Abstract
Background and aims
The paucity of large-scale data exploring the effect of prior bariatric surgery on recurrent stroke outcomes in older individuals with obesity who survived a stroke led us to address the gap, with an emphasis on the risk of recurrent stroke and its trends.
Methods
Retrospective analysis of the National Inpatient Sample data from 2016 to 2019. Older individuals with obesity who survived a stroke (>65 years) and had a recurrent acute ischemic stroke (AIS) hospitalization, with or without prior bariatric surgery (PBS), were identified using ICD-10 codes. Recurrent stroke trends, demographic characteristics, and comorbidities between the cohorts were compared.
Results
Analyzing 643,505 older individuals with obesity who survived a stroke, we identified that 11,820 had undergone PBS. Both groups (no PBS vs. PBS) were predominantly female (59.7 % vs. 73.7 %), identified as white (76.5 % vs. 83.8 %), and covered by Medicare (91.7 % vs. 90.7 %). Diabetes, hyperlipidemia, prior myocardial infarction, and peripheral vascular diseases were more common in those without PBS. In contrast, tobacco use disorder, drug abuse, and valvular diseases were more common in those with PBS. There was no significant difference in the prevalence of hypertension between groups.
Between 2016 and 2019, recurrent AIS hospitalizations were less frequent in the PBS group (4 %–2.9 %, p = 0.035) while remaining stable in the other group (4.4 %–4.2 %, p = 0.064). The risk of recurrent AIS hospitalization was less frequent in the PBS cohort (aOR: 0.77, 95 % CI: 0.60–0.98).
Conclusion
PBS in older individuals with obesity who survived a stroke was associated with a 23 % lower risk of recurrent AIS hospitalization with a decreasing trend of prevalence since 2016. These findings could influence clinical practice and contribute to developing secondary prevention strategies for recurrent stroke among these patients.
Keywords: Obesity, Bariatric surgery, Recurrent stroke, Risk factors
Highlights
-
•
Risk of recurrent acute ischemic stroke hospitalization in older individuals is lowered by 23 % in those with prior bariatric surgery compared to those who do not.
-
•
Bariatric surgery patients are more often women and racially identify as white, followed by native americans.
-
•
The decline in recurrent stroke hospitalizations in the prior bariatric surgery cohort is confounded by survivorship bias.
-
•
Our findings are limited by other potential biases due to the use of administrative data and limitations in ICD-10-CM coding.
1. Introduction
Ischemic stroke, a principal cause of disability and death worldwide, has witnessed a decline in its global age-standardized incidence rate from 1990 to 2019 [1]. Despite this overall decrease, the incidence of ischemic stroke in patients has been shown to escalate with age [1]. This upward demographic trend underscores the heightened vulnerability of older patients to not only an increased risk of ischemic stroke but also to its associated, more severe outcomes and a higher mortality rate [2]. Concurrently, the global prevalence of obesity in adults has surged over the past decade [3]. Obesity in older individuals is exacerbated by physical inactivity and limited access to nutritious foods [4]. Additionally, obesity, being a critical risk factor for stroke, has also been associated with poorer functional recovery, underscoring the importance of addressing this issue in stroke prevention and management [5]. In this context, bariatric surgery emerges as a potential intervention, offering a pathway to substantial weight loss and the reduction of obesity-related complications in adults. A 2022 update to the 1991 guidelines supports considering bariatric surgery for those with BMI >35 and 30–34.9 in those with metabolic disease [6].
Given the increasing aging population in the world and the compounded risks associated in patients with obesity and stroke in older individuals ( ≥ 65 years), it is crucial to examine the outcomes of ischemic stroke in this population group who have undergone bariatric surgery. This study is designed to investigate the prevalence trends of recurrent acute ischemic stroke hospitalizations, comparing those who have undergone bariatric surgery with those who have not.
