Abstract
Direct‐acting antivirals (DAAs) have revolutionized hepatitis C virus (HCV) treatment through their high cure rates and improved safety profiles. We aimed to evaluate the efficacy and safety, and identify the optimal combination, of DAAs for the treatment of chronic HCV. A retrospective study was conducted of 613 patients with chronic HCV who were treated with DAAs. Demographic, HCV genotype, treatment regimen, virological response, and adverse drug event (ADE) data were collected at the initial visit and 4, 8, 12, and 24 weeks later. The rapid virologic response (RVR) and sustained virologic response (SVR) rates were 90.4% and 97.8% for HCV genotype 1, 89.2% and 98.7% for genotype 6, 92.8% and 99% for genotype 2, and 90.9% and 100% for mixed genotype 2/6 or unspecified genotypes, respectively. There were no significant differences in the RVR and SVR rates for the various DAA regimens. The mean ALT, AST, and GGT activities decreased, and the PLT count increased during the treatments. ADEs occurred in 8% of the patients. The commonest ADEs were itching (3.1%), fatigue (1.8%), and dizziness (1.1%). None of the patients discontinued treatment because of an ADE. Posttreatment disease progression occurred in 7.7% of the patients, including liver fibrosis (3.6%), cirrhosis (1.1%), hepatocellular carcinoma (1.1%), and high alpha‐fetoprotein (AFP) (1%). The factors associated with the achievement of RVR were low viral load, the use of sofosbuvir/ledipasvir or sofosbuvir/daclatasvir regimens, and a treatment duration of 12 weeks. No specific factors were found to be associated with the achievement of SVR. Posttreatment disease progression was associated with a high AFP and the use of sofosbuvir/ledipasvir. Thus, DAAs are highly effective and well‐tolerated means of treating chronic HCV, and significantly improve patient outcomes. Their high efficacy and favorable safety profiles highlight the importance of early diagnosis and the use of personalized treatment strategies.
Keywords: chronic hepatitis C, direct‐acting antivirals, efficacy, safety
Virologic response rates to the various DAA regimens, by genotype. Panel (a) shows the virologic response for genotype 1; panel (b) for genotype 6; panel (c) for genotype 2; and panel (d) for mixed or unspecified genotypes. The colors represent different treatment regimens. SOF/LDV: sofosbuvir/ledipasvir; SOF/VEL: sofosbuvir/velpatasvir; SOF/DCV: sofosbuvir/daclatasvir, GZR/EBR: grazoprevir/elbasvir.
Abbreviations
- ADE
adverse drug event
- AFP
alpha‐fetoprotein
- ALT
Alanine aminotransferase
- AST
aspartate aminotransferase
- DAAs
direct‐acting antivirals
- GGT
Gamma Glutamyl Transferase
- HCC
hepatocellular carcinoma
- HCV
Hepatitis C virus
- IFN
interferon
- PLT
Platelet Count
- RBV
ribavirin
- RVR
Rapid Virologic Response
- SVR
Sustained Virologic Response
1. INTRODUCTION
Hepatitis C virus (HCV) infection remains a significant global health challenge, affecting approximately 71 million individuals worldwide, and causing severe liver disease, including cirrhosis and hepatocellular carcinoma (HCC). 1 HCV is the second leading cause of cirrhosis in Vietnam. 2 Direct‐acting antivirals (DAAs) have revolutionized the treatment of chronic HCV, offering high cure rates and favorable safety profiles, compared to previous interferon‐based therapies. The introduction of DAAs, such as sofosbuvir, ledipasvir, velpatasvir, and daclatasvir, has markedly improved patient outcomes, with sustained virologic responses (SVRs) being achieved in >95% of patients, irrespective of HCV genotype. 2 , 3 , 4
Despite the successful use of DAAs in many parts of the world, significant gaps remain in our understanding of their efficacy and safety in diverse patient populations, and particularly in low‐ and middle‐income countries, where hepatitis care is often not prioritized and poverty limits the involvement of patients and the public. 5 , 6
Furthermore, while the overall safety profile of DAAs is favorable, the incidence and management of adverse drug events (ADEs) in various demographic and clinical contexts require further investigation. In addition, despite the high prevalence of SVR, concerns remain regarding long‐term outcomes, such as the progression of liver disease and HCC. Patients with advanced liver disease face significant risks subsequent to virologic cure, which underscores the need for continued surveillance and improved management strategies. 5 , 7 , 8 Therefore, in the present study, we aimed to evaluate the efficacy and safety of DAAs for the treatment of chronic HCV in patients in a large center, and to provide insight into the use of DAAs in Vietnam.
2. MATERIALS AND METHODS
We performed a retrospective study of patients with chronic HCV who had been treated with DAAs at the Liver Clinic of the University Medical Center Ho Chi Minh City, Vietnam, between January 2019 and April 2021.
2.1. Study sample
2.1.1. Inclusion criteria
A confirmed diagnosis of chronic HCV infection, which required an HCV infection of ≥6 months‘ duration, with or without clinical symptoms and cirrhosis, and positive results for anti‐HCV and HCV RNA or anti‐HCV and HCVcAg antibodies. 9
Age ≥18 years, regardless of sex or ethnicity.
