Summary
The double burden of malnutrition (DBM) is a significant public health issue in South and Southeast Asia (SA and SEA). This study aimed to assess the impact of using local and regional ethnicity-specific anthropometric references versus international references on the prevalence of DBM in these regions.
A narrative review of DBM prevalence using local versus international standards was conducted. Additionally, deidentified datasets from India and Indonesia were analyzed to evaluate the effectiveness of different growth standards in identifying DBM. Anthropometric Z-scores were compared, and sensitivity, specificity, and positive predictive value (PPV) were calculated.
WHO standards had the lowest specificity for identifying short stature in India and Indonesia. BMI-for-age charts using WHO Growth Reference (2007) had lower sensitivity and higher specificity for metabolic risk. Local references showed lower stunting and higher overweight or obesity prevalence. International standards overestimated stunting and underestimated obesity, leading to misclassification and missed cases of metabolic risk.
Funding
None.
Keywords: Double burden, Southeast Asia, Malnutrition, Local, Regional, Anthropometry
Search strategy and selection criteria.
For identifying studies reporting double burden of malnutrition using international versus local references or standards, we conducted a literature search using following electronic databases for papers published in English: Medline via OvidSP, Scopus, Global Health via OvidSP and Web of Science, from 2007 (as WHO standards were published in 2006) till 2023. The search used the following keywords/MeSH terms: 1) overnutrition (OR overweight OR obesity), 2) undernutrition (OR stunting OR wasting OR thinness OR underweight), 3) malnutrition, 4) double burden (dual OR double OR burden), 5) prevalence (OR number OR incidence OR survey), 6) adults (OR mother OR father OR parent), 7) infants, children and adolescents (OR school-age OR preschool OR under five or infants), 8) countries (ASEAN OR South East Asia OR Asia OR LMIC OR Brunei Darussalam OR Cambodia OR Indonesia OR Lao PDR OR Malaysia OR Myanmar OR Philippines OR Singapore OR Thailand OR Vietnam). We combined the results from 1) to 7) AND then combined the results with each of the countries' items in number 8). We also identified papers through hand searching of the reference lists of journals.
Introduction
According to the World Health Organisation (WHO), malnutrition refers to both deficiencies or excesses in nutrient intake, imbalance of essential nutrients, or impaired nutrient utilization. Further, the double burden of malnutrition (DBM) is defined as the coexistence of both under and overnutrition in the same population across the life course.1,2 A report on trends in child malnutrition suggests that Africa and Asia bear the greatest share of all forms of malnutrition; in 2019 almost half or more children with stunting/wasting or overweight lived in Asia.3 Recently, DBM has become a major public health problem, especially in low- and middle-income countries (LMIC) of South Asia (SA) and South East Asia (SEA) region.4 For example, the most recent Multiple Indicator Cluster Survey (MICS) conducted in Thailand during 2022, reported an increase in the prevalence rates among children under five (0–59 months) for stunting (12.5% vs 11.9%), and overweight or obesity (10.9% vs 6.9%) as compared to 2005-06.5,6 Several reasons such as rapid economic transition, demographic changes, urbanization, older maternal age, socio-economic inequality, and nutrition transition have been suggested for the increasing prevalence of DBM in SA and SEA countries.
Anthropometric parameters are the commonest method for the classification of DBM. Most studies that have reported DBM in the SA and SEA region have used international growth standards and respective cut-offs. Using international growth standards for anthropometric parameters to classify DBM in the SA and SEA region has limitations of ethnic variation, population diversity, and economic disparity. There is an underestimation of overweight or obesity and an overestimation of stunting in the population of the SA and SEA region. In a cross-sectional study on rural and urban Indian children aged 0–59 months, WHO charts overestimated stunting (14.0% vs 6.8%) and wasting (18.2% vs 9.7%) and underestimated overweight (1.0% vs 3.1%) in comparison with recent Indian references.7 In older Indian children and adolescents, WHO 2007 references classified 15.7% whereas ethnic-specific charts classified 19.1% of subjects as overweight/obese.8 DBM has a serious negative economic impact on individuals as well as populations by increasing the cost of healthcare, reducing productivity and economic growth, and perpetuating the cycle of poverty and ill health. Moreover, inaccurate classification of DBM estimates has potential consequences of ineffective resource allocation of public health programs.
Thus, to assess the impact of the use of local/regional ethnicity-specific anthropometric references versus international standards and references on the prevalence of DBM in SA and SEA, we have focused our review and analysis on DBM in the paediatric population of SA and SEA. Our specific objectives were: 1) To perform a narrative, non-systematic review of the prevalence of double burden of malnutrition in South Asian and Southeast Asian countries using local versus international anthropometric parameters and 2) We use deidentified datasets (0–18 years) from India and Indonesia to assess predictive value of local, regional, and international growth standards or references in identifying stunting or short stature and overweight or obesity.
Methods
Datasets
We use deidentified datasets from India (SA) and Indonesia (SEA) to estimate the prevalence of stunting and overweight or obesity using various growth standards or references. The datasets included in the present study were not utilised for generating the reference data. The institutional ethics committee approved the use of deidentified data on the 20th of December 2023 (JCDC/BHR/23/045).
Indian data
Data for children of age 0–59 months were used from a previous study conducted by the author's group at a tertiary care center in Pune in the period from 2017 to 2022.9 In brief, records of children on whom decimal age, sex and anthropometric parameters were available (height and weight) were included. Further, deidentified records on healthy children coming for vaccinations and children who were diagnosed with a growth-related disorder were also included. Records with incomplete data (on age and anthropometric parameters) were excluded. Height is measured at our centre using a Leicester Height Meter (Child Growth Foundation, UK, accuracy of 0.1 cm) and for children under 2 years of age, recumbent length is measured using an infantometer (Shreeyash electro medicals, Infantometer, India, accuracy of 0.1 cm). Weight is measured using electronic weighing scales (Salter, India) with an accuracy of ±50 g.10 Body mass index (BMI) is calculated as kilograms/meter2.11 An adaptation of the European Society for Pediatric Endocrinology (ESPE) classification of growth disorders12 was used to classify children into different groups of which children with only malnutrition-related disorders (stunting and overweight or obese) were included. Rest of the records (n = 62) were excluded. A total of 2126 children were included in the final data analysis.
Data on 5–18 year olds were collected from a study that was part of a multicentre (6 centres), cross sectional, observational school-based study conducted from July 2016 to October 2017. Three of the six centres were randomly selected and measurement of waist circumference, random blood glucose and blood pressure were performed on all children of age group 9–18 years (n = 1572).13 We also included records of children from the same age group that visited our tertiary care centre in the same period for evaluation by a paediatric endocrinologist for pathological short stature (n = 177). As the available reference dataset for SA region (here, Pakistani) only included girls up to age 15 years, the final data analysis was performed on 875 girls aged 9–15 years (177 with pathological short stature plus 698 out of 1572 from school study after excluding 874 due to the age and sex criteria).14 Height, weight and BMI were measured as mentioned earlier. Waist circumference (WC) was measured by National Health and Nutrition Examination Survey (NHANES) standard protocol with the child standing using a stretch-resistant tape with constant 100 g tension maintained through the use of a special indicator buckle. The tape was applied horizontally above the upper lateral border of right ileum, at the end of expiration and was recorded to the nearest 0.1 cm. Blood pressure was measured on the right arm with the child lying down quietly. Measurements were made by auscultation with a sphygmomanometer and a cuff appropriately sized for the arm size of the participant.8 Random blood glucose (RBG) estimation was performed using a glucometer (Glucometer Elite XL; Bayer Corp, Mishawaka, Ind). The ring finger of the nondominant hand was used to collect blood samples. A blood drop was placed on a reagent strip and inserted into the blood glucose monitoring system and the reading was recorded.13
WC > 90th percentile for age and sex or adult cut-off (males >90 cm, females >80 cm) if lower as per Indian population-specific data, systolic blood pressure (SBP) of greater than 130 mmHg and/or diastolic blood pressure (DBP) of greater than 85 mmHg and RBG of more than 130 mg/dL was considered a metabolic risk factor.15,16
Indonesian data
The data for Indonesian children aged 6–18 years was obtained from the Indonesia Family Life Survey fifth wave (IFLS 5) conducted in 2014 that involved 321 enumeration areas within 13 provinces. IFLS is a large-scale, stratified random sampling, longitudinal survey designed to collect data on the lives of individuals and families across Indonesia.
