Abstract
Black and Latinx Americans are disproportionately at greater risk for having Alzheimer’s disease and related dementias (ADRD) than White Americans. Such differences in risk for ADRD are arguably explained through health disparities, social inequities, and historical policies. Structural racism and discrimination (SRD), defined as “macro-level conditions that limit opportunities, resources, and well-being of less privileged groups,” have been linked with common comorbidities of ADRD, including hypertension, obesity, diabetes, depression. Given the historical impact of SRD—including discriminatory housing policies resulting in racial residential segregation that has been shown to limit access to education, employment, and healthcare—Black and Latinx populations with ADRD are directly or indirectly negatively affected by SRD in terms of access, quality and cost for healthcare. Emerging studies have brought to light the value of structural-level hospital and public health collaboration on care coordination for improving healthcare quality and access, and thus could serve as a macro-level mechanism for addressing disparities for minoritized racial and ethnic populations with ADRD. This paper presents a conceptual framework delineating how care coordination can successfully be achieved through health information technology (HIT) systems and ultimately address SRD. To address health inequities, it is therefore critical that policy initiatives invest in HIT capacities and infrastructures to promote care coordination, identify patient needs and preferences, and promote engagement of patients with ADRD and their caregivers.
Keywords: Structural racism and discrimination, health disparity, ADRD, health information technology, care coordination, system integration
INTRODUCTION
Black and Latinx Americans over 65 years of age have the highest prevalence of Alzheimer’s disease and related dementias (ADRD), with estimates predicting there will be 3.2 million Latinx and 2.2 million Black or African Americans with ADRD by 2060.1 Structural racism and discrimination (SRD), defined as “macro-level conditions that limit opportunities, resources, and well-being of less privileged groups,”2 have been linked with common comorbidities of ADRD including hypertension,3 heart diseases,4 cognitive impairment,5 and diabetes.6 The historical impact of SRD (i.e., housing policies that resulted in racial residential segregation which has been shown to limit access to education, employment, and healthcare)7,8 has created structural barriers in the healthcare delivery system among Black and Latinx populations. These structural barriers are likely to have directly or indirectly affected access, quality and cost of healthcare among older Black and Latinx populations with ADRD.9 However, most of the ADRD literature on improving healthcare access and equity focuses on individual-level factors, while evidence at structural-level factors is lacking.
Chen and colleagues developed the Hospital and Public Health InterdisciPlinarY (HAPPY) framework10 and the patient-centered multi-level personalized patient activation and empowerment framework,”11 which emphasizes the importance of building community capacity to provide healthcare and social services. Evidence shows that cross-sector collaborations between hospitals and public health entities can improve healthcare quality and reduce disparities11,12 for minoritized racial and ethnic populations with ADRD and risk factors.13 Care coordination, specifically, the deliberate organization of patient care and sharing of information across those involved in promoting quality healthcare, can successfully be achieved by leveraging HIT to support efficient data sharing with organizations outside of the healthcare system (e.g., public health, social services) and bidirectional patient-provider communication.14 Health systems have shown innovation in adopting HIT tools to improve efficiency and quality of healthcare delivery. For example, the Veterans Health Administration has used thousands of HIT applications for their veteran population.15 Such efforts were made possible through engagement with stakeholders in the development of digital applications to ensure user-friendly, affordable, accessible, and convenient applications; this can help facilitate adoption and overcome barriers among certain populations. A recent study also demonstrated the effectiveness of telehealth-supported collaborative models (i.e., the telepsychiatry collaborative care model and telepsychiatry/telepsychology–enhanced referral model) in improving perceived patient care access and engagement and health outcomes for patients with complex psychiatric disorders.16
In this article, we present a framework based on the HAPPY model that promotes System-level Multidisciplinary Integration for popuLation health and Equity (SMILE) and explicitly includes HIT (i.e., HAPPY+HIT model). HIT is defined as “the electronic health systems used by healthcare systems, providers, and increasingly by patients to store, share, and analyze health information.”17 HIT is increasingly being used to support care coordination, by leveraging electronic health records (EHRs) to enable both providers and patients to ensure effective transitions of care, especially follow-up care post-ED visits.18,19 HIT has been used to advance patient engagement functionalities by leveraging personal health records from patient portals to actively involve patients and caregivers in managing their healthcare.20 Hospitals that report higher rates of adoption of patient engagement functionalities have been found to have lower readmission rates and higher patient satisfaction rates.21 Despite its promise, however, there is a dearth of knowledge on structural-level HIT adoption that includes community-level HIT infrastructure, hospital-level HIT adoptions, cross-sectional HIT collaborations, and systemic-level efforts, including policies and laws to promote community investment and HIT adoptions. Our framework presents SRD in ADRD care, then focuses on structural-level HIT adoption and delineates the mechanisms through which HIT adoption can be used to reduce SRD for patients with ADRD and their caregivers. We also discuss the challenges in utilizing HIT and call for future studies and policy initiatives that invest in HIT infrastructure for healthcare providers and patients that could support better patient care coordination and patient-provider engagement.
