Abstract
Introduction
Lower statin utilization is reported among women compared to men, however large-scale studies evaluating gender disparities in LDL-C management in individuals with ASCVD and its subtypes remain limited, particularly across age and racial/ethnic subgroups. In this study, we address this knowledge gap using data from a large US healthcare system.
Methods
All adult patients with established ASCVD in the Houston Methodist Learning Health System Registry during 2016–2022 were included. Statin use and dose were extracted from the database. The association between gender and statin utilization was evaluated using multivariate logistic regression analyses in patients with ASCVD overall, across ASCVD subtypes, and by age, racial/ethnic subgroups, and socioeconomic risk factors.
Results
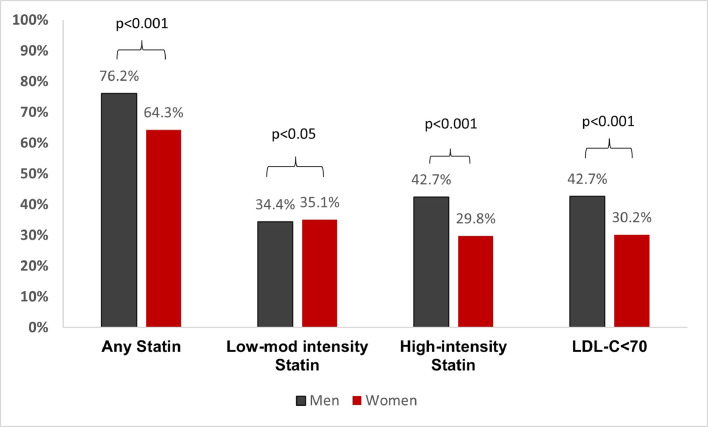
A total of 97,819 patients with prevalent ASCVD were included. Women with ASCVD had lower utilization of any statin (64.3% vs 72.6 %; p < 0.001) and high-intensity statin (29.8% vs 42.5 % p < 0.001) compared with men. In fully adjusted models, women had 40 % lower odds of any (adjusted odds ratio [aOR]:0.58, 95 % CI 0.57–0.60) and high-intensity statin use (aOR:0.59, 0.57–0.61) relative to men. Women were also less likely to have guideline-recommended LDL-C < 70 mg/dL (30.2% vs 42.7 %; p < 0.01). These differences persisted across age, racial/ethnic and socioeconomic subgroups.
Conclusion
Significant gender disparities exist in contemporary lipid management among patients with ASCVD, with women being less likely to receive any and high-intensity statin and achieving guideline defined LDL-C goal compared with men across age and racial/ethnic subgroups. These disparities underscore the need to further understand potential socioeconomic drivers of the observed lower statin uptake in women.
Keywords: Statin, Disparities, Prevention, Gender, Equity, ASCVD
Graphical abstract
Abbreviations and acronyms
- ASCVD
Atherosclerotic Cardiovascular Disease
- LDL-C
Low-density lipoprotein cholesterol
- ADI
Area Deprivation Index
- ICD-10 CM
International Classification of Diseases-10th Revisions-Clinical Modification
- CAD
Coronary Artery Disease
- PAD
Peripheral Artery Disease
- ATC
Anatomic Therapeutic Chemical
- HMH
Houston Methodist Hospital
- NHW
Non-Hispanic White
- NHB
Non-Hispanic Black
- DM
Diabetes Mellitus
1. Introduction
Atherosclerotic cardiovascular disease (ASCVD) is prevalent in approximately 10 % of the adult US population, and can present with clinical events, such as myocardial infarction, stroke, or cardiovascular death [1]. Statins are the cornerstone lipid-lowering modality for primary and secondary ASCVD prevention in men and women [2,3]. The 2018 American College of Cardiology/ American Heart Association (AHA) guideline recommends the use of high-intensity statin therapy for patients ≤ 75 years of age, with moderate-low intensity statin recommended for patients >75 years of age with established ASCVD [4]. These recommendations apply irrespective of gender, with no specific sex-specific recommendations on statin dosing, due to the similar efficacy and pharmacodynamic profile of statins across both sexes [5,6].
The clinical benefits of statins for cardiovascular risk reduction are established for both men and women, however it is well-documented that women with a clinical indication for statin therapy are less likely to be treated with any statin or receive high-intensity statin therapy when compared with their male counterparts [[7], [8], [9], [10], [11]]. In particular, gender variation in statin utilization on a population level among adults with ASCVD across different age, racial and ethnic, and socioeconomic subgroups remains less well-established. Therefore, we leveraged data from a large US healthcare system to determine contemporary patterns in utilization of statins in women compared with men across ASCVD and its subtypes.
2. Methods
2.1. Data source and study design
Houston Methodist Cardiovascular Disease Learning Health System (LHS) Registry was utilized to obtain data for all eligible patients. This LHS Registry is an electronic medical record (EMR) linked registry which includes medical, laboratory and pharmacy data of all adult patients aged ≥18 years that reported to the system-wide Houston Methodist Hospitals (HMH) in Houston, Texas, United States with at least one encounter in the outpatient setting from June 2016 till April 2022. The design, methodology and rationale of Houston Methodist LHS Registry has been described previously [12]. Baseline demographics, diagnoses, comorbidities, clinical parameters, medication use, radiology, laboratory, and outcome measures for all patients reporting across any outpatient setting at HMH were obtained directly from the EMR system using Extract Transform Load scripts and stored in the institution's internal server in a relational database model using Microsoft SQL Server Integration Services. Secondary data such as social vulnerability, Texas-state Area Deprivation Index (ADI) were also linked to the registry at the census tract level by geo-mapping using Federal Information Processing System (FIPS) and ZIP codes. The current study utilized an observational cross-sectional study design using data obtained from the Houston Methodist Cardiovascular Disease LHS registry. This study was approved by the Institutional Review Board at Methodist Online Research Technology Initiative (MORTI), Houston Methodist Hospital. Because of the sensitive nature of the data collected for this study, the corresponding author cannot make the data available upon request.
