Abstract
Purpose
A significant percentage of women experience psychopathological symptoms during the postpartum period, which can impact not only their mental health and well-being but also the relationship between mother and baby. However, studies investigating how specific psychological factors, such as self-compassion and self-criticism, contribute to the development and maintenance of these symptoms are scarce.
Methods
This cross-sectional study aimed to examine the relationship among compassionate self-responding (CSR), uncompassionate self-responding (USR), maternal mental health indicators, mother-infant bonding, and the perceived impact of the COVID-19 pandemic. Data were collected online from 189 Brazilian women with infants aged 0 to 12 months. Participants completed measures of sociodemographic characteristics, Self-Compassion Scale (SCS), Edinburgh Postnatal Depression Scale (EPDS), Postpartum Specific Anxiety Scale (PSAS-BR-RSF-C), Postpartum Bonding Questionnaire (PBQ), and COVID-19–Impact on Quality of Life (COV19-QoL).
Results
Through network analysis, our findings highlighted that postpartum depression played a central role in the structuring of variables in this system. Furthermore, USR, instead of CSR, emerged as the variable most strongly associated with levels of postpartum depression, which, in turn, was associated with mother-infant bonding.
Conclusion
Mitigating levels of self-criticism in mothers may represent a pathway to prevent the development of postpartum depression, which, in turn, could impact the quality of the mother-infant relationship. Given the significance of the child’s early years for their emotional development, intervening early in maternal mental health may be a means to prevent mental disorders in the child as well.
Keywords: Self-criticism, Self-compassion, Postpartum, Pandemic, Network analysis
Introduction
The transition to motherhood entails significant intra and interpersonal changes in a woman's life, often resulting in negative emotional outcomes, such as the onset or exacerbation of mental disorders (Cantwell, 2021). Throughout the postpartum period, symptoms of depression and anxiety are commonly observed, affecting a substantial portion of this population (Chen et al., 2022). These conditions not only affect maternal well-being but also bear implications for the mother-infant relationship (Fallon et al., 2021; Rocha et al., 2020). Studies have demonstrated that children whose mothers experience postpartum depression are at a significantly higher risk of developing cognitive, emotional, social, and behavioral difficulties (Aoyagi et al., 2019; Murray & Cooper, 1996; Slomian et al., 2019). Therefore, there is a critical need for research to address maternal mental health and explore mother-infant bonding, with the aim of identifying potential intervention targets to enhance the overall postpartum experience.
The COVID-19 pandemic has further intensified the mental health concerns faced by postpartum mothers. Studies have documented heightened prevalence rates of depression and anxiety symptoms during this period, underscoring the necessity of investigating the pandemic's impact on postpartum mental health. In their systematic review and meta-analysis, Gao et al. (2022) examined 20,225 postpartum women across 16 countries spanning four continents (Asia, Europe, North America, and South America) during the COVID-19 pandemic. The study revealed a prevalence of 26.7% for depression symptoms and 33.8% for anxiety symptoms among mothers of newborn children. In Brazil, Loret de Mola et al. (2021) found that out of 1042 participants, 29.3% were classified as probable cases of postpartum depression based on the Edinburgh Postnatal Depression Scale (EPDS; Cox et al., 1987; Santos et al., 2007). This research, part of a cohort study, revealed that the prevalence of depressive symptoms in this population was 5.7 times higher during the pandemic compared to data obtained before COVID-19.
The presence of psychopathological symptoms can be detrimental to mother-infant bonding. A systematic review conducted by Slomian et al. (2019) analyzed 122 studies on the untreated consequences of postpartum depression. The results revealed that mothers experiencing depression encountered more substantial challenges in their relationships with their children during the first year of life. In terms of breastfeeding, there was a negative correlation between postpartum depression and breastfeeding practices, which could result in an earlier cessation of exclusive breastfeeding. Moreover, mothers with postpartum depression reported greater dissatisfaction with their breastfeeding experience. Regarding maternal care, the review found a significant link between postpartum depression and increased difficulties in caring for the baby, with depressed mothers exhibiting poorer parenting practices compared to non-depressed mothers.
In efforts to prevent and alleviate psychopathological symptoms while promoting mental health, the concept of self-compassion has received extensive attention in recent decades. Self-compassion is defined as a healthy way of relating to oneself, characterized by a welcoming, warm, and non-evaluative stance towards one’s own suffering (Neff, 2003). The most widely used method for evaluating this construct is the Self-Compassion Scale (SCS; Neff, 2003), which is designed to assess self-compassion through a total factor. It incorporates scores from self-compassion subscales (self-kindness, common humanity, and mindfulness) as well as the inverse scores from self-criticism subscales (self-judgement, isolation, and over-identification). Based on this, research has identified associations between self-compassion and various outcomes, including negative correlations with depression (MacBeth & Gumley, 2012) and anxiety (Neff et al., 2007), and positive associations with well-being (Zessin et al., 2015), quality of life (Mantelou & Karakasidou, 2017), and emotional regulation (Inwood & Ferrari, 2018).
In the context of motherhood, preliminary studies have shown that self-compassion is linked to fewer symptoms of depression and anxiety (Felder et al., 2016; Fonseca & Canavarro, 2018), as well as to engagement in more well-being-related behaviors (Simpson et al., 2021), increased psychological flexibility, and stronger mother-infant bonding (Whittingham & Mitchell, 2021). Moreover, experimental studies have indicated that interventions targeting self-compassion lead to increased maternal self-compassion and significant reductions in depressive symptoms (Fonseca et al., 2019; Guo et al., 2020) and negative affect (Angus et al., 2024). In the context of the COVID-19 pandemic, Fernandes et al. (2021) investigated maternal self-compassion and the mother-infant bond, finding that maternal self-compassion appears to play a crucial role in stabilizing the mother-infant bond during the postpartum period, particularly in the context of the pandemic.
According to Neff (2003), self-criticism is the opposite of self-compassion and is characterized by self-judgment and negative self-evaluation in response to perceived failure or suffering. Neff posits that self-compassion and self-criticism lie on a bipolar continuum, which is why the self-critical components are included in the total factor provided by the SCS. However, recent literature advocates for considering these constructs as independent components (Halamová et al., 2021; Kumlander et al., 2018; López et al., 2015; Muris & Otgaar, 2020), which can be labeled as compassionate self-responding (CSR) and uncompassionate self-responding (USR) (Brenner et al., 2017; Ferrari et al., 2022; Muris et al., 2021). This recommendation arises from the observation that inverse scores for USR may inflate the total factor of self-compassion, and because self-criticism has been associated with higher rates of psychopathology compared to the positive components of self-compassion (Mills et al., 2007; Muris & Petrocchi, 2017). Furthermore, the use of the two factors allows for more accurately identifying which components are associated with the variables being researched.
When considering the perinatal period, a study evaluated the effect of an experiment on self-compassion using the six subscales of the SCS. The results indicated that the mechanisms of change were primarily due to a reduction in USR items rather than an increase in CSR items (Angus et al., 2024). In the same direction, initial evidence suggests that self-criticism serves as a vulnerability factor for the development of postpartum depression (Pedro et al., 2019). Furthermore, another study revealed that mothers exhibiting higher levels of self-criticism demonstrated poorer attachment quality with their children at 20 months of age (Gravener et al., 2012). Thus, it is inferred that excessive self-criticism may influence the bond between mother and infant, thereby influencing the emotional development of the child. However, literature on this topic remains limited, hindering the formation of a consensus regarding the role of self-criticism in maternal mental health.