Height was measured using the Shorr Model 420 tools, while Seca Model 770 scales determined weight. Children older than two had their standing height recorded. Of the 14,956 records, we excluded 4795 as their age was less than 6 years (Reference data for the SEA region, here Thailand, were available from 6 years onwards).17 A subset analysis was performed on 2526 subjects on whom data for blood pressure and blood sugar concentrations was available.
Classification of malnutrition
All anthropometric parameters were converted to Z-scores using WHO standards (0–59 months) and WHO references (6–18 years) published in year 2006–07. Similarly, they were also converted to Z-scores using growth references from SA and SEA (Indian, Pakistani, Thai, and Indonesian) (Table 1).14,17, 18, 19, 20, 21, 22, 23 Malnutrition for children from birth to 59 months was classified using WHO classification of nutritional status.24 Stunting was defined as length/height for age less than −2 standard deviation and overweight or obesity as BMI-for-age more than +2 standard deviation. For children of age 5–18 years, short stature was defined as a height <3rd percentile or two or more standard deviations (SD) below the mean for children of the same sex and age.25 Further, WHO defines overweight and obesity as abnormal or excessive fat accumulation that may impair health. Objectively, childhood overweight or obesity is defined as a body mass index greater than or equal to the 85th percentile for age and sex, according to standardized growth charts,26 however, each reference dataset provides its own cut-off (For example: the Indian Academy of Paediatrics (IAP) defines BMI more than 23 kg/m2 adult equivalent as overweight while WHO defines >+1SD above median BMI as overweight). The cut-offs used in the present study are as per the reference datasets mentioned in Table 1. No organization/individual funders have funded this study.
Table 1.
Reference datasets used to compute Z-scores in the present study.
| Reference dataset | Country-specific | From same region | From different region | International |
|---|---|---|---|---|
| Indian data | ||||
| 0–59 months | Synthetic Indian Growth references18 | The 2022 Pakistani references from birth to 60 months for length/height, weight and body mass index19 | Indonesian National Synthetic Growth Charts20 | WHO 2006 growth standards21 |
| 9–15 year old girls | Revised Indian Academy of Pediatrics growth charts 201522 | A comparison of international and national references to measure the prevalence of stunting in Pakistani school-age girls.14 | Indonesian National Synthetic Growth Charts20 | WHO growth reference for school-aged children and adolescents.23 |
| Indonesian data | ||||
| 6–18 years | Indonesian National Synthetic Growth Charts20 | The 2021 Thai reference from 6 to 19 years for weight and height17 | Revised Indian Academy of Paediatrics growth charts 201522 | WHO growth reference for school-aged children and adolescents.22,23 |
Statistical analysis
Data were analysed using SPSS 26.0 for Windows (IBM SPSS, Bangalore, India). Descriptive statistics were computed for normal and children diagnosed with growth-related disorders under age of 59 months. Pearson correlation coefficient was used to assess the correlation between the Z-scores calculated using various reference datasets. A comparison of anthropometric Z-scores calculated using various reference datasets was made using a paired sample t-test. Sensitivity, specificity, positive predictive value (PPV), and negative predictive values (NPV) for identifying malnutrition by various reference criteria were calculated. p value less than 0.05 was considered significant.
Results
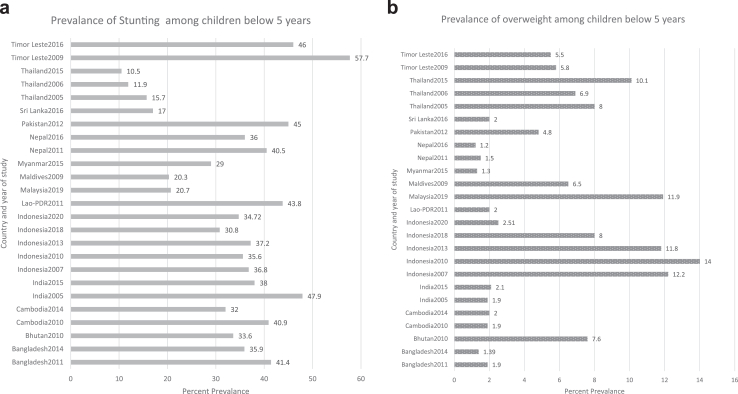
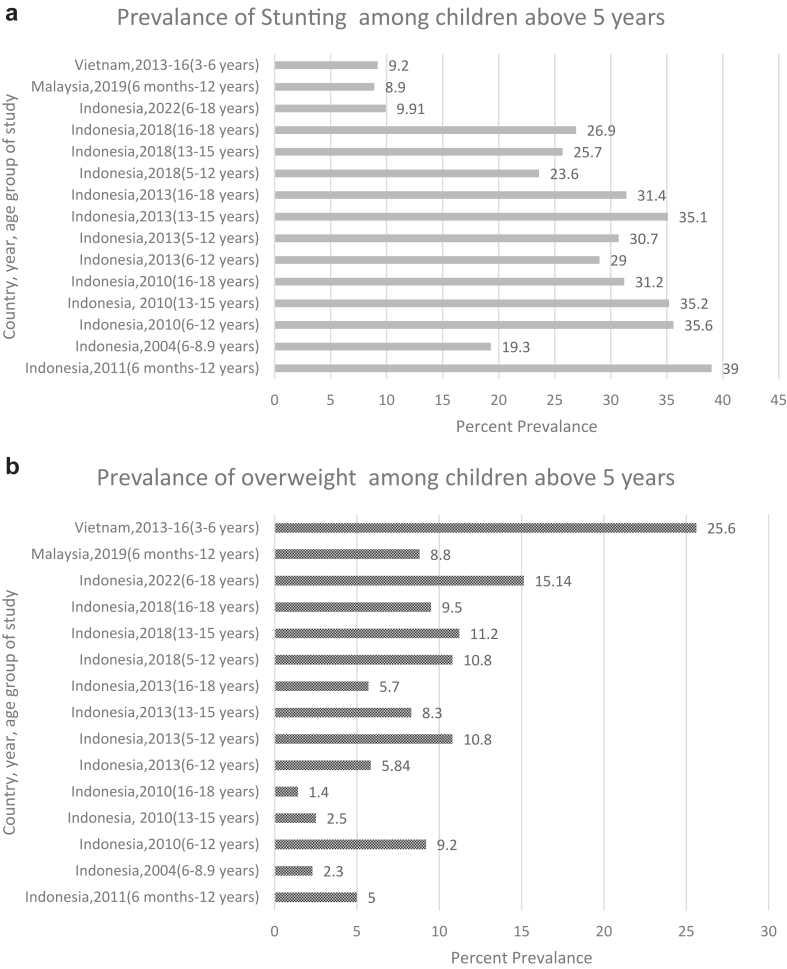
Figs. 1a and b, and 2a, b27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42 illustrate various studies from the SA and SEA regions describing the DBM using WHO reference dataset. Prevalence of stunting and obesity ranges from 33.6% to 47.9% and 1.3–7.6% in SA region with the exception of one Sri Lankan study which reports lower prevalence of stunting (17.0%). The prevalence of stunting in SEA ranged from 8.9% in Malaysia to 46.0% in Timor-Leste while the prevalence of obesity varied from 1.9% in Cambodia to 25.6% in Vietnam. The prevalence of stunting was lower by local anthropometric reference datasets of SA and SEA regions as compared to international references like WHO or Centers for Disease Control and Prevention (CDC) (Table 2).13,14,32,36,43, 44, 45, 46, 47, 48, 49 Also, the prevalence of overweight/obesity was higher in SA and SEA regions by local anthropometric references except for one study each from Thailand (4.3% vs 3.0%) and Pakistan (14.2% vs 13.9%).
