Abstract
Early-stage (stage 1–3) chronic kidney disease (CKD) has an asymptomatic presentation such that most people with CKD are unaware of their disease status and remain undiagnosed. CKD is associated with multiple long-term conditions (MLTC), or multimorbidity, the most common of these being cardiovascular disease, hypertension, and type 2 diabetes. Primary care practitioners (PCPs) are crucial in the early identification and management of patients with CKD. For individuals at high risk of CKD, measurements of estimated glomerular filtration rate, urine albumin–creatinine ratio, and blood pressure should be obtained regularly and recorded in a timely manner. The importance of lifestyle changes in the prevention and management of CKD should also be highlighted. A recent addition to the treatment of CKD in people with and without type 2 diabetes has been the recommendation by clinical practice guidelines of a sodium–glucose co-transporter 2 (SGLT2) inhibitor alongside a renin–angiotensin–aldosterone system inhibitor as foundational therapy. SGLT2 inhibitors prevent CKD progression and reduce fatal and non-fatal kidney and cardiovascular events, hospitalization for heart failure, and all-cause mortality, and they have a favorable safety and tolerability profile. However, uptake has been slow, particularly in people with CKD without type 2 diabetes. A multifaceted approach is required to ensure that people with CKD receive optimal kidney protection. Measures to raise awareness of the importance of early identification and intervention include local/national campaigns via social media and practice-based education; clinical education programs; integration of clinical decision support tools into electronic health records; detection programs built around electronic health records; and good interdisciplinary communication. PCPs at the forefront of multidisciplinary care are best placed to implement the evidence-based clinical practice CKD guidelines for lifestyle modification and guideline-directed medical therapy.
Keywords: Sodium–glucose co-transporter 2 inhibitors, Chronic kidney disease, Primary care practitioners
Plain Language Summary
Chronic kidney disease, or CKD, affects about one in ten adults worldwide. Results from many real-world studies show that early identification and treatment of CKD is crucial to prevent the disease from getting worse. However, because CKD can have no symptoms in its early stages, it is often not diagnosed. Many people with CKD are therefore unaware that they have it. People with CKD are likely to have other long-term health issues as well, including cardiovascular disease, hypertension and diabetes. Primary care practitioners are best placed to offer holistic, patient-centered care to those with CKD, and are the frontline in identifying and managing the risk factors for chronic disease. Primary care practitioners may advise people with CKD on lifestyle changes, such as diet and exercise, as well as helping them understand what treatments are available. Sodium–glucose co-transporter 2 inhibitors have shown strong kidney-protective effects in clinical trials, and recently updated clinical guidelines recommend their use as foundational therapy alongside more established treatments of CKD. These treatments should be prescribed to people with CKD whether they have diabetes or not. For people at high risk of CKD, primary care practitioners should regularly obtain and record measurements of kidney function and blood pressure. Public and primary care practitioner awareness and education, the use of clinical decision support tools, and good communication between healthcare professionals are all important to drive change in primary care and improve the early identification and management of CKD.
Key Summary Points
| The early identification and optimal management of people with chronic kidney disease (CKD) require urgent action. |
| Primary care practitioners are crucial in the identification and management of CKD and are best placed to implement evidence-based clinical practice guidelines for lifestyle modification and guideline-directed medical therapy. |
| Clinical practice guidelines recommend the use of a sodium–glucose co-transporter 2 inhibitor alongside a renin–angiotensin–aldosterone system inhibitor as foundational therapy to treat CKD in patients with and without type 2 diabetes. |
| Sodium–glucose co-transporter 2 inhibitors prevent CKD progression and reduce fatal and non-fatal kidney and cardiovascular events, hospitalization for heart failure, and all-cause mortality. |
| Public and primary care practitioner awareness and education, the adoption of clinical decision support tools, and good interdisciplinary communication are all important to drive change in primary care and improve the early identification and management of CKD. |
Introduction
Chronic kidney disease (CKD) is a global epidemic, present in approximately one in 10 adults worldwide [1]. Early-stage (stages 1–3) CKD has an asymptomatic presentation such that the majority of patients are unaware of their disease status and remain undiagnosed [2, 3]. In a multinational, observational study that utilized electronic medical records and/or insurance claims, the proportion of patients with estimated glomerular filtration rates (eGFR) indicative of stage 3 CKD that lacked a diagnosis code was alarmingly high (61.6–95.5% across countries) [4]. Further, high proportions of people with risk factors for CKD, such as cardiovascular disease (53.0–94.4%), hypertension (59.1–94.6%), and type 2 diabetes (T2D; 50.2–93.7%), remained undiagnosed [4]. Prevalence of urine albumin-to-creatinine ratio (UACR) testing is low, especially in people without T2D [5, 6].
CKD may be defined as abnormalities of kidney structure or function present for longer than 3 months, and, importantly, is a progressive disease [7]. In a retrospective, observational study of people with stage 3 CKD, delayed diagnosis was associated with increased risk of progression to stage 4/5, kidney failure, and the composite endpoint of myocardial infarction, stroke, and hospitalization for heart failure [8]. Slowing progression by identifying and optimally managing CKD at its early stages prevents complications and is cost-effective [7].
CKD is associated with worse morbidity and mortality (Fig. 1) [9–11]. People with CKD often have cardiovascular diseases such as heart failure and often die from cardiovascular causes before development of kidney failure [12]. The pathophysiology is bidirectional between heart failure and CKD [13]. Hypertension and T2D are also often comorbid with CKD [14]. A non-interventional survey conducted in the USA (the PaCE [Patient, Carer, and Economic burden] CKD study) has reported on adverse health-related quality of life, work productivity, and financial burden for people with CKD and their unpaid caregivers compared with the general population [15, 16]. An analysis of digital healthcare systems data (the CaReMe [CArdioRenal and Metabolic] study) found that hospital healthcare costs associated with CKD were high and that care for CKD and heart failure drove much of these costs [1]. Further, in a multinational, non-interventional, prospective cohort study, people with advanced-stage CKD (stages 4–5, including dialysis) reported a higher symptom severity, worse health-related quality of life, and greater work and activity impairment than people with early-stage CKD (stages 2–3) [17]. Disappointingly, a US cross-sectional study of visits to practices for people with CKD showed that the quality of kidney disease-related care had not improved over time (during 2006–2008 and 2012–2014: uncontrolled hypertension 46% and 48%, respectively; renin–angiotensin–aldosterone system [RAAS] inhibitor use 45% and 36%, respectively) [18]. Given the projected rise of risk factors for CKD, the prevalence and associated burdens of CKD will likely increase [19].
Fig. 1.
