Abstract
Background
The Karamoja subregion in north-eastern Uganda has very high Tuberculosis (TB)case notification rates and, until recently, had suboptimal treatment completion rates among patients diagnosed with TB. We evaluated community knowledge, attitudes and practices towards Tuberculosis in order to identify barriers to TB control in this region.
Methods
From September to October 2022, we conducted a community-based survey in four districts in the Karamoja subregion. We collected data on TB knowledge, attitudes, and practices using a structured electronic questionnaire. We generated knowledge, attitude and practice scores. We used a survey-weighted zero-truncated modified Poisson model to assess the association between knowledge/attitude scores and respondents’ characteristics and a complementary log-log model to assess the association between practice scores and respondents’ characteristics. Data analysis was carried out using STATA version 14.
Results
A total of 1927 respondents were interviewed. Of these, 55.5% were female, and 1320 (68.6%) had no formal education. Overall, 68.5% 95% CI (59.6–76.7%) had knowledge scores of ≥ 60%. Higher TB knowledge scores were associated with being employed (adjusted prevalence ratio, aPR = 1.22, 95% CI 1.04–1.42, p = 0.01) while being a wife in a household was associated with lower TB knowledge (aPR = 0.90, 95% CI 0.82–0.99, p = 0.03). Being 25–34 years old was associated with a positive attitude towards TB (PR = 1.06, 1.01–1.11, p = 0.01). Over 85% of respondents would go to the health facility immediately if they had TB signs and symptoms. Almost all respondents (98.6%) would start TB treatment immediately if diagnosed with the disease.
Conclusion
More than two thirds of patients had good knowledge and practices towards TB which can be leveraged to improve uptake of TB control interventions in the region. Additional interventions to improve TB knowledge and practice should focus on specific segments within the communities e.g., older women in the households.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-19986-6.
Keywords: Tuberculosis, Knowledge, Attitudes, Practices, Community survey, Karamoja
Background
Tuberculosis (TB) remains a major cause of morbidity and mortality worldwide. In 2021, an estimated 10 million people fell ill with tuberculosis. In the same year, 1.6 million deaths from TB were recorded [1]. The burden of TB and other infectious diseases is disproportionately distributed across regions, with Southeast Asia and sub-Saharan Africa having the largest share of the global TB burden [2]. Even within countries, the burden of TB disproportionately affects certain vulnerable regions and populations. The Karamoja sub-region in North-eastern Uganda is one such region. The region is home to 1.2 million people but notifies > 5500 TB cases annually translating into a notification rate of approximately 450 per 100,000 higher than the national average of 213/100,000 population. The high TB burden in this region is driven by an intersection of overcrowding, poor nutrition, and poorly ventilated housing [3, 4]. The Karamoja subregion is inhabited by predominantly pastoralist communities and has the lowest human development indicators in the country [5]. In addition, seasonal migrations contribute significantly to the non-completion of TB treatment, resulting in further spread of the disease [6].
The Program for Accelerated Control of TB in Karamoja (PACT-Karamoja) is a five-year funded project funded by the Unites States Agency for International Development that supports TB control activities in the Karamoja subregion [7]. The project focuses on community engagement to improve TB case-finding and adherence to TB treatment. In 2022, The project carried out a community-based survey to identify the knowledge of, attitudes to and practices associated with TB that may fuel transmission or create barriers to uptake of TB control interventions in the region.
Methods
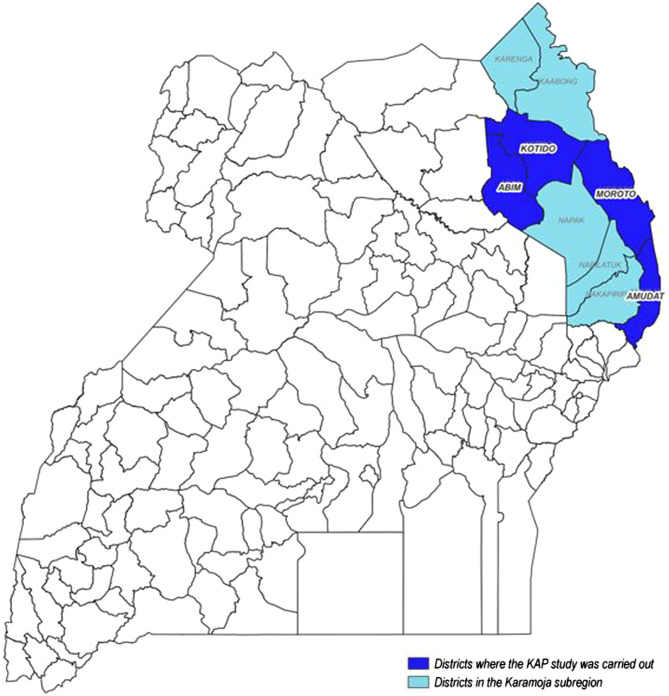
From September to October 2022, we carried out a cross-sectional community-based Knowledge, Attitudes and Practices [8] survey in four districts of the Karamoja subregion (Fig. 1). We purposively selected the districts to represent the three major sub-groups of indigenous peoples that have different lifestyles, cultural values and economic activities that may predispose them to differential community knowledge, attitudes and practices towards TB. Abim district was chosen to represent the agriculturalists, Kotido and Moroto to represent the pastoralists who live in clustered settlements commonly referred to as “Manyattas” and Amudat to represent the agro-pastoralists and cross border populations who live a mobile lifestyle in more than one country. The sample size for this study was powered to provide district-specific estimates of knowledge, attitudes and practices and was adjusted upwards by 25% to cater for non-responsiveness. The final sample size was 1980 respondents (30 eligible individuals from 66 clusters). Details of the sample size calculations are in Supplementary Table 1.
Fig. 1.
Map of Uganda showing the Karamoja Subregion
Selection of households and study respondents
We employed multi-stage sampling. First, we randomly selected 66 clusters (parishes) from a sampling frame of parishes provided by the Uganda Bureau of Statistics. Then, we used systematic sampling to select households from each cluster. In the third and final stage, two eligible individuals were selected from each household. In the Karamoja subregion, household heads are usually older males. Therefore, to ensure a representative number of women, adolescents, and young adults in our study, the team invited the household head plus an additional member who was either a young person aged ≥ 25 years (male or female) or an adolescent aged 15–24 years (male or female) to participate in the survey. The study team visited each household once. We did not replace households where participants declined to participate because this was accounted for in the sample size estimation.
Data collection and analysis
The questionnaire used in this study was adapted from a nationwide survey of knowledge, attitudes, and practices related to TB in Ethiopia [9], and modified to suit the context in the Karamoja subregion. The questionnaire included questions on respondents’ demographics, TB knowledge, attitudes, and practices. It also had questions on TB prevention and preferred modalities for receiving TB-related information.
Due to the insecurity within the region, we were only able to collect data from 58 out of the 66 clusters available. Data was collected by trained research assistants with previous survey experience who conducted face-to-face interviews with respondents using an electronic questionnaire managed by RedCap®. Interviews were conducted in the local languages used in the Karamoja region and lasted approximately one hour.
