Abstract
Background
Thyroid disorders(TD) poses a significant health threat to Americans due to its high incidence rate. Obesity, a common factor linked to thyroid disorders, has garnered increasing attention. While Body mass index (BMI) is a widely used obesity index, it fails to account for the distribution of muscle and fat in the body. Recently, tMFR has emerged as a crucial obesity index in clinical research, warranting further investigation into its association with TD.
Objective
Exploring the association between tMFR and thyroid disorders.
Method
A comprehensive survey and data analysis were conducted using the NHANES database to investigate the relationship between tMFR and the risk of TD. This study utilized multiple logistic regression, smooth curve fitting, and subgroup analysis across four periods from 2011 to 2018.
Result
A total of 11,912 subjects were included in the study, showing a prevalence of 7.14% for TD. The research indicated that tMFR had an inverse correlation with the risk of TD in a comprehensive model (OR = 0.90, 95% CI 0.82 to 1.00). When tMFR was divided into quartiles (Q1-Q4), individuals in the highest quartile had a 28% lower risk of TD than those in Q1 (OR = 0.72, 95% CI 0.57 to 0.91). Analysis using smoothed curve fitting demonstrated a nonlinear relationship between tMFR and TD risk, with the inflection point for tMFR saturation effect identified as 1.5. Subgroup analysis further confirmed the strong association between tMFR and TD risk. Receiver operating characteristic (ROC) curve analysis indicated that tMFR exhibited superior predictive ability for TD relative to BMI.
Conclusion
The study found a negative association between tMFR and the risk of TD; however, additional prospective studies are required to validate these findings.
Keywords: TD, tMFR, Obesity index, Cross-sectional study, NHANES
Introduction
Thyroid disorders(TD) is a prevalent condition within the endocrine system, encompassing various forms such as hyperthyroidism, hypothyroidism, nodule formation, autoimmune inflammation, and tumors. The occurrence of goiter can reach up to 80% in regions with significant iodine deficiency, whereas autoimmune TD is more common in areas with adequate iodine levels [1]. According to the American Thyroid Association (ATA), approximately 12% of Americans experience TD at some point in their lives [2]. A large cross-sectional study of 57,540 respondents in the United States revealed a consistent increase in the prevalence of TD from 1999 to 2018 [3]. Despite advancements in treatment, the specific risk factors for these diseases remain unclear [4]. This underscores the critical need for more comprehensive research on the development and prevention of TD.
Obesity has been identified as a significant risk factor for dominant hypothyroidism, subclinical hypothyroidism, and Hashimoto’s thyroiditis [4, 5]. On the other hand, sarcopenia is characterized by an age-related decrease in muscle mass and reduced physical activity, which is closely linked to thyroid hormones [6, 7]. Prior studies have used BMI and waist circumference as indicators of obesity severity; however, these metrics do not distinguish between muscle and fat distribution within the body. As such, there is a need for a more comprehensive assessment to understand the impact of obesity on thyroid health. These new indicators can offer insights into how different body components influence the prevalence of TD, leading to more effective strategies for disease prevention and treatment.
The pathogenesis of TD is intricate, with obesity being recognized as a significant factor. In recent years, the total body muscle-fat ratio (tMFR) has emerged as a novel obesity index in clinical studies [8–10]. Despite advancements in obesity research, there is a lack of exploration into the potential correlation between tMFR and TD. This study utilized data from the National Health and Nutrition Examination Survey (NHANES) to calculate tMFR based on precise measurements of total muscle mass and total body fat mass using dual-energy X-ray absorptiometry (DXA). The aim of this study is to uncover the possible connection between tMFR and TD, thereby enhancing the scientific foundation for managing obesity and TD holistically and developing more accurate and effective treatment strategies for patients.
Materials and methods
Study population
NHANES is an ongoing national study that has collected a vast amount of data on Americans’ dietary habits and overall health [11]. Before gathering data, participants gave written consent, and the National Center for Health Statistics Ethics Review Board approved the protocol [12]. The data for this study were obtained from the NHANES 2011–2018 cross-sectional survey, which gathered information on TD, tMFR, and demographics. After excluding incomplete tMFR data, missing covariates, and TD questionnaires, the final cohort consisted of 11,912 participants (Fig. 1).
Fig. 1.