FRAMEWORK OF STRUCTURAL RACISM AND DISCRIMINATION IN ADRD
We adapted and expanded the HAPPY framework—which focuses on using local health departments as a health system partner to expand healthcare access and coordinate care for enabling services—to explicitly include HIT and incorporate tenets of the World Health Organization Social Determinants of Health Framework (2010).22 Figure 1 presents a theory of change model that describes how HAPPY + HIT can contribute to the Quadruple Aim of improving healthcare access, quality, reducing cost, and improving health equity.
FIGURE 1.
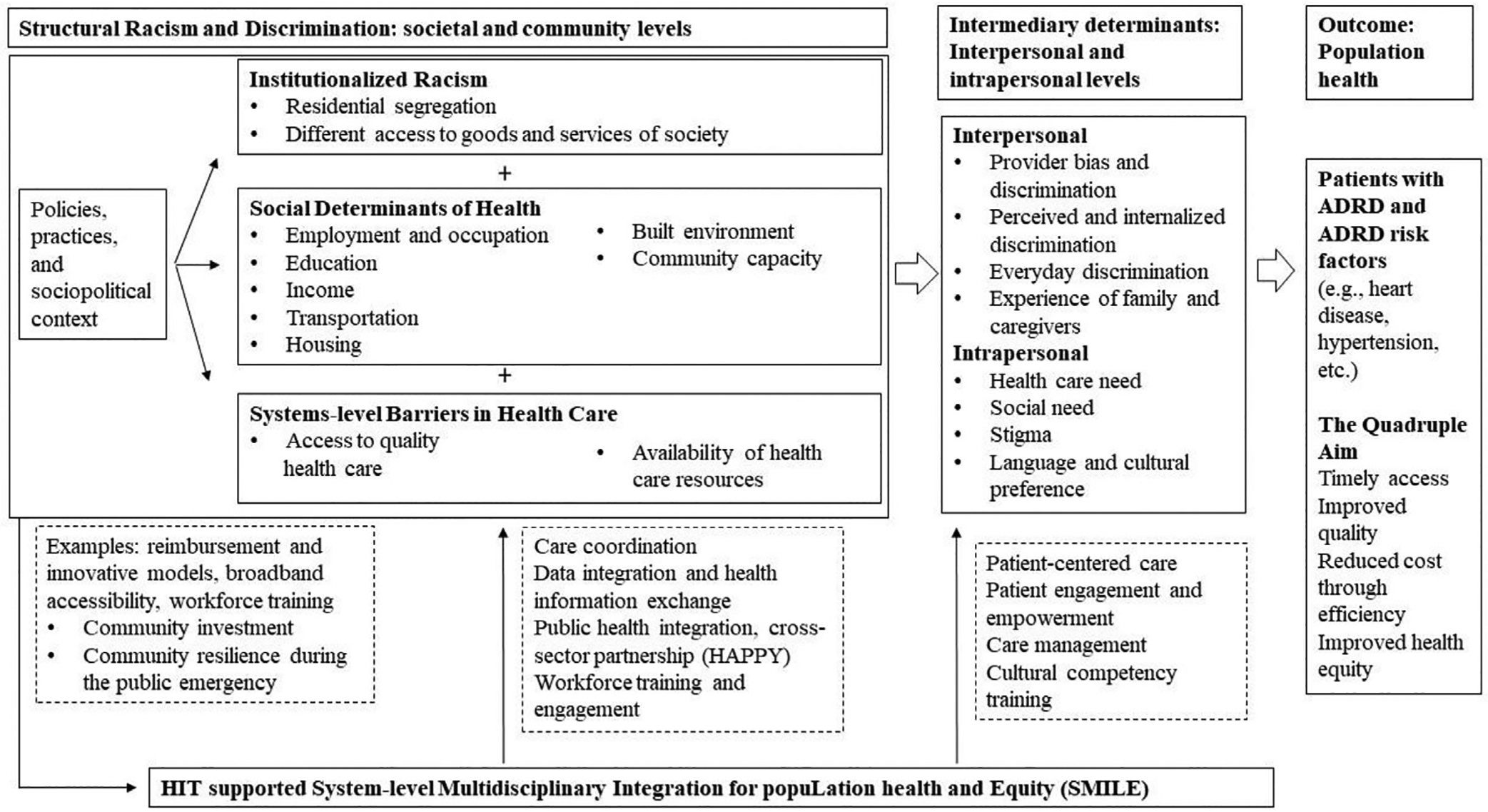
Framework of structural racism and discrimination in ADRD: Hospital and Public Health InterdisciPlinarY Research (HAPPY) + Health Information Technology.
