Abstract
Purpose
To report an unusual case of ocular surface squamous neoplasia (OSSN) associated with human papilloma virus (HPV)-16 infection with an atypical morphology in a young otherwise healthy patient.
Case description
A 17 year-old healthy male was referred to our department for evaluation of a corneal infiltrate with anterior stromal neovascularization in the right eye. One year before, the patient underwent an excision of a corneo-conjunctival lesion that was located inferiorly in the same eye. Histopathological analysis had shown moderate and severe dysplasia of the conjunctival epithelium and resulted positive for HPV-16. We performed a diagnostic incisional biopsy of the limbal conjunctiva and of the corneal epithelium for histological examination and molecular testing for HPV and Chlamydia by using polymerase chain reaction (PCR). Histopathologic evaluation demonstrated low-grade dysplasia of conjunctiva. PCR testing of the corneal epithelium was positive for HPV-16, similarly to the first biopsy performed by another centre. The patient was successfully treated with topical interferon alfa-2b (1,000,000 IU/ml) for a total of six months. After the treatment, the corneal infiltrate improved dramatically with regression of neovascularization and improvement of corneal transparency and vision.
Discussion
The present report described an atypical presentation of HPV-related OSSN due to its unusual morphology, young age of onset and absence of associated comorbidity.
Conclusion
Conservative treatment with topical interferon-alpha 2b could be used to treat successfully HPV-16 positive OSSN, with no corneal irregularity or potential loss of vision compared to surgical excision.
Keywords: Ocular surface squamous neoplasia, corneal neovascularization, human papilloma virus
Introduction
Ocular surface squamous neoplasia (OSSN) is the most common ocular surface tumour with an approximated incidence of 0.02—3.5 per 100,000. It encompasses lesions that range from mild /severe dysplasia to carcinoma in situ, and conjunctival squamous cell carcinoma. The pathogenesis of OSSN is not completely understood. Several risk factors including ultraviolet light exposure, advanced age, human papilloma virus (HPV) infection and immunodeficiency have been recognized. HPV can be transmitted through sexual contact, autoinoculation, or maternally. Of note, HPV-16 is regarded as one of the most carcinogenic subtypes.1–3 Different reviews have highlighted that the prevalence of HPV in ocular surface disease varies dramatically (0–100%), based on differences in the detection assays, geographic location, and genetic susceptibility.2,4–6 OSSN is most often treated with surgical excision which can be associated with cryotherapy. 3 Topical therapy with mitomycin C, 5-fluorouracil or interferon-alpha 2b can be utilized to reduce risk of extension and recurrence. 7 Immunotherapy with interferon-alpha 2b has been used in conjunctival neoplasia that were tested HPV-16/18 positive, showing lower local side effects in comparison to mitomycin c and 5-fluorouracil.3,8 This cytokine displayed anti-viral, anti-neoplastic, and anti-proliferative actions through immune-enhancing mechanisms, with elevated success rates (80–100%). 8
Herein, we described an unusual case of OSSN in a young healthy patient that resulted positive to HPV-16 on polymerase chain reaction (PCR) analysis. Patient signed a general written informed consent to participate to the present report. The study adhered to Declaration of Helsinki (1975) and its following amendments.