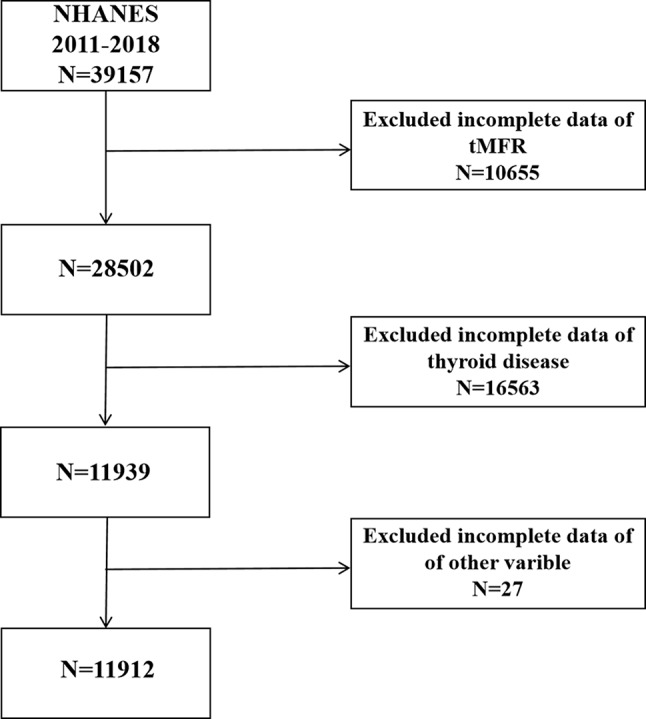
Flowchart of participant selection
Measurement of tMFR
DXA is the preferred method for measuring body composition in NHANES due to its efficiency, user-friendliness, and minimal radiation exposure [13, 14]. Total muscle mass and whole body fat mass are assessed using DXA on a Hologic Discovery Model A densitometer with Apex 3.2 software. The tMFR is calculated as total muscle mass divided by total body fat mass. Exclusions for DXA testing include pregnant individuals, those weighing over 450 pounds, individuals taller than 6 feet 5 inches, and those who have had radiocontrast (barium) within the past 7 days. Additionally, individuals younger than 20 and older than 59 will be excluded from DXA testing.
Evaluation of TD
TD status was ascertained through a self-reported medical condition questionnaire during individual interviews. The NHANES questionnaire item for TD is MCQ 160m, which asks ‘Have you ever been informed of having thyroid problems?’ Respondents answering yes were categorized into the TD group, those answering no were classified as the control group, and ‘don’t know’ or refusal to answer resulted in missing data.
Covariates
This study considered potential confounding variables in the relationship between tMFR and TD, such as sex (Male, Female), age (Years), ethnicity (Mexican American/Other Hispanic/Non-Hispanic White/Non-Hispanic Black/Other Race), education level (Less Than 9th Grade/9-11th Grade/High School Grad/GED or Equivalent/Some College or AA degree/College Graduate or above), marital status (Married/Widowed/Divorced/Separated/Never married), history of diabetes (Yes/No), hypertension (Yes/No), high cholesterol (Yes/No), smoking status (≥ 100 cigarettes in life/< 100 cigarettes in life), alcohol consumption (≥ 12 drinks/year or < 12 drinks/year), and depression (PHQ < 9/PHQ ≥ 9).
Statistical analysis
Statistical analysis was conducted in accordance with NHANES guidelines. Categorical variables were presented as total numbers (n) and percentages (%), while continuous variables were reported as mean ± standard deviation. To compare differences in various factors among the total group, control group, and TD group, we utilized a variety of statistical tests. T-tests and one-way ANOVA were used for continuous variables to assess group differences, while chi-square tests were employed for categorical variables. The selection of these tests was based on the distribution and nature of the data. Specifically, t-tests were utilized for normally distributed continuous variables, one-way ANOVA for comparing means across multiple groups, and chi-square tests for evaluating associations between categorical variables. We utilized three distinct multivariate logistic regression models to examine the connections between tMFR and TD.The models included different levels of adjustment for covariates, starting from an unadjusted model to a fully adjusted model. Smooth curve fitting was then employed to examine the potential nonlinear relationship between tMFR and TD. Subgroup analyses and interactions were also performed for age, sex, race, and categorical variables among the covariates, while controlling for the specified confounders. Statistical analysis was carried out using EmpowerStats and R language (version 4.2.1), with statistical significance set at P < 0.05.
Results
Baseline characteristics
The study included a total of 11,912 subjects, with an average age of 39.52 ± 11.5 years. Among them, 6,040 (50.71%) were male and 5,872 (49.29%) were female. Out of all participants, 851 were reported to have TD, resulting in a prevalence of 7.14%. Statistical significance (P < 0.05) was observed in factors such as age, sex, race, marital status, education level, tMFR, high blood pressure level, high cholesterol level, diabetes, and depression when comparing them with the TD group (Table 1).
Table 1.
