Introduction
Historically, red yeast rice (Red koji) has been a cornerstone in the culinary and medicinal traditions of East Asia, contributing to the production of alcoholic beverages, fermented foods, and notably, tofuyo, a fermented tofu delicacy originating from Okinawa, Japan, since the eighteenth century (Supplementary Figures S1 and S2). The discovery of monacolin K, a natural statin, within Monascus fungi catalyzed the development of lovastatin, heralding a new era in hyperlipidemia management worldwide.1 In Japan, since 2021, red yeast rice supplements have become popular choices for health-conscious individuals because they are effective in regulating low-density lipoprotein cholesterol levels.2 However, recent incidents have cast a shadow over their safety.
A series of acute kidney injury (AKI) incidents associated with these supplements distributed by a specific company, as reported on March 22, 2024, has sparked significant health concerns.S1,S2 This surge in AKI cases, particularly within a short timeframe, suggests the possibility of contamination during a specific production period, raising alarms over the supplement’s safety. Considering these developments, our report gains critical importance, documenting the first series of consecutive AKI cases due to acute tubulointerstitial nephritis (ATIN). Renal biopsies validated the diagnosis of Fanconi syndrome after the intake of red yeast rice supplements. The methods used are described in the Supplementary Methods.
Results
Case 1
A 73-year-old woman, who had been healthy since November 2023, noticed foamy urine. Thus, she visited a nearby clinic in early December 2023. She was admitted to our hospital due to elevated serum creatinine (Cr) levels and urinary problems. We observed hypokalemia, hypophosphatemia, hypouricemia, and metabolic acidosis (Table 1). Urinary β2-microglobulin and N-acetyl-β-D-glucosaminidase levels were also high. Her serum Cr level and estimated glomerular filtration rate were 1.27 mg/dl and 32.2 ml/min per 1.73 m2, respectively. AKI due to renal tubular injury accompanied by Fanconi syndrome was suspected. She was treated with steroid pulse therapy and prednisolone and was temporarily discharged from our hospital with a kidney biopsy scheduled for the following year (due to the New Year holidays). A kidney biopsy was performed on January 18, 2024 (Figure 1a, b, and c). Mild tubular atrophy and fibrosis were observed in the tubulointerstitial region. The findings revealed the convalescent stage of tubulointerstitial nephritis. After a previous medical checkup had revealed that she had dyslipidemia, she had been taking “red yeast rice” supplements since April 2023.