An initial prescription of DAAs, without interferon (IFN) or ribavirin (RBV).
Failure to achieve SVR or a lack of tolerance of previous IFN‐based regimens, with the subsequent prescription of DAAs without IFN.
Follow‐up data available 12 weeks following after the end of treatment.
2.1.2. Exclusion criteria
Pregnancy.
Discontinuations due to reasons other than ADEs were excluded.
Incomplete data.
2.1.3. Definitions of key variables
Rationality of DAA use for HCV treatment: a regimen was considered to be rational if it met all the criteria for indication, dose, contraindications, and treatment duration, according to the WHO (2018), 10 EASL (2020), 11 or the Vietnam Ministry of Health (2021) 9 guidelines.
Rapid virologic response (RVR): HCV RNA concentration below the detection threshold (≤ 15 IU/mL) after 4 weeks of treatment.
SVR: HCV RNA concentration below the detection threshold (≤ 15 IU/mL) 12 weeks after the end of treatment (SVR12).
ADEs: the recorded side effects during DAA treatment, including fatigue, insomnia, itching, dizziness, nausea, headache, diarrhea, and others.
Disease progression: posttreatment outcomes, including liver fibrosis, cirrhosis, HCC, and high alpha‐fetoprotein (AFP) concentration.
Relapse: HCV RNA undetectable during and/or at the end of treatment, but subsequently detectable following its discontinuation. 11
2.2. Study protocol
A retrospective cross‐sectional study was conducted using the outpatient medical records of patients diagnosed with chronic HCV at the Hepatology Clinic, University Medical Center Ho Chi Minh City, between January 2019 to April 2021. We used a structured data collection form to extract the patient demographics, HCV genotypes, treatment regimens, virologic responses, and ADEs from the electronic medical records. Data were recorded at the initial visit (T0), after 4 weeks of DAA treatment (T4), after 8 weeks (T8), at the end of treatment (T12), 12 weeks posttreatment (T24), and during subsequent follow‐up visits. Patient consent was obtained at the original appointment as part of the standard protocol for retrospective data use. The maximum length of posttreatment monitoring varied, with follow‐up lasting up to 2 years. Disease progression was defined based on changes in liver fibrosis, the occurrence of HCC, or increases in AFP levels. Baseline disease status, including the presence of liver fibrosis or HCC, was assessed to compare against posttreatment disease progression.
2.3. Statistical analysis
Descriptive statistics were used to summarize the characteristics of the patients, treatment regimens, virologic responses, and ADEs. The chi‐square test was used to compare the RVR and SVR rates of patients undergoing different treatment regimens. The Friedman test was used to compare the changes in biochemical indices (ALT, AST, GGT, and PLT) at various time points (T0, T4, T12, T24). Logistic regression analysis was used to identify factors associated with the achievement of RVR, ADEs, and disease progression following treatment. Statistical significance was accepted at p <.05, and the data were analyzed using SPSS version 20 (IBM, Inc., Armonk, NY, USA).
3. RESULTS
We analyzed the data for 613 patients who had been diagnosed with chronic HCV between January 2019 to April 2021.
3.1. Treatment patterns
Females accounted for a higher proportion than males, with a mean age of 57.45 ± 13.24 years. Fatty liver disease was the most common comorbidity, affecting 9.5% of patients. Sofosbuvir was the most commonly prescribed drug, administered to 99.3% of the patients. A sofosbuvir/ledipasvir regimen was most frequently used for patients with HCV genotypes 1 (65%) and 6 (59.3%). For patients with HCV genotype 2 and those coinfected with genotypes 2 and 6, or an unspecified genotype, sofosbuvir/velpatasvir was the most commonly prescribed regimen, with prevalences of 50.5% and 61.6%, respectively. The overall rationality rate for the DAA regimens was 84.7%, and the rationality for each regimen is shown in Table 1, reflecting compliance with treatment guidelines and personalized regimens.
TABLE 1.
Rationality of DAA use for HCV treatment.
| Regimen, No. of patients (%) | Criterion | Frequency | Percentage |
|---|---|---|---|
|
Sofosbuvir/ledipasvir (400/90 mg) N1 = 303 (49.4%) |
Indication | 296 | 97.7 |
| Dosage | 303 | 100 | |
| Contraindication | 302 | 99.7 | |
| Treatment duration | 248 | 81.8 | |
| Overall rationality | 241 | 79.5 | |
|
Sofosbuvir/velpatasvir (400/100 mg) N2 = 180 (29.4%) |
Indication | 180 | 100 |
| Dosage | 180 | 100 | |
| Contraindication | 178 | 98.9 | |
| Treatment duration | 172 | 95.6 | |
| Overall rationality | 170 | 94.4 | |
|
Sofosbuvir/daclatasvir (400/60 mg) N3 = 126 (20.5%) |
Indication | 126 | 100 |
| Dosage | 126 | 100 | |
| Contraindication | 124 | 98.4 | |
| Treatment duration | 107 | 84.9 | |
| Overall rationality | 106 | 84.1 | |
|
Grazoprevir/elbasvir (100/50 mg) N4 = 4 (0.7%) |
Indication | 4 | 100 |
| Dosage | 4 | 100 | |
| Contraindication | 4 | 100 | |
| Treatment duration | 2 | 50 | |
| Overall rationality | 2 | 50 | |
|
Overall N = 613 |
Indication | 606 | 98.9 |
| Dosage | 613 | 100 | |
| Contraindication | 608 | 99.2 | |
| Treatment duration | 529 | 86.3 | |
| Overall rationality | 519 | 84.7 |
3.2. Efficacy of DAA regimens in the patients
The prevalences of RVR and SVR were calculated for patients with the various HCV genotypes. As shown in Figure 1, for patients with HCV genotype 1, the prevalences of RVR and SVR were 90.4% and 97.8%, respectively. For patients with HCV genotype 6, the prevalences of RVR and SVR were 89.2% and 98.7%. For patients with HCV genotype 2, the prevalences of RVR and SVR were 92.8% and 99%, respectively. For those with the mixed genotype 2/6 or unspecified genotypes, the prevalences of RVR and SVR were 90.9% and 100%, respectively. There were no significant differences in the prevalences of RVR or SVR for the various DAA regimens. Biochemical indices showed significant improvements, with decreases in the ALT, AST, and GGT activities, and an increase in PLT count (p <.001) (data not shown).