2. Methods
2.1. Data source and study population
We conducted a study using the National Inpatient Sample (NIS), a vast and publicly accessible database of hospital inpatient records in the United States, overseen by the Healthcare Cost and Utilization Project (HCUP) and sponsored by the Agency for Healthcare Research and Quality (AHRQ). The NIS approximates a 20-percent stratified sample of discharges from all HCUP-participating hospitals designed to cover more than 97% of the U.S. population [7]. Approval of an Institutional Review Board was not required because the NIS contains de-identified data.
Focusing on NIS data from 2016 to 2019, we identified the population of hospitalizations of older individuals, defined as those aged 65 and above, who have obesity and a history of diagnosed stroke. Then, patients with hospitalizations for subsequent strokes were identified. We utilized the International Classification of Disease 10th Edition Clinical Modification (ICD-10-CM) codes to identify our target populations. Hospitalizations for stroke events were identified using code I63, while bariatric surgery events were identified with code Z98.84. Hospitalizations with missing information on demographics, comorbidities, and outcomes were excluded from the analysis.
2.2. Study variables and outcomes
Comprehensive data encompassing patient demographics, i.e., age, sex, racial characteristics, socioeconomic status, and insurance type, hospital characteristics such as location, teaching status, and region, were obtained and compared between those with vs. without prior bariatric surgery. Comorbidities were determined and compared through the Elixhauser comorbidity index. The primary outcome of interest was recurrent stroke hospitalization.
2.3. Statistical analysis
The Pearson Chi-square test was used to compare categorical variables, and the Mann-Whitney U test was used to compare continuous variables. Percentages and medians with an interquartile range [IQR] were used for categorical and continuous variables, respectively. Multivariable analysis was performed to obtain adjusted odds ratio (aOR) and 95 % confidence intervals (C.I.) for in-hospital outcomes adjusting for patient and hospital characteristics. Linear-by-linear associated tests were employed in trend analyses. A two-tailed p-value below 0.05 was considered statistically significant. IBM SPSS Statistics 25.0 (IBM Corp., Armonk, New York) was employed for statistical purposes.
3. Results
3.1. Study population
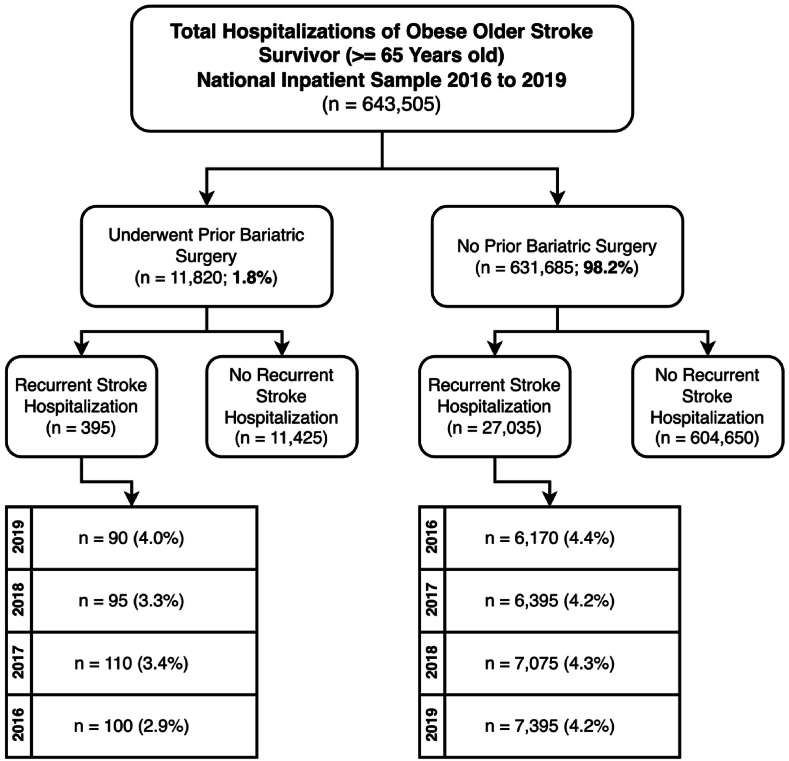
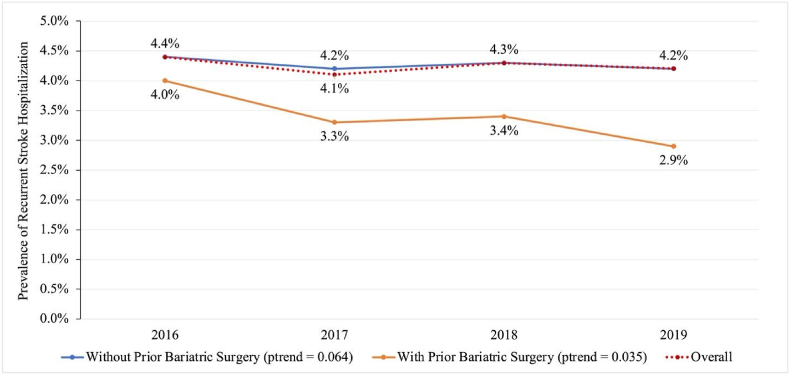