We hypothesize that enhanced HIT infrastructures that promote care coordination and patient engagement (i.e., EHRs and patient portals) are critical for improving healthcare quality for minoritized racial and ethnic populations with ADRD and ADRD risk factors. The rationale is that a care coordination model supported by HIT can potentially address: 1) institutionalized racism by improving equitable societal access,8 2) social determinants of health (SDOH)22 by improving community healthcare capacity, and 3) system-level barriers in healthcare delivery system by having more coordinated and quality healthcare resources.13 Improving the HIT infrastructure can potentially address longstanding systemic barriers to patient access and engagement, user bias, and discrimination, which have implications for the quality of healthcare delivery. Improved HIT-supported services can improve care coordination for patients with ADRD by increasing patient engagement, and identify patient needs (e.g., social support services) and preferences.
ELEMENTS OF THE HAPPY+HIT MODEL
Structural Racism and Discrimination: Societal and Community Levels
SRD is the interaction of macro-level systems and institutions, including housing, education, employment, healthcare, and other systems, that produce and reinforce inequities among minoritized racial and ethnic populations.23 Seminal works suggest that racism can directly and indirectly impact quality of life for minoritized racial and ethnic groups and also influence sociocultural factors, including the quality of education, ability to receive affordable healthcare, and determination of where individuals live.24–27 Camara Jones’ theoretical framework categorizes three levels of racism: institutionalized, personally mediated, and internalized racism.25 Jones defines institutionalized racism as “the differential access to the goods, services, and opportunities of society by race,” and argues that SRD can manifest as differential access to quality healthcare. Similarly, according to Nancy Krieger, SRD pathways include “economic and social deprivation,” “inadequate medical care,” and “ecosystem degradation and alienation from the land.”26 Institutionalized racism in U.S. housing policies produced racial/ethnic residential segregation, which has resulted in differential healthcare quality by neighborhoods, with neighborhoods with higher concentrations of minoritized racial and ethnic populations experiencing lower quality healthcare compared to predominately White neighborhoods.7
Structural Racism and Discrimination: Intermediary Determinants
Provider and institutional bias within the healthcare system has been shown to contribute to disparities in patient care and health outcomes.28 The 2021 Alzheimer’s Disease Facts and Figures reported that “…the ability to obtain a diagnosis, manage the disease, and access care and support services for dementia vary widely depending on race, ethnicity, geography and socioeconomic status.”29 Black/African American patients are two times more likely to have dementia underdiagnosed than Latinx and White patients, which results in delayed care and lower quality of care for Black/African American patients with ADRD.30 In addition, minoritized racial and ethnic populations often have more challenges in accessing and receiving high quality dementia care and support services.29 Minoritized racial and ethnic populations with ADRD are at especially high risk for receiving uncoordinated and low-quality care, with higher rates of hospitalizations particularly among Black and Latinx populations.31 They also experience ADRD diagnoses at later stages, delays in timely primary care with higher levels of impairment at time of referral to ADRD services,32 as well as have lower rates of prescriptions for antidementia medications.33 Although minoritized racial and ethnic populations have disproportionately higher rates of physical inactivity, smoking, and chronic conditions (all of which are risk factors for ADRD),34 these outcomes and behaviors are driven by SDOH factors (e.g., income, education, environmental conditions) that make it difficult to adopt behaviors to mitigate these risk factors.35
HIT Supported System-level Multidisciplinary Integration for population health and Equity (SMILE)
The National Plan to Address Alzheimer’s Disease 2020 noted that public health and health system integration is critical for addressing SDOH and promoting culturally appropriate population assessment, prevention, and treatment of ADRD, as well as risk factors for ADRD.36 Community-based care coordination interventions have been shown to improve quality of care and quality of life for patients with ADRD. Also, patients with ADRD enrolled in care coordination programs have been found to have greater quality of life, less neuropsychiatric symptoms, and less unmet safety and advanced care needs than those not enrolled in care coordination programs.37,38
HIT and care coordination
The 2020 National Health IT Priorities for Research report by the National Coordinator for Health Information Technology,39 has notably acknowledged how HIT can ensure better access for healthcare providers to access health information and improve care coordination. HIT-supported care coordination can play an essential role in managing care for patients with ADRD at home through referrals to community-based social supports services such as home care agencies for additional in-home supports. Access and utilization of patient portals, for example, can support these patients in monitoring their care and keeping in touch with their healthcare team by messaging through patient portals. The information exchange functionalities of HIT systems are critical to the digitalization of healthcare as it relates to interoperability, data management and integration, building predictive tools, surveillance systems, artificial intelligence, and post-discharge remote patient monitoring.40
HIT and Data Integration
Multifaceted and patient specific considerations in the treatment and management of coexisting ADRD chronic conditions are necessary. A well-designed HIT infrastructure can facilitate the information exchange among a multi-disciplinary team of providers (e.g., primary care and hospitals) and advance care coordination for people with complex health needs by leveraging EHRs, participating in health information exchanges, overcoming interoperability barriers, and querying information among healthcare providers and across sectors.
