Abstract
Fibrous dysplasia (FD) is a mosaic skeletal disorder involving the development of benign, expansile fibro-osseous lesions during childhood that cause deformity, fractures, pain, and disability. There are no well-established treatments for FD. Fibroblast activation protein (FAPα) is a serine protease expressed in pathological fibrotic tissues that has promising clinical applications as a biomarker and local pro-drug activator in several pathological conditions. In this study, we explored the expression of FAP in FD tissue and cells through published genetic expression datasets and measured circulating FAPα in plasma samples from patients with FD and healthy donors. We found that FAP genetic expression was increased in FD tissue and cells, and present at higher concentrations in plasma from patients with FD compared to healthy donors. Moreover, FAPα levels were correlated with skeletal disease burden in patients with FD. These findings support further investigation of FAPα as a potential imaging and/or biomarker of FD, as well as a pro-drug activator specific to FD tissue.
Keywords: fibrous dysplasia, fibroblast activation protein, biomarker, protease
1. Introduction
Fibrous dysplasia (FD) is a mosaic skeletal disorder arising from acquired activating variants in GNAS in skeletal stem cells during embryogenesis. When extra-skeletal tissues are also affected, it is called McCune-Albright Syndrome (MAS, OMIM #174800). FD results in the development of benign expansile fibro-osseous lesions in the skeleton during childhood, leading to deformity, fractures, pain, and disability. As with most mosaic disorders, the disease burden is highly variable, ranging from one single lesion (monostotic FD) to the involvement of large portions of the skeleton (polyostotic FD). The histopathology of FD lesions is characterized by the replacement of normal bone and marrow tissue by fibrous tissue mixed with curvilinear trabeculae of poorly mineralized and hypercellular woven bone. FD fibroblasts are highly proliferative abnormal bone marrow stromal cells (BMSCs). These cellular changes are caused by the expression of hyper-signaling Gαs, which produces increased intracellular cyclic adenosine monophosphate (cAMP), leading to the abnormal differentiation and increased proliferation of BMSCs.
There are no well-established treatments for FD. FD BMSCs produce large amounts of RANKL, promoting the local differentiation and activation of osteoclasts, which in turn contribute to FD BMSC proliferation in a positive feedback loop [1]. Treatment with the anti-RANKL monoclonal antibody denosumab, which dramatically inhibits osteoclastogenesis, has shown promising therapeutic effects in a clinical trial [2]. But denosumab does not discriminate between affected and unaffected skeletal tissue, decreasing osteoclastogenesis in the complete skeleton. Osteoclasts are necessary for bone homeostasis, so in principle this therapy should eventually be discontinued to allow normal bone modelling and remodeling to resume. This is especially true for children, who are also the main beneficiaries of FD therapy, but need osteoclasts for appropriate skeletal development. Denosumab discontinuation leads to disease rebound and can cause severe hypercalcemia due to the rapid reactivation of osteoclastogenesis [2,3]. In addition to denosumab, small molecules that specifically target activated Gαs variants are being investigated, but most of the molecules identified also have inhibitory action towards wildtype Gαs [4]. Since FD is a mosaic disease, treatments that specifically target lesional tissue would greatly improve these and other possible treatment drawbacks. Research that focuses on the development of pro-drugs which are activated only within FD lesions may be an answer.
Fibroblast activation protein (FAPα) is a membrane-bound serine protease involved in extracellular matrix degradation. It was originally identified within the stroma of solid tumors, expressed by carcinoma-associated fibroblasts [5]. It can be naturally cleaved and released into the circulation, and since its expression is relatively restricted to fibrotic pathological processes, it has the potential to be utilized as both a circulating biomarker and therapeutic target in an array of diseases involving fibrosis and inflammation [6]. Small molecules and monoclonal antibodies capable of targeting and inhibiting FAPα were developed for cancer treatment. However, they failed to significantly improve disease progression in clinical trials to justify further research on their use as antitumor agents [7,8,9]. Nevertheless, more recent literature has shown that radiolabeled FAPα inhibitors (68Ga-FAPI and 18F-FAPI) can be effective when used as medical imaging pan-tumoral radiotracers in solid tumors [10,11]. FAPα is also a promising pro-drug activating agent for engineered drugs [12,13,14] as it has both proteolytic cleavage site specificity [15], and expression that is relatively confined to pathological fibrotic tissue.
This work follows our recent publication that screened released factors by FD BMSCs that may have therapeutic or diagnostic interest [16]. Here, we report that patients with FD have increased blood FAPα levels compared to healthy donors (HDs), and that there is a clear association of these levels with their disease burden. In addition, we collected and integrated FAP gene expression levels reported in previous publications and publicly available FD-related mRNA expression data published by us, and others. In this search, we found increased FAP mRNA levels in murine FD tissue and cells, as well as in patient-derived FD cells when compared to HDs. We did not observe significant expression changes in human BMSCs engineered to express GαsR201C. Lastly, we report that anti-RANKL therapy decreased FAP expression in human and murine FD tissue.
