Abstract
Background
The lithotomy position (LP) may pose limitations and discomfort for elderly patients and those with a history of lower limb surgery, potentially leading to an increased risk of complications. And the LP is the conventional position during flexible ureteroscopic lithotomy for the treatment of ureteral calculi. However, it has some disadvantages, such as peripheral nerve injury and deep venous thrombosis in the lower limbs, etc. Therefore, we performed a new approach, which is named as modified dorsal recumbent position (MDRP). Currently, there is a lack of systematic analysis and standardization regarding the surgical positioning for flexible ureteroscopic lithotripsy. The objective of the study was to assess whether there were any disparities in the overall duration of the procedure when comparing the MDRP with the LP. The investigation of the optimal position for flexible ureteroscopic lithotomy is essential for enhancing patient safety and comfort.
Methods
This is a prospective, multicenter, randomized clinical trial. A total of 144 patients with renal or ureteral calculi from April 2021 to June 2022 were enrolled. Eligible patients were randomized to the MDRP group (n=72) or LP group (n=72). The patient’s demographics, the placement of the surgical position (time of position placement, time of disinfection and towel laying, time of position return, degree of medical fatigue) and the operation safety (time of operation, time of ureteroscope from bladder neck to ureteral orifice, heart rate, blood pressure) of two groups were compared and analyzed.
Results
Between the two groups, the body positioning time (93.8±31.6 vs. 134.8±40.1 s, P=0.02), operation time (71.8±36.7 vs. 77.7±48.6 min, P=0.04), the time from the bladder neck to the ureteral orifice of the flexible ureteroscope spent by the doctors (3.4±4.7 vs. 10.3±14.7 s, P<0.001) and incidence rate of patient’s lower limb soreness (19.4% vs. 49.7%, P=0.01) in the MDRP group were significantly shorter than those in the LP group. However, there was no significant difference in the stone removal rate (87.6% vs. 85.4%, P=0.09) or postoperative hospitalization days (4.3±1.4 vs. 4.1±1.6 d, P=0.08) between the two groups.
Conclusions
This trial showed that the MDRP could not only effectively shorten the operation time, shorten the time from the bladder neck to the ureteral orifice of the ureteroscopic lithotripsy, but also place the patient’s body in a functional position, stabilize the blood pressure during the operation, improve the comfort of the patient.
Trial Registration
Chinese Clinical Trial Registry (No. ChiCTR2100053416).
Keywords: Modified dorsal recumbent position (MDRP), lithotomy position (LP), flexible ureteroscopic lithotomy
Highlight box.
Key findings
• This trial showed that the modified dorsal recumbent position (MDRP) could effectively shorten the operation time.
What is known and what is new?
• The MDRP has the potential to position the patient’s body in a functional posture.
• This trial showed that the MDRP could shorten the time from the bladder neck to the ureteral orifice of the ureteroscopic lithotripsy.
What is the implication, and what should change now?
• This trial showed that the MDRP could stabilize the blood pressure during the operation, and improve the comfort of the patient.
• Further expanded clinical trials are needed to confirm.
Introduction
The prevalence of patients with urinary stones is increasing. It is reported that about 5–15% of the world’s population is troubled by urinary stones every year (1), and kidney stones account for about 5–15% of patients with urinary stones (2). With the development of lithotripsy technology, equipment and tools (3), ureteroscopic holmium laser lithotripsy has been widely used, which has greatly improved the efficiency of transurethral lithotripsy (4).
The optimal position of the patients during flexible ureteroscopic lithotomy is important. The position needs to be confirmed by doctors and nurses and to be adjusted reasonably according to the requirements of the Operating Room Nursing Practice Guide. The surgical field could be effectively exposed through reasonable surgical posture, which is conducive to the operation of doctors, to save the operation time, reduce the time of patients under anesthesia, and also reduce the possibility of unnecessary iatrogenic injury to patients (5). Nowadays, the main surgical position used in urological surgery is the traditional lithotomy position (LP) (6). Some studies have pointed out that the exposure of the surgical field of the LP can improve the safety and effectiveness of the operation. However, abuse of this position could cause peripheral nerve injury of the patient. About 1.5% to 1.9% of the patients suffered from femoral nerve, obturator nerve, sciatic nerve, common peroneal nerve injury due to the implement of the LP, and it will result in permanent motor disorders (7). At the same time, prolonged lithotomy will increase the possibility of deep venous thrombosis in the lower limbs of patients (8).
