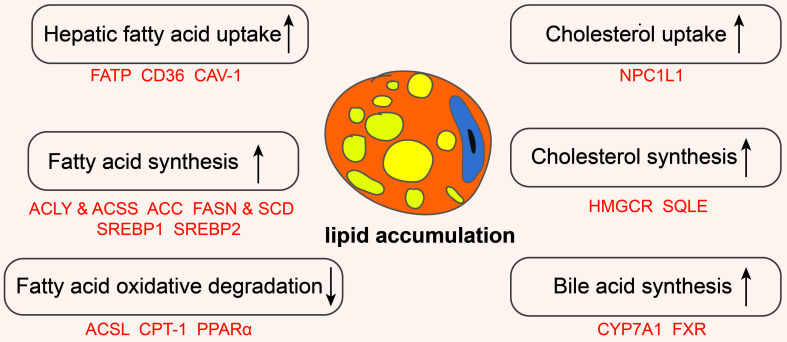
Metabolic dysfunction-associated steatotic liver disease (MASLD), formerly known as non-alcoholic fatty liver disease, has a high global prevalence and can progress to metabolic dysfunction-associated steatohepatitis, cirrhosis, and hepatocellular carcinoma. The pathogenesis of MASLD is primarily driven by disturbances in hepatic lipid metabolism, involving six key processes: increased hepatic fatty acid uptake, enhanced fatty acid synthesis, reduced oxidative degradation of fatty acids, increased cholesterol uptake, elevated cholesterol synthesis, and increased bile acid synthesis. Consequently, maintaining hepatic lipid metabolic homeostasis is essential for effective MASLD management. Numerous novel molecules and Chinese proprietary medicines have demonstrated promising therapeutic potential in treating MASLD, primarily by inhibiting lipid synthesis and promoting lipid oxidation. In this review, we summarized recent research on MASLD, elucidated the molecular mechanisms by which lipid metabolism disorders contribute to MASLD pathogenesis, and discussed various lipid metabolism-targeted therapeutic approaches for MASLD.
Keywords: MASLD, Lipid metabolism, Cholesterol metabolism, Lipogenesis, Lipolysis, lipid metabolism-targeted drugs, Chinese proprietary medicine
Graphical abstract
Introduction
Metabolic dysfunction-associated steatotic liver disease (MASLD) is a clinicopathological syndrome characterized by excessive fat deposition in hepatocytes that is not attributable to alcohol or other known liver-damaging factors. In 2023, non-alcoholic fatty liver disease was renamed MASLD following a Delphi consensus process. This renaming emphasizes the importance of metabolism in the disease and provides a more precise description. Consequently, we use the term MASLD instead of non-alcoholic fatty liver disease. MASLD is an acquired metabolic stress-associated liver injury closely related to insulin resistance and genetic susceptibility. It is one of the most common chronic diseases globally and a significant cause of liver injury in adults. The global prevalence of MASLD is approximately 29.8%.1 According to the National Health and Nutrition Examination Survey III, the prevalence of MASLD in the United States is 18.8%, rising to 28% in the overweight population.2 By 2018, the prevalence of MASLD in China had reached 32.9%, with the total population of MASLD in China expected to increase to 314.58 million people by 2030.3
The development of MASLD is closely linked to genetic alterations and environmental influences. The risk factors can be divided into genetic, epigenetic, and environmental factors.4 Genetic factors include mutations in genes such as I148M PNPLA3, TM6SF2, MBOAT7, and GCKR, which increase susceptibility to MASLD.5 Epigenetic factors include DNA methylation, chromatin remodeling, and non-coding RNAs. For instance, the M6A “writer” protein methyltransferase-like 3 ameliorates MASLD via RNA methylation.6 Additionally, replication protein A1 can maintain lipid metabolism homeostasis and thus ameliorate MASLD by regulating chromatin structure.7 Many non-coding RNAs involved in the regulation of lipid metabolism, such as miR-34a, miR-122, and miR-21, play a role in the development of MASLD.8 Furthermore, environmental factors play a critical role in the progression of MASLD. These include dietary habits, exercise status, and socioeconomic factors. Unhealthy dietary habits, such as high sugar and fat consumption,9 sedentary lifestyles, and infrequent exercise,10,11 increase susceptibility to MASLD.
MASLD can be classified as simple steatosis or metabolic dysfunction-associated steatohepatitis (MASH). MASH is characterized by pathological histological lobular inflammation and ballooning of hepatocytes attributable to MASLD. Prolonged liver injury can lead to cirrhosis and hepatocellular carcinoma (HCC). A common clinical method to diagnose MASLD is the detection of hepatic fat density on MRI.12 Additionally, plasma cytokeratin 18, a marker of hepatocyte apoptosis, has been widely used to assess MASLD.13 In recent years, mutations in the PNPLA3 and TM6SF2 genes have been shown to correlate with the severity of MASLD, highlighting their potential as new diagnostic markers. Furthermore, autophagy-related markers, oxidative stress-related markers, inflammatory factors, and liver fibrosis-related markers can also be used to assess the progression of MASLD.
Many treatments have been developed for MASLD. First, dietary control and appropriate exercise habits can significantly alleviate MASLD. Second, glucagon-like peptide-1 (GLP-1) agonists, sterol-regulatory element binding protein (SREBP) inhibitors, acetyl-CoA carboxylase (ACC) inhibitors, fatty acid synthase (FASN) inhibitors, stearoyl coenzyme A desaturase (SCD) inhibitors, farnesoid X receptor (FXR) agonists, peroxisome proliferator-activated receptor (PPAR) agonists, and certain natural compounds are considered promising treatments. In recent years, there has been tremendous growth in research focused on treating MASLD by modulating lipid metabolism, with an increasing number of drugs in clinical development. However, the treatment of MASLD remains challenging due to population selection issues and the side effects of current drugs. Given the crucial role of lipid metabolism in MASLD, exploring new drugs and targets for lipid metabolism modulation has become a popular direction for treatment research.
Lipid metabolism
Lipids serve as crucial energy sources in the body, and various molecules involved in lipid metabolism play integral roles in different cellular functions. The development of MASLD is closely related to lipid metabolism, particularly the metabolism of triglycerides and cholesterol. Triglycerides are synthesized from fatty acids. In this review, we primarily focus on fatty acid and cholesterol metabolism. The maintenance of hepatic lipid metabolic homeostasis involves three aspects: uptake, synthesis, and catabolism. It is widely believed that an increase in fatty acid uptake and synthesis or a decrease in lipid degradation leads to the development of MASLD. Therefore, researchers have increasingly focused on these aspects, and various viewpoints have been proposed.
Fatty acid metabolism
Fatty acid intake
The hepatic uptake of fatty acids depends on fatty acid transport carriers, including fatty acid transport proteins (FATPs), cluster of differentiation 36 (CD36), and hepatic caveolin-1 (CAV-1).
FATPs
Six FATP isoforms have been identified, with FATP2 and FATP5 primarily found in the liver.14 These transport proteins play crucial roles in the development of MASLD. Downregulation of FATP2 in mice reduces fatty acid uptake and ameliorates hepatic steatosis induced by a high-fat diet.15 Deletion of FATP2 in the mouse liver alters the metabolic landscape by increasing the expression of PPARα-regulated genes.16 Knockdown of FATP5 leads to reduced hepatic fatty acid uptake, which in turn decreases hepatic lipid accumulation.17 However, decreased hepatic FATP5 expression is associated with the histological progression of MASLD, which might be related to the reduction of hepatic lipid content as MASH advances to cirrhosis.18 Thus, FATP5 might have a dual role in the development of MASLD.
CD36
Experiments have confirmed the involvement of CD36 in hepatic fatty acid uptake and lipid accumulation.19 CD36 palmitoylation is an important factor in the pathogenesis of MASLD. In vitro and in vivo studies have demonstrated that inhibiting CD36 palmitoylation can ameliorate fatty acid metabolism disorders and reduce inflammatory reactions.20 Inhibition of CD36 palmitoylation also attenuates MASLD by promoting CD36 localization to hepatocyte mitochondria.21 The palmitoyltransferases DHHC4 and DHHC5 promote fatty acid uptake by targeting CD36.22 Several upstream factors regulating CD36 are also involved in MASLD. Demethylation of the PPARγ DNA promoter increases CD36 expression, leading to excessive lipid accumulation.23 Hepatic Dickkopf-1 enhances fatty acid uptake through the ERK–PPARγ–CD36 axis.24 Deletion of methyltransferase-like 3 in hepatocytes increases CD36 expression and hepatic free fatty acid uptake, promoting MASH development. Hypoxia-inducible factor 1α interacts with the CD36 promoter to increase CD36 expression and enhance fatty acid uptake.25 Additionally, non-coding RNAs such as miR-96-5p,26 miR-100,27 miR-26a,28 and miR-195/miR466829 regulate CD36 expression and affect the development of MASLD.
CAV-1
The role of CAV-1 in the development of MASLD remains controversial due to its role in mediating lipid endocytosis. Although some studies have detected increased CAV-1 expression in the liver tissue of mice with MASLD-fed high-fat diets, others have found a significant reduction in its expression in mice with MASLD.30 Knockdown of CAV-1 in LO2 and AML12 cells resulted in increased steatosis.31 CAV-1 upregulation has been found to attenuate lipid accumulation and promote autophagy in mice with MASLD.32 Interestingly, hepatocyte-specific CAV-1 knockdown significantly altered the gene profile in the development of MASLD without affecting hepatic steatosis and fibrosis.33
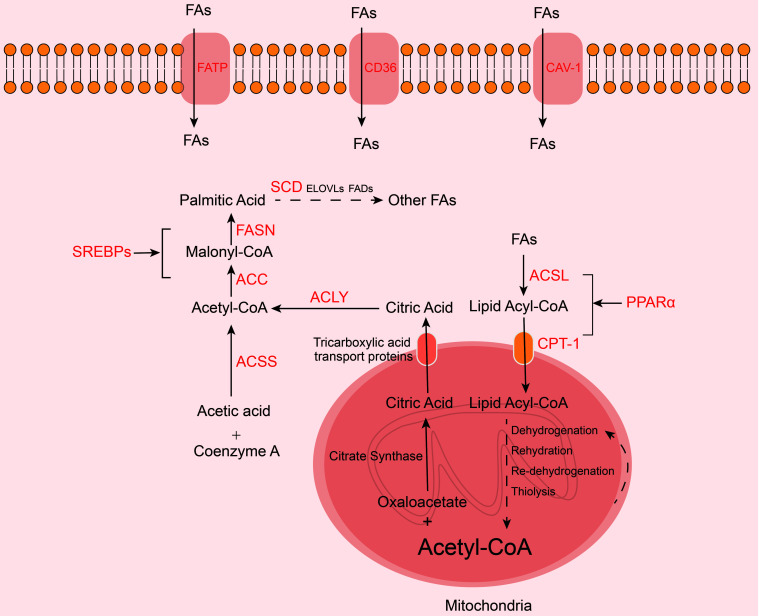
De novo fatty acid synthesis
De novo fatty acid synthesis is a process by which the body converts carbon from carbohydrates, such as glucose, and amino acids, including glutamine, into fatty acids. The raw material for de novo fatty acid synthesis is acetyl-CoA, which is derived from two sources. First, acetyl-CoA in mitochondria is condensed with oxaloacetate, catalyzed by citrate synthase, to form citric acid, which is then transported to the cytosol by tricarboxylic acid transport proteins in the mitochondrial membrane. Citric acid is subsequently modified by ATP citrate lyase (ACLY) to regenerate acetyl-CoA, which is used for fatty acid synthesis. This process is called the citrate shuttle. Second, acetic acid is linked to coenzyme A to synthesize acetyl-CoA, providing additional raw material for fatty acid synthesis, catalyzed by acetyl-CoA synthetase (ACSS). The generated acetyl-CoA is initially converted to malonyl coenzyme A by ACC, the key rate-limiting step. Malonyl coenzyme A is then converted to palmitic acid via FASN. Saturated palmitic acid (FA16:0) can undergo C-chain extension and desaturation by SCD to produce other fatty acid species. These fatty acids can be used to generate more complex lipids. The key enzymes involved in de novo fatty acid synthesis play important roles in the development of MASLD (Fig. 1).
Fig. 1. Fatty acid metabolism. Fatty acid uptake by the liver depends on fatty acid transport carriers, including FATP, CD36, and CAV-1.
The raw material for de novo fatty acid synthesis is acetyl-CoA, which can be obtained via the citrate shuttle pathway or from acetic acid. ACC and FASN catalyze the conversion of acetyl-CoA into saturated palmitic acid, which can be further modified into other fatty acids by enzymes such as SCD. De novo fatty acid synthesis is promoted by SREBPs. Conversely, the β-oxidation of fatty acids occurs in the mitochondria. Fatty acids are converted into fatty acyl-CoA by ACSL and transported via CPT-1 before being oxidized to acetyl-CoA. Fatty acid β-oxidation is promoted by PPARα. FAs, fatty acids; FASN, fatty acid synthase; SREBP, sterol-regulatory element binding protein; FASN, fatty acid synthase; ACC, acetyl-CoA carboxylase; ACLY, ATP citrate lyase; ACSS, acetyl-CoA synthetase; ACSL, acyl-CoA synthetase; PPAR, peroxisome proliferator-activated receptor; CPT-1, carnitine palmitoyltransferase-1.
