Abstract
Oropharyngeal squamous-cell carcinoma (OPSCC) poses significant challenges in diagnosis, treatment, and management and has important medico-legal and forensic implications. In particular, the management of OPSCC and its treatment-related complications can often be challenging. In cases with advanced OPSCC, a loco-regional extension of the tumor can contribute to the destruction of oral cavity tissues, while the radiotherapy treatment can induce profound changes in tissue morphology and structure. These changes, which resemble tumor neoplasms and endovascular effects, are related to a higher risk of fatal bleeding, as reported in the case study illustrated, in which a hemorrhage occurred from a lingual artery, originating from an ulcerative, necrotic, hemorrhagic lesion on the tongue. Bleeding complications in OPSCC and prolonged radiotherapy are associated with high mortality and require comprehensive management strategies to improve survival and quality of life. Autopsy investigations, contributing to the definition of post-mortem diagnosis, can provide valuable insights into the pathogenetic mechanisms underlying bleeding and guide therapeutic decisions and preventive measures. The integration of autopsy and histopathological investigation into clinical practice should be considered as a necessary support to optimize the management of complications in advanced OPSCC patients, emphasizing the importance of a patient-centered approach and continued research.
Keywords: head and neck, oropharyngeal carcinoma, squamous-cell cancer, lingual artery bleeding, autopsy investigation, post-mortem diagnosis
1. Introduction
Head and neck squamous-cell carcinoma (HNSCC), which includes cancers of the oral cavity and oropharynx, is the world’s sixth most common cancer [1].
Oropharyngeal squamous-cell carcinoma (OPSCC) arises from various sites within the oropharynx, including the soft palate, tonsils, base of the tongue, pharyngeal wall, and vallecula. The most common anatomic locations for OPSCCs are the tonsillar complex and the base of the tongue, which account for 96% of oropharyngeal tumors [2].
Traditionally associated with alcohol and tobacco use, the epidemiology of OPSCC has undergone a notable shift due to declining smoking rates and the emergence of human papillomavirus (HPV) as a significant etiological factor [3,4,5]. The incidence of HPV-related OPSCC has risen sharply in high-income countries, with an estimated 55,000 cases and 12,000 deaths annually in the United States alone [6].
The advent of prophylactic HPV vaccination holds the promise of preventing a substantial proportion of OPSCC cases, with HPV-16 implicated in most infections [7,8]. The American Joint Committee on Cancer’s (AJCC) distinction between HPV-positive (HPV+) and HPV-negative (HPV-) OPSCC underscores the different molecular profiles, tumor characteristics, and treatment outcomes [9,10].
The clinical presentation of OPSCC includes a variety of symptoms such as pharyngeal swelling, dysphagia, visible mass, and otalgia, which often mimic benign conditions and require careful diagnostic evaluation [11]. Histologically, OPSCC has several subtypes, each of which has prognostic implications. Prognostic indicators for local recurrence and overall survival include tumor diameter, nodal status, surgical margins, degree of differentiation, invasion pattern, and patient response [12,13].
The management of OPSCC is a comprehensive strategy that encompasses various modalities, including surgery, radiotherapy, chemotherapy, or a combination of these, tailored to the specific type of cancer, its location, and the stage of the disease. The selection of treatment modalities is a careful consideration based on the individual characteristics of the patient’s cancer. Despite advancements in treatment, the nature of OPSCC therapy introduces the potential for long-term complications that significantly impact survivorship and quality of life [14,15]. As the field of oral cancer management evolves, strategies must continually adapt to address and mitigate the potential complications of OPSCC treatment. Achieving a balance between the efficacy of treatment and the possible complications is a complex challenge, necessitating ongoing research and a patient-centered approach to care [16,17,18,19].
In the OPSCC treatment and complications scenario, toxicities are known to be strongly related to the dose of radiotherapy received by normal tissues. Severe late toxicities have been reported in 43% of patients after radiotherapy treatment, and toxicity of this magnitude can last a lifetime; in light of this, it is imperative to implement dose tailoring strategies that are as short as possible to limit the damage. In this direction, several de-escalation studies have been published, such as the PATHOS (Postoperative Adjuvant Treatment for Human Papillomavirus (HPV)-positive Tumors) study, which aims to demonstrate that de-escalation of adjuvant treatment, stratified by risk, not only maintains high survival and short recurrence rates in patients with HPV-positive OPSCC but also improves long-term swallowing function. In any case, the rationale of all these studies is that we need to balance and mitigate the subject’s level of risk of recurrence, keeping in mind that 50–60 Gy is a critical dose range with regard to the risk of long-term dysphagia and radiotherapy-related dystrophy bleeding [20].
In addition to these clinical complexities of managing advanced OPSCC, it is critical to consider the medico-legal and forensic implications that may arise in such cases. The intersection of medical care, legal considerations, and forensic analysis plays a critical role in understanding the circumstances surrounding patient care, treatment decisions, and adverse outcomes in cases of advanced oropharyngeal carcinoma [21,22,23].
2. Clinical Framing and Treatment
The clinical presentation, prognosis, and treatment of oropharyngeal squamous-cell carcinoma (OPSCC) are influenced by several factors, including sex, age at diagnosis, and cancer stage.
Sex differences in OPSCC presentation and prognosis have been reported, with men generally exhibiting a higher incidence of OPSCC attributed to a higher prevalence of risk factors such as tobacco and alcohol use [24,25]. Additionally, human papillomavirus (HPV) infection is more common in men, contributing to differences in tumor biology and clinical outcomes [26].
Sex may influence treatment selection and response in OPSCC. Adjuvant therapies such as chemotherapy and radiotherapy play an important role in the treatment of OPSCC. However, the response to adjuvant therapies may vary according to sex. For example, women have been shown to have a higher susceptibility to certain treatment-related toxicities such as mucositis and dermatitis [27]. These differences in treatment tolerability and toxicity profiles must be carefully considered when tailoring adjuvant therapies for OPSCC patients based on their sex. Strategies such as dose adjustments or alternative treatment options can be used to minimize adverse effects and optimize treatment outcomes [28,29].
Age is another important factor to consider in the treatment of OPSCC because the epidemiology of the disease and tumor biology differ across age groups. OPSCC is typically diagnosed in two different age groups: younger patients (typically under 45 years of age) and older patients (over 55 years of age) [30]. Younger patients are more likely to have HPV-associated OPSCC, which tends to have a more favorable prognosis [31]. In contrast, older patients are more likely to have HPV-negative tumors and may have more frequent comorbidities [32,33,34].
Accurate staging of OPSCC is paramount for treatment planning and prognosis prediction. Staging systems (SS) like the American Joint Committee on Cancer (AJCC) SS provide standardized frameworks for classifying OPSCC based on tumor size, lymph node involvement, and distant metastases, aiding in treatment decisions and prognostic assessments [35]. Early-stage OPSCC, typically classified as T1-T2 tumors, can often be effectively treated with single modalities like surgery or radiation therapy. Minimally invasive surgical techniques such as transoral robotic surgery (TORS) and transoral laser microsurgery (TLM) offer improved functional outcomes and reduced morbidity compared to traditional open surgery [36,37]. Conversely, advanced-stage OPSCC may necessitate multimodality treatment approaches involving surgery, radiotherapy, and chemotherapy [38].