Baseline characteristics of participants N = 11,912, NHANES, USA, 2011–2018
| Variable | Total N = 11,912 | Control group N = 11,061 | TD group N = 851 | P |
|---|---|---|---|---|
| Age, Mean(SD), Year | 39.52(11.50) | 39.13 (11.49) | 44.71 (10.42) | < 0.001 |
| Sex (%) | < 0.001 | |||
| Male | 6,040 | 5869 (53.06%) | 171 (20.09%) | |
| Female | 5,872 | 5192 (46.94%) | 680 (79.91%) | |
| Race (%) | < 0.001 | |||
| Mexican American | 1686 | 1599 (14.46%) | 87 (10.22%) | |
| Other Hispanic | 1207 | 1121 (10.13%) | 86 (10.11%) | |
| Non-Hispanic White | 4145 | 3772 (34.10%) | 373 (43.83%) | |
| Non-Hispanic Black | 2665 | 2517 (22.76%) | 148 (17.39%) | |
| Other Race | 2209 | 2052 (18.55%) | 157 (18.45%) | |
| Marital Status (%) | < 0.001 | |||
| Married | 5786 | 5327 (48.16%) | 459 (53.93%) | |
| Widowed | 163 | 152 (1.37%) | 11 (1.29%) | |
| Divorced | 1099 | 985 (8.91%) | 114 (13.40%) | |
| Separated | 428 | 386 (3.49%) | 42 (4.94%) | |
| Never married | 3104 | 2937 (26.55%) | 167 (19.62%) | |
| Living with partner | 1332 | 1274 (11.52%) | 58 (6.82%) | |
| Education Level (%) | 0.003 | |||
| Less Than 9th Grade | 719 | 688 (6.22%) | 31 (3.64%) | |
| 9-11th Grade | 1457 | 1353 (12.23%) | 104 (12.22%) | |
| High School Grad/GED or Equivalent | 2602 | 2425 (21.92%) | 177 (20.80%) | |
| Some College or AA degree | 3903 | 3633 (32.85%) | 270 (31.73%) | |
| College Graduate or above | 3231 | 2962 (26.78%) | 269 (31.61%) | |
| tMFR, Mean(SD) | 2.095 (1.061) | 1.81 (0.70–8.64) | 1.46 (0.65–6.75) | < 0.001 |
| Q1(0.65–1.38) | 2978 | 2609 (23.59%) | 369 (43.36%) | |
| Q2(1.39–1.77) | 2978 | 2766 (25.01%) | 212 (24.91%) | |
| Q3(1.78–2.42) | 2978 | 2818 (25.48%) | 160 (18.80%) | |
| Q4(2.43–8.63) | 2978 | 2868 (25.93%) | 110 (12.93%) | |
| High Blood Pressure Level(%) | < 0.001 | |||
| Yes | 2899 | 2598 (23.49%) | 301 (35.37%) | |
| No | 9013 | 8463 (76.51%) | 550 (64.63%) | |
| High Cholesterol Level (%) | < 0.001 | |||
| Yes | 2928 | 2567 (23.21%) | 361 (42.42%) | |
| No | 8930 | 8448 (76.38%) | 482 (56.64%) | |
| NA | 54 | 46 (0.42%) | 8 (0.94%) | |
| Diabetes (%) | < 0.001 | |||
| Yes | 892 | 775 (7.01%) | 117 (13.75%) | |
| No | 10,798 | 10,099 (91.30%) | 699 (82.14%) | |
| NA | 222 | 187 (1.69%) | 35 (4.11%) | |
| Smoking Status (%) | 0.11 | |||
| ≥ 100 cigarettes in life | 4718 | 4359 (39.41%) | 359 (42.19%) | |
| <100 cigarettes in life | 7194 | 6702 (60.59%) | 492 (57.81%) | |
| Alcohol Consumption Status | 0.06 | |||
| ≥ 12 drink/year | 1548 | 1448 (13.09%) | 100 (11.75%) | |
| < 12 drink/year | 8175 | 7605 (68.76%) | 570 (66.98%) | |
| NA | 2189 | 2008 (18.15%) | 181 (21.27%) | |
| Depression | < 0.001 | |||
| PHQ < 9 | 6384 | 5950 (53.79%) | 434 (51.00%) | |
| PHQ ≥ 9 | 1100 | 942 (8.52%) | 158 (18.57%) | |
| NA | 4428 | 4169 (37.69%) | 259 (30.43%) |
Continuous variables with normal distributions: means and standard deviations
Continuous variables with skewness: medians and interquartile ranges
Categorical variables: frequencies and percentages
NA: Not available
Power analysis
To ensure that our sample size was adequate for detecting the effects of interest, we conducted a power analysis using G*Power. We established the significance level (α) at 0.05 and the desired power at 0.80. Assuming an odds ratio of 0.90 and a baseline probability of 0.10, the required sample size was calculated to be 8717 participants. Our study included 11,912 participants, which is significantly larger than the required sample size, indicating that our study is sufficiently powered to detect the association between tMFR and the risk of TD.
Analyzing the association between tMFR and risk of TD through logistic regression
A multivariate logistic regression model was utilized to examine the relationship between tMFR and the probability of TD occurrence. Two models, partially adjusted and fully adjusted, were developed to account for potential confounders. The partially adjusted model included demographic variables like age, gender, and race, selected for their established links to the outcomes studied. The fully adjusted model expanded on this by incorporating lifestyle factors (e.g., smoking, alcohol consumption), clinical parameters (e.g., blood pressure, cholesterol), and other relevant confounders from existing literature. By including these variables, the aim was to minimize residual confounding and enhance the accuracy of the associations observed.