Participants’ characteristics were summarized using frequencies and percentages for categorical variables plus mean and standard deviations for continuous variables [10]. Knowledge, attitudes, and practices towards TB were presented using proportions and their 95% confidence intervals (CIs). The distribution of respondents’ characteristics, knowledge, attitudes, and practices were presented in general and by district type. The districts were grouped into three according to the main economic activity (the agriculturists, the pastoralists, and the agro-pastoralists).
We generated composite knowledge scores from questions on the cause of TB, symptoms and signs of TB, TB transmission, diagnosis, treatment and prevention. The maximum possible score was 16. Anyone whose score was 10 or more was regarded to have scored 60% or more. A score of ≥ 60% was regarded as high TB knowledge [11]. We used a survey-weighted, zero-truncated Poisson model to assess the association between knowledge scores and various respondents’ characteristics. Next, we generated composite attitude scores from questions on respondents’ feelings about a TB diagnosis and on disclosure of TB status and feelings about people with TB. Total possible scores on attitude towards TB were 8. Similar to knowledge scores, a score ≥ 60% (≥ 5 correct answers) was regarded as a good attitude towards TB. Finally, a composite practice score was generated from questions on practices associated with seeking care after onset of TB symptoms, readiness to start TB treatment and the type of TB treatment that respondents would start. The total possible score was 16. Similar to knowledge and attitude scores, a score ≥ 60% (10 correct answers) was regarded as good TB practice.
We used a modified Poisson model to assess the association between respondents’ knowledge, their attitudes and their social demographic characteristics. The same model was used to assess the association between respondents’ knowledge and their attitude towards TB. We used a survey-weighted complementary log-log model to assess the association between respondents’ practices and their characteristics. For all multivariate analyses, only factors with a p-value of ≤ 0.2 on bivariate analysis were considered for the multivariate model. Factors were considered significant in the multivariable model if the p-value was ≤ 0.05. All analyses were survey-weighted. Data were analyzed in STATA v 14.0.
Results
Demographic characteristics of respondents
A total of 1927 respondents were interviewed for the survey. The majority were female (55.5%), had no formal education (68.6%) and were peasant farmers (72.1%). Lack of formal education was higher among pastoralists (78.1% vs. 56.3% among agriculturalists and 59.5% - agro-pastoralists) p < 0.01. Half the respondents were between 25 and 44 years (25–34 years-32.73% and 35–44 years,22.60%). Almost all respondents (91.5%) had stayed in their households for ≥ 24 months. Household sizes were large, with 6–10 people per household (Table 1).
Table 1.
Socio-demographic characteristics of respondents a by district in Karamoja region, Uganda,
| Variables | All n (%) (n = 1927) k |
Agriculturalist b | Pastoralists c | Agro-pastoralists d | P Value e |
|---|---|---|---|---|---|
|
n (Col%) 496 (25.7%) |
n (Col %) 1029 (53.4%) |
n (Col %) 402 (20.9%) |
|||
| Age Groups* | |||||
| 18–24 | 289 (15.0) | 77 (15.5) | 155 (15.1) | 57 (14.2) | |
| 25–34 | 630 (32.7) | 158 (31.9) | 338 (32.9) | 134 (33.3) | |
| 35–44 | 435 (22.6) | 106 (21.4) | 245 (23.9) | 84 (20.9) | 0.56 |
| 45–59 | 353 (18.3) | 87 (17.5) | 185 (18.0) | 81 (20.2) | |
| 60 and above | 218 (11.3) | 68 (13.7) | 104 (10.1) | 46 (11.4) | |
| Sex* | |||||
| Male | 857 (44.5%) | 207 (41.7) | 471 (45.8) | 179 (44.5) | 0.32 |
| Female | 1069 (55.5%) | 289 (58.3) | 557 (54.2) | 223 (55.5) | |
| Education* | |||||
| No formal education | 1320 (68.6) | 279 (56.3) | 803 (78.1) | 238 (59.5) | |
| Primary | 383 (19.9) | 148 (29.8) | 137 (13.3) | 98 (24.5) | < 0.01 |
| Secondary and Higher | 221 (11.5) | 69 (13.9) | 88 (8.6) | 64 (16.0) | |
| Respondent household position* | |||||
| Head | 882 (45.8) | 220 (44.4) | 480 (46.7) | 182 (45.3) | |
| Wife | 765 (39.7) | 176 (35.5) | 431 (42.0) | 158 (39.3) | < 0.01 |
| Son/daughter | 223 (11.6) | 76 (15.3) | 100 (9.7) | 47 (11.7) | |
| Other | 55 (2.9) | 24 (4.8) | 16 (1.6) | 15 (3.7) | |
| Length of stay in household prior to survey | |||||
| 6–24 months | 164 (8.5) | 34 (6.9) | 96 (9.3) | 34 (8.5) | 0.27 |
| 24 or more months | 1762 (91.5) | 462 (93.1) | 932 (90.7) | 368 (91.5) | |
| Household size* | |||||
| ≤ 5 people | 665 (34.7) | 147 (29.8) | 386 (37.8) | 132 (33.0) | |
| 6–10 people | 1062 (55.5) | 301 (60.9) | 546 (53.5) | 215 (53.8) | < 0.01 |
| > 10 people | 188 (9.8) | 46 (9.3) | 89 (8.7) | 53 (13.3) | |
| Employment status (Multiple response) | |||||
| Unemployed | 412 (21.4) | 68 (13.7) | 284 (27.6) | 60 (14.9) | < 0.01 |
| Peasant farmer | 1390 (72.1) | 374 (75.4) | 698 (67.8) | 318 (79.1) | < 0.01 |
| Livestock | 306 (15.9) | 46 (9.3) | 201 (19.5) | 59 (14.7) | < 0.01 |
| Trader | 190 (9.9) | 44 (8.9) | 95 (9.2) | 51 (12.7) | 0.09 |
| Others | 246 (12.8) | 61 (12.3) | 137 (13.3) | 48 (11.9) | 0.73 |
| Distance to nearest health facility* | |||||
| ≤ 5 km | 1218 (63.3) | 299 (60.3) | 599 (58.3) | 320 (79.8) | |
| 6–15 km | 508 (26.4) | 155 (31.3) | 300 (29.2) | 53 (13.2) | < 0.01 |
| 16–25 km | 175 (9.1) | 38 (7.7) | 109 (10.6) | 28 (7.0) | |
| > 25 km | 23 (1.2) | 4 (0.8) | 19 (1.9) | 0 (0.0) | |
| Have you heard about TB? | |||||
| Yes | 1798 (93.4) | 452 (91.1) | 981 (95.4) | 365 (90.8) | < 0.01 |
| No | 128 (6.7) | 44 (8.9) | 47 (4.6) | 37 (9.2) | |
a Response rate was 98.2% in all four Districts
b Abim District
c Amudat District
d Kotido and Moroto Districts
e Pearson Chi-square test P-values for comparing Different socio-demographic characteristics by district classification. P ≤ 0.05 is considered significant (5% level of significance)
* Missing values (Age: n = 1, Household: n = 1, Education: n = 2, Distance to HC: n = 2, Household Size: n = 11, all are < 1%
Knowledge about TB
Information on TB symptoms and transmission among respondents is in Table 2. Only 44.6% of respondents knew that a germ causes TB. Almost three quarters thought that TB was transmitted in several ways, including through the air, through sharing utensils and/or shaking hands with sick persons. However, more than 90% of respondents knew coughing was one of the symptoms of TB. A smaller proportion, 44.9%, knew all four cardinal symptoms of TB (cough, evening fevers, night sweats, and weight loss). The overwhelming majority of respondents (99.6%) knew that they should go to a health facility to get diagnosed with TB, and more than half (54.8%) mentioned drugs specifically for TB as the only cure for TB. A lower proportion (47%) knew the correct duration of TB treatment but two-thirds of respondents knew that the importance of adhering to TB treatment until completion. Concerning TB prevention, 71.3% of respondents knew at least one correct way to prevent TB. More than two-thirds, 68.8% (95% CI: 59.6, 76.7) had good TB knowledge, described as a score of ≥ 60%. This proportion did not defer significantly across the subgroups (70,0% (95% CI: 53.0, 82.8) among agriculturalists, 60.6% (95% CI; 52.1, 68.6) among pastoralists and 79.9% (95% CI: 62.4, 90.5) among agro-pastoralists districts. Results are shown in Table 2.