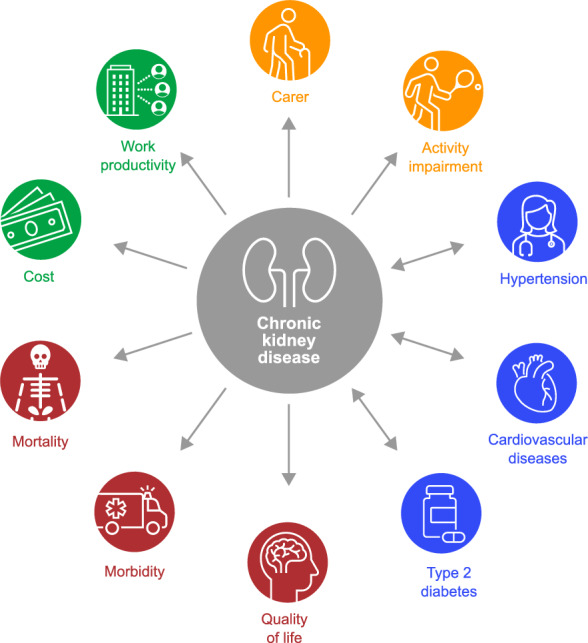
The burden of chronic kidney disease
Globally, CKD carries a significant economic burden, which increases substantially with increasing disease severity. A recent study from the Inside CKD research program found that, in each country/region, annual direct costs associated with CKD management rose by an average factor of 4 with progression from stage 3a to 5 [20]. The rise in mean annual costs per patient was even greater when comparing patients with early-stage CKD undergoing dialysis (stage 3a, mean $3060) with those receiving hemodialysis ($57,334) or peritoneal dialysis ($49,490), and estimates for annual costs of transplantation were also substantially higher (incident, $75,326; subsequent, $16,672) [20]. CKD-associated complications were also associated with significant economic burden: mean annual per patient costs were $18,294 for myocardial infarction, $8463 for heart failure, $10,168 for stroke, and $5975 for acute kidney injury [20]. Although costing definitions in this study varied widely in granularity and/or definition, the overall economic burden of CKD and its complications is undeniable.
Despite the high burden and impact of CKD, the World Health Organization roadmap on non-communicable diseases does not highlight nor address CKD as a priority [21]. A 2023 report by the International Society of Nephrology found that only 35% of countries with non-communicable-disease strategies targeted non-dialysis CKD, and only 25% of countries had national CKD-specific strategies [22]. The International Society of Nephrology, American Society of Nephrology, European Renal Association, and nephrology communities worldwide have recently published an international consensus calling for CKD to be placed on the global public health agenda [23].
CKD is associated with multiple long-term conditions (MLTC), or multimorbidity, the most common comorbidities being cardiovascular disease, hypertension, and T2D [14, 24]. Primary care practitioners (PCPs) are crucial in the early identification and management of patients with CKD. However, there are challenges that may be faced by PCPs, including maintaining awareness of updates to guideline-directed management, fragmented CKD care, the latest information on efficacy and potential safety concerns of novel treatments, lack of engagement of people at risk, people having MLTCs, and treatment affordability and access [25–27]. In addition, management of CKD may be sub-optimal owing to healthcare system factors such as inflexible electronic medical records that are not user friendly and limited time and resources [26].
Here we highlight recent updates to evidence-based clinical practice guidelines and set out recommendations to drive change in primary care and meet the need of early identification and optimal treatment and management of people with CKD. This article is based on previously published research and does not contain any new studies with human participants or animals performed by any of the authors.
Clinical Guidelines for the Management of CKD
PCPs are best placed to offer holistic, patient-centered care to those with CKD. They form long-standing relationships with their patients, see them more frequently than specialists do, and are the frontline in identifying and managing the risk factors for chronic disease. This is supported by the Kidney Disease: Improving Global Outcomes (KDIGO) 2024 clinical practice guideline for the evaluation and management of CKD [7]. This guideline also state that prevention and screening for CKD should be performed by PCPs and specialties such as endocrinology and cardiology, rather than by nephrologists [7].
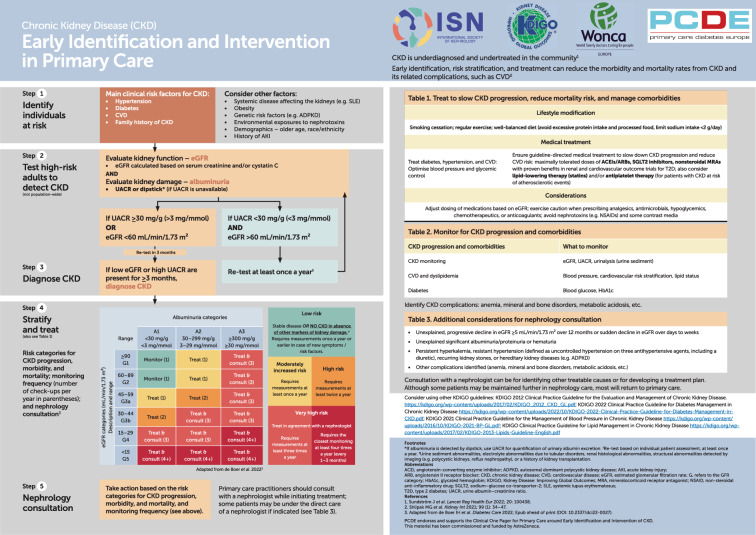
Early identification and management of CKD among those at high risk for CKD is paramount (Fig. 2). Both eGFR and UACR should be measured at each check-up or at least annually (eGFR calculation now excludes race in the USA [28]). Early diagnosis of CKD leads to improvements in CKD management and monitoring practices and attenuated eGFR decline [8]. Indeed, extrapolation of data from a post hoc analysis of the DAPA-CKD study suggests that treatment initiation (versus no initiation) when a patient has an eGFR of 75 mL/min/1.73 m2 could delay kidney failure by about 15.3 years, when eGFR is 60 mL/min/1.73 m2 by about 11.4 years, and when eGFR is 45 mL/min/1.73 m2 by about 7.5 years (Fig. 3) [29, 30]. Furthermore, screening for CKD has been shown to be cost-effective in people with diabetes and hypertension [31], and recent research has shown that population-wide screening for CKD alongside evidence-based treatment with sodium–glucose co-transporter 2 (SGLT2) inhibitors could be cost-effective in the USA [32].
Fig. 2.