Given the established predictive role of self-criticism in various mental disorders (Auerbach et al., 2014; Cohen et al., 2013; Fennig et al., 2008; Pedro et al., 2019; Werner et al., 2019), and the lack of studies evaluating this concept in mothers, there is a critical need to investigate this construct and its impact on maternal mental health. Such research is crucial for preventing mental disorders not only in mothers but also in their infants. With these considerations in mind, the present study aims to contribute to the existing national and international literature by examining potential relationships among self-compassion, self-criticism, indicators of maternal mental health, mother-infant bonding, and the perceived impact of the COVID-19 pandemic on quality of life.
Method
Procedures
This research comprises a cross-sectional, quantitative, and descriptive study conducted via the online platform Qualtrics Survey Software (https://www.qualtrics.com/pt-br/). A convenience sample of Brazilian mothers was recruited through social media platforms from March to November 2022. The inclusion criteria for the study were (1) Brazilian nationality; (2) age 18 years or older; (3) having at least one child between 15 days and 12 months old. Exclusion criteria included (1) incomplete questionnaire responses; (2) a baby with a severe illness or syndrome, as reported by the participant in response to the question "Was your baby born with any severe illness or syndrome?” in the sociodemographic questionnaire. Initially, 262 individuals began filling out the survey. Participants with incomplete questionnaire responses (n = 71) or those reporting babies affected by severe illnesses or syndromes (n = 2) were excluded from the sample, resulting in a final sample of 189 participants. Upon completion of the study, participants received a booklet containing psychoeducational information on mental health in motherhood, prepared by the researchers involved in this study (Gerhardt: Maternal self-compassion in the context of the COVID-19 pandemic: Associations with depression, anxiety, and quality of the mother-baby relationship, unpublished). All variables, including diagnoses, were assessed using self-reported questionnaires.
Ethical procedures
Ethical procedures
This study was approved by the Research Ethics Committee (CEP) of the Pontifical Catholic University of Rio Grande do Sul (PUCRS) on February 4th, 2022, under CAAE number: 55069122.0000.5336. The ethical aspects proposed by the Guidelines and Standards provided for in Resolution No. 510 of the National Health Council (2016) and Resolution 466 of 2012 (CNS 466/2012) were respected. All participants accepted the Informed Consent Form (TCLE) before starting to fill in the instruments.
Materials
Sociodemographic Questionnaire
Maternal-related demographic questions and infant characteristics were asked at the beginning of the survey (see Table 1 for means and frequencies). The questionnaire collected information regarding the women’s age, marital status, occupational situation, level of education, family income, parity, history of psychopathology, gestational diabetes (yes vs. no), type of delivery time (vaginal vs. c-section), baby's gender, time since delivery (baby’s age), and information related to COVID-19.
Table 1.
Maternal and infant characteristics (n=189)
| Variable | Level | Counts | % |
|---|---|---|---|
| Marital Status | Single | 28 | 14.8 |
| Married | 103 | 54.5 | |
| Co-habiting | 56 | 29.6 | |
| Divorced | 2 | 1.1 | |
| In a relationship | Yes | 177 | 94.1 |
| No | 11 | 5.9 | |
| Educational Attainment | Incomplete Elementary Education | 1 | 0.5 |
| Elementary Education | 1 | 0.5 | |
| Incomplete High School Education | 2 | 1.1 | |
| High School Education | 18 | 9.5 | |
| Technical Education | 6 | 3.2 | |
| Incomplete Higher Education | 30 | 15.9 | |
| Complete Higher Education | 48 | 25.4 | |
| Postgraduate | 83 | 43.9 | |
| Occupation | Student | 12 | 6.3 |
| Employed | 76 | 40.2 | |
| Unemployed | 29 | 15.3 | |
| Beneficiary | 1 | 0.5 | |
| Self-employed | 60 | 31.7 | |
| Other | 11 | 5.8 | |
| Family income | Less than R$2.000 | 26 | 13.8 |
| Between R$2.000 and R$6.000 | 69 | 36.5 | |
| Between R$6.000 and R$9.000 | 28 | 14.8 | |
| Up to R$9.000 | 66 | 34.9 | |
| Diagnosis of psychopathology | Yes | 101 | 53.4 |
| Depression | 31 | 31 | |
| Anxiety | 38 | 38 | |
| Depression and anxiety | 12 | 12 | |
| Others | 19 | 19 | |
| No | 88 | 46.6 | |
| Birth order | 1st | 132 | 69.8 |
| 2nd | 45 | 23.8 | |
| 3rd and after | 12 | 6.3 | |
| Type of delivery | Vaginal | 88 | 46.6 |
| Cesarian | 101 | 53.4 | |
| Baby's sex | Female | 83 | 44.1 |
| Male | 105 | 55.9 |
Validated psychological measures
COVID-19–Impact on Quality of Life (COV19-QoL; Repišti et al., 2020): A unidimensional scale developed with the objective of measuring the impact of the COVID-19 pandemic in the quality of life. Participants rate their experiences over the past seven days by responding to six questions (e.g., “I think my quality of life is lower than before”) on a 5-point Likert scale ranging from 1 (completely disagree) to 5 (completely agree). The total score is obtained by averaging the scores across all items, with higher scores indicating a greater perceived impact of the pandemic on quality of life. The scale demonstrated good internal consistency, with Cronbach’s alpha exceeding 0.80 for both populations. For the present study, the scale was translated into Brazilian Portuguese and subjected to psychometric analyses, including confirmatory factor analysis, which yielded good fit indices (CFI = 1.000; TLI = 1.012; RMSEA = 0.000) and reliability indices (Cronbach’s α = 0.87; McDonald’s ω = 0.87).
Self-Compassion Scale (SCS; Neff, 2003; translated and adapted by de Souza & Hutz, 2016). The scale consists of 26 items on a 5-point Likert scale. It includes six subscales that measure the CSR components (self-kindness, common humanity, and mindfulness) and USR components (self-judgment, isolation, and overidentification). The measurement method used was the bi-factor model, generating reliability indices for each subscale: CSR (McDonald’s ω = 0.92) and USR (McDonald’s ω = 0.91). The internal consistency level of the scale’s validation and adaptation for Brazil, using the total factor, was α = 0.92 (de Souza & Hutz, 2016).
Edinburgh Postnatal Depression Scale (EPDS; Cox et al., 1987; validated for the Brazilian population by Santos et al., 2007). It consists of a self-assessment scale comprising 10 items referring to depressive symptoms in the postpartum period, perceived in the last seven days. The total score is based on the sum of the items. The study of the Brazilian version indicates the cutoff point ≥ 10 as adequate for indicative of postpartum depression. The scale has good internal consistency indexes (Cronbach’s α = 0.87). In the present study, the instrument, measured from its total score, maintained a good reliability index (McDonald’s ω = 0.89).
Postpartum Specific Anxiety Scale–Research Short-form–for Global Crises (PSAS-BR-RSF-C; Silverio et al., 2021; validated for the Brazilian population by Gerhardt et al. (Gerhardt et al.: Psychometric properties of the Postpartum Specific Anxiety Scale research short-form for use during global crises in a Brazilian population (PSAS-BR-RSF-C), in preparation)). A 12-item self-report scale was designed to evaluate the individual's level of postpartum anxiety. The factorial structure of the scale includes four factors: maternal competence anxiety and attachment, anxiety for the baby’s safety and well-being, anxiety about practical baby care, and psychosocial adaptation to motherhood. The total score is calculated by summing the item scores, with a cutoff point of 26 indicating a significant level of anxiety. The original scale demonstrated good reliability (McDonald’s ω = 0.87). The instrument was translated into Brazilian Portuguese by Araújo et al. (2024) and its psychometric properties were evaluated prior to this study, showing a reliability index of ω = 0.77 for the Brazilian population.