Table 1.
Physical findings and laboratory data on admission
| Variables | Case 1 | Case 2 | Case 3 |
|---|---|---|---|
| Physical findings | |||
| Age, yr | 73 | 53 | 55 |
| Gender | Female | Female | Female |
| Body mass index, kg/m2 | 20.7 | 21.7 | 24.0 |
| Blood pressure, mm Hg | 142/82 | 154/75 | 154/92 |
| Heart rate, bpm | 82 | 72 | 95 |
| Blood test | |||
| White blood cell, /μl | 5,600 | 5,300 | 8,900 |
| Eosinophil, /μl | 67 | 122 | 195 |
| Hemoglobin, g/dl | 12.1 | 12.9 | 11.0 |
| Platelet, /μl | 22.1 × 104 | 32.0 × 104 | 36.9 ×104 |
| HbA1c, % | 5.8 | 6.1 | 6.3 |
| Serum glucose, mg/dl | 108 | 98 | 102 |
| Total protein, g/dl | 6.9 | 7.3 | 7.6 |
| Serum albumin, g/dl | 4.0 | 4.1 | 4.4 |
| Blood urea nitrogen, mg/dl | 12.1 | 13.3 | 30.6 |
| Serum creatinine, mg/dl | 1.27 | 1.41 | 2.38 |
| eGFR, ml/min per 1.73 m2 | 32.2 | 31.5 | 17.6 |
| Uric acid, mg/dl | 1.6 | 1.2 | 3.5 |
| Serum sodium, mmol/l | 143 | 141 | 143 |
| Serum potassium, mmol/l | 3.2 | 3.4 | 4.2 |
| Serum chloride, mmol/l | 115 | 115 | 108 |
| Serum calcium, mg/dl | 9.1 | 9.2 | 9.8 |
| Serum phosphorus, mg/dl | 1.4 | 1.7 | 3.8 |
| C-reactive protein, mg/dl | 0.047 | 0.035 | 0.064 |
| ASO, IU/ml | 21 | 15 | 135 |
| Antinuclear antibody, U/ml | <40 | <40 | <40 |
| Anti-GBM antibody, U/ml | <2.0 | <2.0 | <2.0 |
| MPO-ANCA, U/ml | <1.0 | <1.0 | <1.0 |
| PR3-ANCA, U/ml | <1.0 | <1.0 | <1.0 |
| IgG, mg/dl | 991 | 1143 | 1168 |
| IgA, mg/dl | 159 | 133 | 219 |
| IgM, mg/dl | 60 | 151 | 122 |
| IgE, IU/ml | 196 | 62 | 4 |
| C3, mg/dl | 126 | 139 | 137 |
| C4, mg | 40 | 52 | 32 |
| Venous blood gas analysis | |||
| pH | 7.348 | 7.252 | 7.364 |
| PCO2, mm Hg | 28.7 | 37.0 | 40.3 |
| HCO3−, mmol/l | 15.4 | 15.7 | 22.4 |
| Base excess, mmol/l | −8.6 | −10.4 | −2.2 |
| Lactate, mmol/l | 0.8 | 0.6 | 0.6 |
| Urinalysis | |||
| pH | 6.0 | 5.5 | 6.0 |
| Urine specific gravity | 1.015 | 1.024 | 1.013 |
| Red blood cell, /HPF | 1–4 | 1–4 | 0–1 |
| White blood cell, /HPF | 1–4 | 1–4 | 1–4 |
| Tubular epithelial cell, /HPF | 5–9 | 0–1 | 0–1 |
| Hyaline cast, /HPF | 0–1 | 1–4 | 0–1 |
| Granule cast, /HPF | 1–4 | 1–4 | 0–1 |
| Urinary protein, g/g Cr | 2.47 | 4.25 | 0.65 |
| NAG, U/l | 27.0 | 30.4 | 19.4 |
| β2MG, μg/l | 52,201 | 8,373 | 19,833 |
| Creatinine, mg/dl | 67.3 | 59.8 | 91.3 |
ANCA, antineutrophil cytoplasmic antibody; ASO, antistreptolysin-O antibody; β2MG, β2-microglobulin; eGFR, estimated glomerular filtration rate; GBM, glomerular basement membrane; HbA1c, glycated hemoglobin; HPF, high power field; MPO, myeloperoxidase; NAG, N-acetyl-β-D-glucosaminidase; PR3, proteinase 3.