FIGURE 1.
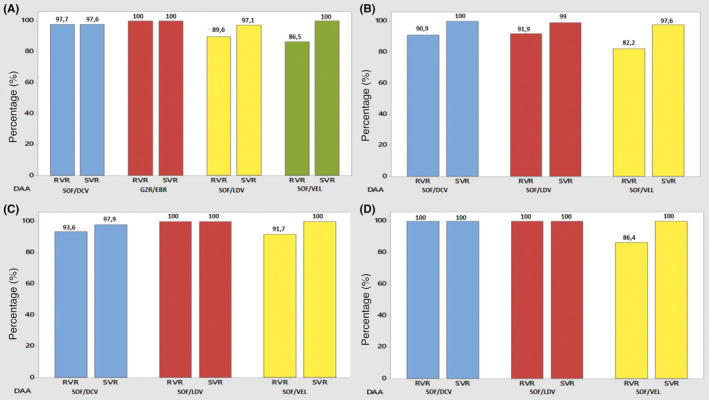
Virologic response rates to the various DAA regimens, by genotype. Panel (A) shows the virologic response for genotype 1; panel (B) for genotype 6; panel (C) for genotype 2; and panel (D) for mixed or unspecified genotypes. The colors represent different treatment regimens. SOF/LDV, Sofosbuvir/ledipasvir; SOF/VEL, Sofosbuvir/velpatasvir; SOF/DCV, Sofosbuvir/daclatasvir, GZR/EBR, Grazoprevir/elbasvir.
3.3. Safety profiles of DAAs
ADEs occurred in 8% of the patients, with the most common being itching (3.1%), fatigue (1.8%), dizziness (1.1%), and insomnia (1%). None of the patients discontinued their treatment because of ADEs. Posttreatment disease progression occurred in 7.7% of the patients, comprising liver fibrosis (3.6%), cirrhosis (1.1%), HCC (1.1%), and a high AFP (1%). The ADEs and posttreatment disease progression associated with each regimen are shown in Table 2.
TABLE 2.
Adverse drug events and disease progression following treatment.
| DAA Regimen No. of patients | No. with at least 1 ADE (%) | Adverse event | Frequency (%) | Disease progression | Frequency (%) |
|---|---|---|---|---|---|
|
Sofosbuvir/ledipasvir (400/90 mg) N = 303 |
31 (10.2) | Fatigue | 9 (3.0) | Progressive liver fibrosis | 3 (1.0) |
| Insomnia | 4 (1.3) | Liver fibrosis | 15 (5.0) | ||
| Itching | 13 (4.3) | Cirrhosis | 5 (1.7) | ||
| Dizziness | 4 (1.3) | Progressive cirrhosis | 2 (0.7) | ||
| Nausea | 2 (0.6) | HCC | 3 (1.0) | ||
| Headache | 1 (0.3) | Increased AFP | 5 (1.7) | ||
|
Diarrhea Other |
1 (0.3) 2 (0.6) |
||||
|
Sofosbuvir/velpatasvir (400/100 mg) N = 180 |
7 (3.9) | Fatigue | 1 (0.6) | Liver fibrosis | 3 (1.7) |
| Itching | 3 (1.7) | Cirrhosis | 2 (1.1) | ||
| Dizziness | 1 (0.6) | HCC | 2 (1.1) | ||
|
Headache Diarrhea |
1 (0.6) 1 (0.6) |
||||
|
Sofosbuvir/daclatasvir (400/60 mg) N = 126 |
11 (8.7) | Fatigue | 1 (0.8) | Progressive liver fibrosis | 2 (1.6) |
| Insomnia | 2 (1.6) | Liver fibrosis | 4 (3.2) | ||
| Itching | 3 (2.4) | Progressive cirrhosis | 1 (0.8) | ||
| Dizziness | 2 (1.6) | HCC | 2 (1.6) | ||
| Nausea | 2 (1.6) | High AFP | 1 (0.8) | ||
| Headache | 2 (1.6) | ||||
|
Grazoprevir/elbasvir (100/50 mg) N = 4 |
0 | 0 | 0 (0.0) | Relapse | 1 (25) |
|
Overall N = 613 |
49 (8) | Fatigue | 11 (1.8) | Progressive liver fibrosis | 5 (0.8) |
| Insomnia | 6 (1) | Liver fibrosis | 22 (3.6) | ||
| Itching | 19 (3.1) | Cirrhosis | 7 (1.1) | ||
| Dizziness | 7 (1.1) | Progressive cirrhosis | 3 (0.5) | ||
| Nausea | 4 (0.7) | HCC | 7 (1.1) | ||
| Headache | 4 (0.7) | High AFP | 6 (1) | ||
| Diarrhea | 2 (0.3) | Relapse | 1 (0.2) | ||
| Other | 2 (0.3) | ||||
Abbreviations: AFP, alpha‐fetoprotein; HCC, hepatocellular carcinoma.