2.2. Study population
The study population included all adult (≥18 years) patients with an established ASCVD diagnosis. International Classification of Diseases-10th Revisions-Clinical Modification codes (ICD-10 CM) were used to identify patients with ASCVD by matching the ICD-10 CM codes in the ‘visit diagnosis’ and ‘problems list’ tables with respective ICD-10 CM codes in ICD code groupers (Supplementary Table 1–3). ASCVD was defined as patients with any diagnosis of coronary artery disease (CAD) peripheral artery disease (PAD) and/or stroke. If a patient had multiple subtypes of ASCVD, i.e. CAD or PAD, they were accounted across both subtypes when reporting results by ASCVD subtypes, but only once when reporting overall ASCVD. Each ICD-10 CM code was evaluated by cardiologists within the department of cardiology at HMH. Patients with unknown gender data were excluded from this analysis.
2.3. Primary independent variable
Gender was the primary independent variable of interest and was defined as a binary variable (women versus men) based on self-reported data.
2.4. Outcomes of interest
The primary outcome of interest was utilization of statins during the study period (June 2016 through April 2022). Attainment of guideline-defined low-density lipoprotein cholesterol (LDL-C) of <70 mg/dL amongst patients with ASCVD was the secondary outcome [13]. Statin use and dose were identified in the database using anatomic therapeutic chemical (ATC) classification codes. Patients without a medication ID for statin were classified as having no statin use. Types of statin included atorvastatin, simvastatin, lovastatin, pravastatin, Fluvastatin, cerivastatin, rosuvastatin and pitavastatin. For the purpose of this analysis, statin utilization was grouped according to any statin use, low-moderate intensity statin and high-intensity statin use. The intensity of each statin type was defined as per the 2013 ACC/AHA cholesterol guidelines (Supplementary Table 4). If the patient was started on low-moderate intensity statin and switched to high-intensity statin use, the statin intensity utilized at the most recent encounter was used as an outcome. All information pertaining current statin use and dosage was recorded based on medication reconciliation reviews with patients at each clinical encounter.
2.5. Covariates
Age was stratified as <45 years, 45–64 years and ≥65 years. Race/ethnicity was self-reported as non-Hispanic White (NHW), non-Hispanic Black (NHB), non-Hispanic Asian, Hispanic and/or Other. Insurance status was categorized as public, private, self-pay or uninsured. ADI was used to determine social disadvantage by categorizing ADI percentiles into five quintiles (Q): Q1 (1–20), Q2 (21–40), Q3 (41–60), Q4 (61–80) and Q5 (81–100), with Q1 representing least disadvantaged and Q5 representing most deprived individual [14]. Each patient was assigned into their corresponding ADI quintile based on their mailing address zip code. Laboratory values of lipid parameters of each patient's clinical encounter where statin use was recorded were also reported. In addition, cardiovascular risk factors such as diabetes mellitus (DM), obesity, smoking, hypertension, chronic kidney disease, heart failure and comorbidities, which were used to determine the Charlson comorbidity index were reported [15].
2.6. Statistical analysis
Categorical variables were presented as frequencies and percentages, while continuous variables were reported as means with standard deviation (SD) or medians with interquartile range (IQR) as appropriate. Gender differences in statin utilization were ascertained in the overall ASCVD population and across the spectrum of ASCVD. To ensure adequate comparison, we included proportion of patients with guideline recommended LDL-C < 70 mg/dL for all outcomes of interest. Where there were multiple values for LDL-C, the most recent value was used for the analysis. Gender differences in statin utilization for categorical variables were assessed using Pearson χ2 test. A p value of <0.05 was considered of statistical significance.
The relationship between gender and statin use was evaluated using multivariable logistic regression analysis. Adjusted models were used to control for potential confounders. Model 1 was adjusted for baseline demographics including age and race/ethnicity. Model 2 adjusted for variables in model 1 plus socioeconomic and cardiovascular risk factors such as cerebrovascular disease, diabetes mellitus (DM), obesity, smoking, hypertension, chronic kidney disease, heart failure, Charlson comorbidity index, insurance status and non-statin lipid-lowering medications (ezetimibe, bempedoic acid, PCSK9-inhibitors, fibrates, omega-3 fatty acids, vascepa, cholesterol absorption inhibitors). Adjusted odds ratio (OR) with 95 % confidence intervals (CI) were calculated to determine the odds of any statin use, low-moderate intensity statin use or high-intensity statin use among women compared with men. This relationship was evaluated across the spectrum of ASCVD and within age, racial/ethnic subgroups, across ADI quintiles and major cardiovascular risk factors, such as DM, hypertension, obesity and dyslipidemia to assess any observed differences across demographic subgroups and varying levels of social disadvantage. In addition, we also assessed yearly gender-specific trends in statin use and dose between calendar year 2016 to 2022 to determine yearly trends in utilization of statins across both genders. For the purpose of this analysis, if the patient had multiple prescriptions over the years, the utilization of statin recorded each year was used as an outcome for that year. Linear regression analysis generating separate models for men and women were used to determine significance of trends over time. All analyses were conducted using STATA (STATACorp Version 14). P value<0.05 was considered significant in all instances.
3. Results
3.1. Descriptive characteristics
Over the study period, 1,071,539 adults ≥18 years of age reported in the outpatient department of HMH. Amongst these, 97,819 had a diagnosis of ASCVD, of which 43,677 (44.7 %) were women (Fig. 1). Women contributed to a higher burden of stroke (53.9% vs 46.1 %), while men were more likely to be diagnosed with CAD (61.6% vs 38.4 %) and PAD (54.3% vs 45.7 %) (Supplementary Table 5). Baseline characteristics differed between men and women with ASCVD (Table 1). Compared with men, women with ASCVD were older, more likely to be NHB, have obesity, higher ADI quintiles, and were less likely to be privately insured. Women also had higher mean LDL-C (92.5 ± 38.9 vs 81.4 ± 35.6; p < 0.01) compared with men.
