Abstract
Background
Patient satisfaction is a crucial indicator of a successful dental implant treatment. Attainment of an aesthetically acceptable final result is central to this success. Hence, the primary objective of this systematic review was to identify aesthetic concerns linked to dental implants within the aesthetic zone.
Methods
An electronic search was conducted on different databases such as PubMed, Medline, and Google Scholar using the key terms “tooth implant,” “anterior implant,” “dental implantation in the aesthetic zone,” and “aesthetic area implant. Following the elimination of duplicate articles and adherence to the inclusion criteria, 14 articles (five randomized clinical trials, four prospective clinical trials, four case series, and one pilot study) published between 2007 and 2020 were deemed suitable for this review.
Results
The selected studies highlighted several aesthetic issues, such as recession, marginal bone loss, gingival loss, and pink aesthetic scores related to dental implants placed in the aesthetic zone.
Conclusion
Addressing these challenges necessitates meticulous treatment planning, effective soft tissue management, regular follow-ups, patient education, expectation management, and collaborative efforts among specialists. A limitation of this systematic review is that it focused solely on studies conducted within a relatively short timeframe (2007–2020). However, it is essential to recognize that significant changes occurred in the treatment procedures and materials within the field during this period. These changes have resulted in notable variances in the treatment protocols utilized across studies, potentially affecting the generalizability of the findings.
Keywords: Dental implants, Aesthetic, Aesthetic zone, Recession, Gingival loss
1. Introduction
In the human mouth, the aesthetic zone extends from canine to canine but may extend to the first or second premolar, depending on the width of the smile. Smile aesthetics are particularly important in this zone; thus, the placement of an implant-supported prosthesis is particularly challenging and complex. Patients have high demands and expectations for procedures performed in this area; therefore, a more comprehensive assessment of this area is needed using different elements of aesthetics (Brägger et al., 2005). Aesthetic implant restorations are defined as those that resemble natural teeth in different aspects (Higginbottom et al., 2004). For example, the placement of a single implant-supported prosthesis in the anterior maxilla can be compared with adjacent natural teeth to achieve a high aesthetic standard (Chang et al., 1999). However, the placement of implant-supported prostheses in the aesthetic zone is highly challenging because the surrounding soft tissues and prostheses are fully visible during a smile, making it an exceedingly sensitive area for patients (Higginbottom et al., 2004). According to the Straightforward, Advanced, and Complex classification system of the International Team for Implantology, implants placed in the anterior maxilla and mandible are considered advanced or complex, depending on the sensitivity of the technique used to replace missing teeth in the aesthetic zone (Paquette et al., 2006).
Placing implant-supported restorations in the edentulous aesthetic area of the maxilla poses a surgical and prosthetic challenge for the specialist, as this requires dealing mostly with medullary bone with low density and the need to consider the absence of the papilla as a pre-existing condition, a low volume of gingiva on the buccal side, a marginal level of soft tissue, the biotypes of gingiva, the visibility of the future restoration of the implant during speech and smiling, and the visibility of the peri-implant mucosa in patients with a high smile line (Cho et al., 2015, Fürhauser et al., 2005, Marković et al., 2022). Challenges that can affect the success rate of implants in aesthetic zones include changes in the peri-implant soft tissue level, prosthesis level, and patients’ subjective assessments. Dentists should consider these parameters when evaluating the success or failure of implant dentistry (Papaspyridakos et al., 2012). There are many soft tissue changes caused by the resorption of the alveolar bone, particularly in the buccal wall, after dental extractions, which can lead to the retraction of soft tissues and dental papilla loss after multiple extractions (Abd-Elrahman et al., 2020). The periodontal ligament and its vascular supply can be lost owing to the mechanisms involved in periodontal healing after tooth extraction (Bramanti et al., 2018). This process can lead to aesthetic problems in the aesthetic zone that cannot be resolved by performing restorations to preserve the emergence profile of the aesthetic area. The maintenance of aesthetics can be achieved only by preserving the bone anatomy and architecture of the soft tissue in the anterior region with the help of implant-supported restorations (Han et al., 2018).
