Abstract
Maxillofacial fractures in the pediatric population are generally managed by conservative approaches such as soft diet and medication or semi-invasive procedures namely inter-maxillary fixation or circum-mandibular wiring. These approaches are preferred over any invasive treatment to minimize injury to the growing skeleton and tooth germs. Displaced fractures that cause functional problems such as restricted mouth opening, malocclusion or impaired breathing, mandate open reduction and internal fixation. However, surgical management is associated with morbidity related to general anesthesia, risk of injury to vital structures, and potential, skeletal or dental growth disturbances. This case report describes a non-invasive method of managing displaced, multiple fractures of the mandible in a pediatric patient, with the use of low intensity pulsed ultrasound to achieve favorable clinical outcomes and nil complications. Neither immobilization of the mandible with inter-maxillary fixation nor open reduction and internal fixation was used. Low intensity pulsed ultrasound therapy is painless and patient-friendly.
Keywords: Pediatric fractures, Parasymphysis, Ramus, Composite splinting
1. Introduction
Maxillofacial trauma in pediatric patients affects the facial form as well as vital functions such as mastication, breathing, and speech.1 Additionally, long-term effects such as growth disturbances2 and psychological imbalances3 have also been reported in literatures. Hence, the objectives in the management of pediatric trauma include early restitution of form and function of facial skeleton, while preventing potential developmental or psychological problems. The treatment principles of pediatric fractures vary from that of adults because of the growing status of the facial skeleton as well as dental apparatus. A conservative approach is generally advocated in the pediatric population to ensure nil impact on a child's anatomic, physiologic, and psychological development.
Mandibular fractures in pediatric patients, when undisplaced or without the presence of malocclusion have been successfully managed by conservative modalities such as soft/liquid diet and medication including antibiotics and analgesics, along with careful observation, till the period of fracture healing.4 Such patients refrained from strenuous physical activities for several weeks to avoid any further trauma to the mandible. Fractures presenting with malocclusion require treatment with a maxillo-mandibular fixation for a duration of 7 – 14 days.5 Fractures associated with malocclusion and/or moderate displacement of fracture segments may be treated effectively by closed reduction using capsplints and circum-mandibular wiring.6 Proponents of conservative therapy or closed management assert that the effective clinical outcomes obtained through such methods are due to 2 major reasons: (1) the high osteogenic potential present in children which facilitates quick fracture healing and remodeling and (2) the remarkable ability for functional adaptation. However, severe displacement of fracture segments leading to functional problems such as restriction in mouth opening, eating, or breathing necessitates open reduction and internal fixation (ORIF).7 Surgical intervention is also mandatory in fractures which may cause potential developmental problems or changes in facial morphology. However, surgical procedures are associated with complications such as injury to vital structures, potential skeletal/dental growth disturbances, and general anesthesia-related morbidity. Hence a non-invasive treatment modality is generally preferred.8
A modality that neither compromises outcomes nor is invasive, is ideal. This technical note presents a novel, non-invasive method of treating a displaced fracture involving the ramus and bilateral parasymphysis, in a 6-year-old patient, using low intensity pulsed ultrasound (LIPUS). None of the conventional modalities used for pediatric fracture management such as circum-mandibular wiring, immobilization of mandible with inter-maxillary fixation (IMF) nor ORIF was used.
2. Case report
A 6-year-old boy, presented to our department with complaints of pain in his lower jaw, restricted mouth opening, and difficulty in chewing. The parent gave a history of road traffic accident 7 days earlier, following which the boy had demonstrated loss of consciousness for a few seconds, intraoral bleeding, pain in the lower anterior jaw and bilateral temporomandibular joint region, along with extraoral swelling on the right side. The patient also had limited mouth opening for 3 days since the accident.
Clinical examination revealed an extraoral scar in the chin region. The mouth opening was restricted to 20 mm with a deviation of the chin to the right side. The other clinical findings elicited were interfragmentary mobility at the left parasymphysis region (between 72 and 73) with anterior open bite and tenderness at the right angle region. Orthopantomogram revealed left parasymphysis and right ramus fracture. CT revealed a displaced fracture of the right ramus and bilateral parasymphysis region (Figs. 1 & 2).