Between 2016 and 2019, we identified a total of 643,505 hospitalizations of older individuals ( ≥ 65 years) with obesity who also had a prior history of stroke. Of those, 11,820 (1.8 %) hospitalized patients had a prior bariatric surgery (PBS) history. From the overall population cohort, 27,430 patient hospitalizations occurred for acute ischemic stroke events, and of those, 395 (1.4 %) of those had a history of PBS [Fig. 1]. Exploring the trends of patient hospitalizations for recurrent acute ischemic stroke events without PBS showed 4.4 % in 2016, 4.2 % in 2017, 4.3 % in 2018, and 4.2 % in 2019 (p = 0.064). On the other hand, patients with recurrent stroke hospitalizations with a history of PBS were 4 % in 2016, 3.3 % in 2017, 3.4 % in 2018, and 2.9 % in 2019 (ptrend = 0.035) [Fig. 2].
Fig. 1.
Study population flow diagram: Older individuals with obesity and stroke survivor hospitalizations, national inpatient sample 2016–2019.
Fig. 2.
Nationwide Trends in Recurrent Acute Ischemic Stroke Hospitalizations in Older Individuals with Obesity and Stroke Survivors with vs. without Prior Bariatric Surgery (2016–2019).
3.2. Baseline characteristics
Our exploration of the differences in the baseline demographic and comorbidity characteristics between the populations of older individuals with obesity with recurrent stroke hospitalizations stratified based on those with and without PBS showed significant differences across various parameters [Table 1]. Age distribution differed significantly between groups, with a median age of 74 years [IQR: 69–80] in the non-PBS cohort and 70 years [IQR: 67–74] in the PBS cohort (p < 0.001). Sex distribution also varied significantly. The non-PBS group comprised 40.28 % males and 59.72 % females, whereas the PBS group included 26.27 % males and 73.73 % females, indicating a higher proportion of females in the PBS cohort (p < 0.001). Racial composition showed that the PBS group had a higher percentage of White individuals (83.81 %) than the non-PBS group (76.46 %). Conversely, the proportions of Black, Hispanic, Asian or Pacific Islander, and Native American individuals were lower in the PBS group compared to the non-PBS group, with these differences being statistically significant (p < 0.001). The PBS cohort was more prevalent in the higher median household income groups (Q3: 25.73 % vs. 24.32 %, and Q4: 19.31 % vs. 17.48 %, p < 0.001). Medicare was the predominant insurance type in both PBS (90.74 %) and non-PBS (91.71 %). Additionally, the proportion of Medicaid use was significantly lower in the PBS group (0.51 % vs. 1.32 %).
Table 1.