Fig. 1.
Flowchart detailing inclusion of study population based on eligibility criteria.
CAD=coronary artery disease; PAD=peripheral artery disease; ASCVD=Atherosclerotic cardiovascular disease.
Table 1.
Baseline characteristics of men and women with atherosclerotic cardiovascular disease.
| Characteristics | ASCVD |
||||
|---|---|---|---|---|---|
| Total Population, n(%) | 97,819 |
||||
| Sample by Gender, n (%) | Men |
Women |
p value | ||
| N | % | N | % | ||
| 54,142 | 55.3 % | 43,677 | 44.7 % | ||
| Age Group (years) | |||||
| <45 | 1741 | 3.2 % | 1822 | 4.2 % | <0.001 |
| 45–64 | 15,703 | 29.0 % | 10,931 | 25.0 % | |
| >=65 | 36,698 | 67.8 % | 30,924 | 70.8 % | |
| Race-Ethnicity | |||||
| Non Hispanic White | 35,907 | 66.3 % | 26,608 | 60.9 % | 0.1226 |
| Non Hispanic Black | 6279 | 11.6 % | 8455 | 19.4 % | |
| Non Hispanic Asian | 3409 | 6.3 % | 2142 | 4.9 % | |
| Non Hispanic Other | 1251 | 2.3 % | 738 | 1.7 % | |
| Hispanics | 6293 | 11.6 % | 5052 | 11.6 % | |
| Unknown Race/Ethnicity | 1003 | 1.9 % | 682 | 1.6 % | |
| Texas State ADI Quintiles | |||||
| Quintile 1 (least deprived) | 14,343 | 26.5 % | 9990 | 22.9 % | <0.001 |
| Quintile 2 | 15,033 | 27.8 % | 11,620 | 26.6 % | |
| Quintile 3 | 10,467 | 19.3 % | 8950 | 20.5 % | |
| Quintile 4 | 8043 | 14.9 % | 7138 | 16.3 % | |
| Quintile 5 (most deprived) | 5214 | 9.6 % | 5112 | 11.7 % | |
| ADI N/A | 1042 | 1.9 % | 867 | 2.0 % | |
| Insurance | |||||
| Public | 32,449 | 59.9 % | 29,068 | 66.6 % | <0.001 |
| Private | 14,173 | 26.2 % | 9816 | 22.5 % | |
| Uninsured or Other or NA | 5285 | 9.8 % | 3171 | 7.3 % | |
| Self-Pay | 2235 | 4.1 % | 1622 | 3.7 % | |
| BMI >30 kg/m2 | |||||
| Obesity | 22,080 | 17,843 | |||
| Obese Class 1+ | 12,698 | 57.5 % | 8753 | 49.1 % | <0.001 |
| Obese Class 2+ | 6991 | 31.7 % | 5826 | 32.7 % | |
| Obese Class 3+ | 2391 | 10.8 % | 3264 | 18.3 % | |
| Lipid Parameters (mean ± SD) | |||||
| LDL-C mg/dL (overall) | 81.4 ± 35.6 | 92.5 ± 38.9 | |||
| HDL-C mg/dL | 45.4 ± 14.2 | 56.8 ± 17.7 | |||
| Triglycerides mg/dL | 130.2 ± 94.0 | 125.3 ± 83.1 | |||
| Lipoprotein A in mnol/dL | 81.6 ± 90.0 | 102.9 ± 113.9 | |||
| LDL-Cholesterol | 38,773 | 31,549 | |||
| <70 | 16,549 | 42.7 % | 9519 | 30.2 % | <0.001 |
| 70–99 | 12,474 | 32.2 % | 10,419 | 33.0 % | |
| 100–129 | 5877 | 15.2 % | 6463 | 20.5 % | |
| 130–159 | 2551 | 6.6 % | 3273 | 10.4 % | |
| 160–189 | 951 | 2.5 % | 1281 | 4.1 % | |
| >=190 | 371 | 1.0 % | 594 | 1.9 % | |
| Risk Factors | |||||
| Current Smoking | 4782 | 8.8 % | 3165 | 7.2 % | <0.001 |
| Hypertension | 49,008 | 90.5 % | 38,064 | 87.1 % | <0.001 |
| Diabetes Mellitus | 18,405 | 34.0 % | 13,126 | 30.1 % | <0.001 |
| Obesity | 20,052 | 37.0 % | 16,392 | 37.5 % | 0.1121 |
| Dyslipidemia | 29,721 | 54.9 % | 23,780 | 54.4 % | 0.1604 |
| Charlson comorbidity index | |||||
| 0 | 3902 | 7.2 % | 2105 | 4.8 % | <0.001 |
| 1 to 3 | 26,491 | 48.9 % | 22,609 | 51.8 % | |
| >=4 | 23,749 | 43.9 % | 18,963 | 43.4 % | |
| Comorbidities | |||||
| Renal Disease | 17,350 | 32.0 % | 12,261 | 28.1 % | <0.001 |
| COPD | 14,351 | 26.5 % | 14,909 | 34.1 % | <0.001 |
| Cancer | 9886 | 18.3 % | 7040 | 16.1 % | <0.001 |
| Heart Failure | 16,530 | 30.5 % | 12,125 | 27.8 % | <0.001 |
| Atrial Fibrillation | 14,756 | 27.3 % | 9505 | 21.8 % | <0.001 |
| Medication Use | |||||
| PCSK9i | 1141 | 2.1 % | 835 | 1.9 % | 0.0306 |
| Ezetimibe | 5718 | 10.6 % | 4155 | 9.5 % | <0.001 |
| Bempedoic Acid | 98 | 0.2 % | 94 | 0.2 % | 0.2294 |
| Icosapent Ethyl | 1612 | 3.0 % | 781 | 1.8 % | <0.001 |
| Fibric Acid Derivatives | 2554 | 4.7 % | 1220 | 2.8 % | <0.001 |
| Bile Acid Sequestrants | 351 | 0.6 % | 444 | 1.0 % | <0.001 |
| Chol Absorption Inhibs. | 4376 | 8.1 % | 2932 | 6.7 % | <0.001 |
| Aspirin | 31,799 | 58.7 % | 21,038 | 48.2 % | <0.001 |
3.2. Differences in utilization of statins and dosing
Women with ASCVD were significantly less likely to utilize any statin (64.3% vs 76.2 %; p < 0.001), particularly high-intensity statin (29.8% vs 42.5 %; p < 0.001) compared with men (Fig. 2). In contrast, there were no major differences in low-moderate intensity statin between women and men (35.1% vs 34.4 %). Similar trends were observed in patients with CAD, PAD and stroke (Supplementary Table 6–8).