Fig. 1.
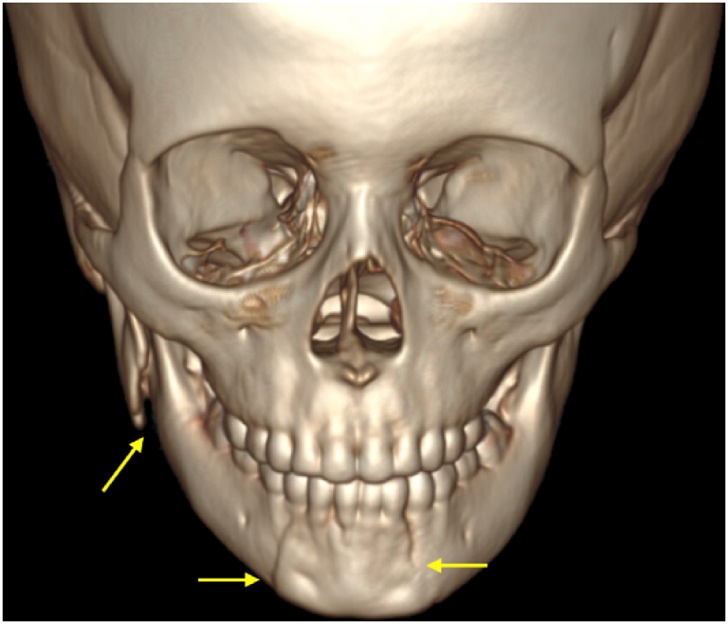
Pre-operative CT image demonstrating displaced ramal fracture and bilateral parasymphysis fracture (frontal view).
Fig. 2.
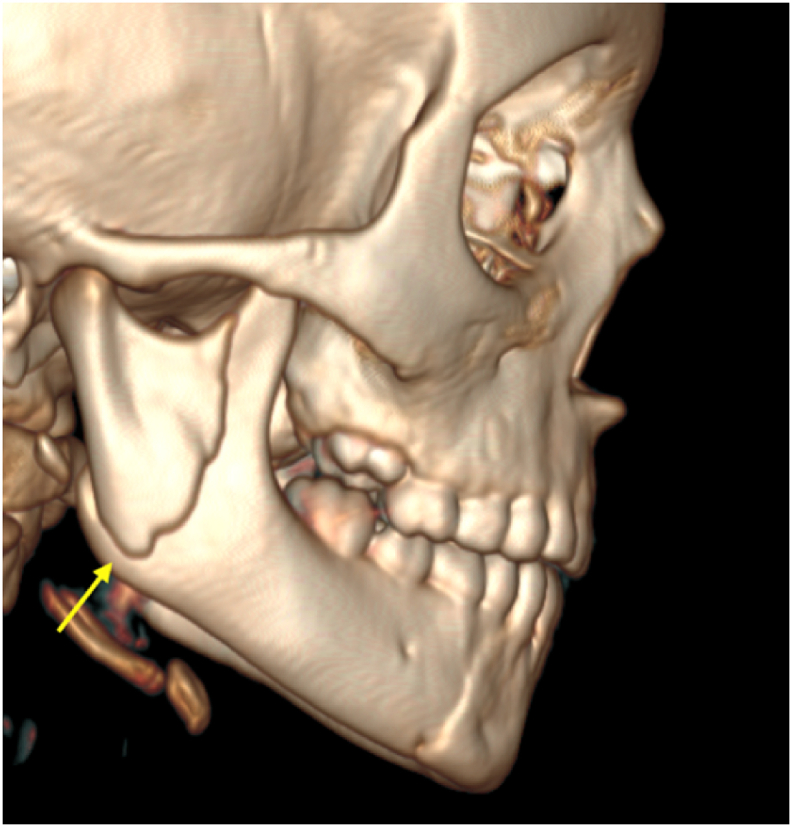
Pre-operative CT image demonstrating displaced ramal fracture and bilateral parasymphysis fracture (lateral view).