Despite optimal initial treatment, some OPSCC patients face disease recurrence or persistence, leading to the consideration of salvage therapies such as re-irradiation or systemic therapy based on disease extent and patient health status [39,40,41]. Recent research has focused on de-escalating treatment intensity to minimize long-term toxicities while maintaining disease control, emphasizing personalized treatment approaches tailored to individual patient factors and tumor characteristics [42,43,44].
The management of OPSCC is a multifaceted journey that, while striving for optimal therapeutic outcomes, is not without potential complications linked to both the disease itself and the modalities employed in its treatment.
Surgery, particularly transoral procedures like transoral robotic surgery (TORS) and transoral laser microsurgery (TLM), is crucial for managing early-stage OPSCC and when organ preservation is not feasible.
3. Complications
Complications such as postoperative hemorrhage, infection, and functional impairments can arise [45,46,47]. Neck dissection, a common procedure, may lead to shoulder dysfunction and lymphedema [48,49]. Radiation therapy, often combined with chemotherapy, is a primary treatment for OPSCC, causing acute complications like mucositis and xerostomia [50,51,52,53]. Late complications include radiation-induced fibrosis and osteoradionecrosis [54,55]. Chemotherapy, especially platinum-based agents, can result in hematological toxicity and gastrointestinal symptoms [56,57,58]. Targeted therapies like EGFR inhibitors and immune checkpoint inhibitors have shown promise but may lead to skin rash and immune-related complications, respectively [59,60,61,62].
Combined treatment with chemotherapy and radiotherapy can lead to various side effects, encompassing skin and mucosal erosion, xerostomia, underlying soft tissue fibrosis, and osteoradionecrosis. Further complications include secondary effects on the surrounding vasculature, including premature atherosclerosis with stenosis and arterial wall weakening due to adventitial fibrosis, elastic filament fragmentation, and vasa vasorum destruction [63].
Among the complications of treatment for OPSCC, oropharyngeal hemorrhage is a rare but life-threatening occurrence [64,65]. It may occur spontaneously after radiochemotherapy due to arterial wall weakening, with vascular erosion more common in advanced or recurrent tumors, infections, and pharyngocutaneous fistulas [66]. The involvement of external carotid artery branches, especially in locally advanced cases, heightens the bleeding risk.
Particularly concerning are cases of hemorrhage in patients without tumor recurrence, where fatality rates can reach 40%. The facial artery and lingual artery are primary sources of such hemorrhage [67].
Oropharyngeal hemorrhage presentations vary based on bleeding severity, encompassing hemoptysis, hematemesis, epistaxis, and persistent or acute hemorrhages. Bleeding may obstruct airways, lead to blood aspiration, and result in asphyxiation. In most cases reported in the literature, it is noted that a major hemorrhagic event is preceded by minor ones, which can serve as a warning sign to identify at-risk patients [68,69].
Operations for oropharyngeal hemorrhage are intricate due to radiation-induced damage, hemodynamic imbalance, and difficulty in localizing the hemorrhage. Endovascular management has demonstrated superior safety and efficacy compared to surgical approaches, effectively halting oropharyngeal hemorrhage [70,71]. For patients with oropharyngeal neoplasms treated with RT who show recurrent bleeding episodes and mucosal ulceration, particularly after the acute treatment phase, hospitalization with prophylactic surgical ligation or embolization of the affected arteries may be recommended [72,73,74].
4. Role of Post-Mortem Investigations and Diagnosis
Post-mortem investigations can often play a key role in evaluating the findings and defining the cause of death in cancer patients and fully understanding the complications, providing a comprehensive analysis of the patient and enabling targeted sampling that would otherwise not be possible [75,76].
Autopsy investigation in cases with a clinical history of advanced neck-oropharyngeal carcinoma should always be conducted following a rigorous autopsy protocol aimed at identifying and documenting the characteristics and extent of the oropharyngeal carcinoma, as well as any elements that might help in determining the cause of death [77]. In fact, a fundamental objective of the autopsy in these cases is represented by the correct identification, documentation, and interpretation of the pathological findings.
On the other hand, it is important to take into consideration that the neck poses significant challenges to the forensic pathologist for several reasons. First of all, the anatomical localization of the alterations, often located in regions of the neck that, due to the conformation and anatomical relationships of the cervical organs, do not allow optimal visualization of the possible findings, often not even with particularly invasive anatomical dissections. In these cases, in fact, the anterior neck structures can also present anatomical variations and characteristics that could make it difficult to distinguish artifacts from pathological findings. Secondly, pathological features may have a degree of expressiveness that complicates the interpretation of post-mortem findings in the neck.
To reduce the practical difficulties in interpreting autopsy results in the neck, important factors must be considered. First, it is essential that the neck is properly dissected during the post-mortem investigation by autopsy. This involves a layer-by-layer dissection of the neck after vascular decompression of the neck by removal of the brain and viscera. Dissection of the neck is best achieved by a series of incisions that maximize exposure of the ventral, lateral, and submental portions of the neck. This dissection may be extended to include the face. Secondly, it is important to be proactive in recognizing the pitfalls and artifacts that may become apparent based on the history, site, and circumstances of the case, always taking into consideration the possible diagnostic traps related to the misinterpretation [78].
The forensic approach first should include a detailed review of the pre-mortem medical records, with particular attention to the patient’s oncological history and treatments received. During the external examination, external signs should be identified and documented, and the neck area should be carefully examined.
As an adjunct and preliminarily to autopsy, post-mortem TC (PMCT) could be useful in selected cases since post-mortem imaging can aid the forensic pathologist, helping in planning the dissection, visualizing any alterations, and helping to clarify the location and extent, as well as the type of any pathological alterations [79,80,81,82,83].
Dissection of the neck structures and internal examination should be performed starting with a U-shaped skin incision on the anterior surface of the neck and thorax (mastoid process → postero-lateral surface of the neck → outer and middle third of the clavicle → sternal angle, and the same on the other side up to the mastoid). This approach allows wide access to the area under investigation and complete visualization of the cervical structures. A progressive layer-by-layer dissection of the structures should be performed to investigate the different anatomic regions and zones of the neck. This dissection, in fact, provides for maximal exposure of the ventral, lateral, and submental portions of the neck. After isolating muscle layers one by one and exposing the cervical organs, an en-bloc dissection of the oro-cervico-respiratory block (tongue–hypopharynx–larynx–trachea–bronchi–lungs), according to the Ghon technique, allows a better visualization of the entire anatomic region, preserving the integrity and anatomic rapports between the cervico-oropharyngeal structures.
Following the described approach, oropharyngeal alterations in head and neck cancer patients can be detected, documented, and characterized, with the aim of understanding the pathophysiological mechanisms related to death and giving a possible focus on the related risks, including in those patients seemingly under control.
Histopathological examination is crucial in these cases to document possible modification related to primitive cancer alterations and document the effects of radiotherapy in the head and neck region associated with severe morpho-structural and vascular alterations, including endovascular phenomena leading to possible fatal bleeding events.
In fact, from a histological point of view, tumor-like lesions manifest as extensive morpho-structural alterations, resembling tumor neoplasms, characterized by tissue necrosis, chronic inflammation, fibrosis, and vasculopathy [84,85]. Endovascular effects, on the other hand, involve pathological changes in blood vessels, such as vascular inflammation, fibrinoid degeneration, and vascular stenosis [86].
Overall, both tumor-like lesions and endovascular effects reflect the severe alterations induced by radiotherapy on the oropharyngeal tissue, predisposing patients to serious complications, including bleeding and further tissue damage. The importance of assessing the risk of fatal bleeding events in patients with advanced oropharyngeal carcinoma treated with radiotherapy, especially those with significant side effects, is therefore crucial.