Aid to the early identification and optimal management of patients with CKD. Taken from the Chronic Kidney Disease (CKD) Early Identification and Intervention in Primary Care document—find the full document in the ISN-KDIGO CKD Early Identification & Intervention toolkit. Available at: https://www.theisn.org/initiatives/toolkits/ckd-early-screening-intervention/). Note that this aid was published before the 2024 updates to the Kidney Disease: Improving Global Outcomes (KDIGO) guidelines were published.
Reproduced with permission
Fig. 3.
Compared with non-initiation, initiation of SGLT2 inhibitors at eGFR 75 mL/min/1.73 m2 could delay kidney failure (eGFR ≤ 10 mL/min/1.73 m2) by 15 years, while initiation at 45 mL/min/1.73 m2 could delay kidney failure by 7.5 years. Adapted from Madero, M. et al. SGLT2 Inhibitor Use in Chronic Kidney Disease: Supporting Cardiovascular, Kidney, and Metabolic Health. Kidney Medicine 2024;6(8):100851 [29], under the terms of the Creative Commons CC-BY license. Initial eGFR decline over first 2 weeks estimated using eGFR slope data from DAPA-CKD acute phase (2-week eGFR change: dapagliflozin 10 mg, −3.70 mL/min/1.73 m2; placebo, −1.00 mL/min/1.73 m2). Projections are based on eGFR from week 2 to end of treatment (DAPA-CKD chronic phase) and assume linear progression of eGFR decline [30]. Example patients with initial eGFR of 45, 60, and 75 mL/min/1.73 m2 used chronic eGFR slope for DAPA-CKD subgroup with eGFR ≥ 45 mL/min/1.73 m2. eGFR at start of chronic phase for patient with initial eGFR 45 mL/min/1.73 m2: dapagliflozin 10 mg, 41.3 mL/min/1.73 m2; placebo, 44.0 mL/min/1.73 m2; eGFR at start of chronic phase for patient with initial eGFR 60 mL/min/1.73 m2: dapagliflozin 10 mg, 56.3 mL/min/1.73 m2; placebo, 59.0 mL/min/1.73 m2; eGFR at start of chronic phase for patient with initial eGFR 75 mL/min/1.73 m2: dapagliflozin 10 mg, 71.3 mL/min/1.73 m2; placebo, 74.0 mL/min/1.73 m2. CKD chronic kidney disease, eGFR estimated glomerular filtration rate, SGLT2 sodium–glucose co-transporter 2
The 2024 KDIGO clinical practice guideline, the 2023 comprehensive review by the European Renal and Cardiovascular Medicine Working Group and European Renal Best Practice Guideline Group (working groups of the European Renal Association), and the 2023 European Society of Hypertension guidelines all highlight the importance of lifestyle changes in the prevention and management of CKD (Fig. 2) [7, 33, 34]. Management of CKD should also include avoiding nephrotoxic medications (e.g., non-steroidal anti-inflammatory drugs), adjustments to dosing (e.g., antibiotics), and the continued monitoring of kidney function. Guidelines recommend tailoring the monitoring of patients according to risk factors such as eGFR and UACR, with patients at greatest risk of progression being monitored more closely [7]. Individualized risk prediction can also help to inform clinical decision-making and enable personalized care for people with CKD. Guidelines recommend that, in patients with CKD stage 3–5, an externally validated risk equation should be employed to evaluate the absolute risk of kidney failure [7, 35–39]. Understanding risk of progression can help to optimize healthcare delivery, identify individuals who will benefit from disease-modifying therapies, and predict outcomes and plan care accordingly. A 5-year kidney failure risk of 3–5% should prompt consideration of transitioning a patient from primary care to the nephrologist setting, and a 2-year kidney failure risk of > 10% should prompt initiation of multidisciplinary care to manage complications of CKD [7].
A landscape-transforming addition to the treatment of CKD, in both people with and without type 2 diabetes, has been the recommendation by clinical practice guidelines of a SGLT2 inhibitor alongside a RAAS inhibitor as foundational therapy (Fig. 2) [7, 33, 34]. SGLT2 inhibitors prevent CKD progression and reduce fatal and non-fatal kidney and cardiovascular events, hospitalization for heart failure, and all-cause mortality [40]. A meta-analysis of six randomized, double-blind, placebo-controlled trials found that SGLT2 inhibitors reduced the risk of serious hyperkalemia (serum potassium ≥ 6.0 mmol/L) in people with T2D at high cardiovascular risk or with CKD without increasing the risk of hypokalemia [41]. RAAS inhibitors have been the cornerstone of CKD treatment for the past two decades [42–44]. However, uptitration of RAAS inhibitor dose may be necessary to achieve the maximum tolerated dose while avoiding hyperkalemia [45]. For patients with hyperkalemia who are not on the maximally tolerated guideline-recommended RAAS inhibitor dose, an anti-hyperkalemic agent may be initiated (e.g., sodium zirconium cyclosilicate) rather than decreasing the dose or stopping the RAAS inhibitor [46]. A non-steroidal mineralocorticoid receptor antagonist may be added for people with T2D, eGFR > 25 mL/min/1.73 m2, normal serum potassium, and albuminuria (> 30 mg/g) [47].
SGLT2 Inhibitors
SGLT2 inhibitors are a foundational therapy for the treatment of people with CKD, regardless of whether they have T2D or not. The potential for kidney protection with SGLT2 inhibitor use was first observed in cardiovascular outcome trials performed in people with T2D (CANVAS, DECLARE-TIMI 58, and EMPA-REG OUTCOME; Table 1) [48–50]. These data suggested that SGLT2 inhibitors decreased albuminuria, slowed eGFR decline, and were associated with reductions in adverse kidney outcomes, incident end-stage kidney disease, and death from kidney causes. Furthermore, these studies included high proportions of people with relatively normal eGFR measurements, highlighting the benefits of early treatment initiation.
Table 1.
