Abstract
A yellow fever virus (YFV)/Japanese encephalitis virus (JEV) chimera in which the structural proteins prM and E of YFV 17D are replaced with those of the JEV SA14-14-2 vaccine strain is under evaluation as a candidate vaccine against Japanese encephalitis. The chimera (YFV/JEV SA14-14-2, or ChimeriVax-JE) is less neurovirulent than is YFV 17D vaccine in mouse and nonhuman primate models (F. Guirakhoo et al., Virology 257:363–372, 1999; T. P. Monath et al., Vaccine 17:1869–1882, 1999). Attenuation depends on the presence of the JEV SA14-14-2 E protein, as shown by the high neurovirulence of an analogous YFV/JEV Nakayama chimera derived from the wild JEV Nakayama strain (T. J. Chambers, A. Nestorowicz, P. W. Mason, and C. M. Rice, J. Virol. 73:3095–3101, 1999). Ten amino acid differences exist between the E proteins of ChimeriVax-JE and the YFV/JEV Nakayama virus, four of which are predicted to be neurovirulence determinants based on various sequence comparisons. To identify residues that are involved in attenuation, a series of intratypic YFV/JEV chimeras containing either single or multiple amino acid substitutions were engineered and tested for mouse neurovirulence. Reversions in at least three distinct clusters were required to restore the neurovirulence typical of the YFV/JEV Nakayama virus. Different combinations of cluster-specific reversions could confer neurovirulence; however, residue 138 of the E protein (E138) exhibited a dominant effect. No single amino acid reversion produced a phenotype significantly different from that of the ChimeriVax-JE parent. Together with the known genetic stability of the virus during prolonged cell culture and mouse brain passage, these findings support the candidacy of this experimental vaccine as a novel live-attenuated viral vaccine against Japanese encephalitis.
The genus Flavivirus of the family Flaviviridae includes many arthropod-transmitted viral pathogens, including Yellow fever virus (YFV), the dengue viruses, and members of the Japanese encephalitis virus (JEV) serogroup and the Tick-borne encephalitis virus (TBEV) complex (33). JEV remains the most important cause of acute epidemic viral encephalitis worldwide (57) and has recently expanded its geographic range to threaten Indonesia and continental Australia (15, 16, 27). Vaccines available for prevention of JE include both inactivated and live-attenuated preparations (57). Formalin-inactivated vaccine produced from mouse brain (JE-Vax) is manufactured in Japan and licensed for use by travelers and military personnel in the United States and some European countries. Although it is effective, the multiple-dose regimen, the relatively high cost, and problems with reactogenicity (4, 41–43) complicate its use. The live-attenuated vaccine (JEV SA14-14-2), prepared from primary hamster kidney cell cultures, is given only in China, as this cell substrate is not acceptable for worldwide use.
To address the need for a second-generation vaccine against JEV, we have developed a candidate live-attenuated vaccine that may be manufactured in cell cultures to modern standards. The vaccine, ChimeriVax-JE, is a genetically engineered derivative of the yellow fever vaccine (YFV 17D), in which the genes encoding the structural proteins premembrane (prM) and envelope (E) of YFV 17D are replaced with the corresponding genes of the attenuated JEV SA14-14-2 strain (6). This experimental vaccine causes an active infection in recipient mice and rhesus monkeys and induces an immunity which is both rapid in onset and long-lasting after a single dose (13). Since the E protein contains the critical neutralizing antibody determinants (18, 26), the protective immune response elicited by vaccination is directed largely at JEV.
In principle, the attenuated phenotype and safety profile of the ChimeriVax-JE virus are based on the derivation of all of its genetic material from proven vaccine strains (YFV 17D and JEV SA14-14-2). YFV 17D vaccine is generally regarded as one of the safest and most effective live-attenuated viral vaccines ever developed and is licensed by national control authorities worldwide (34). The live-attenuated JEV SA14-14-2 vaccine, although less immunogenic than YFV 17D, has had an excellent safety record during widespread use in China (19, 57). Since RNA genomes of flaviviruses have high rates of mutation, it is important to understand the molecular basis for attenuation of experimental live virus vaccines and to demonstrate that multiple genetic determinants govern this property. The amino acid sequences of the prM and E regions of the nonneurovirulent ChimeriVax-JE virus and a corresponding neurovirulent YFV/JEV Nakayama virus differ by 3 and 10 amino acid residues, respectively (6). To evaluate the importance of the differences in the E protein for the attenuated phenotype of ChimeriVax-JE, we constructed a series of intratypic chimeras harboring either single or multiple amino acid reversions in the E protein. Neurovirulence was assessed by intracerebral (i.c.) inoculation in young adult mice.
MATERIALS AND METHODS
Cells and viruses.
Vero cells were originally obtained from Jerry Jennings (U.S. Army Medical Research Institute for Infectious Diseases, Fort Detrick, Md.) and were maintained in alpha minimal essential medium (Gibco/BRL, Grand Island, N.Y.) plus 10% fetal bovine serum (HyClone, Logan, Utah). Construction of the ChimeriVax-JE and YFV/JEV Nakayama viruses has been described previously (6).
Plasmid constructions.
Cloning of pBS/JE SA14-14-2, encoding the E protein region of the primary dog kidney (PDK)-passaged JEV SA14-14-2 strain (11) from nucleotides 1108 to 2472 (JEV numbering), was previously described (6). The reversion K138→E was introduced into this plasmid by subcloning a 110-bp AflIII/NcoI restriction fragment (JEV nucleotides 1320 to 1430) from pBS/JE Nakayama into pBS/JE SA14-14-2, resulting in pBS/JE SAF107E138. The two plasmids pBS/JE SA14-14-2 and pBS/JE SAF107E138 were then used as templates for derivation of plasmids containing additional reversions by site-directed mutagenesis. Mutagenesis was performed using the Transformer site-directed mutagenesis kit (Clontech, Palo Alto, Calif.). Oligonucleotide primers (Table 1) were synthesized at Life Technologies (Grand Island, N.Y.). These included silent restriction sites to facilitate screening for the desired mutations. Convenient restriction sites in some of the mutagenized pBS/JE plasmids were used to create plasmids containing multiple reversions. All plasmids were analyzed by nucleotide sequencing of the E region for the presence of the engineered mutation and to verify the integrity of nonmutagenized regions. A region encompassing the mutation(s) was then subcloned from the pBS/JE plasmids into pYFM5.2/JE SA14-14-2 (6), using NheI and EheI restriction sites. In one case, to generate the single revertant F107→L, a small NheI/AflIII restriction fragment from pBS/JE Nakayama was used to replace the corresponding region of pYFM5.2/JE SA14-14-2.
TABLE 1.
Oligonucleotide primers used for engineering revertant viruses by site-directed mutagenesis
| Purpose or name of primer | Primer sequencea | Marker site(s) |
|---|---|---|
| Mutagenesis of E protein position | ||
| 107 | 5′-GGATGTGGACTGTTCGGGAAGGGGATCCATTGAC | BamHI |
| 176 | 5′-GCTCCTTCGATCGCCCTCAAGCTTGGTGAC | HindIII |
| 177 | 5′-CCTTCGGTAACACTCAAGCTTGGTGAC | HindIII |
| 227 | 5′-CTCCCTTGGACGCCTCCTTCGAGCAC | AatII removed |
| 244 | 5′-ATGGAATTTGAAGAAGCGCATGCCACAAAAC | SphI |
| 264 | 5′-GGCCTCCATCAGGCGTTGGCCGGCGCAATC | NaeI |
| 279 | 5′-AGCTCAGTGAAATTAACTAGTGGCCACCTG | SpeI |
| 315 | 5′-GCGAAAAATCCGGCCGACACTGGTCAC | EagI |
| 439 | 5′-AACTCCATAGGAAAAGCCGTGCACCAAGTG | ApaLI |
| Selectionb | ||
| 1 | 5′-GGAATTCGATATCACGCGTATCGATACC | HindIII/MluI |
| 2 | 5′-CCGGGCTGCAGGATATCGATATCAAGC | EcoRI/EcoRV |
| 3 | 5′-GGGCTGCAGGATATCGCTATCAAGCTTATCG | EcoRI/EcoRV2 |
For each sequence, boldface indicates the codon that mutagenized the relevant residue of the E protein. Silent codon changes are underlined.