5. Illustrative Case
As an illustrative case of post-mortem investigations and comprehensive analysis of OPSCC fatal complications, the case of a 69-year-old woman with a history of advanced oropharyngeal cancer suddenly died after experiencing a severe coughing fit with initial hemoptysis is reported.
Medical history indicated that the patient had initially sought medical attention for an ulcerating neoformation in the oral cavity. Subsequent examinations revealed a moderately differentiated squamous-cell carcinoma. Further investigations, including CT and PET scans, revealed extensive tissue involvement in the cervicofacial region and multiple lymphadenopathies. Diagnosed with cT4bN2c St. IVB, the patient underwent a tracheotomy and PEG placement due to upper airway issues and began treatment with chemotherapy and concomitant radiochemotherapy. Chemotherapy treatment was administered with Cisplatin, given on a weekly schedule for seven weeks at a dosage of 40 mg/m2. Radiotherapy was planned using intensity-modulated radiation therapy (IMRT) techniques. Iso-dose lines were drawn to ensure that the tumor areas received a total dose of 70 Gy, while the vulnerable structures surrounding the tumor area were protected with lower doses, not exceeding 54 Gy.
After treatment, positive results were seen with no loco-regional recurrence, with a six-month therapy-free interval. During this interval, the patient was regularly monitored with otolaryngological clinical examinations, initially monthly and then every two months. One year after tumor diagnosis, the oncological staging revealed advanced-stage disease with suspected lymph node and lung metastases (cT4a, cN2c, pN+, cM1 lymph nodes and lung, Stage IV C), leading to the initiation of biological therapy with Nivolumab, resulting in subsequent good control of neoplastic progression.
In this state of apparently good control of the neoplastic pathology, approximately seven months after the end of radiotherapy and concomitant chemotherapy, the patient died suddenly due to unexpected and unpredictable profuse oropharyngeal bleeding. There were no previous episodes of minor bleeding to suggest sudden fatal major bleeding.
An autopsy was performed to determine the origin of the bleeding, to define any potential triggering and causative factors that led to the unforeseen and tragic event, and so to establish the cause of the death.
5.1. Autopsy Findings
The external examination was unremarkable except for widespread staining of the clothing with blood.
At autopsy, the oral cavity was filled with blood. The tongue showed an ulcerous, necrotic, hemorrhagic lesion extending from the lateral margin of the right portion of the tongue, penetrating the muscular body of the tongue and involving its entire thickness.
The lungs showed a pale appearance in the mid-apical region and a hematogenous distribution in the lower lobes. The airways contained endoluminal blood material from inhalation. The gastrointestinal tract and stomach, up to the pylorus, contained a significant amount of brownish fluid material consistent with ingested blood.
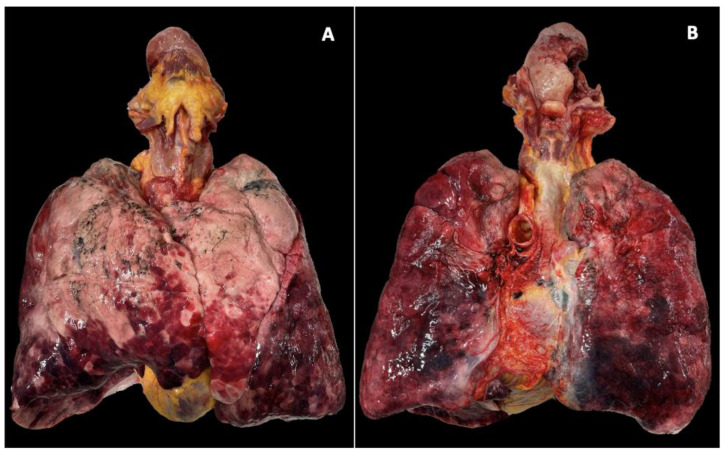
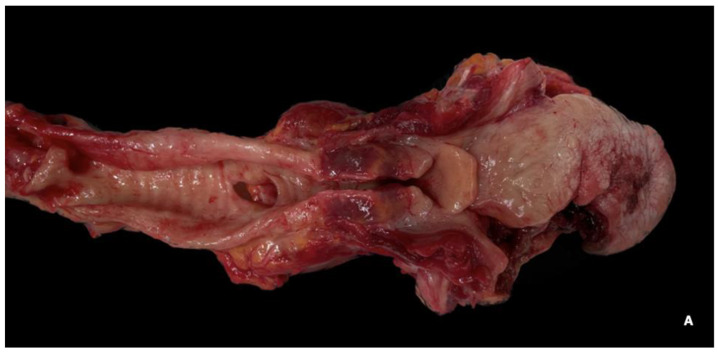
The oro-cervico-respiratory block (tongue–hypopharynx–larynx–trachea–bronchi–lungs) was removed in its entirety, according to the Ghon technique (en bloc), and the tongue–hypopharynx–larynx–trachea portion was examined after formalin fixation to enhance the study of anatomical structures of interest. (Figure 1) The tongue showed a deep ulceration of approximately 2 × 2 cm in the lateral margin of the right portion of the tongue, extending 13 mm into the muscular body of the tongue, affecting the organ through its entire thickness on both the upper and lower surfaces, and reaching approximately 7 mm from the lingual frenulum. (Figure 2A–C)
Figure 1.
Oro-cervico-respiratory block according to the Ghon technique (en bloc). There is a noticeable pale appearance in the mid-apical region of the lungs, and blood is spreading at the bases. The tongue showed an ulcerous, necrotic, hemorrhagic lesion extending from the lateral margin of the right portion of the tongue, penetrating the muscular body of the tongue and involving its entire thickness.
Figure 2.
(A,B) The tongue exhibited an ulcerous, necrotic, hemorrhagic lesion that extended from the lateral margin of the right portion of tongue, penetrating the muscular body of the tongue and affecting it throughout its thickness. (C) Close, serial sections of the ulcerative lesion after formalin fissation revealed necrotic tissue extended and dissociated from hemorrhagic phenomena. Within the necrotic tissue, a vascular branch (branch of the lingual artery) was identified as possible source of the bleeding.
Close, serial sections of the ulcerative lesion revealed necrotic tissue extended and dissociated from hemorrhagic phenomena. Within the necrotic tissue, a vascular branch (branch of the lingual artery) was identified as the source of the bleeding.
5.2. Histopathological Examination
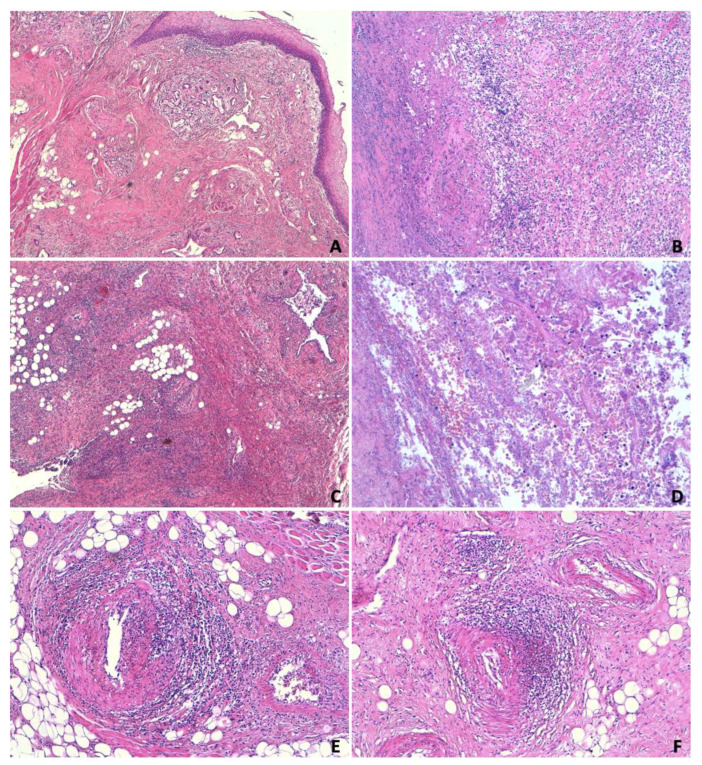
All tissue samples were fixed in formalin, embedded in paraffin, and subjected to routine microscopic histopathological examination using hematoxylin and eosin (H&E) staining. (Figure 3)
Figure 3.