3.4. Factors influencing treatment efficacy, the incidences of ADEs, and disease progression
The factors influencing treatment efficacy are summarized in Table 3, showing significant associations between low viral load, regimen type, and treatment duration with treatment outcomes. Several factors were found to influence treatment outcomes. The factors associated with achieving RVR were low viral load, the use of sofosbuvir/ledipasvir or sofosbuvir/daclatasvir, compared to sofosbuvir/velpatasvir, and a 12‐week duration of treatment, compared to 16 or 20 weeks. No factors were found to be associated with the achievement of SVR. Patients with new HCV infections were more likely to experience ADEs while using DAAs. Disease progression posttreatment was associated with a high AFP concentration and treatment with sofosbuvir/ledipasvir rather than sofosbuvir/velpatasvir.
TABLE 3.
Logistic regression analysis of factors influencing treatment efficacy.
| Variable | Odds Ratio (OR) | 95% Confidence Interval (CI) | p‐value |
|---|---|---|---|
| Low Viral Load | 2.3 | 1.5–3.2 | .002 |
| Sofosbuvir/Ledipasvir Regimen | 1.8 | 1.2–2.5 | .01 |
| 12‐Week Treatment Duration | 1.5 | 1.1–2.1 | .03 |
| High AFP Concentration | 2.7 | 1.9–3.8 | .001 |
| Sofosbuvir/Velpatasvir Regimen | 0.8 | 0.5–1.2 | .15 |
4. DISCUSSION
Although numerous global and local studies have demonstrated the efficacy and safety of DAA‐based regimens, recent research since 2020 has extensively explored the efficacy and safety of specific DAA regimens in patients with different genotypes. The results of the present study contribute to understanding the efficacy and safety of DAA regimens but should be interpreted alongside established WHO guidelines. In addition, we have identified factors related to the efficacy of treatment. A key aspect of the present study was that we monitored the patients who achieve SVR with each DAA regimen for ADEs, and identified factors associated with ADEs after SVR was achieved.
4.1. Treatment patterns
In the present study, the sofosbuvir/ledipasvir regimen was the most frequently prescribed (49.4%), reflecting the high prevalence of genotypes 1 and 6 (76.9%). The grazoprevir/elbasvir regimen was the least prescribed (0.6%), likely because it is indicated for genotypes 1 and 4, and there were no patients with genotype 4 in the present cohort, plus its high cost limits its use for patients with genotype 1. These findings are consistent with those of Thanh (2018), 12 who reported a high level of usage of sofosbuvir/ledipasvir (50%) and a low level of usage of grazoprevir/elbasvir (1.4%) in Vietnam.
For patients with genotype 2 HCV, those co‐infected with genotypes 2 and 6, and those infected with unspecified genotypes, sofosbuvir/velpatasvir was most commonly prescribed combination, with frequencies of 50.5% and 61.6%, respectively. Historically, there was no effective first‐generation DAA combination for genotype 2 HCV, but now, sofosbuvir/daclatasvir and sofosbuvir/velpatasvir administration are recommended. 13 Ahmed et al. 14 demonstrated that sofosbuvir/velpatasvir is highly effective for all genotypes, other than genotype 3. Therefore, it is widely used for patients with genotype 2 HCV, co‐infections, and those infected with unspecified genotypes.
4.2. Efficacy of DAA regimens in patients with chronic HCV
The prevalence of RVR associated with the various DAA regimens varies by genotype. For genotype 1, the overall prevalence of RVR across the four DAA regimens (sofosbuvir/ledipasvir, sofosbuvir/daclatasvir, sofosbuvir/velpatasvir, and grazoprevir/elbasvir) was 90.4%, with no significant differences between the regimens. Tsai et al. reported a 95.3% prevalence of RVR in 149 patients with genotype 1 HCV who were treated with grazoprevir/elbasvir, which is slightly lower than the 100% in the present study, possibly because of the small sample size. Sharafi et al. 15 recorded a prevalence of RVR of 86.7% in 30 patients with genotype 1 HCV who were being administered sofosbuvir/ledipasvir, which is similar to the 89.6% recorded in the present study. For genotype 6, the overall prevalence of RVR for the three DAA regimens (sofosbuvir/ledipasvir, sofosbuvir/daclatasvir, and sofosbuvir/velpatasvir) was 89.2%, again with no significant differences between the regimens. Bich et al. 16 reported prevalences of RVR of 99% for genotype 1 and 99.2% for genotype 6 following sofosbuvir/ledipasvir treatment, which were higher than the prevalences identified in the present study, likely because of the inclusion of difficult‐to‐treat patients (compensated and decompensated cirrhosis). For genotype 2, the overall prevalence of RVR for the three DAA regimens was 92.8%, with no significant differences between them. Finally, for patients co‐infected with genotypes 2 and 6 or infected with unspecified genotypes, the overall prevalence of RVR for the three DAA regimens was 90.9%. However, the administration of sofosbuvir/ledipasvir is not recommended, and because of the small number of patients treated using this combination, its effectiveness may not have been accurately quantified.