Case description
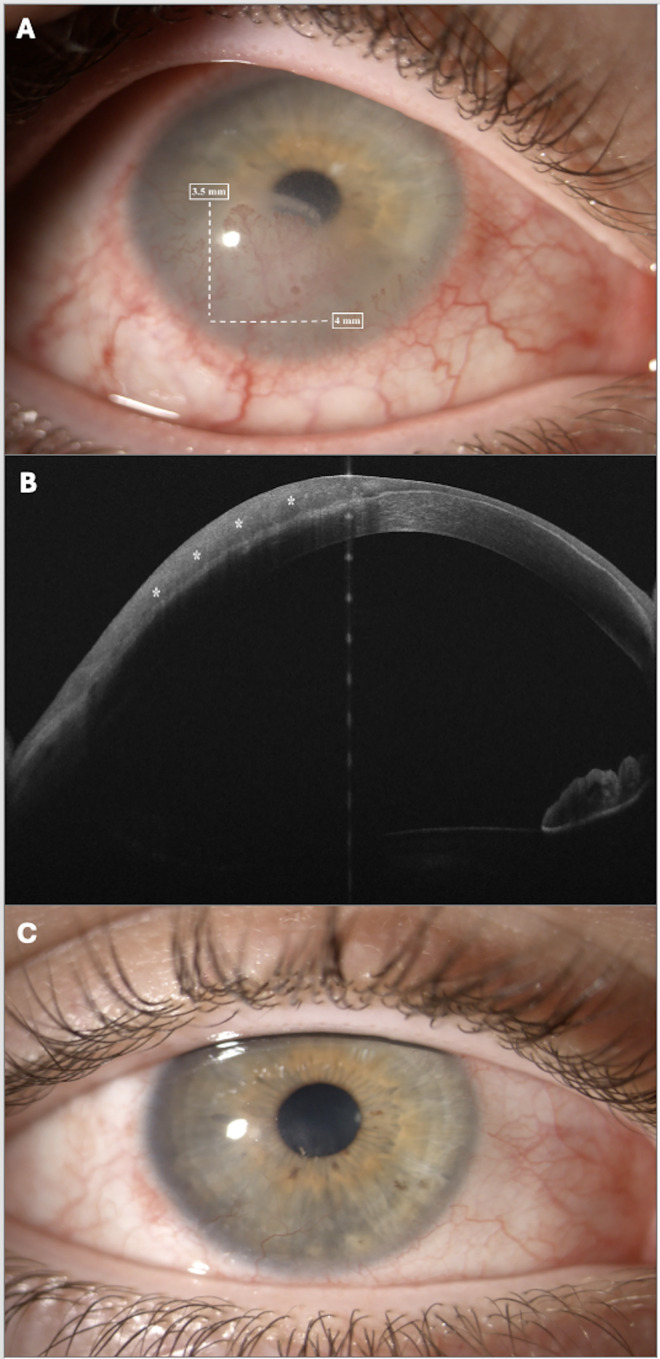
A 17 year-old Caucasian male patient referred to our department for a second evaluation of a corneal infiltrate surrounded by anterior stromal neovascularization in the right eye (RE). He complained about redness, foreign body sensation and photophobia in the past 6 months. The patient had a history of good general health. One year before, he underwent an excision of a corneo-conjunctival lesion located in the inferior sector of the same eye. Unfortunately, photographic documentation of this stage was unavailable, since the surgery was performed in another hospital. Histopathological analysis of this first biopsy showed moderate and severe dysplasia of the conjunctival epithelium, and PCR tested positive for HPV-16 (conjunctival intraepithelial neoplasia grade 3). A course of topical steroids (dexamethasone 0.1% three times daily) for two weeks was prescribed, although with no symptoms relief, nor regression of lesion. Best spectacle corrected visual acuity (BSCVA) was 20/50 and 20/30 by using pin-hole in RE. BSCVA was 20/20 in the left eye (LE). Anterior segment examination of RE showed peripheral superficial corneal neovascularization along 360 degrees, and an inferior corneal infiltrate with stromal neovascularization branching from a conjunctival vessel. The basal length of the infiltrate was 4 mm at the limbus and extended for 3.5 mm into the cornea (Figure 1A). Anterior segment optical coherence tomography revealed the degree of the infiltration, with approximately 50% of involved corneal thickness (Figure 1B). The eye examination was otherwise unremarkable. A diagnostic incisional biopsy of the limbal conjunctiva and of the corneal epithelium was performed. The samples underwent a histological examination that revealed low-grade dysplasia of conjunctiva (conjunctival intraepithelial neoplasia grade 1). Furthermore, PCR test for HPV and Chlamydia was performed. A positivity for HPV-16 was detected, similarly to the first biopsy performed by another centre. The patient was successfully treated with topical interferon alfa-2b (1,000,000 IU/ml) four times/daily for six months with relief of subjective symptoms, and no local or systemic side effects. BSCVA increased to 20/30. The corneal infiltrate improved dramatically with the regression of neovascularization and restoration of corneal transparency (Figure 1C).