SREBPs play critical roles in the development of MASLD by transcriptionally regulating key genes involved in hepatic lipid metabolism. SREBPs are divided into SREBP1 and SREBP2. SREBP1 has two transcripts, SREBP1a and SREBP1c, with SREBP1c being more widely expressed. SREBP1a is expressed in the intestinal epithelium, heart, and macrophages, while SREBP2 is primarily expressed in hepatic and adipose tissue. SREBPs can form trimers with SREBP cleavage-activating protein (SCAP) and INSIG, anchoring the protein in the endoplasmic reticulum (ER). The C-terminal region of SCAP interacts with the C-terminal structural domain of the ER, while the N-terminal region of SCAP contains a sterol-sensing domain sensitive to cholesterol levels. When cholesterol levels are high, SCAP binds with cholesterol and INSIG, resulting in the retention of the entire complex in the ER. Conversely, when cholesterol levels decrease, SCAP does not interact with INSIG, allowing the SREBP–SCAP complex to be internalized into COPII-containing vesicles, which are transported to the Golgi apparatus. Within the Golgi, SREBPs are sequentially cleaved by site-1 protease and site-2 protease, releasing their N-terminal bHLH structural domain into the cytoplasm, where it acts as a transcription factor. The bHLH structural domain migrates to the nucleus, dimerizes, and forms a complex with transcriptional co-activators, activating the transcription of genes with SRE motifs. SREBP1 mainly regulates fatty acid synthesis and LDLR expression, while SREBP2 primarily regulates the expression of cholesterol biosynthetic genes.
ACLY and ACSS
Inhibiting ACLY can reduce hepatic lipid accumulation by suppressing de novo fatty acid synthesis. Recent research has clarified the involvement of ACLY in MASLD. In steatotic cells, ACLY mRNA is efficiently translated in a cap-independent manner, promoting adipogenesis.34 The sirtuin 2–ACLY axis is also involved in MASLD progression, with sirtuin 2 inhibiting ACLY and lipid accumulation.35 Additionally, ACLY is degraded by HMG-CoA reductase degradation protein via ubiquitination, thereby attenuating MASLD.36 ACSS is involved in the synthesis of acetyl-CoA, which promotes hepatic steatosis. Silencing ACSS2 can effectively inhibit the conversion of fructose to acetyl-CoA and fatty acids in mice.37
ACC
ACC, a key enzyme in de novo fatty acid synthesis, plays a significant role in MASLD development. Liver-specific ACC1 knockdown reduces hepatic lipid accumulation and impairs hepatocyte de novo fatty acid synthesis in mice.38 AMPK activates the phosphorylation of ACC1 (Ser79Ala) and ACC2 (Ser212Ala), inhibiting the enzymatic activity of ACC and thereby suppressing lipid synthesis. Mutations at these sites are associated with increased de novo fatty acid synthesis and steatosis in the liver.39
FASN and SCD
FASN and SCD are markers of lipid synthesis and are both upregulated in MASLD. FASN regulation plays an important role in MASLD. Sorting nexin 8 can prevent MASLD by promoting FASN degradation, making the sorting nexin 8–FASN axis a promising target for MASLD prevention and treatment.40 miR-103 can also inhibit hepatic steatosis by targeting FASN and SCD1, which can attenuate MASLD.41 Slug binds to the FSAN promoter, while Slug-associated LSD1 catalyzes H3K9 demethylation, stimulating FASN expression and lipogenesis.42 Furthermore, in MASLD, the levels of mitochondrial pyruvate carrier 1 are positively correlated with hepatic lipid deposition, and mitochondrial pyruvate carrier 1 knockdown affects FASN lactylation at K673, ultimately inhibiting FASN activity.43
SREBP1
SREBP1c induces the expression of ACC, FASN, and SCD, promoting hepatic fatty acid and triglyceride synthesis. Increased SREBP1 expression is observed in patients with MASLD, and SREBP1c overexpression in mice increases hepatic triglyceride levels.44 However, exercise and strength training can reduce hepatic lipid accumulation by downregulating SREBP1.45,46 Activated AMPK phosphorylates SREBPs, reducing their activity and inhibiting hepatic lipid accumulation. VEGFB,47 MD2,48 and protectin DX49 are involved in MASLD development through the AMPK–SREBP1 pathway. mTOR promotes the maturation and nucleation of SREBP1, enhancing lipid synthesis.50 Pancreatic progenitor cell differentiation and proliferation factor reduces hepatic steatosis by inhibiting mTOR/SPRBP1.51 CD36 promotes de novo lipogenesis through INSIG2-dependent SREBP1 hydrolytic processing.52 Additionally, non-coding RNAs including miR-23a/b-3p,53 miR-33-5p,54 and miR-130b-5p55 regulate SREBP1 expression. ZBTB7A,56 ceramide synthase,57 and dihydroxytryptamine58 are believed to upregulate SREBP1, promoting lipid synthesis. Interestingly, although SREBP1a does not contribute to hepatic lipogenesis, its absence in hepatocytes or macrophages exacerbates methionine- and choline-deficient diet-induced MASLD.59
SREBP2
The high-fat, choline-deficient, amino acid-defined diet model is a newly established mouse model of MASH that activates the SREBP2/SCD2 gene and drives liver fibrosis through high-fat feeding.60 The expression of SCD, FASN, and SREBP2 is increased in rats fed a Western diet.61 Moreover, SREBP2 is regulated by the AMPK signaling pathway, and increased expression of SREBP2 alleviates autophagic dysfunction in MASLD.62
Fatty acid β-oxidation
Fatty acid oxidation refers to the process by which fatty acids are degraded in the presence of oxygen to release energy for various biological processes. The most common pathway is the β-oxidation of fatty acids. β-oxidation of long-chain fatty acids occurs in the mitochondria, whereas very-long-chain fatty acids are oxidized in peroxisomes. Mitochondrial β-oxidation consists of three steps. First, fatty acids are activated to fatty acyl-CoA, a reaction catalyzed by acyl-CoA synthetase (ACSL). Second, while the enzyme system catalyzing fatty acid β-oxidation is located in the mitochondrial matrix, long-chain fatty acyl-CoA requires a carrier, namely carnitine palmitoyltransferase-1 (CPT-1), to be transported through the inner mitochondrial membrane. Finally, the β-oxidation of fatty acyl-CoA in the mitochondrial matrix proceeds through a four-step reaction involving dehydrogenation, hydration, re-dehydrogenation, and thiolysis, ultimately producing one molecule of acetyl-CoA and a new molecule of fatty acyl-CoA with two fewer carbons. This cycle repeats several times to gradually produce more acetyl-CoA. Peroxisomal β-oxidation is similar to mitochondrial β-oxidation, but the first step is catalyzed by lipid acyl-CoA oxidase (Fig. 1).
The PPAR system, particularly PPARα, plays an important role in the regulation of lipid metabolism. Activated PPARs form heterodimers with the retinoid X receptor and bind to peroxisome proliferator-responsive elements upstream of certain genes to activate enzymes related to lipid metabolism. PPARα has various roles in lipid metabolism, including promoting fatty acid β-oxidation and inhibiting MASLD development.
ACSL
TANK-binding kinase 1 acts as a scaffolding protein to localize ACSL1 to mitochondria and promote fatty acid oxidation.63 Although ACSL4 is weakly expressed in the liver, it is upregulated in patients with MASLD, which contradicts the conventional belief that ACSL4 promotes fatty acid β-oxidation and inhibits MASLD.64 This might be attributable to ACSL4’s ability to promote inflammation65 and its involvement in ferroptosis.66 Additionally, P115 interacts with ACSL4 and degrades it. P115 is significantly upregulated in the livers of high-fat diet-fed mice, resulting in the downregulation of ACSL4 protein.67 ACSL5 knockdown in mice increases energy expenditure and insulin sensitivity and delays fat absorption.68
CPT-1
Exercise can lead to CPT-1 downregulation, thereby reducing the disruption of lipid metabolism in MASLD.69,70
PPARα
Metabolomic and lipidomic screening revealed that PPARα plays an important role in the progression of MASH to HCC.71 In a mouse model, obese female offspring fed a high-fat diet exhibited impaired hepatic PPARα activation.72 Moreover, PPARα is sex-selective, making male mice more susceptible to MASLD.73 Mechanistically, PPARα can reduce hepatic steatosis by rebuilding the intestinal barrier and regulating the distribution of the intestinal flora.74 Intestinal PPARα in mice with MASLD can promote MASH progression by regulating fatty acid uptake.75 Several molecules can also affect MASLD by influencing PPARα. For example, the anti-adipogenic factor coenzyme Q10 regulates MASLD by upregulating PPARα and CPT-1.76 Programmed cell death 4,77 obesity-associated protein,78 and mothers against decapentaplegic homolog family member 479 promote hepatocyte lipid deposition by inhibiting PPARα-mediated fatty acid oxidation.
Cholesterol metabolism
Cholesterol uptake
The uptake of dietary cholesterol by intestinal epithelial cells is facilitated by Niemann–Pick type C1-like 1 (NPC1L1). The accumulated cholesterol is then esterified by cholesterol acyltransferases, also known as sterol O-acyltransferases, for hepatic uptake.80
NPC1L1
Expression of the human NPC1L1 gene in the mouse liver exacerbates high-fat diet-induced steatosis.81,82
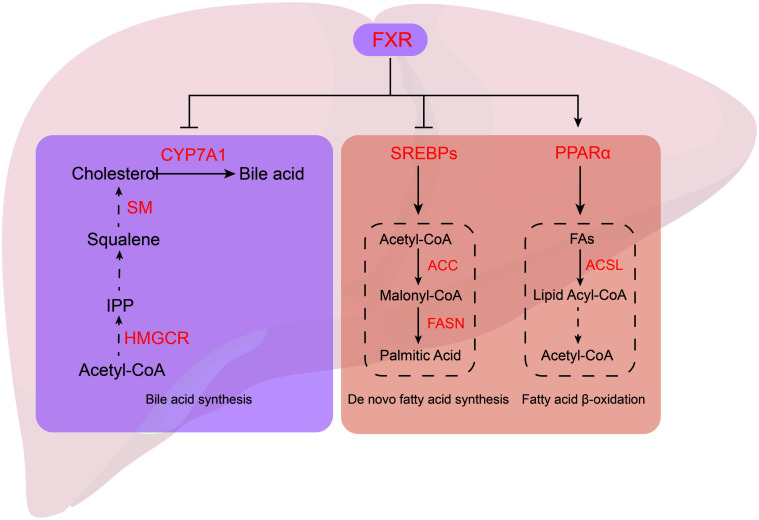
Cholesterol synthesis
Cholesterol synthesis originates from acetyl-CoA through a complex process involving nearly 30 enzymatic steps. This process can be roughly divided into three stages: synthesis of isopentenyl pyrophosphate from acetyl-CoA, synthesis of squalene, and conversion of squalene to cholesterol (Fig. 2). The key enzymes involved in this process are mammalian 3-hydroxy-3-methylglutaryl (HMG)-CoA reductase (HMGCR/HMFR) and squalene monooxygenase (SM/SQLE). HMGCR catalyzes the conversion of HMG-CoA to mevalonate in the first phase, while squalene is oxidized by SM in the third stage to produce 2,3-oxidized squalene, a precursor of cholesterol and sterols.
Fig. 2. Cholesterol metabolism.
The process of cholesterol synthesis is complex and can be roughly divided into three stages: synthesis of IPP from acetyl-CoA, synthesis of squalene, and conversion of squalene to cholesterol. HMGCR and SM are the key enzymes in cholesterol synthesis. The primary route of cholesterol production is bile acid synthesis catalyzed by CTP7A1. FXR is an important regulator of cholesterol metabolism; Its activation inhibits CTP7A1, leading to the inhibition of bile acid synthesis. FXR, farnesoid X receptor; CYP7A1, cholesterol 7α-hydroxylase; SM, squalene monooxygenase; HMGCR, 3-hydroxy-3-methylglutaryl (HMG)-CoA reductase; IPP, isopentenyl pyrophosphate; SREBP, sterol-regulatory element binding protein; PPAR, peroxisome proliferator-activated receptor; FAs, fatty acids; ACC, acetyl-CoA carboxylase; FASN, fatty acid synthase; ACLY, ATP citrate lyase.
HMGCR
Dysregulated cholesterol metabolism can exacerbate MASLD. The development of MASLD is associated with increased HMGCR expression and reduced HMGCR phosphorylation.83 A genomic analysis of a high-fat-fed mouse model of MASLD showed a 2.06-fold upregulation of HMGCR.84 HMGCR is regulated by Dicer1/miR-29, indicating that the Dicer1–miR-29–HMGCR axis is involved in free cholesterol accumulation in the livers of mice with MASLD.85
SM/SQLE
SM/SQLE is implicated in the progression of MASLD to HCC. It is the most significantly overexpressed metabolic gene in patients with MASLD and HCC, and its expression accelerates the development of HCC induced by a high-fat, high-cholesterol diet in mice.86–88 The underlying mechanisms include the promotion of MASH and HCC development through the induction of cholesterol biosynthesis, the SQLE–CA3 axis-mediated lipogenesis,88 and P53-mediated transcriptional regulation of SQLE to suppress cholesterol synthesis and tumor growth.89
Bile acid synthesis
Bile-acid synthesis is the primary pathway for cholesterol catabolism, and the key enzyme in this process is cholesterol 7α-hydroxylase (CYP7A1). Patients with MASLD often exhibit disordered bile acid metabolism. Hepatic bile acid synthesis is mainly regulated by FXR, and FXR activation inhibits de novo bile acid synthesis (Fig. 2).
