Objectives
Despite considerable investments in health research, there is a disconnect between what is known to enhance healthcare and how healthcare is delivered in situ. Knowledge translation (KT) plays a vital role in addressing this disconnect. Some governments promote KT via initiatives that encourage collaboration between researchers, clinicians, communities and others; this includes Maridulu Budyari Gumal SPHERE (Sydney Partnership for Health, Education, Research and Enterprise). To promote KT and address the knowledge-to-action gap, we held an envisionarium with SPHERE members, to generate recommendations to promote KT in, and beyond, SPHERE. Methods: To discern these recommendations, an envisionarium was facilitated with SPHERE members. Participants included researchers, healthcare providers and others (n = 16). Participants considered how KT can be fostered and promoted. Discussion notes and participant responses were thematically analysed. Results: Four recommendations were identified, accompanied by practical steps to action these to enable health and research institutions to foster KT. These include the need to: provide access to resources; reconceptualise impact and innovation; promote the legitimacy of different knowledges; and engage everyone in KT. Conclusions: These recommendations are important for three reasons. First, they demonstrate that KT requires more than funding – it also requires networks that buoy the dynamic flow of knowledge in its varied manifestations. Second, the recommendations demonstrate the importance of supportive organisational mechanisms that inculcate positive, KT-friendly structures or cultures, while affording individuals the opportunity to organically foster innovation. Third, they demonstrate the methodological value of envisionariums to disrupt the status quo and envision different ways to promote KT.
Keywords: Knowledge translation, Health networks, Health organisations, Envisionarium
1. Introduction
A central challenge in health research and practice is the knowledge-to-action gap – the disconnect between what is empirically known to enhance healthcare, and how healthcare is practiced. Knowledge translation (KT) is a discipline that seeks to address this gap [1]. KT is a “dynamic and iterative process”, involving the “synthesis, dissemination, exchange and … application of knowledge” within complex and interconnected research, health and community systems to enhance healthcare [2]. KT is closely related to implementation science [3], but is not restricted to implementation activities. Rather, KT processes are multi-directional, involving an exchange of knowledge between stakeholders, rather than the linear delivery of end-of-project information to a passive audience [[4], [5], [6], [7]].
KT has been used to enhance and support healthcare in diverse contexts. For example, KT platforms helped to collate and make sense of copious data and (mis)information to inform international responses to COVID-19 [8]. Despite such successes, KT is not without its challenges, or shortcomings [9,10]. For example, a review determining the effect of patient engagement in health research on outcomes, found a “weak evidence base” [11]. Oft-cited barriers to, or challenges for, KT include issues of financial support, negative perceptions about the value of KT, the disparate priorities of KT stakeholders, and a lack of required competencies in KT practitioners [12,13]. Further, systematic and “structural factors” have been identified as significantly hindering KT efforts [14]. To address this, governments and organisations have worked to embed KT into research and clinical processes [[15], [16], [17], [18], [19], [20]], including via initiatives to foster collaboration between researchers, services, educators, consumers and carers to support a productive flow of knowledge for better healthcare. One such initiative is, Maridulu Budyari Gumal: Sydney Partnership for Health, Education, Research and Enterprise (SPHERE) [21].
SPHERE was established in 2017 to further and integrate research, education and healthcare to improve health in Greater Sydney (New South Wales, Australia). SPHERE represents a partnership between 15 organisations including two local health districts, two specialty health networks, three universities, and seven medical research institutes (encompassing 50,000 staff and 100,000 students). SPHERE partners work on health needs across the lifespan [21]. To support this work, the KT Platform was established. The Platform develops strategies to build KT capacity in SPHERE, generates and shares health knowledge and advances the science of KT [22].
In the first month of establishing the KT Platform, an envisionarium was held to identify KT needs and challenges in, and beyond, SPHERE. This article reports on this envisionarium and shares four recommendations (to foster KT) that were co-devised by envisionarium participants. To support health organisations seeking to grow their KT capacity, we also share practical steps to action these recommendations which were identified during the envisionarium.
2. Materials and methods
An envisionarium is an extended ideation workshop that utilises design thinking techniques [23]. It involves bringing a group of stakeholders together to address a question or problem with the specific goal of planning for the future. The envisionarium workshop format was developed by members of the SPHERE KT platform specifically to encourage creative, collaborative, and practical planning to support growth and capacity building for diverse stakeholders. The term envisionarium was chosen to evoke visionary thinking; specifically imaginative and innovative future planning that is guided by both experiential and research knowledge. The KT envisionarium aimed to clarify what is exciting or challenging about KT and how can KT capacity be developed?