Moreover, the traditional LP also increases the physiological curvature of the patient’s ureter, making it more complicated for the operator to see the complete ureteral lumen in the surgical field of vision, affecting the time of lens entry, and thus influence the overall efficiency of the operation (9,10). Therefore, doctors adopt different surgical positions according to their own habits and preferences: the waist of the affected side is raised 45° supine position, oblique supine position-LP, new lateral position, etc., but up to now, there is no systematic analysis and standard for the surgical positions of the ureteral soft lithotripsy. We present this article in accordance with the CONSORT reporting checklist (available at https://tau.amegroups.com/article/view/10.21037/tau-24-3/rc).
Methods
Study design
This study is a prospective, multicenter, parallel, openable, randomized clinical trial conducted from April 2021 to June 2022. in Zhongshan Hospital of Fudan University, Zhongshan Hospital Xiamen Branch, Central Hospital of Xuhui District and Central Hospital of Minhang District, which are all high-volume institutions in China. The primary outcome was the comparison of the operation time between two groups. The secondary end points included position time, time from the bladder neck to the ureteral, the angle between two legs, D-dimer on PDO2 and POD14 and incidence of numberless and acid swelling. Patients were screened preoperatively, and those who met the inclusion criteria for the clinical trial underwent one of the surgical positions. The patients voluntarily participated in the clinical trial and provided signed informed consent. On the day of surgery, a random lottery sealed envelope method was employed to determine each patient’s assigned surgical position. This study was approved by the Ethics Committee of Zhongshan Hospital, Fudan University (No. B2021-146R), and all participating institutions were informed and agreed the study. Informed consent was taken from all the patients. The trial was registered at Chinese Clinical Trial Registry (No. ChiCTR2100053416). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Eligibility
The inclusion criteria were: (I) preoperative diagnosis of nephroureteral calculi was in line with the indications of holmium laser lithotripsy via ureteroscope; (II) the study was reviewed and approved by the Ethics Committee; (III) informed consent was signed by the patient. The exclusion criteria were: (I) severe heart, brain or large blood vessel diseases; (II) severe ureteral stenosis; (III) lower limb movement limitation or bone joint and peripheral vascular disease; (V) have cognitive and emotional disorders.
Randomization and treatment
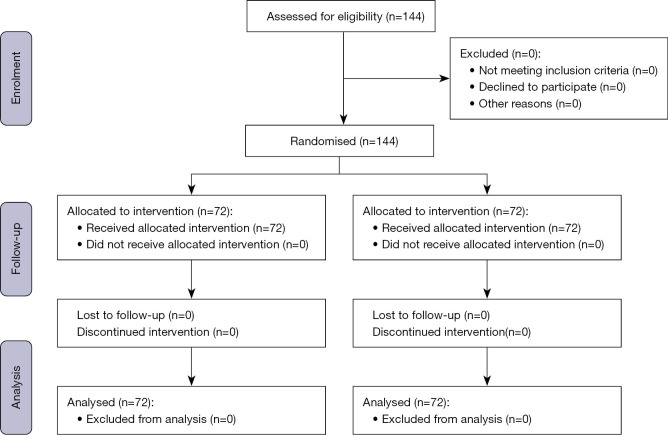
Patients were randomly assigned in a 1:1 allocation ratio to enter the modified dorsal recumbent position (MDRP group) or the LP group. Flow diagram of the progress through the phases of a parallel randomised trial of two groups (see Figure 1).
Figure 1.
Flow diagram of the progress through the phases of a parallel randomised trial of two groups.
The MDRP group used the new herringbone lying position (see Figure 2) on a common operating table, with the patient lay flat. After general anesthesia, the patient was moved towards the foot of the operation table to make their buttocks at the junction of the leg plates on the foot of the table, and the two leg plates open about 80 degrees. If the patient’s limbs are stiff, you can choose to open the healthy side slightly. According to the 2017 version of the Operating Room Nursing Practice Guide, for patients with a history of hip surgery, the legs cannot be opened more than 60 degrees apart, and the affected side is placed under the affected limb with a posture pad. Keep the affected limb in functional position. Stay comfortable. Then the left and right leg pads are exchanged to make the surgeon have adequate standing space for easy operation. Open the patient’s leg fork on the leg board, cushion an adjustable popliteal pad that we designed for improved herringbone recumbent position under the popliteal fossa (see Figure 3), fix it with a special restraint belt, bend the hip 15–30 degrees, make the limb in the functional position, and take warm measures to increase comfort. The placement of this position requires the collaboration of 1 worker, 1 nurse and 1 doctor.