Fig. 1.
a) Prevalence of stunting in children under 60 months of age. b): Prevalence of overweight/obese in children under 60 months of age. Footnote: References for figure [Bangladesh 2011, Bangladesh 2014, Bhutan 2010, Cambodia 2010, Cambodia 2014, India 2005, India 2015, Maldives 2009, Nepal 2011, Nepal 2016, Pakistan 2012, Srilanka 2016, Timor Leste 2009, Timore Leste 2016],26,27 Indonesia 2007,28 Indonesia 2010,29 Indonesia 2013,30 Indonesia 2018,31 Indonesia 2020,32 Malaysia 2019,33 Thailand 2006,34 Thailand 2015.35,36
Fig. 2.
a) Prevalence of stunting in children over 5 years age. b): Prevalence of overweight/obese in children over 5 years age. Footnote: References for figure Indonesia 2018,31 Indonesia 2011,37 Indonesia 2004,38 Indonesia 2013,39 Indonesia 2013,40 Malaysia 2019,41 Vietnam 2013-16.42
Table 2.
Reported Prevalence of double burden in South Asian and South East Asian countries using local and international growth references/standards.
| Study | Parameter studied | Country/region | International | Local/Ethnic specific |
|---|---|---|---|---|
| The double burden of malnutrition in Vietnamese school-aged children and adolescents: a rapid shift over a decade in Ho Chi Minh City36 | Overweight/obesity | Vietnam/SEAR | 5.2% using WHO 2006–07, 4% using (IOTF) | 10.1% (IOTF for Asian) |
| Using the National Indonesian Growth Chart to assess short stature and obesity in urban schoolchildren in Surakarta, Indonesia: comparisons to the WHO 2007 and CDC 2000 Growth Charts43 | Stunting Overweight Obesity |
Indonesia/SEAR | 9.91% (WHO), 11.62% (CDC) 15.14% (WHO), 17.23% (CDC) 10.15% (WHO), 5.07% (CDC) |
0.39% 15.96% 11.77% |
| Indonesian National Growth Reference Charts Better Reflect Height and Weight of Children in West Java, Indonesia, than WHO Child Growth Standards32 |
Stunting Overweight Obesity |
Indonesia/SEAR | 34.72% 2.51% 1.15% |
10.80% 2.08% 0.78% |
| Field Testing of Synthetic Growth Charts in 1–60-Month-Old Indian Children44 | Stunting Obesity |
India/SAR | 14% 1% |
6.8% 3.1% |
| Field Testing of IAP2015 Charts45 | Stunting Obesity |
India/SAR | 4.6–25% 1–6.5% |
2.5–14.8% 1.2–9.6% |
| A comparison of international and national references to measure the prevalence of stunting in Pakistani school age girls14 | Stunting | Pakistan/SAR | WHO-17.49% CDC- 22.72% |
4.94% |
| Comparison of Prevalence of Nutritional Status of Thai Children in the First 2 Years of Life Using National and International Growth Charts46 | Stunting Overweight |
Thailand/SEAR | 17–18% 4.3% |
11% 3.0% |
| Development of Growth Charts of Pakistani Children Aged 4–15 Years Using Quantile Regression: A Cross-sectional Study47 | Stunting Obesity |
Pakistan/SAR | 20.6% 14.2% |
2.7–3.3% 11.6–13.9% |
| Predictive value of WHO vs IAP BMI charts for identification of metabolic risk in Indian children and adolescents13 |
Obesity | India/SAR | 15.7% | 19.1% |
| Measuring obesity among school-aged youth in India: A comparison of three growth references 48 | Obesity Overweight |
India/SAR | 4.95% 11.55% |
5.01% 12.87% |
| Indonesian Children and Adolescents' Body Mass Index: WHO and Asia–Pacific Classification49 | Overweight/obese | Indonesia/SEAR | 5.4% | 12% |
Footnote: IOTF, International Obesity Task Force; CDC, Center for Disease Control and Prevention; WHO, World health organisation; SAR, South Asia Region; SEAR, South East Asia Region; IAP, Indian Academy of Pediatrics.
For the second objective, analysis was performed and presented separately for the two datasets and age groups (0–59 months and 6–18 years). For assessing DBM, stunting was considered for undernutrition, and overweight or obesity for overnutrition. For diagnosing stunting in children of age group 0–59 months, the reference datasets from SA and SEA region had higher specificity than WHO growth standards with comparable sensitivity (except Pakistani reference data, sensitivity of 40.7%) while only Indian references had better sensitivity than the rest of the growth references (86.2% vs 62.0–68.9%); the specificity was comparable. Similarly, for older children, the WHO growth reference (2006–2007) had the lowest sensitivity and specificity in identifying obesity and stunting respectively. With respect to other growth references from the SA and SEA region, all had similar accuracy in identifying these disorders with the exception of the Indonesian growth reference data which had lower sensitivity in identifying stunting as compared to the rest (77.4% vs 93.7–95.4%).
Indian data
Children of age 0–59 months
We studied a subset of 2126 children from previous studies (Birth-59 months) of which 1119 records (52.6%) were boys and 1007 (47.4%) were girls. A total of 243 (11.4%) were diagnosed under the broad category of growth failure and 29 (1.4%) were observed to be more obese. The descriptives of the under 5 children are illustrated in Table 3.
Table 3.
Comparison of anthropometric characteristics of healthy children with children diagnosed with growth disorder (of age 0–59 months from the Indian dataset).
| Parameter | Healthy (n = 1854) |
With diagnosed growth disorder (n = 272) |
|---|---|---|
| Mean ± Std. deviation | Mean ± Std. deviation | |
| Age in Months | 19.4 ± 17.7 | 34.6 ± 16.5 |
| Height in cm | 75.1 ± 17.9 | 77.8 ± 12.0 |
| Weight in Kg | 8.9 ± 4.0 | 9.8 ± 4.5 |
| Body Mass Index Kg/m2 | 14.6 ± 2.3 | 15.6 ± 3.5 |
| Indian Height-for-Age Z score | −0.3 ± 1.4 | −3.5 ± 2.0 |
| Indian BMI-for-Age Z score | −0.2 ± 1.6 | 0.2 ± 2.4 |
| WHO Height-for-Age Z score | −0.8 ± 1.6 | −4.2 ± 2.3 |
| WHO BMI-for-Age Z score | −0.9 ± 1.4 | −0.3 ± 2.4 |
| Pakistani Height-for-Age Z score | −0.2 ± 0.9 | −1.7 ± 1.5 |
| Pakistani BMI-for-Age Z score | −0.4 ± 0.7 | −0.1 ± 1.1 |
| Indonesian Height-for-Age Z score | −0.7 ± 1.5 | −3.6 ± 2.0 |
| Indonesian BMI-for-Age Z score | −0.9 ± 1.5 | −0.7 ± 2.4 |
Footnote- Std, standard; BMI, body mass index; WHO, World Health Organisation.
Correlation analysis of the height-for-age Z-scores and BMI-for age Z-scores using various pairs (Indian/WHO/Pakistani/Indonesian) are illustrated in Table 4. On performing paired samples t-test, there were significant differences in each pair of the height-for-age Z-score as well as the BMI-for-age Z-scores. (p < 0.05 for all). The sensitivity, specificity, PPV and NPV for detecting short stature and obesity are illustrated in Table 5.
Table 4.