The full day envisionarium was held in Sydney, in September 2018. Facilitated by an external consultant with expertise in design thinking [23], participants convened in small groups (≈4) to participate in activities and discussions. Participants were invited to map current relationships within SPHERE; visualise and empathise with the next users of knowledge developed by SPHERE; use the ‘five whys’ technique [24]; generate ideas to promote KT; and devise a KT action plan.
Thirty-seven SPHERE members were invited to the envisionarium due to their experience with or interest in KT. Of the invitees, 16 participated. When asked about their familiarity with KT, most participants reported that they had completed KT training, research and/or projects. Therefore, participants brought considerable knowledge relevant to KT. Approximately 70 % of participants were academic or clinical researchers, while approximately 30 % were health service managers affiliated with local health districts. An artist also participated due to their experience collaborating with researchers to disseminate research data using arts-based methods. Given greater researcher participation, it is unsurprising that research and clinical activity were often discussed during the envisionarium. However, the facilitator sought to address potential marginalisation of service managers by regularly soliciting their views. As discussed later, no consumers or carers participated in the envisionarium, representing a major shortcoming of the event.
Authors KB, AD and ZT took hand-written notes during the envisionarium to document discussion resulting from workshop activities. Materials produced by participants (sticky-notes and butchers' paper with notes and diagrams made in the course of the envisionarium) were retained for analysis. These materials were transcribed into Microsoft Word by the authorship team. Informed by Braun and Clarke's analytical phases [25,26] the authors undertook the following process to produce a set of recommendations to guide future KT activities in SPHERE. 1) familiarisation: all authors reviewed all documents to gain a sense of the materials as a whole; 2) initial coding: all materials were double coded (by two authors) using a deductive approach to determine what is exciting about KT? what challenges are associated with KT? How can KT be promoted? Authors used the comments function in Word to track this process. 3) identification of themes: all authors reviewed initial codes and differences or disagreements between two coding schemes were resolved through discussion. Following the deductive approach outlined above, all authors worked together to identify key issues and elements to produce a set of themes. All initial themes were established via consensus. 4) Refining themes: all authors reviewed the themes and through discussion and critical reflection refined the themes to produce four meta-themes (presented here as recommendations with attendant actions).
To ensure rigour and trustworthiness, envisionarium materials were analysed collaboratively with disagreements resolved through discussion and consensus. Given the authorship team are all researchers, we sought to reflexively acknowledged our professional interests and preoccupations to ensure that we did not focus unduly on themes and content related to research, at the cost of those related to other aspects of KT. The workshop and its outcomes were not subject to ethics approval as envisionarium participants were co-researchers (and some are co-authors), rather than research participants.
3. Results
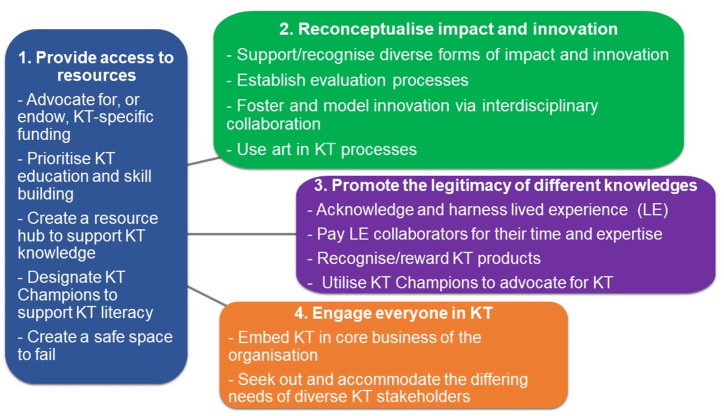
Four recommendations to build KT capacity in health and research institutes emerged through analysis. These recommendations are now shared, alongside practical steps to action these (see Fig. 1). Although the envisionarium focused specifically on KT efforts in SPHERE, the recommendations and actions reported are of a purposefully high-level order to optimise usefulness and relevance to other health and research organisations seeking to foster and grow their KT capacity.
Fig. 1.
Summary of recommendations and actions.
3.1. Provide access to resources
A foundational requirement for successful KT activities is adequate resourcing. KT infrastructure is required to enable individuals, teams, organisations, and societies to connect, exchange, and develop new knowledge and practices. Participants considered various ways to support KT and build organisational capacity. They highlighted the importance of both top-down processes (related to funding priorities and organisational incentives) as well as ground-up approaches (e.g., supporting practitioners and consumers to innovate using existing resources). Participants concluded that KT can be a resource-intensive process but indicated that if time and money are not dedicated to KT, it cannot effectively occur. Resources are also needed for evaluations to clarify what does and does not work in KT processes.