Informed consent for the treatment was obtained from the patient and the necessary approval was obtained from the institutional review board (SRMU/M&HS/SRMDC/2023/S/008).
2.1. Management
The bilateral parasymphysis fracture was reduced by digital manipulation and stabilized using fiber-reinforced composite splint (Interlig, Angelus, Brazil) over the buccal and lingual surfaces of 71, 72, 73, 74, 81, 82, 83, and 84 (Fig. 3). Ideal occlusion was ensured and high points were checked using articulating paper. This was followed by LIPUS therapy for 11 days (Fig. 4). The regimen of LIPUS therapy included a dosage of 0.5 – 1 W/cm2, for a duration of 10 min. The splints were maintained in-situ for 3 weeks and the patient was advised to consume soft diet. No immobilization of the mandible was done. Medications prescribed were Novamox (Amoxycillin 125 mg) 5 mL for 5 days and Ibugesic plus (Ibuprofen 100 mg & Paracetamol 162.5 mg) oral suspension for 2 days. The patient demonstrated nil pain, right from the first day of LIPUS therapy. Substantial improvement in mouth opening was also observed; 34 mm and 40 mm on day 1 and day 4, respectively. Periodic follow-up of the patient was done to evaluate the occlusion, mouth opening, and stability of the splint. The splint removal was done on the day 26, using an ultrasonic scaler.
Fig. 3.

Composite splint in-situ after parasymphyseal fracture reduction.
Fig. 4.

Low intensity pulsed ultrasound therapy.
2.2. Post-operative outcome
The patient demonstrated complete resolution of symptoms by the 4th day; mouth opening of 40 mm, good occlusion, and nil pain. Upon splint removal, no interfragmentary mobility was elicited in the anterior parasymphysis region. Figs. 5 & 6 demonstrates the accurate anatomical reduction and healing of the bilateral parasymphysis and ramus fracture on postoperative CT taken after 4 months.
Fig. 5.
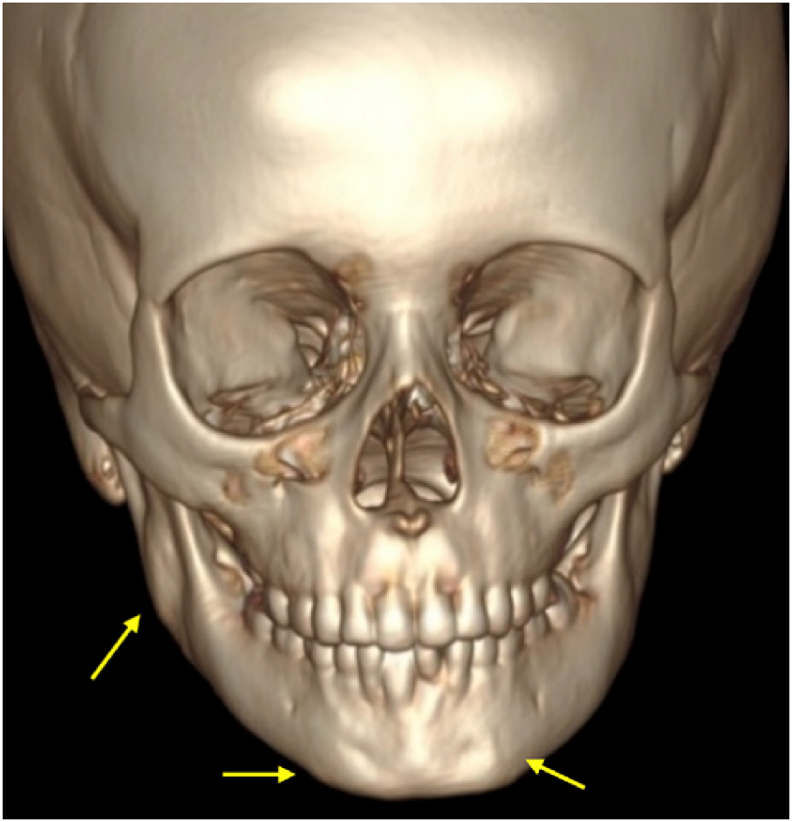
Post-operative CT image demonstrating fracture healing post 4 months of low intensity pulsed ultrasound therapy (frontal view).