Figure 2.
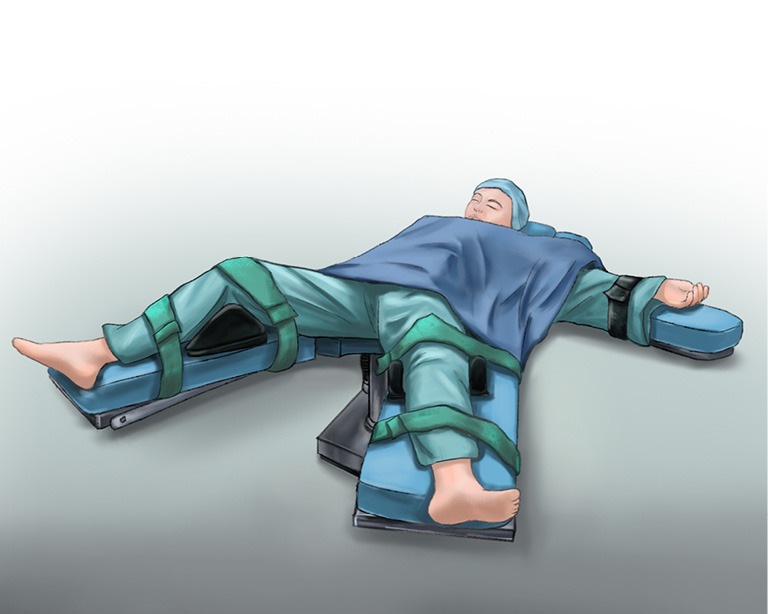
Modified dorsal recumbent position (MDRP). The patient was moved towards the foot of the operation table to make their buttocks at the junction of the leg plates on the foot of the table, and the two leg plates open about 80 degrees. The left and right leg pads are exchanged to make the surgeon have adequate standing space for easy operation.
Figure 3.
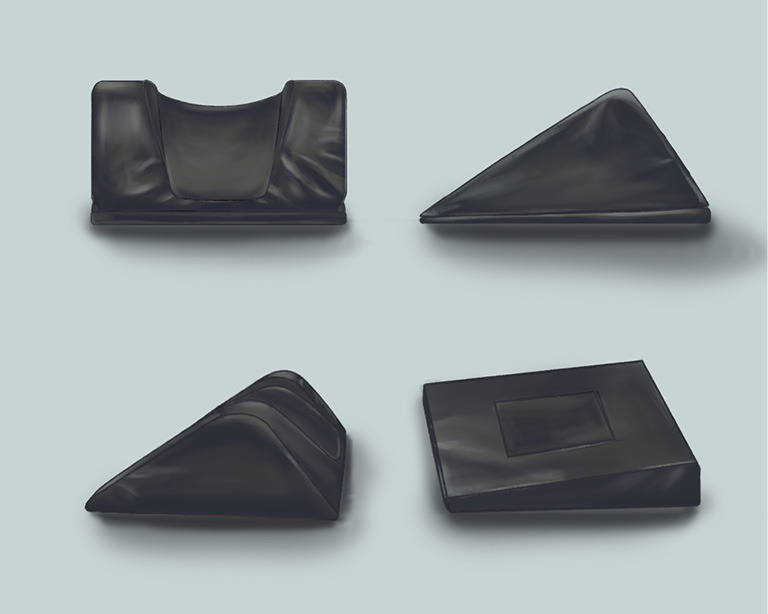
Design for improved herringbone recumbent position. Open the patient’s leg fork on the leg board, cushion an adjustable popliteal pad that designed for improved herringbone recumbent position under the popliteal fossa.
The LP group used the traditional double-leg LP (see Figure 4), use the conventional operating table and leg rest, and the patient lay on his back. After general anesthesia, the patient was moved towards the foot of the table to make and the buttocks on the junction of the table back plate and leg plate, place the LP leg rest on the plane near the hip joint, and place the two legs on the LP leg rest on both sides to expose the perineum to the maximum extent; If the arms are abducted, fix the upper limb with a fixed belt. Keep the patients warm, remove the leg plate, the lower limb abduction is less than 90 degrees, and the angle of thigh flexion can be adjusted according to the surgical needs; If the head is low and the foot is high, shoulder support can be used and fixed to prevent the patient from sliding towards the head end; The leg frame supports the lower leg and knee, and the popliteal fossa is padded with an integrated pad if necessary to prevent damage to blood vessels and nerves. This position arrangement requires the joint collaboration of 2 workers, 1 nurse and 1 doctor.