3.1.1. Actioning this recommendation
There should be sustained advocacy to mandate KT in funding and grant applications in the health sector. This will positively reposition the role and status of KT. As one participant stated, KT should not be “an extra or afterthought, but a core part of how and why projects receive funding”. Participants identified additional avenues to bolster KT, including targeted fellowships for students and researchers to learn KT, dedicated time for service managers and practitioners to engage in KT, including KT responsibilities in job descriptions and mandating paid consumer and carer involvement in research and service development.
Resources for ongoing learning and training about KT are key to building organisational capacity. Organisations might consider establishing a digital or physical knowledge hub – a resource for KT support, advice, literature and best-practice guides. For example, after the envisionarium the KT Platform created a website offering practical resources to promote KT [22].
KT champions – people committed to, and knowledgeable about KT, who serve as ambassadors and role models – can support KT capacity building. KT champions can provide support, guidance and mentorship about KT to students, researchers, clinicians and others. However, appropriate support structures are required to enable KT champions to work effectively. For example, writing KT support activities into an individual's job description, rather than expecting these to be undertaken in addition to existing responsibilities.
Participants noted that, because experimentation and innovation in KT requires time and tolerance of risk, KT practitioners need a safe space in which to fail. Participants noted that learning about what does not work can be as instructive as identifying what does. Therefore, making time and space to share information on both triumphs and failings is an important part of KT resourcing.
Fostering a culture of KT throughout an organisation can inspire people to work creatively and challenge institutional logics that sustain established practices and policies, rather than accommodating new approaches [27]. For example, participants noted that, in some universities and research institutes, people resist KT activities that fall outside the scope of traditional academic key performance indicators (refereed publications, securing research funds) [28]. Thinking critically about how an organisation operates (and the activities it incentivises and values) is the first step to growing and supporting KT practices. As addressed in section 3.2, participants highlighted that a core component of localised KT is reconceptualising impact and innovation to encompass a broader range of actions and outcomes.
3.2. Reconceptualise impact and innovation
KT can enable researchers to bridge the gap between knowledge and practice to benefit individuals and communities. Communicating knowledge to facilitate clinical change is an established aim of KT [5,[29], [30], [31]] and participants highlighted its importance. For example, one participant noted that KT should support “real-world impact” that is felt “on the ground”. While practice change can denote KT impact, participants noted that exchange should also be considered when conceptualising effectiveness. Therefore, measures of KT impact should also include the facilitation of knowledge exchange between stakeholders (researchers, clinicians, consumers etc) to inform the research agenda and enhance practice and policy. Participants observed that exchange requires interpersonal and interinstitutional connections. Indeed, establishing new connections by expanding local networks and engaging with people from different backgrounds (during research and with research outputs) should be conceptualised as a form of impact. However, such impact can be hard to demonstrate and is typically not built into ‘outcome’ expectations in current funding models.
Embracing new ways of thinking can drive innovation in KT. While top-down innovation and culture shifts are key, equally important is situated innovation [32], where change occurs because of, and in response to, specific environments and people. Crucially, situated innovation supports and relies on exchange (described earlier), and responds to the input of next users to drive change as well as clarify problems and solutions.
3.2.1. Actioning this recommendation
Organisations should ensure support for and recognition of impact and innovation approaches that have traditionally been undervalued or ignored. This includes instituting key performance indicators or reporting mechanisms to assess network building and user-engagement; budgeting time and resources for innovation and impact activities; as well as rolling out capacity building activities to support and mandate innovation and impact. Further, establishing responsive evaluations can help to ensure that KT objectives are agile, accommodate next user and stakeholder contributions, and are instantiated as measurable key performance indicators.
Changing the design and operation of research and KT processes can foster innovation. Participants suggested embedding collaboration between disciplines and with different stakeholders into research and KT. Indeed, participants noted that breaking down institutional silos and “looking over the disciplinary fence” bolstered innovation. Such collaborations can be fostered via: meet-and-greet sessions between different departments, research units, or health specialities; short lunch-and-learn research or knowledge showcases; research speed dating events; or KT-and-nibbles social gatherings.