Fig. 6.
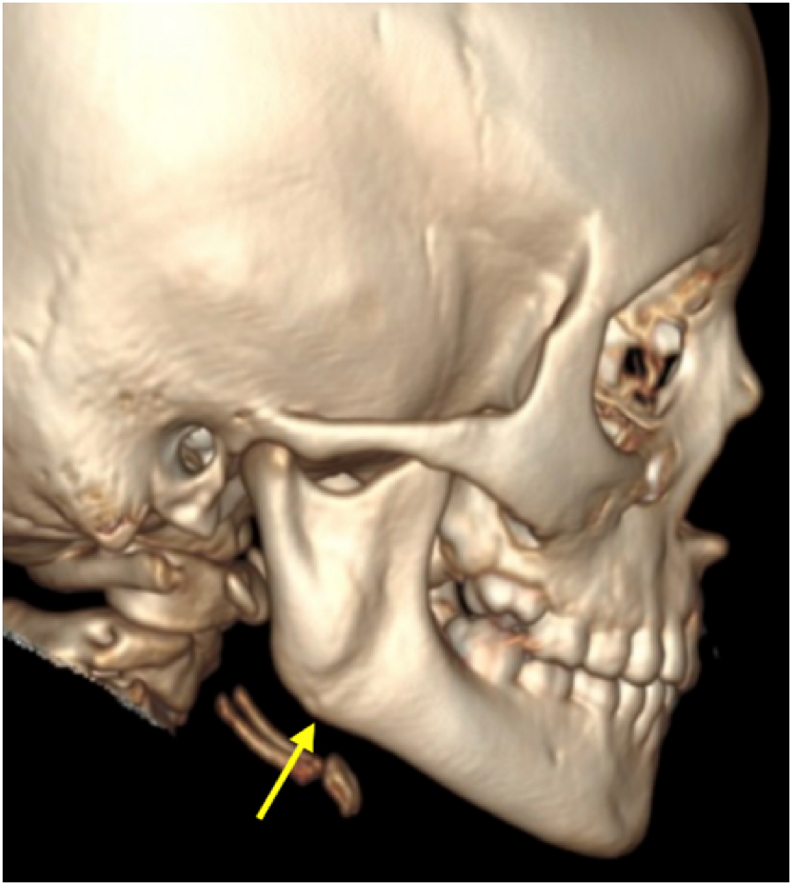
Post-operative CT image demonstrating fracture healing post 4 months of low intensity pulsed ultrasound therapy (lateral view).
3. Discussion
The primary goals of pediatric fracture management encompass early restoration of form as well as functions such as mouth opening and mastication without causing any long-term complications or psychological disturbances. The major concerns during treatment include the potential risk of injury to the skeletal and dental growth. Hence many cases are managed by conservative methods such as soft diet and restricted mouth opening which help prevent violation of the delicate and less developed tissues.9 Lesser invasive techniques such as circum-mandibular wiring, Risdon wiring, or inter-maxillary fixation with wires/elastics are indicated in displaced fractures which present with malocclusion and restricted mouth opening.10 However, the drawbacks of circum-mandibular wiring are many: (1) the need for local or general anesthesia for reduction; (2) trauma to soft tissues; (3) the cumbersome process of taking dental impressions in a child with painful/restricted mouth opening, and (4) the need for fabrication of splints. Further, splints are inconvenient for mastication and maintenance of good oral hygiene. The technique also requires a second appointment for the removal of the wire.