Baseline Characteristics and Outcomes of Recurrent Acute Ischemic Stroke Hospitalizations among Older Individuals with Obesity and Stroke Survivors with vs. without Prior Bariatric Surgery (2016–2019).
| Baseline Demographics | Without PBS (n = 631, 685) | With PBS (n = 11,820) | p-value | |
|---|---|---|---|---|
| Age in years (Median [IQR]) | 74 [69–80] | 70 [67–74] | <0.001b | |
| Sex (%) | Male | 40.28 | 26.27 | <0.001c |
| Female | 59.72 | 73.73 | ||
| Race (%) | White | 76.46 | 83.81 | <0.001c |
| Black | 15.43 | 11.15 | ||
| Hispanic | 6.88 | 3.76 | ||
| Asian or Pacific Islander | 0.83 | 0.49 | ||
| Native American | 0.39 | 0.80 | ||
| Median Household Incomea (%) | 1st: 0 to 25th Quartile | 30.49 | 27.61 | <0.001c |
| 2nd: 26th to 50th Quartile | 27.71 | 27.35 | ||
| 3rd: 51st to 75th Quartile | 24.32 | 25.73 | ||
| 4th: 76th to 100th Quartile | 17.48 | 19.31 | ||
| Payer Type (%) | Medicare | 91.71 | 90.74 | <0.001c |
| Medicaid | 1.32 | 0.51 | ||
| Baseline Comorbidities | ||||
| Hypertension (%) | 83.59 | 83.21 | 0.259c | |
| Hyperlipidemia (%) | 68.20 | 61.59 | <0.001c | |
| Diabetes Mellitus (%) | 60.05 | 52.24 | <0.001c | |
| Smoking (%) | 36.39 | 37.48 | 0.014c | |
| Prior Myocardial Infarction (%) | 15.72 | 12.82 | <0.001c | |
| Peripheral Vascular Disease (%) | 11.87 | 8.84 | <0.001c | |
| Valvular Disease (%) | 3.55 | 3.89 | 0.044c | |
| Drug Abuse (%) | 1.08 | 1.61 | <0.001c | |
| Multivariable Analysis for Outcome | Odds Ratio (95 % C.I. LL – UL) | |||
| Unadjusted Odds of Recurrent Acute Ischemic Stroke | 0.77 (0.69–0.86) | |||
| Adjusted Odds of Recurrent Acute Ischemic Stroke | 0.77 (0.60–0.98)d | |||
C.I. = Confidence Interval; LL = Lower Limits; UL = Upper Limits; a: household income estimated from national quartile for patient zip code; b: p-value <0.05 considered significant and estimated by Mann-Whitney-U test; c: p-value <0.05 considered significant and estimated by Pearson Chi-Square test; d: adjusted for age, sex, race, median household income, payer type, hypertension, hyperlipidemia, diabetes mellitus, smoking, prior myocardial infarction, peripheral vascular disease, valvular disease, drug abuse.
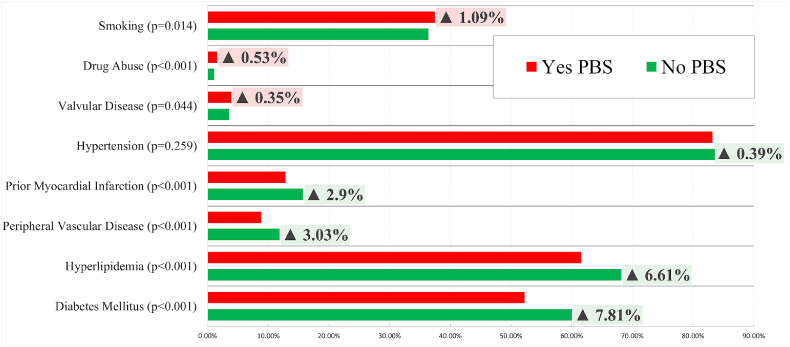
Regarding baseline comorbidities in those with vs. without PBS, there were no significant differences in the prevalence of hypertension between groups despite it being most prevalent (83.21 % vs. 83.59 %, p = 0.259). Significant differences were observed in the prevalence of hyperlipidemia (61.59 % vs. 68.20 %, p < 0.001), diabetes mellitus (52.24 % vs. 60.05 %, p < 0.001), prior myocardial infarction (12.82 % vs. 15.72 %, p < 0.001), peripheral vascular disease (8.84 % vs. 11.87 %, p < 0.001), with these comorbidities being more prevalent in the non-PBS group. Additionally, smoking (37.48 % vs. 36.39 %, p = 0.014), valvular disease (3.89 % vs. 3.55 %, p = 0.044), and drug abuse (1.61 % vs. 1.08 %, p < 0.001) were more prevalent in the PBS group [Fig. 3].