The prevalence of SVR associated with the various DAA regimens also varies by genotype. For genotype 1, the overall prevalence of SVR across the four DAA regimens (sofosbuvir/ledipasvir, sofosbuvir/daclatasvir, sofosbuvir/velpatasvir, and grazoprevir/elbasvir) was 97.8%, with no significant differences among the regimens. Lawitz et al. 17 reported a prevalence of SVR of 93.5% for 62 patients infected with genotype 1 HCV who were treated with grazoprevir/elbasvir, which was lower than the 100% prevalence obtained in the present study, probably because of the small sample size. Chuang et al. 18 reported a prevalence of SVR of 97.6% for 85 patients with genotype 1 who were treated with sofosbuvir/ledipasvir, which is similar to the 97.1% obtained in the present study. For genotype 6, the overall prevalence of SVR for the three DAA regimens (sofosbuvir/ledipasvir, sofosbuvir/daclatasvir, and sofosbuvir/velpatasvir) was 98.7%, with no significant differences between the regimens. Bich et al. 16 reported prevalence of SVR of 99.5% for genotype 1 and 100% for genotype 6 when patients were administered sofosbuvir/ledipasvir, which is consistent with the 99% prevalence for genotype 6 obtained in the present study. For genotype 2, the overall prevalence of SVR obtained for the three DAA regimens was 99%, with no significant differences. For patients co‐infected with genotypes 2 and 6 or infected with unspecified genotypes, the overall prevalence of SVR for the three DAA regimens was 90.9%. However, the use of sofosbuvir/ledipasvir is not recommended, and the data obtained for the small number of patients may not accurately reflect its effectiveness. Tsai et al. 19 reported a prevalence of SVR of 95.7% for the use of sofosbuvir/daclatasvir in 47 patients with genotype 2 HCV, which was similar to the 97.9% prevalence obtained in the present study. Buggisch et al. 20 recorded an overall prevalence of SVR of 99% for 115 patients treated with sofosbuvir/velpatasvir, regardless of the HCV genotype, and 96% for 249 patients treated with sofosbuvir/ledipasvir. Finally, Charatcharoenwitthaya et al. 13 reported SVR prevalences of 97.9%, 96.5%, and 98.0% for sofosbuvir/ledipasvir, sofosbuvir/daclatasvir, and sofosbuvir/velpatasvir, respectively, with no significant differences between the regimens. The prevalences of SVR by genotype were 99.2% for genotype 1, 100% for genotype 2, and 96.7% for genotype 6. Thus, the present results are similar to those obtained in both domestic and international studies, with prevalences of SVR typically >95%. This high efficacy across HCV genotype underscores the efficacy of DAAs in diverse patient populations.
The significant improvements in circulating liver enzyme activities and platelet counts identified in the present study further validate the effectiveness of DAA with respect to an amelioration of liver damage. Abozeid et al. found that the AST and ALT activities of 971 patients had significantly decreased after 4 weeks of treatment and continued to decrease until the end of the treatment period, although their PLT counts did not increase. In contrast, Chen et al. reported statistically significant increases in platelet counts at all the time points assessed: baseline, after 4 weeks of treatment, at the end of treatment, and 12 weeks posttreatment. Thus, the present findings are consistent with the results of previous domestic and international studies.
4.3. Safety profile of DAAs
The ADEs experienced during DAA treatment varied by regimen. For sofosbuvir/ledipasvir, 10.2% of patients experienced ADEs, including itching (4.3%), fatigue (3%), insomnia and dizziness (1.3% each), nausea (0.6%), headache, and diarrhea (0.3% each). Bich et al. 16 found that fatigue (5.1%), loss of appetite (3.8%), and nausea (2.2%) were the commonest ADEs associated with this regimen. For sofosbuvir/daclatasvir, 8.7% of patients experienced ADEs, with itching (2.4%), fatigue (0.8%), insomnia, nausea, dizziness, and headache (1.6% each) being the commonest. Nelson et al. 21 reported that headache (19.7%), fatigue (19.1%), and nausea (11.8%) were the most frequent ADEs associated with this regimen. For sofosbuvir/velpatasvir, 3.9% of patients experienced ADEs, including itching (1.7%), fatigue, dizziness, headache, and diarrhea (1% each). Charatcharoenwitthaya et al. 13 reported that fatigue (11%), insomnia (2.7%), headache (2.5%), diarrhea (1.8%), itching (1%), and joint pain (0.7%) were common ADEs. There were no cases of treatment discontinuation due to ADEs.