2. Material and Methods
2.1. Literature Search
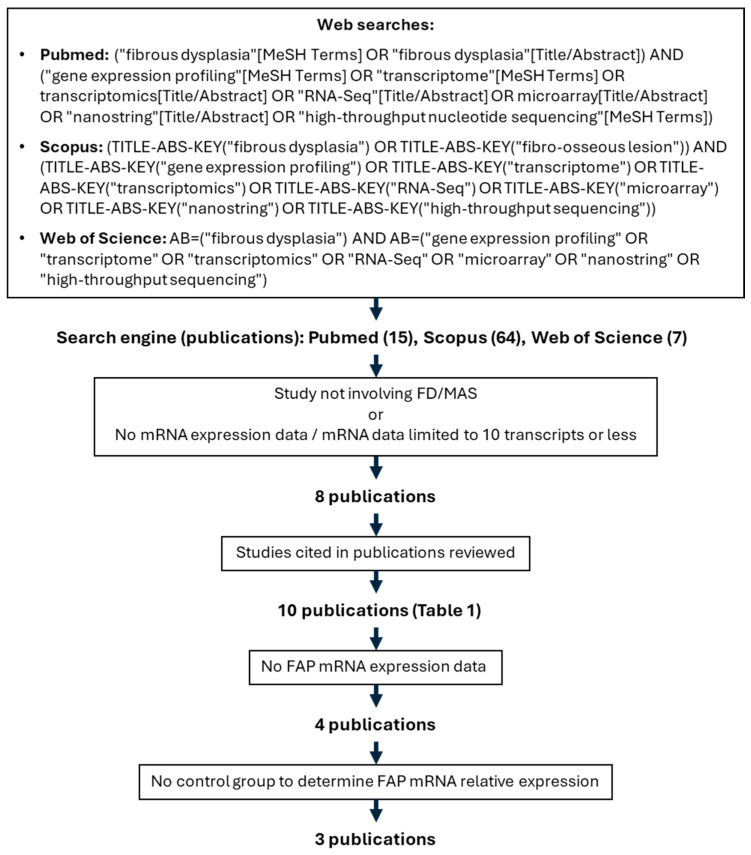
Independent searches and literature reviews were conducted by LNR, ZM and LFdC between 6th August and 9th 2024, following the workflow in Figure 1, which resulted in 10 publications reviewed for FAP expression (Table 1). The full list of articles identified by these searches is included as Supplementary File S1.
Figure 1.
Flow chart showing search terms and inclusion criteria for FAP mRNA relative expression analysis.
Table 1.
Datasets reviewed for FAP expression.
| Study [Ref] | Sample Type | GEO Accession |
mRNA Expression Technique |
FAP Expression Measured? |
FAP Upregulation |
|---|---|---|---|---|---|
| Kim, HY, 2024 [17] | Single cells from FD tissue | GSE263294 | scRNAseq | Yes (scRNAseq) | N/A, no control group |
| Kim, HY, 2024 [17] | FD BSMC vs. normal BMSC-derived organoids (culture) | Not submitted | qPCR | No | N/A |
| Michel Z, 2024 [16] | Human FD and HD BMSCs | GSE261360 | RNAseq | Yes | Yes, FD vs. HD BMSCs |
| Michel Z, 2024 [16] | Mouse BMSCs induced or not to express GαsR201C | GSE261360 | RNAseq | Yes | No |
| De Castro LF, 2023 [1] | Human FD tissue before and after denosumab treatment | GSE250357 | RNAseq | Yes | Yes, FD vs. denosumab-treated FD |
| De Castro LF, 2023 [1] | Mouse FD tissue with or without anti-RANKL treatment and same site control bone | GSE250357 | RNAseq | Yes | Yes, FD vs. anti-RANKL-treated FD and vs. control bone |
| Persichetti, 2021 [18] | FD biopsies | GSE176243 | Nanostring | No | N/A |
| Raimondo D, 2020 [19] | Human BMSC expressing GαsR201C by lentiviral transduction | GSE109818 | Microarray | Yes | No |
| Onodera S, 2020 [20] | GNAS p.R201H iPSC vs. WT iPSC | Not submitted | qPCR | No | N/A |
| Zhou S-H, 2014 [21] | Human FD tissue vs. normal bone | Not submitted | Microarray | No | N/A |
| Piersanti S, 2010 [22] | Human BMSC expressing GαsR201C by lentiviral transduction | Not submitted | qPCR | No | N/A |
| Kiss J, 2010 [23] | FD affected women’s tissue vs. control women’s bone | Not submitted | qPCR | No | N/A |
| Lee C-H, 2008 [24] | FD biopsies vs. GCT and ABC biopsies | Not submitted | Microarray | Unk * | Unk |
Abbreviations: FD = Fibrous dysplasia, N/A = Not applicable, BMSC = Bone marrow stromal cells, HD = Healthy donor, FAP = Fibroblast activation protein, scRNAseq = Single cell RNA sequencing, RANKL = Receptor activator of nuclear factor kappa-Β ligand, iPSC = Induced pluripotent stem cell, GCT = Giant cell tumor, ABC = Aneurysmal bone cyst, Unk = Unknown. * Assessed gene list not available in the publication or its references, FAP was not reported as a differentially expressed gene in any of the sample groups assessed.