Another approach to innovation is collaborating with artists. Using arts-based KT methods and working with artists can result in impactful and appealing activities or products that engage diverse stakeholders [33]. For example, inspired by the envisionarium the KT Platform engaged a group of artists to collaborate with researchers and clinicians across SPHERE to create an installation called “The HIVE”. The installation shared key findings from seven research projects [34]. Participants noted that engaging artists with lived experience and/or who belong to relevant cultural or community groups, helps to produce appropriate and safe KT. Not-for-profit arts organisations can be a good place to start when seeking artists to collaborate with. For example, in Australia, there is a network of regional arts organisations that provide information and advice about, and to, local artists [35]. Similarly, the Artist-Run Alliance provides a free database of artist-run initiatives globally [36].
3.3. Promote the legitimacy of different knowledges
Expanding conceptions of knowledge and what it means to translate knowledge, is key to effective KT. Central to this recommendation is challenging the notion that knowledge is static and something only researchers can discover. It is imperative that KT practitioners accommodate and acknowledge different forms of knowledge, including empirical research knowledge, lived experience and cultural epistemologies [37]. All of these must be nurtured if local innovations are to emerge and be sustained. KT activities can broaden definitions of knowledge and legitimise the importance of experiential knowledge of health(care). Although such knowledge is largely undervalued in the health sciences [[38], [39], [40], [41]], this is changing. For example, in Canada, Australia and elsewhere, patient and public involvement in health research is increasingly mainstream [[42], [43], [44], [45]]. Many participants were enthusiastic about formalising institutional recognition of different modes of knowledge. There was a particularly strong desire to amplify consumer voices in research, clinical and care contexts. As one participant stated, “[we should] start with the end user – the community has to tell you the problem”. Just as lived and cultural knowledge needs to be legitimated, so too does KT knowledge. Participants noted that KT science is a form of knowledge that is poorly understood and subsequently not widely valued. Therefore, there is a need to build the legitimacy of KT.
3.3.1. Actioning this recommendation
Participants identified several ways to acknowledge and harness lived and cultural knowledge in KT and other health processes, including engaging the next users of research before, during and after project completion as advisors or researchers. There is a growing body of literature that provides useful guidance on undertaking this [34,[46], [47], [48]].
Participants also felt that reconceptualising the way research topics are conceived and prioritised is another way to accommodate diverse knowledge types. For example, rather than a researcher suggesting a topic of research, they might invite stakeholders to identify the problems that warrant examination. Further, incorporating consumer representation and participation in organisational processes can serve to foreground experiential knowledge. For example, lived experience representatives should hold positions on funding, ethics and research governance committees and lived experience advisory groups should auspice research projects.
Organisations or researchers must ensure community members and lived experience advisors are recompensed for their contributions. This acknowledges the value of their knowledge and expertise, placing it on an equal footing with that of researchers who are also paid for their time [46]. As successfully done by SPHERE members, organisations should create policies to guide lived experience participation (e.g., [49]). In various countries, national research policies specify pay rates for lived experience participation and these can be adopted by organisations (e.g., [50]).
Institutions seeking to legitimise KT as a valid science and practice need to acknowledge KT activities via awards, funding and key performance indicators. Academics might wish to practice KT but feel pressured to prioritise traditional research outputs [28]. Including KT activities, outputs and outcomes as key performance indicators and allocating time and funds to these can address this hesitancy. Similarly, building in evaluative processes to measure various impacts and outcomes of KT can help researchers to validate KT processes and build an evidence-base. This will also enhance the value and legitimacy of KT. Finally, KT champions (recommendation 1) can build recognition for the value of KT.
3.4. Engage everyone in knowledge translation
Impactful KT requires support from all stakeholders. Simultaneously, to have the most impact, KT strategies need to accommodate the diverse needs and experiences of individuals who have a vested interest in healthcare. Without this, KT processes have limited impact. As one participant remarked, “KT should be everybody's business”.
3.4.1. Actioning this recommendation
KT should be embedded in the core business of an organisation through systemic advocacy and awareness-raising. Inviting departmental or research leaders to facilitate or participate in KT workshops can foster interest in and knowledge about KT. Engaging with chief executives of local health districts and other health service decision-makers can also improve KT recognition and ensure institutional support. This can be done in various ways, including partnering with health districts to distribute KT products. Another approach is to orchestrate deliberative dialogues in which clinical, research and lived experience knowledge is shared directly with relevant policymakers and service decision-makers [51].