Disease progression posttreatment was observed across different DAA regimens. However, this study did not find a statistically significant difference in the risk of disease progression between regimens. It's important to note that pretreatment disease status was not fully assessed, which may affect the interpretation of these findings. For sofosbuvir/daclatasvir, 7.1% showed disease progression, indicated by a high AFP (0.8%) and HCC (1.6%). Kanda et al. 5 reported that in patients without a history of HCC, the occurrence rate was 1.3%, which aligns with our findings. However, in patients with a history of HCC, the rate was significantly higher. This distinction underscores the importance of considering disease history when evaluating treatment outcomes. Rapid changes in the immune system and the “environmental shift” in the liver that is caused by DAAs may promote the development of tumors from preexisting “hidden” or “dysplastic” cancer cells. 5
Studies by Conti et al. 22 and Nakao et al. 23 yielded prevalences of HCC of 3.2% and 1.7%–7% post‐DAA treatment, respectively. In addition, Cardoso et al. 24 , 25 reported a prevalence of HCC of 7.4% 1 year post‐SVR, which was higher than that identified previously for patients who underwent IFN‐based treatment (1.2%–1.4%). Furthermore, Akuta et al. 8 noted a prevalence of HCC of 2.2% in patients who achieved SVR, with diagnoses being made on average 1 year posttreatment, and prevalences of HCC of 1.2%, 2.0%, and 3.1% after 1, 2, and 3 years, respectively. In the present study, the prevalence of HCC 12 weeks following treatment was 1.1%, which is lower than those recorded in other studies, possibly because of variation in the duration of follow‐up.
Among the four patients treated with grazoprevir/elbasvir, one patient (25%) experienced HCV reinfection, but none had a high AFP or developed HCC. This observation does not imply a causal relationship between the regimen and the reinfection. However, the small number of patients treated using this regimen may mean that this is not an accurate reflection of its effectiveness. HCV reinfection is rare in general, but more common in high‐risk groups, such as prisoners, intravenous drug abusers, and those co‐infected with HIV. 26
These findings underscore the importance of continued monitoring, even after SVR is achieved. Previous studies have shown that while DAAs are effective means of achieving virologic cure, they do not entirely eliminate the risk of HCC, particularly in patients with advanced liver disease at baseline. Therefore, sustained posttreatment surveillance is essential for the early detection and management of potential complications.
4.4. Factors influencing treatment efficacy, the incidence of ADEs, and disease progression
We identified three factors that influence whether or not RVR is achieved: pretreatment viral load, the DAA regimen used, and the duration of treatment. The prevalence of RVR decreased as the pretreatment viral load increased, which is consistent with the findings of Colussi et al., 7 who reported a significant correlation between viral load and treatment efficacy (p =.03). The prevalence of RVR was higher for patients on sofosbuvir/ledipasvir or sofosbuvir/daclatasvir than for those on sofosbuvir/velpatasvir. Furthermore, those taking sofosbuvir/velpatasvir often had comorbidities and were taking concurrent medications, which may have reduced the efficacy of the DAA regimen, owing to drug interactions. In addition, patients who underwent treatment for 12 weeks had higher prevalences of RVR than those who underwent treatment for 16 or 20 weeks, possibly because those who were treated for longer had advanced fibrosis or cirrhosis.
No factors were found to be significantly associated with SVR in the present study. Similarly, Thanh et al. 12 reported no significant correlations between the prevalence of SVR12 and patient characteristics, or between the prevalence of RVR and the DAA regimen used. However, Buti et al. 27 found evidence that treatment failure is linked to host factors, viral resistance mutations, and non‐compliance with medication. Choudhary et al. 28 reported that advanced fibrosis is associated with a low prevalence of SVR, especially in patients with severe fibrosis. In the present study, the stage of fibrosis did not affect the prevalence of SVR, likely because patients with advanced fibrosis or cirrhosis underwent long periods of treatment.
We found that the duration of HCV infection was the only factor associated with ADEs: the prevalence of ADEs decreased as the duration of HCV infection increased. However, this relationship may have been influenced by the timing of the initial diagnosis, because patients might have been infected some time earlier. Approximately 20% of HCV‐infected individuals experience early symptoms, such as fatigue, itching, bloating, and digestive disorders, which can contribute to ADEs in recently infected patients. 29
Two factors were found to be linked to posttreatment disease progression: the AFP concentrations 12 weeks after the end of treatment and the sofosbuvir/ledipasvir regimen. High AFP concentrations were associated with a higher prevalence of disease progression. Akuta et al. 8 identified AFP concentration and fibrosis stage as risk factors for HCC in patients who had achieved SVR, but Guarino et al. 30 identified additional risk factors for HCC post‐DAA treatment, including treatment failure, alcohol use, age >65 years, male sex, cirrhosis, genotype 3 HCV, diabetes, metabolic syndrome, HIV co‐infection, severe liver disease, low albumin concentration, low PLT count, and high AFP concentration. An increase in AFP may therefore be a significant factor in the development of HCC. The prevalence of disease progression was higher in patients taking sofosbuvir/ledipasvir than in those taking sofosbuvir/velpatasvir, potentially because of the longer follow‐up period for the former group, given that it began to be administered in 2019, providing sufficient time to detect posttreatment disease progression. The present findings are consistent with those of Sulkowski et al., who demonstrated that certain DAA combinations, especially those including sofosbuvir, are highly effective at inducing rapid and SVRs. Conversely, factors such as a high AFP concentration are associated with disease progression posttreatment, highlighting the need for ongoing surveillance.