Paired samples t-test and Pearson Correlation analysis for height and BMI Z-scores using various reference data for children of age 0–59 months.
| Paired samples correlations | Correlation coefficient between pairs tested (r) | Sig. |
|---|---|---|
| Indian Height-for-Age Z score & WHO Height-for-Age Z scorea | 0.9 | <0.01 |
| Indian Height-for-Age Z score & Pakistani Height-for-Age Z scorea | 0.8 | <0.01 |
| Indian Height-for-Age Z score & Indonesian Height-for-Age Z scorea | 0.9 | <0.01 |
| WHO Height-for-Age Z score & Pakistani Height-for-Age Z scorea | 0.8 | <0.01 |
| WHO Height-for-Age Z score & Indonesian Height-for-Age Z scorea | 0.9 | <0.01 |
| Pakistani Height-for-Age Z score & Indonesian Height-for-Age Z scorea | 0.8 | <0.01 |
| Indian BMI-for-Age Z score & WHO BMI-for-Age Z scorea | 0.9 | <0.01 |
| Indian BMI-for-Age Z score & Pakistani BMI-for-Age Z scorea | 0.9 | <0.01 |
| Indian BMI-for-Age Z score & Indonesian BMI-for-Age Z scorea | 0.7 | <0.01 |
| WHO BMI-for-Age Z score & Pakistani BMI-for-Age Z scorea | 0.9 | <0.01 |
| WHO BMI-for-Age Z score & Indonesian BMI-for-Age Z scorea | 0.8 | <0.01 |
| Pakistani BMI-for-Age Z score & Indonesian BMI-for-Age Z scorea | 0.7 | <0.01 |
Footnote: WHO, World Health Organisation 2006–07; BMI, body mass index.
Statistically significant difference between pairs compared by paired sample t-test with p < 0.05.
Table 5.
Performance of various reference data in identifying malnutrition (stunting and overweight/obese) in Indian children aged 0–59 months (n = 2126).
| Parameter | WHO | Indian | Pakistani | Indonesian |
|---|---|---|---|---|
| Stunting | ||||
| Sensitivity | 98.3 | 95.8 | 40.7 | 93.8 |
| Specificity | 79.3 | 90.6 | 96.9 | 83.3 |
| PPV | 38 | 56.8 | 63 | 42.1 |
| NPV | 99.7 | 99.4 | 92.6 | 99 |
| Obesity | ||||
| Sensitivity | 68.9 | 86.2 | 62 | 65.5 |
| Specificity | 99.1 | 96.7 | 99.9 | 99.5 |
| PPV | 54 | 26.8 | 94.7 | 67.8 |
| NPV | 99.5 | 99.8 | 99.4 | 99.5 |
Footnote: WHO, World Health Organisation; PPV, positive predictive value; NPV, negative predictive value.
Children aged 9–15 years
We studied 875 girls from 9 to 15 years, of which, 597 (68.2%) were records on apparently healthy girls. A total of 177 (20.2%) had been diagnosed under the broad category of pathological short stature (Growth hormone deficiency, GHD), Multiple Pituitary Hormone Deficiency (MPHD), Turner syndrome and chronic kidney disease) and 101 (11.5%) were identified to have at least one parameter of metabolic risk. The descriptive statistics of the study group are illustrated in Table 6.
Table 6.
Comparison of anthropometric characteristics of healthy children with children diagnosed with growth disorder (of age 9–15 years from the Indian dataset).
| Parameter | Healthy (n = 597) |
With diagnosed growth disorder (n = 278) |
|---|---|---|
| Mean ± Std. deviation | Mean ± Std. deviation | |
| Age in years | 11.5 ± 1.4 | 11.6 ± 1.5 |
| Height in cm | 141.5 ± 9.5 | 132.0 ± 19.1 |
| Weight in kg | 33.7 ± 8.3 | 33.4 ± 16.7 |
| Body Mass Index Kg/m2 | 16.6 ± 3.1 | 17.8 ± 4.8 |
| Indian Height-for-Age Z score | −0.5 ± 0.9 | −1.8 ± 2.0 |
| Indian BMI-for-Age Z score | −0.5 ± 2.1 | −0.3 ± 1.5 |
| WHO Height-for-Age Z score | −0.9 ± 1.0 | −2.4 ± 2.2 |
| WHO BMI-for-Age Z score | −0.7 ± 1.4 | −0.6 ± 1.9 |
| Pakistani Height-for-Age Z score | −0.2 ± 0.8 | −1.5 ± 2.0 |
| Pakistani BMI-for-Age Z score | −0.3 ± 3.5 | −0.1 ± 1.5 |
| Indonesian Height-for-Age Z score | 0.1 ± 1.0 | −1.4 ± 2.3 |
| Indonesian BMI-for-Age Z score | −0.9 ± 5.1 | −0.6 ± 1.7 |
Footnote- Std, standard; BMI, body mass index; WHO, World Health Organisation.
The correlation between height-for-age Z-scores using various pairs (Indian/WHO/Pakistani/Indonesian) and BMI-for-age Z-scores is illustrated in Table 7. On performing a paired sample t-test, there were significant differences in each pair of the height-for-age Z-score and BMI-for-age Z-scores. The sensitivity, specificity, PPV, and NPV for detecting short stature and obesity are illustrated in Table 8.
Table 7.
Paired samples t-test and Pearson Correlation analysis for height and BMI z-scores using various reference data for girls of age 9–15 years.
| Paired samples correlations | Correlation coefficient between pairs tested (r) | Sig. |
|---|---|---|
| Indian Height-for-Age Z score & WHO Height-for-Age Z scorea | 0.9 | <0.01 |
| Indian Height-for-Age Z score & Pakistani Height-for-Age Z scorea | 0.9 | <0.01 |
| Indian Height-for-Age Z score & Indonesian Height-for-Age Z scorea | 0.9 | <0.01 |
| WHO Height-for-Age Z score & Pakistani Height-for-Age Z scorea | 0.9 | <0.01 |
| WHO Height-for-Age Z score & Indonesian Height-for-Age Z scorea | 0.9 | <0.01 |
| Pakistani Height-for-Age Z score & Indonesian Height-for-Age Z scorea | 0.99 | <0.01 |
| Indian BMI-for-Age Z score & WHO BMI-for-Age Z scorea | 0.7 | <0.01 |
| Indian BMI-for-Age Z score & Pakistani BMI-for-Age Z scorea | 0.9 | <0.01 |
| Indian BMI-for-Age Z score & Indonesian BMI-for-Age Z scorea | 0.9 | <0.01 |
| WHO BMI-for-Age Z score & Pakistani BMI-for-Age Z scorea | 0.6 | <0.01 |
| WHO BMI-for-Age Z score & Indonesian BMI-for-Age Z scorea | 0.5 | <0.01 |
| Pakistani BMI-for-Age Z score & Indonesian BMI-for-Age Z scorea | 0.9 | <0.01 |
Footnote: WHO, World Health Organisation 2006–07; BMI, body mass index.
Statistically significant difference between pairs compared by paired sample t-test with p < 0.05.
Table 8.
Performance of various reference data in identifying malnutrition (stunting and overweight/obese) in Indian girls aged 9–15 years (n = 875).
| Parameter | WHO | Indian | Pakistani | Indonesian |
|---|---|---|---|---|
| Stunting | ||||
| Sensitivity | 100 | 95.4 | 93.7 | 77.4 |
| Specificity | 84.9 | 100 | 100 | 100 |
| PPV | 62.7 | 100 | 100 | 100 |
| NPV | 100 | 98.8 | 98.4 | 94.5 |
| Obesity | ||||
| Sensitivity | 65.3 | 75.2 | 77.2 | 70.3 |
| Specificity | 94.5 | 93.3 | 91.1 | 93.8 |
| PPV | 74.1 | 73 | 67.8 | 73.1 |
| NPV | 91.8 | 94 | 94.3 | 92.9 |
Footnote: WHO, World Health Organisation; PPV, positive predictive value; NPV, negative predictive value.