CYP7A1
Bioinformatic analysis has revealed that CYP7A1 is involved in the development of MASLD, MASH, and HCC.90,91 In MASLD, CYP7A1 mRNA expression is increased.92 However, CYP7A1 mRNA levels decline with the progression of MASH-associated liver fibrosis.93
FXR
FXR plays a crucial role in the development of MASLD. On one hand, FXR activation promotes the production of short heterodimer partner, which downregulates the rate-limiting enzyme CYP7A1, ultimately inhibiting bile acid synthesis. Studies have demonstrated that FXR activation can prevent MASLD by reducing lipid uptake in a bile acid-dependent manner.94 On the other hand, FXR activation decreases hepatic lipid accumulation by inhibiting triglyceride synthesis, achieved through the induction of short heterodimer partner expression and the downregulation of SREBP1 and FASN.
FXR deficiency in mice results in hepatic steatosis, lipid droplet accumulation in hepatocytes, disturbed glucose metabolism, and elevated blood lipid levels.95 FXR functions as a nuclear transcription factor that regulates glucose and lipid metabolic homeostasis through pyruvate dehydrogenase kinase 4.95 Furthermore, FXR sulfation, a post-translational modification influenced by endogenous hepatic cystathionine γ lyase/hydrogen sulfide, promotes FXR activity, thereby improving MASLD.96 MiR-552-3p ameliorates hepatic lipid metabolism disorders by regulating the transcriptional activity of FXR.97
Drugs that treat MASLD by regulating lipid metabolism
The FDA has approved Rezdiffra (resmetirom), a thyroid hormone receptor β-1 agonist, as the first treatment for MASH. Resmetirom selectively activates thyroid hormone receptor β-1, resulting in a reduction of free thyroxine (T4) levels by approximately 16–19%. Notably, it does not influence the levels of thyrotropin or free triiodothyronine.98 Resmetirom also significantly reduces cholesterol and triglyceride levels and enhances fatty acid oxidation, demonstrating substantial potential for the treatment of MASLD. Meanwhile, there has been increasing interest in developing new drugs for MASLD treatment. In this section, we review recent articles exploring molecular drugs and Chinese proprietary medicines (CPMs) that inhibit MASLD. Most of these drugs/CPMs work by inhibiting fatty acid uptake and synthesis while promoting fatty acid oxidation. Similarly, the inhibition of cholesterol uptake and synthesis, as well as bile acid synthesis, can also be used to improve MASLD. CPMs have shown great potential in MASLD treatment. The modification of inhibitors and activators targeting key regulatory genes, such as GLP-1, SREBP, ACC, FASN, SCD1, PPARα, and FXR, has gained increasing attention in recent years. Improving the therapeutic efficacy of drugs and reducing their potential side effects have become major research goals in this field.
GLP-1 agonists
GLP-1 regulates insulin and glucagon secretion and modulates intestinal motility, and its agonists have been considered promising therapeutics in recent years for reducing the risk of MASLD and its associated mortality.99 GLP-1 agonists, such as semaglutide and liraglutide, effectively treat MASLD by reducing visceral and hepatic fat content.100–102 Semaglutide improves the health-related quality of life in patients with MASLD,103 with daily dosing proving more effective.104 Mechanistically, semaglutide induces modifications in the gut microbiota and ameliorates MASLD.105 Dual GLP-1/GLP-2 receptor agonists,106 as well as dual GLP-1 receptor/glucagon receptor agonists like ALT-801, NN1177, and efinopegdutide,107–109 have shown good therapeutic efficacy in MASLD. The combination of GLP-1 activators with other drugs is also the focus of an increasing number of studies. Combined treatment with semaglutide and the FXR agonist cilofexor, the ACC inhibitor firsocostat, and the ACLY inhibitor has demonstrated better therapeutic efficacy than monotherapy.110,111 Novel GLP-1 activators, such as cinchonine and exendin-4, are also under development.112,113
The findings of clinical trials on GLP-1 agonists are listed in Table 1.103,107,114-122 “\” indicates that no phasing information for the clinical trial could be found.
Table 1. Clinical trials of GLP-1 agonists.
| Drugs | Conclusions | Phase | References |
|---|---|---|---|
| Dulaglutide | Improvement in patients with type 2 diabetes and MASLD | \ | 114 |
| Efinopegdutide | Improvement of MASH and MASLD | Phase II | 107 |
| Exenatide | Improvement in patients with type 2 diabetes and MASLD | \ | 115 |
| Liraglutide | Improvement of MASH and MASLD | Phase II/III | 116–118 |
| Improvement in patients with type 2 diabetes and MASLD | Phase IV | 119 | |
| No improvement in patients with type 2 diabetes and MASLD | Phase IV | 120 | |
| Semaglutide | Improvement of MASH but not liver fibrosis | Phase I/II | 121,122 |
| Improvement of health-related quality of life in patients with MASH and liver fibrosis | Phase II | 103 |
MASLD, metabolic dysfunction-associated steatotic liver disease; MASH, metabolic dysfunction-associated steatohepatitis.
SREBP inhibitors
Betulin is a specific inhibitor of SREBP maturation. It inhibits the transport of SREBP to the Golgi via SCAP,52 thereby inhibiting the processes of fatty acid and cholesterol synthesis. Betulin has shown potential in the treatment of MASLD.123–126 PF-429242 is a specific inhibitor of the proteasome site-1 protease, which inhibits the cleavage and release of the SREBP precursor protein. It is also considered to have potential in MASLD control.127
ACC inhibitors
ACC inhibition reduces lipid accumulation in hepatocytes and inhibits pro-fibrosis activity in liver stem cells, suggesting that small-molecule inhibitors of ACC can attenuate liver fibrosis by reducing hepatocyte lipotoxicity and preventing liver stem cell activation. These findings provide a mechanistic basis for the treatment of patients with MASH and advanced liver fibrosis.128 However, while ACC inhibitors have been found to reverse MASLD, they may also promote hypertriglyceridemia.129 GS-0976 (Firsocostat) has shown promise in alleviating MASH in Phase II clinical trials.130,131 However, firsocostat can cause hyperlipidemia, which can be alleviated by fenofibrate.132,133 The ACC inhibitor ND-654, which mimics the action of ACC phosphorylation, inhibits hepatic de novo fatty acid synthesis.39 In mouse models, treatment with selective ACC1 inhibitors significantly ameliorated hepatic steatosis and liver fibrosis, supporting their use as new therapies for MASLD/MASH.134 Additionally, both the dual ACC1/ACC2 inhibitor PF-05221304135 and the novel ACC1/ACC2 inhibitor WZ66136 have been shown to alleviate MASH in mouse models.
FASN or SCD1 inhibitors
In patients with MASLD, FASN inhibitors such as TVB-2640 (Denifanstat)137 and FT-4101138 reduce hepatic de novo lipogenesis and steatosis. FASstatin may be useful in treating MASLD by targeting and degrading FASN.139 Both the SCD1 inhibitor CAY10566 and a novel SCD1 inhibitor have inhibited hepatic lipid accumulation in mice, suggesting that SCD1 may be an effective target for the treatment of MASLD.140,141
PPAR agonists
Fibrates are clinically available PPARα agonists for MASLD treatment. The literature indicates that PPARα-mediated peroxisome adaptation is crucial for fenofibrate-mediated improvements in MASLD.142 Combining PPARα with other dual-receptor agonists has shown great potential in MASLD treatment. The novel PPARα/γ agonists G4 and G5 effectively inhibited hepatic steatosis while avoiding the side effects of pioglitazone.143 The PPARα/γ agonist aleglitazar significantly reduced hepatic steatosis and fibrosis.144 The PPARα/δ agonist compound H11, which exhibits effective and balanced PPARα/δ agonist activity, has shown promise in MASH treatment.145 Additionally, ZLY18, a quadruple free fatty acid receptor 1 and PPARα/γ/δ agonist, might be a highly effective anti-MASLD drug.146
The findings of the clinical trials on PPAR agonists are listed in Table 2.144,147–150 “\” indicates that no phasing information for the clinical trial could be found.
Table 2. Clinical trials of PPAR agonists.
| Drugs | Targets | Conclusions | Phase | References |
|---|---|---|---|---|
| Aleglitazar | PPARα/γ | Improvement of MASLD and liver fibrosis | \ | 144 |
| Elafibranor | PPARα/δ | Improvement of MASH | Phase II | 147 |
| Lanifibranor | Pan-PPAR | Improvement of MASH and liver fibrosis | Phase III | 148 |
| Saroglitazar | PPARα/γ | Improvement of MASH and MASLD | Phase II | 149,150 |
PPAR, peroxisome proliferator-activated receptor; MASLD, metabolic dysfunction-associated steatotic liver disease; MASH, metabolic dysfunction-associated steatohepatitis.
FXR agonists
Although traditional FXR agonists have been used in the clinic, their side effects have limited their application to some extent. The traditional FXR agonist, obeticholic acid, has been abandoned for MASLD treatment. New FXR agonists, such as nidufexor (LMB763),151 cilofexor,152 and EDP-305,153 have entered clinical trials for the treatment of MASLD or MASH. In recent years, the development of FXR agonists with stronger activity and fewer side effects has received increasing attention. For instance, 1-adamantylcarbonyl-4-phenylpiperazine is an FXR agonist, and its derivative compound 10A was found to be more effective in ameliorating hyperlipidemia, hepatic steatosis, and insulin resistance.154 Additionally, structural optimization of non-bile acid FXR agonists led to the development of compound 42 as an FXR agonist with high efficiency and selectivity for alleviating MASH.155 MET409, an FXR agonist with a unique chemical structure, significantly suppressed hepatic fat content without causing significant or severe side effects in patients with MASH.156 Moreover, tissue-selective FXR agonists have been studied. For example, (E)-3-(3-((2-cyano-4′-dimethylaminobiphenyl-4-ylmethyl)cyclohexanecarbonylamino)-5-fluorophenyl) acrylic acid methyl ester is an entero-selective FXR partial agonist that significantly reduced the extent of liver fibrosis and decreased the levels of fibrosis markers and serum AST.157 BMS-986339 exhibited potent FXR activation and anti-fibrotic efficacy despite its tissue selectivity, reducing the activation of certain genes in the liver.158
The findings of the clinical trials on FXR agonists are listed in Table 3.152,156,159–162
Table 3. Clinical trials of FXR agonists.
| Drugs | Conclusions | Phase | References |
|---|---|---|---|
| Cilofexor | Improvement of MASH | Phase II | 152,159 |
| MET409 | Improvement of MASH | Phase I | 156 |
| Obeticholic acid | Improvement in patients with type 2 diabetes and MASH | Phase II | 160 |
| Tropifexor | Improvement of MASH | Phase II | 161 |
| Vonafexor | Improvement of liver and kidney function in patients with MASH and liver fibrosis | Phase II | 162 |
MASH, metabolic dysfunction-associated steatohepatitis.
Natural compounds
Many natural compounds, including CPMs, are considered promising in the treatment of MASLD. Recent studies on natural compounds and their molecular mechanisms are listed in Table 4.163–187 However, the use of many CPMs for the treatment of MASLD still needs to be tested in rigorous clinical trials. Nevertheless, CPMs remain a valuable resource in modern medicine and have significant potential for the future treatment of MASLD.
Table 4. Drugs that treat MASLD by regulating lipid metabolism.
| Drugs | Mechanism | References |
|---|---|---|
| Andrographolide | Inhibits FATP2 | 163 |
| Baicalein | Inhibits fatty acid synthesis; promotes fatty acid oxidation; activates AMPK; inhibits SREBP1 | 164,165 |
| Berberine/oxyberberine | Inhibits fatty acid synthesis; promotes fatty acid oxidation; regulates SIRT3/AMPK/ACC; downregulates SIRT1/FoxO1/SREBP2; inhibits cholesterol synthesis | 166–170 |
| Curcumin | Inhibits CD36, SLC13A5, and ACLY; regulates CYP2E1, SREBP1c, and PPARα | 171–173 |
| Extract of Dillenia indica L. | Regulates SIRT1/pLKB1/AMPK, HMGCR, and PPARα signaling pathways | 174 |
| Extract of Liriope platyphylla | Inhibits fatty acid uptake and synthesis | 175 |
| Extract of root from Arctium lappa L. | Activates AMPK/ACC/CPT1 | 176 |
| Jian Pi Qing Gan Yin decoction | Activates AMPK/PPARα; inhibits LXRα/SREBP1/NF-κB | 177 |
| Kangtaizhi Granule | Regulates PPARγ, SREBP1, pAKT, FAS, and SIRT1 | 178 |
| Limonin | AMPK agonist; downregulates FASN and SREBP1 | 179,180 |
| Naringenin | Activates the CaMKKβ/AMPK/ACC pathway | 181 |
| Paeoniflorin | Activates LKB1/AMPK and PPARα | 182,183 |
| Puerarin | Inhibits fatty acid uptake and synthesis; promotes fatty acid oxidation; inhibits FASN, SREBP1c; activates AMPK | 184,185 |
| Saikosaponin | Inhibits SREBP1c; activates PPARα; inhibits FASN; promotes ACOX1 and CPT1 | 186,187 |
FATP, fatty acid transport protein; AMPK, AMP-activated protein kinase; SREBP, sterol regulatory element-binding protein; ACC, acetyl-CoA carboxylase; ACLY, ATP citrate lyase; PPAR, peroxisome proliferator-activated receptor; HMGCR, 3-hydroxy-3-methylglutaryl (HMG)-CoA reductase; CPT1, carnitine palmitoyltransferase-1; FASN, fatty acid synthase.