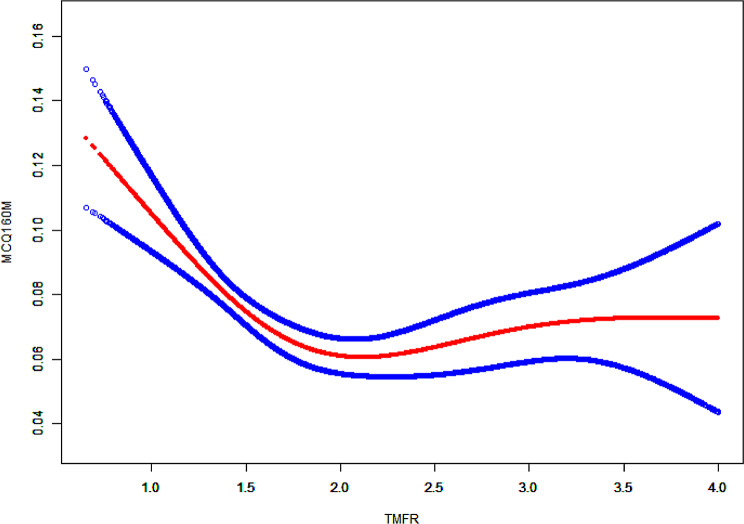
The unadjusted model [odds ratio (OR) = 0.60, 95% confidence interval (CI) 0.54 to 0.66] and partially adjusted model [OR = 0.85 CI 0.77 to 0.94)] both showed a significant negative correlation between tMFR and TD. The fully adjusted model indicated that for each unit increase in tMFR, the risk of TD decreased by 10% [OR = 0.90, CI 0.82 to 1.00)], with statistical significance (P = 0.0415). Refer to Table 2 for details. Interestingly, the results of the tMFR quartiles in this model did not exhibit an equally decreasing trend, revealing a nonlinear negative correlation between tMFR and the risk of TD. This was further illustrated through smooth curve fitting in Fig. 2.
Table 2.
Association between tMFR and TD
| Exposure | Non-adjusted model OR,95%,P |
Minimally-adjusted model OR,95%,P |
Fully-adjusted model OR,95%,P |
|---|---|---|---|
| tMFR | 0.60 (0.54, 0.66) < 0.0001 | 0.85 (0.77, 0.94) 0.0010 | 0.90 (0.82, 1.00) 0.0415 |
| tMFR (Quartile) | |||
| Q1(0.65–1.38) | Ref | Ref | Ref |
| Q2(1.39–1.77) | 0.57 (0.49, 0.68) < 0.0001 | 0.74 (0.62, 0.87) 0.0005 | 0.78 (0.66, 0.93) 0.0057 |
| Q3(1.78–2.42) | 0.43 (0.36, 0.52) < 0.0001 | 0.71 (0.58, 0.86) 0.0006 | 0.78 (0.63, 0.95) 0.0126 |
| Q4(2.43–8.63) | 0.30 (0.24, 0.37) < 0.0001 | 0.63 (0.50, 0.79) < 0.0001 | 0.72 (0.57, 0.91) 0.0060 |
Non-adjusted model: no covariates were adjusted
Minimally-adjusted model: adjusted for age, sex, and race
Fully-adjusted model: adjusted for age, sex, race, marital status, education level, high blood pressure, high cholesterol level, diabetes, smoking status, alcohol consumption status, depression
Fig. 2.
Smooth curve fitting of tMFR and risk of TD
The solid red line represents the smoothed curve fitting between variables, while the dashed blue line represents the 95% confidence interval of the fit.
Saturation effect analysis
To pinpoint the inflection point of the curve, analyses were carried out to assess both threshold and saturation effects. The threshold effect signifies the point at which the relationship between exposure and outcome starts to shift, while the saturation effect occurs when further increases in exposure no longer influence the outcome. The results indicated a saturation effect at tMFR equal to 1.5, as outlined in Table 3. A two-piecewise linear regression approach was employed to explore potential non-linear relationships between the exposure and outcome variables. The inflection point at 1.5 was identified through segmented regression analysis, where two distinct lines were fitted to the data before and after the inflection point to determine the change in slope. The segmented regression analysis was performed using R language (version 4.2.1), and the inflection point was verified through both visual examination of the plotted data and statistical criteria.
Table 3.
Non-linearity addressing of tMFR and TD
| Outcome | OR,95%CI, P value |
|---|---|
| Fitting model by standard linear regression | 0.90 (0.81, 0.99) 0.0385 |
| Fitting model by two-piecewise linear regression | |
| Inflection point | 1.5 |
| < 1.5 | 0.38 (0.25, 0.59) < 0.0001 |
| > 1.5 | 1.01 (0.91, 1.14) 0.8084 |
| P for log likelyhood ratio test | < 0.001 |
We adjusted for all covariates presented in Table 1
Subgroup analysis
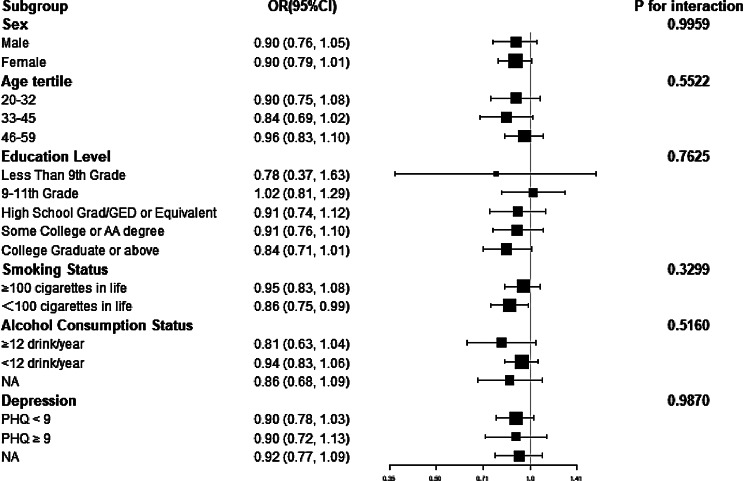
Subgroup and interaction analyses were conducted to investigate potential variations in associations across different subpopulations and to identify any factors that might modify the effects. Subgroups were categorized based on demographic characteristics (e.g., age, gender), lifestyle factors (e.g., smoking status, alcohol consumption), and other relevant variables. Interaction terms were generated by multiplying the primary exposure variable with subgroup indicators, which were then integrated into regression models to determine if the relationship between exposure and outcome differed within subgroups. Statistical tests for interaction were performed using likelihood ratio tests, comparing models with and without interaction terms. Specifically, we assessed risk across various age groups (20–32/33–45/46–59), genders (Male, Female), education levels (Less Than 9th Grade/9-11th Grade/High School Grad/GED or Equivalent/Some College or AA degree/College Graduate or above), smoking status (yes/no), alcohol consumption (yes/no), and presence of depression (yes/no) through subgroup and cross analysis. The results revealed a significant association between tMFR and the risk of TD, with all interactions showing P > 0.05 (Fig. 3).
