Highlights
-
•
Despite their simplified design, training in the use of AEDs enhances effectiveness.
-
•
Participants took 7 s longer to initiate shock with unfamiliar AEDs, experiencing confusion, nervousness, and anxiety.
-
•
Technical aspects of AEDs, such as covers, electrodes, and buttons, contributed to this confusion. However, clear instructions and similarities between devices facilitated usage.
-
•
Our findings underscore the importance of prior training and familiarity with AED models for an effective response to OHCA.
Keywords: First aid training, Defibrillation timing, Technical features, Instructional design, Basic Life Support, Simulation
Abstract
Objective
This study examined the impact of prior familiarity with automated external defibrillator (AED) models on the time of defibrillation and the emotional experiences of laypersons.
Methods
We conducted a randomized cross over simulation study with 123 participants to assess their reactions to both familiar and unfamiliar AED models. The time to first defibrillation was measured using three different AED training models, two of which were previously unknown to the participants. Additionally, semi-structured interviews were held with the participants to gather further insights.
Results
Participants took longer to initiate defibrillation with unfamiliar (M = 34 s) AEDs compared to familiar (M = 27 s) ones. This delay was accompanied by feelings of confusion, nervousness, and anxiety. Factors such as the design of the AED covers, electrodes, and buttons were identified as sources of confusion. Nonetheless, clear instructions and similarities between devices helped facilitate their use.
Conclusion
The findings suggest that AED design and familiarity with different AED designs may affect performance by laypersons. To improve user confidence, it would be useful to familiarize users with a variety of AED models as part of training initiatives. Understanding the impact of AED familiarity on rescuer’s response can guide CPR training strategies and improve outcomes for OHCA. As more AED models become available to the public, the user-friendliness of AEDs may also be improved. It is beneficial for AED manufacturers to consider the results of research when developing new models.
Introduction
Out-of-hospital cardiac arrest (OHCA) remains the leading cause of death worldwide.1 The earlier bystanders begin cardiopulmonary resuscitation (CPR) and use an automated external defibrillator (AED), the better the resuscitation outcomes.2 Laypersons must be able to use AEDs quickly and effectively.3 For every minute that passes before the first defibrillation, the chance of survival to hospital discharge decreases by 10%.4
In addition to the availability of AEDs, other factors can influence defibrillation time. Different AED models have various technical features and software that affect the time needed for heart rhythm analysis and preparation for defibrillation.5 The type of defibrillator significantly influences the time to the first shock delivered.6 Previous studies have determined the technical and other characteristics an AED must have for laypersons to use it most easily and quickly. 3, 7 Future AEDs that combine all the beneficial features from previous research-verified models have been identified and recommended.7 The visibility of power-on mechanisms, the ease of finding the pads, clarity and preciseness of pad placement instructions and step-by −step CPR instructions can increase the ease and speed of use of the AED.3 Devices with open lids or pull handles, detailed voice prompts for pad placement, and step-by-step CPR instructions can enable users to achieve shorter power on time, greater adequacy of pad position, and better CPR performance after shock delivery.7. Design not requiring a separate case, such as zipper cases, decreases the time to power-on.3 Stærk et al.8 identified barriers and facilitators related to AED usage. Often it was described that resuscitation courses were not sufficiently contextualized e.g., used different AED models, or did not train how to unpack and turn on the AED. Facilitators for AED use was recently completed resuscitation course, previous experience with AED use from clinical situations or simulations.
Typically, laypeople are trained on only one type of AED, despite recommendations by Lei et al.7 that training should include different AED devices. Distinctive features of AED devices influence layperson performance; different voice prompts can lead to longer times to resume CPR.3, 9 Research involving college students demonstrated that using an unfamiliar AED model 6 month after CPR with AED training, prolonged the time to shock delivery.7 In addition, other factors such as age10, 11 prior participation in CPR training12 and psychophysical abilities13 affect the quality of CPR performance. Vincent et al.14 in a narrative review of the literature, reported that rescuers experience high levels of stress, noting some correlation between higher stress levels and lower resuscitation performance. Theoretical knowledge of CPR15 and participation in CPR training16, 17 also play significant roles in mitigating stress during CPR. However, the impact of using an unfamiliar AED on stress levels or other emotional experiences during CPR remains unclear.
