Version Changes
Revised. Amendments from Version 2
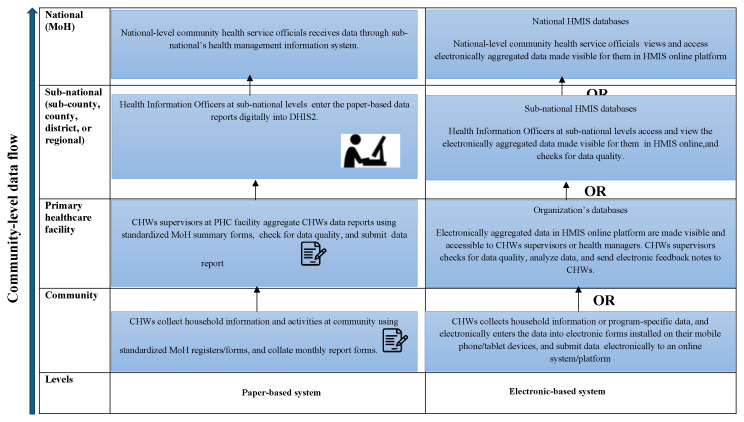
The revised manuscript addresses the reviewer’s concerns through several modifications. The title has been amended to reflect the review’s primary focus areas more accurately, ensuring alignment with the problem statement and aim. A new Figure (Figure 1) has been incorporated to provide a visual representation of CBHIS data flow across all levels of the health system. The results section has undergone refinement, with expanded discussions on the utilisation of CBHIS data and community empowerment. Various statements in these themes have been revised to enhance clarity. Finally, the conclusion has been revised to highlight the review's key findings, providing a more focused and comprehensive summary of the review.
Abstract
Introduction
The community-based health information system (CBHIS) is a vital component of the community health system, as it assesses community-level healthcare service delivery and generates data for community health programme planning, monitoring, and evaluation. CBHIS promotes data-driven decision-making, by identifying priority interventions and programs, guiding resource allocation, and contributing to evidence-based policy development.
Objective
This scoping review aims to comprehensively examine the use of CBHIS in African countries, focusing on data generation, pathways, utilisation of CBHIS data, community accessibility to the data and use of the data to empower communities.
Methods
We utilised Arksey and O'Malley's scoping review methodology. We searched eight databases: PubMed, EMBASE, HINARI, Cochrane Library, Web of Science, Scopus, Google Scholar, and grey literature databases (Open Grey and OAIster). We synthesised findings using a thematic approach.
Results
Our review included 55 articles from 27 African countries, primarily in Eastern and Southern Africa, followed by West Africa. Most of the studies were either quantitative (42%) or qualitative (33%). Paper-based systems are primarily used for data collection in most countries, but some have adopted electronic/mobile-based systems or both. The data flow for CBHIS varies by country and the tools used for data collection. CBHIS data informs policies, resource allocation, staffing, community health dialogues, and commodity supplies for community health programmes. Community dialogue is the most common approach for community engagement, empowerment, and sharing of CBHIS data with communities. Community empowerment tends towards health promotion activities and health provider-led approaches.
Conclusion
CBHIS utilises both paper-based and electronic-based systems to collect and process data. Nevertheless, most countries rely on paper-based systems. Most of the CBHIS investments have focused on digitisation and enhancing data collection, process, and quality. However, there is a need to shift the emphasis towards enabling data utilisation at the community level and community empowerment.
Keywords: Community-based health information systems (CBHIS), Community health systems (CHS), Health systems, Data utilisation, data-driven decision-making, Community accessibility, Community empowerment, Africa
Introduction
Community Health Systems (CHS), defined as the interface between community systems and the formal health system, is the most accessible, equitable, cost-effective, and efficient approach to improving access and coverage of health services in a continuum of the primary health care (PHC) system 1 . A strong CHS is critical for delivering accessible, quality, cost-effective preventive and treatment services, including emergency care 2 .
The Astana Declaration on PHC in 2018 fostered a renewed global interest in strengthening CHS in the context of the Universal Health Coverage (UHC) and other Sustainable Development Goals (SDGs). Integrating community health approaches in health systems is now considered paramount 3 , as CHS can help monitor population-level health system performance, track key indicators related to UHC and other health-related SDGs, and enhance the quality of health information 4 . The success of the CHS in handling global crises, such as the Ebola epidemic in West Africa and the COVID-19 pandemic, further emphasises its importance in providing essential health services at the community level and supporting public health emergency preparedness and response 2 . CHS is thus seen as a crucial aspect of PHC, and its strengthening is essential for achieving UHC and other health-related SDGs 5 .