Knowledge generation and dissemination requires the involvement of diverse individuals, representing different groups. Stakeholders might include consumers, their families, clinicians, researchers, administrators, peer workers and policymakers. It is important to understand their different and sometimes conflicting expectations or needs. Participants discussed instances when KT strategies were poorly aligned to stakeholder needs, resulting in considerable setbacks. Inviting stakeholders to participate in KT planning and operation, including asking consumers and carers to establish the KT agenda at its inception, can ensure KT is fit-for-purpose. Alongside this, KT practitioners can proactively consider the ‘pain and gain’ points for different stakeholders via brainstorming, research and consultation. During the envisionarium, participants imagined stakeholder personas in order to consider diverse KT needs and interests. For example, participants developed the persona of ‘Beryl’ (the clinician) who worked at a hospital and had limited time to read academic journals and few incentives to change her practice. Nevertheless, she wanted patients to do well. She needed clear, brief and accessible information to inform any practice change.
4. Discussion
The recommendations presented here were formed in response to key challenges to effective KT. Reflecting extant literature, challenges pertained to resourcing, perceived legitimacy and stakeholders’ conflicting expectations and behaviours [[12], [13], [14]]. Practical steps to action these recommendations – from sharing skills through workshops and mentoring, to systemic advocacy at an organisational level – also reflect the KT evidence-base [13].
4.1. Implications for practice
As discussed above, SPHERE was formed to foster connections between the diverse stakeholders (clinicians, researchers, service providers, educators, health users, and carers etc.) who people the healthcare landscape. In seeking to foster this connectivity, SPHERE aims to address the knowledge-to-action gap and support a multi-direction flow of knowledge (between all stakeholders) to achieve better health(care) outcomes. Taken together, the recommendations emerging from the envisionarium illustrate that KT is an important element for connectivity. That is, KT models, methods and practices [52] offer a means for heath organisations to conceptualise, establish, maintain, and grow productive networks that unite large numbers of people with differing needs and ways-of-working.
The envirionarium also highlights the importance of embedding KT practitioners within health organisations. The envisionarium was productive partly because all participants had KT experience and/or were committed to building broader recognition and understanding of its value. In this sense, the envisionarium participants epitomised KT champions. The success of the envisionarium is perhaps a testament to the efficacy of KT champions in supporting system and practice change for better KT. The conceptual and practical strategies the participants suggested informed and enhanced the ongoing development of the SPHERE KT Platform. For example, in response to the envisionarium, the Platform recruited 11 KT Ambassadors from different research groups in SPHERE who act as champions by promoting and supporting KT activities across SPHERE.
4.2. Limitations
This article makes no claims to mapping the entire terrain of KT nor to representing the views of everyone invested in KT. A key limitation of the envisionarium was the absence of consumers or carers. In hindsight, this might have reflected the then unexamined assumption that KT expertise and activity was the purview of researchers, rather than consumers. Ironically, this assumption affirms the importance of the envisionarium recommendation that consumers and carers must be involved at all stages of health research and practice, and in KT, specifically. Facilitating consumer and carer involvement in knowledge production and dissemination is part of the ongoing remit of the SPHERE KT Platform. This is indicated in its strategic plan, which was created in response to the envisionarium. Furthermore, to acknowledge the importance of consumer engagement, co-production and participation in research and KT activities, as of 2021, the KT Platform merged with the Consumer and Community Involvement Platform, thereby recognising the importance of lived experience in KT.
5. Conclusions
This article highlights the potential of KT to support productive, innovative, and useful connections between diverse healthcare stakeholders. It also demonstrates the potential of exploratory workshops, such as envisionariums, to encourage creative and ambitious future-focused thinking and planning. In this instance, the envisionarium format provided an opportunity for people with different personal and professional experiences to meet, share, and work together to support organisation-oriented action and growth. Putting different views and experiences into conversation supported innovative thinking by disrupting disciplinary norms and status-quo ways-of-working. The authors hope that the recommendations, and reflections about the envirionarium process, presented here will support the efforts of healthcare and other organisations in the development of their own KT capabilities.
Ethical statement
Review and/or approval by an ethics committee was not needed for this study because it was not conceptualised as a research activity. This text shares recommendations produced during a collaborative workshop (the envisionarium) undertaken between collaborating stakeholders (rather than reporting on data generated through engagement of research participants). All attendees verbally consented to ideas and information generated during the envisionarium being shared via publication. All attendees (some of whom are authors on this paper) subsequently consented to the publication of this text.
Data availability statement
The paper reports on a collaborative, ideas-generation process rather than a research process. Data were not collected. Therefore, no additional data is available.