Table 2.
Knowledge of respondents on TB symptoms and transmission
| Variables | All Districts | Agriculturalist | Pastoralists | Agro-pastoralists | ||
|---|---|---|---|---|---|---|
| % (95% CI) | % (95% CI), | % (95% CI), | % (95% CI), | p-value | ||
| Number of respondents | (N = 1,799) | N = 452 (25.1%) | N = 981 (54.6%) | N = 365 (20.3%) | ||
| Cause of TB | ||||||
| Germs | 29.9 (26.0, 34.1) | 34.4 (25.7, 44.3) | 28.8 (23.3, 35.0) | 28.5 (22.8, 35.1) | < 0.01 | |
| Germs + others | 14.7 (9.6, 21.9) | 3.9 (2.2, 6.9) | 24.6 (18.2, 32.4) | 5.7 (2.1, 14.7) | ||
| Did not know | 55.4 (47.3, 63.2) | 61.7 (51.7, 70.7) | 46.6 (36.7, 56.8) | 65.8 (55.5, 74.8) | ||
| Symptoms of TB | ||||||
| Cough + any other | 90.4 (88.2, 92.2) | 88.7 (82.8, 92.7) | 90.5 (87.0, 93.1) | 91.4 (88.5, 93.7) | 0.12 | |
| All 4 cardinal symptoms a | 44.9 (37.2, 52.8) | 50.9 (43.2, 58.5) | 38.9 (26.5, 52.9) | 51.0 (46.3, 55.8) | ||
| Did not know | 1.4 (0.7, 2.9) | 3.7 (1.4, 9.2) | 0.8 (0.3, 1.9) | 0.7 (0.2, 2.7) | ||
| TB Transmission | ||||||
| Through air only | 3.5 (2.3, 5.4) | 4.3 (1.7, 10.6) | 4.2 (2.8, 6.2) | 1.8 (0.6, 5.5) | ||
| Through air + other ways | 77.0 (71.0, 82.2) | 77.5 (66.4, 85.8) | 74.2 (67.6, 79.9) | 81.1 (65.8, 90.6) | 0.64 | |
| Did not know | 19.4 (15.0, 24.8) | 18.2 (12.0, 26.6) | 21.6 (16.3, 28.1) | 17.1 (8.3, 31.8) | ||
| TB Diagnosis (Multiple response) | ||||||
| Health facility | 99.6 (99.0, 99.8) | 99.8 (99.34, 99.96) | 99.5 (98.6, 99.8) | 99.5 (97.8, 99.9) | 0.58 | |
| Herbalist | 3.7 (2.5, 5.5) | 1.9 (0.7, 4.9) | 3.7 (2.3, 5.9) | 4.9 (2.5, 9.3) | 0.29 | |
| Community elders / healers | 2.1 (1.3, 3.4) | 0.7 (0.2, 1.8) | 3.4 (2.0, 5.9) | 1.2 (0.4, 3.9) | 0.02 | |
| TB treatment | ||||||
| TB medicines only | 54.8 (47.4, 61.9) | 52.3 (37.8, 66.5) | 55.9 (49.0, 62.6) | 55.0 (36.0, 72.6) | 0.56 | |
| TB Medicines + Herbs | 36.1 (27.9, 45.1) | 39.1 (26.2, 53.7) | 32.4 (26.6, 38.9) | 39.7 (19.7, 63.9) | ||
| Does not know | 9.2 (6.4, 12.8) | 8.6 (6.5, 11.2) | 11.7 (7.7, 17.4) | 5.3 (2.0, 13.2) | ||
| Length of TB treatment | ||||||
| < 6 months | 33.4 (25.8, 41.9) | 34.7 (26.5, 43.9) | 34.9 (23.8, 47.9) | 28.9 (22.3, 36.7) | 0.43 | |
| ≥ 6 months | 47.3 (41.2, 53.5) | 43.8 (35.9, 52.1) | 45.2 (37.1, 53.5) | 54.9 (48.5, 61.0) | ||
| Don’t know | 19.3 (15.7, 23.4) | 21.5 (14.8, 30.1) | 19.9 (14.3, 27.0) | 16.2 (13.2, 19.7) | ||
| Consequences of nonadherence to TB treatment | ||||||
| Death or becomes sicker | 97.8 (95.5, 98.9) | 98.9 (96.7, 99.6) | 98.6 (97.1, 99.4) | 95.2 (90.7, 97.6) | 0.01 | |
| Nothing | 1.0 (0.5, 2.0) | 0.2 (0.1, 1.0) | 1.2 (0.5, 3.0) | 1.1 (0.3, 4.4) | 0.41 | |
| I don’t know | 2.5 (1.3, 4.8) | 1.5 (0.6, 3.7) | 1.8 (0.8, 3.7) | 4.5 (2.1, 9.5) | 0.07 | |
| TB prevention | ||||||
| Both TPT + infection control practice e.g., mouth covering | 41.3 (34.7, 48.2) | 44.3 (33.2, 55.9) | 39.0 (30.7, 47.9) | 42.1 (28.3, 57.2) | 0.24 | |
| Either TPT or infection control practice | 30.0 (26.6, 33.6) | 29.8 (22.9, 37.9) | 25.9 (21.2, 31.3) | 36.3 (31.3, 41.6) | ||
| Did not know | 28.7 (22.6, 35.7) | 25.9 (19.9, 32.9) | 35.1 (27.8, 43.3) | 21.6 (11.5, 37.0) | ||
| Overall Knowledge of TB Score (Categorized) | ||||||
| Low TB Knowledge (i.e. <60) | 31.2 (23.3, 40.4) | 30.0 (17.2, 47.0) | 39.4 (31.4, 47.9) | 20.1 (9.5, 37.6) | 0.13 | |
| High TB Knowledge (i.e. ≥60) | 68.8 (59.6, 76.7) | 70.0 (53.0, 82.8) | 60.6 (52.1, 68.6) | 79.9 (62.4, 90.5) | ||
a The four cardinal symptoms of TB are cough, night sweats, weight loss, fever
Composite TB knowledge scores
On analysis of composite knowledge scores, higher TB knowledge scores were associated with being employed (adjusted prevalence ratio, aPR = 1.21, 95% CI 1.03–1.41, p = 0.02), while lower TB knowledge scores were associated with living > 25 km from a health facility (aPR = 0.90, 95% CI 0.82–9.8, p = 0.01) and while being a wife was associated with lower TB knowledge (aPR = 0.89, 95% CI 0.81–0.98, p = 0.02). (Table 3)
Table 3.