Extensive necrotic, hemorrhagic ulceration of the tongue involves both the lateral basal plane and the superficial squamous epithelial lining. (A) The base and edges of this ulceration are covered by a thick layer of necrotic, hemorrhagic material containing assessable cellular debris. (B) The underlying muscle-connective tissue layers host extensive necrotic, granulocytic phenomena (presumably secondary to bacterial superinfection), within which decaying food residues, microbial colonies, and various nerve trunk structures infiltrated by inflammatory elements are identified. (C,D) In the sublingual areas corresponding to the aforementioned ulceration, islands of glandular tissue (attributable to minor salivary glands) with severe dysplastic morpho-structural alterations are present, sometimes giving the picture of a “tumor-like lesion” correlated with the cytolysis effects of prolonged radiotherapy. (E) Adjacent tissues show arteriolar vascular branches with endovascular phenomena causing subtotal luminal stenosis and perivascular changes. (F) The lingual body shows lympho-granulocytic inflammatory infiltrates and focal necrotic, hemorrhagic phenomena, resulting in the fragmentation of striated muscle fibers.
Microscopic examination of formalin-fixed paraffin-embedded tissue sections stained with H&E confirmed the necrotic, hemorrhagic ulceration of the tongue. In the sublingual areas corresponding to the ulceration, islands of tissue with severe morpho-structural alterations, sometimes resembling a “tumor-like lesion”, were present. Adjacent tissue areas showed arteriolar vascular branches with endovasculitic phenomena. The muscular body of the tongue showed lympho-granulocytic inflammatory infiltrates and focal necrotic, hemorrhagic phenomena, resulting in the fragmentation of the muscle-striated fibers. These alterations were attributed to the cytolytic effects of prolonged radiotherapy. On the other hand, the original neoplastic pathology could not be detected.
Brain samples displayed both intracellular and extracellular cerebral edema. The lungs showed alveolar spaces containing erythrocytes. No further significant findings were found in the remaining tissue samples.
In view of these findings, the cause of death was identified as hemorrhage from an ulcerated, necrotic, hemorrhagic lesion on the tongue in a patient with advanced oropharyngeal carcinoma. The loco-regional extension of the tumor contributed to the destruction of oral cavity tissues, while the radiotherapy treatment induced morpho-structural changes, predisposing the patient to bleeding unexpectedly without premonitory signs, suggesting the need for preventive treatment.
In fact, investigations revealed significant alterations attributable to the cytolytic effects of prolonged radiotherapy. Histopathological examination showed radiotherapy-related severe morpho-structural and vascular alterations, including endovascular phenomena, leading to fatal bleeding.
On the other hand, the reported illustrative case provides food for thought regarding the management of OPSCC and treatment-related complications and the importance of post-mortem investigations in understanding these adverse fatal events, highlighting the need for complete and meticulous examination and collaboration between multidisciplinary experts.
6. Future Perspectives
The current literature only partially addresses OPSCC complications. Bleeding complications in OPSCC and prolonged radiotherapy are associated with high mortality and require comprehensive management strategies to improve survival and quality of life.
This study offers a proof of concept that may improve the diagnostic possibilities and the ability to detect the anomalies developed in this type of patient. Autopsy investigations, contributing to the definition of post-mortem diagnosis, can provide valuable insights into the pathogenetic mechanisms underlying bleeding and guide therapeutic decisions and preventive measures. The integration of autopsy and histopathological investigation into clinical practice should be considered as a necessary support to optimize the management of complications in advanced OPSCC patients.
Subsequently, based on this evidence, treatment strategies can be developed in the future, strengthened by the ability to identify early on which of these patients are most prone to these complications. As an example, a personalized approach, also with an artificial intelligence-assisted decision and operative support, may help in better planning of treatment both in terms of doses and in terms of targeting, fully integrating the so-called adaptive radiotherapy. In parallel, the most important steps in radiotherapy preparation, delivery, and evaluation, as well as radiotherapy planning, can consequently be improved by also considering the different complications detected through these multidisciplinary approaches.
7. Conclusions
Bleeding in OPSCC is a dreaded complication associated with high mortality rates and a poor short- and mid-term prognosis. The management of complications associated with OPSCC and its treatments is crucial to improving survival and quality of life. The delicate balance between treatment efficacy and complications requires continuous research and a patient-centered approach to care.
Post-mortem investigations can often play a key role in giving valuable insights into understanding and managing this serious complication. In this scenario, post-mortem findings can provide a solid scientific basis for elucidating the pathogenetic mechanisms underlying bleeding and assessing the impact of radiation therapy on tissue structure and function.
Furthermore, the importance of rigorous postoperative monitoring is evident in order to mitigate risks associated with surgical and combined radiotherapy-chemotherapy treatments. Clinicians should prioritize strategies that reduce the incidence of severe complications, and emerging protocols should incorporate risk management for spontaneous hemorrhage, particularly in patients with advanced or recurrent disease.
The implications for future guidelines are significant: recommendations for dose tailoring, long-term patient monitoring, and interdisciplinary approaches are important to manage the complex needs of OPSCC patients. Additionally, given the possible severe risks associated with combined treatments, there is a critical need for further research into optimizing therapeutic combinations to balance efficacy with patient safety [87].
Author Contributions
Conceptualization, F.C. and A.S. (Alessandro Santurro); methodology, F.C., M.D.S. and A.S. (Alessandro Santurro); validation, V.F. and A.S. (Alfonso Scarpa); data curation, F.C., A.A. and A.S. (Alessandro Santurro); writing—original draft preparation, F.C. and M.D.S.; writing—review and editing, F.A.S., V.F. and A.S. (Alessandro Santurro) All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Ethical review and approval were waived for this study because judicial cases are involved. The processing of the reported personal data was carried out in accordance with the provisions of the Declaration of Helsinki and the requirements for the processing of personal data carried out for scientific research purposes (Auth. Gen. no. 9/2016) of the GPDP—Guarantor for the Protection of Personal Data (adopted with a provision published in the Official Gazette General Series no. 176 of 29 July 2019)—in the case of subjects who are already deceased. The data collected have also been adequately anonymized and processed in accordance with the GDPR—General Data Protection Regulation EU/2016/679—and the Privacy Code (Legislative Decree 30 June 2003, n. 196, and subsequent amendments).
Informed Consent Statement
Not applicable.
Data Availability Statement
The data are included in a legal case in Italy, and for this reason, they are not available.