Postpartum Bonding Questionnaire (PBQ; Brockington et al., 2006; translated and adapted into Brazilian Portuguese by Baldisserotto et al., 2018, psychometrically validated by Baldisserotto et al., 2022). The questionnaire consists of 12 items, reduced from the original 25 items during the validation process. Participants respond on a scale of 0 (never) to 5 (always), with higher scores indicating difficulties in mother-infant bonding. The Brazilian validated version includes three factors: loss of interest, rejection and anger, and anxiety and risk of abuse. A second-order factor analysis revealed a general Impaired Bonding factor. The reliability of the three dimensions was good (α = 0.83, 0.79, and 0.69), as well as the overall scale (McDonald’s ω = 0.83) used in the present study.
Data analysis
Data were stored at Statistical Package for the Social Sciences (SPSS) (version 28), and all statistical analyses were conducted using Jeffreys’s Amazing Statistics Program (JASP; version 0.15). Descriptive analyses were conducted to examine the characteristics of the participants, including sociodemographic factors, levels of self-compassion and self-criticism, indicators of mental health difficulties (postpartum depression and postpartum anxiety), mother-infant bonding, and perceived impact of the COVID-19 pandemic on quality of life. The Shapiro–Wilk test was used to assess the distribution of variables, with p ≤ 0.05 indicating a non-normal distribution. Only respondents providing full data were included in the analysis. Participants with incomplete data had not answered two or more instruments; therefore, imputation methods were not applied.
Spearman correlation analyses were performed to explore the relationships between the variables. Reference values for interpreting the correlations were applied, considering weak (0.1 to 0.29), moderate (0.3 to 0.49), and strong (values greater than 0.5) correlations (Cohen, 1988). Subsequently, a network analysis was conducted using the Graphical Least Absolute Shrinkage and Selection Operator algorithm (GLASSO; Friedman et al., 2008). This approach allows for the examination of partial correlations, which reveal the associations between variables while controlling for the effects of other variables. This helps to provide a more accurate understanding of the data, avoiding spurious correlations. The resulting graph organizes the variables based on the strength of their associations, with variables having higher centrality indicating more associations (Machado et al., 2015). Additionally, network analysis provides descriptive measures such as centrality indices, which can be utilized to model or predict network processes, including the flow of information through a variable (Costantini et al. 2014). While there are various centrality measures, four commonly used indices include: (1) betweenness, this index indicates the extent to which a node facilitates the flow of information between other nodes in the network; (2) closeness, reflecting the proximity of a variable to others, this index measures the inverse of the sum of the shortest path distances from the node to all others; (3) strength, representing the cumulative weight of paths connecting a node to others, this index signifies the overall influence or importance of the node in the network, and (4) expected influence, this index assesses the extent to which a node is expected to influence others based on its connectivity patterns.
Results
Participants
The sample of this study comprised 189 Brazilian women, aged between 18 and 44 years (M = 31.4; SD = 5.5). Among the participants, 92 resided in Rio Grande do Sul (48.6%), 32 in São Paulo (16.9%), and 9 in Paraná (6.9%), while the remaining participants were distributed across other Brazilian states. The average age of the babies at the time of data collection was 5.19 months (SD = 3.89). Regarding social support, 64% of the mothers indicated having a good support network (n = 121), and 75.1% believed that the pandemic had not affected the number of people who were assisting them during this period (n = 142). Additionally, 60.3% of the sample (n = 114) scored above the cutoff for postpartum depression on the EPDS (≥ 10), while 53.9% (n = 102) scored above the cutoff for postpartum anxiety on the PSAS-BR-RSF-C (≥ 26).
Correlations between sociodemographic and outcome variables
Table 2 shows bivariate Spearman correlations between all study variables. Maternal age demonstrated a significant and moderate association with depression (r = − 0.34; p < 0.001), and a weak association with anxiety (r = − 0.28; p < 0.001) and USR (r = − 0.29; p < 0.001), indicating that older mothers exhibited lower levels of depressive and anxious symptoms as well as reduced self-criticism. Family income exhibited a negative and moderate association with EPDS (r = − 0.30; p < 0.001), suggesting that higher income levels were associated with decreased depression. Individuals with a diagnosis of psychopathology displayed a significant and weak association with depression (r = − 0.28; p < 0.001) and mother-infant bonding (r = − 0.26; p < 0.001), and a moderate correlation with USR (r = 0.35; p < 0.001) and CSR (r = − 0.30; p < 0.001). The perception of social support was weakly linked to depression (r = 0.25; p < 0.001) and USR (r = 0.23; p < 0.001), with a positive perception (e.g., “I believe that I have a good support network”) correlating with reduced depression and self-criticism.
Table 2.
Spearman correlations between demographic and outcome variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Mother’s age | — | ||||||||||
| 2. Education | 0.56** | — | |||||||||
| 3. Family income | 0.52** | 0.48** | — | ||||||||
| 4. Psychopathology | 0.07 | 0.10 | 0.06 | — | |||||||
| 5. Social support | 0.00 | 0.00 | − 0.13 | − 0.03 | — | ||||||
| 6. PSAS-BR | − 0.28** | − 0.12 | − 0.18* | − 0.17* | 0.14 | — | |||||
| 7. EPDS | − 0.34** | − 0.19* | − 0.30** | − 0.28** | 0.25** | 0.61** | — | ||||
| 8. COV19-QoL | − 0.18* | − 0.03 | − 0.07 | − 0.15 | 0.12 | 0.36** | 0.55*** | — | |||
| 9. USR | − 0.29* | − 0.11 | − 0.21* | − 0.35** | 0.23** | 0.52** | 0.71*** | 0.46*** | — | ||
| 10. CSR | 0.17* | 0.07 | 0.13 | 0.30** | − 0.14 | − 0.26** | − 0.48*** | − 0.27** | − 0.61** | — | |
| 11. PBQ-12 | − 0.16 | − 0.02 | − 0.08 | − 0.26** | 0.16 | 0.44** | 0.55** | 0.27** | 0.42** | − 0.17* | — |
Note: *p < 0.01, **p < 0.001. In bold moderate to strong correlation, PSAS-BR Postpartum Specific Anxiety Scale–Short Version for Global Crises, EPDS Edinburgh Postnatal Depression Scale, COV19-QoL COVID-19 – Impact on Quality of Life, USR Uncompassionate Self-Responding, CSR Compassionate Self-Responding, PBQ-12 Postpartum Bonding Questionnaire
Significant associations were observed among all the instruments used in this study. In terms of CSR, negative and weak associations were identified with postpartum anxiety (r = − 0.26; p < 0.001) and the impact of the pandemic on quality of life (r = − 0.27; p < 0.001). Furthermore, negative and moderate associations were found with depression (r = − 0.48; p < 0.001), while impairments in the mother-infant exhibit weak correlations with CSR (r = − 0.17; p = 0.014). As for USR, significant associations were found with all variables, featuring moderate correlations with the perceived impact of the pandemic (r = 0.46; p < 0.001) and mother-infant bonding (r = − 0.42; p < 0.001), and strong correlations with postpartum depression (r = − 0.71; p < 0.005) and anxiety (r = − 0.52; p < 0.001).