Remote patient monitoring following hospital discharge,41 data sharing between hospitals and outpatient providers through portals, integrating data into the EHR,42 and automatic notifications regarding care transitions43 are some of the strategies that can support care coordination and facilitate chronic disease management.44 For example, automatic notifications of ED visits and inpatient admissions and discharges to primary care providers encourage timely follow-up and have been found to decrease the risk of readmissions among Medicare fee-for-service beneficiaries.45
Implementing data integration and sharing between institutions to improve care coordination across sectors has the potential to break down longstanding silos and bridge the gap between healthcare providers, community-based organizations, social service agencies, and the public health sector. HIEs allow for the dissemination of ED and hospital records to community-based providers and aim to minimize communication failures that frequently occur during the care transition process.46,47 For home- and community-based services (HCBS), EHRs may support the standardization of HCBS eligibility assessments and even data retrieval. Challenges with data integration include clear communication, staffing, employee skill sets, resources, standardization of policies and system capabilities, which demonstrate the siloed operations of healthcare and social services.48,49
HIT and Data Collection of Social Determinants of Health
Incorporating the collection and use of SDOH data has been highlighted as a strategy to address racial disparities in healthcare delivery.50 Although there is no standardization for SDOH measures, some health systems have begun using these measures and data to improve quality initiatives. The Boston Medical Center tested the feasibility of using a SDOH screening and referral program in their internal medicine clinics and linked SDOH measures to ICD-10 codes in the EHR to help track and monitor patients needing referrals to social supports.51 There have also been recommendations to integrate community-level data into EHRs to expand the reach of initiatives mitigating health inequities by addressing community-wide social needs.52
Health systems that are considering using SDOH measures should use caution to ensure that measures used are applied through a health equity lens. Use of EHRs can result in bias, which can stem from the structural design of the data that is compiled. These data can be impacted by implicit biases of healthcare providers’ documentation in these records, which informs clinical decision-making, thus contributing to system-level discrimination within healthcare.53 Stigmatizing language in EHRs documentation has the potential to cause harm by reinforcing racial bias in healthcare.54 Still, innovative use of EHRs can support care coordination efforts and information sharing between care providers and organizations, which improves the quality of care and access to additional social supports, which is critical for patients with ADRD.
HIT and Patient-Centered Care
HIT has been used to advance patient engagement functionalities.20 This includes effective design of patient portals, which can allow patients to view their medical records, schedule appointments, and communicate with their providers through a platform that can be accessed from multiple devices (i.e., computer or smartphone) with a user-friendly navigation.55 Patient portals have been found to improve adherence to medications, reduce medical errors, and improve patient-provider communication.56 Using alternative devices such as mobile phones have the potential to serve as a temporary solution57 in mitigating barriers to broadband and improve utilization of HIT patient engagement functionalities.
Emerging studies acknowledge HIT’s potential to improve access to patient-centered care for patients with ADRD (and caregivers), especially for those who experience healthcare disparities. Patient portals that are designed to be patient-centered can engage and empower patients and caregivers. As such, we are more likely to observe personalized and efficient care management and treatment plans for patients with ADRD under an effective HIT-facilitated information exchange platform. Integrated data platforms with individual, caregiver, and healthcare provider measures on clinic, healthcare services, social services, and life-course disease development and progression data can improve healthcare delivery and outcomes, particularly for minoritized racial/ethnic patients with ADRD.
THE ROLE OF POLICIES TO ADDRESS THE SRD IN ADRD
Since the Health Information Technology for Economic and Clinical Health (HITECH) Act of 2010 HIT capacity within health systems have increased.58 Still, many patient populations have been excluded from the benefit of engaging with HIT tools to support their health.