Conflicts of Interest
Francesca Consalvo plays the role of Co-Founder in BrainLab s.r.l.—Matteo De Simone plays the role of CEO in BrainLab s.r.l.—Alessandro Santurro plays the role of Scientifica Advisor n BrainLab s.r.l. BrainLab s.r.l. had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Warnakulasuriya S. Global epidemiology of oral and oropharyngeal cancer. Oral Oncol. 2009;45:309–316. doi: 10.1016/j.oraloncology.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 2.Tham T., Ahn S., Frank D., Kraus D., Costantino P. Anatomical subsite modifies survival in oropharyngeal squamous cell carcinoma: National Cancer Database study. Head Neck. 2020;42:434–445. doi: 10.1002/hed.26019. [DOI] [PubMed] [Google Scholar]
- 3.Lechner M., Liu J., Masterson L., Fenton T.R. HPV-associated oropharyngeal cancer: Epidemiology, molecular biology and clinical management. Nat. Rev. Clin. Oncol. 2022;19:306–327. doi: 10.1038/s41571-022-00603-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gillison M.L., Chaturvedi A.K., Anderson W.F., Fakhry C. Epidemiology of Human Papillomavirus-Positive Head and Neck Squamous Cell Carcinoma. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2015;33:3235–3242. doi: 10.1200/JCO.2015.61.6995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Senkomago V., Henley S.J., Thomas C.C., Mix J.M., Markowitz L.E., Saraiya M. Human Papillomavirus-Attributable Cancers—United States, 2012–2016. MMWR. Morb. Mortal. Wkly. Rep. 2019;68:724–728. doi: 10.15585/mmwr.mm6833a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Siegel R.L., Miller K.D., Wagle N.S., Jemal A. Cancer statistics, 2023. CA A Cancer J. Clin. 2023;73:17–48. doi: 10.3322/caac.21763. [DOI] [PubMed] [Google Scholar]
- 7.Schache A.G., Powell N.G., Cuschieri K.S., Robinson M., Leary S., Mehanna H., Rapozo D., Long A., Cubie H., Junor E., et al. HPV-Related Oropharynx Cancer in the United Kingdom: An Evolution in the Understanding of Disease Etiology. Cancer Res. 2016;76:6598–6606. doi: 10.1158/0008-5472.CAN-16-0633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Donà M.G., Rollo F., Pichi B., Spriano G., Moretto S., Covello R., Pellini R., Benevolo M. Evolving Profile of HPV-Driven Oropharyngeal Squamous Cell Carcinoma in a National Cancer Institute in Italy: A 10-Year Retrospective Study. Microorganisms. 2020;8:1498. doi: 10.3390/microorganisms8101498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Craig S.G., Anderson L.A., Schache A.G., Moran M., Graham L., Currie K., Rooney K., Robinson M., Upile N.S., Brooker R., et al. Recommendations for determining HPV status in patients with oropharyngeal cancers under TNM8 guidelines: A two-tier approach. Br. J. Cancer. 2019;120:827–833. doi: 10.1038/s41416-019-0414-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Golusinski P., Di Maio P., Pehlivan B., Colley S., Nankivell P., Kong A., Hartley A., Mehanna H. Evidence for the approach to the diagnostic evaluation of squamous cell carcinoma occult primary tumors of the head and neck. Oral Oncol. 2019;88:145–152. doi: 10.1016/j.oraloncology.2018.11.020. [DOI] [PubMed] [Google Scholar]
- 11.McIlwain W.R., Sood A.J., Nguyen S.A., Day T.A. Initial symptoms in patients with HPV-positive and HPV-negative oropharyngeal cancer. JAMA Otolaryngol Head Neck Surg. 2014;140:441–447. doi: 10.1001/jamaoto.2014.141. [DOI] [PubMed] [Google Scholar]
- 12.Albergotti W.G., Schwarzbach H.L., Abberbock S., Ferris R.L., Johnson J.T., Duvvuri U., Kim S. Defining the Prevalence and Prognostic Value of Perineural Invasion and Angiolymphatic Invasion in Human Papillomavirus-Positive Oropharyngeal Carcinoma. JAMA Otolaryngol Head Neck Surg. 2017;143:1236–1243. doi: 10.1001/jamaoto.2017.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dirven R., Ebrahimi A., Moeckelmann N., Palme C.E., Gupta R., Clark J. Tumor thickness versus depth of invasion—Analysis of the 8th edition American Joint Committee on Cancer Staging for oral cancer. Oral Oncol. 2017;74:30–33. doi: 10.1016/j.oraloncology.2017.09.007. [DOI] [PubMed] [Google Scholar]
- 14.Turner L., Mupparapu M., Akintoye S.O. Review of the complications associated with treatment of oropharyngeal cancer: A guide for the dental practitioner. Quintessence Int. 2013;44:267–279. doi: 10.3290/j.qi.a29050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahadian H., Yassaei S., Bouzarjomehri F., Ghaffari Targhi M., Kheirollahi K. Oral Complications of The Oromaxillofacial Area Radiotherapy. Asian Pac. J. Cancer Prev. 2017;18:721–725. doi: 10.22034/APJCP.2017.18.3.721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gatto V., Scopetti M., La Russa R., Santurro A., Cipolloni L., Viola R.V., Di Sanzo M., Frati P., Fineschi V. Advanced Loss Eventuality Assessment and Technical Estimates: An Integrated Approach for Management of Healthcare-Associated Infections. Curr. Pharm. Biotechnol. 2019;20:625–634. doi: 10.2174/1389201020666190408095050. [DOI] [PubMed] [Google Scholar]
- 17.Paduano S., Uomo R., Amato M., Riccitiello F., Simeone M., Valletta R. Cyst-like periapical lesion healing in an orthodontic patient: A case report with five-year follow-up. G. Ital. Di Endod. 2013;27:95–104. doi: 10.1016/j.gien.2013.09.002. [DOI] [Google Scholar]
- 18.D’Errico S., Zanon M., Radaelli D., Padovano M., Santurro A., Scopetti M., Frati P., Fineschi V. Medication Errors in Pediatrics: Proposals to Improve the Quality and Safety of Care Through Clinical Risk Management. Front. Med. 2022;8:814100. doi: 10.3389/fmed.2021.814100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Borro M., Gentile G., Cipolloni L., Foldes-Papp Z., Frati P., Santurro A., Lionetto L., Simmaco M. Personalised Healthcare: The DiMA Clinical Model. Curr. Pharm. Biotechnol. 2017;18:242–252. doi: 10.2174/1389201018666170208125131. [DOI] [PubMed] [Google Scholar]
- 20.Hargreaves S., Beasley M., Hurt C., Jones T.M., Evans M. Deintensification of Adjuvant Treatment After Transoral Surgery in Patients with Human Papillomavirus-Positive Oropharyngeal Cancer: The Conception of the PATHOS Study and Its Development. Front. Oncol. 2019;9:936. doi: 10.3389/fonc.2019.00936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Santurro A., Vullo A.M., Borro M., Gentile G., La Russa R., Simmaco M., Frati P., Fineschi V. Personalized Medicine Applied to Forensic Sciences: New Advances and Perspectives for a Tailored Forensic Approach. Curr. Pharm. Biotechnol. 2017;18:263–273. doi: 10.2174/1389201018666170207141525. [DOI] [PubMed] [Google Scholar]