Discussion
MASLD represents a continuum of liver diseases that includes simple steatosis and metabolic dysfunction-associated steatohepatitis. The global prevalence of MASLD is estimated to be as high as 29.8%, making it one of the most significant diseases. Most patients with MASLD are asymptomatic and only present with incidental findings of hepatomegaly or slight-to-moderate increases in ALT and AST levels during routine physical examinations. The current primary approach for treating MASLD is reducing hepatic steatosis by regulating lipid metabolism. Dietary control and appropriate exercise can significantly improve the symptoms of MASLD. Additionally, drugs such as FXR agonists, PPARα agonists, and SREBP1 inhibitors have been explored for MASLD treatment because of their ability to regulate lipid metabolism.
The pathology of MASLD is characterized by hepatic steatosis, the development of which is mainly related to dysregulated hepatic lipid metabolism. The development of MASLD is generally attributed to six factors: increased hepatic fatty acid uptake and synthesis, decreased fat oxidation, increased cholesterol uptake and synthesis, and increased bile acid synthesis. (1) Regarding increased fatty acid uptake, FATP and CD36 are upregulated in MASLD. Although CAV-1 is involved in fat uptake, its role in MASLD remains controversial. (2) Concerning increased de novo lipogenesis, ACLY, ACSS, ACC, FASN, and SCD, key enzymes involved in de novo fatty acid synthesis, are upregulated in MASLD. Among them, SREBP1 can sense cholesterol levels and affect MASLD by transcriptionally regulating key genes involved in hepatic lipid metabolism. SREBP1 induces ACC, FASN, SCD, and other lipid synthesis genes to promote hepatic fatty acid and triglyceride synthesis. SREBP1 has been considered to have great potential as a treatment target for MASLD. (3) Inhibition of fatty acid oxidation can also lead to MASLD. Inhibition of ACSL and CPT-1, key enzymes in lipolysis, can exacerbate hepatic steatosis. Fatty acid oxidation can be regulated by PPARα, and PPARα activation promotes CPT1 expression, thereby enhancing fatty acid β-oxidation. Dysregulated cholesterol metabolism is also involved in the development of MASLD. (4) Increased cholesterol uptake can exacerbate MASLD through increased NPC1L1 expression. (5) Regarding increased cholesterol synthesis, HMGCR, a key enzyme for cholesterol synthesis, is upregulated in MASLD. SM has also been found to play an important role in the progression of MASLD to HCC. (6) Finally, increased bile acid synthesis is involved in the development of MASLD. CYP7A1, a key enzyme involved in bile acid synthesis, has elevated expression in MASLD. Hepatic bile acid synthesis is mainly regulated by FXR, and FXR activation inhibits de novo bile acid synthesis, thereby ameliorating MASLD.
Conclusions
Although much research has investigated the mechanisms of MASLD development, some unanswered questions remain. Peroxisomes are involved in the β-oxidation of extra-long-chain fatty acids, but little research has assessed the connection between peroxisomes and MASLD. Current models of MASLD are mainly based on oleic acid-induced cells and high-fat diet-fed mice, which do not fully capture the dynamic process of MASH fibrosis that can progress to cirrhosis and HCC. Thus, the need for novel, low-cost, and rapid MASLD models for life science research is evident. Despite numerous new drugs, including molecule drugs and CPMs, entering clinical trials in recent years, the treatment of MASLD remains ineffective given the large MASLD population. Lipid metabolism, as an important mechanism in the development of MASLD, has been the primary focus of MASLD treatment. Therefore, the exploration of new drugs and targets that regulate lipid metabolism for MASLD treatment is an area that requires in-depth research.
References
- 1.Le MH, Yeo YH, Li X, Li J, Zou B, Wu Y, et al. 2019 global nafld prevalence: A systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2022;20(12):2809–2817.e2828. doi: 10.1016/j.cgh.2021.12.002. [DOI] [PubMed] [Google Scholar]
- 2.Younossi ZM, Stepanova M, Negro F, Hallaji S, Younossi Y, Lam B, et al. Nonalcoholic fatty liver disease in lean individuals in the united states. Medicine (Baltimore) 2012;91(6):319–327. doi: 10.1097/MD.0b013e3182779d49. [DOI] [PubMed] [Google Scholar]
- 3.Zhou J, Zhou F, Wang W, Zhang XJ, Ji YX, Zhang P, et al. Epidemiological features of nafld from 1999 to 2018 in china. Hepatology. 2020;71(5):1851–1864. doi: 10.1002/hep.31150. [DOI] [PubMed] [Google Scholar]
- 4.Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 5.Eslam M, Valenti L, Romeo S. Genetics and epigenetics of nafld and nash: Clinical impact. J Hepatol. 2018;68(2):268–279. doi: 10.1016/j.jhep.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 6.Qin Y, Li B, Arumugam S, Lu Q, Mankash SM, Li J, et al. M(6)a mrna methylation-directed myeloid cell activation controls progression of nafld and obesity. Cell Rep. 2021;37(6):109968. doi: 10.1016/j.celrep.2021.109968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yin Q, Li Y, Zhou Z, Li X, Li M, Liu C, et al. Rpa1 controls chromatin architecture and maintains lipid metabolic homeostasis. Cell Rep. 2022;40(2):111071. doi: 10.1016/j.celrep.2022.111071. [DOI] [PubMed] [Google Scholar]
- 8.Hochreuter MY, Dall M, Treebak JT, Barrès R. Micrornas in non-alcoholic fatty liver disease: Progress and perspectives. Mol Metab. 2022;65:101581. doi: 10.1016/j.molmet.2022.101581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leslie T, Pawloski L, Kallman-Price J, Escheik C, Hossain N, Fang Y, et al. Survey of health status, nutrition and geography of food selection of chronic liver disease patients. Ann Hepatol. 2014;13(5):533–540. [PubMed] [Google Scholar]
- 10.Gerber L, Otgonsuren M, Mishra A, Escheik C, Birerdinc A, Stepanova M, et al. Non-alcoholic fatty liver disease (nafld) is associated with low level of physical activity: A population-based study. Aliment Pharmacol Ther. 2012;36(8):772–781. doi: 10.1111/apt.12038. [DOI] [PubMed] [Google Scholar]
- 11.Patel AH, Peddu D, Amin S, Elsaid MI, Minacapelli CD, Chandler TM, et al. Nonalcoholic Fatty Liver Disease in Lean/Nonobese and Obese Individuals: A Comprehensive Review on Prevalence, Pathogenesis, Clinical Outcomes, and Treatment. J Clin Transl Hepatol. 2023;11(2):502–515. doi: 10.14218/JCTH.2022.00204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wong VW, Adams LA, de Lédinghen V, Wong GL, Sookoian S. Noninvasive biomarkers in nafld and nash - current progress and future promise. Nat Rev Gastroenterol Hepatol. 2018;15(8):461–478. doi: 10.1038/s41575-018-0014-9. [DOI] [PubMed] [Google Scholar]
- 13.Noureddin M, Lam J, Peterson MR, Middleton M, Hamilton G, Le TA, et al. Utility of magnetic resonance imaging versus histology for quantifying changes in liver fat in nonalcoholic fatty liver disease trials. Hepatology. 2013;58(6):1930–1940. doi: 10.1002/hep.26455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koo SH. Nonalcoholic fatty liver disease: Molecular mechanisms for the hepatic steatosis. Clin Mol Hepatol. 2013;19(3):210–215. doi: 10.3350/cmh.2013.19.3.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Falcon A, Doege H, Fluitt A, Tsang B, Watson N, Kay MA, et al. Fatp2 is a hepatic fatty acid transporter and peroxisomal very long-chain acyl-coa synthetase. Am J Physiol Endocrinol Metab. 2010;299(3):E384–393. doi: 10.1152/ajpendo.00226.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perez VM, Gabell J, Behrens M, Wase N, DiRusso CC, Black PN. Deletion of fatty acid transport protein 2 (fatp2) in the mouse liver changes the metabolic landscape by increasing the expression of pparα-regulated genes. J Biol Chem. 2020;295(17):5737–5750. doi: 10.1074/jbc.RA120.012730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Doege H, Grimm D, Falcon A, Tsang B, Storm TA, Xu H, et al. Silencing of hepatic fatty acid transporter protein 5 in vivo reverses diet-induced non-alcoholic fatty liver disease and improves hyperglycemia. J Biol Chem. 2008;283(32):22186–22192. doi: 10.1074/jbc.M803510200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Enooku K, Tsutsumi T, Kondo M, Fujiwara N, Sasako T, Shibahara J, et al. Hepatic fatp5 expression is associated with histological progression and loss of hepatic fat in nafld patients. J Gastroenterol. 2020;55(2):227–243. doi: 10.1007/s00535-019-01633-2. [DOI] [PubMed] [Google Scholar]
- 19.Koonen DP, Jacobs RL, Febbraio M, Young ME, Soltys CL, Ong H, et al. Increased hepatic cd36 expression contributes to dyslipidemia associated with diet-induced obesity. Diabetes. 2007;56(12):2863–2871. doi: 10.2337/db07-0907. [DOI] [PubMed] [Google Scholar]
- 20.Zhao L, Zhang C, Luo X, Wang P, Zhou W, Zhong S, et al. Cd36 palmitoylation disrupts free fatty acid metabolism and promotes tissue inflammation in non-alcoholic steatohepatitis. J Hepatol. 2018;69(3):705–717. doi: 10.1016/j.jhep.2018.04.006. [DOI] [PubMed] [Google Scholar]
- 21.Zeng S, Wu F, Chen M, Li Y, You M, Zhang Y, et al. Inhibition of fatty acid translocase (fat/cd36) palmitoylation enhances hepatic fatty acid β-oxidation by increasing its localization to mitochondria and interaction with long-chain acyl-coa synthetase 1. Antioxid Redox Signal. 2022;36(16-18):1081–1100. doi: 10.1089/ars.2021.0157. [DOI] [PubMed] [Google Scholar]
- 22.Wang J, Hao JW, Wang X, Guo H, Sun HH, Lai XY, et al. Dhhc4 and dhhc5 facilitate fatty acid uptake by palmitoylating and targeting cd36 to the plasma membrane. Cell Rep. 2019;26(1):209–221.e205. doi: 10.1016/j.celrep.2018.12.022. [DOI] [PubMed] [Google Scholar]
- 23.Hajri T, Zaiou M, Fungwe TV, Ouguerram K, Besong S. Epigenetic regulation of peroxisome proliferator-activated receptor gamma mediates high-fat diet-induced non-alcoholic fatty liver disease. Cells. 2021;10(6):1355. doi: 10.3390/cells10061355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang Z, Huang X, Zhang J, You K, Xiong Y, Fang J, et al. Hepatic dkk1-driven steatosis is cd36 dependent. Life Sci Alliance. 2023;6(1):e202201665. doi: 10.26508/lsa.202201665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pan X, Queiroz J, Hussain MM. Nonalcoholic fatty liver disease in clock mutant mice. J Clin Invest. 2020;130(8):4282–4300. doi: 10.1172/jci132765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.El-Derany MO, AbdelHamid SG. Upregulation of mir-96-5p by bone marrow mesenchymal stem cells and their exosomes alleviate non-alcoholic steatohepatitis: Emphasis on caspase-2 signaling inhibition. Biochem Pharmacol. 2021;190:114624. doi: 10.1016/j.bcp.2021.114624. [DOI] [PubMed] [Google Scholar]
- 27.Smolka C, Schlösser D, Hohnloser C, Bemtgen X, Jänich C, Schneider L, et al. Mir-100 overexpression attenuates high fat diet induced weight gain, liver steatosis, hypertriglyceridemia and development of metabolic syndrome in mice. Mol Med. 2021;27(1):101. doi: 10.1186/s10020-021-00364-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ding D, Ye G, Lin Y, Lu Y, Zhang H, Zhang X, et al. Microrna-26a-cd36 signaling pathway: Pivotal role in lipid accumulation in hepatocytes induced by pm(2.5) liposoluble extracts. Environ Pollut. 2019;248:269–278. doi: 10.1016/j.envpol.2019.01.112. [DOI] [PubMed] [Google Scholar]
- 29.Guo J, Fang W, Sun L, Lu Y, Dou L, Huang X, et al. Ultraconserved element uc.372 drives hepatic lipid accumulation by suppressing mir-195/mir4668 maturation. Nat Commun. 2018;9(1):612. doi: 10.1038/s41467-018-03072-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Qiu Y, Liu S, Chen HT, Yu CH, Teng XD, Yao HT, et al. Upregulation of caveolin-1 and sr-b1 in mice with non-alcoholic fatty liver disease. Hepatobiliary Pancreat Dis Int. 2013;12(6):630–636. doi: 10.1016/s1499-3872(13)60099-5. [DOI] [PubMed] [Google Scholar]