Network analysis
In the network analysis, sociodemographic variables such as mother’s age, family income, perception of social support, and diagnosis of psychopathology formed a separate cluster and were independent of the main system. Therefore, these variables were excluded from further analysis. The final model (Fig. 1) revealed that postpartum depression played a central role in the organization of the model, directly linked with postpartum anxiety, impairment in the mother-infant bond, USR, and the impact of the pandemic on quality of life. Impairment in the mother-infant bond was primarily associated with postpartum depression, indicating its dependence on these symptoms. Surprisingly, impaired mother-infant bonding showed no significant relationship with anxiety levels or the perceived impact of the pandemic. Additionally, CSR did not emerge as a significant factor, except for its association with USR. An alternative model (Fig. 2) utilizing the total self-compassion score was conducted, and it exhibited a significant relationship with the rest of the system. However, when considering the separate components of CSR and USR, the association between CSR and the other variables primarily occurred through USR rather than CSR itself.
Fig. 1.
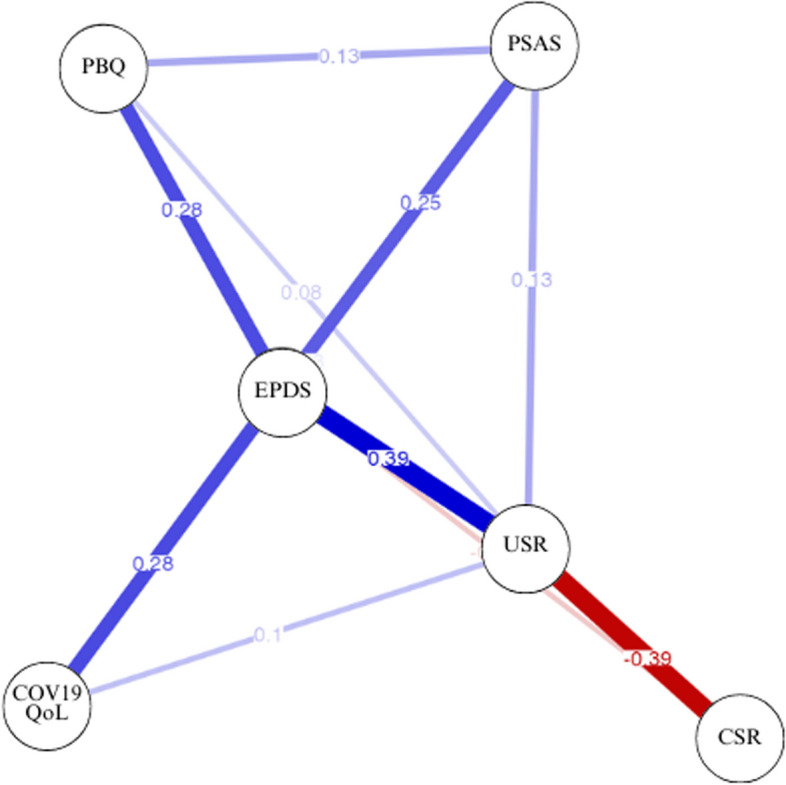
Network analysis (CSR and USR). Note: Abbreviations: COV19-QoL = COVID-19–Impact on Quality of Life; EPDS = Edinburgh Postnatal Depression Scale; PSAS-BR = Postpartum Specific Anxiety Scale–Short Version for Global Crises; PBQ_12 = Postpartum Bonding Questionnaire; USR = Uncompassionate Self-Responding; CSR = Compassionate Self-Responding. Figure provided by JASP (version 0.15)
Fig. 2.
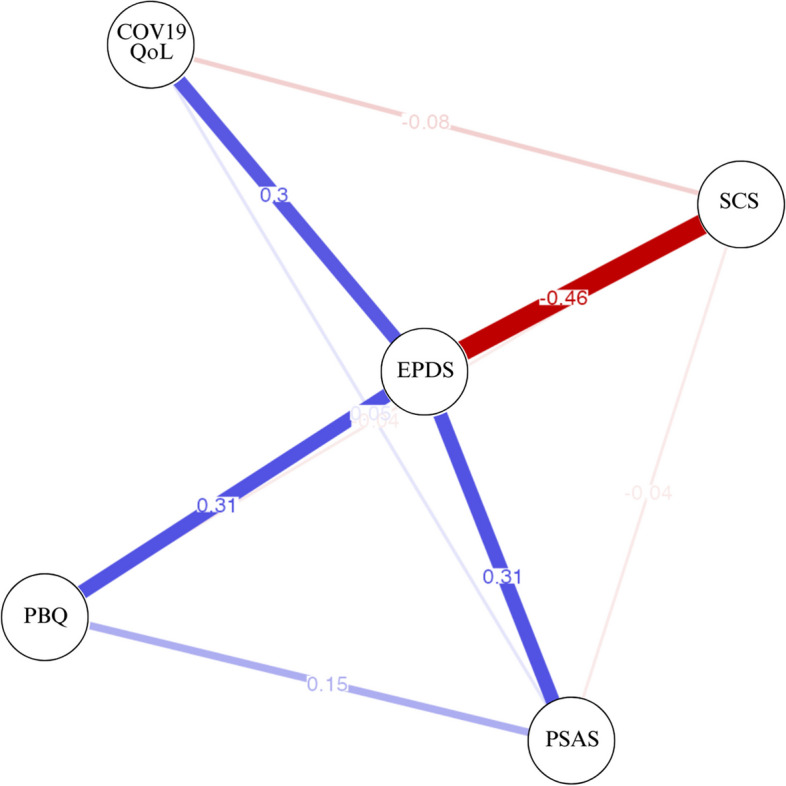
Network analysis (Self-compassion Scale Total Score). Note: Abbreviations: COV19-QoL = COVID-19–Impact on Quality of Life; EPDS = Edinburgh Postnatal Depression Scale; PSAS-BR = Postpartum Specific Anxiety Scale–Short Version for Global Crises; PBQ_12 = Postpartum Bonding Questionnaire; SCS = Self-compassion Scale Total Score. Figure provided by JASP (version 0.15)
Regarding centrality measures, as shown in Table 3, EPDS demonstrates the highest levels of betweenness, closeness, strength, and expected influence, underscoring its substantial influence within the system. Similarly, USR garners a moderately high strength centrality score, indicating its significant importance in the network. Overall, depression and self-criticism emerge as the most influential variables based on their scores, playing pivotal roles in facilitating connections and exerting influence within the network. In contrast, anxiety, CSR, the impact of COVID-19 on quality of life, and mother-infant bonding exhibited lower centrality scores, suggesting that they wield less influence within the network.
Table 3.
Centrality measures per variable
| Network | ||||
|---|---|---|---|---|
| Variable | Betweenness | Closeness | Strength | Expected influence |
| EPDS | 1.84 | 1.77 | 1.54 | 1.43 |
| PSAS-BR | − 0.58 | − 0.65 | − 0.46 | 0.26 |
| USR | 0.49 | 0.63 | 0.98 | -0.16 |
| CSR | − 0.58 | − 0.65 | − 0.62 | -1.68 |
| COV19-QoL | − 0.58 | − 0.55 | − 0.78 | 0.02 |
| PBQ-12 | − 0.58 | − 0.54 | − 0.65 | 0.11 |
Note : EPDS Edinburgh Postnatal Depression Scale, PSAS-BR Postpartum Specific Anxiety Scale–Short Version for Global Crises, COV19-QoL COVID-19–Impact on Quality of Life, PBQ-12 Postpartum Bonding Questionnaire
Discussion
The aim of this study was to investigate the association between self-compassion and self-criticism with maternal mental health outcomes and mother-infant bonding. A cross-sectional design was used and we conducted a network analysis on data obtained from Brazilian mothers. Our findings indicate that self-criticism is strongly and significantly associated with maternal mental health, highlighting its importance in developing potential interventions in this area. Moreover, our results emphasize the importance of regarding compassionate self-responding and uncompassionate self-responding as separate constructs rather than diametrically opposed traits. These findings reinforce existing literature that advocates for incorporating the bi-factor model of the SCS into research and practice (Brenner et al., 2017; Ferrari et al., 2022; Halamová et al., 2021; Muris & Otgaar, 2020).