Figure 1.
(A) Slit-lamp photograph before starting interferon alfa-2b treatment. External photograph depicting in right eye an inferior corneal infiltrate with stromal neovascularization branching from a conjunctival vessel. The lesion extended at limbus for 4 mm (white arrow) and 3.5 mm into cornea (white arrow). (B) Anterior segment optical coherence tomography (AS-OCT) findings. AS-OCT illustrated the abnormal hyper-reflective region (asterisk) suggestive of ocular surface squamous neoplasia. The lesion extended for about 50% of corneal depth. (C) Slit-lamp photograph after six months of interferon alfa-2b treatment. External photograph after 6 months of interferon alfa-2b treatment. The corneal infiltrate improved dramatically with regression of neovascularization and restored corneal transparency.
Discussion
The present report described an unusual presentation of HPV-related OSSN. No raised papilliform or gelatinous appearance that typically characterizes conjunctival intraepithelial neoplasia was detected, but rather corneal stromal infiltration and neovascularization. Furthermore, the young age of the patient was atypical as well, since OSSN commonly affects 50-years-older patients. 3 Conversely, young patients presenting OSSN are usually associated with other conditions, including xeroderma pigmentosum, human immunodeficiency syndrome, or systemic immunosuppression. 9 Only another previous report described HPV-related OSSN in otherwise healthy subjects similarly to the present case. 10 We believed that a minimally-invasive biopsy may be the best diagnostic histopathological procedure as compared to full-thickness excision, to avoid irregular astigmatism secondary to an asymmetric anterior stroma dissection in a full-thickness approach. Conservative treatment with topical interferon-alpha 2b was successful in restoring corneal transparency without additional surgical excision.
In conclusion, topical treatment with interferon-alpha 2b may be a more successful therapeutic option than surgical excision in treating the lesion, and also in preventing vision loss.
Acknowledgements
None.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Karl Anders Knutsson https://orcid.org/0000-0002-9615-2839
Francesco Bandello https://orcid.org/0000-0003-3238-9682
References
- 1.Di Girolamo N. Association of human papilloma virus with pterygia and ocular-surface squamous neoplasia. Eye 2012; 26: 202–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Woods M, Chow S, Heng B, et al. Detecting human papillomavirus in ocular surface diseases. Invest Ophthalmol Vis Sci 2013; 54: 8069–8078. [DOI] [PubMed] [Google Scholar]
- 3.Chalkia AK, Bontzos G, Spandidos DAet al. et al. Human papillomavirus infection and ocular surface disease. Int J Oncol 2019; 54: 1503–1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scott IU, Karp CL, Nuovo GJ. Human papillomavirus 16 and 18 expression in conjunctival intraepithelial neoplasia. Ophthalmology 2002; 109: 542–547. [DOI] [PubMed] [Google Scholar]
- 5.Sen S, Sharma A, Panda A. Immunohistochemical localization of human papilloma virus in conjunctival neoplasias: a retrospective study. Indian J Ophthalmol 2007; 55: 361–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Koning MN, Waddell K, Magyezi J, et al. Genital and cutaneous human papillomavirus (HPV) types in relation to conjunctival squamous cell neoplasia: a case-control study in Uganda. Infect Agent Cancer 2008; 3: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cohen VML, O'Day RF. Management issues in conjunctival tumours: ocular surface squamous neoplasia. Ophthalmol Ther 2020; 9: 181–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nanji AA, Sayyad FE, Karp CL. Topical chemotherapy for ocular surface squamous neoplasia. Curr Opin Ophthalmol 2013; 24: 336–342. [DOI] [PubMed] [Google Scholar]
- 9.Karp CL, Scott IU, Chang TSet al. et al. Conjunctival intraepithelial neoplasia: a possible marker for human immunodeficiency virus infection? Arch Ophthal 1996; 114: 257–261. [DOI] [PubMed] [Google Scholar]
- 10.Rajagopal R, Agarwal M, Iyer G, et al. Ocular surface squamous neoplasia in a healthy young child. Indian J Ophthalmol Case Rep 2021; 1: 229–230. [Google Scholar]