- 22.La Russa R., Fineschi V., Di Sanzo M., Gatto V., Santurro A., Martini G., Scopetti M., Frati P. Personalized Medicine and Adverse Drug Reactions: The Experience of An Italian Teaching Hospital. Curr. Pharm. Biotechnol. 2017;18:274–281. doi: 10.2174/1389201018666170207124835. [DOI] [PubMed] [Google Scholar]
- 23.Busardò F.P., Frati P., Santurro A., Zaami S., Fineschi V. Errors and malpractice lawsuits in radiology: What the radiologist needs to know. La Radiol. Medica. 2015;120:779–784. doi: 10.1007/s11547-015-0561-x. [DOI] [PubMed] [Google Scholar]
- 24.Klasen C., Wuerdemann N., Rothbart P., Prinz J., Eckel H.N.C., Suchan M., Kopp C., Johannsen J., Ziogas M., Charpentier A., et al. Sex-specific aspects in patients with oropharyngeal squamous cell carcinoma: A bicentric cohort study. BMC Cancer. 2023;23:1054. doi: 10.1186/s12885-023-11526-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sung H., Ferlay J., Siegel R.L., Laversanne M., Soerjomataram I., Jemal A., Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA A Cancer J. Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 26.Chaturvedi A.K., Graubard B.I., Broutian T., Pickard R.K., Tong Z.Y., Xiao W., Kahle L., Gillison M.L. NHANES 2009-2012 Findings: Association of Sexual Behaviors with Higher Prevalence of Oral Oncogenic Human Papillomavirus Infections in U.S. Men. Cancer Res. 2015;75:2468–2477. doi: 10.1158/0008-5472.CAN-14-2843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ferreira M.N., Ramseier J.Y., Leventhal J.S. Dermatologic conditions in women receiving systemic cancer therapy. Int. J. Women’s Dermatol. 2019;5:285–307. doi: 10.1016/j.ijwd.2019.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Honorato J., Rebelo M.S., Dias F.L., Camisasca D.R., Faria P.A., Azevedo e Silva G., Lourenço S.Q. Gender differences in prognostic factors for oral cancer. Int. J. Oral Maxillofac. Surg. 2015;44:1205–1211. doi: 10.1016/j.ijom.2015.04.015. [DOI] [PubMed] [Google Scholar]
- 29.Dolezal J.M., Rosenberg A.J. Induction Chemotherapy in Low-Risk HPV+ Oropharyngeal Cancer. Curr. Treat. Options Oncol. 2022;23:54–67. doi: 10.1007/s11864-022-00941-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Strohl M.P., Wai K.C., Ha P.K. De-intensification strategies in HPV-related oropharyngeal squamous cell carcinoma-a narrative review. Ann. Transl. Med. 2020;8:1601. doi: 10.21037/atm-20-2984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fasano M., D’Onofrio I., Belfiore M.P., Angrisani A., Caliendo V., Della Corte C.M., Pirozzi M., Facchini S., Caterino M., Guida C., et al. Head and Neck Squamous Cell Carcinoma in Elderly Patients: Role of Radiotherapy and Chemotherapy. Cancers. 2022;14:472. doi: 10.3390/cancers14030472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rettig E.M., Fakhry C., Khararjian A., Westra W.H. Age Profile of Patients with Oropharyngeal Squamous Cell Carcinoma. JAMA Otolaryngol.—Head Neck Surg. 2018;144:538–539. doi: 10.1001/jamaoto.2018.0310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barrett T.F., Mazul A.L., Stepan K.O., Wood C.B., Paniello R.C., Zevallos J.P., Massa S., Jackson R.S., Schmitt N.C., Zenga J., et al. The role of age in treatment decisions for oral cavity squamous cell carcinoma: Analysis of the National Cancer Database. Oral Oncol. 2021;118:105330. doi: 10.1016/j.oraloncology.2021.105330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dickstein D.R., Lehrer E.J., Hsieh K., Hotca A., Jones B.M., Powers A., Sharma S., Liu J., Gupta V., Mell L., et al. Management of Older Adults with Locally Advanced Head and Neck Cancer. Cancers. 2022;14:2809. doi: 10.3390/cancers14112809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bozec A., Culié D., Poissonnet G., Demard F., Dassonville O. Current Therapeutic Strategies in Patients with Oropharyngeal Squamous Cell Carcinoma: Impact of the Tumor HPV Status. Cancers. 2021;13:5456. doi: 10.3390/cancers13215456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Meccariello G., Catalano A., Cammaroto G., Iannella G., Vicini C., Hao S.P., De Vito A. Treatment Options in Early Stage (Stage I and II) of Oropharyngeal Cancer: A Narrative Review. Medicina. 2022;58:1050. doi: 10.3390/medicina58081050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Howard J., Masterson L., Dwivedi R.C., Riffat F., Benson R., Jefferies S., Jani P., Tysome J.R., Nutting C. Minimally invasive surgery versus radiotherapy/chemoradiotherapy for small-volume primary oropharyngeal carcinoma. Cochrane Database Syst. Rev. 2016;12:CD010963. doi: 10.1002/14651858.CD010963.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maniaci A., Hao S.P., Cancemi F., Giardini D., Checcoli E., Soprani F., Iannella G., Vicini C., Cocuzza S., La Mantia I., et al. Surgical Treatment for Advanced Oropharyngeal Cancer: A Narrative Review. Medicina. 2023;59:304. doi: 10.3390/medicina59020304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liao C.T., Chang J.T., Wang H.M., Ng S.H., Hsueh C., Lee L.Y., Lin C.H., Chen I.H., Huang S.F., Cheng A.J., et al. Salvage therapy in relapsed squamous cell carcinoma of the oral cavity: How and when? Cancer. 2008;112:94–103. doi: 10.1002/cncr.23142. [DOI] [PubMed] [Google Scholar]
- 40.Röösli C., Studer G., Stoeckli S.J. Salvage treatment for recurrent oropharyngeal squamous cell carcinoma. Head Neck. 2010;32:989–996. doi: 10.1002/hed.21273. [DOI] [PubMed] [Google Scholar]
- 41.Taniguchi A.N., Sutton S.R., Nguyen S.A., Kejner A.E., Albergotti W.G. The Lack of Standardized Outcomes for Surgical Salvage of HPV-Positive Recurrent Oropharyngeal Squamous Cell Carcinoma: A Systematic Scoping Review. Cancers. 2023;15:2832. doi: 10.3390/cancers15102832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gabani P., Lin A.J., Barnes J., Oppelt P., Adkins D.R., Rich J.T., Zevallos J.P., Daly M.D., Gay H.A., Thorstad W.L. Radiation therapy dose de-escalation compared to standard dose radiation therapy in definitive treatment of HPV-positive oropharyngeal squamous cell carcinoma. Radiother. Oncol. J. Eur. Soc. Ther. Radiol. Oncol. 2019;134:81–88. doi: 10.1016/j.radonc.2019.01.016. [DOI] [PubMed] [Google Scholar]
- 43.Kabalan S., Papadopoulos-Nydam G., Jeffery C.C., Rieger J., Constantinescu G. Temporal Trends in Clinician-Assessed and Patient-Reported Swallowing Outcomes in Oropharyngeal Cancer Patients. Am. J. Speech-Lang. Pathol. 2023;32:492–505. doi: 10.1044/2022_AJSLP-22-00196. [DOI] [PubMed] [Google Scholar]