- 31.Li M, Chen D, Huang H, Wang J, Wan X, Xu C, et al. Caveolin1 protects against diet induced hepatic lipid accumulation in mice. PLoS One. 2017;12(6):e0178748. doi: 10.1371/journal.pone.0178748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Xue W, Wang J, Jiang W, Shi C, Wang X, Huang Y, et al. Caveolin-1 alleviates lipid accumulation in nafld associated with promoting autophagy by inhibiting the akt/mtor pathway. Eur J Pharmacol. 2020;871:172910. doi: 10.1016/j.ejphar.2020.172910. [DOI] [PubMed] [Google Scholar]
- 33.Han M, Piorońska W, Wang S, Nwosu ZC, Sticht C, Wang S, et al. Hepatocyte caveolin-1 modulates metabolic gene profiles and functions in non-alcoholic fatty liver disease. Cell Death Dis. 2020;11(2):104. doi: 10.1038/s41419-020-2295-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Siculella L, Giannotti L, Testini M, Gnoni GV, Damiano F. In steatotic cells, atp-citrate lyase mrna is efficiently translated through a cap-independent mechanism, contributing to the stimulation of de novo lipogenesis. Int J Mol Sci. 2020;21(4):1206. doi: 10.3390/ijms21041206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Guo L, Guo YY, Li BY, Peng WQ, Chang XX, Gao X, et al. Enhanced acetylation of atp-citrate lyase promotes the progression of nonalcoholic fatty liver disease. J Biol Chem. 2019;294(31):11805–11816. doi: 10.1074/jbc.RA119.008708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li K, Zhang K, Wang H, Wu Y, Chen N, Chen J, et al. Hrd1-mediated acly ubiquitination alleviate nafld in db/db mice. Metabolism. 2021;114:154349. doi: 10.1016/j.metabol.2020.154349. [DOI] [PubMed] [Google Scholar]
- 37.Zhao S, Jang C, Liu J, Uehara K, Gilbert M, Izzo L, et al. Dietary fructose feeds hepatic lipogenesis via microbiota-derived acetate. Nature. 2020;579(7800):586–591. doi: 10.1038/s41586-020-2101-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mao J, DeMayo FJ, Li H, Abu-Elheiga L, Gu Z, Shaikenov TE, et al. Liver-specific deletion of acetyl-coa carboxylase 1 reduces hepatic triglyceride accumulation without affecting glucose homeostasis. Proc Natl Acad Sci U S A. 2006;103(22):8552–8557. doi: 10.1073/pnas.0603115103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lally JSV, Ghoshal S, DePeralta DK, Moaven O, Wei L, Masia R, et al. Inhibition of acetyl-coa carboxylase by phosphorylation or the inhibitor nd-654 suppresses lipogenesis and hepatocellular carcinoma. Cell Metab. 2019;29(1):174–182.e175. doi: 10.1016/j.cmet.2018.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hu Y, He W, Huang Y, Xiang H, Guo J, Che Y, et al. Fatty acid synthase-suppressor screening identifies sorting nexin 8 as a therapeutic target for nafld. Hepatology. 2021;74(5):2508–2525. doi: 10.1002/hep.32045. [DOI] [PubMed] [Google Scholar]
- 41.Zhang M, Tang Y, Tang E, Lu W. Microrna-103 represses hepatic de novo lipogenesis and alleviates nafld via targeting fasn and scd1. Biochem Biophys Res Commun. 2020;524(3):716–722. doi: 10.1016/j.bbrc.2020.01.143. [DOI] [PubMed] [Google Scholar]
- 42.Liu Y, Lin H, Jiang L, Shang Q, Yin L, Lin JD, et al. Hepatic slug epigenetically promotes liver lipogenesis, fatty liver disease, and type 2 diabetes. J Clin Invest. 2020;130(6):2992–3004. doi: 10.1172/jci128073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gao R, Li Y, Xu Z, Zhang F, Xu J, Hu Y, et al. Mitochondrial pyruvate carrier 1 regulates fatty acid synthase lactylation and mediates treatment of nonalcoholic fatty liver disease. Hepatology. 2023;78(6):1800–1815. doi: 10.1097/hep.0000000000000279. [DOI] [PubMed] [Google Scholar]
- 44.Shimano H, Horton JD, Shimomura I, Hammer RE, Brown MS, Goldstein JL. Isoform 1c of sterol regulatory element binding protein is less active than isoform 1a in livers of transgenic mice and in cultured cells. J Clin Invest. 1997;99(5):846–854. doi: 10.1172/jci119248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bae JY. Resistance exercise regulates hepatic lipolytic factors as effective as aerobic exercise in obese mice. Int J Environ Res Public Health. 2020;17(22):8307. doi: 10.3390/ijerph17228307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dos Santos GF, Veras ASC, de Freitas MC, McCabe J, Seraphim PM, Teixeira GR. Strength training reduces lipid accumulation in liver of obese wistar rats. Life Sci. 2019;235:116834. doi: 10.1016/j.lfs.2019.116834. [DOI] [PubMed] [Google Scholar]
- 47.Li R, Li Y, Yang X, Hu Y, Yu H, Li Y. Reducing vegfb accelerates nafld and insulin resistance in mice via inhibiting ampk signaling pathway. J Transl Med. 2022;20(1):341. doi: 10.1186/s12967-022-03540-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Luo W, Ye L, Hu XT, Wang MH, Wang MX, Jin LM, et al. Md2 deficiency prevents high-fat diet-induced ampk suppression and lipid accumulation through regulating tbk1 in non-alcoholic fatty liver disease. Clin Transl Med. 2022;12(3):e777. doi: 10.1002/ctm2.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jung TW, Kyung EJ, Kim HC, Shin YK, Lee SH, Park ES, et al. Protectin dx ameliorates hepatic steatosis by suppression of endoplasmic reticulum stress via ampk-induced orp150 expression. J Pharmacol Exp Ther. 2018;365(3):485–493. doi: 10.1124/jpet.117.246686. [DOI] [PubMed] [Google Scholar]
- 50.Han J, Li E, Chen L, Zhang Y, Wei F, Liu J, et al. The creb coactivator crtc2 controls hepatic lipid metabolism by regulating srebp1. Nature. 2015;524(7564):243–246. doi: 10.1038/nature14557. [DOI] [PubMed] [Google Scholar]
- 51.Ma N, Wang YK, Xu S, Ni QZ, Zheng QW, Zhu B, et al. Ppdpf alleviates hepatic steatosis through inhibition of mtor signaling. Nat Commun. 2021;12(1):3059. doi: 10.1038/s41467-021-23285-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zeng H, Qin H, Liao M, Zheng E, Luo X, Xiao A, et al. Cd36 promotes de novo lipogenesis in hepatocytes through insig2-dependent srebp1 processing. Mol Metab. 2022;57:101428. doi: 10.1016/j.molmet.2021.101428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li L, Zhang X, Ren H, Huang X, Shen T, Tang W, et al. Mir-23a/b-3p promotes hepatic lipid accumulation by regulating srebp-1c and fas. J Mol Endocrinol. 2021;68(1):35–49. doi: 10.1530/jme-20-0324. [DOI] [PubMed] [Google Scholar]
- 54.Pan JH, Cha H, Tang J, Lee S, Lee SH, Le B, et al. The role of microrna-33 as a key regulator in hepatic lipogenesis signaling and a potential serological biomarker for nafld with excessive dietary fructose consumption in c57bl/6n mice. Food Funct. 2021;12(2):656–667. doi: 10.1039/d0fo02286a. [DOI] [PubMed] [Google Scholar]
- 55.Liu X, Chen S, Zhang L. Downregulated microrna-130b-5p prevents lipid accumulation and insulin resistance in a murine model of nonalcoholic fatty liver disease. Am J Physiol Endocrinol Metab. 2020;319(1):E34–e42. doi: 10.1152/ajpendo.00528.2019. [DOI] [PubMed] [Google Scholar]
- 56.Zhou JP, Ren YD, Xu QY, Song Y, Zhou F, Chen MY, et al. Obesity-induced upregulation of zbtb7a promotes lipid accumulation through srebp1. Biomed Res Int. 2020;2020:4087928. doi: 10.1155/2020/4087928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kim YR, Lee EJ, Shin KO, Kim MH, Pewzner-Jung Y, Lee YM, et al. Hepatic triglyceride accumulation via endoplasmic reticulum stress-induced srebp-1 activation is regulated by ceramide synthases. Exp Mol Med. 2019;51(11):1–16. doi: 10.1038/s12276-019-0340-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Seidu T, McWhorter P, Myer J, Alamgir R, Eregha N, Bogle D, et al. Dht causes liver steatosis via transcriptional regulation of scap in normal weight female mice. J Endocrinol. 2021;250(2):49–65. doi: 10.1530/joe-21-0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Araki M, Nakagawa Y, Saito H, Yamada Y, Han SI, Mizunoe Y, et al. Hepatocyte- or macrophage-specific srebp-1a deficiency in mice exacerbates methionine- and choline-deficient diet-induced nonalcoholic fatty liver disease. Am J Physiol Gastrointest Liver Physiol. 2022;323(6):G627–g639. doi: 10.1152/ajpgi.00090.2022. [DOI] [PubMed] [Google Scholar]
- 60.Wei G, An P, Vaid KA, Nasser I, Huang P, Tan L, et al. Comparison of murine steatohepatitis models identifies a dietary intervention with robust fibrosis, ductular reaction, and rapid progression to cirrhosis and cancer. Am J Physiol Gastrointest Liver Physiol. 2020;318(1):G174–g188. doi: 10.1152/ajpgi.00041.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gabbia D, Roverso M, Guido M, Sacchi D, Scaffidi M, Carrara M, et al. Western diet-induced metabolic alterations affect circulating markers of liver function before the development of steatosis. Nutrients. 2019;11(7):1602. doi: 10.3390/nu11071602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cheng C, Deng X, Xu K. Increased expression of sterol regulatory element binding protein-2 alleviates autophagic dysfunction in nafld. Int J Mol Med. 2018;41(4):1877–1886. doi: 10.3892/ijmm.2018.3389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Huh JY, Reilly SM, Abu-Odeh M, Murphy AN, Mahata SK, Zhang J, et al. Tank-binding kinase 1 regulates the localization of acyl-coa synthetase acsl1 to control hepatic fatty acid oxidation. Cell Metab. 2020;32(6):1012–1027.e1017. doi: 10.1016/j.cmet.2020.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Duan J, Wang Z, Duan R, Yang C, Zhao R, Feng Q, et al. Therapeutic targeting of hepatic acsl4 ameliorates nash in mice. Hepatology. 2022;75(1):140–153. doi: 10.1002/hep.32148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Singh AB, Kan CFK, Kraemer FB, Sobel RA, Liu J. Liver-specific knockdown of long-chain acyl-coa synthetase 4 reveals its key role in vldl-tg metabolism and phospholipid synthesis in mice fed a high-fat diet. Am J Physiol Endocrinol Metab. 2019;316(5):E880–e894. doi: 10.1152/ajpendo.00503.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wei S, Qiu T, Wang N, Yao X, Jiang L, Jia X, et al. Ferroptosis mediated by the interaction between mfn2 and ireα promotes arsenic-induced nonalcoholic steatohepatitis. Environ Res. 2020;188:109824. doi: 10.1016/j.envres.2020.109824. [DOI] [PubMed] [Google Scholar]
- 67.Sen P, Kan CFK, Singh AB, Rius M, Kraemer FB, Sztul E, et al. Identification of p115 as a novel acsl4 interacting protein and its role in regulating acsl4 degradation. J Proteomics. 2020;229:103926. doi: 10.1016/j.jprot.2020.103926. [DOI] [PubMed] [Google Scholar]
- 68.Bowman TA, O’Keeffe KR, D’Aquila T, Yan QW, Griffin JD, Killion EA, et al. Acyl coa synthetase 5 (acsl5) ablation in mice increases energy expenditure and insulin sensitivity and delays fat absorption. Mol Metab. 2016;5(3):210–220. doi: 10.1016/j.molmet.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Luo Y, Chen Q, Zou J, Fan J, Li Y, Luo Z. Chronic intermittent hypoxia exposure alternative to exercise alleviates high-fat-diet-induced obesity and fatty liver. Int J Mol Sci. 2022;23(9):5209. doi: 10.3390/ijms23095209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zheng F, Cai Y. Concurrent exercise improves insulin resistance and nonalcoholic fatty liver disease by upregulating ppar-γ and genes involved in the beta-oxidation of fatty acids in apoe-ko mice fed a high-fat diet. Lipids Health Dis. 2019;18(1):6. doi: 10.1186/s12944-018-0933-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ahmed EA, El-Derany MO, Anwar AM, Saied EM, Magdeldin S. Metabolomics and lipidomics screening reveal reprogrammed signaling pathways toward cancer development in non-alcoholic steatohepatitis. Int J Mol Sci. 2022;24(1):210. doi: 10.3390/ijms24010210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Heinecke F, Mazzucco MB, Fornes D, Roberti S, Jawerbaum A, White V. The offspring from rats fed a fatty diet display impairments in the activation of liver peroxisome proliferator activated receptor alpha and features of fatty liver disease. Mol Cell Endocrinol. 2020;511:110818. doi: 10.1016/j.mce.2020.110818. [DOI] [PubMed] [Google Scholar]