Cardiorenal outcomes of SGLT2 inhibitors observed in phase 3 clinical trials
| Phase 3 clinical trial (N) | Patients | Endpoints | Hazard ratio (95% CI) versus placebo; P |
|---|---|---|---|
| Canagliflozin (100 mg) | |||
| CANVAS (N = 10,142) [48] | T2D, aged ≥ 30 years with history of ASCVD or aged ≥ 50 years at high risk of CVD | Composite of death from CV causes, non-fatal MI, or non-fatal stroke | 0.86 (0.75–0.97); < 0.001 |
| Progression of albuminuria | 0.73 (0.67–0.79) | ||
| Composite of 40% reduction in eGFR, renal-replacement therapy, or death from renal causes | 0.60 (0.47–0.77) | ||
| CREDENCE (N = 4401) [51] | T2D, aged ≥ 30 years with eGFR 30 to < 90 mL/min/1.73 m2 and UACR 300–5000 mg/g | Composite of ESKD, doubling of serum creatinine, or death from renal or CV causes | 0.70 (0.59–0.82); < 0.0001 |
| Dapagliflozin (10 mg) | |||
| DECLARE-TIMI 58 (N = 17,160) [49] | T2D, aged ≥ 40 years with or at risk of ASCVD | MACE (CV death, MI, or ischemic stroke) | 0.93 (0.84–1.03); 0.17 |
| Composite of CV death or hospitalization for heart failure | 0.83 (0.73–0.95); 0.005 | ||
| Composite of 40% reduction in eGFR, ESKD, or death from renal or CV causes | 0.76 (0.67–0.87) | ||
| DAPA-CKD (N = 4304) [52] | With or without T2D, aged ≥ 18 years with eGFR 25–75 mL/min/1.73 m2 and UACR 200–5000 mg/g | Composite of ESKD, decrease in eGFR ≥ 50% or death from renal or CV causes | 0.61 (0.51–0.72); < 0.001 |
| Empagliflozin (10 mg) | |||
| EMPA-REG OUTCOME (N = 7020)* [50] | T2D, aged ≥ 18 years at high risk of CV events | Composite of death from CV causes, non-fatal MI, or non-fatal stroke | 0.86 (0.74–0.99); 0.04 |
| EMPA-KIDNEY (N = 6909) [53] | With or without T2D, aged ≥ 18 years with eGFR 20 to < 45 mL/min/1.73 m2, regardless of the level of albuminuria, or eGFR 45 to < 90 mL/min/1.73 m2 and UACR ≥ 200 mg/g | Composite of ESKD, decrease in eGFR ≥ 40%, eGFR < 10 mL/min/1.73 m2, or death from renal causes | 0.72 (0.64–0.82); < 0.001 |
ASCVD atherosclerotic cardiovascular disease, CV cardiovascular, CVD cardiovascular disease, eGFR estimated glomerular filtration rate, ESKD end-stage kidney disease, MACE major adverse cardiovascular events, MI myocardial infarction, SGLT2 sodium–glucose co-transporter 2, T2D type 2 diabetes, UACR urine albumin-to-creatinine ratio
*Patients randomized to empagliflozin 10 mg, empagliflozin 25 mg, or placebo
Subsequent clinical trials were performed specifically in people with CKD, both with and without T2D (Table 1), with different primary composite kidney outcomes consisting of decrease in eGFR of ≥ 40% or ≥ 50%, sustained eGFR < 10 mL/min/1.73 m2, incident end-stage kidney disease, or death from kidney or cardiovascular causes.
In the CREDENCE study, canagliflozin 100 mg daily significantly reduced the incidence of the primary outcome (relative risk of the composite of end-stage kidney disease [dialysis for ≥ 30 days, kidney transplantation, or eGFR < 15 mL/min/1.73 m2 for ≥ 30 days], doubling of serum creatinine from baseline sustained for ≥ 30 days, or death from renal or cardiovascular causes was 30% lower with canagliflozin compared with placebo; event rates of 43.2 and 61.2 per 1000 patient-years, respectively [HR 0.70; 95% CI 0.59–0.82]) in a population with T2D, an eGFR 30 to < 90 mL/min/1.73 m2, and UACR 300–5000 mg/g [51].
The DAPA-CKD and EMPA-KIDNEY studies assessed the efficacy of SGLT2 inhibitors in people with CKD with or without T2D. In the DAPA-CKD study, dapagliflozin 10 mg daily significantly reduced the incidence of the primary outcome (occurrence of any of sustained decline of ≥ 50% in eGFR from baseline, end-stage kidney disease, or death from renal or cardiovascular causes; incidence was 9.2% versus 14.5% in the dapagliflozin and placebo groups, respectively [HR 0.61; 95% CI 0.51–0.72]) in a population with eGFR 25–75 mL/min/1.73 m2 and UACR 200–5000 mg/g. The result was consistent for patients with or without T2D [52]. In the EMPA-KIDNEY study, empagliflozin 10 mg daily significantly reduced the incidence of the primary outcome (composite of progression of kidney disease [end-stage kidney disease, sustained eGFR of < 10 mL/min/1.73 m2, sustained decrease from baseline eGFR of ≥ 40%, or death from renal causes] or death from cardiovascular causes); incidence was 13.1% versus 16.9% in the empagliflozin and placebo groups, respectively (HR 0.72, 95% CI 0.64–0.82) in a population with eGFR 20 to < 45 mL/min/1.73 m2 regardless of the level of albuminuria or with eGFR 45 to < 90 mL/min/1.73 m2 and UACR ≥ 200 mg/g. The result was consistent for patients with or without T2D [53]. Given that there is a high proportion of people with CKD who do not have T2D and that these patients are prescribed SGLT2 inhibitors at a lower rate than those with CKD who have T2D [54], prescribing SGLT2 inhibitors to patients without T2D would significantly improve their cardiorenal protection.
SGLT2 inhibitors have a favorable safety and tolerability profile [40, 55]. However, there is an increased risk of mycotic genital infections (occurring more frequently in women than men [56]). PCPs should monitor and treat appropriately, and can help to manage these side effects by educating patients about appropriate hygiene. There also remains a risk of SGLT2 inhibitor-associated ketoacidosis in patients with diabetes, although the absolute rates are low and events occur mainly in high-risk patients. In addition to diabetes, factors that may predispose individuals to ketoacidosis include insulin deficiency, surgical stress, caloric restriction, and alcohol abuse [57]. Ketoacidosis should be monitored, and current guidelines recommend that SGLT2 inhibitors are temporarily discontinued in situations that predispose to ketoacidosis (e.g., surgical stress and prolonged fasting) and restarted promptly once these risk factors have resolved. A review article published in 2022 called for a re-assessment of so-called sick-day discontinuation of SGLT2 inhibitors, given the low rates of ketoacidosis in cardiovascular outcome trials and in hospitalized patients with T2D; however, further research is needed to better characterize the risk of ketoacidosis in these patient populations [58]. Patients prescribed SGLT2 inhibitors should be educated on the signs and symptoms of ketoacidosis and advised to seek medical attention should signs and symptoms occur. The absolute benefits of SGLT2 inhibitor use in people with CKD, with or without T2D, far outweigh the risks [40].
A decrease in eGFR of 2–5 mL/min/1.73 m2 may occur within the first few weeks after SGLT2 inhibitor initiation. Although important for PCPs to be aware of, this dip is largely reversed and does not affect long-term cardiovascular and kidney outcomes [59, 60]. The expected dip does not require the frequency of CKD monitoring to be altered and is generally not an indication to discontinue SGLT2 inhibitors [7]. However, a sufficiently large decrease (> 30%) may be a sign of acute kidney injury and should be investigated. Additional monitoring of eGFR may be warranted in patients treated with RAAS inhibitors.