Visual satisfaction of an implant-supported prosthesis and its surrounding soft tissues without any dehiscence or fenestration in the aesthetic zone is considered an important factor in the success of implants in this zone and depends on both white and pink aesthetics (Tettamanti et al., 2016). It is well-documented that implants usually work well in the long term (Becker et al., 2016). However, if the bone in the visible area shrinks before receiving an implant-supported tooth, it may affect the success of a standard implant procedure (Qabbani et al., 2017). Although immediate and delayed implants have similar rates of survival, the duration of treatment is reduced with immediate implants, with enhanced maintenance of soft and hard tissue that facilitates the placement of implants in an ideal position (Esposito et al., 2017, Esposito et al., 2010). Many risk factors leading to implant failure in the aesthetic zone, especially in the maxilla, may already be present in the patient, and anatomical changes and bone remodeling can occur even after atraumatic tooth loss. In the aesthetic zone, a major component of implant success is the appearance of soft tissue, which is one of the main considerations for patients seeking treatment with implant-supported prostheses in this region (Farmer and Darby, 2014).
The perception of aesthetics is subjective, varies from patient to patient, and can be greatly influenced by socioeconomic status (Alkhatib et al., 2004). Moreover, the aesthetic outcomes of the procedures are appreciated more among patients than among prosthodontists (Chang et al., 1999). Successful implants depend on osseointegration during the healing process and the stability and functional loading of the implants (Rokn et al., 2014).
The primary objective of this systematic review was to identify aesthetic concerns associated with dental implants within the aesthetic zone.
2. Methodology
2.1. Databases and search strategy
A thorough electronic search encompassed multiple databases—PubMed, Scopus, ScienceDirect, Embase, Google Scholar, and Web of Science—to gather international literature published between 2007 and 2020. This search utilized diverse Medical Subject Heading terms such as “tooth implant,” “anterior implant,” “immediate implant,” “dental implants,” “dental implantation in the aesthetic zone,” “aesthetic area implant,” and terms related to issues in aesthetic implants within the aesthetic zone.
2.2. Study selection
The titles and abstracts were screened using specific criteria for inclusion and exclusion. Data extraction for relevant variables was performed by the author, and a systematic review was conducted.
The inclusion criteria included prospective randomized clinical trials (RCTs), retrospective studies, and case series in the databases. RCTs were not the sole focus because of their limited availability, and this study aimed to offer a comprehensive overview. The included RCTs effectively addressed pertinent inquiries, such as follow-up duration and aesthetic considerations—marginal bone loss and recession associated with implants in aesthetic zones. The included studies analyzed clinical and/or radiographic aspects, such as marginal bone loss, soft tissue outcomes, and pink esthetic scores post-dental implant placement in the aesthetic zone, involving patients aged 18 years or older.
The exclusion criteria were systematic literature reviews, editorials, studies with patients under 18 years of age, and publications in languages other than English.
2.3. Study outcomes and data extraction
The following data were collected from all the articles, including the author, publication year, study type, patient count and age range, number of dental implants, duration of follow-up, and aesthetic issues such as marginal bone loss, soft tissue outcomes, and pink esthetic scores. This data was duplicated by extracting it using predefined Excel spreadsheets.
3. Results
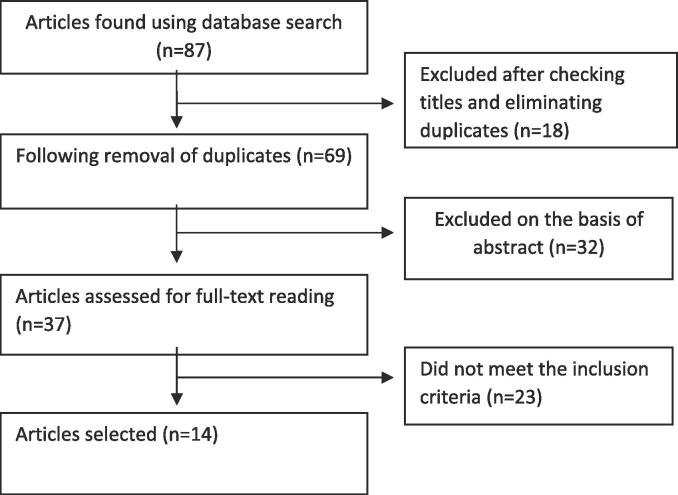
In December 2023, an initial electronic search was conducted across various databases including PubMed, Web of Science, Embase, Scopus, ScienceDirect, and Google Scholar. Of the 87 initially identified studies, 18 duplicates were excluded. After screening titles and abstracts, 32 additional studies were excluded, leaving 37 studies. Subsequently, 23 studies were found unsuitable based on the inclusion criteria. Ultimately, 14 articles met all the criteria and were included in this systematic review, providing comprehensive data on the issues related to dental implants in the aesthetic zone (Fig. 1).