Fig. 3.
Differences of Comorbidities in Recurrent Acute Ischemic Stroke Hospitalizations in Older Individuals Surviving Stroke with vs. without Prior Bariatric Surgery (2016–2019).
3.3. Odds of recurrent stroke hospitalization
The unadjusted analysis showed that those with PBS had decreased odds of having recurrent acute ischemic stroke hospitalization by 23 % (OR: 0.77 [95 % C.I. 0.69–0.86]). After adjusting for all baseline demographics and comorbidities, the association remained significant (aOR: 0.77 [95 % C.I. 0.60–0.98]), suggesting that bariatric surgery may be protective against this outcome even when considering other influencing factors.
4. Discussion
The study presented investigates the impact of bariatric surgery on the incidence of recurrent acute ischemic stroke hospitalizations among older individuals with obesity with a history of stroke. Our findings present compelling evidence that bariatric surgery may serve as a significant protective measure against hospitalizations for the recurrence of acute ischemic strokes in older individuals with obesity with a history of stroke by 23 %. The reduced odds remain significant even after adjustment for age, gender, race, income, and comorbidities.
Bariatric surgery has been shown to reduce the risk of ischemic stroke by 51 % in a pooled analysis of observational studies [8]. Williams et al., in their analysis, found the procedure to reduce the risk of ischemic stroke by 46 % in one year and 22 % in five-year follow-ups [9]. Additionally, amongst stroke survivors, bariatric surgery has been shown to reduce the odds of all-cause mortality by 42 % during their hospitalizations [10]. Our study adds further value by suggesting that bariatric surgery may protect against hospitalizations for stroke recurrence in older individuals with obesity who have survived a stroke.
In addition to our findings related to stroke recurrence, our study also provides insights into the demographic and clinical characteristics of older individuals with obesity who have survived a stroke. The higher prevalence of females in the bariatric surgery group could reflect gender-specific healthcare behavior or differences in willingness to undergo the procedure. Moreover, the differences in racial composition and socioeconomic status between the groups point to potential disparities that may influence access to, and hence the outcomes of, bariatric surgery and stroke care. While hypertension remained the prevalent comorbidity in both groups, notable differences in other comorbidities, specifically the higher prevalence of prior myocardial infarction, peripheral vascular disease, hyperlipidemia, and diabetes mellitus in the non-surgical group, highlight a cumulative risk factor burden that further underscores the protective potential of bariatric surgery.
Our trend analysis underscores a consistent decrease in the percentage of recurrent stroke hospitalizations over the observed period (2016–2019) among the bariatric surgery cohort, juxtaposed against a relatively stable incidence in the non-surgical group. This finding may be influenced by survivorship bias. Individuals at higher risk of recurrent stroke may have experienced such events early in the study period (notably in 2016), leading to a natural diminution in the incidence of recurrent strokes in subsequent years due to the attrition of high-risk individuals.
Bariatric surgery is a complex and invasive procedure, and it is not suitable for all individuals. The older population is at a higher risk of complication rates from the surgery. Hence, the decision to undergo bariatric surgery should be made on a case-by-case basis [11] [DM Pechman 2019]. This approach emphasizes the importance of patient-centered care and informed clinical judgment.