The purpose of this study was to determine how prior knowledge of the AED model affects the time to shock and the emotional experiences of laypersons when using an unfamiliar AED model.
Materials and methods
Study design
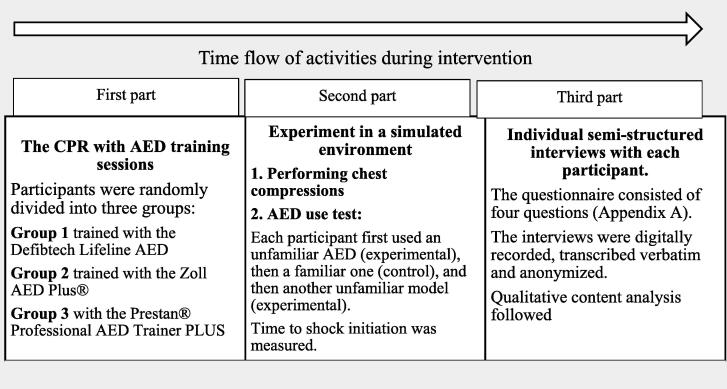
We conducted a randomized cross-over simulation study. The reporting of the study adheres to the extensions of the STROBE statements as outlined in the Reporting Guidelines for Health Care Simulation Research.18 The research consists of three parts (Fig. 1). The protocol and measuring instruments were tested on a group of six students who had first aid exercises at the Faculty of Health of the University of Ljubljana. We did not include them in the final analysis. The protocol was partially adapted after testing (change of measuring instrument).
Fig. 1.
Time flow chart of the activities of the research.
Participants
Participants were volunteers who attended a free CPR and AED training session. The invitation was published on the websites and bulletin boards of various societies (scouts, student organizations, Faculty of Health of the University of Ljubljana, retirement associations). We also informed them that after session they would have the possibility to participate in research on the topic of AED use. The inclusion criterion was a minimum age of 18 years. Individuals who were interested in the CPR course signed up for a specific appointment. We held the courses when we had enough applicants. We randomly assigned the applicants in three groups.
Procedure
The content of CPR training sessions was based on the ERC Guidelines for Resuscitation 2021.19 For the theoretical lecture, we used Microsoft PowerPoint. Then, all research participants practiced CPR and AED use. The research participants from Group 1 trained with the Defibtech Lifeline AED, Group 2 with the Zoll AED Plus®, and Group 3 with the Prestan® Professional AED Trainer PLUS. Participants were unaware that they would be tested on unfamiliar AED models after the lecture and practice sessions. The model participants trained with is a control AED. The models with which they were later tested are experimental AEDs. To ensure consistency in training, all sessions were led by the same licensed first-aid instructor, who holds a university medical degree.
In the second part of the study, we conducted an experiment in a simulated environment thus simulation is investigational method for our research. It took place in a separate room to ensure a quiet setting, with only one research participant and the test conductor present. Before starting, each participant received the same verbal instructions: “A man has collapsed in front of you, you have ensured safety, determined that he is not breathing, and you have already called an ambulance.” The experiment commenced with participants performing chest compressions on the CPR Laerdal-Little Anni QCPR Learning Model. The training model was shirtless. Five seconds into the compressions, the experimenter (ŽM) placed the AED training model beside the head of the CPR training model on the side where the participant was kneeling. Upon placement of the AED, participants were instructed to use it. The experiment began once the experimenter gave permission to start the AED.
Immediately after completing the second part of the study, individual semi-structured interviews were conducted with each participant. These interviews were based on a semi-structured questionnaire (see Appendix A) developed from a literature review and refined after pilot interviews. The interviews were conducted by EDŠ, a doctoral student of Public Health at the Faculty of Medicine, University of Ljubljana, and a teaching assistant for First Aid. Anonymity and a quiet environment were ensured during the interviews. Participants were allowed to refer to the AEDs they had used in the experiment while responding. The interviews were digitally recorded, transcribed verbatim, and anonymized. Field notes were also taken during and after the interviews and were included in the final analysis. Transcripts were not returned to participants for feedback, and no repeated interviews were conducted. The first, second, and third authors performed qualitative content analysis on the interview transcripts. Each transcript was read, qualitatively coded, reviewed, and labelled using inductive content analysis.22 All authors (EDŠ, DS, ŽM) analyzed each interview independently, generating codes for each statement that reflected the interviewees’ opinions. After individual analyses, the authors reached a consensus on the categories and themes. Themes and categories were defined inductively after establishing codes to condense observations from the data and were not predetermined. To ensure anonymity, interviewees’ names were changed, and they did not provide feedback on the findings.