2.2. Human Specimens
Forty-seven adult patients with FD were evaluated at the NIH Clinical Center as part of a longstanding natural history protocol (NIH 98-D-0145, NCT00001727 in www.clinicaltrials.gov). The study was approved by the NIDCR Institutional Review Board and all subjects gave informed consent/assent. FD disease burden was calculated using a validated method (Skeletal Burden Score [SBS]) [16]. This study includes patients undergoing treatment with bisphosphonates, and those who paused therapy for more than a year before donating blood for this study, who were considered off-drug (Table 2). Serum samples from 22 HDs were purchased (Valley Biomedical, Winchester, VA, USA) and donors were considered to have SBS = 0. The demographic information of both subject groups is reported in Table 2 and individual values are available in Supplementary File S2.
Table 2.
Demographic data of plasma donors.
| Fibrous Dysplasia (FD) Patients | Healthy Donors (HDs) | |
|---|---|---|
| Subjects—n | 47 | 22 |
| Females—n (%) | 30 (63.8%) | 8 (36.4%) |
| Age—mean ± SD (range) | 33 ± 13 (18–71) | 42 ± 15 (18–70) |
| FD burden—mean ± SD (range) | 37 ± 23 (2.8–75) | 0 |
| Currently on bisphosphonates—n (%) | 10 (21%) | 0 |
| Any endocrinopathy—n (%) | 35 (74%) | 0 |
2.3. FAPα Determination
An FAPα Human ELISA Kit with a sensitivity of 12 pg/mL and range of 12–4000 pg/mL was purchased from Abcam (Cambridge, UK, catalog number ab193701) and used to measure FAPα in plasma samples according to the manufacturer’s instructions. Plasma samples were diluted 200-fold prior to ELISA assay as recommended by the manufacturer.
2.4. FAP/Fap mRNA Expression Level Analyses
Expression data from publicly available datasets was obtained from NCBI GEO repository (Table 1) and differential expression of FAP between sample groups was calculated. The methods for the obtention and characteristics of these samples are described in their corresponding publications.
2.5. Statistical Analysis
Statistical analysis of data in Figure 2 is described in their respective publications. For plasmatic FAPα levels and SBS data we used GraphPad Prism 9.00 (GraphPad Software, Inc., La Jolla, CA, USA), and conducted group comparisons using unpaired, two-tailed t-test after evaluating normality with the D’Agostino-Pearson test. Spearman correlation was calculated for plasmatic FAPα levels and SBS. For these analyses, SBS in HDs was considered 0. A linear regression of plasmatic FAPα determinations and SBS was also performed.
Figure 2.
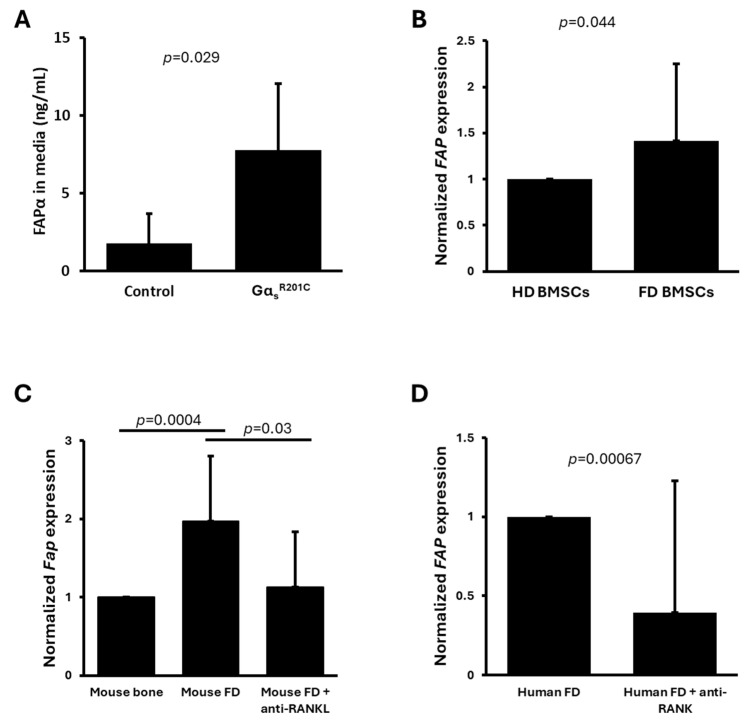
FAPα is produced by altered bone marrow stromal cells (BMSCs) in fibrous dysplasia (FD) tissue, and its expression is normalized with anti-RANKL therapy. Data retrieved and adapted from published studies and genetic expression datasets [1,16]. (A) FAPα is secreted by mouse BMSCs cultures induced to express FD-causing GαsR201C (n = 5/group) [16]. (B) FAP expression is upregulated in patient-derived FD BMSC compared to healthy volunteers (HD) BMSCs (n = 4/group) [16]. (C) Fap expression is upregulated in mouse FD lesions compared to healthy littermate bone tissue, and anti-RANKL therapy normalizes its expression (n = 6 WT mice, 5 FD mice, 6 anti-RANKL-treated FD mice) [25]. (D) FAP expression is downregulated in human FD tissue after anti-RANKL therapy with denosumab (n = 6) [25]. Data is presented as averages and standard deviation in (A) and average and standard error in (B,C).