Inter-maxillary fixation as a treatment modality is common in surgical practice to manage undisplaced/less displaced dentate fractures, condyle fractures, and fractures that are naturally splinted by muscles such as ramus or zygomatic arch fractures. In children, IMF is established with the use of the arch bar and wires/elastics, inter-dental wiring, or silk sutures.11 However instituting IMF is not always feasible in children because of poor compliance and technical limitations such as wire slippage through primate spaces or unfavorable dental morphology. Further, IMF is associated with numerous disadvantages. It is time consuming, traumatic to tissues, and prone to avulsion of teeth during twisting of wires and needle stick injuries. Importantly, IMF can compromise the nutritional status of the patient by reducing intake of food. Also, IMF is contraindicated in patients with existing respiratory problems or epilepsy. Orthodontic brackets with elastics have been used by some surgeons for the immobilization of the mandible. Though the technique is non-invasive and patient-friendly, it does not provide sufficient rigidity or stability to hold the fractured fragments and hence not suitable for severely displaced fractures. When placed improperly, it can also lead to subluxation of teeth.
ORIF is chosen for fractures that are severely displaced and cause functional problems like impaired breathing, mouth opening, or eating. Fractures that are not amenable to closed reduction are also managed by surgery. ORIF facilitates early recovery of function and accuracy of anatomic reduction but is associated with complications related to general anesthesia and morbidity due to surgical intervention; specifically, injury to vital structures such as nerves, dental follicles, and skeletal growth centers, along with the need for the second surgery for plate removal. Complications related to plate per se are also reported in literature namely allergy to metal and stress shielding.12 Resorbable plates negate the need for re-surgery but they are expensive. By conventional norms, the patient discussed in this report, required immobilization of the mandible or management by semi-invasive modality or surgical intervention due to the presence of multiple fractures, malocclusion, and the severity of ramal displacement. But none of these were instituted yet good clinical results were achieved using LIPUS therapy and splinting with composite. The therapeutic benefits of LIPUS have been established by numerous studies.13 It facilitates fracture healing by 4 mechanisms: (1) promoting angiogenesis through the increase of vascular endothelial growth factor; (2) elevating the levels of chondroitin sulfate which is crucial for supporting the osseous framework; (3) mineralization of soft tissue callus; and (4) expediting bone remodeling.14 Further, LIPUS eliminates pain-inducing chemical mediators from the fracture site, reduces the need for post-operative analgesics, and improves patient comfort.15 In this patient, by virtue of its biomechanical actions, LIPUS eliminated the pain associated with fractures permitting the child to move the mandible without any discomfort. The splint prevented the inter-fragmentary mobility at the bilateral parasymphyseal region. As elucidated by Ellis et al.16 functional movements of the mandible facilitated physiological restitution of normal mandibular anatomy as well as occlusion, without any pain or trismus.
The positives of using LIPUS therapy along with splinting, are the following: (1) relief of pain in the fracture site, from the first day of LIPUS therapy; (2) no necessity for immobilization of mandible and hence, early restitution of function; (3) restoration of occlusion and facial symmetry; (4) avoidance of general anesthesia and its associated risks; and (5) avoidance of surgical procedure that may pose a risk to skeletal growth or injury to dental roots.
The limitation of this article is sample size. A prospective clinical study with a larger sample size would provide more conclusive results that maybe used to formulate treatment algorithm for trauma management in pediatric management.
In conclusion, LIPUS therapy is an effective modality to manage pediatric mandibular fracture without mandibular immobilization or ORIF. It reduces pain in the fracture site, promotes fracture healing, and facilitates early restitution of function. It is non-invasive, painless, and economical to use.
Funding
Nil.
Ethical statement
Informed consent has been obtained from the patient.
Approval number from Institutional Review Board: SRMU/M&HS/SRMDC/2023/S/008.
Declaration of competing interest
None.
Author contributions
Elavenil Panneerselvam - Treatment planning, Treatment, Treatment review & Manuscript writing.
Chandini Ravikumar - Treatment, Treatment review & Manuscript writing.
Trishala Annamalai Rajan - Treatment, Treatment review & Manuscript writing.
Sasikala Balasubramanian - Treatment review.
Krishnakumar Raja V.B. - Critical appraisal of manuscript.