Fig. 1.
Search strategy for related articles.
Among the 14 articles included, five were RCTs (Barakat et al., 2017, Bramanti et al., 2018, De Rouck et al., 2009, Esposito et al., 2011, Guljé et al., 2013), four were prospective clinical trials (Abadzhiev et al., 2014, Han et al., 2018, Mitsias et al., 2020, Rossi et al., 2010), four were case series (Cosyn et al., 2011, Hinze et al., 2018, Kan et al., 2007, Nguyen et al., 2020), and one was a pilot study (Pohl et al., 2020). These studies varied in sample size, ranging from three to 49 participants, with participants aged between 18 and 87 years. The follow-up durations across these studies ranged from 3 to 72 months. Detailed outcomes are presented in Table 1.
Table 1.
Characteristics of included studies.
| Author | Study type | No. of patients | Age (years) | No. of implants | Follow-up period (months) | Aesthetic problems |
|---|---|---|---|---|---|---|
| Bramanti et al., 2018 [9] | RCT | 40 | NA | 40 | 36 |
CIIP: PAS: 10.30 ± 2.53 SST: PAS = 12.15 ± 0.76 |
| Han et al., 2018 [10] | Prospective clinical trial | 30 | 20–82 | 40 | 12 |
SST: change in the gingival margin = 0.17 ± 0.67 mm SST: eight out of 15 patients experience recession |
| De Rouck et al., 2009 [19] | RCT | 24 | ≥ 18 | 24 | 12 | Mid facial recession = 0.41 mm |
| Esposito et al., 2011 [20] | RCT | 30 | NA | 59 | 12 | Marginal bone loss = 0.97 ± 0.56 |
| Gulje et al. 2012 [21] | RCT | 49 | 20–70 | 104 | 12 | Marginal bone loss = 0.2 ± 0.22 |
| Barakat et al., 2017 [22] | RCT | 20 | 20–50 | 20 | 7 |
CIIP: 2.12 ± 0.64 mm probing depth and 1.61 ± 0.78 mm vertical bone loss SST: 1.73 ± 0.28 mm probing depth and 0.44 ± 0.24 mm vertical bone loss |
| Rossi et al., 2010 [23] | Prospective | 35 | ≥ 18 | 38 | 24 | Marginal bone loss = 0.75 ± 0.71 |
| Abadzhiev et al., 2014 [24] | Prospective clinical trial | 25 | 20–64 | 26 | 24 |
CIIP: 12 % bone loss (5 mm) and gingiva loss (5 mm) SST: 0.8 mm bone loss (2 %) attached gingiva (2 %) |
| Mitsias et al., 2020 [25] | Prospective clinical trial | 10 | ≥ 18 | 10 | 42 |
SST: mid-facial recession = 0.19 mm (0.10–0.28 mm) |
| Kan et al. 2007 [26] | Case series | 23 | 25–63 | 23 | 12 | Mid facial recession = 34.8 % Showed > 1.5 mm recession |
| Cosyn et al., 2011 [27] | Case series | 25 | ≥ 18 | 25 | 36 | Mid facial recession = 0.34 mm PAS = Mean 10.48, 16 %, ≤7 |
| Hinze et al., 2018 [28] | Case series | 15 | 26–66 | 17 | 3 | SST: mesial papilla height change (0.31 ± 0.64 mm) and distal papilla height change (0.38 ± 0.57 mm) |
| Nguyen et al., 2019 [29] | Case series | 3 | 62–87 | 4 | 24–72 | No changes in soft tissue dimensions while using SST. |
| Pohl et., 2019 [30] | Pilot study | 12 | ≥ 18 | 12 | 12 | The defect of the buccal alveolar bone was 4.96 mm (min, 2.26 mm; max, 9.68 mm), and the mean mesio-distal extension was 4.25 mm (min, 3.2 mm; max, 5.91 mm). |
RCT, randomized controlled trial; PAS, pink aesthetic score; SST, socket shield technique; CIIP, conventional immediate implant placement.