3. Results
The literature search for high throughput mRNA expression analyses of FD tissue and cultured FD cells resulted in 10 publications. Of these, five were excluded, as their analysis did not include FAP. One study did not report FAP as a gene modulated in any of the pathologies assessed and did not provide a list of genes measured [24]. One study included FAP expression in single-cell RNAseq from three FD tissue samples, but did not report differential expression in comparison to normal cells, and thus was excluded [17] (Figure 1, Table 1). Three publications measured FAP expression as part of high throughput mRNA datasets. One of these three studies is our previously reported article in which we also demonstrated increased secretion of FAPα protein into the culture media of BMSCs derived from a doxycycline-inducible FD mouse model [16]. This data has been reproduced again in Figure 2A. In this study, bone marrow was plated, cleared from hematopoietic cells by negative immunoselection of CD45+ cells to enrich BMSCs, and split in 6-well plates. Some wells were induced in vitro to express GαsR201C by adding doxycycline in the media, and media levels of FAPα were measured, showing a 4.4-fold increase in GαsR201C-expressing cultures compared to uninduced cultures. However, no significant differences were found at the mRNA expression level in these cultures 48 h after initiating GαsR201C expression induction. In the same study, using human cells, media FAPα levels did not show a significant difference between FD and HD BMSCs. However, measurements of additional well-known disease-associated factors in these samples also failed to show significant differences to control cultures, likely due to the high variability involved in the study of human samples from multiple donors, as discussed in the publication [16]. However, these human cultures showed a significant increase in FAP mRNA expression (Figure 2B). On the other hand, analyses from an additional mRNA expression dataset of human BMSCs engineered by lentiviral transduction to express GαsR201C showed no changes in the expression levels of FAP [19].
In a different study we published [1,25], FD lesions were induced by the conditional expression of GαsR201C in the appendicular skeleton of mice. RNAseq relative expression analysis of the lesions in comparison to normal bone also showed a significant increase in Fap expression, which was partially normalized after four weeks of anti-RANKL therapy (Figure 2C). In the same publication, human FD biopsies from a Phase 1 clinical trial obtained before and after denosumab (anti-RANKL monoclonal antibody) treatment showed reduced expression of FAP after six months of denosumab therapy (Figure 2D).
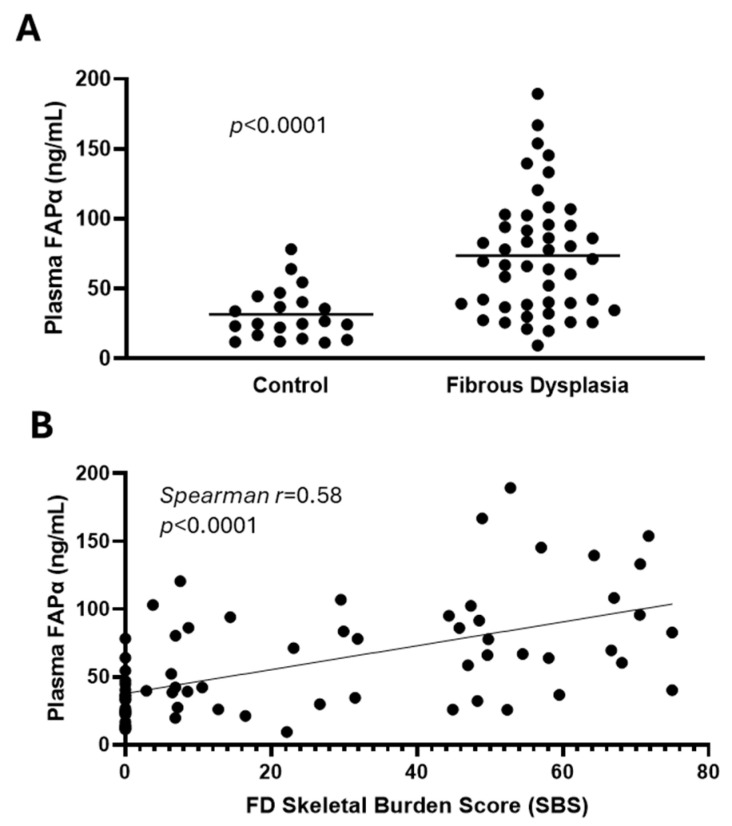
With this preliminary evidence, we explored the role of FAPα as a biochemical biomarker of FD, comparing its blood levels in 47 patients with FD to that of 22 healthy donors (Table 1). FD patients showed plasmatic FAPα levels more than twice as high as healthy donors (Figure 3A), which was strongly correlated with FD disease burden (Figure 3B).