Recommendations to Drive Change in Primary Care
People may have misgivings when diagnosed with a disease with no tangible symptoms. PCPs can reframe CKD as a marker of overall health, with holistic management of kidney function and the risk factors for CKD at the core [61]. Simple explanations of kidney function tests like eGFR and UACR and the meaning of the results may empower people to talk more openly about CKD [62]. Despite fears of a CKD diagnosis, people want to be informed as early as possible [63].
To raise awareness of the importance of early CKD identification and intervention in the public and PCPs, several measures could be adopted. Public awareness could be increased through local/national campaigns and practice-based education. Among PCPs, clinical education programs and exposure on social media could raise awareness and knowledge of CKD. Protocols to streamline early diagnosis and CKD management could be built into primary care workflows. For example, integrating clinical decision support tools into electronic health record platforms can provide up-to-date evidence-based recommendations to guide decisions and improve workflow. The Kidney Failure Risk Equation is the most widely used clinical decision support tool in nephrology practices, although its use is limited in primary care [64]. Automated risk calculation within the electronic medical health systems could help to identify the patients who can be treated at primary care. Incorporating automatic prompts into support tools to encourage PCPs to assess for eGFR, UACR, and blood pressure could improve early identification of CKD [65]. Good communication with a specialist should be nurtured for the shared care of patients. For example, when PCPs were given targeted training on the KDIGO guidelines and the need for early assessment, and network support for specific patients via instant messaging with specialists, there was almost a doubling in the diagnosis of CKD stages 3–5 over 6 months [66]. National guidelines for the management of CKD in primary care should be updated in line with the recent evidence-based clinical practice guidelines.
To monitor and treat accordingly, patients can be stratified by eGFR and UACR measurements (Fig. 2). We emphasize the importance of continuous patient monitoring and observing trends in eGFR and UACR to plan follow-up. Very high-risk patients should be treated in collaboration with a nephrologist. Additional considerations for nephrologist consultation include unexplained decrease in eGFR over 12 months, rapid decrease in eGFR over days to weeks, and unexplained proteinuria or hematuria (Fig. 2).
We recommend a specific call to action for people with CKD and without T2D. PCPs may feel more comfortable prescribing SGLT2 inhibitors to people who have both CKD and T2D owing to familiarity with the treatment effect in this population. Further, people living with CKD and without T2D may be perceived as at a lower risk than those with T2D, hence they are less likely to receive treatment [54]. The FLIEDER study showed that patients with stage 3a–4 CKD without T2D were at increased risk of adverse cardiorenal outcomes, yet only a small proportion of patients were treated with cardiorenal-protective medications (uses of angiotensin-converting enzyme inhibitor and angiotensin II receptor blocker were 34.5% and 20.6%, respectively) [67]. Similar results were observed in the observational OPTIMISE-CKD study, which found that baseline kidney-protective treatment use (RAAS inhibitors or SGLT2 inhibitors) among patients with incident CKD was low, particularly in patients without T2D. Across the three countries studied (Sweden, Japan, and the USA), only 18–48% of people with stage 3–4 CKD without T2D at baseline were receiving kidney-protective treatment. Furthermore, in people with stage 3–4 CKD lacking treatment at baseline, only 8–20% initiated treatment within 12 months [54].
National policies have been introduced in Japan, the USA, and Spain to prevent, treat, and slow progression of CKD [68–71]. The implementation of such policies across the globe, with a focus on PCPs’ unique position to identify and manage patients with CKD at an early stage, is required. In addition, electronic health records and the development of long-term plans for maximizing the data collected by renal registries should be invested in. Epidemiology, trends in treatment and outcomes, monitoring of kidney care quality, and unaddressed patient needs may all be recorded in renal registries [72]. Renal registries could also be expanded to include earlier stages of CKD [73]. Detection programs could be built around electronic health records and local reimbursement/reward practices. Finally, hand in hand with detection programs, PCPs could be educated about clinically coding the identification of CKD, even in the early stages. The eGFR and UACR of patients with risk factors for CKD should be recorded in a timely manner, and, if appropriate, a CKD diagnosis promptly coded.
Conclusion
Early identification and intervention are critical in slowing CKD progression and reducing the associated kidney and cardiovascular morbidity and mortality. Responsibility for the early identification and optimal management of CKD should be shared among all clinicians. PCPs at the forefront of multidisciplinary care are best placed to implement the evidence-based clinical practice CKD guidelines for lifestyle modification and guideline-directed medical therapy.
Acknowledgments
Medical Writing/Editorial Assistance
Medical writing support for this manuscript was provided by Nathan Price-Lloyd, PhD, of Oxford PharmaGenesis, Oxford, UK, and was funded by AstraZeneca.
Author Contributions
Pamela Kushner, Kamlesh Khunti, Ana Cebrián, and Gary Deed contributed to the conception and design of the article. All authors (Pamela Kushner, Kamlesh Khunti, Ana Cebrián, and Gary Deed) commented on draft versions of the manuscript. All authors (Pamela Kushner, Kamlesh Khunti, Ana Cebrián, and Gary Deed) read and approved the final manuscript.
Funding
Funding for the journal’s Open Access and Rapid Service Fee was provided by AstraZeneca.
Data Availability
Data sharing is not applicable to this article because no datasets were generated or analyzed during the current study.