Fig. 3.
Subgroup and interaction analysis of the relationship between tmfr and TD risk
Multiple comparison correction
Due to the numerous subgroup analyses and interaction tests conducted in this study, we applied the Bonferroni correction to mitigate the increased risk of Type I errors (false positives). A total of 18 comparisons were performed. Using the Bonferroni correction method, the adjusted significance level for each test was calculated as follows: Aadj =0.05/18 = 0.00277. After applying the Bonferroni correction, none of the p-values fell below the adjusted significance level of 0.00277. Consequently, no results from the interaction tests can be deemed statistically significant after correction, which reinforces the robustness of the subgroup analysis results.
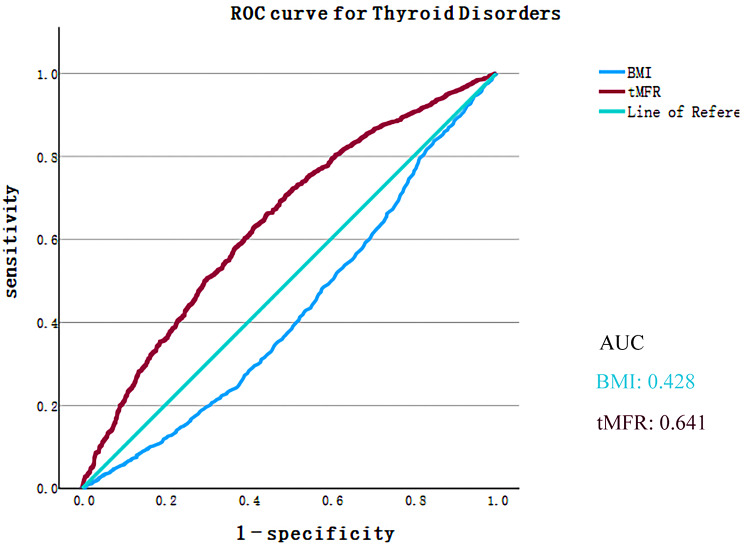
Receiver operating characteristic (ROC) curve analysis
To further evaluate the efficacy of tMFR in predicting TD risk, ROC curve analysis was conducted comparing BMI and tMFR. The results indicated that tMFR demonstrated a superior predictive ability for TD compared to BMI, with AUC values (95% CI) for the anthropometric parameters as follows: tMFR: 0.641 (0.622–0.660) and BMI: 0.428 (0.407–0.449) (Fig. 4).
Fig. 4.
ROC curve analysis for predicting TD
Discussion
The results of this large cross-sectional study involving 11,912 adults indicated a negative correlation between tMFR and the risk of TD, with a nonlinear relationship observed. Specifically, the study revealed a significant negative correlation when tMFR values were less than 1.5, as determined through threshold effect and saturation effect analysis. Subgroup and interaction analyses further supported the robustness of these findings. These results are crucial for enhancing our understanding of the intricate nature of TD risk and for developing more precise predictive models.
As a novel obesity index, tMFR has been associated with chronic kidney disease and has been shown to predict the risk of endocrine disorders such as metabolic syndrome and insulin resistance [15, 16]. However, to date, no studies have explored the relationship between tMFR and TD.The calculation of tMFR involves dividing the total muscle mass of the body by the total fat mass. The findings of this research demonstrated an inverse relationship between tMFR and TD susceptibility, suggesting that a higher muscle mass and lower fat mass were correlated with decreased TD risk. Various studies have recognized obesity as a substantial contributing factor to TD susceptibility [17–19]. However, previous research primarily relied on BMI to assess obesity, overlooking the impact of muscle to fat ratio on the body. As a more comprehensive and precise measure of obesity, tMFR may better depict the relationship between obesity and TD. We further substantiate this argument by constructing ROC curves. These findings illuminate the intricate connection between obesity and TD, offering new perspectives for future investigations.