Figure 3.
Circulating FAPα concentration is significantly higher in plasma from fibrous dysplasia (FD) patients than from the plasma of healthy donors (HD) and is associated with their disease burden. (A) Level of FAPα in plasma from FD patients compared to HD. (B) Correlation of FAPα with skeletal disease burden score of FD patients. HDs were considered to have a score of zero (absence of disease). The line represents linear regression.
4. Discussion
The evidence reported here demonstrates that FAP has increased expression in FD tissue, and more specifically, in abnormal FD BMSCs. Given its expression as a defining characteristic of pathological fibrosis, its potential as a pro-drug cleaving activator, and the availability of FAPα-targeting drugs with good tolerability in humans [7,8], FAPα has attracted the attention of researchers across disciplines studying disorders involving fibrosis. This positions FAPα as an interesting translational research candidate in FD, with potential to improve diagnosis and treatment.
FAPα may be useful in the imaging realm of disease workup, however, additional studies are needed to show its performance compared to the current standard. Radiolabeled FAPα inhibitors (68Ga-FAPI and 18F-FAPI) imaging by PET/CT have shown efficacy in labeling a wide range of solid carcinomas via interactions with cancer-associated fibroblasts [10,11], and may improve lesional localization and activity measurement in FD. Two bone-avid molecules, 99m-technetium-methylene diphosphonate (99mTc-MDP) and more recently 18F-NaF [25] effectively demarcate skeletal FD lesions and are essential in determining disease burden and guiding patient treatment plans. In addition, 18F-NaF (and not 99mTc-MDP) accurately captures lesion activity through analysis of local standard uptake values (SUV) which can be used as a measurement of lesion improvement [2]. However, considering that their mechanism of action involves integration with mineralized tissue, it is unclear if these radiotracers have the capacity to target FD lesions with low or absent mineral content. In contrast, radiolabeled FAPα inhibitors may offer visualization for non-skeletal lesions in FD/MAS, i.e., intramuscular myxomas, or others that remain to be characterized [26]. Indeed, 18F-FAPI PET/CT has already been tested on a patient with FD [27] and it showed increased uptake in lesional tissue compared to 18F-Fludeoxyglucose, which is a poor radiotracer for FD. Comparative studies imaging the same patients using 18F-FAPI and 18F-NaF PET/CT, the current standard, are necessary to better understand the way these radiotracers perform in FD.
FAPα may also be useful as a biomarker. We demonstrated a correlation of FAPα circulating levels and disease burden that is as strong as other well-known FD biomarkers such as RANKL, the bone turnover markers alkaline phosphatase (ALP), osteocalcin, C-terminal telopeptide of type I collagen (CTX-I), and N-terminal pro-peptide of type I procollagen (PINP) [16]. Importantly, while bone turnover markers are associated with virtually all skeletal pathologies, FAPα is highly specific for fibrotic tissue. Including FAPα with bone turnover markers in FD diagnostic blood panels could provide both diagnostic and prognostic insights for FD. Studies of FAPα in additional cohorts of FD patients may confirm our observations.
FAPα has a relatively specific cleavage substrate that can be engineered as a pro-drug lock, targeting activation in FAP-expressing diseased tissue. Pharmacologic research has recently focused on tethering drugs to locking peptides, which allows their local activation in target tissues [28]. This can be particularly beneficial in mosaic diseases which involve variable regions of the body, rather than full organs or systems. FD’s unique fibro-osseous histology shows production and rapid remodeling of large amounts of extracellular matrix in which FAP is distinctively expressed. In addition, FAPα has a relatively specific substrate cleavage site, allowing it to be recognized and cleaved by engineered drugs. Several proof of principle study assays have been carried out to explore the capacity of FAPα as a local pro-drug activator of engineered cytotoxic pro-drugs for cancer treatment, including the combination with photoactivation in peptide-locked photosensitizers [12,13,14]. In addition, MMP2 is another protease highly expressed in FD BMSCs [16,19,25,29]. However, it is more broadly expressed in non-pathological tissues and its target cleavage site overlaps with those of other metalloproteases. Nevertheless, an anti-TNFα antibody locked with a peptide cleavable by MMP2/9 showed therapeutic effects equivalent to unmodified anti-TNFα in a mouse model of rheumatoid arthritis, but animals treated with MMP2/9 activable pro-drug lacked the systemic immunodepression secondary effects that animals receiving the unmodified antibody showed [29]. Denosumab is an anti-osteoclastic, RANKL-neutralizing antibody with demonstrated efficacy for FD treatment. However, it leads to a systemic abrogation of osteoclasts, which are necessary for bone growth and turnover. This obliges treatment discontinuation, which in turn generates a rapid rebound of resorption activity and associated co-morbidities such as acute hypercalcemia and FD lesion reactivation. With these considerations, creating a denosumab-like monoclonal antibody with a FAPα-cleavable peptide that only activates in FAP-expressing FD lesions could allow sustained therapy by eliminating off-target effects and potentially promote local reactivation of normal bone turnover as lesions normalize their cellular composition and reduce FAP expression.