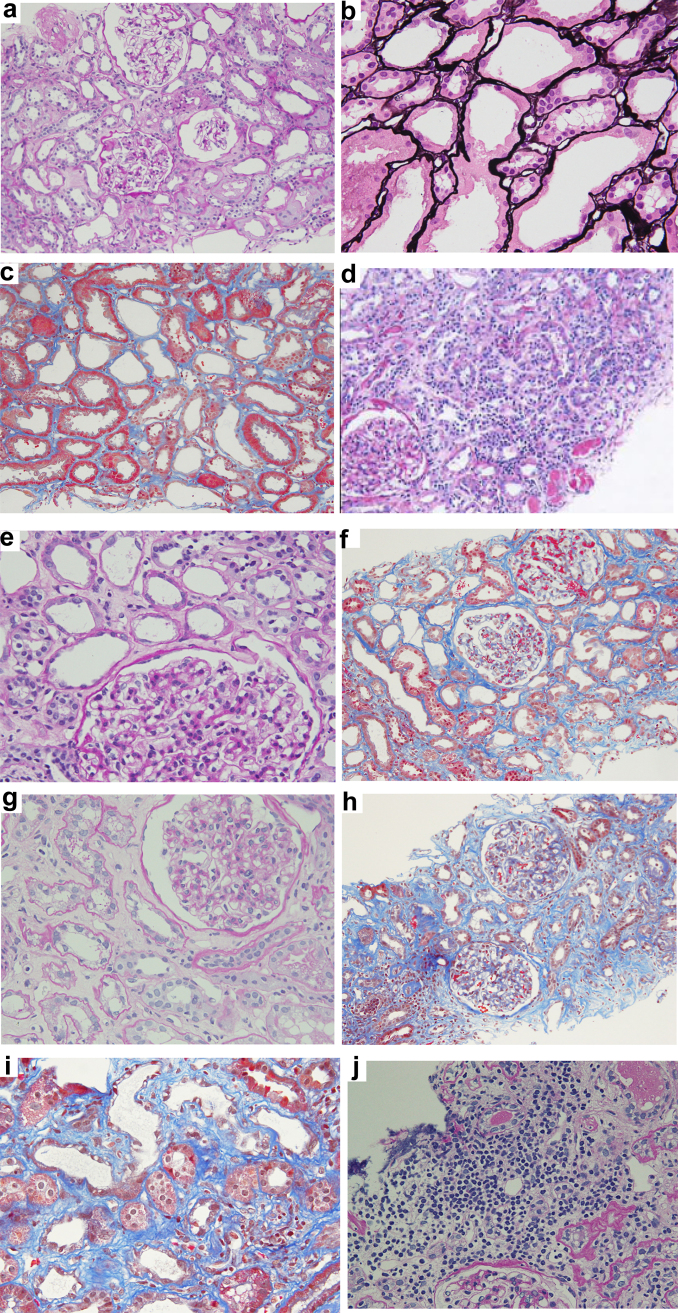
Figure 1.
In case 1, the photomicrographs of renal biopsy revealed flattened proximal tubular cells, loss of the brush border, and sloughing of proximal tubular cells; (a) periodic acid-Schiff staining, ×200; (b) periodic acid-methenamine-silver staining, ×400. (c) Masson trichrome staining revealed mild interstitial fibrosis, ×200. Photomicrographs of renal biopsy from case 2 (d) show several inflammatory cells in the tubulointerstitium. We observed fibrosis and atrophic proximal tubules, as indicated by periodic acid-Schiff staining, ×200. (e) There was no mesangial proliferation, stromal expansion, or thickening of basement membrane. There was a diffuse, mild expansion of mesangial matrix in the glomerulus, as indicated by periodic acid-Schiff staining, ×400. (f) Masson trichrome staining revealed the presence of interstitial fibrosis, ×200. In case 3, we observed shedding and regeneration of renal tubular epithelium in the photomicrographs of renal biopsy. (g) Periodic acid-Schiff, ×400. Masson trichrome staining revealed stromal expansion, fibrosis, and tubular atrophy (h) ×200, and (i) ×400. (j) Severe infiltration of inflammatory cells locally into the tubulointerstitium (Periodic acid-Schiff staining, ×400).
Case 2
A 53-year-old woman had been suffering from generalized fatigue since the end of December 2023. By January 2024, she had lost weight and noticed that her urine was foamy and cloudy. Therefore, she visited a nearby clinic on January 17, 2024. She underwent an annual health check, and there were no abnormalities other than dyslipidemia. She was admitted to our hospital due to elevated serum Cr levels and urinary problems. We observed hypokalemia, hypophosphatemia, hypouricemia, and metabolic acidosis, along with positive urine protein, urinary occult blood, and urine sugar (Table 1). Urinary β2-microglobulin and N-acetyl-β-D-glucosaminidase levels were also high. Her serum Cr level and estimated glomerular filtration rate were 1.41 mg/dl and 31.5 ml/min per 1.73 m2, respectively. AKI due to renal tubular injury accompanied by Fanconi syndrome was suspected. A kidney biopsy was performed on February 1, 2024 (Figure 1d, e, and f). Severe inflammatory cell infiltration was observed in the tubulointerstitial region. Therefore, she was treated with steroid pulse therapy and prednisolone and was discharged. She had been taking “red yeast rice” supplements since April 2023.