Innovative and Reimbursement Models
Healthcare delivery models that use team-based approaches and financial incentives can be designed to promote community collaboration and expand community-HIT capacity.59–61 For example, the Health Outcomes, Planning, and Education for Alzheimer’s (HOPE) Act supports healthcare providers’ ability to bill and be reimbursed for care management of ADRD, using the new Current Procedural Terminology (CPT) codes.62 Innovative models, such as accountable care organizations (ACOs) purport to improve care coordination both through tailored healthcare design and incorporation of SDOH. Specifically, ACOs provide financial incentives to providers (e.g., using CPT codes to reimburse for dementia care management activities) to promote care coordination across care settings.63 ACOs are positioned to ensure comprehensive needs assessments are provided to adults with complex health needs to determine what patients need to safely remain in the community and ensure they receive nonmedical care such as Meals on Wheels and adult day care.
Broadband Accessibility
Barriers in home broadband access, especially among underserved patients remains challenging.64 Evidence has shown that access to home-based broadband has followed historical racial residential segregation patterns within metropolitan areas, with areas with high concentrations of minoritized racial/ethnic populations being less likely to have in home broadband. Broadband inaccessibility has been characterized as a SDOH, as it restricts patient access to healthcare resources including health information and digital-based health services and their medical data.65 The COVID-19 pandemic has exacerbated these barriers. As HIT patient engagement functionalities become more sophisticated, having access to broadband at higher speeds will be imperative.
Workforce Training and Engagement
Effective coordination requires a team of numerous healthcare providers across an array of trained medical staff (e.g., primary care providers, case managers, or social workers) who can understand and address these complex issues of ADRD. Ensuring the healthcare workforce is effectively trained and competent in HIT is an essential component in successfully utilizing HIT to support care coordination.66 For example, Community health workers (CHWs) play an important role in building connections between healthcare systems and the community by serving as liaisons between healthcare settings and communities.67 CHWs, who are uniquely positioned to increase the availability of culturally competent care, would benefit from healthcare organizational efforts to incorporate strategies for using HIT tools.
THE ERA FOR HIT-INTEGRATED CARE COORDINATION
The COVID-19 pandemic has advanced the way the healthcare industry utilizes HIT. Evidence has suggested that HIT is a useful tool to expand healthcare access by utilizing remote providers, streamlining treatment, and easing burnout among frontline healthcare providers.68 Further, HIT has been recognized as a feasible alternative for readily assessing and diagnosing ADRD, allowing for earlier interventions, easier follow-up care and easier management of ADRD. Use of HIT for care coordination, especially among older populations with chronic conditions, present its own set of challenges that must be considered. Older adults are generally less comfortable navigating through technology, may lack access to internet, or may be dealing with limitations that affect their ability to utilize technology.69 Thus, more research on the unique challenges for patients with ADRD effectively utilizing HIT, especially among minoritized populations with ADRD is critical for addressing health inequities.
Highlights.
-
What is the primary question addressed by this study?
This paper presents a conceptual framework delineating how care coordination can successfully be achieved through health information technology (HIT) systems and hence reduce structural racism and discrimination (SRD) for ADRD patients and their caregivers.
-
What is the main finding of this study?
Based on the literature review, we hypothesize that enhanced HIT infrastructures that promote care coordination and patient engagement are critical to improving healthcare quality for racial and ethnic minority groups with ADRD. The rationale is that HIT supported care coordination model can potentially address: (1) institutionalized racism by improving equitable societal access, (2) structural barriers in healthcare delivery system by having more coordinated and quality healthcare resources, and (3) structural and social determinants of health by improving community healthcare capacity.
-
What is the meaning of the finding?
Improved HIT-supported services can improve care coordination for ADRD patients, identify patient needs and preferences, and thus understand health disparities for ADRD patients.
DISCLOSURES
This study is supported by the National Institute on Aging (R01AG62315) and the National Institute on Minority Health and Health Disparities (R01MD011523S1).
Footnotes
No conflicts of interest.
DATA STATEMENT
The data has not been previously presented orally or by poster at scientific meetings.