- 44.Perry A., Lee S.H., Cotton S., Kennedy C. Therapeutic exercises for affecting post-treatment swallowing in people treated for advanced-stage head and neck cancers. Cochrane Database Syst. Rev. 2016;2016:CD011112. doi: 10.1002/14651858.CD011112.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Golusiński W., Golusińska-Kardach E. Current Role of Surgery in the Management of Oropharyngeal Cancer. Front. Oncol. 2019;9:388. doi: 10.3389/fonc.2019.00388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dziegielewski P.T., Teknos T.N., Durmus K., Old M., Agrawal A., Kakarala K., Marcinow A., Ozer E. Transoral robotic surgery for oropharyngeal cancer: Long-term quality of life and functional outcomes. JAMA Otolaryngol.—Head Neck Surg. 2013;139:1099–1108. doi: 10.1001/jamaoto.2013.2747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Garden A.S., Dong L., Morrison W.H., Stugis E.M., Glisson B.S., Frank S.J., Beadle B.M., Gunn G.B., Schwartz D.L., Kies M.S., et al. Patterns of disease recurrence following treatment of oropharyngeal cancer with intensity modulated radiation therapy. Int. J. Radiat. Oncol. Biol. Phys. 2013;85:941–947. doi: 10.1016/j.ijrobp.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 48.Anand A., Vidhyadharan S., Subramaniam N., Balsubramanian D., Battoo A.J., Iyer S., Thankappan K. Selective Neck Dissection in Oral Cavity Cancer Is Not Without Morbidity. Indian J. Surg. Oncol. 2021;12:5–11. doi: 10.1007/s13193-020-01209-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Möckelmann N., Busch C.J., Münscher A., Knecht R., Lörincz B.B. Timing of neck dissection in patients undergoing transoral robotic surgery for head and neck cancer. Eur. J. Surg. Oncol. J. Eur. Soc. Surg. Oncol. Br. Assoc. Surg. Oncol. 2015;41:773–778. doi: 10.1016/j.ejso.2015.02.002. [DOI] [PubMed] [Google Scholar]
- 50.Trotti A., Bellm L.A., Epstein J.B., Frame D., Fuchs H.J., Gwede C.K., Komaroff E., Nalysnyk L., Zilberberg M.D. Mucositis incidence, severity and associated outcomes in patients with head and neck cancer receiving radiotherapy with or without chemotherapy: A systematic literature review. Radiother. Oncol. J. Eur. Soc. Ther. Radiol. Oncol. 2003;66:253–262. doi: 10.1016/S0167-8140(02)00404-8. [DOI] [PubMed] [Google Scholar]
- 51.Sroussi H.Y., Epstein J.B., Bensadoun R.J., Saunders D.P., Lalla R.V., Migliorati C.A., Heaivilin N., Zumsteg Z.S. Common oral complications of head and neck cancer radiation therapy: Mucositis, infections, saliva change, fibrosis, sensory dysfunctions, dental caries, periodontal disease, and osteoradionecrosis. Cancer Med. 2017;6:2918–2931. doi: 10.1002/cam4.1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nascimento M.L., Farias A.B., Carvalho A.T., Albuquerque R.F., Ribeiro L.N., Leao J.C., Silva I.H. Impact of xerostomia on the quality of life of patients submitted to head and neck radiotherapy. Med. Oral Patol. Oral Y Cir. Bucal. 2019;24:e770–e775. doi: 10.4317/medoral.23131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vissink A., Mitchell J.B., Baum B.J., Limesand K.H., Jensen S.B., Fox P.C., Elting L.S., Langendijk J.A., Coppes R.P., Reyland M.E. Clinical management of salivary gland hypofunction and xerostomia in head-and-neck cancer patients: Successes and barriers. Int. J. Radiat. Oncol. Biol. Phys. 2010;78:983–991. doi: 10.1016/j.ijrobp.2010.06.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Brook I. Late side effects of radiation treatment for head and neck cancer. Radiat. Oncol. J. 2020;38:84–92. doi: 10.3857/roj.2020.00213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sumitsawan Y., Chaiyasate S., Chitapanarux I., Anansuthiwara M., Roongrotwattanasiri K., Vaseenon V., Tooncam H. Late complications of radiotherapy for nasopharyngeal carcinoma. Auris Nasus Larynx. 2009;36:205–209. doi: 10.1016/j.anl.2008.04.006. [DOI] [PubMed] [Google Scholar]
- 56.Amini A., Eguchi M., Jones B.L., Stokes W.A., Gupta A., McDermott J.D., Massarelli E., Bradley C.J., Karam S.D. Comparing outcomes of concurrent chemotherapy regimens in patients 65 years old or older with locally advanced oropharyngeal carcinoma. Cancer. 2018;124:4322–4331. doi: 10.1002/cncr.31740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Abernethy A.P., Wheeler J.L., Zafar S.Y. Management of gastrointestinal symptoms in advanced cancer patients: The rapid learning cancer clinic model. Curr. Opin. Support. Palliat. Care. 2010;4:36–45. doi: 10.1097/SPC.0b013e32833575fd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Colvin L.A. Chemotherapy-induced peripheral neuropathy: Where are we now? Pain. 2019;160:S1–S10. doi: 10.1097/j.pain.0000000000001540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chitsike L., Duerksen-Hughes P.J. Targeted Therapy as a Potential De-Escalation Strategy in Locally Advanced HPV-Associated Oropharyngeal Cancer: A Literature Review. Front. Oncol. 2021;11:730412. doi: 10.3389/fonc.2021.730412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Huang Y., Lan Y., Zhang Z., Xiao X., Huang T. An Update on the Immunotherapy for Oropharyngeal Squamous Cell Carcinoma. Front. Oncol. 2022;12:800315. doi: 10.3389/fonc.2022.800315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nishino M., Ramaiya N.H., Hatabu H., Hodi F.S. Monitoring immune-checkpoint blockade: Response evaluation and biomarker development. Nat. Rev. Clin. Oncol. 2017;14:655–668. doi: 10.1038/nrclinonc.2017.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Topalian S.L., Hodi F.S., Brahmer J.R., Gettinger S.N., Smith D.C., McDermott D.F., Powderly J.D., Carvajal R.D., Sosman J.A., Atkins M.B., et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N. Engl. J. Med. 2012;366:2443–2454. doi: 10.1056/NEJMoa1200690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Swain R.E., Biller H.F., Ogura J.H., Harvey J.E. An experimental analysis of causative factors and protective methods in carotid artery rupture. Arch. Otolaryngol. 1974;99:235–241. doi: 10.1001/archotol.1974.00780030245001. [DOI] [PubMed] [Google Scholar]
- 64.Self E.M., Bumpous J., Ziegler C., Wilson L., Potts K. Risk factors for hemorrhage after chemoradiation for oropharyngeal squamous cell carcinoma. JAMA Otolaryngol.—Head Neck Surg. 2013;139:356–361. doi: 10.1001/jamaoto.2013.103. [DOI] [PubMed] [Google Scholar]
- 65.Leedman S., Thompson A., Phillips T., Sader C. Major haemorrhage after non-surgical management of oropharyngeal squamous cell carcinoma. J. Laryngol. Otol. 2023;137:667–672. doi: 10.1017/S0022215122001918. [DOI] [PubMed] [Google Scholar]