Statistical analysis
The data on the measured times of AED use (time to shock) were analyzed using IBM SPSS software (version 26.0). Descriptive analyses of continuous variables were conducted and expressed as means and standard deviations. We performed the Kolmogorov-Smirnov and Shapiro-Wilk tests to assess the normality of each continuous variable. For normally distributed data, we used the paired t-test, and for non-normally distributed data, we applied the non-parametric Wilcoxon test. The significance level was set at p < 0.05.
Ethical approval
The research was approved by the University of Ljubljana, Faculty of Health Sciences, Chair of Public Health, on September 28, 2022. All participants signed written informed consent forms. Persons who wished to withdraw from the survey during the training had the opportunity to leave any time. The participants were assured about their anonymity and confidentiality of their information. Prior to performing the interviews, all subjects were informed about the objectives of the study, the voluntary nature of their participation, the data collection methods, the reason of recording the interviews, the role of the interviewer and the participants, as well as confidentiality and anonymity of the information. The present study was conducted in terms of the principles of the revised Declaration of Helsinki.
Results
The survey was conducted between July 2022 and July 2023. The training sessions lasted 120 min, divided into theoretical and practical parts. A total of 139 participants were initially attended CPR course, and 130 were involved in the study. We included 123 participants in the final analysis; of these there were 31% (n = 38) each in the first and second groups, and 38% (n = 47) in the third. Seven were excluded due to errors in the execution of the experiment (technical error when measuring time), incomplete data, lack of AED proficiency, or prior familiarity with at least one of the experimental AEDs. We conducted 15 sessions, each with 8–12 participants. Most of the study participants were female (85%). The participant age ranged from 18 to 60 years, with an average age of 35 years. The majority were employed (63%), followed by students (32%). Over a third had completed a second Bologna degree (40%). (Table 1).
Table 1.
Demographic data of all participants.
| female | male | ||||
| Sex | 85% (n = 104) |
15% (n = 19) |
|||
| ≤ 20 | 21–30 | 31–40 | 41–50 | > 50 | |
| Age (groups) | 14% (n = 17) |
33% (n = 41) |
15% (n = 18) |
25% (n = 31) |
13% (n = 16) |
| primary school | secondary school | higher education – 1st cycle of Bologna | higher education 2nd cycle of Bologna | higher education 3rd cycle of Bologna | |
| Education | 2% (n = 2) |
33% (n = 41) |
20% (n = 25) |
40% (n = 49) |
6% (n = 74) |
| middle schooler | student | employed | other | ||
| Status | 4% (n = 5) |
32% (n = 39) |
63% (n = 77) |
2% (n = 104) |
|
| Yes | No | ||||
| Nursing or pharmacy students | 30% (n = 12) |
70% (n = 27) |
On average, participants took 7 s less to deliver first shock with a familiar AED (Table 2).
Table 2.
Comparison of the times (median, percentiles) to shock when use familiar and unfamiliar AEDs.
| Times (in seconds) e-AEDs (M; P25; P75) | Times (in seconds) c-AED (M; P25, P75) | c-AED: e-AEDs | |
|---|---|---|---|
| Time to deliver first shock1+2+3 | 27 (22; 34) | 34 (26,5; 45) | p = 0.000 (Wilcoxon test (Z = -6.215) |
| Turning on the AED 1 | 16 (7; 23) | 17,5 (9; 28) | p = 0.000 (Wilcoxon test (Z = -3.644) |
| Electrodes 2 | 22 (18; 29) | 28,5 (22; 38,5) | p = 0.000 (Wilcoxon test (Z = -5.582) |
| Pause 3 | 3 (2; 4) | 3,5 (2,5; 4) | p = 0.012 (Wilcoxon test (Z = -2.505) |
1 time to AED activation; 2 time to electrode placement; 3 time from recommended defibrillation to its implementation; C-AED control AED; e- AED experimental AEDs.