Funding
This research did not receive any specific funding.
CRediT authorship contribution statement
Ann Dadich: Writing – review & editing, Writing – original draft, Methodology, Investigation, Formal analysis, Conceptualization. Priya Vaughan: Writing – review & editing, Writing – original draft, Formal analysis. Chloe Watfern: Writing – review & editing, Writing – original draft, Formal analysis. Zoi Triandafilidis: Writing – review & editing, Writing – original draft, Methodology, Investigation, Formal analysis, Conceptualization. Stephanie Habak: Writing – review & editing, Formal analysis. Katherine M. Boydell: Writing – review & editing, Methodology, Investigation, Formal analysis, Conceptualization.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Author Ann Dadich is a section editor for Heliyon Public Health, but was not involved in processing or reviewing this article for Heliyon.
Acknowledgements
We gratefully acknowledge the contribution of envisionarium participants who have not acted as authors on this paper: Jacqueline Center, Dominiek Coates, Valsamma Eapen, Karyn Joyner, Julia Lappin, Elizabeth McInnes, Sandy Middleton, Siobhan Schabrun, Jane Ussher, Christopher White, Adrienne Withall and others who prefer not to be named.
References
- 1.Martin K., Mullan Z., Horton R. Overcoming the research to policy gap. Lancet Global Health. 2019;7(Supp. 1):S1–s2. doi: 10.1016/S2214-109X(19)30082-8. [DOI] [PubMed] [Google Scholar]
- 2.CIHR Knowledge translation Canada: CIHR (Canadian institutes of health research) 2020. https://cihr-irsc.gc.ca/e/29529.html [Available from:
- 3.Nilsen P. Making sense of implementation theories, models and frameworks. Implement. Sci. 2015;10(1):53. doi: 10.1186/s13012-015-0242-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Braithwaite J., Churruca K., Long J., Ellis L., Herkes J. When complexity science meets implementation science: a theoretical and empirical analysis of systems change. BMC Med. 2018;16(63):1–14. doi: 10.1186/s12916-018-1057-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haworth-Brockman M. Winnipeg, Manitoba: National Collaborating Centre for Infectious Diseases (NCCID) University of Manitoba; 2016. Translating knowledge to practice: the case for knowledge brokering [Website]https://nccid.ca/translating-knowledge-practice-case-knowledge-brokering/ [updated Mar. Available from: [Google Scholar]
- 6.Green L.W. Making research relevant: if it is an evidence-based practice, where's the practice-based evidence? Fam. Pract. 2008;25:i20–i24. doi: 10.1093/fampra/cmn055. [DOI] [PubMed] [Google Scholar]
- 7.Lee R., Garvin T. Moving from information transfer to information exchange in health and health care. Soc. Sci. Med. 2003;53(3):449–464. doi: 10.1016/s0277-9536(02)00045-x. [DOI] [PubMed] [Google Scholar]
- 8.El-Jardali F., Bou-Karroum L., Fadlallah R. Commentary: amplifying the role of knowledge translation platforms in the COVID-19 pandemic response. Health Res. Pol. Syst. 2020;18(58):1–7. doi: 10.1186/s12961-020-00576-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oliver K., Kothari A., Mays N. The dark side of coproduction: do the costs outweigh the benefits for health research? Health Res. Pol. Syst. 2019;17(33):1–10. doi: 10.1186/s12961-019-0432-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dadich A., Vaughan P., Boydell K. The unintended negative consequences of knowledge translation in healthcare: a systematic scoping review. Health Sociol. Rev. 2023:1–19. doi: 10.1080/14461242.2022.2151372. [DOI] [PubMed] [Google Scholar]
- 11.Manafo E., Petermann L., Mason-Lai P., Vandall-Walker V. Patient engagement in Canada: a scoping review of the 'how' and 'what' of patient engagement in health research. Health Res. Pol. Syst. 2019;16(5):1–11. doi: 10.1186/s12961-018-0282-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gagliardi A., Berta W., Kothari A., Boyko J., Urquhart R. Integrated knowledge translation (IKT) in health care: a scoping review. Implement. Sci. 2015;11(1):38. doi: 10.1186/s13012-016-0399-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mallidou A.A., Atherton P., Chan L., Frisch N., Glegg S., Scarrow G. Core knowledge translation competencies: a scoping review. BMC Health Serv. Res. 2018;18(1):502. doi: 10.1186/s12913-018-3314-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Williams O., Sarre S., Papoulias S.C., Knowles S., Robert G., Beresford P., et al. Lost in the shadows: reflections on the dark side of co-production. Health Res. Pol. Syst. 2020;18(43):1–10. doi: 10.1186/s12961-020-00558-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Health and Medical Research Council . Australian Government; Canberra, Australia: 2022. Research Translation.https://www.nhmrc.gov.au/research-policy/research-translation-and-impact [Available from: [Google Scholar]