4.1. Strengths and limitations
It is imperative to approach our findings with an understanding of the study's limitations. Being observational in nature, we cannot provide causal inferences. The reliance on administrative data in our study introduces potential biases due to limitations in coding and reporting. While coding for obesity is specific [12] [K Suissa 2022], it lacks sensitivity, often missing patients with obesity, as they are not coded as such. This may affect the representativeness of our study population and limit the generalizability of our findings to the broader population in the community. Additionally, the analysis may not be sufficiently powered to fully understand the effects of survivorship bias on the downward trend of recurrent stroke hospitalization in the bariatric surgery cohort. Furthermore, the nature of our data limits a detailed examination of the different types of bariatric surgery, quality of healthcare delivery, treatment compliance to comorbidities such as diabetes and hypertension, the influence of provider approach to healthcare delivery, the specific BMI for each cohort, and their respective associations with recurrent stroke hospitalization.
Despite these limitations, our study contributes valuable insights into the potential benefits of bariatric surgery beyond weight loss—specifically, its role in reducing the risk of stroke recurrence in a vulnerable population segment. However, prospective and randomized studies are required to establish the optimal role of bariatric surgery in managing older individuals with obesity who survive a stroke.
5. Conclusions
Analyzing data from the National Inpatient Sample from 2016 to 2019, our study investigated the impact of bariatric surgery on hospitalizations for recurrent stroke in older individuals. The study found that hospitalizations for recurrent stroke decreased over time in patients who had undergone bariatric surgery compared to those who had not. Despite limitations such as the observational design, potential coding biases, and survivorship bias, our findings suggest that bariatric surgery is a viable intervention to lower stroke recurrence risk in this population.
-
•
Bariatric Surgery and Stroke Recurrence: Bariatric surgery is associated with a significant decrease in the risk of recurrent stroke hospitalizations.
-
•
Protective Effect: The odds of recurrent acute ischemic stroke hospitalizations are reduced by 23 % in older individuals who undergo bariatric surgery.
-
•
Future Research: Prospective and randomized studies are necessary to investigate further the role of bariatric surgery in managing stroke risk among older individuals with obesity.
Declaration of Artificial Intelligence (AI) and AI-assisted technologies
During the preparation of this work, the author(s) did not use Artificial intelligence technologies.
Grant support
No grant support was received for this research work.
Ethics Approval
Not applicable.
Patient consent
Not applicable.
Credit statement
Arankesh Mahadevan: Investigation, Writing - Original Draft, Writing - Review & Editing, Project administration; Advait Vasavada: Investigation, Writing - Original Draft, Writing - Review & Editing; Nafisa Reyaz: Investigation, Writing - Original Draft; Srinishant Rajarajan: Investigation, Writing - Original Draft; Kalaivani Babu: Investigation, Writing - Original Draft; Dakshin Meenashi Sundaram: Investigation, Writing - Original Draft; Dhayashri Dhavapalani: Investigation, Writing – Review & Editing; Samir Vanani: Investigation, Writing – Review & Editing; Ashley Thompson-Edwards: Investigation, Writing – Review & Editing; Dharshana Prem Anand: Investigation, Writing – Review & Editing; Sushmitha Garikipati: Investigation, Writing – Review & Editing; Rupak Desai: Conceptualization, Methodology, Formal analysis, Visualization, Writing - Review & Editing, Supervision.
Declaration of competing Interest
None.
Acknowledgments
None.
Footnotes
Abstract presented at the 2024 International Stroke Conference as an oral presentation by 1st author (AM) and won the Junior Investigator Award and travel grant.
The research abstract was presented at the 2024 International Stroke Conference, Phoenix, Arizona, as an oral presentation by the first author (AM). First Author (AM) was awarded the Junior Investigator Award and Travel Grant (1000 USD) for the presentation.
Contributor Information
Arankesh Mahadevan, Email: arankeshmahadevan@gmail.com.
Advait Vasavada, Email: advait2163@gmail.com.
Nafisa Reyaz, Email: reyaz.nafisa@gmail.com.
Srinishant Rajarajan, Email: srinishantrajarajan@gmail.com.