Out of a total of 123 participants, 31 reported confusion when using an unfamiliar AED training model, along with feelings of nervousness (n = 11) and anxiety (n = 8). The use of an unfamiliar model also led to a lack of confidence and increased discomfort and stress among participants (Table 2). Conversely, when using the familiar AED training model, participants felt safer and more confident, as one participant expressed: “I felt more confident with the familiar AED” (Table 3).
Table 3.
Comparison of feelings experienced by research participants (n = 123).
|
FAMILIAR AED |
UNFAMILIAR AED |
||
|---|---|---|---|
| Categories | Code (n) | Categories | Code (n) |
| Easier to use | Easier to use (10) More understandable (1) | Disorientation | Confusion (31) Lost (4) |
| Self-confidence | Sovereignty (7) Self-confidence (5) Certainty (3) Focus (1) |
Negative emotions | Nervousness (11) Fear (8) Panic (7) Concern (1) Powerlessness (2) |
| Fewer negative emotions | No Fear (1) Less panic (1) Less nervousness (1) |
Lack of knowledge | Ignorance (8) Non-sovereignty (2) |
| Feelings of pleasure | You feel better (7) Comfortableness (7) | Stress | Stress (5) |
| A surprise | Surprise (3) Reluctance (2) | ||
| Discomfort | Unpleasantness (5) | ||
| Doubt about performance | Uncertainty (3) | ||
When using an unfamiliar AED training model, participants (n = 123) were confused by the various technical features of the devices. The most common issues were with the AED cover (n = 29), a non-illuminated power button (n = 14), and the shock button (n = 10). Additionally, different voices and visual instructions also caused confusion (Table 4).
Table 4.
Factors that, according to interviewees (n = 123), confuse a person when using an unfamiliar AED training model.
| Categories | Subcategories | Codes (n) |
|---|---|---|
| Technical characteristics of the device | AED cover | Difficult opening of the AED (29) AED had a cover (5) |
| Characteristics of electrodes | Electrode packing method (7) Electrode storage location (9) Picture instructions on the electrodes (7) Different electrodes (8) |
|
| Features of buttons | Undistinctive power buttons (14) Nondescript shock buttons (10) Different button position (3) Light signals on the button (1) Too many buttons (1) |
|
| Instructions | Voice instructions | Different voice instructions (16) Scarcity of voice instructions (2) |
| Pictorial instructions | Different pictorial instructions (7) Too many picture instructions (5) | |
| How to store the AED | Bag | The AED was in the bag (12) |
We explored what motivated participants (n = 123) to handle and continue using an unfamiliar device despite their unfamiliarity with the AED training model. The dominant response was that the devices were similar and functioned in a comparable manner. One participant noted, “Logically done, makes sense. If you roughly know what you are working with, you can manage when it’s slightly different. It is like a phone; you get a new one, and you know how it works” (U48SK2). Besides the similarity of the devices and their operation, participants noted that their ability to handle the unfamiliar model was also influenced by the previous workshop and their prior knowledge, as one stated, “… the fact that we have already learned about AED in other courses” (U4SK1). Verbal and visual instructions for the AED were also found to be helpful. However, some participants mentioned their desire to help people and save lives as motivating factors, with comments like, “… because I wanted to save lives” (U9SK1) and “… to help and save lives” (U7SK1) (Table 5).
Table 5.
Factors that, according to interviewees (n = 123) opinions, help a person to use an unfamiliar AED training model.
| Categories | Codes (n) |
|---|---|
| AED instructions | AED audio instructions (21) AED guides you (6) Light signals (3) Pictorial instructions (8) Clear instructions (2) Pictorial instructions on the electrodes (1) |
| Technical characteristics of the devices | Device similarity (14) Similar buttons (2) |
| Mode of operation of devices | Similar modes of operation (37) |
| Knowledge | Prior training (24) Prior knowledge (10) |
| Altruism | Helping a person (15) Save a life (3) |
Discussion
Prior knowledge of the AED model shortens the time until the first shock. When using an unfamiliar AED model, rescuers experienced more negative emotions such as confusion, nervousness, fear, panic, and stress. Respondents highlighted their lack of knowledge but also pointed out several features of the device that aid in the use of an unfamiliar AED model, such as audio instructions and similar features across different AEDs. Additionally, participants emphasized that they could rely on previous knowledge and training when using an unfamiliar AED model.