The main aesthetic concerns identified in the selected studies were marginal bone loss, midfacial recession, and gingival loss. Several studies indicated a midfacial recession ranging from 0.34 to 1.5 mm to be an aesthetic problem after receiving dental implants in the aesthetic zone (Cosyn et al., 2011, De Rouck et al., 2009, Han et al., 2018, Kan et al., 2007, Mitsias et al., 2020) Only two studies mentioned the pink aesthetic score. The mean scores were 10.48 in a study (Cosyn et al., 2011) and 12.15 ± 0.76 in another study (Bramanti et al., 2018) that used the socket shield technique (SST) for dental implants. Other challenges related to aesthetics that were examined in the selected studies were gingival loss (Han et al., 2018, Abadzhiev et al., 2014), probing depth (Barakat et al., 2017), change in papilla height (Hinze et al., 2018), and defects in the buccal alveolar bone (Pohl et al., 2020).
Only three studies compared the two techniques (SST and (Conventional immediate implant placement) CIIP) for dental implants, and SST showed more promising results in all three studies. The rate of aesthetic problems such as probing depth and bone loss was higher in CIIP (Abadzhiev et al., 2014, Barakat et al., 2017, Bramanti et al., 2018).
4. Discussion
This systematic review focused on examining the aesthetic issues associated with dental implants in the aesthetic zone, including concerns such as marginal bone loss, alterations in soft tissues, and achieving desirable pink aesthetics. Over the past ten years, advancements in implant dentistry have fostered a deeper recognition of the aesthetic expectations of both clinicians and patients. This shift has steered implant dentistry from a predominantly function-driven, surgically oriented approach to emphasizing aesthetics and the integration of prosthetic and biological considerations (Priest, 2007). In nature, what is visually appealing often functions effectively, and applying this principle to implant dentistry can lead to treatment outcomes that harmonize aesthetics with functionality.
Several studies have highlighted the aesthetic shortcomings of implants without providing comprehensive details regarding the assessment of these issues (Ericsson et al., 2000). In a multicenter study spanning 5 years, a 10 % failure rate was documented; however, the specific parameters employed to identify the reasons behind aesthetic failures were not disclosed (Henry et al., 1996). Another study labeled poor aesthetic outcomes as complications rather than outright failures, citing issues such as improper restoration contours, inadequate shade matching, and gingival recession resulting in implant exposure as examples of such complications (Goodacre et al., 1999).
Complications in the pink tissue area of the aesthetic zone can arise owing to multiple errors occurring before, during, or after implant placement. Although various factors contribute to these problems, their occurrence can be significantly reduced by ensuring proper spacing between implants, meticulous timing during site preparation, and precise implant positioning (Wheeler, 2007). Additionally, considering that the gingival biotype is crucial for achieving optimal aesthetics, a thicker biotype should be preferred, especially for mitigating gingival recession—a prevalent aesthetic complication associated with dental implants (Kois, 2004). The delicate and minimally traumatic handling of soft tissues is paramount to achieving natural-looking outcomes (Buser et al., 2004). Poor handling of soft tissues frequently leads to aesthetic shortcomings in restorations, and addressing these concerns can pose significant challenges. An essential measure for minimizing scarring in the soft tissue environment surrounding the implant entails performing incisions solely within the attached gingiva (Sculean et al., 2014).