The reported diagnosis of a psychopathological condition, along with the scores on the EPDS and PSAS-BR-RSF, are crucial factors to consider as they may have influenced the outcomes of this study. The prevalence rates observed in this study are higher than those reported in other Brazilian studies that investigated postpartum depression symptoms during the pandemic, which reported rates of 29.3% of probable cases based on the EPDS (Loret de Mola et al., 2021), as well as international studies that identified a prevalence of 26.7% for depression symptoms and 33.8% for anxiety symptoms (Gao et al., 2022). One explanation for these findings is rooted in the recruitment methodology utilized in this study, which involved the use of social media alongside an image captioned “Participate in research on the mental health of postpartum women.” It is hypothesized that women already receiving mental health care may have been more inclined to participate in this study. In relation to the lack of association between diagnoses and the scores of EPDS and PSAS-BR-RSF-C, one hypothesis is that the questionnaires evaluate current active symptoms, whereas the reported diagnosis pertains to lifelong conditions.
While CSR demonstrated significant correlations with all examined variables, the network analysis model using partial correlations did not support these findings. Specifically, CSR was only associated with USR, suggesting that this was its primary mode of influence. This outcome aligns with recent research advocating for the differentiation of these two constructs (Costa et al., 2016; Halamová et al., 2021; Kumlander et al., 2018; Muris & Otgaar, 2020; Muris & Petrocchi, 2017). Literature suggests that the items assessing self-criticism, which are inversely scored in the total self-compassion score provided by the SCS, may artificially inflate its overall measurement. In the current study, upon exploring the network analysis using the total score and the two separate components, it became evident that CSR lacked significant associations with levels of depression and anxiety unless linked to USR. Conversely, USR exhibited the strongest and most significant correlations with these psychopathologies. Based on these findings, our study concurs with the authors who advocate for measuring CSR and USR, rather than the total factor of the SCS. Additionally, other scales such as the Forms of Self-Criticising and Self-Reassuring Scale (FSCRS; Baião et al., 2015) can be utilized to measure both concepts separately.
One hypothesis for the results concerning CSR is rooted in the perception that self-compassion may be culturally associated with various myths, such as indulgence, weakness, self-pity, complacency, and selfishness (Neff, 2015). Additionally, societal expectations and idealizations of the maternal role may contribute to the amplification of self-criticism when mothers perceive a discrepancy between societal demands and their self-perception (Arrais et al., 2014; Douglas & Michaels, 2005). This misalignment can significantly impact the development and persistence of psychopathological symptoms, necessitating interventions that extend beyond adopting a self-kind posture. Excessive self-criticism may possess deeply ingrained characteristics that cannot be effectively addressed through self-compassion alone. The study aligns with the suggestion made by Halamová et al. (2021) that addressing excessive self-criticism may require adopting an assertive and protective stance.
Network analysis provides valuable insights into potential intervention targets within a system, with the results of this analysis offering significant implications. Notably, the graphical representation of node disposition suggests a potential predictive relationship between USR and levels of depression, which is associated with levels of anxiety and the perceived impact of the COVID-19 pandemic on quality of life. Additionally, corroborating existing literature, depression appears to predict impairments in mother-infant bonding. Considering centrality measures, interventions targeting self-criticism and postpartum depression are crucial for influencing other variables within the network. These findings underscore the interconnectedness of these variables and emphasize the potential efficacy of interventions targeting self-criticism in reducing postpartum depression levels, which could subsequently alleviate impairments in mother-infant bonding.
The low scores related to anxiety symptoms have led to controversial hypotheses. The lack of methodological consensus (Matthey et al., 2003; Pawluski et al., 2017; Silverio et al., 2021), symptoms concealed by measures targeting postpartum depression (Loyal et al., 2020), and discrepancies regarding prevalence (Dennis et al., 2017) suggest a possible underreporting of maternal anxiety cases, as well as greater difficulty in understanding the disorder and identifying its impacts (Dennis et al., 2017; Goodman et al., 2016). In this study, an innovative scale was employed to specifically measure postpartum anxiety (Gerhardt et al.: Psychometric properties of the Postpartum Specific Anxiety Scale research short-form for use during global crises in a Brazilian population (PSAS-BR-RSF-C), in preparation; Silverio et al., 2021), and the results indicate that these symptoms are associated with higher levels of depressive symptoms but do not have a direct impact on the quality of the mother-infant relationship. It is hypothesized that depression symptoms can lead mothers to experience greater difficulties in connecting with their babies, as well as having reduced energy to attend to their needs (Kornfield et al., 2021; Righetti-Veltema et al., 2002). Conversely, maternal anxiety may result in increased concerns regarding the baby and lead to overprotection (Jones et al., 2021). Although the literature highlights the negative impacts of overprotection over time (Van Der Bruggen et al., 2008; Van Petegem et al., 2022), in the context of mother-infant bonding during the first year, it may not necessarily pose an issue. Studies with broader and more representative samples, utilizing specific measures for the assessment of postpartum anxiety, are necessary to initiate the development of a consensus in the literature about this topic.
Although these results suggest potential intervention pathways, it is important to consider the limitations of this study. The sample size and diversity may not allow for generalization to the entire Brazilian population. The majority of participants were residents of Rio Grande do Sul and São Paulo, primarily from urban and well-developed areas. Additionally, the sample predominantly comprised women with higher education levels, which could restrict the generalizability of the findings. Furthermore, data collection was conducted online, and all measures were self-reported, introducing the possibility of uncontrollable biases. The self-reported nature of the data might also be susceptible to social desirability bias, potentially affecting the accuracy of the reported information.
Conclusion
The network analysis conducted in this study offers valuable insights for guiding future interventions. We propose conducting randomized controlled trials (RCTs) to assess the effectiveness of intervention programs aimed at mitigating postpartum depression, with a specific focus on reducing self-criticism and fostering self-compassion strategies. Our findings underscore the importance of addressing cultural misconceptions surrounding self-compassion and cultivating a protective and assertive approach to counteract excessive self-criticism. For instance, interventions like the Emotion-Focused Training for Self-Compassion and Self-Protection (EFT-SCP; Halamová et al., 2021) show promise in this regard. Furthermore, we recommend integrating psychoeducation, psychological flexibility, emotion regulation abilities, and guidance on enhancing social support and parenting skills into these interventions. Moreover, longitudinal studies are highly recommended to assess the sustained impact of these interventions on postpartum depression and mother-infant bonding. Following participants over an extended period will allow for the evaluation of long-term benefits on maternal mental health and child well-being, thus advancing our understanding of effective strategies in this critical area.
Acknowledgements
Not applicable.
Abbreviations
- EPDS
Edinburgh Postnatal Depression Scale
- SCS
Self-Compassion Scale
- CSR
Compassionate Self-Responding
- USR
Uncompassionate Self-Responding
- PSAS-BR-RSF-C
Postpartum Specific Anxiety Scale–Research Short-form–for Global Crises
- PBQ
Postpartum Bonding Questionnaire
- COV19-QoL
COVID-19 Impact on Quality of Life
- CFI
Comparative Fit Index
- TLI
Tucker Lewis Index
- RMSEA
Root mean squared error of approximation
Authors’ contributions
BCG designed the study; collected, analyzed, and interpreted the data; and wrote the manuscript. JGS: analyzed and interpreted the data and wrote the manuscript. CZ collected the data and wrote the manuscript. AXA contributed to the study design and supervised the data collection, analyses, and manuscript writing. All authors made substantial contributions to the preparation and writing of the manuscript. The final version of the manuscript was approved by all the authors, who also provided their consent for their names to be included in the manuscript.