Indonesian data
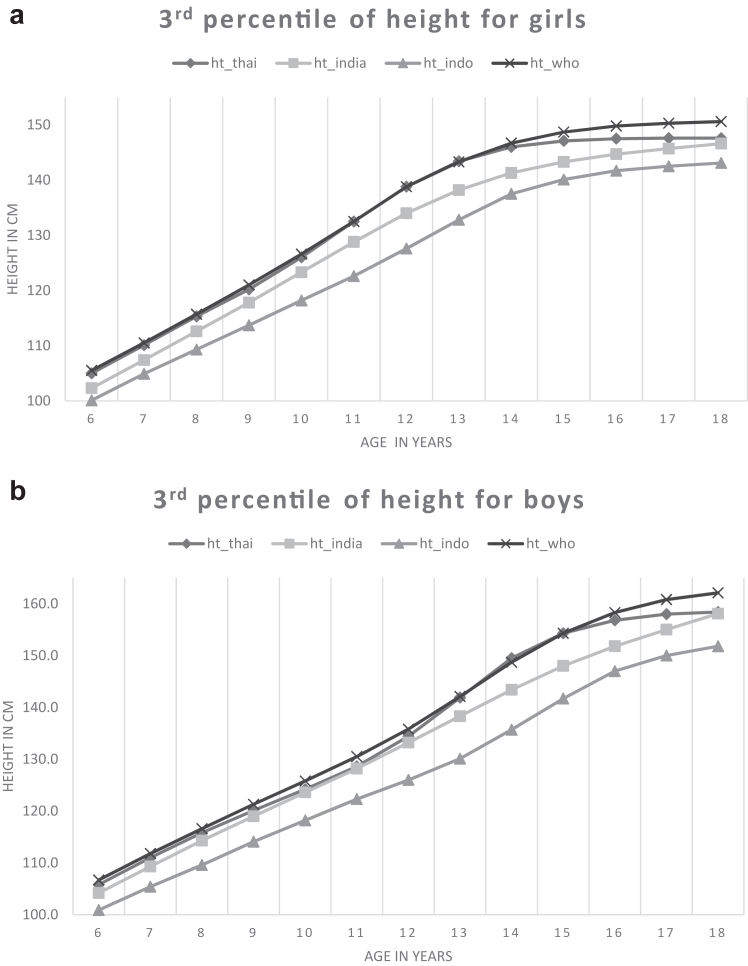
We studied anthropometric data on 10,161 records of 6–18-year-old children from Indonesia. Of these children, 5121 (50.4%) were boys and 5040 (49.6%) were girls. The mean age of the study population was 11.5 ± 3.3 years. The descriptive characteristics of the study sample are illustrated in Table 9. As the dataset was obtained from The Fifth Wave of the Indonesia Family Life Survey, etiological diagnosis of short stature was not available. We, therefore, firstly compared the 3rd percentile of height for age for both sexes using the normative data for height available from Indonesia, Thailand, India and WHO as shown in Fig. 3a and b20,22,23; the 3rd centile for height was the lowest for Indonesian reference data in both sexes.
Table 9.
Anthropometric characteristics of children from 6 to 18 yrs from the Indonesian dataset (N = 10,161).
| Parameter | Boys |
Girls |
|---|---|---|
| Mean ± Std. deviation | Mean ± Std. deviation | |
| Age (years) | 11.5 ± 3.2 | 11.5 ± 3.3 |
| Height (cm) | 138.1 ± 18.3 | 136.3 ± 15.6 |
| Weight (Kg) | 33.8 ± 13.5 | 33.7 ± 12.5 |
| BMI (kg/m2) | 16.9 ± 3.0 | 17.4 ± 3.4 |
| Indonesian height Z score | −0.2 ± 1.0 | −0.2 ± 1.0 |
| Indian height for age Z-score | −0.4 ± 1.2 | −0.7 ± 0.9 |
| WHO height Z score | −1.2 ± 1.0 | −1.3 ± 0.9 |
| Indonesian BMI Z score | −0.7 ± 1.3 | −0.5 ± 1.3 |
| Indian BMI Z score | −0.3 ± 0.9 | −0.1 ± 0.9 |
| WHO BMI Z score | −0.5 ± 1.3 | −0.4 ± 1.2 |
Footnote: STD, standard; BMI, body mass index; WHO, World Health Organisation.
Fig. 3.
a) 3rd percentile for height for girls- 6–18 years. b: 3rd percentile for height for boys- 6–18 years. Footnote: Ref.20,22,23
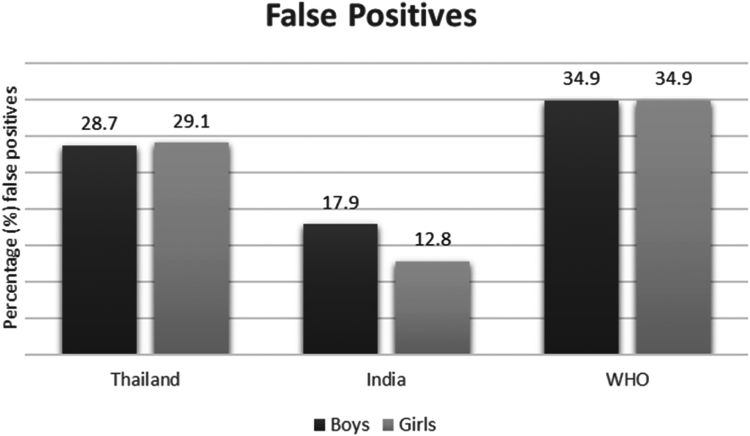
Further, the number of subjects screened as having short stature by sex in comparison with Indonesian reference data are illustrated in Fig. 4. Highest number of subjects classified as having short stature in comparison to Indonesian reference data were by WHO reference data and lowest by Indian reference data i.e. results in comparison with the Indian reference data were the closest. A subset analysis of 2526 subjects on whom data on blood pressure and fasting blood sugar were available was performed. Of these, 1237 (49%) were boys and 1289 (51%) were girls. A total of 554 (21.9%) participants were identified as having at least one positive parameter of metabolic risk (high blood pressure or high fasting blood glucose). The sensitivity, specificity, PPV and NPV for identifying metabolic risk in overweight or obese subjects is illustrated in Table 10.
Fig. 4.
False positives for short stature by sex using various reference datasets in comparison to the Indonesian reference data (n = 10,161). Footnote: The Y-axis represents % false positive subjects classified as short (Z-score < -2.0) and X-axis represents various reference datasets used to compute height Z-score. The n for boys is 5121 and girls is 5040.
Table 10.
Performance of various reference data in identifying metabolic risk in overweight/obese Indonesian children aged 6–18 years (n = 2526).
| Parameter | WHO | Indian | Thailand | Indonesian |
|---|---|---|---|---|
| Sensitivity | 15.8 | 25.4 | 10.1 | 5.9 |
| Specificity | 91.6 | 86.4 | 96.6 | 98.3 |
| PPV | 34.4 | 34.7 | 45.5 | 50.7 |
| NPV | 79.4 | 80.4 | 79.2 | 78.8 |
Footnote: WHO, World Health Organisation; PPV, positive predictive value; NPV, negative predictive value.
Discussion
Our literature review suggests that international anthropometric reference datasets overestimate the prevalence of stunting while normalizing overweight or obesity as compared to local anthropometric reference datasets. Data analysis on the Indian and Indonesian datasets suggests that the WHO growth standards and references yield the lowest specificity (highest false positives) in identifying short stature for both India (SA region) and Indonesia (SEA region). Our results on Indian data also suggest that BMI-for-age charts calculated using WHO growth references have lower sensitivity and higher specificity in identifying metabolic risk, particularly in children aged 6–18 years. We also found that for 6–18-year-old Indian children, after the local growth reference dataset, the dataset from the same region (Pakistan) had much better predictive value than the international references (WHO) for both stunting and obesity. However, the same result could not be replicated in Indian children from birth to 5 years and Indonesian children aged 6–18 years for overweight or obesity. This may be as a result of using BMI adult equivalent cut-offs of 23 and 27 to define overweight and obesity in Indian children and variation in the method of producing the growth charts. (LMS, quantile regression, etc).