We found that using an unfamiliar AED increased the time to shockby an average of 7 s. Users activated a familiar AED 4 s faster than an unfamiliar one and placed the electrodes 5 s more quickly. Furthermore, from the shock advice to shock initiation, it took longer to use the unfamiliar model. Although Lei et al.7 did not find significant differences in the times to the first defibrillation between a known and an unknown AED, similar to our study, they noted differences in the times when the AED was turned on and when the AED advised defibrillation, as well as in the time to restart chest compressions. Survival in OHCA is also influenced by the duration of interruptions in chest compressions during CPR, which occur in favor of AED use; the shorter the interruption, the better the resuscitation outcome.23 Stærk et al.8 in a related simulation study conducted among hospital ward staff on duty (physicians, nurses, the cardiac arrest team) found several other challenges in operating the AED, including failed shock delivery and inadequate placement of the electrodes. Many of the challenges were related to insufficient training with different AED models compared to the AED available in the clinical setting and lacking training of opening and turning on the AED, i.e., contextual skills in operating the AED.
We identified technical characteristics that influenced the time to shock. These features include the AED cover, electrode features, button features, and instructions. Comments from user interviews support previous findings regarding device design. Lei et al.7 found that the time to turn on AED was longer when an AED was stored in a bag rather than readily accessible. Some participants in our study expressed confusion due to the AEDs being kept in bags, as one noted: “This bag bothered me a little. I spent a long time.” (U47SK2). In contrast, an AED in a bag can be an advantage if the AED needs to be picked up and brought to the scene of a cardiac arrest, as would happen in real life. Percival et al.9 identified challenges such as opening the AED cover, the power button being not visible, and various technical characteristics of the electrodes that complicated the handling of the AED. However, consistent design elements across different models, such as the power button, shock button, and electrodes, as well as similar operational modes, were also noted as helpful in using an unfamiliar AED training model. Yeung et al.24 in their systematic review emphasized that features of AED can have an impact on its use and further research should be directed to making devices user-friendly and robust to untrained layperson. In addition to technical features, participants in our study mentioned that different voices and visual instructions were factors that hindered their use of an unfamiliar AED model. We noticed that more than half of the participants in our study, when they used an unfamiliar AED, followed the voice instructions. They did not listen to the instructions when using a familiar AED. Conversely, audio and visual instructions were evaluated as significant aids in managing the unfamiliar training model of the AED. Other studies have also shown that voice guidance assists laypersons in recognizing cardiac arrests, performing CPR, and using AEDs. AED voice instructions are crucial in helping laypeople feel more confident and in control.25 However, adherence to these instructions could also increase the time to shock. If the AED user focuses on the voice instructions, it may prolong the pauses during chest compressions, potentially extending them beyond the recommended duration.5
Our simulation took place on the same day, immediately following the CPR training sessions. We conducted it immediately after the training, as we wanted that rescuer to compare the feelings when using AEDs. We found that use of an unfamiliar AED model during CPR causes additional negative emotions such as stress, panic, and confusion to the user. We assume that in the event of actual resuscitation, stress would further increase when using an unfamiliar AED. The results of related research20, 21 also show that AED skills are maintained for up to a year or more, so we assume that our results would be the same after such a time. In general, stress reduces the effectiveness of CPR.14 Numerous studies3, 7, 9, 14 have confirmed the influence of prior training on the quality of CPR performance and in reducing stress levels among rescuers. Even brief training can be helpful in improving speed of shock delivery and electrode pad placement.26 Thirty-four interviewees in our research emphasized the importance of prior knowledge as an important factor that helped them use an unfamiliar AED. It is crucial for laypersons to be familiar with their AED in an actual OHCA situation to ensure faster and more confident use, which in turn makes the process easier and less stressful. One possible way to better prepare lay people for the real situation of resuscitation is to include at least two AED training models in the training process. If this is not feasible, using a video or image presentation of several AED models could serve as a viable alternative.