Declarations
Conflict of Interest
Ana Cebrián has received grants from Merck Sharp & Dohme and speaker honoraria from AstraZeneca, Boehringer Ingelheim, Eli Lilly and Company, Janssen, Merck Sharp & Dohme, Mundipharma, Novartis Pharmaceuticals, Novo Nordisk, and Sanofi. Gary Deed reports advisory board fees from AstraZeneca and Boehringer Ingelheim, as well as non-financial involvement in the START Trial (The George Institute) of SGLT2 inhibitors as first-line therapy to improve renal outcomes in T2D. He is a consultant to Abbott, Amgen, AstraZeneca, Boehringer Ingelheim, Lilly, Merck Sharp & Dohme, Novartis, Novo Nordisk, Sanofi, and Sequiris. Kamlesh Khunti has received consultancy fees from Amgen, AstraZeneca, Bristol Myers-Squibb, Boehringer Ingelheim, Eli Lilly and Company, Novo Nordisk, Sanofi, Servier, Pfizer, Roche, Daiichi-Sankyo, Embecta, and Nestlé Health Science; research support from AstraZeneca, Boehringer Ingelheim, Eli Lilly and Company, Merck, Novo Nordisk, Roche, Sanofi, Servier, Oramed Pharmaceuticals, Daiichi-Sankyo, and Applied Therapeutics; and speaker’s bureau fees from AstraZeneca, Boehringer Ingelheim, Eli Lilly and Company, Merck, Novo Nordisk, Sanofi, Servier, and Roche. Pamela Kushner has received speaker’s bureau and advisory board fees from Abbott, AstraZeneca, Boehringer Ingelheim, Eli Lilly and Company, and Novo Nordisk A/S; speaker’s fees from Bayer AG and Boehringer Ingelheim; and honoraria from AstraZeneca and Eli Lilly and Company.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
References
- 1.Sundström J, Bodegard J, Bollmann A, et al. Prevalence, outcomes, and cost of chronic kidney disease in a contemporary population of 2·4 million patients from 11 countries: the CaReMe CKD study. Lancet Reg Health Eur. 2022;20:100438. 10.1016/j.lanepe.2022.100438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fraser SD, Blakeman T. Chronic kidney disease: identification and management in primary care. Pragmat Obs Res. 2016;7:21–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chu CD, McCulloch CE, Banerjee T, et al. CKD awareness among US adults by future risk of kidney failure. Am J Kidney Dis. 2020;76(2):174–83. 10.1053/j.ajkd.2020.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tangri N, Moriyama T, Schneider MP, et al. Prevalence of undiagnosed stage 3 chronic kidney disease in France, Germany, Italy, Japan and the USA: results from the multinational observational REVEAL-CKD study. BMJ Open. 2023;13(5):e067386. 10.1136/bmjopen-2022-067386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nichols GA, Déruaz-Luyet A, Brodovicz KG, Kimes TM, Rosales AG, Hauske SJ. Kidney disease progression and all-cause mortality across estimated glomerular filtration rate and albuminuria categories among patients with vs without type 2 diabetes. BMC Nephrol. 2020;21(1):167. 10.1186/s12882-020-01792-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tangri N, Alvarez CS, Arnold M, Barone S, Cebrián A, Chen H, et al. Suboptimal monitoring and management in patients with unrecorded stage 3 chronic kidney disease in real-world settings: insights from REVEAL-CKD. Eur J Clin Invest. 2024. 10.1111/eci.14282. 10.1111/eci.14282 [DOI] [PubMed] [Google Scholar]
- 7.KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int. 2024;105(4S):S117–S314. [DOI] [PubMed]
- 8.Tangri N, Peach EJ, Franzén S, Barone S, Kushner PR. Patient management and clinical outcomes associated with a recorded diagnosis of stage 3 chronic kidney disease: the REVEAL-CKD study. Adv Ther. 2023;40(6):2869–85. 10.1007/s12325-023-02482-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carney EF. The impact of chronic kidney disease on global health. Nat Rev Nephrol. 2020;16(5):251. 10.1038/s41581-020-0268-7 [DOI] [PubMed] [Google Scholar]
- 10.Gansevoort RT, Correa-Rotter R, Hemmelgarn BR, et al. Chronic kidney disease and cardiovascular risk: epidemiology, mechanisms, and prevention. Lancet. 2013;382(9889):339–52. 10.1016/S0140-6736(13)60595-4 [DOI] [PubMed] [Google Scholar]
- 11.Verberne WR, Das-Gupta Z, Allegretti AS, et al. Development of an international standard set of value-based outcome measures for patients with chronic kidney disease: a report of the International Consortium for Health Outcomes Measurement (ICHOM) CKD Working Group. Am J Kidney Dis. 2019;73(3):372–84. 10.1053/j.ajkd.2018.10.007 [DOI] [PubMed] [Google Scholar]
- 12.Zoccali C, Mark PB, Sarafidis P, et al. Diagnosis of cardiovascular disease in patients with chronic kidney disease. Nat Rev Nephrol. 2023;19(11):733–46. 10.1038/s41581-023-00747-4 [DOI] [PubMed] [Google Scholar]
- 13.Szlagor M, Dybiec J, Młynarska E, Rysz J, Franczyk B. Chronic kidney disease as a comorbidity in heart failure. Int J Mol Sci. 2023;24(3):2988. 10.3390/ijms24032988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.MacRae C, Mercer SW, Guthrie B, Henderson D. Comorbidity in chronic kidney disease: a large cross-sectional study of prevalence in Scottish primary care. Br J Gen Pract. 2021;71(704):e243–9. 10.3399/bjgp20X714125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chadban S, Esposito C, Rangaswami J, Wu M-S, Hull R, Elsayed H, et al. #4529 PACE-CKD: Financial burden and work productivity of patients with CKD and caregivers: results from a US survey. Nephrol Dial Transplant. 2023;38(Suppl 1):4529. [Google Scholar]
- 16.Esposito C, Chadban S, Rangaswami J, et al. #3990 PACE-CKD: Health-related quality of life of patients with CKD and caregivers: results from a US survey. Nephrol Dial Transplant. 2023;38(Suppl 1):3990. [Google Scholar]
- 17.Carrero J, Pollock C, Kanda E, et al. #3393 Patient-reported outcomes in early versus advanced chronic kidney disease: evidence from baseline data in the discover CKD prospective study. Nephrol Dial Transplant. 2023;38.
- 18.Tummalapalli SL, Powe NR, Keyhani S. Trends in quality of care for patients with CKD in the United States. Clin J Am Soc Nephrol. 2019;14(8):1142–50. 10.2215/CJN.00060119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kovesdy CP. Epidemiology of chronic kidney disease: an update 2022. Kidney Int Suppl. 2022;12(1):7–11. 10.1016/j.kisu.2021.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jha V, Al-Ghamdi SMG, Li G, et al. Global economic burden associated with chronic kidney disease: a pragmatic review of medical costs for the inside CKD research programme. Adv Ther. 2023;40(10):4405–20. 10.1007/s12325-023-02608-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization: Reducing noncommunicable diseases: a signature roadmap for the WHO European Region. https://www.who.int/europe/publications/i/item/WHO-EURO-2022-6620-46386-67147. Accessed July 2023.
- 22.ISN Global Kidney Health Atlas. https://www.theisn.org/initiatives/global-kidney-health-atlas/. Accessed 2023.