Selection primers were tested for efficiency; primer 3 was used preferentially.
RNA transcription and transfection.
Full-length cDNA templates were assembled by in vitro ligation of restriction fragments derived from pYF5′3′IV/JE SA14-14-2 (6) and the various mutagenized versions of pYFM5.2/JE SA14-14-2 after digestion with NheI and BspEI and purification of the appropriate fragments from agarose gels. The templates were transcribed using an AmpliScribe SP6 kit in the presence of methylated cap analog (Epicentre, Madison, Wis.). RNA transfection of Vero cells was done in the presence of Lipofectin (Gibco/BRL), using approximately 250 ng of RNA transcript as originally described (46). Viruses were harvested from the cultures approximately 3 days after transfection, and 1/10 of the volume of harvested medium was used for amplification of virus on Vero cells. Amplified viruses (Vero passage 1) were harvested after onset of cytopathic effects, and recovered virus was quantitated by plaque titration on Vero cells. Viruses were not plaque purified prior to neurovirulence testing, but nucleotide sequence analysis was done for each revertant to verify the presence of the engineered mutation(s) (see below).
Nucleotide sequence analysis.
Total RNA was extracted using Trizol (Gibco/BRL) either from infected Vero cell monolayers at passage 1 or from homogenates of virus-infected mouse brain (10% [wt/vol] in phosphate-buffered saline plus 10% fetal calf serum). Sequencing of the prM-E region for each virus was done using reverse transcription-PCR-based methods as previously described (13). Reaction mixtures were analyzed on a model 310 Genetic Analyzer (PE Applied Biosystems, Foster City, Calif.), and DNA sequences were refined using Sequencher 3.0 software (GeneCodes, Ann Arbor, Mich.). Amino acid sequence comparisons were performed using BLAST searches (3), and sequence alignments of related viruses were performed using CLUSTAL W (55).
Mouse experiments.
All studies involving mice were conducted in vertebrate animal biosafety level 3 facilities in accordance with the U.S. Department of Agriculture Animal Welfare Act (9 CFR Parts 1 to 3) as described in the Guide for Care and Use of Laboratory Animals. Protocols were approved by Institutional Animal Care and Use committees. Three- to four-week-old outbred mice (ICR) were purchased from either Harlan Sprague-Dawley (Indianapolis, Ind.) or Taconic Farms, Inc. (Germantown, N.Y.). Neurovirulence testing was done by i.c. inoculation of anesthetized mice with 0.03 ml of either phosphate-buffered saline or M199 medium (Gibco/BRL) plus 10% fetal bovine serum, containing approximately 10,000 PFU of virus. Virus doses were confirmed by plaque assay of the inocula on Vero cells. Endpoints of the neurovirulence experiments were scored as both mortality ratios and average survival times (ASTs). Any mice found in a moribund condition were euthanatized and scored as dead. Statistical significance of mortality differences was measured by proportions of survivors in test groups versus controls, using Fisher's exact test.
RESULTS
Design of the intratypic viruses.
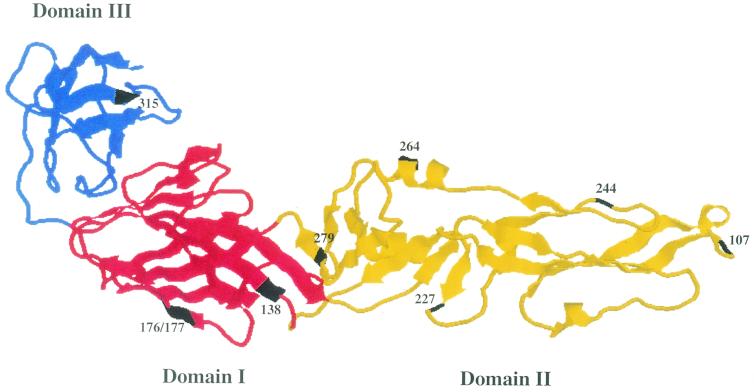
The attenuated JEV SA14-14-2 was originally developed in China by prolonged passage of its virulent JEV SA14 parent in primary hamster cell culture, followed by multiple passages of plaque-purified virus sequentially using peripheral inoculation of hamsters and suckling mice, to improve immunogenicity (summarized in references 1, 37, and 57). Mutations responsible for the attenuated phenotype of the vaccine strain were subsequently predicted by comparing its nucleotide sequence with that of its parent (1, 37, 38, 40). The availability of the three-dimensional structure of the E protein of TBEV (44) and the homology-based model for the E protein of JEV (25) has guided the development of hypotheses about the roles of amino acid substitutions in the JEV E protein in the attenuation process. The positions of the residues which differentiate ChimeriVax-JE from the YFV/JEV Nakayama virus are shown in Fig. 1. Single mutations (at E protein residue 315 [E315] and E439) are found in domain III and the C-terminal stem-anchor region, respectively. Three mutations (at E138 and E176/177) map to domain I (central domain), and the remaining five (at E107, E227, E264, E279, and E244) map to domain II (dimerization domain). We designated residues as “cluster specific,” on the basis of their locations within the different functional regions of the protein. The underlying hypothesis was that if the full neurovirulence phenotype involves multiple genetic determinants, distinguishable levels of virulence would correlate with the extent of reversions in the various clusters. Table 2 shows the list of single and multiple site revertants of the ChimeriVax-JE virus which were tested in this study.
FIG. 1.
Ribbon diagram of the E protein structure based on the model of the soluble fragment of TBEV (44). Numbered arrows indicate positions in domain I, II, or III of the E protein of candidate residues involved in the attenuation phenotype of the ChimeriVax-JE virus.
TABLE 2.
List of revertants of ChimeriVax-JE used to identify residues involved in the attenuated phenotypea
| E protein amino acid position | Residue
|
Revertant
|
|||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| YFV/Nakayama | YFV/SA14-14-2 | Single site
|
Multiple site
|
||||||||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | |||
| 107 | L | F | L | F | F | F | F | F | F | F | F | L | L | F | L | L | F | L | F | L | L |
| 138 | E | K | K | E | K | K | K | K | K | K | K | K | E | E | E | E | E | E | E | K | E |
| 176 | I | V | V | V | V | V | V | V | V | V | I | I | V | I | I | V | V | V | I | I | I |
| 177 | T | A | A | A | A | A | A | A | A | A | T | T | A | T | T | A | A | A | T | T | T |
| 227 | P | S | S | S | P | S | S | S | S | S | S | S | S | S | S | S | P | P | P | P | P |
| 244 | E | G | G | G | G | E | G | G | G | G | G | G | G | G | G | G | G | G | G | G | G |
| 264 | Q | H | H | H | H | H | Q | H | H | H | H | H | H | H | H | H | Q | Q | Q | Q | Q |
| 279 | K | M | M | M | M | M | M | K | M | M | M | M | M | M | M | K | K | K | K | K | K |
| 315 | A | V | V | V | V | V | V | V | A | V | V | V | V | V | V | V | V | V | V | V | V |
| 439 | K | R | R | R | R | R | R | R | R | K | R | R | R | R | R | R | R | R | R | R | R |
Candidate neurovirulence determinants (boldface) were introduced singly or as multiples in exchange for the YFV/JEV SA14-14-2-specific residue.