Figure 4.
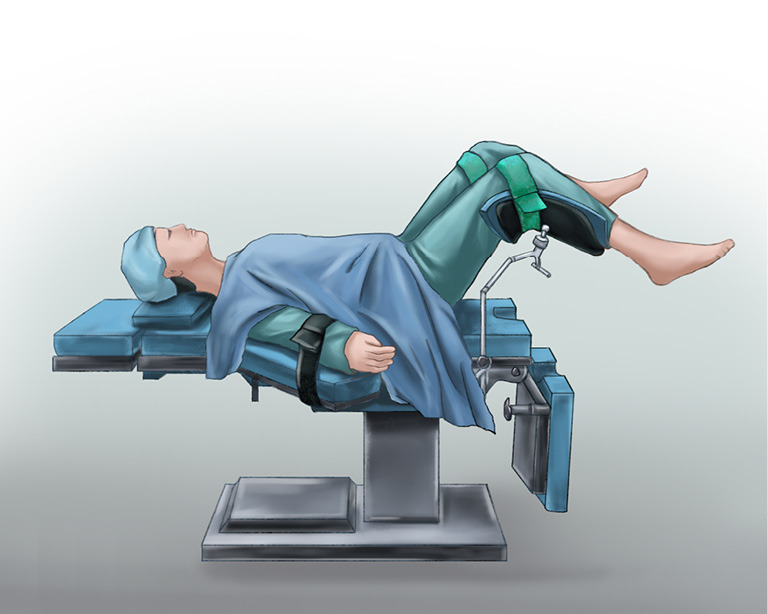
Lithotomy position (LP). The patient was moved towards the foot of the table to make the buttocks on the junction of the table back plate and leg plate, place the lithotomy position leg rest on the plane near the hip joint, and place the two legs on the lithotomy position leg rest on both sides to expose the perineum to the maximum extent; If the arms are abducted, fix the upper limb with a fixed belt. Remove the leg plate, the lower limb abduction is less than 90 degrees.
Statistical analysis
The intention-to-treat principle was adhered to for all randomized patients during data analysis. Statistical analysis was conducted using IBM Corp’s SPSS software, version 22.0 (Armonk, NY, USA). Comparisons between the two groups were performed utilizing the χ2 test and Fisher exact test for categorical parameters, while continuous variables were assessed using the t-test or analysis of variance. A significance level of P<0.05 (two-sided) was considered statistically significant.
Results
Patients
A total of 144 patients were enrolled and randomly allocated to the MDRP group (n=72) or the LP group (n=72). The baseline clinical characteristics of the patients enrolled were well balanced (Table 1).
Table 1. Patient’s demographics of the two groups.
| Outcomes | MDRP group (n=72) | LP group (n=72) | P |
|---|---|---|---|
| Sex | 0.60 | ||
| Male | 50 (69.4) | 46 (63.9) | |
| Female | 22 (30.6) | 26 (36.1) | |
| Age (years) | 52.6±12.3 | 53.2±11.6 | 0.51 |
| BMI (kg/m2) | 24.7±2.8 | 25.1±3.1 | 0.48 |
| Hypertension | 25 (34.7) | 12 (16.7) | 0.21 |
| Diabetes mellitus | 15 (20.8) | 6 (8.3) | 0.057 |
| Coronary disease | 6 (8.3) | 3 (4.2) | 0.49 |
| DVT | 1 (1.4) | 0 (0.0) | 0.50 |
Data are presented as n (%) or mean ± standard deviation. MDRP group: the modified dorsal recumbent position group; LP group: the lithotomy position group. BMI, body mass index; DVT, deep venous thrombosis.
Intraoperative outcome
The time needed to position patient in the MDRP group was much less than LP group (93.8±31.6 vs. 134.8±40.1 s, P=0.02). Meanwhile, the time needed for the procedure from bladder neck to enter ureteral orifice was much less in the MDRP group than LP group (3.4±4.7 vs. 10.3±14.7 s, P<0.001). And the total operation duration was much less than in the MDRP group than LP group (71.8±36.7 vs. 77.7±48.6 s, P=0.04) (Table 2).