A survey-weighted zero-truncated Poisson Model for Individual-level factors Associated with knowledge about TB
| Variables | Unadjusted IRR (95% CI) | P-Value | Adjusted IRR (95% CI) | P-Value |
|---|---|---|---|---|
| Age | ||||
| 18–24 | Reference | Reference | ||
| 25–34 | 0.98 (0.91, 1.06) | 0.667 | 1.00 (0.94, 1.07) | 0.97 |
| 35–44 | 0.97 (0.89, 1.06) | 0.534 | 0.98 (0.91, 1.06) | 0.63 |
| 45–59 | 0.99 (0.92, 1.06) | 0.695 | 1.01 (0.93, 1.10) | 0.77 |
| 60 and above | 0.99 (0.89, 1.10) | 0.852 | 1.04 (0.89, 1.22) | 0.61 |
| Sex | ||||
| Male | Reference | Reference | ||
| Female | 0.94 (0.88, 1.01) | 0.101 | 1.02 (0.96, 1.08) | 0.35 |
| Education | ||||
| No formal education | Reference | Reference | ||
| Primary | 1.01 (0.96, 1.07) | 0.68 | 0.98 (0.92, 1.05) | 0.51 |
| Secondary and Higher | 1.00 (0.89, 1.12) | 0.961 | 0.99 (0.91, 1.07) | 0.74 |
| Household Position | ||||
| Head | Reference | Reference | ||
| Wife | 0.91 (0.83, 0.99) | 0.029 | 0.89 (0.81, 0.98) | 0.02 |
| Children (i.e. Son/daughter) | 1.02 (0.95, 1.10) | 0.554 | 1.01 (0.94, 1.10) | 0.75 |
| Other | 1.14 (1.06, 1.23) | 0.001 | 1.13 (1.05, 1.21) | < 0.01 |
| Time stayed in household | ||||
| 6–24 months | Reference | Reference | ||
| 24 or more months | 0.93 (0.84, 1.03) | 0.161 | 0.95 (0.87, 1.03) | 0.22 |
| Household size | ||||
| ≤ 5 people | Reference | Reference | ||
| 6–10 people | 1.06 (0.99, 1.13) | 0.083 | 1.05 (0.99, 1.12) | 0.11 |
| > 10 people | 0.89 (0.74, 1.08) | 0.25 | ||
| Employment Status | ||||
| Unemployed (not working) | Reference | Reference | ||
| Employed (or Working) | 1.22 (1.06, 1.39) | 0.005 | 1.21 (1.03, 1.41) | 0.02 |
| Distance to Health Facility | ||||
| ≤ 5 km | Reference | Reference | ||
| 6–15 km | 0.94 (0.84, 1.05) | 0.274 | 0.96 (0.87, 1.07) | 0.47 |
| 16–25 km | 1.03 (0.88, 1.21) | 0.676 | 1.05 (0.92, 1.19) | 0.45 |
| > 25 km | 0.92 (0.86, 0.98) | 0.007 | 0.90 (0.82, 9.8) | 0.01 |
Respondents’ attitudes towards TB
Information about the attitude of respondents towards TB is summarized in Table 4. The majority of respondents, 65.5%, expressed mixed emotions towards a TB diagnosis (i.e. happy and sad, ashamed or fearful), 23.2% expressed only positive emotions (i.e., happy that the cause of their problems has been found) while 10% expressed only negative emotions towards a TB diagnosis. About one in five participants (20.9%) mentioned that they would not disclose their TB diagnosis to anyone. Of those who said they would share their TB diagnosis, 76.4% mentioned that they would only disclose to a healthcare worker. Asked how they felt towards patients with TB disease, most of the respondents mentioned that they act towards them as to all other people, including trying to help them (45.1%), while one in three patients (28.5%) said they would stay away from these people because of fear of TB transmission. However, 39% of respondents acknowledged that, on the whole, the community was mostly supportive of those with TB. Overall, 71.3% (95% CI 65.3–76.6) had a good attitude towards TB.
Table 4.