References
- 1.Matthews KA, Xu W, Gaglioti AH, et al. : Racial and ethnic estimates of Alzheimer’s disease and related dementias in the United States (2015–2060) in adults aged ≥65 years. Alzheimer’s Dement 2019; 15:17–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lukachko A, Hatzenbuehler ML, Keyes KM: Structural racism and myocardial infarction in the United States. Soc Sci Med 2014; 103:42–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kershaw KN, Diez Roux AV, Burgard SA, et al. : Metropolitan-level racial residential segregation and black-white disparities in hypertension. Am J Epidemiol 2011; 174:537–545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kershaw KN, Osypuk TL, Do DP, et al. : Neighborhood-level racial/ethnic residential segregation and incident cardiovascular disease. Circulation 2015; 131:141–148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weuve J, Barnes LL, Mendes de Leon CF, et al. : Cognitive aging in black and white Americans: Cognition, cognitive decline, and incidence of Alzheimer disease dementia. Epidemiology 2018; 29:151–159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Whitaker KM, Everson-Rose SA, Pankow JS, et al. : Experiences of discrimination and incident Type 2 diabetes mellitus: The Multi-Ethnic Study of Atherosclerosis (MESA). Am J Epidemiol 2017; 186:445–455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Williams DR, Collins C: Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep 2001; 116:404–416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bailey ZD, Krieger N, Agénor M, et al. : Structural racism and health inequities in the USA: evidence and interventions. Lancet 2017; 389:1453–1463 [DOI] [PubMed] [Google Scholar]
- 9.Alvidrez J, Tabor DC: Now is the time to incorporate the construct of structural racism and discrimination into health research. Ethn Dis 2021; 31:283–284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen J, Bloodworth R, Novak P, et al. : Reducing preventable hospitalization and disparity: association with local health Department Mental Health Promotion Activities. Am J Prev Med 2018; 54:103–112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen J, Mullins CD, Novak P, et al. : Personalized strategies to activate and empower patients in health care and reduce health disparities. Health Educ Behav 2016; 43:25–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen J, Novak P, Barath D, et al. : Local Health Departments’ Promotion of mental health care and reductions in 30-day all-cause readmission rates in Maryland. Med Care 2018; 56:153–161 [DOI] [PubMed] [Google Scholar]
- 13.Wang N, Albaroudi A, Benjenk I, et al. : Exploring hospital-based health information technology functions for patients with Alzheimer’s Disease and related Dementias. PrevMed Rep 2021; 23:101459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fulmer T, Reuben DB, Auerbach J, et al. : Actualizing better health and health care for older adults. Health Affairs 2021; 40:219–225 [DOI] [PubMed] [Google Scholar]
- 15.Vega R, Goldsack J, Patel S, et al. : Putting digital health innovation into practice: learning from The VHA. Health Affairs Forefront 2022., Available at: https://www-healthaffairs-org.proxy-um.researchport.umd.edu/do/10.1377/forefront.20220217.522347/. Accessed March 14, 2022 [Google Scholar]
- 16.Bruce ML, Sirey JA: Integrated care for depression in older primary care patients can. J Psychiatry 2018; 63:439–446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.What Is Health Information Technology Fact Sheet. Office of the National Coordinator for Health Information Technology. Available at: https://www.healthit.gov/sites/default/files/pdf/health-information-technology-fact-sheet.pdf. Accessed March 1, 2022. [Google Scholar]
- 18.Foster B, Krasowski MD: The use of an electronic health record patient portal to access diagnostic test results by emergency patients at an academic medical center: Retrospective Study. JMed Internet Res 2019; 21:e13791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rahurkar S, Vest JR, Finnell JT, et al. : Trends in user-initiated health information exchange in the inpatient, outpatient, and emergency settings. J Am Med Inform Assoc 2021; 28:622–627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Asagbra OE, Burke D, Liang H: The association between patient engagement HIT functionalities and quality of care: does more mean better? Int J Med Inform 2019; 130:103893. [DOI] [PubMed] [Google Scholar]
- 21.Elysee G, Yu H, Herrin J, et al. : Association between 30-day readmission rates and health information technology capabilities in US hospitals. Medicine 2021; 100:e24755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.A Conceptual Framework for Action on the Social Determinants of Health. World Health Organization, 2010. Available at: https://www.who.int/social_determinants/corner/SDHDP2.pdf?ua=1. Accessed August 16, 2021 [Google Scholar]
- 23.Powell JA: Structural racism: building upon the insights of John Calmore A Tribute to John O. Calmore’s Work. NC L Rev 2007; 86:791–816 [Google Scholar]