To determine if a single reversion could alter the neurovirulence phenotype, each of the residues which differentiate the E proteins of the JEV Nakayama and JEV SA14-14-2 strains were individually reverted and tested. Residues E176 and E177 were reverted together because of their proximity. Beyond the analysis of single revertants, the construction of multiple site revertants was complicated due to the large number of possible combinations. We therefore adopted a strategy based on the relationship between passage history and accumulation of sequential mutations in the JEV SA14-14-2 E protein, while also taking into account their domain-specific locations. Within domain II, E107 was regarded as a distinct cluster because of its distal location in this fingerlike region of the protein. E138, at the base of domain II, was segregated because of its probable role as a neurovirulence determinant for JEV (7, 53). The remaining residues in domain II (E227, E264, and E279) were initially reverted together as a single cluster, based on their general vicinity within the proximal portion of the domain. Residue E279 was later tested in combination with residues E107 and E138, as it was suspected to contribute a dominant effect in its cluster. Residue E244 was not included in the construction of multiple revertant viruses, because its presence in the parental JEV SA14 strain suggests that it is not a virulence determinant (13). Residues E315 and E439 were reverted individually due to their locations in either domain III or the stem-anchor region, respectively.
Nucleotide sequence analysis.
The E protein region of each revertant virus underwent nucleotide sequence analysis at passage level 1 (first amplification of the transfection harvest on Vero cells), which was the preparation used for mouse neurovirulence testing. Sequence analysis revealed the presence of the engineered mutations and only a few additional silent mutations. Revertant 1 (E107) contained the silent mutation C→T at nucleotide position 294 of the E gene, which originated from the cDNA fragment subcloned from the pBS/JE Nakayama plasmid. Every virus containing the reversion at K138→E also introduced a silent mutation (A→G) at nucleotide position 372 of the E gene, which originated from the fragment of JEV Nakayama cDNA used to generate pBS/JE SAF107E138 (see Materials and Methods). Two other silent mutations were included during the site-directed mutagenesis to revert residues E227 and E264 (T→C at nucleotide position 672 and A→C at position 807). Both of these mutations were detected in the respective revertant viruses.
Mouse neurovirulence testing.
The neurovirulence of single and multiple site revertants was expressed as the mortality ratio and AST following i.c. inoculation with virus. The ChimeriVax-JE (YFV/JEV SA14-14-2) and YFV/JEV Nakayama viruses (both at passage level 1 on Vero cells) were used as the attenuated and virulent controls, respectively. Results are shown in Table 3. Revertant viruses were classified into three groups, based on the level of associated mortality. Lethal revertants (mortality ratios of ≥89% [not significantly different from YFV/JEV Nakayama]) included 13, 16, 17, and 19. Sublethal revertant viruses (mortality ratios between 13 and 38% [significantly different from YFV/JEV Nakayama, but not ChimeriVax-JE]) included 11, 12, 14, and 15. Attenuated revertants included those in which no mortality occurred, except for revertant 6, for which one of eight mice succumbed 5 days postinoculation. ASTs for all mice with mortality endpoints varied from 9 to 13 days, essentially the same as those for the YFV/JEV Nakayama virus control.
TABLE 3.
Neurovirulence testing of revertant viruses by i.c. inoculation of 4-week-old ICR mice with 104 PFU of virus
| Virus or revertanta | No. of dead mice/total no. of mice (%)b | AST (days) |
|---|---|---|
| YFV/JEV SA14-14-2 | 0/8 (0) | |
| 1 (107; F→L) | 0/8 (0) | |
| 2 (138; K→E) | 0/8 (0) | |
| 3 (227; S→P) | 0/8 (0) | |
| 4 (244; G→E) | 0/8 (0) | |
| 5 (264; H→Q) | 0/8 (0) | |
| 6 (279; M→K) | 1/8 (13) | |
| 7 (315; V→A) | 0/8 (0) | |
| 8 (439; R→K) | 0/8 (0) | |
| 9 (176/177; V/A→I/T) | 0/8 (0) | |
| 10 (107, 176/177) | 0/8 (0) | |
| 11 (107, 138)c | 1/8 (13) | 9.0 |
| 12 (138, 176/177) | 1/8 (13) | 13.0 |
| 13 (107, 138, 176/177)d | 9/9 (100) | 9.4 |
| 14 (107, 138, 279) | 3/8 (38) | 11.3 |
| 15 (138, 227, 264, 279) | 2/9 (22) | 11.5 |
| 16 (107, 138, 227, 264, 279) | 8/9 (89) | 9.4 |
| 17 (138, 176/177, 227, 264, 279) | 9/9 (100) | 9.0 |
| 18 (107, 176/177, 227, 264, 279) | 0/8 (0) | |
| 19 (107, 138, 176/177, 227, 264, 279) | 8/8 (100) | 8.1 |
| YFV/JEV Nakayama | 8/8 (100) | 9.3 |
| YFV/JEV Nakayama | 7/8 (88) | 11.6 |
Viruses with neurovirulent phenotypes are indicated by boldface. For viruses 1 to 9, the positions of and reversions at the single sites are indicated. For viruses 10 to 19, the positions of the multiple reversions are indicated.
For revertants 1 to 12 compared with YFV/JEV SA14-14-2, there was no significance. For revertants 14 and 15 compared with YFV/JEV Nakayama, P was 0.01 and 0.002, respectively. For revertants 13, 16, and 17 and YFV/JEV Nakayama compared with YFV/JEV SA14-14-2, P was <0.0001, <0.0005, <0.0001, and <0.0001, respectively.
One of two experiments; the mortality ratio for the second experiment was 0%.
One of two experiments; mortality was identical for the second experiment (AST was 9.9 days).
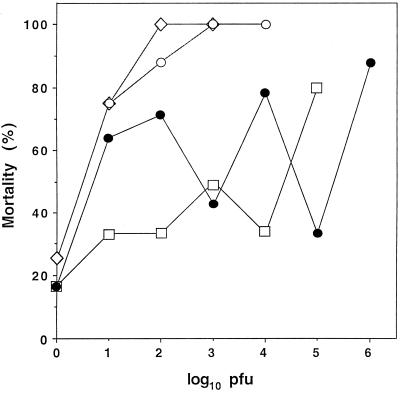
Within the group of lethal revertants, revertant 13 contained the lowest number of substitutions (four). To determine if its level of neurovirulence was quantitatively the same as that of the YFV/JEV Nakayama virus, graded dose testing was done (Fig. 2). Revertant 11 was also analyzed because it exhibited a dramatic difference in mortality from revertant 13, while differing only by the absence of the E176/177 cluster. Revertant 13 exhibited a 50% lethal dose (LD50) of less than 10 PFU. For revertant 11, two independently derived clones showed variable mortality ratios over doses between 1 and 100,000 PFU, making the LD50 measurement indeterminant. At the dose of 10,000 PFU, mortality ranged from 35 to 80%. Because of this variability, revertant 11 was sequenced using RNA from infected mouse brains to determine whether new mutations had occurred during replication of this virus in vivo. Analysis of the prM-E region for three separate samples revealed no differences from the sequence determined for the original passage 1 virus. It should be noted that two different lineages of ICR mice {Hsd:ICR(CD-1R) and Tac:Icr:Ha[ICR]fBR} were used for the initial neurovirulence testing (Table 3) and the LD50 determinations (Fig. 2), respectively. The former exhibited a mortality ratio of 13% whereas the latter exhibited the higher mortality ratios at the 10,000-PFU dose. These two random-bred ICR stocks have been sustained using different breeding protocols following their common origin as the Fox Chase version in 1959. We suspect that genetic differences among these mice may partly account for the variable neurovirulence properties of revertant 11 observed in these experiments.