Funding
This study was supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq).
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Declarations
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Angus, B. M., Saling, L. L., & Moffitt, R. L. (2024). Self-compassionate reflective writing for affect regulation in Australian perinatal women. Applied Psychology,16(2), 745–764. 10.1111/aphw.12514 10.1111/aphw.12514 [DOI] [PubMed] [Google Scholar]
- Aoyagi, S. S., Takei, N., Nishimura, T., Nomura, Y., & Tsuchiya, K. J. (2019). Association of late-onset postpartum depression of mothers with expressive language development during infancy and early childhood: The HBC study. PeerJ,7, e6566.y. 10.7717/peerj.6566 10.7717/peerj.6566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arrais, A. D., Mourão, M. A., & Fragalle, B. (2014). O pré-natal psicológico como programa de prevenção à depressão pós-parto [Psychological prenatal care as a prevention program for postpartum depression]. Saúde e Sociedade,23(1), 251–264. 10.1590/S0104-12902014000100020 10.1590/S0104-12902014000100020 [DOI] [Google Scholar]
- Auerbach, R. P., Ho, M. H. R., & Kim, J. C. (2014). Identifying cognitive and interpersonal predictors of adolescent depression. Journal of Abnormal Child Psychology,42(6), 913–924. 10.1007/s10802-013-9845-6 10.1007/s10802-013-9845-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baião, R., Gilbert, P., McEwan, K., & Carvalho, S. (2015). Forms of self-criticising/attacking & self-reassuring scale: Psychometric properties and normative study. Psychology and Psychotherapy,88(4), 438–452. 10.1111/papt.12049 10.1111/papt.12049 [DOI] [PubMed] [Google Scholar]
- Baldisserotto, M. L., Griep, R. H., Oates, J., & Theme-Filha, M. M. (2022). Cross-cultural adaptation of the Postpartum Bonding Questionnaire (PBQ) to Brazil: Assessment of the measurement properties of construct validity and reliability. Current Psychology,42(30), 26275–26285. 10.1007/s12144-022-03742-3 10.1007/s12144-022-03742-3 [DOI] [Google Scholar]
- Baldisserotto, M. L., Theme-Filha, M. M., Griep, R. H., Oates, J., Renó Junior, J., & Cavalsan, J. P. (2018). Transcultural adaptation to the Brazilian Portuguese of the Postpartum Bonding Questionnaire for assessing the postpartum bond between mother and baby. Cadernos De Saúde Pública,34(7), e00170717. 10.1590/0102-311X00170717 10.1590/0102-311X00170717 [DOI] [PubMed] [Google Scholar]
- Brenner, R. E., Heath, P. J., Vogel, D. L., & Credé, M. (2017). Two is more valid than one: Examining the factor structure of the Self-Compassion Scale (SCS). Journal of Counseling Psychology,64(6), 696. 10.1037/cou0000211 10.1037/cou0000211 [DOI] [PubMed] [Google Scholar]
- Brockington, I. F., Fraser, C., & Wilson, D. (2006). The Postpartum Bonding Questionnaire: A validation. Archives of Women’s Mental Health,9(5), 233–242. 10.1007/s00737-006-0132-1 10.1007/s00737-006-0132-1 [DOI] [PubMed] [Google Scholar]
- Cantwell, R. (2021). Mental disorder in pregnancy and the early postpartum. Anaesthesia,76, 76–83. 10.1111/anae.15424 10.1111/anae.15424 [DOI] [PubMed] [Google Scholar]
- Chen, Q., Li, W., Xiong, J., & Zheng, X. (2022). Prevalence and risk factors associated with postpartum depression during the COVID-19 pandemic: A literature review and meta-analysis. International Journal of Environmental Research and Public Health,19(4), 2219. 10.3390/ijerph19042219 10.3390/ijerph19042219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, J. (1988). Statistical Power Analysis for the Behavioral Sciences (2nd ed.). Routledge. 10.4324/9780203771587
- Cohen, J. R., Young, J. F., Hankin, B. L., Yao, S., Zhu, X. Z., & Abela, J. R. (2013). Personality predispositions in Chinese adolescents: The relation between self- criticism, dependency, and prospective internalizing symptoms. Journal of Social and Clinical Psychology,32(6), 596. 10.1521/jscp.2013.32.6.596 10.1521/jscp.2013.32.6.596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa, J., Marôco, J., Pinto-Gouveia, J., Ferreira, C., & Castilho, P. (2016). Validation of the psychometric properties of the self-compassion scale: testing the factorial validity and factorial invariance of the measure among borderline personality disorder, anxiety disorder, eating disorder and general populations. Clin Psychol Psychother,23(5), 460–468. 10.1002/cpp.1974 10.1002/cpp.1974 [DOI] [PubMed] [Google Scholar]
- Costantini, G., Epskamp, S., Borsboom, D., Perugini, M., Mõttus, R., Waldorp, L. J., & Cramer, A. O. (2015). State of the aRt personality research: A tutorial on network analysis of personality data in R. Journal of Research in Personality,54, 13–29. 10.1016/j.jrp.2014.07.003 10.1016/j.jrp.2014.07.003 [DOI] [Google Scholar]
- Cox, J. L., Holden, J. M., & Sagovsky, R. (1987). Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. The British Journal of Psychiatry,150(6), 782–786. 10.1192/bjp.150.6.782 10.1192/bjp.150.6.782 [DOI] [PubMed] [Google Scholar]
- de Araújo, K. M. S. T., Wendland, J., Souza, B. D. F. R., de Melo, M. G., Araújo, L. T., & Baptista, R. S. (2024). Adaptação transcultural e validade de conteúdo da Postpartum Specific Anxiety Scale (PSAS) para o português brasileiro [Cross-cultural adaptation and content validity of the Postpartum Specific Anxiety Scale (PSAS) for Brazilian Portuguese]. Revista Eletrônica Acervo Saúde,24(1), e14243–e14243. 10.25248/reas.e14243.2024 10.25248/reas.e14243.2024 [DOI] [Google Scholar]
- de Souza, L. K., & Hutz, C. S. (2016). Adaptation of the self-compassion scale for use in Brazil: Evidences of construct validity. Temas Em Psicologia,24(1), 159–172. 10.9788/TP2016.1-11 10.9788/TP2016.1-11 [DOI] [Google Scholar]
- Dennis, C. L., Falah-Hassani, K., & Shiri, R. (2017). Prevalence of antenatal and postnatal anxiety: Systematic review and meta-analysis. The British Journal of Psychiatry,210(5), 315–323. 10.1192/bjp.bp.116.187179 10.1192/bjp.bp.116.187179 [DOI] [PubMed] [Google Scholar]
- Douglas, S., & Michaels, M. (2005). The mommy myth: The idealization of motherhood and how it has undermined all women. Free Press. [Google Scholar]
- Fallon, V., Silverio, S. A., Halford, J. C. G., Bennett, K. M., & Harrold, J. A. (2021). Postpartum-specific anxiety and maternal bonding: Further evidence to support the use of childbearing specific mood tools. Journal of Reproductive and Infant Psychology,39(2), 114–124. 10.1080/02646838.2019.1680960 10.1080/02646838.2019.1680960 [DOI] [PubMed] [Google Scholar]