Fig. 2.
Utilization of statins in patients with atherosclerotic cardiovascular disease, stratified by gender.
Stratification of these results by age and racial groups revealed consistent results, with women significantly less likely to utilize any statin or high-intensity statin across all age (<45, 45–64, ≥65 years) and racial subgroups (NHW, NHB, Asians, Hispanics) (Table 2). These disparities were most prominent in the younger age group (<45 years) for all statin dosages (any statin 29.3% vs 48.2 %; low-moderate intensity statin 13.4% vs 15.9 %; high-intensity statin 16.1% vs 32.7 %; p < 0.001).
Table 2.
Utilization of statins amongst men and women with atherosclerotic cardiovascular disease across age and racial/ethnic subgroups.
| ASCVD | Any Statin Use |
Low-moderate Intensity Statin |
High Intensity Statin |
LDL-C < 70 mg/dL |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | P value | Men | Women | P value | Men | Women | P value | Total M/F | Men | Women | P value | |
| Total Population | 54,142 | 43,677 | 41,257 (76.2) | 28,100 (64.3) | <0.001 | 18,630 (34.4) | 15,347 (35.1) | 23,037 (42.5) | 12,998 (29.8) | <0.001 | 38,773/31,549 | 16,549 (42.7) | 9519 (30.2) | 0.001 | |
| Age, years | |||||||||||||||
| <45 | 1741 | 1822 | 839 (48.2) | 534 (29.3) | <0.001 | 276 (15.9) | 244 (13.4) | <0.001 | 570 (32.7) | 294 (16.1) | <0.001 | 1227/ | |||
| 1151 | 289 (23.6) | 260 (22.6) | 0.001 | ||||||||||||
| 45–64 | 15,703 | 10,931 | 11,647 (74.2) | 6494 (54.9) | 4401 (28.0) | 3164 (28.9) | 7438 (47.4) | 3423 (31.3) | 11,452/7868 | 4053 (35.4) | 1951 (24.8) | ||||
| ≥65 | 36,698 | 30,924 | 28,771 (78.4) | 21,072 (68.1) | 13,953 (38.0) | 11,939 (38.6) | 15,029 (41.0) | 9281 (30.0) | 26,094/22,530 | 12,207 (46.8) | 7308 (32.4) | ||||
| Race/Ethnicity | |||||||||||||||
| Non-Hispanic White | 35,907 | 26,608 | 27,496 (76.6) | 16,930 (63.6) | 0.009 | 12,500 (34.8) | 9473 (35.6) | 0.087 | 15,246 (42.5) | 7.583 (28.5) | 0.006 | 25,643/18,920 | 11,131 (43.4) | 5681 (30.0) | <0.001 |
| Non-Hispanic Black | 6279 | 8455 | 4521 (72.0) | 5524 (65.3) | 1945 (31.0) | 2753 (32.6) | 2620 (41.7) | 2813 (33.3) | 4761/ | 6613 | 1806 (37.9) | 1895 (28.7) | |||
| Non-Hispanic Asian | 3409 | 2142 | 2730 (80.1) | 1429 (66.7) | 1419 (41.6) | 919 (42.9) | 1364 (40.0) | 537 (25.1) | 2394/ | 1478 | 1048 (43.8) | 461 (31.2) | |||
| Hispanic | 6293 | 5052 | 4797 (76.2) | 3329 (65.9) | 1964 (31.2) | 1713 (33.9) | 2876 (45.7) | 1657 (32.8) | 4677/ | 3710 | 2063 (44.1) | 1235 (33.3) | |||
| Other | 1251 | 738 | 959 (76.7) | 460 (62.3) | 460 (36.8) | 262 (35.5) | 507 (40.5) | 208 (28.2) | 765/ | 477 | 295 (38.6) | 145 (30.4) | |||
| Unknown | 1003 | 682 | 754 (75.2) | 428 (62.8) | 342 (34.1) | 227 (33.3) | 424 (42.3) | 200 (29.3) | 533/351 | 206 (38.6) | 102 (29.1) | ||||
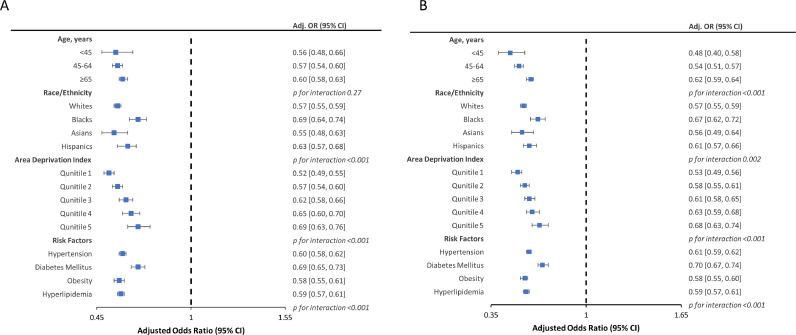
3.3. Statin utilization after multivariable adjustment
After adjustment for relevant baseline demographic, socioeconomic and clinical risk factors, women remained significantly less likely to utilize any statin (adjusted OR 0.58, 95 % CI [0.57, 0.60]) or high-intensity statin (adjusted OR 0.59, 95 % CI [0.57, 0.61]) compared with men (Table 3). Despite the small overall effect size, women had higher odds of utilizing low-moderate intensity statin (OR 1.05, 95 % CI [1.02, 1.08]). These results were consistent across the spectrum of ASCVD.