- 23.Francis A, Harhay MN, Ong ACM, et al. Chronic kidney disease and the global public health agenda: an international consensus. Nat Rev Nephrol. 2024;20:473. 10.1038/s41581-024-00820-6 [DOI] [PubMed] [Google Scholar]
- 24.Khunti K, Sathanapally H, Mountain P. Multiple long term conditions, multimorbidity, and co-morbidities: we should reconsider the terminology we use. BMJ. 2023;383:2327. 10.1136/bmj.p2327 [DOI] [PubMed] [Google Scholar]
- 25.Nee R, Yuan CM, Narva AS, Yan G, Norris KC. Overcoming barriers to implementing new guideline-directed therapies for chronic kidney disease. Nephrol Dial Transplant. 2023;38(3):532–41. 10.1093/ndt/gfac283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sperati CJ, Soman S, Agrawal V, et al. Primary care physicians’ perceptions of barriers and facilitators to management of chronic kidney disease: a mixed methods study. PLoS ONE. 2019;14(8):e0221325. 10.1371/journal.pone.0221325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khunti K, Jabbour S, Cos X, et al. Sodium-glucose co-transporter-2 inhibitors in patients with type 2 diabetes: barriers and solutions for improving uptake in routine clinical practice. Diabetes Obes Metab. 2022;24(7):1187–96. 10.1111/dom.14684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Delgado C, Baweja M, Crews DC, et al. A unifying approach for GFR estimation: recommendations of the NKF-ASN Task Force on reassessing the inclusion of race in diagnosing kidney disease. Am J Kidney Dis. 2022;79(2):268–88.e1. 10.1053/j.ajkd.2021.08.003 [DOI] [PubMed] [Google Scholar]
- 29.Madero M, Chertow GM, Mark PB. SGLT2 inhibitor use in chronic kidney disease: supporting cardiovascular, kidney, and metabolic health. Kidney Med. 2024;6(8):100851. 10.1016/j.xkme.2024.100851 [DOI] [Google Scholar]
- 30.Heerspink HJL, Jongs N, Chertow GM, et al. Effect of dapagliflozin on the rate of decline in kidney function in patients with chronic kidney disease with and without type 2 diabetes: a prespecified analysis from the DAPA-CKD trial. Lancet Diabetes Endocrinol. 2021;9(11):743–54. 10.1016/S2213-8587(21)00242-4 [DOI] [PubMed] [Google Scholar]
- 31.Komenda P, Ferguson TW, Macdonald K, et al. Cost-effectiveness of primary screening for CKD: a systematic review. Am J Kidney Dis. 2014;63(5):789–97. 10.1053/j.ajkd.2013.12.012 [DOI] [PubMed] [Google Scholar]
- 32.Cusick MM, Tisdale RL, Chertow GM, Owens DK, Goldhaber-Fiebert JD. Population-wide screening for chronic kidney disease: a cost-effectiveness analysis. Ann Intern Med. 2023;176(6):788–97. 10.7326/M22-3228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mancia G, Kreutz R, Brunström M, et al. ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension Endorsed by the European Renal Association (ERA) and the International Society of Hypertension (ISH). J Hyperten. 2023. 10.1097/HJH.0000000000003480. 10.1097/HJH.0000000000003480 [DOI] [Google Scholar]
- 34.Mark PB, Sarafidis P, Ekart R, et al. SGLT2i for evidence based cardiorenal protection in diabetic and non-diabetic chronic kidney disease: a comprehensive review by EURECA-m and ERBP working groups of ERA. Nephrol Dial Transplant. 2023;38(11):2444–55. [DOI] [PMC free article] [PubMed]
- 35.Schroeder EB, Yang X, Thorp ML, et al. Predicting 5-year risk of RRT in stage 3 or 4 CKD: development and external validation. Clin J Am Soc Nephrol. 2017;12(1):87–94. 10.2215/CJN.01290216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grams ME, Brunskill NJ, Ballew SH, et al. The kidney failure risk equation: evaluation of novel input variables including eGFR estimated using the CKD-EPI 2021 equation in 59 cohorts. J Am Soc Nephrol. 2023;34(3):482–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Major RW, Shepherd D, Medcalf JF, Xu G, Gray LJ, Brunskill NJ. The kidney failure risk equation for prediction of end stage renal disease in UK primary care: an external validation and clinical impact projection cohort study. PLoS Med. 2019;16(11):e1002955. 10.1371/journal.pmed.1002955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zacharias HU, Altenbuchinger M, Schultheiss UT, et al. A predictive model for progression of CKD to kidney failure based on routine laboratory tests. Am J Kidney Dis. 2022;79(2):217–30.e1. 10.1053/j.ajkd.2021.05.018 [DOI] [PubMed] [Google Scholar]
- 39.Landray MJ, Thambyrajah J, McGlynn FJ, et al. Epidemiological evaluation of known and suspected cardiovascular risk factors in chronic renal impairment. Am J Kidney Dis. 2001;38(3):537–46. 10.1053/ajkd.2001.26850 [DOI] [PubMed] [Google Scholar]
- 40.Nuffield Department of Population Health Renal Studies Group; SGLT2 inhibitor Meta-Analysis Cardio-Renal Trialists’ Consortium. Impact of diabetes on the effects of sodium glucose co-transporter-2 inhibitors on kidney outcomes: collaborative meta-analysis of large placebo-controlled trials. Lancet. 2022;400(10365):1788–801. [DOI] [PMC free article] [PubMed]
- 41.Neuen BL, Oshima M, Agarwal R, et al. Sodium-glucose cotransporter 2 inhibitors and risk of hyperkalemia in people with type 2 diabetes: a meta-analysis of individual participant data from randomized controlled trials. Circulation. 2022;145(19):1460–70. 10.1161/CIRCULATIONAHA.121.057736 [DOI] [PubMed] [Google Scholar]
- 42.Lewis EJ, Hunsicker LG, Bain RP, Rohde RD. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The Collaborative Study Group. N Engl J Med. 1993;329(20):1456–62. 10.1056/NEJM199311113292004 [DOI] [PubMed] [Google Scholar]
- 43.Lewis EJ, Hunsicker LG, Clarke WR, et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med. 2001;345(12):851–60. 10.1056/NEJMoa011303 [DOI] [PubMed] [Google Scholar]
- 44.Brenner BM, Cooper ME, de Zeeuw D, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med. 2001;345(12):861–9. 10.1056/NEJMoa011161 [DOI] [PubMed] [Google Scholar]
- 45.Kanda E, Rastogi A, Murohara T, et al. Clinical impact of suboptimal RAASi therapy following an episode of hyperkalemia. BMC Nephrol. 2023;24(1):18. 10.1186/s12882-022-03054-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group. KDIGO 2020 Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease. Kidney Int. 2020;98(4S):S1–115. [DOI] [PubMed] [Google Scholar]
- 47.Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2024 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. 2024;105(4S):S117–314. [DOI] [PubMed] [Google Scholar]