5. Conclusions
FAPα is a serine protease specifically expressed in FD that has potential to be used as a disease biomarker in blood biochemical tests and medical imaging. Its relatively specific target cleavage sequence makes it a promising candidate as a local pro-drug activator in FD lesions. This exploratory study may open novel translational research avenues to test the clinical applications enabled by FAPα in FD.
Acknowledgments
We thank Rebeca Galisteo for her continuous support in the laboratory.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/cells13171434/s1, File S1: Search terms and results for the publications reviewed for high throughput mRNA expression data of FD cells and tissue; File S2: Individual data of patients with FD and healthy donors for SBS, plasmatic FAPα levels, sex, age, presence of endocrinopathies and ongoing bisphosphonate treatment.
Author Contributions
Conceptualization, L.F.d.C.; methodology, Z.M., L.N.R. and L.F.d.C.; validation, Z.M., L.N.R. and L.F.d.C.; formal analysis, L.N.R., Z.M. and L.F.d.C.; investigation, L.N.R., Z.M. and L.F.d.C.; resources, M.T.C. and A.M.B.; data curation, L.N.R., Z.M., A.M.B. and L.F.d.C.; writing—original draft preparation, L.F.d.C.; writing—review and editing, L.N.R., Z.M., M.T.C., A.M.B. and L.F.d.C.; visualization, L.F.d.C.; supervision, A.M.B. and L.F.d.C.; project administration, A.M.B. and L.F.d.C.; funding acquisition, M.T.C. and A.M.B. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of the National Institutes of Health (98D0145/MODCR000783).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Literature search results are available in Supplementary File S1. GEO gene expression datasets reviewed on 6 to 9 August 2024 for the publications in Table 1 are indicated in the GEO accession column and can be accessed at https://www.ncbi.nlm.nih.gov/geo/, accessed on 9 August 2024. Data reproduced in Figure 2 has been adapted from previous publications [1,16]. Data in Figure 3 and Table 2 is available in Supplementary File S2.
Conflicts of Interest
Although the NIH Medical Research Scholars Program, which provided a stipend for LNR while carrying out this study, was in part funded by the Foundation for the NIH from the Doris Duke Charitable Foundation, Genentech, the American Association for Dental Research, the Colgate-Palmolive Company, and other private donors, the funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Funding Statement
This research was supported by the Division of Intramural Research, NIDCR via the Intramural Research Program of the National Institutes of Health, Department of Health and Human Services (ZIA DE000649, ZIADE000758). This research was also made possible through the NIH Medical Research Scholars Program, a public–private partnership supported jointly by the NIH and contributions to the Foundation for the NIH from the Doris Duke Charitable Foundation, Genentech, the American Association for Dental Research, the Colgate-Palmolive Company, and other private donors.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.de Castro L.F., Whitlock J.M., Michel Z., Pan K., Taylor J., Szymczuk V., Boyce B., Martin D., Kram V., Galisteo R., et al. RANKL inhibition reduces lesional cellularity and Gαs variant expression and enables osteogenic maturation in fibrous dysplasia. Bone Res. 2024;12:10. doi: 10.1038/s41413-023-00311-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Castro L.F., Michel Z., Pan K., Taylor J., Szymczuk V., Paravastu S., Saboury B., Papadakis G.Z., Li X., Milligan K., et al. Safety and Efficacy of Denosumab for Fibrous Dysplasia of Bone. N. Engl. J. Med. 2023;388:766–768. doi: 10.1056/NEJMc2214862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anastasilakis A.D., Makras P., Yavropoulou M.P., Tabacco G., Naciu A.M., Palermo A. Denosumab Discontinuation and the Rebound Phenomenon: A Narrative Review. J. Clin. Med. 2021;10:152. doi: 10.3390/jcm10010152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhattacharyya N., Hu X., Chen C.Z., Mathews Griner L.A., Zheng W., Inglese J., Austin C.P., Marugan J.J., Southall N., Neumann S., et al. A high throughput screening assay system for the identification of small