Limitations
This study only compared times and experiences with familiar and unfamiliar AEDs. A more in-depth analysis could involve comparing individual AED models and incorporating multiple teaching models. Additionally, the study was conducted in a simulated environment, which means the time and emotional experiences may differ from those in actual cases. However, simulation is increasingly regarded as an accepted tool for evaluation while performance markers in simulator-based studies show a high agreement with findings in real cases.24 We attempted to mitigate the risk of bias in learning thorough the three different tests through the order of tests (unfamiliar, familiar and unfamiliar). In comparing times, we only considered the duration of actual AED use by the experimenter, subtracting any time accounted for by the software of the AED training models, as this varied between individual AEDs. These could change the times of actual use of AEDs in a real situation. Results and opinions with an unfamiliar AED could be different if the participants had not just used a familiar AED. The sample included people who voluntarily attended a CPR course with an AED and wanted to participate in the research. We cannot generalize the sample to the population. Due to the explorative nature of the study, it was not based on a sample size calculation, the sample size was limited. There is indirectness in the comparisons between the previously reported stress identified in CPR and the findings of stress using and AED.
Conclusion
The findings suggest that AED design and familiarity with different AED designs may affect performance by laypersons. To improve user confidence, it would be useful to familiarize users with a variety of AED models as part of training initiatives. Understanding the impact of AED familiarity on rescuer’s response can guide CPR training strategies and improve outcomes for OHCA. As more AED models become available to the public, the user-friendliness of AEDs may also be improved. It is beneficial for AED manufacturers to consider the results of research when developing new models.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
CRediT authorship contribution statement
Damjan Slabe: Writing – review & editing, Methodology, Investigation, Conceptualization. Žiga Metelko: Writing – original draft, Methodology. Eva Dolenc Šparovec: Writing – review & editing, Writing – original draft, Methodology, Investigation, Formal analysis, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resplu.2024.100758.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Yan S., Gan Y., Jiang N., et al. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Crit Care. 2020;24:61. doi: 10.1186/s13054-020-2773-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bircher N.G., Chan P.S., Xu Y. Delays in cardiopulmonary resuscitation, defibrillation, and epinephrine administration all decrease survival in in-hospital cardiac arrest. Anesthesiology. 2019;130:414–422. doi: 10.1097/ALN.0000000000002563. [DOI] [PubMed] [Google Scholar]
- 3.Mosesso V.N., Shapiro A.H., Stein K., Burkett K., Wang H. Effects of AED device features on performance by untrained laypersons. Resuscitation. 2009;80:1285–1289. doi: 10.1016/j.resuscitation.2009.07.016. [DOI] [PubMed] [Google Scholar]
- 4.Cummins R.O. From concept to standard-of-care? Review of the clinical experience with automated external defibrillators. Ann Emerg Med. 1989;18:1269–1275. doi: 10.1016/S0196-0644(89)80257-4. [DOI] [PubMed] [Google Scholar]
- 5.Müller M.P., Poenicke C., Kurth M., et al. Quality of basic life support when using different commercially available public access defibrillators. Scand J Trauma Resusc Emerg Med. 2015;23 doi: 10.1186/s13049-015-0123-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fleischhackl R., Losert H., Haugk M., et al. Differing operational outcomes with six commercially available automated external defibrillators. Resuscitation. 2004;62:167–174. doi: 10.1016/j.resuscitation.2004.03.018. [DOI] [PubMed] [Google Scholar]
- 7.Lei C.Y., Qin H.W., Dong X.J., You J.L., Zhang L. Layperson’s performance on an unconversant type of AED device: a prospective crossover simulation experimental study. World J Emerg Med. 2022;13:98–105. doi: 10.5847/WJEM.J.1920-8642.2022.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stærk M., Lauridsen K.G., Niklassen J., Nielsen R.P., Krogh K., Løfgren B. Barriers and facilitators for successful AED usage during in-situ simulated in-hospital cardiac arrest. Resusc Plus. 2022;10 doi: 10.1016/j.resplu.2022.100257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Percival N.B., Pearson A., Jones J., Wilkins M., Caird J.K. Ease of use of Automated External Defibrillators (AEDs) by older adults. Proc Hum Factors Ergon Soc Annual Meeting. 2012;56:906–910. doi: 10.1177/1071181312561194. [DOI] [Google Scholar]