Improper implant selection can cause aesthetic issues. Initially, the size of the implant should closely match the diameter of the missing tooth at the bone crest. However, wide-necked implants have been found to reduce the amount of available bone on the facial side of the implant, leading to aesthetic problems. In the case of multiple implants, wide-necked implants can decrease interim implant bone space, causing bone resorption. In recent years, there has been a trend away from using oversized implants to improve aesthetic outcomes in the anterior region of the upper jaw (Buser et al., 2004). Optimal aesthetics seem to be achievable by maintaining a substantial amount of facial bone, facilitated by the use of implants with a diameter of less than 4 mm (Rodriguez and Rosenstiel, 2012). The presence of keratinized tissue is not obligatory for implant placement, but it is preferable in the aesthetic zone to ensure tissue stability and improve overall aesthetics. If soft tissue grafting is necessary, it can be performed either before implant placement or during stage II implant-uncovering surgery (Krekeler et al., 1985, Strub et al., 1991).
Treatment alternatives for gingival recession defects without surgery include achieving optimal plaque control, eliminating overhanging subgingival restorations, implementing behavioral modification interventions, and utilizing desensitizing agents. When surgery is necessary, the most reliable treatment options for both single and multiple recession defects are coronally advanced flap and tunnelling procedures, often combined with a connective tissue graft (Imber and Kasaj, 2021). Grafting the exposure using a guided bone regeneration technique and adjunct soft tissue augmentation could effectively restore unaesthetic recession exposure. Recovery of midfacial recession by soft tissue augmentation alone may be successful, as is presented hereafter (Gluckman and Du Toit, 2015).
Several recommendations have been proposed to enhance the aesthetic outcomes of implant positioning. First, the implant placement depends on the type of restoration. Second, the implant platform should be positioned approximately 3 mm below the expected facial gingival margin for the planned restoration. Third, aligning the implant center at least 3 mm toward the palate from the projected facial margins is advisable (Buser et al., 2004). Fourth, it is crucial to maintain an interim implant spacing of 3 mm between adjacent implant platforms to prevent resorption of the interproximal alveolar crest and decrease the papillary height. Lastly, for optimal results, it is recommended to ensure that the implants emerge through the palatal incisal edge of the subsequent crown positions (Priest, 2007).
5. Limitations
Notably, the included studies exhibited significant heterogeneity. Only a handful of studies have directly compared the outcomes of the implant techniques. Consequently, the impact of the choice of approach on the final results remains uncertain. Additional prospective and ideally randomized clinical trials are required to ascertain the factors influencing aesthetic outcomes after implant placement in the aesthetic zone.
6. Conclusion
Aesthetics-related issues during dental implant procedures in the aesthetic zone can include the following: marginal bone loss, which refers to the reduction of bone around the implant that can affect the appearance and stability of the implant-supported restoration; soft tissue complications, which include problems with the gum tissue around the implant that can lead to uneven contours or discoloration, affecting the overall aesthetic outcome; and concerns regarding the pink aesthetic score, which evaluates the soft tissue aesthetics around the implant, including the shape and color of the gums. A low score indicates an adverse effect on the natural appearance of the final restoration.
Careful treatment planning, soft tissue management, regular follow-up, patient education and expectation management, and collaboration among specialists can effectively manage and minimize aesthetic problems during dental implant procedures in the aesthetic zone, ensuring better outcomes and patient satisfaction.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Peer review under responsibility of King Saud University.