Attitudes towards TB
| Variables | All Districts % (95% CI) (N = 1,799) |
Agriculturalist % (95% CI) N = 452 (25.1%) |
Pastoralists c % (95% CI) N = 982 (54.6%) |
Agro-pastoralists %(95% CI) N = 365 (20.3%) |
p-value |
|---|---|---|---|---|---|
| How would you feel if you were found to have TB? | |||||
| Negative emotions a | 10.3 (7.7, 13.7) | 14.8 (9.0, 23.2) | 11.5 (9.6, 13.8) | 4.0 (1.5, 10.6) | 0.20 |
| Both positive and negative emotions | 66.5 (58.9, 73.3) | 67.3 (59.6, 74.1) | 63.9 (49.6, 76.1) | 71.5 (65.6, 76.7) | |
| Positive emotions b | 23.2 (16.7, 31.4) | 17.9 (12.7, 24.8) | 24.6 (13.5, 40.5) | 24.5 (20.6, 28.8) | |
| Who would you talk to about your illness if you had TB? | |||||
| No one | 20.9 (17.0, 25.5) | 27.3 (20.1, 35.9) | 16.5 (11.7, 22.7) | 21.2 (16.0, 27.6) | 0.28 |
| Community member c | 2.7 (1.3, 5.3) | 2.9 (0.8, 9.9) | 3.2 (1.3, 7.3) | 1.6 (0.3, 9.4) | |
| Health care worker | 76.4 (72.2, 80.2) | 69.9 (62.1, 76.6) | 80.4 (73.7, 85.7) | 77.1 (72.3, 81.3) | |
| Which statement is closest to you feeling about people with TB disease? | |||||
| They deserve their illness | 1.5 (0.7, 3.1) | 0.8 (0.2, 2.8) | 2.3 (1.0, 5.5) | 1.0 (0.2, 5.1) | 0.04 |
| I stay away to avoid infection (though I want help them). | 55.5 (46.4, 64.3) | 43.5 (35.1, 52.3) | 55.7 (45.3, 65.6) | 67.2 (51.1, 80.1) | |
| I try to help them as I do all other people | 42.9 (34.5, 51.8) | 55.8 (46.6, 64.6) | 42.0 (32.8, 51.8) | 31.8 (19.8, 46.9) | |
| In your community, how is a person who has TB usually regarded/treated? | |||||
| Most people reject them | 8.6 (6.1, 12.0) | 7.8 (5.2, 11.6) | 10.7 (7.4, 15.2) | 5.8 (2.2, 14.4) | 0.18 |
| They are avoided by family/friends | 49.1 (44.9, 53.4) | 45.5 (38.6, 52.6) | 47.2 (40.3, 54.2) | 56.0 (48.2, 63.6) | |
| The community supports them | 37.0 (32.8, 41.4) | 41.4 (36.4, 46.6) | 38.8 (30.9, 47.3) | 29.6 (24.6, 35.1) | |
| Other | 0.5 (0.3, 0.9) | 0.7 (0.3, 2.2) | 0.1 (0.04, 0.5) | 0.9 (0.3, 2.7) | |
| Don’t know | 4.8 (2.5, 9.1) | 4.6 (2.1, 9.8) | 3.2 (1.5, 6.9) | 7.7 (2.7, 20.0) | |
| Attitude Towards TB Scores (Categorized) | |||||
| Poor Attitude (i.e. score < 60) | 28.7 (23.4, 34.7) | 27.6 (22.4, 33.5) | 24.3 (17.9, 32.1) | 36.1 (26.2, 47.4) | 0.11 |
| Good attitude (i.e. score ≥ 60) | 71.3 (65.3, 76.6) | 72.4 (66.5, 77.6) | 75.7 (67.9, 82.1) | 63.9 (52.6, 73.8) | |
a Negative emotions were described as embarrassment, shame, sadness, hopelessness, fear
b Positive emotions were described as happiness
c Community member was either a relative, neighbor, parent, close friend
Composite attitude scores
On analysis of composite attitude scores, respondents who are aged 25–34 years old were more likely to have a positive attitude towards patients with TB (aPR = 1.06, 1.00-1.11, p = 0.04) and respondents who lived 6–15 km from the health facility (aPR = 1.06, 1.01–1.11, p = 0.01) were more likely to have positive attitudes towards patients with TB. (Table 5)
Table 5.
A survey weighted generalized Poisson Model for Individual-level factors Associated with attitudes towards TB
| Variables | Unadjusted IRR (95% CI) | P-Value | Adjusted IRR (95% CI) | P-Value |
|---|---|---|---|---|
| Age | ||||
| 18–24 | Reference | Reference | ||
| 25–34 | 1.06 (1.02, 1.11) | 0.01 | 1.06 (1.00, 1.11) | 0.04 |
| 35–44 | 1.05 (0.99, 1.12) | 0.09 | 1.04 (0.98, 1.10) | 0.18 |
| 45–59 | 1.06 (1.00, 1.13) | 0.04 | 1.04 (0.98, 1.13) | 0.18 |
| 60 and above | 1.14 (1.06, 1.22) | < 0.01 | 1.08 (0.99, 1.18) | 0.10 |
| Sex | ||||
| Male | Reference | |||
| Female | 1.01 (0.98, 1.04) | 0.58 | ||
| Education | ||||
| No formal education | Reference | Reference | ||
| Primary | 0.94 (0.89, 0.99) | 0.03 | 0.97 (0.93, 1.02) | 0.23 |
| Secondary and Higher | 0.98 (0.94, 1.03) | 0.52 | 0.96 (0.89, 1.04) | 0.33 |
| Household Position | ||||
| Head | Reference | Reference | ||
| Wife | 0.96 (0.92, 1.01) | 0.08 | 0.97 (0.93, 1.00) | 0.05 |
| Son/daughter | 1.00 (0.94, 1.06) | 0.89 | 1.04 (0.96, 1.12) | 0.36 |
| Other | 0.95 (0.89, 1.02) | 0.18 | 0.94 (0.84, 1.05) | 0.29 |
| Time stayed in household | ||||
| 6–24 months | Reference | Reference | ||
| 24 or more months | 1.6 (0.98, 1.14) | 0.14 | 1.06 (0.99, 1.13) | 0.15 |
| Household size | ||||
| ≤ 5 people | Reference | |||
| 6–10 people | 1.01 (0.97, 1.04) | 0.75 | ||
| > 10 people | 0.97 (0.86, 1.10) | 0.63 | ||
| Employment Status | ||||
| Unemployed (not working) | Reference | |||
| Employed (or Working) | 0.99 (0.94, 1.04) | 0.67 | ||
| Distance to Health Facility | ||||
| ≤ 5 km | Reference | Reference | ||
| 6–15 km | 1.06 (1.02, 1.10) | < 0.01 | 1.06 (1.01, 1.11) | 0.01 |
| 16–25 km | 0.94 (0.86, 1.03) | 0.16 | 0.94 (0.85, 1.04) | 0.20 |
| > 25 km | 0.89 (0.80, 0.999) | 0.05 | 0.89 (0.78, 1.01) | 0.07 |
| Knowledge of TB | ||||
| Low TB Knowledge (i.e. <60) | Reference | Reference | ||
| High TB Knowledge (i.e. ≥60) | 1.05 (0.98, 1.14) | 0.18 | 1.06 (0.99, 1.14) | 0.12 |
Communities’ overall practices towards TB
Information about the practices of the communities is summarized in Table 6. The majority of study respondents 85.8% said they would visit a health facility as soon as they realized that they had the cardinal signs and symptoms of TB while 98.6% said they would start TB treatment immediately. Almost all respondents (98.9%) said they would opt for modern medicine to treat TB.
Table 6.