- 16.Lowitja Institute . Lowitja Institute; Melbourne: 2020. Position Paper: Knowledge Translation to Research Impact for Empowerment. [Google Scholar]
- 17.Williams M., editor. Profiling Excellence: Indigenous Knowledge Translation. Lowitja Institute; Melbourne: 2021. [Google Scholar]
- 18.National Health and Medical Research Council . Australia Australian Government; 2022. Annual NHMRC Research Translation Symposium Canberra.https://www.nhmrc.gov.au/symposium [Available from: [Google Scholar]
- 19.Lavis J.N. Research, public policymaking, and knowledge-translation processes: Canadian efforts to build bridges. J. Continuing Educ. Health Prof. 2006;26(1):37–45. doi: 10.1002/chp.49. [DOI] [PubMed] [Google Scholar]
- 20.Evans S., Scarbrough H. Supporting knowledge translation through collaborative translational research initiatives: 'bridging' versus 'blurring' boundary-spanning approaches in the UK CLAHRC initiative. Soc. Sci. Med. 2014;106:119–127. doi: 10.1016/j.socscimed.2014.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maridulu Budyari Gumal the Sydney Partnership for Health E Research and Enterprise (SPHERE). About us. 2024. https://www.thesphere.com.au/about-us/ [Available from:
- 22.SPHERE Knowledge Translation Strategic Platform . SPHERE Knowledge Translation Strategic Platform; Sydney, NSW: 2020. SPHERE | in the Know [Website]https://www.sphereintheknow.com/ [Available from: [Google Scholar]
- 23.Boydell K.M., Honey A., Glover H., Gill K., Tooth B., Coniglio F., et al. Making lived-experience research accessible: a design thinking approach to co-creating knowledge translation resources based on evidence. Int. J. Environ. Res. Publ. Health. 2021;18(17):1–9. doi: 10.3390/ijerph18179250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Serrat O. Springer; Singapore: 2017. Knowledge Solutions: Tools, Methods, and Approaches to Drive Organizational Performance. [Google Scholar]
- 25.Braun V., Clarke V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006;3(2):77–101. [Google Scholar]
- 26.Clarke V., Braun V. Teaching thematic analysis: overcoming challenges and developing strategies for effective learning. Psychol. 2013;26:120–123. [Google Scholar]
- 27.Alvesson M., Sandberg J. Generating research questions through problematization. Acad. Manag. Rev. 2011;36(2):247–271. [Google Scholar]
- 28.Boydell K.M., Hodgins M., Gladstone B.M., Stasiulis E., Belliveau G., Cheu H., et al. Arts-based health research and academic legitimacy: transcending hegemonic conventions. Qual. Res. 2016;16(6):681–700. [Google Scholar]
- 29.Wensing M., Grol R. Knowledge translation in health: how implementation science could contribute more. BMC Med. 2019;17(88):1–6. doi: 10.1186/s12916-019-1322-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yamada J., Shorkey A., Barwick M., Widger K., Stevens B.J. The effectiveness of toolkits as knowledge translation strategies for integrating evidence into clinical care: a systematic review. BMJ Open. 2015;5(4) doi: 10.1136/bmjopen-2014-006808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Barwick M. Journeys in Implementation [Internet]. Canada. 2018 https://melaniebarwick.wordpress.com/2018/02/21/is-a-rose-by-any-other-name-still-a-rose-why-knowledge-translation-and-implementation-science-are-not-synonymous/ [cited 2021]. Available from: [Google Scholar]
- 32.Dittrich Y., Eriksén S., Wessels B. Learning through situated innovation: why the specific is crucial for participatory design research. Scand. J. Inf. Syst. 2014;26(1):29–56. [Google Scholar]
- 33.Boydell K. Using performative art to communicate research: dancing experiences of psychosis. Can. Theat. Rev. 2011;146(Spring):12–17. [Google Scholar]
- 34.Watfern C., Triandafilidis Z., Vaughan P., Doran B., Dadich A., Disher-Quill K., et al. Coalescing, cross-pollinating, crystalising: developing and evaluating an art installation about health knowledge. Qual. Health Res. 2023;33(1–2):127–140. doi: 10.1177/10497323221145120. [DOI] [PubMed] [Google Scholar]
- 35.Regional Arts N.S.W. Regional arts network [website]. The rocks, NSW: regional arts NSW. 2021. https://regionalartsnsw.com.au/about-the-network/ [Available from:
- 36.Artist Run Alliance. Explore leading indie art scenes [Website]. Tel Aviv: Alfred Cooperative Institute for Art & Culture; n.d. [Available from: https://artistrunalliance.org/our-vision/.