References
- Abadzhiev M., Nenko P., Velcheva P. Conventional immediate implant placement and immediate placement with sock-et-shield technique—Which is better. Int. J. Clin. Med. Res. 2014;1:176–180. [Google Scholar]
- Abd-Elrahman A., Shaheen M., Askar N., Atef M. Socket shield technique vs conventional immediate implant placement with immediate temporization. Randomized clinical trial. Clin. Implant Dent. Relat. Res. 2020;22:602–611. doi: 10.1111/cid.12938. [DOI] [PubMed] [Google Scholar]
- Alkhatib M.N., Holt R., Bedi R. Prevalence of self-assessed tooth discolouration in the United Kingdom. J. Dent. 2004;32:561–566. doi: 10.1016/j.jdent.2004.06.002. [DOI] [PubMed] [Google Scholar]
- Barakat D.A., Hassan R.S., Eldibany R.M. Evaluation of the socket shield technique for immediate implantation. Alex. Dent. J. 2017;42:155–161. [Google Scholar]
- Becker S.T., Beck-Broichsitter B.E., Rossmann C.M., Behrens E., Jochens A., Wiltfang J. Long-term survival of straumann dental implants with TPS surfaces: A retrospective study with a follow-up of 12 to 23 years. Clin. Implant Dent. Relat. Res. 2016;18:480–488. doi: 10.1111/cid.12334. [DOI] [PubMed] [Google Scholar]
- Brägger U., Karoussis I., Persson R., Pjetursson B., Salvi G., Lang N. Technical and biological complications/failures with single crowns and fixed partial dentures on implants: A 10-year prospective cohort study. Clin. Oral Implants Res. 2005;16:326–334. doi: 10.1111/j.1600-0501.2005.01105.x. [DOI] [PubMed] [Google Scholar]
- Bramanti E., Norcia A., Cicciù M., Matacena G., Cervino G., Troiano G., Zhurakivska K., Laino L. Postextraction dental implant in the aesthetic zone, socket shield technique versus conventional protocol. J. Craniofac. Surg. 2018;29:1037–1041. doi: 10.1097/SCS.0000000000004419. [DOI] [PubMed] [Google Scholar]
- Buser D., Martin W., Belser U.C. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int. J. Oral Maxillofac. Implants. 2004;19(Suppl):43–61. [PubMed] [Google Scholar]
- Chang M., Odman P.A., Wennström J.L., Andersson B. Esthetic outcome of implant-supported single-tooth replacements assessed by the patient and by prosthodontists. Int. J. Prosthodont. 1999;12:335–341. [PubMed] [Google Scholar]
- Cho S.-C., Froum S.J., Kamer A.R., Loomer P.M., Romanos G., Demiralp B. Implants in the anterior maxilla: Aesthetic challenges. Int. J. Dent. 2015;2015 doi: 10.1155/2015/152420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cosyn J., Eghbali A., De Bruyn H., Collys K., Cleymaet R., De Rouck T. Immediate single-tooth implants in the anterior maxilla: 3-year results of a case series on hard and soft tissue response and aesthetics. J. Clin. Periodontol. 2011;38:746–753. doi: 10.1111/j.1600-051X.2011.01748.x. [DOI] [PubMed] [Google Scholar]
- De Rouck T., Collys K., Wyn I., Cosyn J. Instant provisionalization of immediate single-tooth implants is essential to optimize esthetic treatment outcome. Clin. Oral Implants Res. 2009;20:566–570. doi: 10.1111/j.1600-0501.2008.01674.x. [DOI] [PubMed] [Google Scholar]
- Ericsson I., Nilson H., Lindh T., Nilner K., Randow K. Immediate functional loading of Brånemark single tooth implants. An 18 months’ clinical pilot follow-up study. Clin. Oral Implants Res. 2000;11:26–33. doi: 10.1034/j.1600-0501.2000.011001026.x. [DOI] [PubMed] [Google Scholar]
- Esposito M., Grusovin M.G., Polyzos I.P., Felice P., Worthington H.V. Interventions for replacing missing teeth: dental implants in fresh extraction sockets (immediate, immediate-delayed and delayed implants) Cochrane Database Syst. Rev. 2010 doi: 10.1002/14651858.CD005968.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esposito M., Pellegrino G., Pistilli R., Felice P. Rehabilitation of postrior atrophic edentulous jaws: Prostheses supported by 5 mm short implants or by longer implants in augmented bone? One-year results from a pilot randomised clinical trial. Eur. J. Oral Implantol. 2011;4:21–30. [PubMed] [Google Scholar]