molecule inhibitors of gsp. PLoS ONE. 2014;9:e90766. doi: 10.1371/journal.pone.0090766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scanlan M.J., Raj B.K., Calvo B., Garin-Chesa P., Sanz-Moncasi M.P., Healey J.H., Old L.J., Rettig W.J. Molecular cloning of fibroblast activation protein alpha, a member of the serine protease family selectively expressed in stromal fibroblasts of epithelial cancers. Proc. Natl. Acad. Sci. USA. 1994;91:5657–5661. doi: 10.1073/pnas.91.12.5657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yazbeck R., Jaenisch S.E., Abbott C.A. Potential disease biomarkers: Dipeptidyl peptidase 4 and fibroblast activation protein. Protoplasma. 2018;255:375–386. doi: 10.1007/s00709-017-1129-5. [DOI] [PubMed] [Google Scholar]
- 7.Hofheinz R.D., al-Batran S.E., Hartmann F., Hartung G., Jager D., Renner C., Tanswell P., Kunz U., Amelsberg A., Kuthan H., et al. Stromal antigen targeting by a humanised monoclonal antibody: An early phase II trial of sibrotuzumab in patients with metastatic colorectal cancer. Onkologie. 2003;26:44–48. doi: 10.1159/000069863. [DOI] [PubMed] [Google Scholar]
- 8.Nemunaitis J., Vukelja S.J., Richards D., Cunningham C., Senzer N., Nugent J., Duncan H., Jones B., Haltom E., Uprichard M.J. Phase I trial of PT-100 (PT-100), a cytokine-inducing small molecule, following chemotherapy for solid tumor malignancy. Cancer Investig. 2006;24:553–561. doi: 10.1080/07357900600894732. [DOI] [PubMed] [Google Scholar]
- 9.Narra K., Mullins S.R., Lee H.O., Strzemkowski-Brun B., Magalong K., Christiansen V.J., McKee P.A., Egleston B., Cohen S.J., Weiner L.M., et al. Phase II trial of single agent Val-boroPro (Talabostat) inhibiting Fibroblast Activation Protein in patients with metastatic colorectal cancer. Cancer Biol. Ther. 2007;6:1691–1699. doi: 10.4161/cbt.6.11.4874. [DOI] [PubMed] [Google Scholar]
- 10.Kratochwil C., Flechsig P., Lindner T., Abderrahim L., Altmann A., Mier W., Adeberg S., Rathke H., Rohrich M., Winter H., et al. (68)Ga-FAPI PET/CT: Tracer Uptake in 28 Different Kinds of Cancer. J. Nucl. Med. 2019;60:801–805. doi: 10.2967/jnumed.119.227967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mu X., Mo B., Qin J., Li Z., Chong W., Zeng Y., Lu L., Zhang L., Fu W. Comparative analysis of two timepoints on [(18)F]FAPI-42 PET/CT in various cancers. Eur. J. Hybrid Imaging. 2023;7:27. doi: 10.1186/s41824-023-00186-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Luo Y., Zeng Z., Shan T., Xu X., Chen J., He Y., Zhang T., Huang Z., Chai G., Huang Y., et al. Fibroblast activation protein alpha activatable theranostic pro-photosensitizer for accurate tumor imaging and highly-specific photodynamic therapy. Theranostics. 2022;12:3610–3627. doi: 10.7150/thno.70308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brennen W.N., Rosen D.M., Chaux A., Netto G.J., Isaacs J.T., Denmeade S.R. Pharmacokinetics and toxicology of a fibroblast activation protein (FAP)-activated prodrug in murine xenograft models of human cancer. Prostate. 2014;74:1308–1319. doi: 10.1002/pros.22847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chai X.P., Sun G.L., Fang Y.F., Hu L.H., Liu X., Zhang X.W. Tumor-targeting efficacy of a BF211 prodrug through hydrolysis by fibroblast activation protein-alpha. Acta Pharmacol. Sin. 2018;39:415–424. doi: 10.1038/aps.2017.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huang C.H., Suen C.S., Lin C.T., Chien C.H., Lee H.Y., Chung K.M., Tsai T.Y., Jiaang W.T., Hwang M.J., Chen X. Cleavage-site specificity of prolyl endopeptidase FAP investigated with a full-length protein substrate. J. Biochem. 2011;149:685–692. doi: 10.1093/jb/mvr017. [DOI] [PubMed] [Google Scholar]