FIG. 2.
Graded-dose neurovirulence testing of revertants 11 and 13 by i.c. inoculation of ICR mice. YFV/JEV Nakayama was used as the virulent control. Two independent clones of revertant (Rev.) 11 were used in this experiment. Mortalities at different doses were as follows: 0 logs, revertant 11-1 (1 of 6), revertant 11-2 (1 of 6), revertant 13 (not done), and YFV/JEV Nakayama (2 of 8); 1 log, revertant 11-1 (9 of 14), revertant 11-2 (2 of 6), revertant 13 (6 of 8), and YFV/JEV Nakayama (6 of 8); 2 logs, revertant 11-1 (10 of 14), revertant 11-2 (2 of 6), revertant 13 (7 of 8), and YFV/JEV Nakayama (8 of 8); 3 logs, revertant 11-1 (6 of 14), revertant 11-2 (3 of 6), revertant 13 (8 of 8), and YFV/JEV Nakayama (8 of 8); 4 logs, revertant 11-1 (11 of 14), revertant 11-2 (2 of 6), revertant 13 (8 of 8), and YFV/JEV Nakayama (not done); 5 logs, revertant 11-1 (4 of 12), revertant 11-2 (4 of 5), and revertant 13 and YFV/JEV Nakayama (not done); 6 logs, revertant 11-1 (7 of 8), and revertants 11-2, 13, and YFV/JEV Nakayama (not done). Differences between 11-1 and YFV/JEV Nakayama were significant for doses of 3 logs (P = 0.012), and 5 logs (P = 0.01). Differences between 11-2 and YFV/JEV Nakayama were significant for doses of 2 logs (P = 0.015) and 4 logs (P = 0.015) (Fisher's exact test). Symbols: open diamonds, YFV/JEV Nakayama; open circles, revertant 13; solid circles, revertant 11-1; open squares, revertant 11-2.
To further investigate the variability in mortality ratios observed with revertant 11, additional experiments were done with this revertant, as well as additional revertants, in ICR mice of both lineages. In Ha[ICR]fBR mice, revertants 11, 12, and 13 were compared at a dose of 4.0 logs using ChimeriVax-JE and YFV/JEV Nakayama viruses as controls. Mortality ratios and ASTs were as follows: revertant 11, seven of eight dead (AST of 10.6 days); revertant 12, three of nine dead (AST of 14.7 days); revertant 13, eight of eight dead (AST of 11.1 days); YFV/JEV Nakayama, eight of eight dead (AST of 9.1 days); ChimeriVax, zero of eight dead. In CD-1R mice, revertants 11, 12, and 15 were compared in an independent experiment using ChimeriVax-JE and YFV/JEV Nakayama viruses as controls. Mortality ratios were as follows: for revertant 11 at 4.0 logs, one of eight dead (day 10); for revertant 12 at 4.0 logs, one of eight dead (day 14); for revertant 12 at 4.7 logs, zero of seven dead; for revertant 15 at 4.0 logs, one of eight paralyzed; for revertant 15 at 4.7 logs, zero of seven dead; for ChimeriVax-JE at 6.0 logs, zero of eight dead; for YFV/JEV Nakayama at 4.0 logs, seven of seven dead (AST of 9.1 days).
Taken together with the results presented in Table 3 and Fig. 2, the data indicate that a distinct difference in the behavior of revertant 11 occurs between ICR mice of the two lineages and that this is not due to a general increase in the sensitivity of the Ha[ICR]fBR mice to these viruses, as neither the ChimeriVax-JE virus nor another sublethal revertant differed in their virulence phenotype between the two mouse strains. Furthermore, revertant 11 exhibited a variable mortality ratio across a wide range of doses, but its phenotype did not resemble that of the YFV/JEV Nakayama virus. The neurovirulence properties of revertant 11 are governed by the strain of mouse employed, and the revertant cannot be classified as either completely attenuated or fully virulent.
DISCUSSION
We used a previously established genetic system (6) to test whether the attenuated phenotype of the ChimeriVax-JE virus could be defined in terms of specific amino acid residues of the E protein. This question is relevant to the use of the virus as a live-attenuated vaccine against JE. A nominal requirement for such a vaccine is the presence of multiple mutations which independently contribute to attenuation. In the case of other flaviviruses, this has commonly been observed among pairs of virulent and attenuated viruses (14, 24, 40). YFV 17D vaccine, for example, differs from the parental Asibi strain by a total of 32 amino acid substitutions, 12 of which occur in the E protein and are believed to include virulence determinants (14). Despite this, it is known that as few as two mutations in the E protein of the YFV 17D vaccine can revert the virus to a neurovirulent phenotype, although this is a very rare occurrence (22). This points out the fact that absolute stabilization of the vaccine phenotype in a cell culture-passaged virus is very problematic, a reality that has been faced for other live-attenuated viral vaccines such as poliovirus (45, 54). To address the question of whether single or multiple amino acid reversions in the E protein of ChimeriVax-JE were required to increase its neurovirulence properties, we tested viruses which contained substitutions at sites known to be associated with the attenuation process.
In general, the severities of the neurovirulence phenotypes correlated directly with the number of engineered reversions. Single substitutions (with the exception of revertant 6) produced attenuated viruses. Further studies are needed to determine whether the 13% mortality rate for revertant 6 reflects a real neurovirulence difference from the ChimeriVax-JE virus. Two to three substitutions produced either attenuated (revertant 10) or sublethal (revertants 11, 12, and 14) viruses. Four substitutions created a sublethal revertant when two clusters were included (revertant 15 [E138, E227, E264, E279]) but a lethal revertant when three clusters were involved (revertant 13 [E107, E138, E176/177]). This latter combination of four reversions is probably sufficient for restoration of full neurovirulence, since the LD50 of revertant 13 (Fig. 2) is similar to that of the YFV/JEV Nakayama virus, previously determined to be less than 10 PFU (6). More than four substitutions generated lethal revertants, but only when the E138 reversion was present (see below). It should therefore be emphasized that, except for revertant 13, all viruses with four or fewer substitutions had mortality ratios significantly less than that of the virulent YFV/JEV Nakayama virus (P ≤ 0.01).
The level of neurovirulence was affected not only by the number of engineered reversions but also by their specific combination. For example, revertant 18 (E107, E176/177, E227, E264, E279) was attenuated, whereas revertant 17 (E138, E176/177, E227, E264, E279) was fully neurovirulent. In this case, substitution at the E138 cluster rather than at E107 conferred neurovirulence in the presence of the E176/177 and E227-E264-E279 reversions. Residue E138 has been identified as a principal virulence determinant of JEV in the background of the JaOArS982 and NT109 strains (7, 53). Our data are generally consistent with this finding. Although a single reversion at E138 was insufficient to restore neurovirulence, its presence together with any other reverted cluster (such as in revertants 11, 12, and 15) always produced viruses with at least sublethal phenotypes. Thus, while reversion at residue E138 has a dominant effect on neurovirulence properties of the ChimeriVax-JE virus, it must occur with multiple other reversions to restore a fully neurovirulent phenotype. Residue E138 lies in the so-called “hinge” region at the domain I-II interface of the E protein. Studies with several flaviviruses have provided data indicating that mutations within this region modulate virulence phenotypes in mice (5, 7, 12, 17, 29, 30, 53). This is believed to occur through effects of such mutations on the low-pH-induced dimer-to-trimer structural transition of the E protein associated with virus entry.