- 10.Park H.J., Jeong W.J., Moon H.J., et al. Factors associated with high-quality cardiopulmonary resuscitation performed by bystander. Emerg Med Int. 2020;2020:1–6. doi: 10.1155/2020/8356201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Takei Y., Nishi T., Matsubara H., Hashimoto M., Inaba H. Factors associated with quality of bystander CPR: The presence of multiple rescuers and bystander-initiated CPR without instruction. Resuscitation. 2014;85:492–498. doi: 10.1016/j.resuscitation.2013.12.019. [DOI] [PubMed] [Google Scholar]
- 12.Riggs M., Franklin R., Saylany L. Associations between cardiopulmonary resuscitation (CPR) knowledge, self-efficacy, training history and willingness to perform CPR and CPR psychomotor skills: a systematic review. Resuscitation. 2019;138:259–272. doi: 10.1016/j.resuscitation.2019.03.019. [DOI] [PubMed] [Google Scholar]
- 13.Dolenc Šparovec E., Slabe D., Eržen I., Kovačič U. Evaluation of a newly developed first aid training programme adapted for older people. BMC Emerg Med. 2023;23:134. doi: 10.1186/s12873-023-00907-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vincent A., Semmer N.K., Becker C., Beck K., Tschan F., Bobst C., et al. Does stress influence the performance of cardiopulmonary resuscitation? a narrative review of the literature. J Crit Care. 2021;63:223–230. doi: 10.1016/j.jcrc.2020.09.020. [DOI] [PubMed] [Google Scholar]
- 15.Slabe D., Oven A. Evaluation of Slovenian occupational therapists’ theoretical knowledge and stress levels connected with providing cardiopulmonary resuscitation. INQUIRY: J Health Care Organ Provision Financ. 2020;57 doi: 10.1177/0046958020963683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hansen C.M., Rosenkranz S.M., Folke F., et al. Lay bystanders’ perspectives on what facilitates cardiopulmonary resuscitation and use of automated external defibrillators in real cardiac arrests. J Am Heart Assoc. 2017;6 doi: 10.1161/JAHA.116.004572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Villalobos F., Del Pozo A., Rey-Reñones C., et al. Lay people training in CPR and in the use of an automated external defibrillator, and its social impact: a community health study. Int J Environ Res Public Health. 2019;16 doi: 10.3390/ijerph16162870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cheng A., Kessler D., Mackinnon R., et al. Reporting guidelines for health care simulation research: extensions to the CONSORT and STROBE statements. Simul Healthc. 2016;11:238–248. doi: 10.1097/SIH.0000000000000150. [DOI] [PubMed] [Google Scholar]
- 19.Olasveengen T.M., Semeraro F., Ristagno G., et al. European Resuscitation Council Guidelines 2021: basic life support. Resuscitation. 2021;161:98–114. doi: 10.1016/j.resuscitation.2021.02.009. [DOI] [PubMed] [Google Scholar]
- 20.Christenson J., Nafziger S., Compton S., et al. The effect of time on CPR and automated external defibrillator skills in the Public Access Defibrillation Trial. Resuscitation. 2007;74:52–62. doi: 10.1016/j.resuscitation.2006.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beckers S.K., Fries M., Bickenbach J., et al. Retention of skills in medical students following minimal theoretical instructions on semi and fully automated external defibrillators. Resuscitation. 2007;72:444–450. doi: 10.1016/j.resuscitation.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 22.Elo S., Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62:107–115. doi: 10.1111/j.1365-2648.2007.04569.x. [DOI] [PubMed] [Google Scholar]
- 23.Valenzuela T.D., Roe D.J., Cretin S., Spaite D.W., Larsen M.P. Estimating effectiveness of cardiac arrest interventions. Circulation. 1997;96:3308–3313. doi: 10.1161/01.CIR.96.10.3308. [DOI] [PubMed] [Google Scholar]
- 24.Yeung J., Okamoto D., Soar J., Perkins G.D. AED training and its impact on skill acquisition, retention and performance–a systematic review of alternative training methods. Resuscitation. 2011;82:657–664. doi: 10.1016/j.resuscitation.2011.02.035. [DOI] [PubMed] [Google Scholar]
- 25.Shimamoto T., Nishiyama C., Ohura T., Kawamura T., Iwami T. Psychological conflicts in bystander cardiopulmonary resuscitation for out-of-hospital cardiac arrest. Int J First Aid Educ. 2020;3:10–21. doi: 10.21038/ijfa.2020.0201. [DOI] [Google Scholar]
- 26.Mitchell K.B., Gugerty L., Muth E. Effects of brief training on use of automated external defibrillators by people without medical expertise. Human Factors. 2008;50:301–310. doi: 10.1518/001872008X250746. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.