Although the cross-sectional nature of our research prevents the establishment of causality, several potential mechanisms may elucidate the observed relationship between tMFR and TD. Firstly, adipose tissue functions not merely as a storage organ but also as an endocrine organ that secretes various hormones and cytokines [20]. An increase in adipose tissue may result in an imbalance of these hormones and factors, thereby affecting thyroid function and elevating the risk of TD [21, 22]. Secondly, higher muscle mass is associated with improved metabolic health. Muscle tissue can influence systemic metabolism and inflammation through the secretion of myokines, such as myostatin, which may aid in maintaining healthy thyroid function [23, 24].Chronic low-grade inflammation, often linked to obesity, could adversely impact thyroid function [25].Furthermore, obesity and low muscle mass are closely associated with insulin resistance, which may influence thyroid function through various pathways, including alterations in the metabolism and action of thyroid hormones [26, 27]. Lastly, the imbalance between adipose and muscle tissues may result in hormonal disturbances, such as those involving sex hormones and cortisol, which play a crucial role in thyroid function [28].These potential mechanisms highlight the intricate interplay between body composition and thyroid health. Future studies, particularly those employing longitudinal and experimental designs, are necessary to further clarify these mechanisms and establish causality.
These findings have several potential implications for clinical practice: (1) Screening and Risk Assessment: tMFR could serve as an additional metric for screening TD risk, particularly in individuals with obesity or metabolic syndrome. Incorporating tMFR into routine assessments may facilitate the identification of individuals at heightened risk for TD. (2) Interventions: Interventions designed to enhance muscle mass, such as resistance training and dietary modifications, could prove beneficial in mitigating TD risk. Clinicians should consider recommending lifestyle changes that promote muscle mass increase and fat mass reduction as part of a comprehensive approach to thyroid health management. (3) Personalized Medicine: Gaining insights into individual body composition profiles could assist in tailoring personalized treatment plans for TD, thereby optimizing outcomes based on specific patient characteristics.
Due to constraints inherent in Dual-Energy X-ray Absorptiometry (DXA) measurements, we were unable to include participants outside the specified age range. This limitation has implications for the generalizability of our findings.The exclusion of younger and older age groups suggests that our results may not fully capture the relationship between tMFR and TD risk across the entire lifespan. For example, adolescence represents a critical period characterized by hormonal changes and rapid growth, which may influence muscle and fat distribution as well as thyroid function [29]. Similarly, older adults often experience sarcopenia (the loss of muscle mass) and alterations in fat distribution, potentially impacting thyroid health in ways that differ from those observed in younger adults [30].The metabolic and endocrine systems undergo significant transformations throughout life, and these changes can modulate the relationship between body composition and thyroid function. Consequently, our findings are primarily applicable to the adult population within the defined age range and may not be representative of the effects in younger or older individuals.To address this limitation, future studies should aim to include a broader age range, encompassing both adolescents and older adults. Longitudinal studies that track changes in tMFR and thyroid health over time across various age groups would provide a more comprehensive understanding of how age-related changes in body composition impact thyroid function.
This study has multiple strengths. Firstly, the data is sourced from NHANES, encompassing 11,912 samples that represent a diverse range of social classes and ethnicities in the United States. Additionally, by excluding confounding factors, we were able to establish a nonlinear relationship between tMFR and the risk of TD. The identification of the curve’s inflection point through threshold effect and saturation effect analysis enhanced the clinical relevance of our findings. Furthermore, the robustness of the results was confirmed through subgroup analyses and cross-tests stratified by various factors including age, sex, education level, smoking status, alcohol use status, and depression.
The study has several limitations. Firstly, it was conducted in a cross-sectional manner, which means that no causal relationship between exposure factors and outcomes could be determined. Secondly, the use of dxa to measure total body muscle mass and total body fat in the NHANES database was limited to people aged 20–59, therefore the results may not be generalizable to individuals outside this age range. Thirdly, the sample size that included objective measurements of thyroid function (TSH, T3, T4) during our study period was limited, and there was no feasible method to classify TD more accurately through clinical diagnosis or thyroid function testing. Finally, NHANES primarily gathers cross-sectional data, which means it collects information from each participant at a single point in time; consequently, it is challenging to gain insights into tMFR over time and the risk of TD through longitudinal data.
Future research should expand the age range to encompass both adolescents and older adults, as hormonal changes and sarcopenia may differentially influence thyroid function in these populations. Furthermore, longitudinal studies are crucial for establishing causality and for elucidating how variations in tMFR impact thyroid health over time. Additionally, incorporating objective measures of thyroid function, such as TSH, T3, and T4, alongside self-reported TD status, will enhance the accuracy of the findings. Randomized controlled trials aimed at examining changes in body composition could further clarify the benefits of optimizing muscle and fat distribution for thyroid health. These research directions will improve the generalizability and applicability of our findings.
Conclusion
This study analyzed 11,912 samples from four NHANES cycles (2011–2018) and identified a negative correlation between tMFR and TD risk. Further prospective studies and animal experiments are required to confirm this relationship. These investigations will enhance our understanding of how tMFR influences TD risk, offering more robust scientific support for future clinical approaches and therapies.
Acknowledgements
We would like to thank all participants in this study.