- 24.Jones CP: Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health 2000; 90:1212–1215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gee GC, Ford CL: Structural racism and health inequities: old issues, new directions1. Du Bois Rev: SocSci Res Race 2011; 8:115–132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krieger N: Discrimination and health inequities. Int J Health Serv 2014; 44:643–710 [DOI] [PubMed] [Google Scholar]
- 27.LaVeist TA: Segregation, poverty, and empowerment: health consequences for African Americans. Milbank Q 1993; 71:41–64 [PubMed] [Google Scholar]
- 28.Smedley BD, Stith AY, Nelson AR, eds. Medicine I of: Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care., Washington, DC: The National Academies Press, 2003. Available at: https://www.nap.edu/catalog/12875/unequal-treatment-confronting-racial-and-ethnic-disparities-in-health-care. Accessed February 10, 2022 [PubMed] [Google Scholar]
- 29.Race, Ethnicity and Alzheimer’s in America. Alzheimer’s Association, 2021. Available at: https://www.alz.org/media/Documents/alzheimers-facts-and-figures-special-report.pdf. Accessed August 15, 2021
- 30.Gianattasio KZ, Prather C, Glymour MM, Ciarleglio A, Power MC: Racial disparities and temporal trends in dementia misdiagnosis risk in the United States. Alzheimer’s Dement 2019; 5:891–898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Davydow DS, Zivin K, Katon WJ, et al. : Neuropsychiatric disorders and potentially preventable hospitalizations in a Prospective Cohort Study of Older Americans. J Gen Intern Med 2014; 29:1362–1371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bassuk SS, Glass TA, Berkman LF: Social disengagement and incident cognitive decline in community-dwelling elderly persons. Ann Intern Med 1999; 131:165–173 [DOI] [PubMed] [Google Scholar]
- 33.Thorpe CT, Fowler NR, Harrigan K, et al. : Racial and ethnic differences in initiation and discontinuation of antidementia drugs by medicare beneficiaries. J Ame Geriatr Soc 2016; 64:1806–1814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chin AL, Negash S, Hamilton R: Diversity and disparity in dementia: the impact of ethnoracial differences in Alzheimer’s disease. Alzheimer Dis Assoc Disord 2011; 25:187–195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Woolf SH, Braveman P: Where health disparities begin: the role of social and economic determinants—and why current policies may make matters worse. Health Affairs 2011; 30:1852–1859 [DOI] [PubMed] [Google Scholar]
- 36.National Plan to Address Alzheimer’s Disease 2020 Update. U.S. Department of Health and Human Services, 2020. Available at: https://aspe.hhs.gov/sites/default/files/migrated_legacy_files//197726/NatlPlan2020.pdf. Accessed August 23, 2021
- 37.Vickrey BG, Mittman BS, Connor KI, et al. : The effect of a disease management intervention on quality and outcomes of dementia care. Ann Intern Med 2006; 145:713–726 [DOI] [PubMed] [Google Scholar]
- 38.Samus QM, Johnston D, Black BS, et al. : A multidimensional home-based care coordination intervention for elders with memory disorders: the Maximizing Independence at Home (MIND) Pilot Randomized Trial. Am J Geriatr Psychiatry 2014; 22:398–414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.National Health IT Priorities for Research: A Policy and Development Agenda: Office of the National Coordinator for Health Information Technology, 2020. Available at: https://www.healthit.gov/sites/default/files/page/2020-01/PolicyandDevelopmentAgenda.pdf. Accessed October 29, 2021
- 40.Atasoy H, Greenwood BN, McCullough JS: The digitization of patient care: a review of the effects of electronic health records on health care quality and utilization. Annu Rev Public Health 2019; 40:487–500 [DOI] [PubMed] [Google Scholar]
- 41.Brennan KA, Kang H, Kraus S, et al. : Harnessing remote patient monitoring technology to improve transitions of care. J Am Geriatr Soc 2021; 69(suppl 1):S63 [Google Scholar]
- 42.Orenstein D: EHR Integration: A Digital Health Imperative. Health Catalyst 2021, Available at: https://www.healthcatalyst.com/insights/EHR-integration-digital-health-imperative. Accessed February 10, 2021 [Google Scholar]
- 43.Office of the National Coordinator for Health Information Technology: Improving Hospital Transitions and Care Coordination Using Automated Admission, Discharge and Transfer Alerts. 2013. Available at: https://www.healthit.gov/sites/default/files/onc-beacon-lg1-adt-alerts-for-toc-and-care-coord.pdf. Accessed January 2022
- 44.Poku MK, Kagan CM, Yehia B: Moving from care coordination to care integration. J Gen Internal Med 2019; 34:1906–1909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Unruh MA, Jung HY, Kaushal R, et al. : Hospitalization event notifications and reductions in readmissions of Medicare fee-for-service beneficiaries in the Bronx, New York. J Am Med Inform Assoc 2017; 24:e150–e156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vest JR, Kern LM, Silver MD, et al. : The potential for community-based health information exchange systems to reduce hospital readmissions. J Am Med Inform Assoc 2015; 22:435–442 [DOI] [PubMed] [Google Scholar]