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Mukherjee C.G., Mukherjee U. Maxillofacial trauma in children. Int J Clin Pediatr Dent. 2012;5:231–236. doi: 10.5005/jp-journals-10005-1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khatri A., Kalra N. A conservative approach to pediatric mandibular fracture management: outcome and advantages. Indian J Dent Res. 2011;22:873–876. doi: 10.4103/0970-9290.94692. [DOI] [PubMed] [Google Scholar]
- 3.Tandon P., Aurora J.K., Kumar V., et al. Management of pediatric maxillofacial trauma using acrylic cap splint followed by circummandibular wiring: a single centric study. The Traumaxilla. 2020;2:49–52. doi: 10.1177/26323273221085708. [DOI] [Google Scholar]
- 4.Nezam S., Kumar A., Shukla J.N., et al. Management of mandibular fracture in pediatric patient. Natl J Maxillofac Surg. 2018;9:106–109. doi: 10.4103/njms.NJMS_54_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pickrell B.B., Serebrakian A.T., Maricevich R.S. Mandible fractures. Semin Plast Surg. 2017;31:100–107. doi: 10.1055/s-0037-1601374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Priya Vellore K., Gadipelly S., Dutta B., et al. Circummandibular wiring of symphysis fracture in a five-year-old child. Case Rep Dent. 2013;2013 doi: 10.1155/2013/930789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goth S., Sawatari Y., Peleg M. Management of pediatric mandible fractures. J Craniofac Surg. 2012;23:47–56. doi: 10.1097/SCS.0b013e318240c8ab. [DOI] [PubMed] [Google Scholar]
- 8.John B., John R.R., Stalin A., et al. Management of mandibular body fractures in pediatric patients: a case report with review of literature. Contemp Clin Dent. 2010;1:291–296. doi: 10.4103/0976-237X.76406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wolfswinkel E.M., Weathers W.M., Wirthlin J.O., et al. Management of pediatric mandible fractures. Otolaryngol Clin North Am. 2013;46:791–806. doi: 10.1016/j.otc.2013.06.007. [DOI] [PubMed] [Google Scholar]
- 10.Kumar N., Richa, Gauba K. Modified closed cap splint: conservative method for minimally displaced pediatric mandibular fracture. Saudi Dent J. 2018;30:85–88. doi: 10.1016/j.sdentj.2017.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Farber S.J., Nguyen D.C., Harvey A.A., et al. An alternative method of intermaxillary fixation for simple pediatric mandible fractures. J Oral Maxillofac Surg. 2016;74:582.e1–582.e8. doi: 10.1016/j.joms.2015.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sharma A., Patidar D.C., Gandhi G., et al. Mandibular fracture in children: a new approach for management and review of literature. Int J Clin Pediatr Dent. 2019;12:356–359. doi: 10.5005/jp-journals-10005-1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abel A.R., Reeve G.S. Low-intensity pulsed ultrasound therapy: a nonsurgical treatment modality for mandible fracture nonunion. Facial Plast Surg. 2021;37:571–575. doi: 10.1055/s-0041-1724123. [DOI] [PubMed] [Google Scholar]
- 14.Wei Y., Guo Y. Clinical applications of low-intensity pulsed ultrasound and its underlying mechanisms in dentistry. Appl Sci. 2022;12 doi: 10.3390/app122311898. [DOI] [Google Scholar]
- 15.Gopalan A., Panneerselvam E., Doss G.T., et al. Evaluation of efficacy of low intensity pulsed ultrasound in facilitating mandibular fracture healing-A blinded randomized controlled clinical trial. J Oral Maxillofac Surg. 2020;78:997.e1–997.e7. doi: 10.1016/j.joms.2020.01.036. [DOI] [PubMed] [Google Scholar]
- 16.Ellis E., Throckmorton G.S. Treatment of mandibular condylar process fractures: biological considerations. J Oral Maxillofac Surg. 2005;63:115–134. doi: 10.1016/j.joms.2004.02.019. [DOI] [PubMed] [Google Scholar]