Table 3.
Odds of statin utilization in women vs men across the spectrum of atherosclerotic cardiovascular disease.
| Any Statin |
Low-moderate Intensity Statin |
High Intensity Statin |
|||||
|---|---|---|---|---|---|---|---|
| Men | Women (OR 95 % CI) | P value | Women (OR 95 % CI) | P value | Women (OR 95 % CI) | P value | |
| ASCVD | |||||||
| Model 1 | 1 (Ref) | 0.55 (0.54–0.57) | <0.001 | 1.03 (1.00–1.06) | 0.008 | 0.57 (0.55–0.58) | <0.001 |
| Model 2 | 1 (Ref) | 0.58 (0.57–0.60) | <0.001 | 1.05 (1.02–1.08) | <0.001 | 0.59 (0.57–0.61) | <0.001 |
| CAD | |||||||
| Model 1 | 1 (Ref) | 0.56 (0.54–0.58) | <0.001 | 1.06 (1.03–1.10) | <0.001 | 0.60 (0.58–0.62) | <0.001 |
| Model 2 | 1 (Ref) | 0.57 (0.55–0.59) | <0.001 | 1.07 (1.04–1.11) | <0.001 | 0.61 (0.58–0.62) | <0.001 |
| PAD | |||||||
| Model 1 | 1 (Ref) | 0.63 (0.59–0.67) | <0.001 | 1.0 (0.94–1.06) | <0.001 | 0.62 (0.58–0.66) | <0.001 |
| Model 2 | 1 (Ref) | 0.67 (0.63–0.71) | <0.001 | 1.02 (0.96–1.08) | <0.001 | 0.65 (0.61–0.69) | <0.001 |
| Stroke | |||||||
| Model 1 | 1 (Ref) | 0.60 (0.58–0.63) | <0.001 | 1.04 (0.99–1.08) | <0.001 | 0.59 (0.56–0.62) | <0.001 |
| Model 2 | 1 (Ref) | 0.64 (0.61–0.67) | <0.001 | 1.05 (1.01–1.10) | <0.001 | 0.61 (0.59–0.64) | <0.001 |
Model 1 is adjusted for demographics including age and race/ethnicity.
Model 2 is adjusted for model 1 + insurance status, chronic kidney disease, cerebrovascular disease, diabetes mellitus, obesity, smoking, hypertension, heart failure, charlson-comorbidity index, non-statin lipid lowering meds.
ASCVD = atherosclerotic cardiovascular disease; CAD = coronary artery disease; PAD= peripheral artery disease.
Upon evaluation within age and racial and ethnic subgroups, women remained less likely to be on any statin or high-intensity statin across all age and racial subgroups compared with men (Fig. 3). However, increased odds of utilization of low-moderate intensity statin among women (vs men) were observed in NHW (OR 1.03, 95 % CI [1.00, 1.07]), Hispanic (OR 1.12, 95 % CI [1.03, 1.22]) and women ≥45 years of age (45–64 years: OR 1.07, 95 % CI [1.01, 1.13]; ≥65 years: OR 1.05, 95 % CI [1.01, 1.08]) (Supplementary Fig. 1). In addition, women across all ADI quintiles were significantly less likely to utilize any statin and high-intensity statin compared with men, with women in Q1 having the least effect sizes. Further, consistent results were observed when evaluated across major cardiovascular risk factors, with women with diabetes mellitus, hypertension, obesity and/or dyslipidemia having significantly lower odds of using any statin, particularly high-intensity statin, but higher odds of utilizing low-moderate intensity statin compared with men.
Fig. 3.
Odds of statin utilization in women vs men with atherosclerotic cardiovascular disease, stratified by age, race/ethnicity, adi quintiles and cardiovascular risk factors:A) Multi-variate adjusted odds of any statin utilization in women compared with men, B) Multi-variate adjusted odds of high-intensity statin utilization in women compared with men.
Odds of statin utilization after adjusting for age, race/ethnicity, insurance status, ADI, chronic kidney disease, cerebrovascular disease, diabetes mellitus, obesity, smoking, hypertension, heart failure, charlson-comorbidity index, non-statin lipid lowering meds.
3.4. Gender-Specific yearly trends in statin use
Between 2016 and 2022, overall trend in the percentage use of any statin amongst ASCVD patients increased from 77 % to 78 % for men and 63 % to 68 % for women (p < 0.01) (Fig. 4). Similar trends were observed in patients taking high-intensity statins, which increased from 39 % to 49 % in men and 26 % to 38 % in women (p < 0.01). In contrast, a decline in utilization of low-moderate intensity statin was observed amongst both men (39 % to 30 %) and women (37 % to 32 %) over the study duration.
Fig. 4.
Yearly trends of statin use in women vs men with atherosclerotic cardiovascular disease.
3.5. Guideline recommended LDL-C < 70 mg/dL goal attainment
Laboratory data of LDL-C values were available for 38,773 (71.6 %) men and 31,549 (72.2 %) women with ASCVD. Women with ASCVD were significantly less likely to have guideline-defined goal of LDL-C < 70 mg/dL compared with men (30.2% vs 42.7 %; p < 0.001). Consistent results were observed across all age and racial and ethnic subgroups.
4. Discussion
This cross-sectional analysis of ∼98,000 patients with ASCVD in a large US healthcare system demonstrates significant gender disparities in contemporary LDL-C management using statins (Central Illustration). Women were significantly less likely to utilize any statin, particularly high-intensity statins compared with men. In contrast, women were more likely to receive low-moderate intensity statin. In addition, women with established ASCVD were also significantly less likely to have guideline defined goal of LDL<70 mg/dL compared with men. The lower use of overall statins and high-intensity statin amongst women was consistent across age and racial strata. These disparities persisted throughout the study period, and were observed even after adjusting for baseline, socioeconomic and clinical risk factors.