In contrast to those at the E138 cluster, reversions at the other sites were not absolutely required for reconstitution of lethal or even sublethal phenotypes. However, reversions at each cluster contributed to measurable increases in neurovirulence. Reversion at residue E107 had minimal or sublethal effects in combination with a reversion at a single other cluster (revertants 10 and 11). However, a marked enhancement of virulence occurred in viruses containing the E107 reversion plus reversions at two or more additional clusters (when E138 was included). Its effect in combination with reversions at the E227-E264-E279 cluster has not been tested, but this would be expected to result in a sublethal or attenuated virus. Residue E107 lies within a highly conserved hairpin motif encompassing amino acids 98 to 111 of domain II (25). This region is believed to contain the fusogenic peptide, based on studies with Murray Valley encephalitis and dengue 2 viruses (47, 48). Mutations near this region change the fusion properties of the E protein in cell culture and have been associated with alterations in neurovirulence (10, 44).
The E176/177 cluster was identified as an independent virulence determinant by comparison of revertant 13 (E107, E138, E176/177 [100% mortality]) with revertant 11 (E107, E138 [13% mortality]; P < 0.005). This conclusion is also supported by comparison of revertants 15 (E138, E227, E264, E279) and 17 (E138, E176/177, E227, E264, E279), where inclusion of E176/177 increased mortality from 22 to 100% (P < 0.005). Thus, as for residues E138 and E107, reversion at the E176/177 cluster enhanced the virulence of viruses containing reversions at each of the other clusters. Residues E176/177 lie within the central domain of the E protein, a region enriched in conformational epitopes which are sensitive to low pH. Structural changes associated with the reorganization of the E protein dimer into the fusion-active trimer are believed to occur within this domain (2, 52). The region surrounding the E176/177 cluster has been implicated as a virulence locus on the basis of numerous genetic and functional studies. For YFV, residue E173 is a position where the YFV 17D vaccine differs from the virulent Asibi, French viscerotropic, and French neurotropic strains (14, 21). Neuroadaptation of YFV 17D vaccine to mouse brain is associated with reversion of this residue (I173→T) (51). In addition, a mutation at residue E181 in the TBEV affects mouse neurovirulence by lowering the threshold for low-pH-induced fusion of the E protein (20). Although we have not demonstrated whether reversions at both E176 and E177 are required for the effect of this cluster on neurovirulence, data discussed below suggest that E176 may be the more important determinant.
Within the E227-E264-E279 cluster, reversion at E279 appeared to increase neurovirulence, since revertant 11 (E107, E138) caused 13% mortality, whereas revertant 14 (E107, E138, E279) caused 38% mortality, even though this difference was not statistically significant (P > 0.05). Residue E279 lies within the hinge region of the E protein and may affect its properties in a manner similar to that of the E138 residue. Studies with Murray Valley encephalitis virus have shown that mutations near this position can impair the hemagglutination and fusion properties of the E protein and reduce neuroinvasiveness for mice (29, 31). The full neurovirulence effect contributed by the E227-E264-E279 cluster required at least one additional reversion beyond E279 (compare revertant 14 with revertant 16 [E107, E138, E227, E264, E279]; 89% mortality; P = 0.043). There is some evidence that E264, rather than E227, accounts for this effect, since an E227 serine is present in all JEV SA14 strains and their cell culture-passaged derivatives, and the mutation to proline at this residue occurs instead in the JEV Nakayama strain. These conclusions about the roles of both the E176/177 and E227-E264-E279 clusters in attenuation are also supported by comparison of the sequences of the parental JEV SA14 strain and its attenuated derivatives (1, 37, 40). The attenuated JEV SA14-5-3 strain (an early progenitor of JEV SA14-14-2) contains substitutions at E107, E138, E176, and E279. These mutations remained stable during sequential primary hamster kidney and PDK cell passage. However, substitutions at E177 and E264 were unstable after PDK cell passage and reverted back to the original residues, despite the virus remaining attenuated. Thus, reversions at these two positions may not independently contribute a strong effect to neurovirulence. The JEV SA14-2-8 virus, another attenuated derivative of the SA-14 parent, and not a progenitor of JEV SA14-14-2, also contains the same mutations at E138 and E176 as does the JEV SA14-14-2 virus (in addition to three other substitutions specific to its E protein). Although the data taken together suggest that E176 and E279 may be the principal virulence determinants of their clusters, the effects of combinations of substitutions within either cluster on neurovirulence remain unpredictable, and comparisons with E proteins of other attenuated strains may be complicated by the presence of unrelated mutations. Full understanding of the contribution of residues within the E176/177 and E227-E264-E279 clusters will require systematic studies of additional engineered revertants.
With regard to the substitutions in domain III (E315) and the stem-anchor region (E439), viruses containing single reversions at these residues were attenuated. However, a revertant containing both substitutions was not tested in our experimental system. Residue E315 lies along the distal surface of domain III, a region which has been previously implicated in the process of virion attachment to host cells (44). In YFV and JEV, mutations in the vicinity of E315 are associated with altered virus tropism and changes in virulence (22, 23, 39, 49). Residue E439 lies within a predicted alpha-helical segment of the stem-anchor region whose structural integrity is required for stability of the prM-E heterodimer, based on studies with TBEV (2). The conservative nature of the K→R substitution at position E439 in ChimeriVax-JE may mitigate against any major effect of this mutation on the properties of the E protein; however, this remains to be tested. In short, we cannot at present exclude the possibility that a combination of reversions at residues E315 and E439 could increase the neurovirulence of ChimeriVax-JE, but determinants in domains I and II alone are clearly capable of conferring high-level neurovirulence. Testing of additional combinations of multiple site revertants is needed to further understand the quantitative contributions of the various virulence determinants tested here. It should be emphasized that, in addition to the reversions in the E protein, it remains possible that effects of mutations in the prM region (where three conservative substitutions occur between the ChimeriVax-JE and YFV/JEV Nakayama viruses [6]) could conceivably contribute to enhanced neurovirulence. We also acknowledge that any conclusions drawn here about the proposed functional role of the various mutations in the attenuated phenotype of ChimeriVax-JE remain speculative in the absence of direct experimental data examining their effects on the structure and function of the E protein.
Based on the data presented here, we believe that no single amino acid reversion in the E protein of ChimeriVax-JE to that of JEV Nakayama could restore a mouse neurovirulent phenotype. This suggests a relatively stable genetic basis for attenuation of this experimental vaccine. In fact, ChimeriVax-JE may be safer than the YFV 17D vaccine, based on clinical experience and collective mouse and primate neurovirulence data. Vaccination of humans with YFV 17D has caused only 21 known cases of postvaccinal encephalitis, the majority in infants, despite administration of over 300 million doses (34). No case of postvaccinal encephalitis has been reported with the use of JEV SA14-14-2 vaccine (57). Experimentally, neurovirulence occurs in mice inoculated with YFV 17D at a dose as low as 1.4 log10 PFU, while ChimeriVax-JE causes 0% mortality even at doses of 6 log10 PFU (6, 13). Moreover, ChimeriVax-JE is less neurovirulent than YFV 17D in primate neurovirulence testing (35, 36). Although the results reported here are promising with regard to the safety profile of ChimeriVax-JE, they cannot be generalized to the primate system, where host range differences could influence the virulence profiles of the revertant viruses. In some cases, however, concordance between mouse and monkey neurovirulence among flavivirus strains has been observed elsewhere (32). Appropriate animal testing to establish the attenuation phenotype in conjunction with verification of stability of the virus upon serial passage in vitro and in vivo and confirmation of the vaccine genotype at the final step of manufacturing are minimal requirements to be met in terms of monitoring for the emergence of a virulent revertant.