Case 3
A 55-year-old woman noticed general malaise, decreased appetite, weight loss, frequent urination, and foamy urine in mid-December 2023. By January 2024, the aforementioned symptoms had improved. When she had a regular medical checkup on January 31, 2024, she was found to have impaired kidney function. Therefore, she visited our hospital the next day. A health checkup did not reveal kidney dysfunction in her. However, because she was diagnosed with dyslipidemia, she had been taking “red yeast rice” supplements since April 2023. Urine protein, urinary occult blood, and urinary sugar were positive, whereas urinary β2-microglobulin and N-acetyl-β-D-glucosaminidase levels were high (Table 1). Although there were no electrolyte abnormalities, anemia was observed. Her serum Cr level and estimated glomerular filtration rate were 2.38 mg/dl and 17.6 ml/min per 1.73 m2, respectively. A kidney biopsy was performed on February 8, 2024 (Figure 1g, h, i, and j). A severe degree of inflammatory cell infiltration was observed in the tubulointerstitial region, and monocytes were predominant. Therefore, she was treated with steroid pulse therapy and prednisolone and was discharged. The lymphocyte transformation test was performed using the “red yeast rice” supplement that she regularly used, and the results were positive.
Discussion
ATIN is a drug-induced condition, attributable to a wide range of pharmaceuticals, such as antibiotics, nonsteroidal antiinflammatory drugs, and proton pump inhibitors, which are reported to induce ATIN in 70% to 80% of cases.3,4 Uniquely, the cases presented herein document the first instances of ATIN potentially linked to the consumption of red yeast rice supplements, a previously unreported association. Furthermore, these cases are directly linked to a specific product sold by a particular company, and the lot numbers were later identified. In addition, all the cases reported the patients not taking other medications. In all 3 cases, kidney function improved gradually after discontinuation of the supplement, but it had not fully recovered after 3 months of discontinuation. Therefore, all the cases were transferred to chronic kidney disease. This association raises the possibility of potential contamination by foreign substances during the production or quality control processes of this specific red yeast rice supplement. This consideration significantly amplifies the significance of the findings and underscores the urgent need for a targeted investigation. The specificity of the supplement in question draws attention to the potential health risks associated with red yeast rice supplements in general and highlights the critical importance of rigorous manufacturing standards to prevent the inclusion of harmful contaminants (Supplementary Discussion).
Not all strains of Monascus fungi are alike. M pilosus, M ruber, and M purpureus are predominantly used in food products across Japan, Taiwan, and China. Crucially, certain strains of M purpureus and M ruber have an active gene that produces citrinin, a mycotoxin known to cause renal toxicity.5 Citrinin’s nephrotoxicity varies across species but has been implicated in porcine nephropathy and can synergistically enhance the toxic effects of ochratoxin A.6 Notably, whole-genome analyses reveal that M pilosus does not produce citrinin, indicating that the choice of Monascus strain is critical to ensuring the safety of red yeast rice products.7 Consequently, whereas red yeast rice maintains a strong safety profile when properly prepared, attention to the specific Monascus strain used is paramount. Kobayashi Pharmaceutical Co. Ltd. has confirmed that their red yeast rice supplement, which has been recently discussed in Japan, does not contain citrinin, underscoring their commitment to safety.
On March 29, 2024, the Japan Ministry of Health, Labor, and Welfare made a critical announcement regarding the detection of puberulic acid in red yeast rice supplements.S3 In addition to puberulic acid, 2 other candidate compounds were detected; and it was reported on May 28, 2024 that puberulic acid alone was nephrotoxic.S3 Puberulic acid, a 7-membered ring organic compound (troponoid) with the molecular formula C8H6O6, is known for its bactericidal activity against Gram-positive bacteria and malaria, indicative of its potent bioactivity.8 Originating from the Penicillium species, this compound’s introduction into red yeast rice products raises concerns over the potential for unintended contamination. The discovery of puberulic acid underscores the critical importance of stringent hygiene and quality control measures in the manufacturing process. Contamination with blue mold, from which puberulic acid is derived, suggests possible lapses in the handling or storage of raw materials and in the sterilization of culture vessels. This situation highlights the broader issue of potential contamination of various bioactive substances during production. Red yeast rice naturally contains a diverse array of compounds, such as organic acids, amino acids, sterols, and polysaccharides.9 The inadvertent inclusion of Penicillium, and consequently puberulic acid, during manufacturing illustrates the complex challenges faced in ensuring the purity and safety of dietary supplements. The causative contaminant, including the other 2 compounds is currently being identified by the Japan Ministry of Health, Labor, and Welfare and the Japan National Institute of Health Sciences.