Respondents’ practices associated with TB
| Variables | All Districts % (95% CI) (n = 1,799) i |
Agriculturalist % (95% CI) N = 452 (25.1%) |
Pastoralists % (95% CI) N = 982 (54.6%) |
Agro-pastoralists % (95% CI) N = 365 (20.3%) |
p-value | ||
|---|---|---|---|---|---|---|---|
| If you had the following symptoms, cough for 2 weeks or more, night sweats, fever and some weight loss, at what point would you go to the health facility? | |||||||
| I will go immediately. | 85.8 (80.8, 89.6) | 85.4 (77.4, 91.0) | 90.0 (86.0, 92.9) | 76.2 (71.9, 80.0) | < 0.01 | ||
| I would not go if symptoms don’t get worse. | 5.9 (2.6, 12.8) | 3.7 (2.5, 5.4) | 2.5 (0.9, 6.6) | 15.4 (8.6, 26.2) | |||
| When alternative treatment does not work. | 2.3 (1.2, 4.5) | 2.4 (0.9, 5.8) | 3.1 (1.6, 5.9) | 0.5 (0.1, 2.2) | |||
| When symptoms last for 3–4 weeks. | 4.6 (2.7, 8.0) | 6.0 (2.9, 12.1) | 3.5 (1.6, 7.6) | 6.3 (2.1, 17.6) | |||
| I will not go at all. | 0.5 (0.2, 1.2) | 0.6 (0.1, 3.8) | 0.4 (0.1, 1.2) | 0.7 (0.1, 3.9) | |||
| I will go If a cultural leader tells me to | 0.8 (0.4, 1.9) | 1.9 (0.5, 7.4) | 0.5 (0.2, 1.7) | 0.8 (0.2, 3.0) | |||
| Why would you not want to go to any healthcare facility, if you had the symptoms?Multiple Response | |||||||
| Not clear that the symptoms are serious | 6.4 (3.0, 13.2) | 4.0 (1.7, 9.2) | 3.5 (1.4, 8.4) | 14.9 (7.9, 26.4) | < 0.01 | ||
| Not sure where to go | 1.5 (0.7, 3.4) | 1.1 (0.4, 3.3) | 1.3 (0.4, 4.3) | 2.4 (0.6, 9.6) | 0.61 | ||
| It will be too expensive/hard to reach | 4.8 (3.2, 7.1) | 5.5 (3.3, 9.3) | 2.3 (0.9, 5.3) | 8.4 (5.8, 12.1) | < 0.01 | ||
| Do not trust medical worker/have poor attitudes | 1.1 (0.6, 2.0) | 0.6 (0.1, 2.6) | 1.1 (0.4, 3.0) | 1.5) | 0.64 | ||
| Cannot leave work | 1.2 (0.6, 2.5) | 1.7 (0.8, 3.8) | 0.6 (0.2, 1.6) | 2.4 (0.7, 8.5) | 0.12 | ||
| If you are found to have TB would you be ready to start treatment immediately? | |||||||
| Yes | 98.6 (95.1, 99.6) | 99.7 (98.8, 99.9) | 99.5 (97.7, 99.9) | 95.1 (87.1, 98.2) | |||
| No | 1.4 (0.4, 4.9) | 0.3 (0.1, 1.2) | 0.5 (0.1, 2.3) | 4.9 (1.8, 12.9) | < 0.01 | ||
| If yes, what would you opt for? | |||||||
| Modern medicine | 98.9 (97.9, 99.4) | 97.2 (93.8, 98.7) | 99.3 (98.1, 99.7) | 99.3 (97.3, 99.8) | |||
| Traditional herbs | 0.8 (0.4, 1.7) | 2.0 (0.7, 5.5) | 0.6 (0.2, 1.7) | 0.4 (0.05, 2.9) | 0.06 | ||
| Witchdoctor | 0.1 (0.01, 0.2) | 0.2 (0.02, 1.4) | 0.00 | 0.1 (0.01, 0.5) | |||
| Others | 0.3 (0.1, 0.5) | 0.6 (0.2, 1.8) | 0.1 (0.04, 0.42) | 0.3 (0.1, 1.1) | |||
| Practices towards TB Scores (categorized) | |||||||
| Poor (i.e. score < 60) | 2.8 (1.4, 5.3) | 3.0 (1.3, 6.7) | 1.3 (0.7, 2.5) | 5.0 (1.8, 12.8) | 0.10 | ||
| Good (i.e. score ≥ 60) | 97.2 (94.7, 98.6) | 97.0 (93.3, 98.7) | 98.7 (97.5, 99.3) | 95.0 (87.2, 98.2) | |||
Composite practice scores
On analysis of composite practice scores, children in households were more likely to have good practices towards TB disease (aPR = 2.44, 95% CI 0.97–6.13, p = 0.05) whereas respondents ≥ 60 years (aPR = 0.58, 95% CI 0.39–0.86, p < 0.01) and females (aPR = 0.54, 95% CI 0.32–0.91, p = 0.02) were less likely to have good practices towards TB (Table 7).
Table 7.
A survey weighted complementary log-log model for individual-level factors associated with good practices towards TB disease
| Variables | Unadjusted OR (95% CI) | P-Value | Adjusted OR (95% CI) | P-Value |
|---|---|---|---|---|
| District Type | ||||
| Agriculturalists | Reference | |||
| Pastoralists | 1.15 (0.87, 1.54) | 0.33 | ||
| Agro-Pastoralists | 0.78 (0.52, 1.17) | 0.23 | ||
| Age | ||||
| 18–24 | Reference | Reference | ||
| 25–34 | 1.04 (0.79, 1.37) | 0.78 | 1.33 (0.86, 2.06) | 0.19 |
| 35–44 | 0.88 (0.65, 1.19) | 0.39 | 1.12 (0.71, 1.77) | 0.62 |
| 45–59 | 0.64 (0.46, 0.89) | < 0.01 | 0.85 (0.54, 1.32) | 0.46 |
| 60 and above | 0.40 (0.22, 0.72) | < 0.01 | 0.58 (0.39, 0.86) | < 0.01 |
| Sex | ||||
| Male | Reference | Reference | ||
| Female | 0.72 (0.51, 1.01) | 0.05 | 0.54 (0.32, 0.91) | 0.02 |
| Education | ||||
| No formal education | Reference | Reference | ||
| Primary | 1.40 (0.93, 2.11) | 0.11 | 1.12 (0.82, 1.53) | 0.49 |
| Secondary and Higher | 1.52 (1.01, 2.28) | 0.04 | 1.08 (0.79, 1.46) | 0.64 |
| Household Position | ||||
| Head | Reference | Reference | ||
| Wife | 1.21 (0.84, 1.77) | 0.31 | 1.60 (0.92, 2.77) | 0.09 |
| Children (i.e. Son/daughter) | 2.11 (1.31, 2.40) | < 0.01 | 2.44 (0.97, 6.13) | 0.05 |
| Household size | ||||
| ≤ 5 people | Reference | Reference | ||
| 6–10 people | 07.74 (0.52, 1.04) | 0.08 | 0.95 (0.72, 1.24) | 0.68 |
| > 10 people | 0.71 (0.52, 0.99) | 0.04 | 0.89 (0.63, 1.28) | 0.54 |
| Employment Status | ||||
| Unemployed (not working) | Reference | |||
| Employed (or Working) | 0.92 (0.63, 1.34) | 0.65 | ||
| Distance to Health Facility | ||||
| ≤ 5 km | Reference | |||
| 6–15 km | 1.08 (0.78, 1.50) | 0.64 | ||
| 16–25 km | 1.19 (0.81, 1.74) | 0.38 | ||
| > 25 km | 1.31 (0.76, 2.25) | 0.33 | ||
Note For variable “Time stayed in household”, some of the cells are empty, remembering that the prevalence was approximately 98%. So this variable was omitted. A complementary log-log model was used due to the same reason above (very high/very rare prevalence. In our case, it was extremely high ~ 98%)
Preferred modes of receiving TB education
The majority of respondents (59.3%) preferred to receive their TB information through community outreaches while 28.3% preferred to receive their TB information at the health facility (through health education talks). Almost no respondents choose electronic or print media as a means of receiving TB information Table 8.