Finally, the results of this study may also be applicable to understanding the molecular basis of neurovirulence of other closely related flaviviruses. To address this question, amino acid sequences surrounding residues E107, E138, E176, E264, and E279 of the JEV Nakayama strain (28) were analyzed using the BLAST search program. Top-scoring E protein sequences were then aligned with CLUSTAL W (Fig. 3). Viruses with the highest scores were Murray Valley encephalitis virus (9), Kunjin virus (8), West Nile virus (WN-RO9750 strain) (50), and St. Louis encephalitis virus (56), in that order. The presence of highly conserved amino acid sequences encompassing positions E107, E138, E264, and E279 (and a less conserved E176 region) raises the possibility that mutations at the equivalent residues or adjacent residues may affect the virulence phenotypes of the related flaviviruses. Any such mutations would most likely be constrained by the potential for deleterious effects on critical functions associated with these various regions of the E protein, which could reduce viral fitness. Because the E proteins of the JEV serogroup viruses generally exhibit a high level of amino acid homology, it is possible that other conserved regions may harbor additional determinants of neurovirulence not identified here, as other studies have suggested (39). In any case, identification of residues in the E protein which govern neurovirulence is a starting point for further investigations. These might include mutagenesis of the critical determinants and surrounding residues, in conjunction with molecular clone technology, to generate additional live-attenuated virus vaccine candidates in the ChimeriVax background.
FIG. 3.
Sequence alignment (CLUSTAL W) of the E proteins of JEV serogroup members in regions surrounding the residues involved in attenuation (indicated in boldface). Residues of the JEV SA14-14-2 strain are shown above the alignments. The hyphen denotes a missing residue in the alignment for JEV. Symbols indicate fully conserved (asterisks), strongly conserved (colons), or weakly conserved (periods) residues. Strains were as follows: JE-Nakayama, JEV Nakayama strain (28); Murray Valley, Murray Valley encephalitis strain (9); Kunjin, Kunjin virus strain (8); WN-RO9750, West Nile virus RO9750 strain (50); St. Louis, St. Louis encephalitis strain (56).
ACKNOWLEDGMENTS
We thank Brigitte T. Huber and Sue Hurta (Tufts University) for biosafety level 3 facility support and Chuck Miller, OraVax, Inc., and Deborah Droll, Saint Louis University, for expert technical assistance.
This work was supported in part by grants from the NIAID (AI-136798 [OraVax] and AI-43512-03 [T.J.C.]), the WHO Global Program for Vaccines and Immunization (T.J.C.), and the Edward Mallinckrodt, Jr. Foundation (T.J.C.).
REFERENCES
- 1.Aihara S, Chunming R, Yong-Xin Y, Lee T, Watanabe K, Komiya T, Sumiyoshi H, Hashimoto H, Nomoto A. Identification of mutations that occurred on the genome of Japanese encephalitis virus during the attenuation process. Virus Genes. 1991;5:95–109. doi: 10.1007/BF00571925. [DOI] [PubMed] [Google Scholar]
- 2.Allison S L, Stiasny K, Stadler K, Mandl C W, Heinz F X. Mapping of functional elements in the stem-anchor region of tick-borne encephalitis virus envelope protein E. J Virol. 1999;73:5605–5612. doi: 10.1128/jvi.73.7.5605-5612.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Altschul S F, Madden T L, Schaffer A A, Zhang J, Zhang Z, Miller W, Lipman D J. Gapped BLAST and PSI-BLAST: a new generation of protein database search programs. Nucleic Acids Res. 1997;25:3389–3402. doi: 10.1093/nar/25.17.3389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berg S W, Mitchell B S, Hanson R K, Olafson R P, Williams R P, Tueller J E, Burton R J, Novak D M, Tsai T F, Wignall F S. Systemic reactions in U.S. marine corps personnel who received Japanese encephalitis vaccine. Clin Infect Dis. 1997;24:265–266. doi: 10.1093/clinids/24.2.265. [DOI] [PubMed] [Google Scholar]
- 5.Cecilia D, Gould E A. Nucleotide changes responsible for loss of neuroinvasiveness in Japanese encephalitis virus neutralization-resistant mutants. Virology. 1991;181:70–77. doi: 10.1016/0042-6822(91)90471-m. [DOI] [PubMed] [Google Scholar]
- 6.Chambers T J, Nestorowicz A, Mason P W, Rice C M. Yellow fever/Japanese encephalitis chimeric viruses: construction and biological properties. J Virol. 1999;73:3095–3101. doi: 10.1128/jvi.73.4.3095-3101.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen L-K, Lin Y-L, Liao C-L, Lin C-G, Huang Y-L, Yeh C-T, Lai S-C, Jan J-T, Chin C. Generation and characterization of organ-tropism mutants of Japanese encephalitis virus in vivo and in vitro. Virology. 1996;223:79–88. doi: 10.1006/viro.1996.0457. [DOI] [PubMed] [Google Scholar]
- 8.Coia G, Parker M D, Speight G, Byrne M E, Westaway E G. Nucleotide and complete amino acid sequences of Kunjin virus: definitive gene order and characteristics of the virus-specified proteins. J Gen Virol. 1988;69:1–21. doi: 10.1099/0022-1317-69-1-1. [DOI] [PubMed] [Google Scholar]
- 9.Dalgarno L, Trent D W, Strauss J H, Rice C M. Partial nucleotide sequence of the Murray Valley encephalitis virus genome. Comparison of the encoded polypeptides with yellow fever virus structural and non-structural proteins. J Mol Biol. 1986;187:309–323. doi: 10.1016/0022-2836(86)90435-3. [DOI] [PubMed] [Google Scholar]
- 10.Despres P, Frenkiel M-P, Deubel V. Differences between cell membrane fusion activities of two dengue type-1 isolates reflect modifications of viral structure. Virology. 1993;196:209–219. doi: 10.1006/viro.1993.1469. [DOI] [PubMed] [Google Scholar]
- 11.Eckels K H, Yong-Xin Y, Dubois D R, Marchette N J, Trent D W, Johnson A J. Japanese encephalitis virus live-attenuated vaccine, Chinese strain SA14-14-2: adaptation to primary canine kidney cell cultures and preparation of a vaccine for human use. Vaccine. 1988;6:513–518. doi: 10.1016/0264-410x(88)90103-x. [DOI] [PubMed] [Google Scholar]
- 12.Gualano R C, Pryor M J, Cauchi M R, Wright P J, Davidson A D. Identification of a major determinant of mouse neurovirulence of dengue virus type 2 using stably cloned genomic-length cDNA. J Gen Virol. 1998;79:437–446. doi: 10.1099/0022-1317-79-3-437. [DOI] [PubMed] [Google Scholar]