- 73.Smati S, Polizzi A, Fougerat A, Ellero-Simatos S, Blum Y, Lippi Y, et al. Integrative study of diet-induced mouse models of nafld identifies pparα as a sexually dimorphic drug target. Gut. 2022;71(4):807–821. doi: 10.1136/gutjnl-2020-323323. [DOI] [PubMed] [Google Scholar]
- 74.Silva-Veiga FM, Miranda CS, Vasques-Monteiro IML, Souza-Tavares H, Martins FF, Daleprane JB, et al. Peroxisome proliferator-activated receptor-alpha activation and dipeptidyl peptidase-4 inhibition target dysbiosis to treat fatty liver in obese mice. World J Gastroenterol. 2022;28(17):1814–1829. doi: 10.3748/wjg.v28.i17.1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yan T, Luo Y, Yan N, Hamada K, Zhao N, Xia Y, et al. Intestinal peroxisome proliferator-activated receptor α-fatty acid-binding protein 1 axis modulates nonalcoholic steatohepatitis. Hepatology. 2023;77(1):239–255. doi: 10.1002/hep.32538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chen K, Chen X, Xue H, Zhang P, Fang W, Chen X, et al. Coenzyme q10 attenuates high-fat diet-induced non-alcoholic fatty liver disease through activation of the ampk pathway. Food Funct. 2019;10(2):814–823. doi: 10.1039/c8fo01236a. [DOI] [PubMed] [Google Scholar]
- 77.Du X, Osoro EK, Chen Q, Yan X, Gao D, Wu L, et al. Pdcd4 promotes lipid deposition by attenuating pparα-mediated fatty acid oxidation in hepatocytes. Mol Cell Endocrinol. 2022;545:111562. doi: 10.1016/j.mce.2022.111562. [DOI] [PubMed] [Google Scholar]
- 78.Wei X, Zhang J, Tang M, Wang X, Fan N, Peng Y. Fat mass and obesity-associated protein promotes liver steatosis by targeting pparα. Lipids Health Dis. 2022;21(1):29. doi: 10.1186/s12944-022-01640-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Qin G, Wang GZ, Guo DD, Bai RX, Wang M, Du SY. Deletion of smad4 reduces hepatic inflammation and fibrogenesis during nonalcoholic steatohepatitis progression. J Dig Dis. 2018;19(5):301–313. doi: 10.1111/1751-2980.12599. [DOI] [PubMed] [Google Scholar]
- 80.Ko CW, Qu J, Black DD, Tso P. Regulation of intestinal lipid metabolism: Current concepts and relevance to disease. Nat Rev Gastroenterol Hepatol. 2020;17(3):169–183. doi: 10.1038/s41575-019-0250-7. [DOI] [PubMed] [Google Scholar]
- 81.Toyoda Y, Takada T, Yamanashi Y, Suzuki H. Pathophysiological importance of bile cholesterol reabsorption: Hepatic npc1l1-exacerbated steatosis and decreasing vldl-tg secretion in mice fed a high-fat diet. Lipids Health Dis. 2019;18(1):234. doi: 10.1186/s12944-019-1179-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Yamanashi Y, Takada T, Tanaka Y, Ogata Y, Toyoda Y, Ito SM, et al. Hepatic niemann-pick c1-like 1 exacerbates non-alcoholic fatty liver disease by re-absorbing specific biliary oxysterols. Biomed Pharmacother. 2022;156:113877. doi: 10.1016/j.biopha.2022.113877. [DOI] [PubMed] [Google Scholar]
- 83.Min HK, Kapoor A, Fuchs M, Mirshahi F, Zhou H, Maher J, et al. Increased hepatic synthesis and dysregulation of cholesterol metabolism is associated with the severity of nonalcoholic fatty liver disease. Cell Metab. 2012;15(5):665–674. doi: 10.1016/j.cmet.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Li T, Yan H, Geng Y, Shi H, Li H, Wang S, et al. Target genes associated with lipid and glucose metabolism in non-alcoholic fatty liver disease. Lipids Health Dis. 2019;18(1):211. doi: 10.1186/s12944-019-1154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Liu MX, Gao M, Li CZ, Yu CZ, Yan H, Peng C, et al. Dicer1/mir-29/hmgcr axis contributes to hepatic free cholesterol accumulation in mouse non-alcoholic steatohepatitis. Acta Pharmacol Sin. 2017;38(5):660–671. doi: 10.1038/aps.2016.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Liang JQ, Teoh N, Xu L, Pok S, Li X, Chu ESH, et al. Dietary cholesterol promotes steatohepatitis related hepatocellular carcinoma through dysregulated metabolism and calcium signaling. Nat Commun. 2018;9(1):4490. doi: 10.1038/s41467-018-06931-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Liu D, Wong CC, Fu L, Chen H, Zhao L, Li C, et al. Squalene epoxidase drives nafld-induced hepatocellular carcinoma and is a pharmaceutical target. Sci Transl Med. 2018;10(437):eaap9840. doi: 10.1126/scitranslmed.aap9840. [DOI] [PubMed] [Google Scholar]
- 88.Liu D, Wong CC, Zhou Y, Li C, Chen H, Ji F, et al. Squalene epoxidase induces nonalcoholic steatohepatitis via binding to carbonic anhydrase iii and is a therapeutic target. Gastroenterology. 2021;160(7):2467–2482.e2463. doi: 10.1053/j.gastro.2021.02.051. [DOI] [PubMed] [Google Scholar]
- 89.Sun H, Li L, Li W, Yang F, Zhang Z, Liu Z, et al. P53 transcriptionally regulates sqle to repress cholesterol synthesis and tumor growth. EMBO Rep. 2021;22(10):e52537. doi: 10.15252/embr.202152537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Jia X, Zhai T. Integrated analysis of multiple microarray studies to identify novel gene signatures in non-alcoholic fatty liver disease. Front Endocrinol (Lausanne) 2019;10:599. doi: 10.3389/fendo.2019.00599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Wu C, Zhou Y, Wang M, Dai G, Liu X, Lai L, et al. Bioinformatics analysis explores potential hub genes in nonalcoholic fatty liver disease. Front Genet. 2021;12:772487. doi: 10.3389/fgene.2021.772487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Jiao N, Baker SS, Chapa-Rodriguez A, Liu W, Nugent CA, Tsompana M, et al. Suppressed hepatic bile acid signalling despite elevated production of primary and secondary bile acids in nafld. Gut. 2018;67(10):1881–1891. doi: 10.1136/gutjnl-2017-314307. [DOI] [PubMed] [Google Scholar]
- 93.Suga T, Yamaguchi H, Ogura J, Shoji S, Maekawa M, Mano N. Altered bile acid composition and disposition in a mouse model of non-alcoholic steatohepatitis. Toxicol Appl Pharmacol. 2019;379:114664. doi: 10.1016/j.taap.2019.114664. [DOI] [PubMed] [Google Scholar]
- 94.Clifford BL, Sedgeman LR, Williams KJ, Morand P, Cheng A, Jarrett KE, et al. Fxr activation protects against nafld via bile-acid-dependent reductions in lipid absorption. Cell Metab. 2021;33(8):1671–1684.e1674. doi: 10.1016/j.cmet.2021.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Deng W, Fan W, Tang T, Wan H, Zhao S, Tan Y, et al. Farnesoid x receptor deficiency induces hepatic lipid and glucose metabolism disorder via regulation of pyruvate dehydrogenase kinase 4. Oxid Med Cell Longev. 2022;2022:3589525. doi: 10.1155/2022/3589525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Xu W, Cui C, Cui C, Chen Z, Zhang H, Cui Q, et al. Hepatocellular cystathionine γ lyase/hydrogen sulfide attenuates nonalcoholic fatty liver disease by activating farnesoid x receptor. Hepatology. 2022;76(6):1794–1810. doi: 10.1002/hep.32577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Fan L, Lai R, Ma N, Dong Y, Li Y, Wu Q, et al. Mir-552-3p modulates transcriptional activities of fxr and lxr to ameliorate hepatic glycolipid metabolism disorder. J Hepatol. 2021;74(1):8–19. doi: 10.1016/j.jhep.2020.07.048. [DOI] [PubMed] [Google Scholar]
- 98.Kokkorakis M, Boutari C, Hill MA, Kotsis V, Loomba R, Sanyal AJ, et al. Resmetirom, the first approved drug for the management of metabolic dysfunction-associated steatohepatitis: Trials, opportunities, and challenges. Metabolism. 2024;154:155835. doi: 10.1016/j.metabol.2024.155835. [DOI] [PubMed] [Google Scholar]
- 99.Krishnan A, Schneider CV, Hadi Y, Mukherjee D, AlShehri B, Alqahtani SA. Cardiovascular and mortality outcomes with glp-1 receptor agonists vs other glucose-lowering drugs in individuals with nafld and type 2 diabetes: A large population-based matched cohort study. Diabetologia. 2024;67(3):483–493. doi: 10.1007/s00125-023-06057-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Liao C, Liang X, Zhang X, Li Y. The effects of glp-1 receptor agonists on visceral fat and liver ectopic fat in an adult population with or without diabetes and nonalcoholic fatty liver disease: A systematic review and meta-analysis. PLoS One. 2023;18(8):e0289616. doi: 10.1371/journal.pone.0289616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Gu Y, Sun L, Zhang W, Kong T, Zhou R, He Y, et al. Comparative efficacy of 5 sodium-glucose cotransporter protein-2 (sglt-2) inhibitor and 4 glucagon-like peptide-1 (glp-1) receptor agonist drugs in non-alcoholic fatty liver disease: A grade-assessed systematic review and network meta-analysis of randomized controlled trials. Front Pharmacol. 2023;14:1102792. doi: 10.3389/fphar.2023.1102792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Gu Y, Sun L, He Y, Yang L, Deng C, Zhou R, et al. Comparative efficacy of glucagon-like peptide 1 (glp-1) receptor agonists, pioglitazone and vitamin e for liver histology among patients with nonalcoholic fatty liver disease: Systematic review and pilot network meta-analysis of randomized controlled trials. Expert Rev Gastroenterol Hepatol. 2023;17(3):273–282. doi: 10.1080/17474124.2023.2172397. [DOI] [PubMed] [Google Scholar]
- 103.Romero-Gómez M, Armstrong MJ, Funuyet-Salas J, Mangla KK, Ladelund S, Sejling AS, et al. Improved health-related quality of life with semaglutide in people with non-alcoholic steatohepatitis: A randomised trial. Aliment Pharmacol Ther. 2023;58(4):395–403. doi: 10.1111/apt.17598. [DOI] [PubMed] [Google Scholar]
- 104.Yuan X, Gao Z, Yang C, Duan K, Ren L, Song G. Comparing the effectiveness of long-term use of daily and weekly glucagon-like peptide-1 receptor agonists treatments in patients with nonalcoholic fatty liver disease and type 2 diabetes mellitus: A network meta-analysis. Front Endocrinol (Lausanne) 2023;14:1170881. doi: 10.3389/fendo.2023.1170881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Mao T, Zhang C, Yang S, Bi Y, Li M, Yu J. Semaglutide alters gut microbiota and improves nafld in db/db mice. Biochem Biophys Res Commun. 2024;710:149882. doi: 10.1016/j.bbrc.2024.149882. [DOI] [PubMed] [Google Scholar]
- 106.Kim ER, Park JS, Kim JH, Oh JY, Oh IJ, Choi DH, et al. A glp-1/glp-2 receptor dual agonist to treat nash: Targeting the gut-liver axis and microbiome. Hepatology. 2022;75(6):1523–1538. doi: 10.1002/hep.32235. [DOI] [PubMed] [Google Scholar]
- 107.Romero-Gómez M, Lawitz E, Shankar RR, Chaudhri E, Liu J, Lam RLH, et al. A phase iia active-comparator-controlled study to evaluate the efficacy and safety of efinopegdutide in patients with non-alcoholic fatty liver disease. J Hepatol. 2023;79(4):888–897. doi: 10.1016/j.jhep.2023.05.013. [DOI] [PubMed] [Google Scholar]
- 108.Nestor JJ, Parkes D, Feigh M, Suschak JJ, Harris MS. Effects of alt-801, a glp-1 and glucagon receptor dual agonist, in a translational mouse model of non-alcoholic steatohepatitis. Sci Rep. 2022;12(1):6666. doi: 10.1038/s41598-022-10577-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Monfeuga T, Norlin J, Bugge A, Gaalsgaard ED, Prada-Medina CA, Latta M, et al. Evaluation of long acting glp1r/gcgr agonist in a dio and biopsy-confirmed mouse model of nash suggest a beneficial role of glp-1/glucagon agonism in nash patients. Mol Metab. 2024;79:101850. doi: 10.1016/j.molmet.2023.101850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Desjardins EM, Wu J, Lavoie DCT, Ahmadi E, Townsend LK, Morrow MR, et al. Combination of an acly inhibitor with a glp-1r agonist exerts additive benefits on nonalcoholic steatohepatitis and hepatic fibrosis in mice. Cell Rep Med. 2023;4(9):101193. doi: 10.1016/j.xcrm.2023.101193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Alkhouri N, Herring R, Kabler H, Kayali Z, Hassanein T, Kohli A, et al. Safety and efficacy of combination therapy with semaglutide, cilofexor and firsocostat in patients with non-alcoholic steatohepatitis: A randomised, open-label phase ii trial. J Hepatol. 2022;77(3):607–618. doi: 10.1016/j.jhep.2022.04.003. [DOI] [PubMed] [Google Scholar]