- 16.Michel Z., Raborn L.N., Spencer T., Pan K.S., Martin D., Roszko K.L., Wang Y., Robey P.G., Collins M.T., Boyce A.M., et al. Transcriptomic Signature and Pro-Osteoclastic Secreted Factors of Abnormal Bone-Marrow Stromal Cells in Fibrous Dysplasia. Cells. 2024;13:774. doi: 10.3390/cells13090774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim H.Y., Charton C., Shim J.H., Lim S.Y., Kim J., Lee S., Ohn J.H., Kim B.K., Heo C.Y. Patient-Derived Organoids Recapitulate Pathological Intrinsic and Phenotypic Features of Fibrous Dysplasia. Cells. 2024;13:729. doi: 10.3390/cells13090729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Persichetti A., Milanetti E., Palmisano B., di Filippo A., Spica E., Donsante S., Coletta I., Venti M.D.S., Ippolito E., Corsi A., et al. Nanostring technology on Fibrous Dysplasia bone biopsies. A pilot study suggesting different histology-related molecular profiles. Bone Rep. 2022;16:101156. doi: 10.1016/j.bonr.2021.101156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Raimondo D., Remoli C., Astrologo L., Burla R., La Torre M., Verni F., Tagliafico E., Corsi A., Del Giudice S., Persichetti A., et al. Changes in gene expression in human skeletal stem cells transduced with constitutively active Gsalpha correlates with hallmark histopathological changes seen in fibrous dysplastic bone. PLoS ONE. 2020;15:e0227279. doi: 10.1371/journal.pone.0227279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Onodera S., Saito A., Hojo H., Nakamura T., Zujur D., Watanabe K., Morita N., Hasegawa D., Masaki H., Nakauchi H., et al. Hedgehog Activation Regulates Human Osteoblastogenesis. Stem Cell Rep. 2020;15:125–139. doi: 10.1016/j.stemcr.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhou S.H., Yang W.J., Liu S.W., Li J., Zhang C.Y., Zhu Y., Zhang C.P. Gene expression profiling of craniofacial fibrous dysplasia reveals ADAMTS2 overexpression as a potential marker. Int. J. Clin. Exp. Pathol. 2014;7:8532–8541. [PMC free article] [PubMed] [Google Scholar]
- 22.Piersanti S., Remoli C., Saggio I., Funari A., Michienzi S., Sacchetti B., Robey P.G., Riminucci M., Bianco P. Transfer, analysis, and reversion of the fibrous dysplasia cellular phenotype in human skeletal progenitors. J. Bone Miner. Res. 2010;25:1103–1116. doi: 10.1359/jbmr.091036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kiss J., Balla B., Kosa J.P., Borsy A., Podani J., Takacs I., Lazary A., Nagy Z., Bacsi K., Kis A., et al. Gene expression patterns in the bone tissue of women with fibrous dysplasia. Am. J. Med. Genet. A. 2010;152A:2211–2220. doi: 10.1002/ajmg.a.33559. [DOI] [PubMed] [Google Scholar]
- 24.Lee C.H., Espinosa I., Jensen K.C., Subramanian S., Zhu S.X., Varma S., Montgomery K.D., Nielsen T.O., van de Rijn M., West R.B. Gene expression profiling identifies p63 as a diagnostic marker for giant cell tumor of the bone. Mod. Pathol. 2008;21:531–539. doi: 10.1038/modpathol.3801023. [DOI] [PubMed] [Google Scholar]
- 25.Papadakis G.Z., Manikis G.C., Karantanas A.H., Florenzano P., Bagci U., Marias K., Collins M.T., Boyce A.M. (18) F-NaF PET/CT IMAGING IN FIBROUS DYSPLASIA OF BONE. J. Bone Miner. Res. 2019;34:1619–1631. doi: 10.1002/jbmr.3738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fu S., Tian Z., Zhang C., He Y. Monosotic fibrous dysplasia and solitary intramuscular myxoma of the head and neck: A unique presentation of Mazabraud’s syndrome and a literature review. Oncol. Lett. 2015;10:3087–3094. doi: 10.3892/ol.2015.3633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mu X., Li Z., Qin J., Wang Z., Fu W. Comparison of 18 F-FAPI and 18 F-FDG PET/CT in a Patient with Fibrous Dysplasia. Clin. Nucl. Med. 2024;49:e182–e183. doi: 10.1097/RLU.0000000000005089. [DOI] [PubMed] [Google Scholar]
- 28.Poreba M. Protease-activated prodrugs: Strategies, challenges, and future directions. FEBS J. 2020;287:1936–1969. doi: 10.1111/febs.15227. [DOI] [PubMed] [Google Scholar]
- 29.Lu Y.C., Chuang C.H., Chuang K.H., Chen I.J., Huang B.C., Lee W.H., Wang H.E., Li J.J., Cheng Y.A., Cheng K.W., et al. Specific activation of pro-Infliximab enhances selectivity and safety of rheumatoid arthritis therapy. PLoS Biol. 2019;17:e3000286. doi: 10.1371/journal.pbio.3000286. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Literature search results are available in Supplementary File S1. GEO gene expression datasets reviewed on 6 to 9 August 2024 for the publications in Table 1 are indicated in the GEO accession column and can be accessed at https://www.ncbi.nlm.nih.gov/geo/, accessed on 9 August 2024. Data reproduced in Figure 2 has been adapted from previous publications [1,16]. Data in Figure 3 and Table 2 is available in Supplementary File S2.