- 13.Guirakhoo F, Zhang Z-X, Chambers T J, Delagrave S, Arroyo J, Barrett A D T, Monath T P. Immunogenicity, genetic stability, and protective efficacy of a recombinant, chimeric yellow fever-Japanese encephalitis virus (ChimeriVax-JE) as a live, attenuated vaccine candidate against Japanese encephalitis. Virology. 1999;257:363–372. doi: 10.1006/viro.1999.9695. [DOI] [PubMed] [Google Scholar]
- 14.Hahn C S, Dalrymple J M, Strauss J H, Rice C M. Comparison of the virulent Asibi strain of yellow fever virus with the 17D vaccine strain derived from it. Proc Natl Acad Sci USA. 1987;84:2019–2023. doi: 10.1073/pnas.84.7.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hanna J N, Ritchie S A, Phillips D A, Shield J, Bailey M C, Mackenzie J S, Poidinger M, McCall B J, Mills P J. An outbreak of Japanese encephalitis in the Torres Strait, Australia, 1995. Med J Aust. 1996;165:256–260. doi: 10.5694/j.1326-5377.1996.tb124960.x. [DOI] [PubMed] [Google Scholar]
- 16.Hanna J N, Ritchie S A, Phillips D A, Lee J M, Hills S L, van den Hurk A F, Pyke A T, Johansen C A, Mackenzie J S. Japanese encephalitis in north Queensland, Australia, 1998. Med J Aust. 1999;170:533–536. doi: 10.5694/j.1326-5377.1999.tb127878.x. [DOI] [PubMed] [Google Scholar]
- 17.Hasegawa H, Yoshida M, Shiosaka T, Fujita S, Kobayashi Y. Mutations in the envelope protein of Japanese encephalitis virus affect entry into cultured cells and virulence in mice. Virology. 1992;191:158–165. doi: 10.1016/0042-6822(92)90177-q. [DOI] [PubMed] [Google Scholar]
- 18.Heinz F X. Epitope mapping of flavivirus glycoproteins. Adv Virus Res. 1986;31:103–168. doi: 10.1016/s0065-3527(08)60263-8. [DOI] [PubMed] [Google Scholar]
- 19.Hennessy S, Zhengle L, Tsai T F, Strom B L, Chao-Min W, Hui-Lian L, Tai-Xiang W, Hong-Ji Y, Qi-Mau L, Karabatsos N, Bilker W B, Halstead S B. Effectiveness of live-attenuated Japanese encephalitis vaccine (SA14–14-2): a case-control study. Lancet. 1996;347:1583–1586. doi: 10.1016/s0140-6736(96)91075-2. [DOI] [PubMed] [Google Scholar]
- 20.Holtzmann H, Stiasny K, Ecker M, Kunz C, Heinz F X. Characterization of monoclonal antibody-escape mutants of tick-borne encephalitis virus with reduced neuroinvasiveness. J Gen Virol. 1997;78:31–37. doi: 10.1099/0022-1317-78-1-31. [DOI] [PubMed] [Google Scholar]
- 21.Jennings A D, Whitby J E, Minor P D, Barrett A D T. Comparison of the nucleotide and deduced amino acid sequences of the envelope protein genes of the wild-type French viscerotropic strain of yellow fever virus and the live vaccine strain, French neurotropic vaccine, derived from it. Virology. 1993;192:692–695. doi: 10.1006/viro.1993.1090. [DOI] [PubMed] [Google Scholar]
- 22.Jennings A D, Gibson C A, Miller B R, Mathews J H, Mitchell C J, Roehrig J T, Wood D J, Taffs F, Sil B K, Whitby S N, Whitby J E, Monath T P, Minor P D, Sanders P G, Barrett A D T. Analysis of a yellow fever virus isolated from a fatal case of vaccine-associated human encephalitis. J Infect Dis. 1994;169:512–518. doi: 10.1093/infdis/169.3.512. [DOI] [PubMed] [Google Scholar]
- 23.Jiang W R, Lowe A, Higgs S, Reid H, Gould E A. Single amino acid codon changes detected in louping ill virus antibody-resistant mutants with reduced virulence. J Gen Virol. 1993;74:931–935. doi: 10.1099/0022-1317-74-5-931. [DOI] [PubMed] [Google Scholar]
- 24.Kinney R M, Butrapet S, Chang G-J J, Tsuchiya K R, Roehrig J T, Bhamarapravati N, Gubler D J. Construction of infectious cDNA clones for dengue 2 virus: strain 16681 and its attenuated vaccine derivative, strain PDK-53. Virology. 1997;230:300–308. doi: 10.1006/viro.1997.8500. [DOI] [PubMed] [Google Scholar]
- 25.Kolaskar A S, Kulkarni-Kale U. Prediction of three-dimensional structure and mapping of conformational epitopes of envelope glycoprotein of Japanese encephalitis virus. Virology. 1999;261:31–42. doi: 10.1006/viro.1999.9859. [DOI] [PubMed] [Google Scholar]
- 26.Konishi E, Yamaoka M, Khin-Sane-Win, Kurane I, Mason P W. Induction of protective immunity against Japanese encephalitis in mice by immunization with a plasmid encoding Japanese encephalitis virus premembrane and envelope genes. J Virol. 1998;72:4925–4930. doi: 10.1128/jvi.72.6.4925-4930.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mackenzie J S, Lindsay M D, Coelen R J, Broom A K, Hall R A, Smith D W. Arboviruses causing human disease in the Australasian zoogeographic region. Arch Virol. 1994;136:447–467. doi: 10.1007/BF01321074. [DOI] [PubMed] [Google Scholar]
- 28.McAda P C, Mason P W, Schmaljohn C S, Dalrymple J M, Mason T L, Fournier M J. Partial nucleotide sequence of the Japanese encephalitis virus genome. Virology. 1987;158:348–360. doi: 10.1016/0042-6822(87)90207-8. [DOI] [PubMed] [Google Scholar]
- 29.McMinn P C, Lee E, Hartley S, Roehrig J T, Dalgarno L, Weir R C. Murray Valley encephalitis virus envelope protein antigenic variants with altered hemagglutination properties and reduced neuroinvasiveness in mice. Virology. 1995;211:10–20. doi: 10.1006/viro.1995.1374. [DOI] [PubMed] [Google Scholar]
- 30.McMinn P C, Marshall I D, Dalgarno L. Neurovirulence and neuroinvasiveness of Murray Valley encephalitis virus mutants selected by passage in a monkey kidney cell line. J Gen Virol. 1995;76:865–872. doi: 10.1099/0022-1317-76-4-865. [DOI] [PubMed] [Google Scholar]
- 31.McMinn P C, Weir R C, Dalgarno L. A mouse-attenuated envelope protein variant of Murray Valley encephalitis virus with altered fusion activity. J Gen Virol. 1996;77:2085–2088. doi: 10.1099/0022-1317-77-9-2085. [DOI] [PubMed] [Google Scholar]
- 32.Monath T P, Cropp C B, Bowen G S, Kemp G E, Mitchell C J, Gardner J J. Variation in virulence for mice and rhesus monkeys among St. Louis encephalitis virus strains of different origin. Am J Trop Med Hyg. 1980;29:948–962. doi: 10.4269/ajtmh.1980.29.948. [DOI] [PubMed] [Google Scholar]
- 33.Monath T P, Heinz F X. Flaviviruses. In: Fields B N, Knipe D M, Howley P M, editors. Fields virology. 3rd ed. Philadelphia, Pa: Lippincott-Raven Publishers; 1996. pp. 961–1034. [Google Scholar]
- 34.Monath T P. Yellow fever. In: Plotkin S A, editor. Vaccines. 3rd ed. Philadelphia, Pa: W. B. Saunders; 1999. pp. 815–879. [Google Scholar]
- 35.Monath T P, Soike K, Levenbook I, Zhang Z-X, Arroyo J, Delagrave S, Myers G, Barrett A D T, Shope R E, Ratterree M, Chambers T J, Guirakhoo F. Recombinant, chimaeric live, attenuated vaccine (ChimeriVax) incorporating the envelope genes of Japanese encephalitis (SA14–14-2) virus and the capsid and nonstructural genes of yellow fever (17D) virus is safe, immunogenic and protective in non-human primates. Vaccine. 1999;17:1869–1882. doi: 10.1016/s0264-410x(98)00487-3. [DOI] [PubMed] [Google Scholar]