- 112.Xue H, Xing HJ, Wang B, Fu C, Zhang YS, Qiao X, et al. Cinchonine, a potential oral small-molecule glucagon-like peptide-1 receptor agonist, lowers blood glucose and ameliorates non-alcoholic steatohepatitis. Drug Des Devel Ther. 2023;17:1417–1432. doi: 10.2147/dddt.S404055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Mahalingam S, Bellamkonda R, Arumugam MK, Perumal SK, Yoon J, Casey C, et al. Glucagon-like peptide 1 receptor agonist, exendin-4, reduces alcohol-associated fatty liver disease. Biochem Pharmacol. 2023;213:115613. doi: 10.1016/j.bcp.2023.115613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kuchay MS, Krishan S, Mishra SK, Choudhary NS, Singh MK, Wasir JS, et al. Effect of dulaglutide on liver fat in patients with type 2 diabetes and nafld: Randomised controlled trial (d-lift trial) Diabetologia. 2020;63(11):2434–2445. doi: 10.1007/s00125-020-05265-7. [DOI] [PubMed] [Google Scholar]
- 115.Liu L, Yan H, Xia M, Zhao L, Lv M, Zhao N, et al. Efficacy of exenatide and insulin glargine on nonalcoholic fatty liver disease in patients with type 2 diabetes. Diabetes Metab Res Rev. 2020;36(5):e3292. doi: 10.1002/dmrr.3292. [DOI] [PubMed] [Google Scholar]
- 116.Khoo J, Hsiang JC, Taneja R, Koo SH, Soon GH, Kam CJ, et al. Randomized trial comparing effects of weight loss by liraglutide with lifestyle modification in non-alcoholic fatty liver disease. Liver Int. 2019;39(5):941–949. doi: 10.1111/liv.14065. [DOI] [PubMed] [Google Scholar]
- 117.Armstrong MJ, Hull D, Guo K, Barton D, Hazlehurst JM, Gathercole LL, et al. Glucagon-like peptide 1 decreases lipotoxicity in non-alcoholic steatohepatitis. J Hepatol. 2016;64(2):399–408. doi: 10.1016/j.jhep.2015.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Khoo J, Hsiang J, Taneja R, Law NM, Ang TL. Comparative effects of liraglutide 3 mg vs structured lifestyle modification on body weight, liver fat and liver function in obese patients with non-alcoholic fatty liver disease: A pilot randomized trial. Diabetes Obes Metab. 2017;19(12):1814–1817. doi: 10.1111/dom.13007. [DOI] [PubMed] [Google Scholar]
- 119.Petit JM, Cercueil JP, Loffroy R, Denimal D, Bouillet B, Fourmont C, et al. Effect of liraglutide therapy on liver fat content in patients with inadequately controlled type 2 diabetes: The lira-nafld study. J Clin Endocrinol Metab. 2017;102(2):407–415. doi: 10.1210/jc.2016-2775. [DOI] [PubMed] [Google Scholar]
- 120.Smits MM, Tonneijck L, Muskiet MH, Kramer MH, Pouwels PJ, Pieters-van den Bos IC, et al. Twelve week liraglutide or sitagliptin does not affect hepatic fat in type 2 diabetes: A randomised placebo-controlled trial. Diabetologia. 2016;59(12):2588–2593. doi: 10.1007/s00125-016-4100-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Newsome PN, Buchholtz K, Cusi K, Linder M, Okanoue T, Ratziu V, et al. A placebo-controlled trial of subcutaneous semaglutide in nonalcoholic steatohepatitis. N Engl J Med. 2021;384(12):1113–1124. doi: 10.1056/NEJMoa2028395. [DOI] [PubMed] [Google Scholar]
- 122.Flint A, Andersen G, Hockings P, Johansson L, Morsing A, Sundby Palle M, et al. Randomised clinical trial: Semaglutide versus placebo reduced liver steatosis but not liver stiffness in subjects with non-alcoholic fatty liver disease assessed by magnetic resonance imaging. Aliment Pharmacol Ther. 2021;54(9):1150–1161. doi: 10.1111/apt.16608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Farage AE, Abdo W, Osman A, Abdel-Kareem MA, Hakami ZH, Alsulimani A, et al. Betulin prevents high fat diet-induced non-alcoholic fatty liver disease by mitigating oxidative stress and upregulating nrf2 and sirt1 in rats. Life Sci. 2023;322:121688. doi: 10.1016/j.lfs.2023.121688. [DOI] [PubMed] [Google Scholar]
- 124.Kim KD, Jung HY, Ryu HG, Kim B, Jeon J, Yoo HY, et al. Betulinic acid inhibits high-fat diet-induced obesity and improves energy balance by activating ampk. Nutr Metab Cardiovasc Dis. 2019;29(4):409–420. doi: 10.1016/j.numecd.2018.12.001. [DOI] [PubMed] [Google Scholar]
- 125.Mu Q, Wang H, Tong L, Fang Q, Xiang M, Han L, et al. Betulinic acid improves nonalcoholic fatty liver disease through yy1/fas signaling pathway. Faseb j. 2020;34(9):13033–13048. doi: 10.1096/fj.202000546R. [DOI] [PubMed] [Google Scholar]
- 126.Quan HY, Kim DY, Kim SJ, Jo HK, Kim GW, Chung SH. Betulinic acid alleviates non-alcoholic fatty liver by inhibiting srebp1 activity via the ampk-mtor-srebp signaling pathway. Biochem Pharmacol. 2013;85(9):1330–1340. doi: 10.1016/j.bcp.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 127.Bitter A, Nüssler AK, Thasler WE, Klein K, Zanger UM, Schwab M, et al. Human sterol regulatory element-binding protein 1a contributes significantly to hepatic lipogenic gene expression. Cell Physiol Biochem. 2015;35(2):803–815. doi: 10.1159/000369739. [DOI] [PubMed] [Google Scholar]
- 128.Bates J, Vijayakumar A, Ghoshal S, Marchand B, Yi S, Kornyeyev D, et al. Acetyl-coa carboxylase inhibition disrupts metabolic reprogramming during hepatic stellate cell activation. J Hepatol. 2020;73(4):896–905. doi: 10.1016/j.jhep.2020.04.037. [DOI] [PubMed] [Google Scholar]
- 129.Goedeke L, Bates J, Vatner DF, Perry RJ, Wang T, Ramirez R, et al. Acetyl-coa carboxylase inhibition reverses nafld and hepatic insulin resistance but promotes hypertriglyceridemia in rodents. Hepatology. 2018;68(6):2197–2211. doi: 10.1002/hep.30097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Lawitz EJ, Coste A, Poordad F, Alkhouri N, Loo N, McColgan BJ, et al. Acetyl-coa carboxylase inhibitor gs-0976 for 12 weeks reduces hepatic de novo lipogenesis and steatosis in patients with nonalcoholic steatohepatitis. Clin Gastroenterol Hepatol. 2018;16(12):1983–1991.e1983. doi: 10.1016/j.cgh.2018.04.042. [DOI] [PubMed] [Google Scholar]
- 131.Loomba R, Kayali Z, Noureddin M, Ruane P, Lawitz EJ, Bennett M, et al. Gs-0976 reduces hepatic steatosis and fibrosis markers in patients with nonalcoholic fatty liver disease. Gastroenterology. 2018;155(5):1463–1473.e1466. doi: 10.1053/j.gastro.2018.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Dandan M, Han J, Mann S, Kim R, Li K, Mohammed H, et al. Acetyl-coa carboxylase inhibitor increases ldl-apob production rate in nash with cirrhosis: Prevention by fenofibrate. J Lipid Res. 2023;64(3):100339. doi: 10.1016/j.jlr.2023.100339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Lawitz EJ, Bhandari BR, Ruane PJ, Kohli A, Harting E, Ding D, et al. Fenofibrate mitigates hypertriglyceridemia in nonalcoholic steatohepatitis patients treated with cilofexor/firsocostat. Clin Gastroenterol Hepatol. 2023;21(1):143–152.e143. doi: 10.1016/j.cgh.2021.12.044. [DOI] [PubMed] [Google Scholar]
- 134.Tamura YO, Sugama J, Iwasaki S, Sasaki M, Yasuno H, Aoyama K, et al. Selective acetyl-coa carboxylase 1 inhibitor improves hepatic steatosis and hepatic fibrosis in a preclinical nonalcoholic steatohepatitis model. J Pharmacol Exp Ther. 2021;379(3):280–289. doi: 10.1124/jpet.121.000786. [DOI] [PubMed] [Google Scholar]
- 135.Ross TT, Crowley C, Kelly KL, Rinaldi A, Beebe DA, Lech MP, et al. Acetyl-coa carboxylase inhibition improves multiple dimensions of nash pathogenesis in model systems. Cell Mol Gastroenterol Hepatol. 2020;10(4):829–851. doi: 10.1016/j.jcmgh.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Gao YS, Qian MY, Wei QQ, Duan XB, Wang SL, Hu HY, et al. Wz66, a novel acetyl-coa carboxylase inhibitor, alleviates nonalcoholic steatohepatitis (nash) in mice. Acta Pharmacol Sin. 2020;41(3):336–347. doi: 10.1038/s41401-019-0310-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Loomba R, Mohseni R, Lucas KJ, Gutierrez JA, Perry RG, Trotter JF, et al. Tvb-2640 (fasn inhibitor) for the treatment of nonalcoholic steatohepatitis: Fascinate-1, a randomized, placebo-controlled phase 2a trial. Gastroenterology. 2021;161(5):1475–1486. doi: 10.1053/j.gastro.2021.07.025. [DOI] [PubMed] [Google Scholar]
- 138.Beysen C, Schroeder P, Wu E, Brevard J, Ribadeneira M, Lu W, et al. Inhibition of fatty acid synthase with ft-4101 safely reduces hepatic de novo lipogenesis and steatosis in obese subjects with non-alcoholic fatty liver disease: Results from two early-phase randomized trials. Diabetes Obes Metab. 2021;23(3):700–710. doi: 10.1111/dom.14272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Xu S, Wu X, Wang S, Xu M, Fang T, Ma X, et al. Trim56 protects against nonalcoholic fatty liver disease by promoting the degradation of fatty acid synthase. J Clin Invest. 2024;134(5):e166149. doi: 10.1172/jci166149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Kurikawa N, Takagi T, Wakimoto S, Uto Y, Terashima H, Kono K, et al. A novel inhibitor of stearoyl-coa desaturase-1 attenuates hepatic lipid accumulation, liver injury and inflammation in model of nonalcoholic steatohepatitis. Biol Pharm Bull. 2013;36(2):259–267. doi: 10.1248/bpb.b12-00702. [DOI] [PubMed] [Google Scholar]
- 141.Zhou Y, Zhong L, Yu S, Shen W, Cai C, Yu H. Inhibition of stearoyl-coenzyme a desaturase 1 ameliorates hepatic steatosis by inducing ampk-mediated lipophagy. Aging (Albany NY) 2020;12(8):7350–7362. doi: 10.18632/aging.103082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Jiang S, Uddin MJ, Yu X, Piao L, Dorotea D, Oh GT, et al. Peroxisomal fitness: A potential protective mechanism of fenofibrate against high fat diet-induced non-alcoholic fatty liver disease in mice. Diabetes Metab J. 2022;46(6):829–842. doi: 10.4093/dmj.2021.0274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Guru B, Tamrakar AK, Manjula SN, Prashantha Kumar BR. Novel dual pparα/γ agonists protect against liver steatosis and improve insulin sensitivity while avoiding side effects. Eur J Pharmacol. 2022;935:175322. doi: 10.1016/j.ejphar.2022.175322. [DOI] [PubMed] [Google Scholar]
- 144.Grobbee EJ, de Jong VD, Schrieks IC, Tushuizen ME, Holleboom AG, Tardif JC, et al. Improvement of non-invasive tests of liver steatosis and fibrosis as indicators for non-alcoholic fatty liver disease in type 2 diabetes mellitus patients with elevated cardiovascular risk profile using the ppar-α/γ agonist aleglitazar. PLoS One. 2022;17(11):e0277706. doi: 10.1371/journal.pone.0277706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Feng Z, Xiang J, Liu H, Li J, Xu X, Sun G, et al. Design, synthesis, and biological evaluation of triazolone derivatives as potent pparα/δ dual agonists for the treatment of nonalcoholic steatohepatitis. J Med Chem. 2022;65(3):2571–2592. doi: 10.1021/acs.jmedchem.1c02002. [DOI] [PubMed] [Google Scholar]
- 146.Zhou Z, Ren Q, Jiao S, Cai Z, Geng X, Deng L, et al. Discovery of new and highly effective quadruple ffa1 and pparα/γ/δ agonists as potential anti-fatty liver agents. Eur J Med Chem. 2022;229:114061. doi: 10.1016/j.ejmech.2021.114061. [DOI] [PubMed] [Google Scholar]
- 147.Ratziu V, Harrison SA, Francque S, Bedossa P, Lehert P, Serfaty L, et al. Elafibranor, an agonist of the peroxisome proliferator-activated receptor-α and -δ, induces resolution of nonalcoholic steatohepatitis without fibrosis worsening. Gastroenterology. 2016;150(5):1147–1159.e1145. doi: 10.1053/j.gastro.2016.01.038. [DOI] [PubMed] [Google Scholar]
- 148.Francque SM, Bedossa P, Ratziu V, Anstee QM, Bugianesi E, Sanyal AJ, et al. A randomized, controlled trial of the pan-ppar agonist lanifibranor in nash. N Engl J Med. 2021;385(17):1547–1558. doi: 10.1056/NEJMoa2036205. [DOI] [PubMed] [Google Scholar]