As per the WHO statement of 2019, prevalence of stunting and obesity in SA and SEA are 31.7% and 24.7% (stunting) and 2.5% and 7.5% (obesity) respectively.3 The disadvantage of using WHO charts is that they are likely to over diagnose underweight and stunting in a large number of apparently normal children in developing countries.50 Concerns regarding adoption of WHO 2006 standards have been expressed by many authors from Indonesia, Czechoslovakia, Malawi etc. as these standards are likely to over diagnose stunting and underweight.51 As far as India is concerned, there are many studies that have shown higher number of false positives while using WHO growth standards or references. For <59 months, difference in sensitivity of 7.2% between WHO and Indian (synthetic) cut-offs in identifying stunting have been reported.7 Another study reported no significant difference in the prevalence of underweight but found that WHO standards estimated a significantly higher prevalence of stunting in Indian children <5 years of age.52 Higher prevalence of short stature as per WHO charts (>6 years) in Indian school children has also been reported.45 Even for pathological short stature, a study on 5–18 year old Indian children reported that ninety subjects short by WHO criteria had normal stature as per the IAP criteria. Authors also report that identification of one child with a pathological cause would have required evaluation of 45 subjects classified as short by the WHO references. They concluded that the use of WHO criteria causes unwarranted work-up in a substantial number of subjects.53 A Thai study reports that fewer children, particularly girls, were classified as stunted when using national standards (11.0%) compared to international standards (17.0–18.0%).54
As data on etiological diagnosis of short stature were not available from the Indonesian dataset, we compared the 3rd percentile for height for both sexes using reference data and found that the WHO reference dataset had higher value of 3rd percentile as compared to Indonesian, Indian and Thai references. Marked mismatch exists between WHO standards/references and Indonesian height and weight data. Indonesian children of both sexes are observed to be significantly shorter and mature slightly earlier than the WHO standards or references suggest.20 Similar results have been reported by various countries. For example, anthropometric measurements of school going-girls of the Punjab (Pakistan) showed that when 3rd, 50th and 90th percentiles of weight, height and BMI were compared with WHO standards, the values were observed to be significantly lower.55 A study on growth parameters of Sri Lankan children during infancy also concluded that the WHO multicentre growth reference study data seems to be inappropriate for monitoring growth of Sri Lankan children.56 Malaysian growth charts also show that the 3rd percentile differs from the WHO by an average of approximately 4 cm, therefore, more Malaysian children were classified as stunted if the WHO growth standards were used.57 A study on length and height percentiles of children in the South-East Asian Nutrition Surveys (SEANUTS) analysed data on 14,202 children from Malaysia, Thailand, Vietnam, and Indonesia, and reports that pooled SEANUTS percentile values were found to differ from the WHO references and the study, therefore, suggested that this should be kept in mind when using WHO growth curves to assess length or height in these populations.58
The exact opposite of this has been observed in European children with growth concerns–use of WHO growth standards or references leads to a significant reclassification to normal height, potentially delaying or leading to missed diagnosis of a growth disorder.59 In a meta-analysis on studies from 55 countries involving over 11 million children of age 0–59 months, 44–48% of means were at least ±0.25 SD away from corresponding mean values in WHO standards at four or more time points. Among outliers, Europeans were generally above 0.5 SD, and Asian Indians were below −0.5 SD, suggesting inter-population differences.60 Use of an appropriate growth standard or reference is important to detect short stature and growth charts form a part of the clinical armoury for detecting diseases or conditions with short stature.61 However, inappropriately using the International charts may increase the financial burden of evaluating stunting in healthy children of LMIC from SA and SEA. Moreover, targeted government programs are being implemented in these countries to reduce the prevalence of stunting, while the children classified as stunted may be healthy short children, with growth in line with their genetic potential.
With the increasing prevalence of obesity in SA and SEA, BMI is an important screening tool predicting diseases related to obesity. As per the WHO data, noncommunicable diseases (NCDs), principally cardiovascular diseases, are responsible for 62.0% of all deaths (9 million people) in SEA.62 A meta-analysis suggests that childhood obesity is significantly and positively associated with adult systolic blood pressure (Zr = 0.11; 95% CI: 0.07, 0.14), DBP (Zr = 0.11; 95% CI: 0.07, 0.14), and tri-glycerides (Zr = 0.08; 95% CI: 0.03, 0.13), and is significantly and inversely associated with adult high density lipoprotein (Zr = −0.06; 95% CI: −0.10, −0.02). The authors concluded that childhood obesity may be a risk factor for adult cardiovascular disease and associated mortality.63 Asian populations are observed to have a different relationship between BMI, body fat and health risks in comparison with Europeans. The proceedings of the Asia–Pacific Perspective meeting for Redefining Obesity and its Treatment suggest that in Asia, people should be categorized as overweight when BMI exceeds 23.0 kg/m2 and obese when BMI exceeds 25.0 kg/m2.64 Thus, for Asian countries where CVD is the commonest cause of death and childhood obesity is one of the few major modifiable risk factors, early detection (high sensitivity) is critical. WHO 2007 references identified a greater number of children as false negatives by classifying overweight or obese at risk as having normal BMI. Similar to a previous study in India, a Pakistani study has also shown that WHO 2007 BMI-for-age references are not suitable for Pakistani children and demonstrated that Pakistani children were observed to have substantially lower BMI percentiles than their counterparts in the reference population.13,65 A study from Indonesia also reported that while using WHO BMI-for-age classification, the number of children and adolescents, observed to be overweight and obesity was lower.36 In contrast, a Malaysian study has shown that the use of WHO Child Growth Standards and WHO Growth References are likely to over-diagnose obesity and thinness/underweight in Malaysian children.57 Other Indonesian studies using Indonesian growth chart report either a slightly higher or lower rate of overweight and obesity compared to the WHO charts.32,49
To the best of our knowledge, there are very few studies which have assessed DBM in SA and SEA from the lens of using ethnic specific versus international references in the paediatric population. Also, ours is the first study to report the predictive value of various local, regional, and international standards or references for identifying stunting and overweight or obesity in relation to pathological short stature and metabolic syndrome risk, respectively. Ours is also the first study to report performance of anthropometric parameters in a group of children (Indian and Indonesian respectively) using reference data from a country of same region (Pakistan and Thailand respectively) and a country of different region (Indonesia and India respectively). Our study is limited by the fact that we could not test data on 0–59 months children from SEA due to lack of availability of a de-identified dataset; also, the Indonesian dataset did not have data on stunting, hence data these were not reported. Moreover, reference data used from Pakistan only provided data for height and BMI for girls. The reference data available from Thailand did not have mean, standard deviation or LMS values, and hence Z-scores could not be computed, we thus used binary classification of height cut-off less than -2SD for height-for-age to define short stature. Thai reference data also did not include data on BMI-for-age and hence we used weight-for-height as a surrogate to define overweight or obesity. Most of the Z-scores computed by us were using LMS values, however, for those reference datasets that did not provide LMS values, Z-scores were computed using mean and standard deviation. Finally, for the diagnosis and intervention of DBM in SA and SEA countries, we suggest that growth charts based on ethnicity/geographic region (like the Indian subcontinent, etc) rather than a single standard or reference may be developed, however, implementation of these recommendations has potential challenges of cost and data availability.
In conclusion, our study suggests that local anthropometric growth reference data are more accurate in identifying the double burden of malnutrition in children from the South and Southeast Asia region. The WHO growth standards or references over-estimate stunting and under-estimate obesity, thereby increasing the burden of evaluating apparently healthy short children and missing overweight or obese children at metabolic risk. The latter is critical for early intervention to reduce cardiovascular disease mortality. For countries that do not have an anthropometric growth reference data, the reference data from country of the same region may be used rather than international reference datasets to prevent misdiagnosing malnutrition. Finally, we suggest, that while it is important to use WHO/international references for intercountry/global comparisons; for diagnosis and intervention for DBM in SA and SEA countries, it may be prudent to develop growth charts based on ethnicity and geographic region (like Indian subcontinent, SEA, etc) rather than a single international growth standard or reference.
Contributors
A.V.K., V.V.K., S.W., and A.B.P conceived the study. C.O. and N.A.K. curated the data. C.O. performed the statistical analysis and drafted the initial manuscript. A.V.K. supervised and supported the study. A.B.P., S.W., A.G.M., G.A, K.W., M.J., P.D., and V.V.K. collated and analyzed the data. All authors reviewed, edited, and approved the final manuscript.
Declaration of interests
We declare no competing interest.
Acknowledgements
No funding was received to conduct the study described in this manuscript.