Kalaivani Babu, Email: ajukalaivanibabu@gmail.com.
Dakshin Meenashi Sundaram, Email: dakshinnsundar@gmail.com.
Dhayashri Dhavapalani, Email: dhavapalani@googlemail.com.
Samir Vanani, Email: samir.vanani@outlook.com.
Ashley Thompson-Edwards, Email: ashleympthompson@gmail.com.
Dharshana Prem Anand, Email: dr.dharshanaprem@gmail.com.
Sushmitha Garikipati, Email: sushmithagarikipati6@gmail.com.
Praveena Sunkara, Email: praveenasunkara@gmail.com.
Rupak Desai, Email: drrupakdesai@gmail.com.
References
- 1.Ding Q., Liu S., Yao Y., Liu H., Cai T., Han L. Global, regional, and national burden of ischemic stroke, 1990-2019. Neurology. 2022;98:e279–e290. doi: 10.1212/WNL.0000000000013115. [DOI] [PubMed] [Google Scholar]
- 2.Kelly-Hayes M. Influence of age and health behaviors on stroke risk: lessons from longitudinal studies. J Am Geriatr Soc. 2010;58(Suppl 2):S325–S328. doi: 10.1111/j.1532-5415.2010.02915.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Malik V.S., Willet W.C., Hu F.B. Nearly a decade on - trends, risk factors and policy implications in global obesity. Nat Rev Endocrinol. 2020;16:615–616. doi: 10.1038/s41574-020-00411-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Malenfant J.H., Batsis J.A. Obesity in the geriatric population - a global health perspective. J Glob Health Rep. 2019;3 doi: 10.29392/joghr.3.e2019045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim N.Y., Choi Y.A. Obesity impairs functional recovery of older stroke patients with possible sarcopenia: a retrospective cohort study. J Clin Med. 2023;12 doi: 10.3390/jcm12113676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eisenberg D., Shikora S.A., Aarts E., et al. American society of metabolic and bariatric surgery (ASMBS) and international federation for the surgery of obesity and metabolic disorders (IFSO) indications for metabolic and bariatric surgery. Obes Surg. 2022;33:3–14. doi: 10.1007/s11695-022-06332-1. 2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Overview of the national (Nationwide) inpatient sample (NIS). [DOI] [PMC free article] [PubMed]
- 8.Kwok C.S., Pradhan A., Khan M.A., et al. Bariatric surgery and its impact on cardiovascular disease and mortality: a systematic review and meta-analysis. Int J Cardiol. 2014;173:20–28. doi: 10.1016/j.ijcard.2014.02.026. [DOI] [PubMed] [Google Scholar]
- 9.Williams M.D., Kim S., Sarran M., et al. The effect of bariatric surgery on ischemic stroke risk. Surg Obes Relat Dis. 2021;17:1949–1955. doi: 10.1016/j.soard.2021.09.006. [DOI] [PubMed] [Google Scholar]
- 10.Han H., Chen L., Wang M., Wei X., Ruan Y., He J. Benefits of bariatric surgery in patients with acute ischemic stroke-a national population-based study. Surg Obes Relat Dis. 2019;15:1934–1942. doi: 10.1016/j.soard.2019.08.020. [DOI] [PubMed] [Google Scholar]
- 11.Pechman D.M., Munoz Flores F., Kinkhabwala C.M., et al. Bariatric surgery in the elderly: outcomes analysis of patients over 70 using the ACS-NSQIP database. Surg Obes Relat Dis. 2019;15:1923–1932. doi: 10.1016/j.soard.2019.08.011. [DOI] [PubMed] [Google Scholar]
- 12.Suissa K., Schneeweiss S., Lin K.J., Brill G., Kim S.C., Patorno E. Validation of obesity-related diagnosis codes in claims data. Diabetes Obes Metabol. 2021;23:2623–2631. doi: 10.1111/dom.14512. [DOI] [PMC free article] [PubMed] [Google Scholar]