Abbreviations
- ATA
American Thyroid Association
- NHANES
National Health and Nutrition Examination Survey
- BMI
Body mass index
- CI
Confidence interval
- DXA
Dual-energy X-ray absorptiometry
- OR
Odds ratio
- ROC
Receiver operating characteristic
- TD
Thyroid disorders
- TSH
Thyroid stimulating hormone
- tMFR
Total body muscle-fat ratio
Author contributions
Ziming Wang, Xu Jiao, Yun Lu and Xu Jiao designed the research. Ziming Wang, Mingfei Li, Yifan Miao, Yang Wang, Xu Jiao, Yun Lu collected, analyzed the data, and drafted the manuscript. Hao Chen, Shuang Zhao and Shihan Guo revised the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This research was funded by Sichuan Province Administration of Traditional Chinese Medicine (Document No.31 of Sichuan Province Finance Department in 2021).
Data availability
The National Health and Nutrition Examination Survey dataset is publicly available at the National Center for Health Statistics of the Center for Disease Control and Prevention (https://www.cdc.gov/nchs/nhanes/index.htm). Data used in the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
The portions of this study involving human participants, human materials, or human data were conducted in accordance with the Declaration of Helsinki and were approved by the NCHS Ethics Review Board. The patients/participants provided their written informed consent to participate in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Ziming Wang and Mingfei Li contributed equally to this article.
Contributor Information
Hao Chen, Email: 1415949133@qq.com.
Yun Lu, Email: 0550@cdutcm.edu.cn.
References
- 1.Vanderpump MP. The epidemiology of thyroid disease. BRIT MED BULL. 2011;99:39–51. 10.1093/bmb/ldr030 [DOI] [PubMed] [Google Scholar]
- 2.Ji S. SSC: the novel self-stack ensemble model for thyroid disease prediction. PLoS ONE. 2024;19(1):e295501. 10.1371/journal.pone.0295501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang X, Wang X, Hu H, Qu H, Xu Y, Li Q. Prevalence and trends of thyroid disease among adults, 1999–2018. Endocr Pract. 2023;29(11):875–80. 10.1016/j.eprac.2023.08.006 [DOI] [PubMed] [Google Scholar]
- 4.Liu F, Zhang X. Hypertension and obesity: risk factors for thyroid disease. Front Endocrinol. 2022;13:939367. 10.3389/fendo.2022.939367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marzullo P, Minocci A, Tagliaferri MA, Guzzaloni G, Di Blasio A, De Medici C, Aimaretti G, Liuzzi A. Investigations of thyroid hormones and antibodies in obesity: leptin levels are associated with thyroid autoimmunity independent of bioanthropometric, hormonal, and weight-related determinants. J Clin Endocr Metab. 2010;95(8):3965–72. 10.1210/jc.2009-2798 [DOI] [PubMed] [Google Scholar]
- 6.Chen J, Wei L, Zhu X, Xu W, Zou Y, Qi X, Fang J, Wang X, Shi X, Sheng Y, et al. TT3, a more practical Indicator for evaluating the relationship between Sarcopenia and thyroid hormone in the Euthyroid Elderly compared with FT3. Clin Interv Aging. 2023;18:1285–93. 10.2147/CIA.S420558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Szlejf C, Suemoto CK, Janovsky C, Barreto SM, Diniz M, Lotufo PA, Bensenor IM. Thyroid function and Sarcopenia: results from the ELSA-Brasil Study. J Am Geriatr Soc. 2020;68(7):1545–53. 10.1111/jgs.16416 [DOI] [PubMed] [Google Scholar]
- 8.Kurinami N, Sugiyama S, Yoshida A, Hieshima K, Miyamoto F, Kajiwara K, Jinnouchi T, Jinnouchi H. Correlation of body muscle/fat ratio with insulin sensitivity using hyperinsulinemic-euglycemic clamp in treatment-naïve type 2 diabetes mellitus. Diabetes Res Clin Pr. 2016;120:65–72. 10.1016/j.diabres.2016.07.018 [DOI] [PubMed] [Google Scholar]
- 9.Karakoc HC, Zileli M, Yaman O, Paksoy K. Can lumbar paraspinal muscle/fat ratio and spinopelvic parameters predict short-term outcomes after decompressive surgeries in lumbar disc herniation and lumbar spinal stenosis? J Craniovertebral Ju. 2023;14(3):236–44. 10.4103/jcvjs.jcvjs_40_23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Song W, Hu H, Ni J, Zhang H, Zhang H, Lu J, Wang K, Mao W, Peng B. Prognostic value of total body muscle-fat ratio in patients with kidney stone disease: a US population-based study. Heliyon. 2023;9(9):e20339. 10.1016/j.heliyon.2023.e20339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Borrud L, Chiappa MM, Burt VL, Gahche J, Zipf G, Johnson CL, Dohrmann SM. National Health and Nutrition Examination Survey: national youth fitness survey plan, operations, and analysis. Vital Health Stat 2. 2012;2014(163):1–24. [PubMed] [Google Scholar]