- 36.Monath T P, Levenbook I, Soike K, Zhang Z-X, Ratterree M, Draper K, Barrett A D T, Nichols R, Weltzin R, Arroyo J, Guirakhoo F. Chimeric yellow fever virus 17D-Japanese encephalitis virus vaccine: dose-response effectiveness and extended safety testing in rhesus monkeys. J Virol. 2000;74:1742–1751. doi: 10.1128/jvi.74.4.1742-1751.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ni H, Burns N J, Chang G-J J, Zhang M J, Wills M R, Trent D W, Sanders P G, Barrett A D T. Comparison of nucleotide and deduced amino acid sequence of the 5′ non-coding region and structural protein genes of the wild-type Japanese encephalitis virus strain SA 14 and its attenuated vaccine derivatives. J Gen Virol. 1994;75:1505–1510. doi: 10.1099/0022-1317-75-6-1505. [DOI] [PubMed] [Google Scholar]
- 38.Ni H, Chang G-J J, Xie H, Trent D W, Barrett A D T. Molecular basis of attenuation of neurovirulence of wild-type Japanese encephalitis virus strain SA14. J Gen Virol. 1995;76:409–413. doi: 10.1099/0022-1317-76-2-409. [DOI] [PubMed] [Google Scholar]
- 39.Ni H, Barrett A D T. Attenuation of Japanese encephalitis virus by selection of its mouse brain receptor preparation escape mutants. Virology. 1998;241:30–36. doi: 10.1006/viro.1997.8956. [DOI] [PubMed] [Google Scholar]
- 40.Nitayaphan S, Grant J A, Chang G-J J, Trent D W. Nucleotide sequence of the virulent SA-14 strain of Japanese encephalitis virus and its attenuated vaccine derivative, SA-14-14-2. Virology. 1990;177:541–552. doi: 10.1016/0042-6822(90)90519-w. [DOI] [PubMed] [Google Scholar]
- 41.Nothdurft H D, Jelinek T, Marschang A, Maiwald H, Kapaun A, Loscher T. Adverse reactions to Japanese encephalitis vaccine in travellers. J Infect. 1996;32:119–122. doi: 10.1016/s0163-4453(96)91281-5. [DOI] [PubMed] [Google Scholar]
- 42.Ohtaki E, Matsuishi T, Hirano Y, Maekawa K. Acute disseminated encephalomyelitis after treatment with Japanese B encephalitis vaccine (Nakayama-Yoken and Beijing strains) J Neurol Neurosurg Psychiatry. 1995;59:316–317. doi: 10.1136/jnnp.59.3.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Plesner A-M, Ronne T, Wachmann H. Case-control study of allergic reactions to Japanese encephalitis vaccine. Vaccine. 2000;18:1830–1836. doi: 10.1016/s0264-410x(99)00403-x. [DOI] [PubMed] [Google Scholar]
- 44.Rey F A, Heinz F X, Mandl C, Kunz C, Harrison S C. The envelope glycoprotein from tick-borne encephalitis virus at 2 A resolution. Nature. 1995;375:291–298. doi: 10.1038/375291a0. [DOI] [PubMed] [Google Scholar]
- 45.Rezapkin G V, Norwood L P, Taffs R E, Dragunsky E M, Levenbook I S, Chumakov K M. Microevolution of type 3 Sabin strain of poliovirus in cell cultures and its implications for oral poliovirus vaccine quality control. Virology. 1995;211:377–384. doi: 10.1006/viro.1995.1420. [DOI] [PubMed] [Google Scholar]
- 46.Rice C M, Grakoui A, Galler R, Chambers T J. Transcription of infectious yellow fever RNA from full-length cDNA templates produced by in vitro ligation. New Biol. 1989;1:285–296. [PubMed] [Google Scholar]
- 47.Roehrig J T, Hunt A R, Johnson A J, Hawkes R A. Synthetic peptides derived from the deduced amino acid sequence of the E-glycoprotein of Murray Valley encephalitis virus elicit antiviral antibody. Virology. 1989;171:49–60. doi: 10.1016/0042-6822(89)90509-6. [DOI] [PubMed] [Google Scholar]
- 48.Roehrig J T, Johnson A J, Hunt A R, Bolin R A, Chu M C. Antibodies to dengue 2 virus E-glycoprotein synthetic peptides identify antigenic conformation. Virology. 1990;177:668–675. doi: 10.1016/0042-6822(90)90532-v. [DOI] [PubMed] [Google Scholar]
- 49.Ryman K D, Ledger T N, Campbell G A, Watowich S J, Barrett A D T. Mutation in a 17D-204 vaccine substrain-specific envelope protein epitope alters the pathogenesis of yellow fever virus in mice. Virology. 1998;244:59–65. doi: 10.1006/viro.1998.9057. [DOI] [PubMed] [Google Scholar]
- 50.Savage H M, Ceianu C, Nicolescu G, Karabatsos N, Lanciotti R, Vladimirescu A, Laiv L, Ungureanu A, Romanca C, Tsai T F. Entomologic and avian investigations of an epidemic of West Nile fever in Romania 1996, with serological and molecular characterization of a virus isolate from mosquitoes. Am J Trop Med Hyg. 1999;61:600–611. doi: 10.4269/ajtmh.1999.61.600. [DOI] [PubMed] [Google Scholar]
- 51.Schlesinger J J, Chapman S, Nestorowicz A, Rice C M, Ginocchio T E, Chambers T J. Replication of yellow fever virus in the mouse central nervous system: comparison of neuroadapted and non-neuroadapted virus and partial sequence analysis of the neuroadapted strain. J Gen Virol. 1996;77:1277–1285. doi: 10.1099/0022-1317-77-6-1277. [DOI] [PubMed] [Google Scholar]
- 52.Stiasny K, Allison S L, Marchler-Bauer A, Kunz C, Heinz F X. Structural requirements for low-pH-induced rearrangements in the envelope glycoprotein of tick-borne encephalitis virus. J Virol. 1996;70:8142–8147. doi: 10.1128/jvi.70.11.8142-8147.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sumiyoshi H, Tignor G H, Shope R E. Characterization of a highly attenuated Japanese encephalitis virus generated from molecularly cloned cDNA. J Infect Dis. 1995;171:1144–1151. doi: 10.1093/infdis/171.5.1144. [DOI] [PubMed] [Google Scholar]
- 54.Taffs R E, Chumakov K M, Rezapkin G V, Lu Z, Douthitt Z M, Dragunsky E M, Levenbook I S. Genetic stability and mutant selection in Sabin 2 strain of oral poliovirus vaccine grown under different cell culture conditions. Virology. 1995;209:366–373. doi: 10.1006/viro.1995.1268. [DOI] [PubMed] [Google Scholar]
- 55.Thompson J D, Higgins D G, Gibson T J. CLUSTAL W: improving the sensitivity of progressive multiple sequence alignment through sequence weighting, position-specific gap penalties and weight matrix choice. Nucleic Acids Res. 1994;22:4673–4680. doi: 10.1093/nar/22.22.4673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Trent D W, Kinney R M, Johnson B J, Vorndam A V, Grant J A, Deubel V, Rice C M, Hahn C. Partial nucleotide sequence of St. Louis encephalitis virus RNA: structural proteins, NS1, ns2a, and ns2b. Virology. 1987;156:293–304. doi: 10.1016/0042-6822(87)90409-0. [DOI] [PubMed] [Google Scholar]
- 57.Tsai T F, Yu Y X. Japanese encephalitis vaccines. In: Plotkin S A, Mortimer E A, editors. Vaccines. 2nd ed. Philadelphia, Pa: W. B. Saunders and Company; 1994. pp. 671–713. [Google Scholar]