- 66.Wong S.J., Machtay M., Li Y. Locally recurrent, previously irradiated head and neck cancer: Concurrent re-irradiation and chemotherapy, or chemotherapy alone? J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2006;24:2653–2658. doi: 10.1200/JCO.2005.05.3850. [DOI] [PubMed] [Google Scholar]
- 67.Chou C.T., Rath T.J., Johnson J.T., Goyal L.K. Catastrophic Hemorrhage After Chemoradiation for Advanced Stage Oropharyngeal Carcinoma: A Case Series. Laryngoscope. 2021;131:1049–1052. doi: 10.1002/lary.29167. [DOI] [PubMed] [Google Scholar]
- 68.Araujo A.V., Wax M.K., Clayburgh D.R., Andersen P.E., Chandra R.A., Li R.J. Acute and definitive management of oropharyngeal hemorrhage in patients with squamous cell carcinoma of the oropharynx. Head Neck. 2024;46:896–904. doi: 10.1002/hed.27632. [DOI] [PubMed] [Google Scholar]
- 69.Johnstone C., Rich S.E. Bleeding in cancer patients and its treatment: A review. Ann. Palliat. Med. 2018;7:265–273. doi: 10.21037/apm.2017.11.01. [DOI] [PubMed] [Google Scholar]
- 70.Chou W.C., Lu C.H., Lin G., Hong Y.S., Chen P.T., Hsu H.C., Chen J.S., Yeh K.Y., Wang H.M., Liaw C.C. Transcutaneous arterial embolization to control massive tumor bleeding in head and neck cancer: 63 patients’ experiences from a single medical center. Support. Care Cancer Off. J. Multinatl. Assoc. Support. Care Cancer. 2007;15:1185–1190. doi: 10.1007/s00520-007-0234-y. [DOI] [PubMed] [Google Scholar]
- 71.Zussman B., Gonzalez L.F., Dumont A., Tjoumakaris S., Rosenwasser R., Hasan D., Cognetti D., Axelrod R., Jabbour P. Endovascular management of carotid blowout. World Neurosurg. 2012;78:109–114. doi: 10.1016/j.wneu.2011.08.024. [DOI] [PubMed] [Google Scholar]
- 72.Greve J., Bas M., Schuler P., Turowski B., Scheckenbach K., Budach W., Bölke E., Bergmann C., Lang S., Arweiler-Harbeck D., et al. Acute arterial hemorrhage following radiotherapy of oropharyngeal squamous cell carcinoma. Strahlenther Onkol. 2010;186:269–273. doi: 10.1007/s00066-010-2114-5. [DOI] [PubMed] [Google Scholar]
- 73.Liang N.L., Guedes B.D., Duvvuri U., Singh M.J., Chaer R.A., Makaroun M.S., Sachdev U. Outcomes of interventions for carotid blowout syndrome in patients with head and neck cancer. J. Vasc. Surg. 2016;63:1525–1530. doi: 10.1016/j.jvs.2015.12.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Okamura H.O., Kamiyama R., Takiguchi Y., Kimizuka K., Ishikawa N., Kishimoto S. Histopathological examination of ruptured carotid artery after irradiation. ORL J. Oto-Rhino-Laryngol. Its Relat. Spec. 2002;64:226–228. doi: 10.1159/000058030. [DOI] [PubMed] [Google Scholar]
- 75.Iacobuzio-Donahue C.A., Michael C., Baez P., Kappagantula R., Hooper J.E., Hollman T.J. Cancer biology as revealed by the research autopsy. Nat. Rev. Cancer. 2019;19:686–697. doi: 10.1038/s41568-019-0199-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Pisapia D.J., Salvatore S., Pauli C., Hissong E., Eng K., Prandi D., Sailer V.W., Robinson B.D., Park K., Cyrta J., et al. Next-Generation Rapid Autopsies Enable Tumor Evolution Tracking and Generation of Preclinical Models. JCO Precis. Oncol. 2017;2017:PO.16.00038. doi: 10.1200/PO.16.00038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bradley P.J., Ferlito A., Lowe J., Devaney K.O., Wei W.I., Rinaldo A. A head and neck cancer patient dies! Why perform an autopsy: For the relatives, for the clinicians or for the pathologists? Acta Oto-Laryngol. 2003;123:348–354. doi: 10.1080/0036554021000001349. [DOI] [PubMed] [Google Scholar]
- 78.Pollanen M.S. Pitfalls and Artifacts in the Neck at Autopsy. Acad. Forensic Pathol. 2016;6:45–62. doi: 10.23907/2016.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Cartocci G., Santurro A., Frati P., La Russa R., Fineschi V. Radiology in Forensic Medicine: From Identification to Post-mortem Imaging. Springer; Cham, Switzerland: 2019. Imaging Techniques for Postmortem Forensic Radiology; pp. 29–42. [DOI] [Google Scholar]
- 80.Mentink M.G., Latten B.G.H., Bakers F.C.H., Mihl C., Benali F., Nelemans P.J., Rennenberg R.J.M.W., Koopmans R.P., Bergmans D.C.J.J., Kubat B., et al. Efficacy of postmortem CT and tissue sampling in establishing the cause of death in clinical practice: A prospective observational study. J. Clin. Pathol. 2024;77:259–265. doi: 10.1136/jcp-2021-207946. [DOI] [PubMed] [Google Scholar]
- 81.Cartocci G., Santurro A., Neri M., Zaccagna F., Catalano C., La Russa R., Turillazzi E., Panebianco V., Frati P., Fineschi V. Post-mortem computed tomography (PMCT) radiological findings and assessment in advanced decomposed bodies. La Radiol. Medica. 2019;124:1018–1027. doi: 10.1007/s11547-019-01052-6. [DOI] [PubMed] [Google Scholar]
- 82.Vullo A., Panebianco V., Cannavale G., Aromatario M., Cipolloni L., Frati P., Santurro A., Vullo F., Catalano C., Fineschi V. Post-mortem magnetic resonance foetal imaging: A study of morphological correlation with conventional autopsy and histopathological findings. La Radiol. Medica. 2016;121:847–856. doi: 10.1007/s11547-016-0672-z. [DOI] [PubMed] [Google Scholar]
- 83.La Russa R., Catalano C., Di Sanzo M., Scopetti M., Gatto V., Santurro A., Viola R.V., Panebianco V., Frati P., Fineschi V. Postmortem computed tomography angiography (PMCTA) and traditional autopsy in cases of sudden cardiac death due to coronary artery disease: A systematic review and meta-analysis. La Radiol. Medica. 2019;124:109–117. doi: 10.1007/s11547-018-0943-y. [DOI] [PubMed] [Google Scholar]
- 84.Örgüç S., Arkun R. Tumor-like Lesions of Bone and Soft Tissues and Imaging Tips for Differential Diagnosis. Semin. Musculoskelet. Radiol. 2020;24:613–626. doi: 10.1055/s-0040-1721378. [DOI] [PubMed] [Google Scholar]
- 85.Aguiar C., Pina P., Medeiros N., Teixeira M., Ribeiro L., Oliveira P. Necrosis of the Tongue as a Late Complication of Radiotherapy. Iran. J. Otorhinolaryngol. 2023;35:285–288. doi: 10.22038/IJORL.2023.67124.3305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Curi M.M., Cardoso C.L., Benites A.F.C., Bueno P.M. Delayed tongue necrosis simultaneous with bilateral osteoradionecrosis of the jaw secondary to head and neck irradiation. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2017;123:e28–e32. doi: 10.1016/j.oooo.2016.10.010. [DOI] [PubMed] [Google Scholar]
- 87.Santurro A., Frati P., Fineschi V. Risk Management, Patient Safety and Quality in Health Care. Curr. Pharm. Biotechnol. 2021;22:1962–1963. doi: 10.2174/138920102215210928154236. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data are included in a legal case in Italy, and for this reason, they are not available.