- Esposito M., Zucchelli G., Cannizzaro G., Checchi L., Barausse C., Trullenque-Eriksson A., Felice P. Immediate, immediate-delayed (6 weeks) and delayed (4 months) post-extractive single implants: 1-year post-loading data from a randomised controlled trial. Eur. J. Oral Implantol. 2017;10:11–26. [PubMed] [Google Scholar]
- Farmer M., Darby I. Ridge dimensional changes following single-tooth extraction in the aesthetic zone. Clin. Oral Implants Res. 2014;25:272–277. doi: 10.1111/clr.12108. [DOI] [PubMed] [Google Scholar]
- Fürhauser R., Florescu D., Benesch T., Haas R., Mailath G., Watzek G. Evaluation of soft tissue around single-tooth implant crowns: the pink esthetic score. Clin. Oral Implants Res. 2005;16:639–644. doi: 10.1111/j.1600-0501.2005.01193.x. [DOI] [PubMed] [Google Scholar]
- Gluckman H., Du Toit J. The management of recession midfacial to immediately placed implants in the aesthetic zone. Int. Dent. Afr. Ed. 2015;5:6–15. [Google Scholar]
- Goodacre C.J., Kan J.Y., Rungcharassaeng K. Clinical complications of osseointegrated implants. J. Prosthet. Dent. 1999;81:537–552. doi: 10.1016/s0022-3913(99)70208-8. [DOI] [PubMed] [Google Scholar]
- Guljé F., Abrahamsson I., Chen S., Stanford C., Zadeh H., Palmer R. Implants of 6 mm vs. 11 mm lengths in the posterior maxilla and mandible: A 1-year multicenter randomized controlled trial. Clin. Oral Implants Res. 2013;24:1325–1331. doi: 10.1111/clr.12001. [DOI] [PubMed] [Google Scholar]
- Han C.-H., Park K.-B., Mangano F.G. The modified socket shield technique. J. Craniofac. Surg. 2018;29:2247–2254. doi: 10.1097/SCS.0000000000004494. [DOI] [PubMed] [Google Scholar]
- Henry P.J., Laney W.R., Jemt T., Harris D., Krogh P.H., Polizzi G., Zarb G.A., Herrmann I. Osseointegrated implants for single-tooth replacement: A prospective 5-year multicenter study. Int. J. Oral Maxillofac. Implants. 1996;11:450–455. [PubMed] [Google Scholar]
- Higginbottom F., Belser U., Jones J.D., Keith S.E. Prosthetic management of implants in the esthetic zone. Int. J. Oral Maxillofac. Implants. 2004;19(Suppl):62–72. [PubMed] [Google Scholar]
- Hinze M., Janousch R., Goldhahn S., Schlee M. Volumetric alterations around single-tooth implants using the socket-shield technique: preliminary results of a prospective case series. Int. J. Esthet. Dent. 2018;13:146–170. [PubMed] [Google Scholar]
- Imber J.-C., Kasaj A. Treatment of gingival recession: When and how? Int. Dent. J. 2021;71:178–187. doi: 10.1111/idj.12617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kan J.Y.K., Rungcharassaeng K., Sclar A., Lozada J.L. Effects of the facial osseous defect morphology on gingival dynamics after immediate tooth replacement and guided bone regeneration: 1-year results. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2007;65:13–19. doi: 10.1016/j.joms.2007.04.006. [DOI] [PubMed] [Google Scholar]
- Kois, J.C., 2004. Predictable single-tooth peri-implant esthetics: five diagnostic keys. Compend. Contin. Educ. Dent. Jamesburg NJ 1995 25, 895–896, 898, 900 passim; quiz 906–907. [PubMed]
- Krekeler G., Schilli W., Diemer J. Should the exit of the artificial abutment tooth be positioned in the region of the attached gingiva? Int. J. Oral Surg. 1985;14:504–508. doi: 10.1016/s0300-9785(85)80056-9. [DOI] [PubMed] [Google Scholar]
- Marković A., Mišić T., Janjić B., Šćepanović M., Trifković B., Ilić B., Todorović A.M., Marković J., Dard M.M. Immediate vs early loading of bone level tapered dental implants with hydrophilic surface in rehabilitation of fully edentulous maxilla: clinical and patient centered outcomes. J. Oral Implantol. 2022;48:358–369. doi: 10.1563/aaid-joi-D-21-00045. [DOI] [PubMed] [Google Scholar]