Table 8.
Preferred mode of receiving TB education
| Variables | All Districts % (95% CI) (n = 1,799) i |
Agriculturalist District, b % (95% CI) N = 452 (25.1%) |
Pastoralists District(s), c % (95% CI) N = 982 (54.6%) |
Agro-pastoralists District, d % (95% CI) N = 365 (20.3%) |
p-value |
|---|---|---|---|---|---|
|
How would you like health information about TB delivered to you and members of your household? (one answer required) | |||||
| Community outreach | 59. 3 (50.1, 67.9) | 70.1 (59.3, 79.1) | 62.8 (52.3, 72.2) | 42.6 (31.8, 54.2) | |
| Electronic media/print | 0.2 (0.04, 0.8) | 0.6 (0.1, 3.2) | 0.02 (0.0, 0.2) | 0.1 (0.01, 0.9) | |
| Health Facility | 28.3 (22.8, 34.6) | 22.8 (17.1, 29.8) | 26.5 (18.7, 36.3) | 36.8 (29.5, 44.9) | < 0.01 |
| Others | 11.3 (7.8, 16.1) | 6.2 (2.8, 13.4) | 9.3 (6.5, 13.0) | 20.0 (15.4, 25.6) | |
| Don’t Know | 0.8 (0.4, 1.5) | 0.3 (0.1, 0.9) | 1.4 (0.6, 2.9) | 0.4 (0.091, 1.6) | |
Discussion
Overall, results from this community survey show that more than two thirds of respondents had adequate knowledge and positive practices towards TB. While knowledge of the cause and transmission of TB was mixed, knowledge of TB symptoms, diagnosis and treatment was higher. Although more than half of respondents did not know the cause of TB and more than three- quarters of respondents had the misconception that TB was transmitted in various ways including sharing of utensils and shaking hands, almost all respondents (90%) knew cough as one of the cardinal symptoms of TB. Low knowledge on the cause and transmission of TB has been reported from other community surveys in sub-Saharan Africa [9, 12–15] and has been shown to negatively affect health seeking behavior as well as contribute to stigma towards those suffering from the disease [16, 17].
However, knowledge of diagnosis and treatment was higher. Almost all respondents knew that TB should be diagnosed at a health facility and that nonadherence could result in death or worsening of disease. However, only half of all respondents knew that modern medicines were the best option for treating TB and that the correct duration of treatment was six months or longer. Other surveys in sub-Saharan Africa have also shown higher knowledge of TB diagnosis and treatment [18–21] and in developing countries, this has been linked to improved uptake of and adherence to TB treatment [22, 23]. On the other hand, one third of all respondents believed that modern medicines could be mixed with herbal medicines in the treatment of TB. This belief is prevalent in Uganda [15, 24] and may negatively affect the management of TB due to drug-drug interactions [25].
Similar to findings from Nigeria [18], high TB knowledge scores were associated with being employed and living near the health facility. This may be due to improved access to information among this group of respondents. On the other hand, low TB knowledge scores were associated with being a wife in a household and living far from the health facility, signaling limited interaction with other members of the community due to the demands of household and child care duties and or due to residing in more rural communities, which are not easily reached by community awareness messages.
In general, the community had mixed attitudes towards TB. Almost two-thirds of respondents expressed both fear and happiness towards a TB diagnosis, with the fear driven by perceived reactions of the community towards their disease. This was followed by a very low willingness to disclose a TB diagnosis to members of one’s community. High TB-associated stigma rates have also been among other communities in Ethiopia [13], the Gambia [26], and Uganda [27]. TB stigma makes patients reluctant to seek TB care services, receive a TB diagnosis, and initiate treatment for TB [28]. TB stigma also isolates patients with TB, making adherence to treatment challenging [29].
Three out of four respondents mentioned that they could prevent TB by either taking TB medicines (TB preventive therapy) or covering their mouth when they coughed. This knowledge could be leverage to improve uptake of TB preventive therapy.
Study strengths and limitations
Our study included the major societal groups in the Karamoja subregion and represented women and youth often marginalized in this community. Our findings are, therefore, generalizable to this subregion. However, our study, which mainly relied on self-reported patient attitudes and practices is consequently liable to desirability bias, leading to an overestimation of positive responses. We used trained and experienced data collectors who speak the local languages used in the Karamoja subregion to reduce the likelihood of this happening. We also interviewed patients individually and maintained the anonymity of patient responses.
Conclusion
More than two thirds of patients had good knowledge and practices towards TB which can be leveraged to improve uptake of TB control interventions in the region. Additional interventions to improve TB knowledge and practice should focus on community education on cause and transmission of TB and should focus on specific segments within the communities e.g., older women in the households.
Recommendations
To increase the uptake of TB healthcare services in the region, increased focus should be placed on community sensitization on TB’s cause and transmission. This should be prioritized, especially for women and people in remote communities. Community sensitization should be carried out through community outreaches or health-facility-based health talks since these are the most preferred means of health education. In addition, evidence-based interventions to reduce TB-related stigma, e.g., community education and forming community-based support groups for patients and their families should be implemented.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We acknowledge the Uganda Ministry of Health (MoH) and the National TB and Leprosy Program for their support towards the execution of this study. We thank the United States Agency for International Development for funding this study. We thank all the district health officers and health facility managers for the assistance rendered to the Investigators. Finally, we thank all members of the communities where this study was carried. We thank the community leaders who guided the research assistants during the household visits and the respondents for sparing time to respond to our inquiry.
Abbreviations
- TB
Tuberculosis
- WHO
World Health Organisation
- ART
Antiretroviral Treatment
- HIV
Human Immunodeficiency Virus
- MOH
Ministry of Health
- USAID-PACT
UCST: Uganda National Council for Science and Technology
Author contributions
WK, AE and SZM conceptualized and designed the study. KW and SZM obtained data. EM and JM analyzed and interpreted data. WK and SZM drafted the manuscript. SZM, WK, TN, JM, JL, PS, ST, CA, TS, MM, ER and MGNM performed critical revisions. All authors read and approved the final manuscript.
Funding
The study was funded by the USAID PACT Karamoja project. Grant Number: 72061720CA00003.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon written request.
Declarations
Ethical approval and consent to participate
Ethical approval for this study was granted by the Makerere University Infectious Diseases Institute Research and Ethics Committee (Ref: 010/202) and the Uganda National Council for Science and Technology (Ref: HS2342ES). We obtained administrative clearance from each district before conducting the study. Finally, we obtained written informed consent from all study respondents before their participation. Informed consent was obtained in English or one of three languages commonly spoken in the area (Karamojong, Swahili or Pokot). For participants who could not read and write, we obtained Informed consent in the presence of an independent witness who could read and write.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO. Global tuberculosis report 2022: Geneva.
- 2.WHO. WHO Global Tuberculosis Report and reflects:high Burden TB Country List 2020. Geneva; 2019.