In conclusion, the present findings from a Vietnamese cohort provide further evidence regarding the efficacy and safety of DAAs. The high efficacy and favorable safety profiles identified highlight the importance of early diagnosis and personalized treatment strategies for this disease. Furthermore, ongoing surveillance and management post‐SVR, especially for patients with advanced liver disease, are essential to mitigate the risk of disease progression and ensure long‐term health.
AUTHOR CONTRIBUTIONS
TDV, VTTB and QTHB contributed to the study conception, design, data collection, analysis, and manuscript writing. HLT revised manuscript. TDV supervised the study and critically revised the manuscript. All authors reviewed and approved the final version of the manuscript.
FUNDING INFORMATION
This study was not supported by any sponsor or funder.
CONFLICT OF INTEREST STATEMENT
The authors declare that the research was conducted in the absence of any commercial or financial relationship that could be construed as a potential conflict of interest.
CONSENT
Patient consent was obtained.
ETHICS STATEMENT
The study was conducted in accordance with the Declaration of Helsinki and approved by the Biomedical Research Ethics Committee of the University of Medicine and Pharmacy, Ho Chi Minh City (Approval No. 678/HDDD‐DHYD).
ACKNOWLEDGMENTS
We extend our sincere appreciation to the Faculty of Medicine, University of Medicine and Pharmacy at Chi Minh City, Vietnam. We also acknowledge the cooperation and support of the staff and patients at the Liver Clinic, University Medical Center Ho Chi Minh City throughout this study.
Vo TD, Bui VTT, Lam HT, Bui QTH. High efficacy and safety of direct‐acting antivirals for the treatment of chronic hepatitis C: A cohort study conducted in Vietnam. Pharmacol Res Perspect. 2024;12:e70007. doi: 10.1002/prp2.70007
DATA AVAILABILITY STATEMENT
The data and code supporting the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Thong VD, Akkarathamrongsin S, Poovorawan K, Tangkijvanich P, Poovorawan Y. Hepatitis C virus genotype 6: virology, epidemiology, genetic variation and clinical implication. World J Gastroenterol. 2014;20(11):2927‐2940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Thong VD, Anh HTV. Prediction of esophageal varices based on serum‐ascites albumin gradient in cirrhotic patients. Gastroenterology Insights. 2021;12(2):270‐277. [Google Scholar]
- 3. Due OT et al. Systematic review with meta‐analysis: efficacy and safety of direct‐acting antivirals for chronic hepatitis C genotypes 5 and 6. Biomed Res Int. 2019;2019:2301291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Abdelaty LN, Elnaggar AA, Said AA, Hussein RRS. Ledipasvir/Sofosbuvir versus Daclatasvir/Sofosbuvir for the treatment of chronic hepatitis C genotype 4 patients. Curr Drug Saf. 2020;15(1):53‐60. [DOI] [PubMed] [Google Scholar]
- 5. Kanda T, Lau GKK, Wei L, et al. APASL HCV guidelines of virus‐eradicated patients by DAA on how to monitor HCC occurrence and HBV reactivation. Hepatol Int. 2019;13(6):649‐661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lazarus, J.V. , Roel E., and Elsharkawy A.M., Hepatitis C Virus Epidemiology and the Impact of Interferon‐Free Hepatitis C Virus Therapy. Cold Spring Harb Perspect Med, 2020. 10(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Colussi G, Donnini D, Brizzi RF, et al. Sustained virologic response to direct‐acting antiviral agents predicts better outcomes in hepatitis C virus‐infected patients: a retrospective study. World J Gastroenterol. 2019;25(40):6094‐6106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Akuta N, Suzuki F, Sezaki H, et al. Complex Association of Virus‐ and Host‐Related Factors with hepatocellular carcinoma rate following hepatitis C virus clearance. J Clin Microbiol. 2019;57(1):e01463‐18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Health, V.M.o . Thong tu so 2065/QD‐BYT ban hanh ngay 29/04/2021 ve Huong dan chan doan va dieu tri benh gan vi rut C. 2021: Ha Noi, VietNam.