- Mitsias, M.M., Bratos, M., Siormpas, K., Pikos, M.A., Kotsakis, G.A., Root Membrane Group, 2020. Longitudinal Soft Tissue Changes During Periodontal Ligament-Mediated Immediate Implant Placement with the Root-Membrane Technique. Int. J. Oral Maxillofac. Implants 35, 379–385. doi: 10.11607/jomi.7245. [DOI] [PubMed]
- Nguyen V.G., Flanagan D., Syrbu J., Nguyen T.T. Socket shield technique used in conjunction with immediate implant placement in the anterior maxilla: A case series. Clin. Adv. Periodontics. 2020;10:64–68. doi: 10.1002/cap.10087. [DOI] [PubMed] [Google Scholar]
- Papaspyridakos P., Chen C.-J., Singh M., Weber H.-P., Gallucci G.O. Success criteria in implant dentistry: A systematic review. J. Dent. Res. 2012;91:242–248. doi: 10.1177/0022034511431252. [DOI] [PubMed] [Google Scholar]
- Paquette D.W., Brodala N., Williams R.C. Risk factors for endosseous dental implant failure. Dent. Clin. North Am. 2006;50(361–374):vi. doi: 10.1016/j.cden.2006.05.002. [DOI] [PubMed] [Google Scholar]
- Pohl V., Fürhauser L., Haas R., Pohl S. Gingival recession behavior with immediate implant placement in the anterior maxilla with buccal dehiscence without additional augmentation-a pilot study. Clin. Oral Investig. 2020;24:1455–1464. doi: 10.1007/s00784-019-03176-5. [DOI] [PubMed] [Google Scholar]
- Priest G.F. The esthetic challenge of adjacent implants. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2007;65:2–12. doi: 10.1016/j.joms.2007.03.015. [DOI] [PubMed] [Google Scholar]
- Qabbani, A.A., Razak, N.H.A., Kawas, S.A., Sheikh Abdul Hamid, S., Wahbi, S., Samsudin, A.R., 2017. The Efficacy of Immediate Implant Placement in Extraction Sockets for Alveolar Bone Preservation: A Clinical Evaluation Using Three-Dimensional Cone Beam Computerized Tomography and Resonance Frequency Analysis Value. J. Craniofac. Surg. 28, e318–e325. doi: 10.1097/SCS.0000000000003569. [DOI] [PubMed]
- Rodriguez A.M., Rosenstiel S.F. Esthetic considerations related to bone and soft tissue maintenance and development around dental implants: Report of the Committee on Research in Fixed Prosthodontics of the American Academy of Fixed Prosthodontics. J. Prosthet. Dent. 2012;108:259–267. doi: 10.1016/S0022-3913(12)60174-7. [DOI] [PubMed] [Google Scholar]
- Rokn A., Rasouli Ghahroudi A.A., Daneshmonfared M., Menasheof R., Shamshiri A.R. Tactile sense of the surgeon in determining bone density when placing dental implant. Implant. Dent. 2014;23:697–703. doi: 10.1097/ID.0000000000000173. [DOI] [PubMed] [Google Scholar]
- Rossi F., Ricci E., Marchetti C., Lang N.P., Botticelli D. Early loading of single crowns supported by 6-mm-long implants with a moderately rough surface: a prospective 2-year follow-up cohort study. Clin. Oral Implants Res. 2010;21:937–943. doi: 10.1111/j.1600-0501.2010.01942.x. [DOI] [PubMed] [Google Scholar]
- Sculean A., Gruber R., Bosshardt D.D. Soft tissue wound healing around teeth and dental implants. J. Clin. Periodontol. 2014;41(Suppl 15):S6–S. doi: 10.1111/jcpe.12206. [DOI] [PubMed] [Google Scholar]
- Strub J.R., Gaberthüel T.W., Grunder U. The role of attached gingiva in the health of peri-implant tissue in dogs. 1. Clinical findings. Int. J. Periodont. Restorative Dent. 1991;11:317–333. [PubMed] [Google Scholar]
- Tettamanti S., Millen C., Gavric J., Buser D., Belser U.C., Brägger U., Wittneben J.-G. Esthetic evaluation of implant crowns and peri-implant soft tissue in the anterior maxilla: Comparison and reproducibility of three different indices. Clin. Implant Dent. Relat. Res. 2016;18:517–526. doi: 10.1111/cid.12306. [DOI] [PubMed] [Google Scholar]
- Wheeler S.L. Implant complications in the esthetic zone. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2007;65:93–102. doi: 10.1016/j.joms.2007.03.009. [DOI] [PubMed] [Google Scholar]