In conclusion, these cases presented mark the inaugural identification of ATIN possibly induced by red yeast rice supplements, a finding that underscores the need for vigilance in monitoring the safety of such products. Although the historical use and rigorous testing of red yeast rice suggest a generally low risk for kidney dysfunction, the detection of puberulic acid in these supplements introduces a new dimension to the potential health risks, implicating it as a contributory factor to the observed severe ATIN cases. Further research on how harmful puberulic acid and other possible contaminants in red yeast rice supplements are to the kidneys is needed.
Patient Consent
Written informed consent was obtained from each patient.
Disclosure
All the authors declared no competing interests.
Acknowledgments
We greatly appreciate Yutaka Yamaguchi’s assistance in histopathological diagnosis.
Data Availability Statement
The data supporting the findings of this study are openly available from the corresponding author. We did not use any underlying codes for data generation.
Author Contributions
MA and HK wrote the manuscript. YM, SH, YA, and KM contributed to data collection and kidney biopsy. MA, YM, SH, and TM discussed the results and contributed to the final manuscript. All the authors have read and approved the final version of the manuscript.
Data Sharing Statement
The data supporting the findings of this study are openly available from the corresponding author. We did not use any underlying codes for data generation.
Footnotes
Supplementary Methods.
Supplementary References.
Figure S1. Appearance of red yeast rice.
Figure S2. Tofuyo, a food that has been passed down through generations in Okinawa, Japan.
Supplementary Material
Supplementary Methods. Supplementary References. Figure S1. Appearance of red yeast rice. Figure S2. Tofuyo, a food that has been passed down through generations in Okinawa, Japan.
References
- 1.Endo A., Negishi Y., Iwashita T., Mizukawa K., Hirama M. Biosynthesis of ML-236B (compactin) and monacolin K. J Antibiot (Tokyo) 1985;38:444–448. doi: 10.7164/antibiotics.38.444. [DOI] [PubMed] [Google Scholar]
- 2.Fukami H., Higa Y., Hisano T., Asano K., Hirata T., Nishibe S. A review of red yeast rice, a traditional fermented food in Japan and East Asia: its characteristic ingredients and application in the maintenance and improvement of health in lipid metabolism and the circulatory system. Molecules. 2021;26:1619. doi: 10.3390/molecules26061619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Muriithi A.K., Leung N., Valeri A.M., et al. Biopsy-proven acute interstitial nephritis, 1993–2011: a case series. Am J Kidney Dis. 2014;64:558–566. doi: 10.1053/j.ajkd.2014.04.027. [DOI] [PubMed] [Google Scholar]
- 4.Praga M., González E. Acute interstitial nephritis. Kidney Int. 2010;77:956–961. doi: 10.1038/ki.2010.89. [DOI] [PubMed] [Google Scholar]
- 5.Xiong Z., Cao X., Wen Q., et al. An overview of the bioactivity of monacolin K / lovastatin. Food Chem Toxicol. 2019;131 doi: 10.1016/j.fct.2019.110585. [DOI] [PubMed] [Google Scholar]
- 6.Bennett J.W., Klich M. Mycotoxins. Clin Microbiol Rev. 2003;16:497–516. doi: 10.1128/CMR.16.3.497-516.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang M., Jiang N., Xian H., Wei D., Shi L., Feng X. Effects of light intensity and color on the biomass, extracellular red pigment, and citrinin production of Monascus ruber. J Chromatogr A. 2016;1429:22–29. doi: 10.1016/j.chroma.2015.12.004. [DOI] [PubMed] [Google Scholar]
- 8.Noguchi Y., Hirose T., Ishiyama A., et al. Synthesis and stereochemical determination of an antiparasitic pseudo-aminal type monoterpene indole alkaloid. J Nat Med. 2016;70:302–317. doi: 10.1007/s11418-016-1012-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhu B., Qi F., Wu J., et al. Red yeast rice: a systematic review of the traditional uses, chemistry, pharmacology, and quality control of an important Chinese folk medicine. Front Pharmacol. 2019;10:1449. doi: 10.3389/fphar.2019.01449. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Methods. Supplementary References. Figure S1. Appearance of red yeast rice. Figure S2. Tofuyo, a food that has been passed down through generations in Okinawa, Japan.
Data Availability Statement
The data supporting the findings of this study are openly available from the corresponding author. We did not use any underlying codes for data generation.