- 3.Houdet J, Muloopa H, Ochieng C, et al. Cost benefit analysis of the mining sector in Karamoja, Uganda. Kampala, Uganda: IUCN Uganda Country Office. ix + 82p; 2014. [Google Scholar]
- 4.Lorent N, Choun K, Thai S, et al. Community-based active tuberculosis case finding in poor urban settlements of Phnom Penh, Cambodia: a feasible and effective strategy. PLoS ONE. 2014;9(3):e92754. 10.1371/journal.pone.0092754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Uganda Bureau of Statistics., The 2014 Uganda Population and Housing Census [Internet]. Vol. VII. 2014. http://www.ubos.org/onlinefiles/uploads/ubos/NPHC/NPHC 2014 PROVISIONAL RESULTS REPORT.pdf. 2014.
- 6.Boru CG, Shimels T, Bilal AI. Factors contributing to non-adherence with treatment among TB patients in Sodo Woreda, Gurage Zone, Southern Ethiopia: a qualitative study. J Infect Public Health. 2017;10(5):527–33. 10.1016/j.jiph.2016.11.018 [DOI] [PubMed] [Google Scholar]
- 7.USAID-PACT. USAID-Programme for Accerelated Control of Tuberculosis in Karamoja: Project baseline assesment report; April 2020. 2020.
- 8.Kaplan R, Caldwell J, Hermans S, et al. An integrated community TB-HIV adherence model provides an alternative to DOT for Tuberculosis patients. Cape Town. 2016;20(9):1185–91. [DOI] [PubMed] [Google Scholar]
- 9.Datiko DG, Habte D, Jerene D, et al. Knowledge, attitudes, and practices related to TB among the general population of Ethiopia: findings from a national cross-sectional survey. PLoS ONE. 2019;14(10):e0224196. 10.1371/journal.pone.0224196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oppel E-M, Winter V, Schreyögg J. Evaluating the link between human resource management decisions and patient satisfaction with quality of care. Health Care Manage Rev. 2017;42(1):53–64. 10.1097/HMR.0000000000000087 [DOI] [PubMed] [Google Scholar]
- 11.Kazaura M, Kamazima SR. Knowledge, attitudes and practices on tuberculosis infection prevention and associated factors among rural and urban adults in northeast Tanzania: a cross-sectional study. PLOS Global Public Health. 2021;1(12):e0000104. 10.1371/journal.pgph.0000104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bati J, Legesse M, Medhin G. Community’s knowledge, attitudes and practices about tuberculosis in Itang special district, Gambella region, south western Ethiopia. BMC Public Health. 2013;13(1):734. 10.1186/1471-2458-13-734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sima BT, Belachew T, Abebe F. Knowledge, attitude and perceived stigma towards tuberculosis among pastoralists; do they differ from sedentary communities? A comparative cross-sectional study. PLoS ONE. 2017;12(7):e0181032. 10.1371/journal.pone.0181032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mbuthia GW, Olungah CO, Ondicho TG. Knowledge and perceptions of tuberculosis among patients in a pastoralist community in Kenya: a qualitative study. Pan Afr Med J, 2018. 30(1). [DOI] [PMC free article] [PubMed]
- 15.Obuku EA, Meynell C, Kiboss-Kyeyune J, et al. Socio-demographic determinants and prevalence of Tuberculosis knowledge in three slum populations of Uganda. BMC Public Health. 2012;12:1–9. 10.1186/1471-2458-12-536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Castelnuovo B. Review of compliance to anti tuberculosis treatment and risk factors for defaulting treatment in Sub Saharan Africa. Afr Health Sci, 2010. 10(4). [PMC free article] [PubMed]
- 17.Kankya C, Mugisha A, Muwonge A et al. Myths, perceptions knowledge, attitudes, and practices (KAP) linked to mycobacterial infection management among the pastoralist communities of Uganda. 2011.
- 18.Balogun MR, Sekoni AO, Meloni ST et al. Predictors of Tuberculosis knowledge, attitudes and practices in urban slums in Nigeria: a cross-sectional study. Pan Afr Med J, 32 2019. [DOI] [PMC free article] [PubMed]
- 19.Kazoora H, Majalija S, Kiwanuka N, et al. Knowledge, attitudes and practices regarding risk to human infection due to Mycobacterium bovis among cattle farming communities in western Uganda. Zoonoses Public Health. 2016;63(8):616–23. 10.1111/zph.12273 [DOI] [PubMed] [Google Scholar]
- 20.Legesse M, Ameni G, Mamo G, et al. Knowledge and perception of pulmonary tuberculosis in pastoral communities in the middle and Lower Awash Valley of Afar region, Ethiopia. BMC Public Health. 2010;10(1):187. 10.1186/1471-2458-10-187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cramm JM, Finkenflügel HJ, Møller V, et al. TB treatment initiation and adherence in a South African community influenced more by perceptions than by knowledge of tuberculosis. BMC Public Health. 2010;10(1):1–8. 10.1186/1471-2458-10-72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Anggraini MT, Lahdji A, Akbari FZ. The Relationship Between Knowledge And Attitudes With Adherence To Taking Medication For Pulmonary Tuberculosis Patients. in Proceeding International Seminar of Community Health and Medical Sciences (ISOCMED). 2022.
- 23.Tola HH, Azar T, Shojaeizadeh D, et al. Tuberculosis treatment non-adherence and lost to follow up among TB patients with or without HIV in developing countries: a systematic review. Iran J Public Health. 2015;44(1):1. [PMC free article] [PubMed] [Google Scholar]
- 24.Buregyeya E, Kulane A, Colebunders R, et al. Tuberculosis knowledge, attitudes and health-seeking behaviour in rural Uganda. Int J Tuberculosis Lung Disease. 2011;15(7):938–42. 10.5588/ijtld.10.0211 [DOI] [PubMed] [Google Scholar]
- 25.Gorman G. Mechanisms and implication of drug-herbal interactions. Bioequivalence Bioavailab. 2012;4:13–4. [Google Scholar]
- 26.Bashorun AO, Linda C, Omoleke S, et al. Knowledge, attitude and practice towards tuberculosis in Gambia: a nation-wide cross-sectional survey. BMC Public Health. 2020;20:1–13. 10.1186/s12889-020-09685-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Macfarlane L, Newell JN. A qualitative study exploring delayed diagnosis and stigmatisation of Tuberculosis amongst women in Uganda. J Int Health. 2012;4(2):143–7. 10.1016/j.inhe.2011.12.002 [DOI] [PubMed] [Google Scholar]
- 28.Zawedde-Muyanja S, Manabe YC, Cattamanchi A, et al. Patient and health system level barriers to and facilitators for tuberculosis treatment initiation in Uganda: a qualitative study. BMC Health Serv Res. 2022;22(1):831. 10.1186/s12913-022-08213-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yang W-T, Gounder CR, Akande T et al. Barriers and delays in tuberculosis diagnosis and treatment services: does gender matter? Journal of Tuberculosis research treatment, 2014. 2014. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon written request.