- 47.Chen M, Guo S, Tan X: Does health information exchange improve patient outcomes? empirical evidence from Florida hospitals. Health Affairs 2019; 38:197–204 [DOI] [PubMed] [Google Scholar]
- 48.Walker DM, Yeager VA, Lawrence J, et al. : Identifying opportunities to strengthen the public health informatics infrastructure: exploring Hospitals’ Challenges with Data Exchange. Milbank Q 2021; 99:393–425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Khan S, Shea CM, Qudsi HK: Barriers to local public health chronic disease surveillance through health information exchange: a capacity assessment of Health Departments in the Health Information Network of South Texas. J Public Health Manag Pract 2017; 23:e10–e17 [DOI] [PubMed] [Google Scholar]
- 50.Jean-Francois B, Bailey Lash T, Dagher RK, et al. : The potential for health information technology tools to reduce racial disparities in maternal morbidity and mortality. J Women’s Health 2021; 30:274–279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Buitron de la Vega P, Losi S, Sprague Martinez L, et al. : Implementing an EHR-based screening and referral system to address social determinants of health in primary care. Med Care 2019; 57 (suppl 2):S133–S139 [DOI] [PubMed] [Google Scholar]
- 52.Zhang X, Hailu B, Tabor DC, et al. : Role of health information technology in addressing health disparities: patient, clinician, and system perspectives. Med Care 2019; 57:S115–S120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rozier MD, Patel KK, Cross DA: Electronic health records as biased tools or tools against bias: a conceptual model. Milbank Q 2020; 100:134–150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sun M, Oliwa T, Peek ME, et al. : Negative patient descriptors: documenting racial bias in the electronic health record. Health Affairs 2022; 41:203–211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Irizarry T, Dabbs AD, Curran CR: Patient portals and patient engagement: a state of the science review. J Med Internet Res 2015; 17:e4255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dendere R, Slade C, Burton-Jones A, et al. : Patient portals facilitating engagement with inpatient electronic medical records: a systematic review. J Med Internet Res 2019; 21:e12779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Serrano KJ, Thai CL, Greenberg AJ, et al. : Progress on broadband access to the internet and use of mobile devices in the United States: tracking healthy people 2020 goals. Public Health Rep 2017; 132:27–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Apathy NC, Holmgren AJ, Adler-Milstein J: A decade post-HITECH: critical access hospitals have electronic health records but struggle to keep up with other advanced functions. J Am Med Inform Assoc 2021; 28:1947–1954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bruce ML, Sirey JA: Integrated care for depression in older primary care patients can. J Psychiatry 2018; 63:439–446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Goldfarb D, Allen AM, Nisson LE, et al. : Design and development of a community-based, interdisciplinary, collaborative dementia care program. Am J Geriatr Psychiatry 2022; 30:651–660 [DOI] [PubMed] [Google Scholar]
- 61.Heintz H, Monette P, Epstein-Lubow G, et al. : Emerging collaborative care models for dementia care in the primary care setting: a Narrative Review. Am J Geriatr Psychiatry 2020; 28:320–330 [DOI] [PubMed] [Google Scholar]
- 62.Improving HOPE Act Fact Sheet 2021. Alzheimer’s Impact Movement, May 2021. Available at: https://alzimpact.org/media/serve/id/5c9e43d66e8dc. Accessed October 28, 2021.
- 63.Chen J, Benjenk I, Barath D, et al. : Disparities in preventable hospitalization among patients with Alzheimer diseases. Am J Prev Med 2021; 60:595–604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ahluwalia SC, Friedman E, Siconolfi D, et al. : Promises and pitfalls of health information technology for home- and community-based services. J Appl Gerontol 2021; 40:558–565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bauerly BC, McCord RF, Hulkower R, et al. : Broadband access as a public health issue: the role of law in expanding broadband access and connecting underserved communities for better health outcomes. J Law Med Ethics 2019; 47:39–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Fridsma D: Basic informatics literacy: building a health information technology workforce. J Am Med Inform Assoc 2016; 23:666. [DOI] [PubMed] [Google Scholar]
- 67.Payne J, Razi S, Emery K, et al. : Integrating Community Health Workers (CHWs) into Health Care Organizations. J Community Health 2017; 42:983–990 [DOI] [PubMed] [Google Scholar]
- 68.Kvedar J, Coye MJ, Everett W: Connected health: a review of technologies and strategies to improve patient care with telemedicine and telehealth. Health Aff (Millwood) 2014; 33:194–199 [DOI] [PubMed] [Google Scholar]
- 69.Lam K, Lu AD, Shi Y, et al. : Assessing telemedicine unreadiness among older adults in the United States during the COVID-19 pandemic. JAMA Internal Med 2020; 180:1389–1391 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data has not been previously presented orally or by poster at scientific meetings.