- 149.Gawrieh S, Noureddin M, Loo N, Mohseni R, Awasty V, Cusi K, et al. Saroglitazar, a ppar-α/γ agonist, for treatment of nafld: A randomized controlled double-blind phase 2 trial. Hepatology. 2021;74(4):1809–1824. doi: 10.1002/hep.31843. [DOI] [PubMed] [Google Scholar]
- 150.Siddiqui MS, Idowu MO, Parmar D, Borg BB, Denham D, Loo NM, et al. A phase 2 double blinded, randomized controlled trial of saroglitazar in patients with nonalcoholic steatohepatitis. Clin Gastroenterol Hepatol. 2021;19(12):2670–2672. doi: 10.1016/j.cgh.2020.10.051. [DOI] [PubMed] [Google Scholar]
- 151.Chianelli D, Rucker PV, Roland J, Tully DC, Nelson J, Liu X, et al. Nidufexor (lmb763), a novel fxr modulator for the treatment of nonalcoholic steatohepatitis. J Med Chem. 2020;63(8):3868–3880. doi: 10.1021/acs.jmedchem.9b01621. [DOI] [PubMed] [Google Scholar]
- 152.Patel K, Harrison SA, Elkhashab M, Trotter JF, Herring R, Rojter SE, et al. Cilofexor, a nonsteroidal fxr agonist, in patients with noncirrhotic nash: A phase 2 randomized controlled trial. Hepatology. 2020;72(1):58–71. doi: 10.1002/hep.31205. [DOI] [PubMed] [Google Scholar]
- 153.Ratziu V, Rinella ME, Neuschwander-Tetri BA, Lawitz E, Denham D, Kayali Z, et al. Edp-305 in patients with nash: A phase ii double-blind placebo-controlled dose-ranging study. J Hepatol. 2022;76(3):506–517. doi: 10.1016/j.jhep.2021.10.018. [DOI] [PubMed] [Google Scholar]
- 154.Qin T, Gao X, Lei L, Zhang W, Feng J, Wang X, et al. Structural optimization and biological evaluation of 1-adamantylcarbonyl-4-phenylpiperazine derivatives as fxr agonists for nafld. Eur J Med Chem. 2023;245(Pt 1):114903. doi: 10.1016/j.ejmech.2022.114903. [DOI] [PubMed] [Google Scholar]
- 155.Li J, Liu M, Li Y, Sun DD, Shu Z, Tan Q, et al. Discovery and optimization of non-bile acid fxr agonists as preclinical candidates for the treatment of nonalcoholic steatohepatitis. J Med Chem. 2020;63(21):12748–12772. doi: 10.1021/acs.jmedchem.0c01065. [DOI] [PubMed] [Google Scholar]
- 156.Harrison SA, Bashir MR, Lee KJ, Shim-Lopez J, Lee J, Wagner B, et al. A structurally optimized fxr agonist, met409, reduced liver fat content over 12 weeks in patients with non-alcoholic steatohepatitis. J Hepatol. 2021;75(1):25–33. doi: 10.1016/j.jhep.2021.01.047. [DOI] [PubMed] [Google Scholar]
- 157.Shim S, Krishnaiah M, Sankham MR, Kim I, Lee Y, Shin I, et al. Discovery of (e)-3-(3-((2-cyano-4′-dimethylaminobiphenyl-4-ylmethyl)cyclohexanecarbonylamino)-5-fluorophenyl)acrylic acid methyl ester, an intestine-specific, fxr partial agonist for the treatment of nonalcoholic steatohepatitis. J Med Chem. 2022;65(14):9974–10000. doi: 10.1021/acs.jmedchem.2c00641. [DOI] [PubMed] [Google Scholar]
- 158.Nara SJ, Jogi S, Cheruku S, Kandhasamy S, Jaipuri F, Kathi PK, et al. Discovery of bms-986339, a pharmacologically differentiated farnesoid x receptor agonist for the treatment of nonalcoholic steatohepatitis. J Med Chem. 2022;65(13):8948–8960. doi: 10.1021/acs.jmedchem.2c00165. [DOI] [PubMed] [Google Scholar]
- 159.Younis IR, Kirby BJ, Billin AN, Xiao D, Song Q, Watkins TR, et al. Pharmacokinetics, pharmacodynamics, safety and tolerability of cilofexor, a novel nonsteroidal farnesoid x receptor agonist, in healthy volunteers. Clin Transl Sci. 2023;16(3):536–547. doi: 10.1111/cts.13469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Mudaliar S, Henry RR, Sanyal AJ, Morrow L, Marschall HU, Kipnes M, et al. Efficacy and safety of the farnesoid x receptor agonist obeticholic acid in patients with type 2 diabetes and nonalcoholic fatty liver disease. Gastroenterology. 2013;145(3):574–582.e571. doi: 10.1053/j.gastro.2013.05.042. [DOI] [PubMed] [Google Scholar]
- 161.Sanyal AJ, Lopez P, Lawitz EJ, Lucas KJ, Loeffler J, Kim W, et al. Tropifexor for nonalcoholic steatohepatitis: An adaptive, randomized, placebo-controlled phase 2a/b trial. Nat Med. 2023;29(2):392–400. doi: 10.1038/s41591-022-02200-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Ratziu V, Harrison SA, Loustaud-Ratti V, Bureau C, Lawitz E, Abdelmalek M, et al. Hepatic and renal improvements with fxr agonist vonafexor in individuals with suspected fibrotic nash. J Hepatol. 2023;78(3):479–492. doi: 10.1016/j.jhep.2022.10.023. [DOI] [PubMed] [Google Scholar]
- 163.Ran LS, Wu YZ, Gan YW, Wang HL, Wu LJ, Zheng CM, et al. Andrographolide ameliorates hepatic steatosis by suppressing fatp2-mediated fatty acid uptake in mice with nonalcoholic fatty liver disease. J Nat Med. 2023;77(1):73–86. doi: 10.1007/s11418-022-01647-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Li P, Zhang R, Wang M, Chen Y, Chen Z, Ke X, et al. Baicalein prevents fructose-induced hepatic steatosis in rats: In the regulation of fatty acid de novo synthesis, fatty acid elongation and fatty acid oxidation. Front Pharmacol. 2022;13:917329. doi: 10.3389/fphar.2022.917329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Sun W, Liu P, Wang T, Wang X, Zheng W, Li J. Baicalein reduces hepatic fat accumulation by activating ampk in oleic acid-induced hepg2 cells and high-fat diet-induced non-insulin-resistant mice. Food Funct. 2020;11(1):711–721. doi: 10.1039/c9fo02237f. [DOI] [PubMed] [Google Scholar]
- 166.Li QP, Dou YX, Huang ZW, Chen HB, Li YC, Chen JN, et al. Therapeutic effect of oxyberberine on obese non-alcoholic fatty liver disease rats. Phytomedicine. 2021;85:153550. doi: 10.1016/j.phymed.2021.153550. [DOI] [PubMed] [Google Scholar]
- 167.Shan MY, Dai Y, Ren XD, Zheng J, Zhang KB, Chen B, et al. Berberine mitigates nonalcoholic hepatic steatosis by downregulating sirt1-foxo1-srebp2 pathway for cholesterol synthesis. J Integr Med. 2021;19(6):545–554. doi: 10.1016/j.joim.2021.09.003. [DOI] [PubMed] [Google Scholar]
- 168.Sharma A, Anand SK, Singh N, Dwarkanath A, Dwivedi UN, Kakkar P. Berbamine induced activation of the sirt1/lkb1/ampk signaling axis attenuates the development of hepatic steatosis in high-fat diet-induced nafld rats. Food Funct. 2021;12(2):892–909. doi: 10.1039/d0fo02501a. [DOI] [PubMed] [Google Scholar]
- 169.Yu M, Alimujiang M, Hu L, Liu F, Bao Y, Yin J. Berberine alleviates lipid metabolism disorders via inhibition of mitochondrial complex i in gut and liver. Int J Biol Sci. 2021;17(7):1693–1707. doi: 10.7150/ijbs.54604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Zhang YP, Deng YJ, Tang KR, Chen RS, Liang S, Liang YJ, et al. Berberine ameliorates high-fat diet-induced non-alcoholic fatty liver disease in rats via activation of sirt3/ampk/acc pathway. Curr Med Sci. 2019;39(1):37–43. doi: 10.1007/s11596-019-1997-3. [DOI] [PubMed] [Google Scholar]
- 171.Lee M, Nam SH, Yoon HG, Kim S, You Y, Choi KC, et al. Fermented curcuma longa l. Prevents alcoholic fatty liver disease in mice by regulating cyp2e1, srebp-1c, and ppar-α. J Med Food. 2022;25(4):456–463. doi: 10.1089/jmf.2021.K.0098. [DOI] [PubMed] [Google Scholar]
- 172.Mun J, Kim S, Yoon HG, You Y, Kim OK, Choi KC, et al. Water extract of curcuma longa l. Ameliorates non-alcoholic fatty liver disease. Nutrients. 2019;11(10):2536. doi: 10.3390/nu11102536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Sun Q, Niu Q, Guo Y, Zhuang Y, Li X, Liu J, et al. Regulation on citrate influx and metabolism through inhibiting slc13a5 and acly: A novel mechanism mediating the therapeutic effects of curcumin on nafld. J Agric Food Chem. 2021;69(31):8714–8725. doi: 10.1021/acs.jafc.1c03105. [DOI] [PubMed] [Google Scholar]
- 174.Poornima MS, Sindhu G, Billu A, Sruthi CR, Nisha P, Gogoi P, et al. Pretreatment of hydroethanolic extract of dillenia indica l. Attenuates oleic acid induced nafld in hepg2 cells via modulating sirt-1/p-lkb-1/ampk, hmgcr & ppar-α signaling pathways. J Ethnopharmacol. 2022;292:115237. doi: 10.1016/j.jep.2022.115237. [DOI] [PubMed] [Google Scholar]
- 175.Le TNH, Choi HJ, Jun HS. Ethanol extract of liriope platyphylla root attenuates non-alcoholic fatty liver disease in high-fat diet-induced obese mice via regulation of lipogenesis and lipid uptake. Nutrients. 2021;13(10):3338. doi: 10.3390/nu13103338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Ma K, Sheng W, Gao R, Feng J, Huang W, Cui L, et al. Ethanolic extract of root from arctium lappa l ameliorates obesity and hepatic steatosis in rats by regulating the ampk/acc/cpt-1 pathway. J Food Biochem. 2022;46(12):e14455. doi: 10.1111/jfbc.14455. [DOI] [PubMed] [Google Scholar]
- 177.Liu W, Shang J, Deng Y, Han X, Chen Y, Wang S, et al. Network pharmacology analysis on mechanism of jian pi qing gan yin decoction ameliorating high fat diet-induced non-alcoholic fatty liver disease and validated in vivo. J Ethnopharmacol. 2022;295:115382. doi: 10.1016/j.jep.2022.115382. [DOI] [PubMed] [Google Scholar]
- 178.Zhang J, Du H, Shen M, Zhao Z, Ye X. Kangtaizhi granule alleviated nonalcoholic fatty liver disease in high-fat diet-fed rats and hepg2 cells via ampk/mtor signaling pathway. J Immunol Res. 2020;2020:3413186. doi: 10.1155/2020/3413186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Li Y, Yang M, Lin H, Yan W, Deng G, Ye H, et al. Limonin alleviates non-alcoholic fatty liver disease by reducing lipid accumulation, suppressing inflammation and oxidative stress. Front Pharmacol. 2021;12:801730. doi: 10.3389/fphar.2021.801730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Wang SW, Lan T, Chen HF, Sheng H, Xu CY, Xu LF, et al. Limonin, an ampk activator, inhibits hepatic lipid accumulation in high fat diet fed mice. Front Pharmacol. 2022;13:833705. doi: 10.3389/fphar.2022.833705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Yang Y, Wu Y, Zou J, Wang YH, Xu MX, Huang W, et al. Naringenin attenuates non-alcoholic fatty liver disease by enhancing energy expenditure and regulating autophagy via ampk. Front Pharmacol. 2021;12:687095. doi: 10.3389/fphar.2021.687095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Hao R, Shan S, Yang D, Zhang H, Sun Y, Li Z. Peonidin-3-o-glucoside from purple corncob ameliorates nonalcoholic fatty liver disease by regulating mitochondrial and lysosome functions to reduce oxidative stress and inflammation. Nutrients. 2023;15(2):372. doi: 10.3390/nu15020372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Li YC, Qiao JY, Wang BY, Bai M, Shen JD, Cheng YX. Paeoniflorin ameliorates fructose-induced insulin resistance and hepatic steatosis by activating lkb1/ampk and akt pathways. Nutrients. 2018;10(8):1024. doi: 10.3390/nu10081024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Pham TH, Lee GH, Jin SW, Lee SY, Han EH, Kim ND, et al. Puerarin attenuates hepatic steatosis via g-protein-coupled estrogen receptor-mediated calcium and sirt1 signaling pathways. Phytother Res. 2022;36(9):3601–3618. doi: 10.1002/ptr.7526. [DOI] [PubMed] [Google Scholar]
- 185.Zhou J, Zhang N, Aldhahrani A, Soliman MM, Zhang L, Zhou F. Puerarin ameliorates nonalcoholic fatty liver in rats by regulating hepatic lipid accumulation, oxidative stress, and inflammation. Front Immunol. 2022;13:956688. doi: 10.3389/fimmu.2022.956688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Gu Y, Duan S, Ding M, Zheng Q, Fan G, Li X, et al. Saikosaponin d attenuates metabolic associated fatty liver disease by coordinately tuning pparα and insig/srebp1c pathway. Phytomedicine. 2022;103:154219. doi: 10.1016/j.phymed.2022.154219. [DOI] [PubMed] [Google Scholar]
- 187.Li X, Ge J, Li Y, Cai Y, Zheng Q, Huang N, et al. Integrative lipidomic and transcriptomic study unravels the therapeutic effects of saikosaponins a and d on non-alcoholic fatty liver disease. Acta Pharm Sin B. 2021;11(11):3527–3541. doi: 10.1016/j.apsb.2021.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]