- 10. Organization, W.H ., Guidelines for the Care and Treatment of Persons Diagnosed with Chronic Hepatitis C Virus Infection. Geneva: World Health Organization; 2018. [PubMed] [Google Scholar]
- 11. Pawlotsky J‐M et al. EASL Recommendations on Treatment of Hepatitis C: Final Update of the Series. 2020;73(5):1170‐1218. [DOI] [PubMed] [Google Scholar]
- 12. Thanh NTL. Evaluate the Use of Direct‐Acting Antivirals in Treatment and the Quality of Life of Hepatitis C Patients at the Hospital for Tropical Diseases. University of Medicine and Pharmacy at Ho Chi Minh city; 2018. [Google Scholar]
- 13. Charatcharoenwitthaya P et al. Real‐world effectiveness and safety of sofosbuvir and nonstructural protein 5A inhibitors for chronic hepatitis C genotype 1, 2, 3, 4, or 6: a multicentre cohort study. BMC Gastroenterol. 2020;20(1):47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ahmed H, Abushouk AI, Attia A, et al. Safety and efficacy of sofosbuvir plus velpatasvir with or without ribavirin for chronic hepatitis C virus infection: a systematic review and meta‐analysis. J Infect Public Health. 2018;11(2):156‐164. [DOI] [PubMed] [Google Scholar]
- 15. Sharafi H, Alavian SH, Behnava B, Saeid Rezaee‐Zavareh M, Nikbin M, Alavian SM. Real‐life efficacy of generic sofosbuvir/ledipasvir for treatment of Iranian patients with chronic hepatitis C: a cohort study. Caspian J Intern Med. 2020;11(1):41‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bich NTN. Efficacy and Safety of Sofosbuvir and Ledipasvir in Treating Chronic Hepatitis C Patients with Genotype 1 or 6 at the Ho Chi Minh City University Medical Center. University of Medicine and Pharmacy at Ho Chi Minh city; 2020. [Google Scholar]
- 17. Sulkowski M, Hezode C, Gerstoft J, et al. Efficacy and safety of 8 weeks versus 12 weeks of treatment with grazoprevir (MK‐5172) and elbasvir (MK‐8742) with or without ribavirin in patients with hepatitis C virus genotype 1 mono‐infection and HIV/hepatitis C virus co‐infection (C‐WORTHY): a randomised, open‐label phase 2 trial. Lancet. 2015;385(9973):1087‐1097. [DOI] [PubMed] [Google Scholar]
- 18. Chuang WL, Chien RN, Peng CY, et al. Ledipasvir/sofosbuvir fixed‐dose combination tablet in Taiwanese patients with chronic genotype 1 hepatitis C virus. J Gastroenterol Hepatol. 2016;31(7):1323‐1329. [DOI] [PubMed] [Google Scholar]
- 19. Tsai WL, Wang CF, Cheng JS, Chen WC, Bair MJ, Lo CC. Sofosbuvir‐based regimen for genotype 2 HCV infected patients in Taiwan: a real world experience. PLoS One. 2020;15(1):e0227424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Buggisch P, Wursthorn K, Stoehr A, et al. Real‐world effectiveness and safety of sofosbuvir/velpatasvir and ledipasvir/sofosbuvir hepatitis C treatment in a single centre in Germany. PLoS One. 2019;14(4):e0214795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nelson DR, Cooper JN, Lalezari JP, et al. All‐oral 12‐week treatment with daclatasvir plus sofosbuvir in patients with hepatitis C virus genotype 3 infection: ALLY‐3 phase III study. Hepatology. 2015;61(4):1127‐1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Conti F, Buonfiglioli F, Scuteri A, et al. Early occurrence and recurrence of hepatocellular carcinoma in HCV‐related cirrhosis treated with direct‐acting antivirals. J Hepatol. 2016;65(4):727‐733. [DOI] [PubMed] [Google Scholar]
- 23. Nakao Y, Hashimoto S, Abiru S, et al. Rapidly growing, moderately differentiated HCC: a clinicopathological characteristic of HCC occurrence after IFN‐free DAA therapy? J Hepatol. 2018;68(4):854‐855. [DOI] [PubMed] [Google Scholar]
- 24. Cardoso AC, Moucari R, Figueiredo‐Mendes C, et al. Impact of peginterferon and ribavirin therapy on hepatocellular carcinoma: incidence and survival in hepatitis C patients with advanced fibrosis. J Hepatol. 2010;52(5):652‐657. [DOI] [PubMed] [Google Scholar]
- 25. Cardoso H, Vale AM, Rodrigues S, et al. High incidence of hepatocellular carcinoma following successful interferon‐free antiviral therapy for hepatitis C associated cirrhosis. J Hepatol. 2016;65(5):1070‐1071. [DOI] [PubMed] [Google Scholar]
- 26. Huang CF, Yu ML. Unmet needs of chronic hepatitis C in the era of direct‐acting antiviral therapy. Clin Mol Hepatol. 2020;26(3):251‐260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Buti M, Esteban R. Management of direct antiviral agent failures. Clin Mol Hepatol. 2016;22(4):432‐438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Choudhary NS, Saigal S, Gautam D, et al. Efficacy and safety of Sofosbuvir based regimens for treatment of hepatitis C recurrence after living donor liver transplantation: an experience from India. J Clin Exp Hepatol. 2018;8(2):121‐124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zoratti, M. and W.H. Organization , Guidelines for the Care and Treatment of Persons Diagnosed with Chronic Hepatitis C Virus Infection: Web Annex 3.1: Adult Hepatitis C Virus Treatment Systematic Review. World Health Organization. 2018. [PubMed] [Google Scholar]
- 30. Guarino M, Sessa A, Cossiga V, et al. Direct‐acting antivirals and hepatocellular carcinoma in chronic hepatitis C: a few lights and many shadows. World J Gastroenterol. 2018;24(24):2582‐2595. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data and code supporting the findings of this study are available from the corresponding author upon reasonable request.