Table 2. Comparison of the intraoperative outcome.
| Outcomes | MDRP group (n=72) | LP group (n=72) | P |
|---|---|---|---|
| Time needed to positioning patient (second) | 93.8±31.6 | 134.8±40.1 | 0.02 |
| Time needed for the procedure from bladder neck to enter ureteral orifice (second) | 3.4±4.7 | 10.3±14.7 | <0.001 |
| Total operation duration (minute) | 71.8±36.7 | 77.7±48.6 | 0.04 |
Data are presented as mean ± standard deviation. MDRP group: the modified dorsal recumbent position group; LP group: the lithotomy position group.
Postoperative outcome
The incidence rate of lower limb soreness in the MDRP group was much less than LP group (19.4% vs. 49.7%, P=0.01). However, there was no significant difference in the stone removal rate (87.6% vs. 85.4%, P=0.09) or postoperative hospitalization days (4.3±1.4 vs. 4.1±1.6 d, P=0.08) between the two groups (Table 3). The absence of significant adverse effects or unintended consequences was observed in both groups.
Table 3. Comparison of postoperative outcome.
| Outcomes | MDRP group (n=72) | LP group (n=72) | P |
|---|---|---|---|
| Incidence rate of patient’s lower limb soreness (%) | 19.4 | 49.7 | 0.01 |
| Postoperative hospitalization days, mean ± standard deviation | 4.3±1.4 | 4.1±1.6 | 0.08 |
| Stone removal rate (%) | 87.6 | 85.4 | 0.09 |
MDRP group: the modified dorsal recumbent position group; LP group: the lithotomy position group.
Discussion
This trial is, to our knowledge, the first available well designed multicenter randomized clinical trial to directly compare the safety and efficacy of MDRP vs. LP for flexible ureteroscopic lithotomy. The result showed that MDRP had some advantages over LP.
Relevant research on improving the safety and comfort of ureteroscopic lithotripsy shows that posture nursing for patients can optimize the operation effect, shorten the operation time, improve the comfort of patients, and reduce postoperative pain, thus improving the treatment effect (11). Improved herringbone recumbent position has a relatively small impact on hemodynamics compared with the double leg LP and is more comfortable when the patient is conscious (12). For pregnant women, the new herringbone recumbent position is more comfortable than the LP, and the operation is safer and more convenient (13). Additionally, the traditional LP has certain compression on the blood vessels and nerves of the lower extremities, which is easy to cause venous thrombosis of the lower extremities, nerve injury, surgical pressure sores, etc. (14); the new herringbone recumbent position is also suitable for patients with femoral neck fracture, intertrochanteric fracture and subtrochanteric fracture after internal fixation, which can fully consider the comfort of patients and reduce joint and nerve injury on the premise of ensuring operation.
To improve the satisfaction of medical staff and workers, the new herringbone recumbent position does not need to raise the legs when placing the body position. The included angle between the two legs is less than 80°. It is in a natural separation state, which does not affect the standing position of the operator and is convenient for the first assistant. At the same time, the new herringbone recumbent position only needs one person to complete the placement of the body position without special outrigger body positioning device, which greatly saves time, effectively reduces the body position preparation process and workload (15), improves the working efficiency of the itinerant nurses and workers, and thus improves the satisfaction of the medical workers.
The application of the new herringbone posture in the flexible ureteroscopic lithotripsy can not only effectively improve the safety of the flexible ureteroscopic lithotripsy, optimize the operation effect, effectively shorten the operation time, shorten the time from the bladder neck to the ureteral orifice of the flexible ureteroscopic lithotripsy, make the patient’s body in the functional position, the operation center rate and blood pressure fluctuation more stable, but also improve the patient’s comfort, and improve the satisfaction of medical staff. It has significance for promoting in clinical practice.
Conclusions
This trial showed that the MDRP could not only effectively shorten the operation time, shorten the time from the bladder neck to the ureteral orifice of the ureteroscopic lithotripsy, but also place the patient’s body in a functional position, stabilize the blood pressure during the operation, improve the comfort of the patient.