These results are consistent with prior studies, which have similarly reported gender disparities in utilization of statins, particularly guideline-recommended statin dose for secondary prevention of cardiovascular disease in women compared with men across different disease populations [7,9,[16], [17], [18]]. Results from the PALM (Provider Assessment of Lipid Management) registry showed that women with ASCVD were 18 % less likely to receive a guideline-recommended statin compared with men [7]. Similarly, women were also less likely to fill a high-intensity statin prescription following hospitalization for myocardial infarction [9]. These trends have also been observed amongst women veterans with type 2 DM, with 14 % lower odds of using any statin compared with men [10]. Further, it is known that women are less likely to receive high-intensity statin (vs men) following the identification of subclinical atherosclerosis (by coronary artery calcium scoring) [11].
Our findings, which accumulates one of the largest single center data across ASCVD subtypes substantiates results observed in prior reports. Women had 42 % lower odds of using statins despite having higher mean LDL-C levels and were less likely to attain guideline-defined goal of LDL-C < 70 mg/dL compared with their male counterparts. Given that our study period included results from after the 2013 ACC/AHA cholesterol guidelines, these findings are particularly concerning and predispose women with established cardiovascular disease to substantial risk of vascular events and mortality, which are preventable with guideline-recommended pharmacotherapy [19].
It is important to note that we observed consistent disparities across all pre-specified age groups and racial and ethnic subgroups. Despite restricting our analysis to adult ASCVD population, we noticed that the magnitude of the gender difference in the use of any statin and high-intensity statins was largest amongst young adults similar to a prior report of aggregated electronic medical record data [17]. This is concerning as young women have been shown to have the slowest rate of decline in cardiovascular disease rates in the United States [20]. These results remained unchanged even after adjusting for important demographic and patient-level confounders, thereby suggesting that young women remain consistently less intensively treated across a broad range of patient characteristics.
It has been previously reported that once a statin is initiated, women with established ASCVD are less likely than men to be up-titrated or receive high-intensity statin dosage [9]. In this study, we found that women were slightly more likely to receive low-moderate intensity statin, but less likely to achieve guideline recommended goal of LDL<70 mg/dL, relative to men. We observed encouraging temporal trends, where an increasing trend in high-intensity statin usage was observed amongst both men and women with a reduction in the gender gap.
Reasons for the observed disparities are multifactorial, and likely attributed to patient characteristics, such as age, socioeconomic status, higher prevalence of comorbidities, patient preference, higher rates of discontinuation, or due to physician inertia [7,[21], [22], [23]]. Importantly therapeutic inertia may be observed in women of reproductive age, given that lipid-lowering drugs including statins are contraindicated during pregnancy, and recommended to be discontinued while planning a pregnancy until after the breastfeeding period is over. This can lead to potential loss of statin years in women [24]. A prior analysis from the PALM registry has reported the lack of statin prescription from physicians to be the biggest contributor to gender disparities in statin use [7]. In addition, women with cardiovascular disease are also less likely to be treated as intensively as male patients [25]. However, the reasons for underutilization of statins are not limited to healthcare disparities. Analysis of USAGE (Understanding Statin Use in America and Gaps in Patient Education), an internet-based self-reported survey found that women were more likely to experience side effects, particularly myopathy following statin use which was frequently cited as the reason for stopping or switching their statins compared to male patients [22]. It is plausible that this may be a contributing factor to the increased utilization of low-moderate intensity statin observed in women in this analysis. Further, women have also been shown to have less belief in the safety and efficacy of statins when compared with men [7]. Other pertinent reasons also include preference of diet and regular exercise over the use of statin medication to prevent their risk of adverse cardiovascular events [23]. Future research could leverage natural language processing techniques to analyze unstructured clinical notes and capture reasons behind the lack of statin use. Identifying patterns in physician recommendations and patient adherence documented in clinical notes can help gain deeper insights into the gender disparities observed in statin use.
Addressing gender disparities in statin use requires a multifaceted approach. Community based approaches to increasing cardiovascular risk awareness, addressing cultural and societal biases, promoting shared decision-making, having focused campaigns on the importance of women's cardiovascular health, and increasing access to care, particularly for women with underserved and socially disadvantaged backgrounds may help reduce the stigma around statin use [7,26,27]. Many women may not be aware of their cardiovascular risk or benefits or statin therapy. Educational and focused campaigns targeted towards women can help encourage more women with ASCVD to take statin as an adjunct therapy with adequate exercise and healthy diet. In addition, it is important for health-care providers to involve women in the decision-making process when it comes to statin use. Further, increasing access to affordable and timely care for primary prevention of ASCVD may aid in decreasing burden of overall ASCVD.
There are certain limitations which should be considered while interpreting current results. First, although we present results from one the largest single-center analysis, given that this data was obtained from one US healthcare system makes it less likely to be generalized. Second, gender was captured as binary, hence we could not identify non-binary gender groups. Third, pregnant women were not excluded from this analysis as including such cases reflects a more nuanced and patient-centered approach to managing ASCVD risk. However, while statin use remains controversial during pregnancy, only six women in our dataset who met the study criteria were pregnant at the time statin use was recorded. Due to this small number, we did not conduct a separate sensitivity analysis for pregnant women. This small sample size may limit the generalizability of our findings regarding statin use in pregnant women with ASCVD. Fourth, the current analysis is limited by outpatient data, and does not include inpatient hospital data. Fifth, we used medication reconciliation reviews to ascertain utilization of statins, which involves asking the patients whether they are currently ‘on’ the medication. Although this is attributed to give insight into whether a patient was currently taking their medication or not, it is plausible that some patients may have been prescribed statins but do not take them. Six, due to lack of available data, we could not discern the reasons behind underutilization of statins in women. Finally, the year 2022 only includes data of the first four months (until April 2022), and therefore is not representative of the entire calendar year.
5. Conclusion
Our results demonstrate that significant gender disparities persist in contemporary LDL-C management using statins among US patients with ASCVD. Women are significantly less likely to utilize any statin, particularly high-intensity statin compared with men. Women with ASCVD are also less likely to have guideline defined goal of LDL-C < 70 mg/dL. These disparities persist across age and racial/ethnic strata.