- 37.Boydell K. The journey to a wider understanding of ways of knowing: knowledge translation and the arts. LEARNing Landscapes. 2019;12(1):19–27. [Google Scholar]
- 38.Greenhalgh T., Snow R., Ryan S., Rees S., Salisbury H. Six 'biases' against patients and carers in evidence-based medicine. BMC Med. 2015;13(200):1–11. doi: 10.1186/s12916-015-0437-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Greenhalgh T., Howick J., Maskrey N. Evidence based medicine: a movement in crisis? Br. Med. Bull. 2014;348:1–7. doi: 10.1136/bmj.g3725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kelly M.P., Health I., Howick J., Greenhalgh T. The importance of values in evidence-based medicine. BMC Med. Ethics. 2015;16(69):1–8. doi: 10.1186/s12910-015-0063-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pearce T., Maple M., Shakeshaft A., Wayland S., McKay K. What is the co-creation of new knowledge? A content analysis and proposed definition for health interventions. Int. J. Environ. Res. Publ. Health. 2020;17(7):1–18. doi: 10.3390/ijerph17072229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Renwick L., McWilliams C., Schaff O., Russell L., Ramsdale S., Morris R.L. Stakeholder identified research priorities for early intervention in psychosis. Health Expect. 2022;25(6):2960–2970. doi: 10.1111/hex.13604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Koren Solvang P., Sveen U., Søberg H.L. User involvement in the making: positions and types of knowledge enacted in the interaction between service users and researchers in user panel meetings. Health Expect. 2021;24(4):1424–1432. doi: 10.1111/hex.13281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mackintosh N., Sandall J., Collison C., Carter W., Harris J. Employing the arts for knowledge production and translation: visualizing new possibilities for women speaking up about safety concerns in maternity. Health Expect. 2018;21(3):647–658. doi: 10.1111/hex.12660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Camden C., Meziane S., Maltais D., Cantin N., Brossard-Racine M., Berbari J., et al. Research and knowledge transfer priorities in developmental coordination disorder: results from consultations with multiple stakeholders. Health Expect. 2019;22(5):1156–1164. doi: 10.1111/hex.12947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.NHMRC (National Health and Medical Research Council) NHMRC (National Health and Medical Research Council); Canberra, ACT: 2016 Sep. Statement on Consumer and Community Involvement in Health and Medical Research. [Google Scholar]
- 47.Bellingham B., Kemp H., Boydell K., Isobel S., Gill K., River J. Towards epistemic justice doing: examining the experiences and shifts in knowledge of lived experience researchers over the course of a mental health research training program. International journal of mental health nursing. 2021;30(6):1588–1598. doi: 10.1111/inm.12910. [DOI] [PubMed] [Google Scholar]
- 48.Vargas C., Whelan J., Brimblecombe J., Allender S. Co-creation, co-design, co-production for public health – a perspective on definitions and distinctions. Public Health Research & Practice. 2022;32(2) doi: 10.17061/phrp3222211. [DOI] [PubMed] [Google Scholar]
- 49.Elder E., Black Dog Institute Lived Experience Advisors . Randwick: Black Dog Institute; 2023. Lived Experience Engagement Framework. [Google Scholar]
- 50.National Mental Health Commission . In: Paid Participation Policy: for People with a Lived Experience of Mental Health Difficulties, Their Families and Support People. Commission N.M.H., editor. Australian Government; Australia: 2019. [Google Scholar]
- 51.Boydell K.M., Dew A., Hodgins M., Bundy A., Gallego G., Iljadica A., et al. How can researchers and policy makers work together? Deliberative dialogues in Canada and Australia. J. Disabil. Pol. Stud. 2017;28(1):13–22. [Google Scholar]
- 52.Sudsawad P. Southwest Educational Development Laboratory; 2007. Knowledge Translation: Introduction to Models, Strategies and Measures. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The paper reports on a collaborative, ideas-generation process rather than a research process. Data were not collected. Therefore, no additional data is available.