- Felder, J. N., Lemon, E., Shea, K., Kripke, K., & Dimidjian, S. (2016). Role of self- compassion in psychological well-being among perinatal women. Archives of Women’s Mental Health,19(4), 687–690. 10.1007/s00737-016-0628-2 10.1007/s00737-016-0628-2 [DOI] [PubMed] [Google Scholar]
- Fennig, S., Hadas, A., Itzhaky, L., Roe, D., Apter, A., & Shahar, G. (2008). Self-criticism is a key predictor of eating disorder dimensions among inpatient adolescent females. International Journal of Eating Disorders,41(8), 762–765. 10.1002/eat.20573 10.1002/eat.20573 [DOI] [PubMed] [Google Scholar]
- Fernandes, D. V., Canavarro, M. C., & Moreira, H. (2021). Postpartum during COVID-19 pandemic: Portuguese mothers’ mental health, mindful parenting, and mother-infant bonding. Journal of Clinical Psychology,77(9), 1997–2010. 10.1002/jclp.23130 10.1002/jclp.23130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrari, M., Ciarrochi, J., Yap, K., Sahdra, B., & Hayes, S. C. (2022). Embracing the complexity of our inner worlds: Understanding the dynamics of self-compassion and self-criticism. Mindfulness,13(7), 1652–1661. 10.1007/s12671-022-01897-5 10.1007/s12671-022-01897-5 [DOI] [Google Scholar]
- Fonseca, A., & Canavarro, M. C. (2018). Exploring the paths between dysfunctional attitudes towards motherhood and postpartum depressive symptoms: The moderating role of self-compassion. Clinical Psychology & Psychotherapy,25(1), e96–e106. 10.1002/cpp.2145 10.1002/cpp.2145 [DOI] [PubMed] [Google Scholar]
- Fonseca, A., Monteiro, F., Alves, S., Gorayeb, R., & Canavarro, M. C. (2019). Be a mom, a web-based intervention to prevent postpartum depression: The enhancement of self-regulatory skills and its association with postpartum depressive symptoms. Frontiers in Psychology,10, 265. 10.3389/fpsyg.2019.00265 10.3389/fpsyg.2019.00265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman, J., Hastie, T., & Tibshirani, R. (2008). Sparse inverse covariance estimation with the graphical lasso. Biostatistics,9(3), 432–441. 10.1093/biostatistics/kxm045 10.1093/biostatistics/kxm045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao, S., Su, S., Zhang, E., Liu, R., Zhang, Y., Wang, C., Liu, J., Xie, S., Yin, C., & Yue, W. (2022). Psychological health status in postpartum women during COVID-19 pandemic: A systematic review and meta-analysis. Journal of Affective Disorders,319, 99–111. 10.1016/j.jad.2022.08.107 10.1016/j.jad.2022.08.107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman, J. H., Watson, G. R., & Stubbs, B. (2016). Anxiety disorders in postpartum women: A systematic review and meta-analysis. Journal of Affective Disorders,203, 292–331. 10.1016/j.jad.2016.05.033 10.1016/j.jad.2016.05.033 [DOI] [PubMed] [Google Scholar]
- Gravener, J. A., Rogosch, F. A., Oshri, A., Narayan, A. J., Cicchetti, D., & Toth, S. L. (2012). The relations among maternal depressive disorder, maternal expressed emotion, and toddler behavior problems and attachment. Journal of Abnormal Child Psychology,40(5), 803–813. 10.1007/s10802-011-9598-z 10.1007/s10802-011-9598-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo, L., Zhang, J., Mu, L., & Ye, Z. (2020). Preventing postpartum depression with mindful self-compassion intervention: A randomized control study. The Journal of Nervous and Mental Disease,208(2), 101–107. 10.1097/NMD.0000000000001096 10.1097/NMD.0000000000001096 [DOI] [PubMed] [Google Scholar]
- Halamová, J., Kanovský, M., Varšová, K., & Kupeli, N. (2021). Randomised controlled trial of the new short-term online emotion focused training for self-compassion and self- protection in a nonclinical sample. Current Psychology,40(1), 333–343. 10.1007/s12144-018-9933-4 10.1007/s12144-018-9933-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inwood, E., & Ferrari, M. (2018). Mechanisms of change in the relationship between self- compassion, emotion regulation, and mental health: A systematic review. Applied Psychology: Health and Well-Being,10(2), 215–235. 10.1111/aphw.12127 10.1111/aphw.12127 [DOI] [PubMed] [Google Scholar]
- Jones, L. B., Hall, B. A., & Kiel, E. J. (2021). Systematic review of the link between maternal anxiety and overprotection. Journal of Affective Disorders,295, 541–551. 10.1016/j.jad.2021.08.065 10.1016/j.jad.2021.08.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kornfield, S. L., White, L. K., Waller, R., Njoroge, W., Barzilay, R., Chaiyachati, B. H., ... & Gur, R. E. (2021). Risk and resilience factors influencing postpartum depression and mother-infant bonding during COVID-19. Health Affairs, 40(10), 1566–1574. 10.1377/hlthaff.2021.00803 [DOI] [PMC free article] [PubMed]
- Kumlander, S., Lahtinen, O., Turunen, T., & Salmivalli, C. (2018). Two is more valid than one, but is six even better? The factor structure of the Self-Compassion Scale (SCS). PLoS ONE,13(12), e0207706. 10.1371/journal.pone.0207706 10.1371/journal.pone.0207706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- López, A., Sanderman, R., Smink, A., Zhang, Y., Van Sonderen, E., Ranchor, A., & Schroevers, M. J. (2015). A reconsideration of the Self-Compassion Scale’s total score: Self-compassion versus self-criticism. PLoS ONE,10(7), e0132940. 10.1371/journal.pone.0132940 10.1371/journal.pone.0132940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loret de Mola, C., Martins-Silva, T., Carpena, M. X., Del-Ponte, B., Blumenberg, C., Martins, R. C., Dias, I. M., Terribele, F. B., de Avila, A. B., Marmitt, L. P., Meucci, R., & Cesar, J. A. (2021). Maternal mental health before and during the COVID-19 pandemic in the 2019 Rio Grande birth cohort. Revista Brasileira De Psiquiatria,43(4), 402–406. 10.1590/1516-4446-2020-1673 10.1590/1516-4446-2020-1673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loyal, D., Sutter, A. L., & Rascle, N. (2020). Screening beyond postpartum depression: Occluded anxiety component in the EPDS (EPDS-3A) in French mothers. Maternal and Child Health Journal,24, 369–377. 10.1007/s10995-020-02885-8 10.1007/s10995-020-02885-8 [DOI] [PubMed] [Google Scholar]
- MacBeth, A., & Gumley, A. (2012). Exploring compassion: A meta-analysis of the association between self-compassion and psychopathology. Clinical Psychology Review,32(6), 545–552. 10.1016/j.cpr.2012.06.003 10.1016/j.cpr.2012.06.003 [DOI] [PubMed] [Google Scholar]
- Machado, W. D. L., Vissoci, J., & Epskamp, S. (2015). Análise de rede aplicada à Psicometria e à Avaliação Psicológica. Psicometria, 125–146.