- 48.Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377(7):644–57. 10.1056/NEJMoa1611925 [DOI] [PubMed] [Google Scholar]
- 49.Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380(4):347–57. 10.1056/NEJMoa1812389 [DOI] [PubMed] [Google Scholar]
- 50.Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–28. 10.1056/NEJMoa1504720 [DOI] [PubMed] [Google Scholar]
- 51.Perkovic V, Jardine MJ, Neal B, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380(24):2295–306. 10.1056/NEJMoa1811744 [DOI] [PubMed] [Google Scholar]
- 52.Heerspink HJL, Stefánsson BV, Correa-Rotter R, et al. Dapagliflozin in patients with chronic kidney disease. N Engl J Med. 2020;383(15):1436–46. 10.1056/NEJMoa2024816 [DOI] [PubMed] [Google Scholar]
- 53.Herrington WG, Staplin N, Wanner C, et al. Empagliflozin in patients with chronic kidney disease. N Engl J Med. 2023;388(2):117–27. 10.1056/NEJMoa2204233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tangri N, Svensson MK, Bodegård J, et al. Mortality, health care burden, and treatment of CKD: a multinational, observational study (OPTIMISE-CKD). Kidney. 2024;5(3):352–62. 10.34067/KID.0000000000000374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Toyama T, Neuen BL, Jun M, et al. Effect of SGLT2 inhibitors on cardiovascular, renal and safety outcomes in patients with type 2 diabetes mellitus and chronic kidney disease: a systematic review and meta-analysis. Diabetes Obes Metab. 2019;21(5):1237–50. 10.1111/dom.13648 [DOI] [PubMed] [Google Scholar]
- 56.Thong KY, Yadagiri M, Barnes DJ, et al. Clinical risk factors predicting genital fungal infections with sodium-glucose cotransporter 2 inhibitor treatment: the ABCD nationwide dapagliflozin audit. Prim Care Diabetes. 2018;12(1):45–50. 10.1016/j.pcd.2017.06.004 [DOI] [PubMed] [Google Scholar]
- 57.Palmer BF, Clegg DJ. Euglycemic ketoacidosis as a complication of SGLT2 inhibitor therapy. Clin J Am Soc Nephrol. 2021;16(8):1284–91. 10.2215/CJN.17621120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Khunti K, Aroda VR, Bhatt DL, et al. Re-examining the widespread policy of stopping sodium-glucose cotransporter-2 inhibitors during acute illness: a perspective based on the updated evidence. Diabetes Obes Metab. 2022;24(11):2071–80. 10.1111/dom.14805 [DOI] [PubMed] [Google Scholar]
- 59.Jongs N, Chertow GM, Greene T, et al. Correlates and consequences of an acute change in eGFR in response to the SGLT2 inhibitor dapagliflozin in patients with CKD. J Am Soc Nephrol. 2022;33(11):2094–107. 10.1681/ASN.2022030306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Oshima M, Jardine MJ, Agarwal R, et al. Insights from CREDENCE trial indicate an acute drop in estimated glomerular filtration rate during treatment with canagliflozin with implications for clinical practice. Kidney Int. 2021;99(4):999–1009. 10.1016/j.kint.2020.10.042 [DOI] [PubMed] [Google Scholar]
- 61.Simmonds R, Evans J, Feder G, et al. Understanding tensions and identifying clinician agreement on improvements to early-stage chronic kidney disease monitoring in primary care: a qualitative study. BMJ Open. 2016;6(3):e010337. 10.1136/bmjopen-2015-010337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kushner PR, DeMeis J, Stevens P, Gjurovic AM, Malvolti E, Tangri N. Patient and clinician perspectives: to create a better future for chronic kidney disease, we need to talk about our kidneys. Adv Ther. 2024;41(4):1318–24. 10.1007/s12325-024-02794-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wright Nunes J, Roney M, Kerr E, Ojo A, Fagerlin A. A diagnosis of chronic kidney disease: despite fears patients want to know early. Clin Nephrol. 2016;86(2):78–86. 10.5414/CN108831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Alexiuk M, Elgubtan H, Tangri N. Clinical decision support tools in the electronic medical record. Kidney Int Reports. 2024;9(1):29–38. 10.1016/j.ekir.2023.10.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Willis A, Crasto W, Gray LJ, et al. Effects of an electronic software “prompt” with health care professional training on cardiovascular and renal complications in a multiethnic population with type 2 diabetes and microalbuminuria (the GP-Prompt Study): results of a pragmatic cluster-randomized trial. Diabetes Care. 2020;43(8):1893–901. 10.2337/dc19-2243 [DOI] [PubMed] [Google Scholar]
- 66.Pesce F, Pasculli D, Pasculli G, et al. “The Disease Awareness Innovation Network” for chronic kidney disease identification in general practice. J Nephrol. 2022;35(8):2057–65. 10.1007/s40620-022-01353-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wanner C, Schuchhardt J, Bauer C, et al. Clinical characteristics and disease outcomes in non-diabetic chronic kidney disease: retrospective analysis of a US healthcare claims database. J Nephrol. 2023;36(1):45–54. 10.1007/s40620-022-01340-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Advancing American Kidney Health. https://www.federalregister.gov/documents/2019/07/15/2019-15159/advancing-american-kidney-health. Accessed Oct 2023.
- 69.Fukui A, Yokoo T, Nangaku M, Kashihara N. New measures against chronic kidney diseases in Japan since 2018. Clin Exp Nephrol. 2019;23(11):1263–71. 10.1007/s10157-019-01786-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Alcázar R, Egocheaga MI, Orte L, et al. SEN-SEMFYC consensus document on chronic kidney disease. Nefrologia. 2008;28(3):273–82. [PubMed] [Google Scholar]
- 71.Gorostidi M, Santamaría R, Alcázar R, et al. Spanish Society of Nephrology document on KDIGO guidelines for the assessment and treatment of chronic kidney disease. Nefrologia. 2014;34(3):302–16. [DOI] [PubMed] [Google Scholar]
- 72.van der Veer SN, Couchoud C, Morton RL. The role of kidney registries in expediting large-scale collection of patient-reported outcome measures for people with chronic kidney disease. Clin Kidney J. 2021;14(6):1495–503. 10.1093/ckj/sfab061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jager KJ, Åsberg A, Collart F, et al. A snapshot of European registries on chronic kidney disease patients not on kidney replacement therapy. Nephrol Dial Transplant. 2021;37(1):8–13. 10.1093/ndt/gfab252 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article because no datasets were generated or analyzed during the current study.