References
- 1.World Health Organization . 2017. Double burden of malnutrition.http://www.who.int/nutrition/double-burden-malnutrition/en/ [Google Scholar]
- 2.Shrimpton R., Rokx C. World Bank; Washington: 2012. The double burden of malnutrition: a review of global evidence. Health, nutrition and population discussion paper.https://openknowledge.worldbank.org/handle/10986/27417 [Google Scholar]
- 3.United Nations Children’s Fund (UNICEF) World Health Organization; Geneva: 2020. World Health Organization, international bank for reconstruction and development/the World bank. Levels and trends in child malnutrition: key findings of the 2020 edition of the joint child malnutrition estimates. [Google Scholar]
- 4.Alem A.Z., Yeshaw Y., Liyew A.M., et al. Double burden of malnutrition and its associated factors among women in low- and middle-income countries: findings from 52 nationally representative data. BMC Publ Health. 2023;23:1479. doi: 10.1186/s12889-023-16045-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Statistical Office of Thailand . Bangkok: National Statistical Office of Thailand; 2023. Thailand Multiple indicator cluster survey 2022, survey findings report.https://mics-surveys-prod.s3.amazonaws.com/MICS6/East%20Asia%20and%20the%20Pacific/Thailand/2022/Survey%20findings/MICS2022_National%20%28English%29.pdf [Google Scholar]
- 6.Thailand National Statistical Office . Bangkok: National Statistical Office; 2006. Thailand Multiple indicator cluster survey (MICS) December 2005–February 2006, final report.https://mics-surveys-prod.s3.amazonaws.com/MICS3/East%20Asia%20and%20the%20Pacific/Thailand/2005-2006/Final/Thailand%202005-06%20MICS_English.pdf [Google Scholar]
- 7.Mehta S., Oza C., Karguppikar M., Khadilkar V., Khadilkar A. Field testing of synthetic growth charts in 1–60-month-old Indian children. Indian J Endocr Metab. 2022;26:180–185. doi: 10.4103/ijem.ijem_9_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oza C., Khadilkar V., Gondhalekar K., Kajale N., Khadilkar A. Predictive value of WHO vs. IAP BMI charts for identification of metabolic risk in Indian children and adolescents. J Pediatr Endocrinol Metab. 2021;34:1605–1610. doi: 10.1515/jpem-2021-0411. [DOI] [PubMed] [Google Scholar]
- 9.Dange N.S., Khadilkar V., Kore V., et al. Comparison of WHO 2006 growth standards and synthetic Indian references in assessing growth in normal children and children with growth-related disorders. Indian J Endocr Metab. 2024;28:220–226. doi: 10.4103/ijem.ijem_380_23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.http://salter.com/content/9073 WH3R.pdf (salter.com)
- 11.Centres for disease Control and prevention. Body Mass Index (BMI); 2022. https://www.cdc.gov/healthyweight/assessing/bmi/index.html [cited 2023 Jun 19] Available from: [Google Scholar]
- 12.Wit J.M. International classification of pediatric endocrine diagnoses. Horm Res Paediatr. 2016;86:212–214. doi: 10.1159/000448893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khadilkar A.V., Lohiya N., Mistry S., et al. Random blood glucose concentrations and their association with body mass index in Indian school children. Indian J Endocr Metab. 2019;23:529–535. doi: 10.4103/ijem.IJEM_536_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Qaisar R., Karim A. A comparison of international and national references to measure the prevalence of stunting in Pakistani school-age girls. Sci Rep. 2022;12:5501. doi: 10.1038/s41598-022-09511-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.IDF consensus definition of metabolic syndrome in children and adolescents, Last update: 05/04/2017. https://www.idf.org/e-library/consensus-statements/61-idfconsensus-definition-of-metabolic-syndrome-in-childrenand-adolescents Available from:
- 16.Saudek C.D., Herman W.H., Sacks D.B., Bergenstal R.M., Edelman D., Davidson M.B. A new look at screening and diagnosing diabetes mellitus. J Clin Endocrinol Metab. 2008;93:2447–2453. doi: 10.1210/jc.2007-2174. [DOI] [PubMed] [Google Scholar]
- 17.Nutrition Division Ministry of Public Health Thailand . Bangkok: Thamduay Jai Co., Ltd.; 2021. A guide to using growth benchmarks for children aged 6-19 years.https://nutrition2.anamai.moph.go.th/th/book/201949 [cited 2023 April 9] Available from: [Google Scholar]
- 18.Khadilkar V., Khadilkar A.V., Kajale N. Indian growth references from 0-18-year-old children and adolescents–a comparison of two methods. Indian J Endocr Metab. 2019;23:635–644. doi: 10.4103/ijem.IJEM_555_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Akbar N., Aslam M., Petersen J.H., Mustafa G. The 2022 Pakistani references from birth to 60 months for length/height, weight and body mass index. Acta Paediatr. 2023;112:1249–1258. doi: 10.1111/apa.16770. [DOI] [PubMed] [Google Scholar]
- 20.Pulungan A.B., Julia M., Batubara J.R.L., Hermanussen M. Indonesian national synthetic growth charts. Acta Scientific Paediatrics. 2018;1:20–34. [Google Scholar]
- 21.Bloem M. The 2006 WHO child growth standards. BMJ. 2007;334:705–706. doi: 10.1136/bmj.39155.658843.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khadilkar V., Yadav S., Agrawal K.K., et al. Revised IAP growth charts for height, weight and body mass index for 5-to 18-year-old Indian children. Indian Pediatr. 2015;52:47–55. doi: 10.1007/s13312-015-0566-5. [DOI] [PubMed] [Google Scholar]
- 23.de Onis M., Onyango A.W., Borghi E., Siyam A., Nishida C., Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85:660–667. doi: 10.2471/BLT.07.043497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mansourian M., Marateb H.R., Kelishadi R., et al. First growth curves based on the World Health Organization reference in a nationally representative sample of pediatric population in the Middle East and North Africa (MENA): the CASPIAN-III study. BMC Pediatr. 2012;12:149. doi: 10.1186/1471-2431-12-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nwosu B.U., Lee M.M. Evaluation of short and tall stature in children. Am Fam Physician. 2008;78:597–604. [PubMed] [Google Scholar]
- 26.Lumeng J.C., Gahagan S., Blenner S., Wilbur M.B., Frank D.A. 2008. Chapter 23: feeding and eating conditions. Developmental-be-havioral pediatrics: Evidence and practice; pp. 757–789. [Google Scholar]
- 27.Bates K., Gjonça A., Leone T. Double burden or double counting of child malnutrition? The methodological and theoretical implications of stunting overweight in low- and middle-income countries. J Epidemiol Community Health. 2017;71:779–785. doi: 10.1136/jech-2017-209008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Akombi B.J., Chitekwe S., Sahle B.W., Renzaho A.M.N. Estimating the double burden of malnutrition among 595,975 children in 65 low- and middle-income countries: a meta-analysis of demographic and health surveys. Int J Environ Res Public Health. 2019 Aug 13;16(16):2886. doi: 10.3390/ijerph16162886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Riset Kesehatan Dasar 2007 . 2008. Jakarta: badan penelitian dan pengembangan kesehatan departemen kesehatan. [Google Scholar]
- 30.Riset Kesehatan Dasar 2010 . 2010. Jakarta: badan penelitian dan pengembangan kesehatan departemen kesehatan. [Google Scholar]
- 31.Rachmi C.N., Agho K.E., Li M., Baur L.A. Stunting, underweight and overweight in children aged 2.0-4.9 years in Indonesia: prevalence trends and associated risk factors. PLoS One. 2016;11 doi: 10.1371/journal.pone.0154756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Riset Kesehatan Dasar 2018 . 2018. Jakarta: badan penelitian dan pengembangan kesehatan departemen kesehatan. [Google Scholar]