- 12.Ye J, Hu Y, Chen X, Yin Z, Yuan X, Huang L, Li K. Association between the weight-adjusted waist index and stroke: a cross-sectional study. BMC Public Health. 2023;23(1):1689. 10.1186/s12889-023-16621-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baran DT, Faulkner KG, Genant HK, Miller PD, Pacifici R. Diagnosis and management of osteoporosis: guidelines for the utilization of bone densitometry. Calcified Tissue Int. 1997;61(6):433–40. 10.1007/s002239900362 [DOI] [PubMed] [Google Scholar]
- 14.Heymsfield SB, Wang J, Heshka S, Kehayias JJ, Pierson RN. Dual-photon absorptiometry: comparison of bone mineral and soft tissue mass measurements in vivo with established methods. Am J Clin Nutr. 1989;49(6):1283–9. 10.1093/ajcn/49.6.1283 [DOI] [PubMed] [Google Scholar]
- 15.Jhee JH, Joo YS, Han SH, Yoo TH, Kang SW, Park JT. High muscle-to-fat ratio is associated with lower risk of chronic kidney disease development. J Cachexia Sarcopeni. 2020;11(3):726–34. 10.1002/jcsm.12549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Seo YG, Song HJ, Song YR. Fat-to-muscle ratio as a predictor of insulin resistance and metabolic syndrome in Korean adults. J Cachexia Sarcopeni. 2020;11(3):710–25. 10.1002/jcsm.12548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Song RH, Wang B, Yao QM, Li Q, Jia X, Zhang JA. The impact of obesity on thyroid autoimmunity and dysfunction: a systematic review and Meta-analysis. Front Immunol. 2019;10:2349. 10.3389/fimmu.2019.02349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fussey JM, Beaumont RN, Wood AR, Vaidya B, Smith J, Tyrrell J. Does obesity cause thyroid Cancer? A mendelian randomization study. J Clin Endocr Metab. 2020;105(7):e2398–407. 10.1210/clinem/dgaa250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pappa T, Alevizaki M. Obesity and thyroid cancer: a clinical update. Thyroid. 2014;24(2):190–9. 10.1089/thy.2013.0232 [DOI] [PubMed] [Google Scholar]
- 20.Lidell ME, Betz MJ, Enerbäck S. Brown adipose tissue and its therapeutic potential. J Intern Med. 2014;276(4):364–77. 10.1111/joim.12255 [DOI] [PubMed] [Google Scholar]
- 21.Xu C, Yang X, Liu W, Yuan H, Yu C, Gao L, Zhao J. Thyroid stimulating hormone, independent of thyroid hormone, can elevate the serum total cholesterol level in patients with coronary heart disease: a cross-sectional design. Nutr Metab. 2012;9(1):44. 10.1186/1743-7075-9-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ma Y, Shen S, Yan Y, Zhang S, Liu S, Tang Z, Yu J, Ma M, Niu Z, Li Z et al. Adipocyte Thyroid Hormone β Receptor-Mediated Hormone Action Fine-tunes Intracellular Glucose and Lipid Metabolism and Systemic Homeostasis. Diabetes 2023, 72(5):562–574. [DOI] [PubMed]
- 23.Pedersen BK, Febbraio MA. Muscles, exercise and obesity: skeletal muscle as a secretory organ. Nat Rev Endocrinol. 2012;8(8):457–65. 10.1038/nrendo.2012.49 [DOI] [PubMed] [Google Scholar]
- 24.Schnyder S, Handschin C. Skeletal muscle as an endocrine organ: PGC-1α, myokines and exercise. Bone. 2015;80:115–25. 10.1016/j.bone.2015.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fontenelle LC, Feitosa MM, Severo JS, Freitas TE, Morais JB, Torres-Leal FL, Henriques GS, Do NMD. Thyroid function in human obesity: underlying mechanisms. Horm Metab Res. 2016;48(12):787–94. 10.1055/s-0042-121421 [DOI] [PubMed] [Google Scholar]
- 26.Strączkowski M, Nikołajuk A, Stefanowicz M, Matulewicz N, Fernandez-Real JM, Karczewska-Kupczewska M. Adipose tissue and Skeletal Muscle Expression of Genes Associated with thyroid hormone action in obesity and insulin resistance. Thyroid. 2022;32(2):206–14. 10.1089/thy.2021.0351 [DOI] [PubMed] [Google Scholar]
- 27.Laclaustra M, Moreno-Franco B, Lou-Bonafonte JM, Mateo-Gallego R, Casasnovas JA, Guallar-Castillon P, Cenarro A, Civeira F. Impaired sensitivity to thyroid hormones is Associated with Diabetes and metabolic syndrome. Diabetes Care. 2019;42(2):303–10. 10.2337/dc18-1410 [DOI] [PubMed] [Google Scholar]
- 28.Walczak K, Sieminska L. Obesity and thyroid Axis. Int J Env Res Pub He 2021, 18(18). [DOI] [PMC free article] [PubMed]
- 29.Staníková D, Krajčovičová L, Lobotková D, Vitariušová E, Tichá Ľ, Pribilincová Z, Ukropcová B, Ukropec J, Staník J. Thyroid hormone levels and BMI-SDS changes in adolescents with obesity. Front Endocrinol. 2023;14:1304970. 10.3389/fendo.2023.1304970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hu X, Zhang L, Zhang M, Mi W, Sun Y, Wang Y, Zou H, Liu C, Xu S. Correlation of subclinical hypothyroidism with Sarcopenia and its components in the Chinese older adults. Endocrine. 2024;84(3):1030–9. 10.1007/s12020-023-03654-7 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The National Health and Nutrition Examination Survey dataset is publicly available at the National Center for Health Statistics of the Center for Disease Control and Prevention (https://www.cdc.gov/nchs/nhanes/index.htm). Data used in the current study are available from the corresponding author upon reasonable request.