Supplementary
The article’s supplementary files as
Acknowledgments
Funding: This study was supported by the Special Fund for Clinical Research of Zhongshan Hospital (No. ZSLCYJ202067), and the Fund of Doctor’s Innovation and Transformation Ability Training Program (No. SHDC2022CRS036).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the Ethics Committee of Zhongshan Hospital, Fudan University (No. B2021-146R), and all participating institutions were informed and agreed the study. Informed consent was taken from all the patients. The trial was registered at Chinese Clinical Trial Registry (No. ChiCTR2100053416). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Footnotes
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at https://tau.amegroups.com/article/view/10.21037/tau-24-3/rc
Trial Protocol: Available at https://tau.amegroups.com/article/view/10.21037/tau-24-3/tp
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-24-3/coif). The authors have no conflicts of interest to declare.
Data Sharing Statement
Available at https://tau.amegroups.com/article/view/10.21037/tau-24-3/dss
References
- 1.Sharma R, Choudhary A, Das RK, et al. Can a brief period of double J stenting improve the outcome of extracorporeal shock wave lithotripsy for renal calculi sized 1 to 2 cm? Investig Clin Urol 2017;58:103-8. 10.4111/icu.2017.58.2.103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Duan K, Liu Q, Wang Y, et al. Curative effect analysis of 115 cases of lower caliceal calculi treated by double-J tube pre-dilation ureteroscope. Southwest National Defense Medicine 2015;25:389-91. [Google Scholar]
- 3.Liu G, Xiao X, Yang K, et al. Observation on the curative effect of ureteroscopic lithotripsy for 45 cases of kidney stones larger than 2 cm. Chongqing Medical Journal 2019;48:2318-22. [Google Scholar]
- 4.Peng L, Wen J, Zhong W. The application of Moses technique in urinary stone lithotripsy [J/CD]. Chinese Journal of Endoscopic Urology (electronic edition) 2018;12:361-3. [Google Scholar]
- 5.Tang Y, Feng X, Sun Y. Investigation on the knowledge, attitude, and behavior of the operating room nurses on the placement of surgical positions. Nursing Research 2013;27:3123-6. [Google Scholar]
- 6.Tao Y, Wang Q, Cao J. Application of the new Trendelenberg position in transureteroscopic holmium laser lithotripsy. Integrated Chinese and Western Medicine Nursing (Chinese and English) 2018;4:115-7. [Google Scholar]
- 7.Deveneau NE, Forbis C, Lipetskaia L, et al. The Effect of Lithotomy Position on Nerve Stretch: A Cadaveric Study. Female Pelvic Med Reconstr Surg 2017;23:457-61. 10.1097/SPV.0000000000000421 [DOI] [PubMed] [Google Scholar]
- 8.Gelder C, McCallum AL, Macfarlane AJR, et al. A systematic review of mechanical thromboprophylaxis in the lithotomy position. Surgeon 2018;16:365-71. 10.1016/j.surge.2018.03.005 [DOI] [PubMed] [Google Scholar]
- 9.Kaplan AG, Lipkin ME, Scales CD, Jr, et al. Use of ureteral access sheaths in ureteroscopy. Nat Rev Urol 2016;13:135-40. 10.1038/nrurol.2015.271 [DOI] [PubMed] [Google Scholar]
- 10.Cho SY. Current status of flexible ureteroscopy in urology. Korean J Urol 2015;56:680-8. 10.4111/kju.2015.56.10.680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lv W. Observe the value of posture nursing in patients with complicated ureteral calculi. Continuing Medical Education 2021;35:114-5. [Google Scholar]
- 12.You X, Zhou W, Wang J, et al. Comparative study of herringbone and lithotomy positions in patients undergoing gynecological endoscopic surgery. Journal of Nursing 2013;28:55-7. [Google Scholar]
- 13.Geavlete P, Multescu R, Geavlete B. Pushing the boundaries of ureteroscopy: current status and future perspectives. Nat Rev Urol 2014;11:373-82. 10.1038/nrurol.2014.118 [DOI] [PubMed] [Google Scholar]
- 14.Fan L. Nursing progress in prevention of complications of lithotomy during operation. Contemporary Nurses 2015;(02):13-6. [Google Scholar]
- 15.Chen L, Ma D, Nie H, et al. A clinical study on flexible ureteroscopy combined with percutaneous nephrolithotomy in treatment of complex renal stones. Journal of Minimally Invasive Urology 2017;6:340-2. [Google Scholar]