- 33.Novina N., Hermanussen M., Scheffler C., et al. Indonesian national growth reference charts better reflect height and weight of children in west java, Indonesia, than WHO child growth standards. J Clin Res Pediatr Endocrinol. 2020;12:410–419. doi: 10.4274/jcrpe.galenos.2020.2020.0044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Muda W.M., Sundaram J.K., Gen T.Z. Khazanah Research Institute: Kuala Lumpur; Malaysia: 2019. Addressing malnutrition in Malaysia. [Google Scholar]
- 35.Thailand National Statistical Office . National Statistical Office; Bangkok, Thailand: 2006. Thailand Multiple indicator cluster survey (MICS) December 2005- February 2006, final report. [Google Scholar]
- 36.Benedict L., Hong S.A., Winichagoon P., Tejativaddhana P., Kasemsup V. Double burden of malnutrition and its association with infant and young child feeding practices among children under-five in Thailand. Public Health Nutr. 2021;24:3058–3065. doi: 10.1017/S1368980020003304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mai T.M., Pham N.O., Tran T.M., et al. The double burden of malnutrition in Vietnamese school-aged children and adolescents: a rapid shift over a decade in Ho Chi Minh City. Eur J Clin Nutr. 2020;74:1448–1456. doi: 10.1038/s41430-020-0587-6. [DOI] [PubMed] [Google Scholar]
- 38.Sandjaja S., Budiman B., Harahap H., et al. Food consumption and nutritional and biochemical status of 0·5-12-year-old Indonesian children: the SEANUTS study. Br J Nutr. 2013;110:S11–S20. doi: 10.1017/S0007114513002109. [DOI] [PubMed] [Google Scholar]
- 39.Julia M., van Weissenbruch M.M., Delemarre-van de Waal H.A., Surjono A. Influence of socioeconomic status on the prevalence of stunted growth and obesity in prepubertal Indonesian children. Food Nutr Bull. 2004;25:354–360. doi: 10.1177/156482650402500405. [DOI] [PubMed] [Google Scholar]
- 40.Sandjaja Poh B.K., Rojroonwasinkul N., Le Nyugen B.K., et al. Relationship between anthropometric indicators and cognitive performance in Southeast Asian school-aged children. Br J Nutr. 2013;110:S57–S64. doi: 10.1017/S0007114513002079. [DOI] [PubMed] [Google Scholar]
- 41.Riset Kesehatan Dasar 2013 . 2013. Jakarta: badan penelitian dan pengembangan kesehatan departemen kesehatan. [Google Scholar]
- 42.Poh B.K., Wong J.E., Lee S.T., et al. Triple burden of malnutrition among Malaysian children aged 6 months to 12 years: current findings from SEANUTS II Malaysia. Public Health Nutr. 2023:1–36. doi: 10.1017/S1368980023002239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Minh Do L., Lissner L., Ascher H. Overweight, stunting, and concurrent overweight and stunting observed over 3 years in Vietnamese children. Glob Health Action. 2018;11 doi: 10.1080/16549716.2018.1517932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Moelyo A.G., Candrarukmi D., Rachma U.P. Using the National Indonesian Growth Chart to assess short stature and obesity in urban schoolchildren in Surakarta, Indonesia: comparisons to the WHO 2007 and CDC 2000 Growth Charts. Paediatr Indones. 2022;62:180–185. [Google Scholar]
- 45.Lohiya N., Khadilkar V., Pawar S., Khadilkar A., Chiplonkar S., Jahagirdar R. Field testing of IAP2015 charts. Indian J Pediatr. 2018;85:723–728. doi: 10.1007/s12098-018-2621-4. [DOI] [PubMed] [Google Scholar]
- 46.Mo-Suwan L., Choprapawon C. Comparison of prevalence of nutritional status of Thai children in the first 2 years of life using national and international growth charts. J Med Assoc Thai. 2016;99:58–64. [PubMed] [Google Scholar]
- 47.Iftikhar S., Khan N., Siddiqui J.S., Baig-Ansari N. Development of growth charts of Pakistani children aged 4-15 years using quantile regression: a cross-sectional study. Cureus. 2018;10 doi: 10.7759/cureus.2138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Stigler M.H., Arora M., Dhavan P., et al. Measuring obesity among school-aged youth in India: a comparison of three growth references. Indian Pediatr. 2011;48:105–110. doi: 10.1007/s13312-011-0041-x. [DOI] [PubMed] [Google Scholar]
- 49.Jajat J., Suherman A. Atlantis Press; 2020. Indonesian children and adolescents' body mass index: WHO and Asia-Pacific classification. In 4th international conference on sport science, health, and physical education (ICSSHPE 2019) pp. 263–266. [Google Scholar]
- 50.Khadilkar V.V., Khadilkar A.V., Chiplonkar S.A. Growth performance of affluent Indian preschool children: a comparison with the new WHO growth standard. Indian Pediatr. 2010;47:869–872. doi: 10.1007/s13312-010-0147-6. [DOI] [PubMed] [Google Scholar]
- 51.Khadilkar V., Khadilkar A. Growth charts: a diagnostic tool. Indian J Endocr Metab. 2011;15:166–171. doi: 10.4103/2230-8210.84854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.John J. Vol. 10. Med J Dr. DY Patil Univ; 2017. Comparison of World Health Organization growth standards with Indian academy of pediatrics growth charts of under five children in a rural area of Puducherry; p. 22. [Google Scholar]
- 53.Patel R., Dave C., Agarwal N., Mendpara H., Shukla R., Bajpai A. Predictive value of IAP 2015, IAP 2007 and WHO growth charts in identifying pathological short stature. Indian Pediatr. 2021;58:149–151. [PubMed] [Google Scholar]
- 54.Hong S.A., Mongkolchati A., Chompikul J., Mo-Suwan L., Choprapawon C. Comparison of prevalence of nutritional status of Thai children in the first 2 Years of life using national and international growth chart. J Med Assoc Thai. 2016;99:58–64. [PubMed] [Google Scholar]
- 55.Karim A., Qaisar R. Anthropometric measurements of school-going-girls of the Punjab, Pakistan. BMC Pediatr. 2020;20:223. doi: 10.1186/s12887-020-02135-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Perera P.J., Fernanado M.P., Ranathunga N., Sampath W., Samaranayake R., Mettananda S. Growth parameters of Sri Lankan children during infancy: a comparison with World Health Organization multicentre growth reference study. J Hum Growth Dev. 2014;24:11–15. [Google Scholar]
- 57.Institute for Medical Research . Ministry of Health, Malaysia; Kuala Lumpur: 2015. Development of growth charts for Malaysian children: technical report. [Google Scholar]
- 58.Rojroongwasinkul N., Bao Kle N., Sandjaja S., et al. Length and height percentiles for children in the South-East Asian nutrition surveys (SEANUTS) Public Health Nutr. 2016;19:1741–1750. doi: 10.1017/S1368980015003316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Christesen H.T., Pedersen B.T., Pournara E., Petit I.O., Júlíusson P.B. Short stature: comparison of WHO and national growth standards/references for height. PLoS One. 2016;11 doi: 10.1371/journal.pone.0157277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Natale V., Rajagopalan A. Worldwide variation in human growth and the World Health Organization growth standards: a systematic review. BMJ Open. 2014;4 doi: 10.1136/bmjopen-2013-003735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Scherdel P., Botton J., Rolland-Cachera M.-F., et al. Should the WHO growth charts be used in France? PLoS One. 2015;10 doi: 10.1371/journal.pone.0120806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.https://www.who.int/southeastasia/health-topics/noncommunicable-diseases
- 63.Umer A., Kelley G.A., Cottrell L.E., Giacobbi P., Jr., Innes K.E., Lilly C.L. Childhood obesity and adult cardiovascular disease risk factors: a systematic review with meta-analysis. BMC Publ Health. 2017;17:683. doi: 10.1186/s12889-017-4691-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.WHO/IASO/IOTF . Read. Health Communications Australia; Melbourne: 2000. The Asia-Pacific perspective: redefining obesity and its treatment. [Google Scholar]
- 65.Asif M., Aslam M., Wyszyńska J., Altaf S. Vol. 75. Minerva Pediatr (Torino); 2023. Establishing Body Mass Index growth charts for Pakistani children and adolescents using the lambda-mu-sigma (LMS) and quantile regression method; pp. 866–875. [DOI] [PubMed] [Google Scholar]