CRediT authorship contribution statement
Izza Shahid: Writing – review & editing, Writing – original draft, Visualization, Validation, Methodology, Investigation, Conceptualization. Priyanka Satish: Writing – review & editing, Writing – original draft, Validation. Rakesh Gullapelli: Validation, Formal analysis, Data curation. Juan C Nicholas: . Zulqarnain Javed: Writing – review & editing, Visualization, Project administration. Eleonora Avenatti: Writing – review & editing, Writing – original draft, Validation. Budhaditya Bose: Formal analysis, Data curation. Shiwani Mahajan: Writing – review & editing, Writing – original draft. Trisha Roy: Writing – review & editing. Garima Sharma: Writing – review & editing, Supervision. Fatima Rodriguez: Writing – review & editing, Supervision. Julia Andrieni: Writing – review & editing. Stephen L Jones: Writing – review & editing. Sadeer Al-Kindi: Writing – review & editing, Supervision, Project administration. Miguel Cainzos-Achirica: Writing – review & editing, Validation, Project administration, Methodology, Data curation. Khurram Nasir: Writing – review & editing, Supervision, Resources, Project administration, Methodology, Data curation, Conceptualization.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
FR reports consulting fees from Novartis, NovoNordisk (CEC), Esperion, and HealthPals. KN is on the advisory board of Amgen, Novartis, Novo Nordisk, and his research is partly supported by the Jerold B. Katz Academy of Translational Research. All other authors report no disclosures relevant to the work of this manuscript.
Acknowledgments
Acknowledgement
None.
Sources of Funding
None.
Author agreement
We wish to draw the attention of the Editor to the following facts which may be considered as potential conflicts of interest and to significant financial contributions to this work.
[FR reports consulting fees from Novartis, NovoNordisk (CEC), Esperion, and HealthPals. KN is on the advisory board of Amgen, Novartis, Novo Nordisk, and his research is partly supported by the Jerold B. Katz Academy of Translational Research. All other authors report no disclosures relevant to the work of this manuscript].
We wish to confirm that has been no significant financial support for this work that could have influenced its outcome.
We confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. We further confirm that the order of authors listed in the manuscript has been approved by all of us.
We confirm that we have given due consideration to the protection of intellectual property associated with this work and that there are no impediments to publication, including the timing of publication, with respect to intellectual property. In so doing we confirm that we have followed the regulations of our institutions concerning intellectual property.
We further confirm that any aspect of the work covered in this manuscript that has involved either experimental animals or human patients has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript
We understand that the Corresponding Author is the sole contact for the Editorial process (including Editorial Manager and direct communications with the office). He/she is responsible for communicating with the other authors about progress, submissions of revisions and final approval of proofs. We confirm that we have provided a current, correct email address which is accessible by the Corresponding Author.
Signed by all authors as follows:
Izza Shahid MBBS, Priyanka Satish MD, Rakesh Gullapelli MS, Juan C Nicholas BS, Zulqarnain Javed PhD MBBS MPH, Eleonora Avenatti MD, Budhaditya Bose MS, Shiwani Mahajan MD, Trisha Roy MD, Garima Sharma MD, Fatima Rodriguez MD MPH, Julia Andrieni MD, Stephen L Jones MD, Sadeer Al-Kindi MD, Miguel Cainzos-Achirica MD, Khurram Nasir MD MPH MSc Date: 03/30/2024
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ajpc.2024.100722.
Appendix. Supplementary materials
References
- 1.Gu J., Sanchez R., Chauhan A., Fazio S., Wong N. Lipid treatment status and goal attainment among patients with atherosclerotic cardiovascular disease in the United States: a 2019 update. Am J Prev Cardiol. 2022;10 doi: 10.1016/j.ajpc.2022.100336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stone N.J., Robinson J.G., Lichtenstein A.H., Bairey Merz C.N., Blum C.B., Eckel R.H., et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American college of cardiology/American heart association task force on practice guidelines. J Am Coll Cardiol. 2014;63(25):2889–2934. doi: 10.1016/j.jacc.2013.11.002. Pt B. [DOI] [PubMed] [Google Scholar]
- 3.Taylor F., Ward K., Moore T.H., Burke M., Davey Smith G., Casas J.P., et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2011;(1) doi: 10.1002/14651858.CD004816.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grundy S.M., Stone N.J., Bailey A.L., Beam C., Birtcher K.K., Blumenthal R.S., et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: executive summary: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. J Am Coll Cardiol. 2019;73(24):3168–3209. doi: 10.1016/j.jacc.2018.11.002. [DOI] [PubMed] [Google Scholar]
- 5.Virani S.S. Statins in the primary and secondary prevention of cardiovascular disease in women: facts and myths. Tex Heart Inst J. 2013;40(3):288–289. [PMC free article] [PubMed] [Google Scholar]
- 6.Fulcher J., O'Connell R., Voysey M., Emberson J., Blackwell L., Mihaylova B., et al. Efficacy and safety of LDL-lowering therapy among men and women: meta-analysis of individual data from 174,000 participants in 27 randomised trials. Lancet. 2015;385(9976):1397–1405. doi: 10.1016/S0140-6736(14)61368-4. [DOI] [PubMed] [Google Scholar]