- Mantelou, A., & Karakasidou, E. (2017). The effectiveness of a brief self-compassion intervention program on self-compassion, positive and negative affect and life satisfaction. Psychology,8, 590–610. 10.4236/psych.2017.84038 10.4236/psych.2017.84038 [DOI] [Google Scholar]
- Matthey, S., Barnett, B., Howie, P., & Kavanagh, D. J. (2003). Diagnosing postpartum depression in mothers and fathers: Whatever happened to anxiety? Journal of Affective Disorders,74(2), 139–147. 10.1016/S0165-0327(02)00012-5 10.1016/S0165-0327(02)00012-5 [DOI] [PubMed] [Google Scholar]
- Mills, A., Gilbert, P., Bellew, R., McEwan, K., & Gale, C. (2007). Paranoid beliefs and self- criticism in students. Clinical Psychology & Psychotherapy,14(5), 358–364. 10.1002/cpp.537 10.1002/cpp.537 [DOI] [Google Scholar]
- Muris, P., & Otgaar, H. (2020). The process of science: A critical evaluation of more than 15 years of research on self-compassion with the Self-Compassion Scale. Mindfulness,11(6), 1469–1482. 10.1007/s12671-020-01363-0 10.1007/s12671-020-01363-0 [DOI] [Google Scholar]
- Muris, P., Otgaar, H., López, A., Kurtic, I., & van de Laar, I. (2021). The (non) protective role of self-compassion in internalizing symptoms: Two empirical studies in adolescents demonstrating unwanted effects of using the Self-Compassion Scale total score. Mindfulness,12, 240–252. 10.1007/s12671-020-01514-3 10.1007/s12671-020-01514-3 [DOI] [Google Scholar]
- Muris, P., & Petrocchi, N. (2017). Protection or vulnerability? A meta-analysis of the relations between the positive and negative components of self-compassion and psychopathology. Clinical Psychology & Psychotherapy,24(2), 373–383. 10.1002/cpp.2005 10.1002/cpp.2005 [DOI] [PubMed] [Google Scholar]
- Murray, L., & Cooper, P. J. (1996). The impact of postpartum depression on child development. International Review of Psychiatry,8(1), 55–63. 10.3109/09540269609037817 10.3109/09540269609037817 [DOI] [Google Scholar]
- Neff, K. D. (2003). The development and validation of a scale to measure self-compassion. Self and Identity,2, 223–250. 10.1080/15298860309027 10.1080/15298860309027 [DOI] [Google Scholar]
- Neff, K. D. (2015). The five myths of self-compassion. Psychotherapy Networker,39(5), 30–35. [Google Scholar]
- Neff, K. D., Kirkpatrick, K. L., & Rude, S. S. (2007). Self-compassion and adaptive psychological functioning. Journal of Research in Personality,41(1), 139–154. 10.1016/j.jrp.2006.03.004 10.1016/j.jrp.2006.03.004 [DOI] [Google Scholar]
- Pawluski, J. L., Lonstein, J. S., & Fleming, A. S. (2017). The neurobiology of postpartum anxiety and depression. Trends in Neurosciences,40(2), 106–120. 10.1016/j.tins.2016.11.009 10.1016/j.tins.2016.11.009 [DOI] [PubMed] [Google Scholar]
- Pedro, L., Branquinho, M., Canavarro, M. C., & Fonseca, A. (2019). Self-criticism, negative automatic thoughts and postpartum depressive symptoms: The buffering effect of self- compassion. Journal of Reproductive and Infant Psychology,37(5), 539–553. 10.1080/02646838.2019.1597969 10.1080/02646838.2019.1597969 [DOI] [PubMed] [Google Scholar]
- Repišti, S., Jovanović, N., Kuzman, M. R., Medved, S., Jerotić, S., Ribić, E., Majstorović, T., Simoska, S. M., Novotni, L., Milutinović, M., Stoilkovska, B. B., Radojičić, T., Ristić, I., Zebić, M., Pemovska, T., & Russo, M. (2020). How to measure the impact of the COVID-19 pandemic on quality of life: COV19-QoL, the development, reliability and validity of a new scale. Global Psychiatry. 10.2478/gp-2020-0016 10.2478/gp-2020-0016 [DOI] [Google Scholar]
- Righetti-Veltema, M., Conne-Perréard, E., Bousquet, A., & Manzano, J. (2002). Postpartum depression and mother–infant relationship at 3 months old. Journal of Affective Disorders,70(3), 291–306. 10.1016/S0165-0327(01)00367-6 10.1016/S0165-0327(01)00367-6 [DOI] [PubMed] [Google Scholar]
- Rocha, N. A. C. F., Dos Santos Silva, F. P., Dos Santos, M. M., & Dusing, S. C. (2020). Impact of mother-infant interaction on development during the first year of life: A systematic review. Journal of Child Health Care,24(3), 365–385. 10.1177/1367493519864742 10.1177/1367493519864742 [DOI] [PubMed] [Google Scholar]
- Santos, I. S., Matijasevich, A., Tavares, B. F., Barros, A. J. D., Botelho, I. P., Lapolli, C., da Magalhães, P. V., S. Barbosa, A. P. P. N., & Barros, F. C. (2007). Validation of the Edinburgh Postnatal Depression Scale (EPDS) in a sample of mothers from the 2004 Pelotas Birth Cohort Study. Cadernos de Saúde Pública,23(11), 2577–2588. 10.1590/S0102-311X2007001100005 10.1590/S0102-311X2007001100005 [DOI] [PubMed] [Google Scholar]
- Silverio, S. A., Davies, S. M., Christiansen, P., Aparicio-García, M. E., Bramante, A., Chen, P., Costas-Ramón, N., de Weerth, C., Della Vedova, A. M., Infante Gil, L., Lustermans, H., Wendland, J., Xu, J., Halford, J. C. G., Harrold, J. A., & Fallon, V. (2021). A validation of the Postpartum Specific Anxiety Scale 12-item research short- form for use during global crises with five translations. BMC Pregnancy and Childbirth,21(1), 112. 10.1186/s12884-021-03597-9 10.1186/s12884-021-03597-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson, K. M., Semenchuk, B. N., & Strachan, S. M. (2021). Put MY mask on first: Mothers’ reactions to prioritizing health behaviours as a function of self-compassion and fear of self-compassion. Journal of Health Psychology,27(5), 1259–1266. 10.1177/1359105321995979 10.1177/1359105321995979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slomian, J., Honvo, G., Emonts, P., Reginster, J. Y., & Bruyère, O. (2019). Consequences of maternal postpartum depression: A systematic review of maternal and infant outcomes. Women’s Health,15, 1745506519844044. 10.1177/1745506519844044 10.1177/1745506519844044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Der Bruggen, C. O., Stams, G. J. J., & Bögels, S. M. (2008). Research review: the relation between child and parent anxiety and parental control: a meta-analytic review. J Child Psychol Psychiatry,49(12), 1257–1269. 10.1111/j.1469-7610.2008.01898.x 10.1111/j.1469-7610.2008.01898.x [DOI] [PubMed] [Google Scholar]
- Van Petegem, S., Albert Sznitman, G., Darwiche, J., & Zimmermann, G. (2022). Putting parental overprotection into a family systems context: Relations of overprotective parenting with perceived coparenting and adolescent anxiety. Family Process,61(2), 792–807. 10.1111/famp.12709 10.1111/famp.12709 [DOI] [PubMed] [Google Scholar]
- Werner, A. M., Tibubos, A. N., Rohrmann, S., & Reiss, N. (2019). The clinical trait self- criticism and its relation to psychopathology: A systematic review–Update. Journal of Affective Disorders,246, 530–547. 10.1016/j.jad.2018.12.069 10.1016/j.jad.2018.12.069 [DOI] [PubMed] [Google Scholar]
- Whittingham, K., & Mitchell, A. E. (2021). Birth, breastfeeding, psychological flexibility and self-compassion as predictors of mother–infant emotional availability in a cross- sectional study. Infant Mental Health Journal,42(5), 718–730. 10.1002/imhj.21935 10.1002/imhj.21935 [DOI] [PubMed] [Google Scholar]
- Zessin, U., Dickhäuser, O., & Garbade, S. (2015). The relationship between self-compassion and well-being: A meta-analysis. Applied Psychology,7(3), 340–364. 10.1111/aphw.12051 10.1111/aphw.12051 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