- 7.Nanna M.G., Wang T.Y., Xiang Q., Goldberg A.C., Robinson J.G., Roger V.L., et al. Sex differences in the use of statins in community practice. Circ Cardiovasc Qual Outcomes. 2019;12(8) doi: 10.1161/CIRCOUTCOMES.118.005562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Virani S.S., Woodard L.D., Ramsey D.J., Urech T.H., Akeroyd J.M., Shah T., et al. Gender disparities in evidence-based statin therapy in patients with cardiovascular disease. Am J Cardiol. 2015;115(1):21–26. doi: 10.1016/j.amjcard.2014.09.041. [DOI] [PubMed] [Google Scholar]
- 9.Peters S.A.E., Colantonio L.D., Zhao H., Bittner V., Dai Y., Farkouh M.E., et al. Sex differences in high-intensity statin use following myocardial infarction in the United States. J Am Coll Cardiol. 2018;71(16):1729–1737. doi: 10.1016/j.jacc.2018.02.032. [DOI] [PubMed] [Google Scholar]
- 10.Buchanan C.H., Brown E.A., Bishu K.G., Weeda E., Axon R.N., Taber D.J., et al. The magnitude and potential causes of sex disparities in statin therapy in veterans with type 2 diabetes: a 10-year nationwide longitudinal cohort study. Womens Health Issues. 2022;32(3):274–283. doi: 10.1016/j.whi.2021.10.003. [DOI] [PubMed] [Google Scholar]
- 11.Al-Kindi S., Tashtish N., Rashid I., Sullivan C., Neeland I.J., Robinson M., et al. Impact of low/no-charge coronary artery calcium scoring on statin eligibility and outcomes in women: the CLARIFY study. Am J Prev Cardiol. 2022;12 doi: 10.1016/j.ajpc.2022.100392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nasir K, Gullapelli R, Nicolas JC, Bose B, Nwana N, Butt SA, Shahid I, Cainzos-Achirica M, Patel K, Bhimaraj A, Javed Z, Andrieni J, Al-Kindi S, Jones SL, Zoghbi WA. Houston Methodist cardiovascular learning health system (CVD-LHS) registry: Methods for development and implementation of an automated electronic medical record-based registry using an informatics framework approach. Am J Prev Cardiol. 2024;18:100678. doi: 10.1016/j.ajpc.2024.100678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grundy S.M., Stone N.J., Bailey A.L., Beam C., Birtcher K.K., Blumenthal R.S., et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol. J Am Coll Cardiol. 2019;73(24):e285–e350. doi: 10.1016/j.jacc.2018.11.003. [DOI] [PubMed] [Google Scholar]
- 14.Johnson A.E., Zhu J., Garrard W., Thoma F.W., Mulukutla S., Kershaw K.N., et al. Area deprivation index and cardiac readmissions: evaluating risk-prediction in an electronic health record. J Am Heart Assoc. 2021;10(13) doi: 10.1161/JAHA.120.020466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Charlson M.E., Pompei P., Ales K.L., MacKenzie C.R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 16.Nelson A.J., Haynes K., Shambhu S., Eapen Z., Cziraky M.J., Nanna M.G., et al. High-intensity statin use among patients with atherosclerosis in the U.S. J Am Coll Cardiol. 2022;79(18):1802–1813. doi: 10.1016/j.jacc.2022.02.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Al-Kindi S.G., DeCicco A., Longenecker C.T., Dalton J., Simon D.I., Zidar D.A. Rate of statin prescription in younger patients with severe dyslipidemia. JAMA Cardiology. 2017;2(4):451–452. doi: 10.1001/jamacardio.2016.5162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sigvant B., Wiberg-Hedman K., Bergqvist D., Rolandsson O., Wahlberg E. Risk factor profiles and use of cardiovascular drug prevention in women and men with peripheral arterial disease. Eur J Cardiovasc Prev Rehabil. 2009;16(1):39–46. doi: 10.1097/HJR.0b013e32831c1383. [DOI] [PubMed] [Google Scholar]
- 19.Baigent C., Blackwell L., Emberson J., Holland L.E., Reith C., Bhala N., et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376(9753):1670–1681. doi: 10.1016/S0140-6736(10)61350-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Benjamin E.J., Blaha M.J., Chiuve S.E., Cushman M., Das S.R., Deo R., et al. Heart disease and stroke statistics-2017 update: a report from the american heart association. Circulation. 2017;135(10):e146–e603. doi: 10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gamboa C.M., Colantonio L.D., Brown T.M., Carson A.P., Safford M.M. Race-sex differences in statin use and low-density lipoprotein cholesterol control among people with diabetes mellitus in the reasons for geographic and racial differences in stroke study. J Am Heart Assoc. 2017;6(5) doi: 10.1161/JAHA.116.004264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Karalis D.G., Wild R.A., Maki K.C., Gaskins R., Jacobson T.A., Sponseller C.A., et al. Gender differences in side effects and attitudes regarding statin use in the understanding statin use in America and gaps in patient education (USAGE) study. J Clin Lipidol. 2016;10(4):833–841. doi: 10.1016/j.jacl.2016.02.016. [DOI] [PubMed] [Google Scholar]
- 23.Bradley C.K., Wang T.Y., Li S., Robinson J.G., Roger V.L., Goldberg A.C., et al. Patient-reported reasons for declining or discontinuing statin therapy: insights from the PALM registry. J Am Heart Assoc. 2019;8(7) doi: 10.1161/JAHA.118.011765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Klevmoen M., Bogsrud M.P., Retterstøl K., Svilaas T., Vesterbekkmo E.K., Hovland A., et al. Loss of statin treatment years during pregnancy and breastfeeding periods in women with familial hypercholesterolemia. Atherosclerosis. 2021;335:8–15. doi: 10.1016/j.atherosclerosis.2021.09.003. [DOI] [PubMed] [Google Scholar]
- 25.Keteepe-Arachi T., Sharma S. Cardiovascular disease in women: understanding symptoms and risk factors. Eur Cardiol. 2017;12(1):10–13. doi: 10.15420/ecr.2016:32:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Entwistle V.A., Cribb A., Watt I.S. Shared decision-making: enhancing the clinical relevance. J R Soc Med. 2012;105(10):416–421. doi: 10.1258/jrsm.2012.120039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mosca L., Linfante A.H., Benjamin E.J., Berra K., Hayes S.N., Walsh B.W., et al. National study of physician awareness and adherence to cardiovascular disease prevention guidelines. Circulation. 2005;111(4):499–510. doi: 10.1161/01.CIR.0000154568.43333.82. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.