A community-based health information system (CBHIS) is a vital system that encompasses information about the collection and flow of data, assessment and enhancement of data quality, and utilisation of community health data. It is essential for ensuring accurate data collection to support governance and management of CHS and decision-making at local, sub-national, and national levels 4, 6, 7 . CBHIS data also enable advocacy for vulnerable populations 6 , serve as an early warning alert and response (EWAR) tool, support case management and community health units/posts, enable health trend analyses, and reinforce the communication of health challenges to diverse groups 8 .
The four fundamental functions of CBHISs are data generation, data compilation, analysis and synthesis, and communication and use 8 . CBHISs gather health and other relevant data, ensure its quality, relevance, and timeliness, and transform it into useful information for health-related decision-making. However, the CBHIS requires critical health system inputs, including human resources (community health workers), budgetary allocation, and day-to-day operational management, to function efficiently 4, 5, 8, 9 . Many low- and middle-income countries (LMICs) face challenges in establishing and maintaining CBHIS due to insufficient government funding 4 , leading to significant gaps in community-level health data quality 5, 6, 10 , and thus limiting the demand and utilisation of CBHIS in decision-making processes 11 . This underutilisation of CBHIS data in decision-making processes can be attributed to fragmented community-based reporting systems 10 , lack of coordination between data producers and users 12, 13 , multiple parallel information subsystems 13 , and variations in the decentralisation of community health decisions 14 . Furthermore, limited integration of CBHIS with the formal Health Management Information System (HMIS), insufficient funding for the CHS 2, 4, 6, 15 , and contextual factors beyond technical aspects of data processes and organisational aspects impact the use of evidence in the CHS 13, 14 .
Although several African countries have embraced digital platforms, most countries (71 %) continue to rely on paper-based systems to collect CBHIS data 1, 2 . Several infrastructural constraints, including limited access to cell phones, stable electrical power supplies, and mobile networks, impede the adoption of digital systems 10, 13, 16– 18 . However, some countries, such as Malawi, Zambia, Ghana, and Kenya, have successfully adopted simple feature phones with simple SMS-based reporting systems, enabling real-time data transmission to all healthcare systems 4, 19 .
Several African countries have recently invested in enhancing their CHS and strengthening their CBHIS systems 20 . These efforts have included the digitisation of existing CBHIS systems to improve community health programs and work towards providing universal access to PHC services 21 . However, most CBHIS systems in these countries are partner-driven, program-specific, and heavily reliant on donors' and partners’ financial and technical support, as evidenced in the Democratic Republic of Congo (DRC), Egypt, Namibia, and Kenya 1, 10, 17 . As a result, the landscape of CBHIS data is disjointed and fragmented, failing to integrate with the national HMIS 10 .
There are limited reviews on CBHIS in Africa. A review by Mekonnen et al. 4 examined the current status and implementation challenges of CBHIS in LMICs-Africa but did not focus on CBHIS data processes, utilisation of CBHIS data on health system decision-making, or community access to CBHIS data and community empowerment. Our review focuses on these aspects of the CBHIS. We aim to address the gap in these aspects and inform efforts to enhance the CHS, ultimately contributing to improved community health service coverage and tracking progress towards UHC and other health-related SDGs. To comprehensively understand CBHIS functionality and its potential impact on community health outcomes, we systematically examined four key aspects: data generation processes, data flow pathways, CBHIS data utilisation, and community access and utilisation of this data for empowerment.
Methods
This scoping review adopted the Arksey and O'Malley’s Framework 22 to comprehensively examine the development, implementation, and utilisation of CBHIS in Africa. This framework guided the methodological processes for our review. We adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) reporting guidelines 23 . Our review was registered in the Open Science Framework 24 .
Eligibility criteria
We selected eligible studies using the Population, Concept, and Context (PCC) framework recommended for scoping reviews.
Population: We included primary studies of any study design that examined the CBHIS data sources, processes, pathways, utilisation, and accessibility of data at the community level, involving community members, community health workers, local actors, and other stakeholders such as policymakers, community-based organisations, and health non-governmental organisations.
Concept: We included studies that explored and discussed various aspects of CBHIS, encompassing experiences in CBHIS development and utilisation, sources of CBHIS data, data generation processes, CBHIS data pathways, utilisation of CBHIS data in informing evidence-based decision-making, community accessibility of the CBHIS data and empowerment.
Context/setting: We included studies conducted in Africa.
We excluded studies on CBHIS conducted in high-income countries, studies published in languages other than English, reviews (systematic, scoping, literature, etc.), conference abstracts, opinions, and editorials on CBHIS.
Information sources and search
We developed the search strategy in consultation with a health research librarian. An initial search was conducted in July 2023, and an updated search in November 2023. Seven databases were searched: PubMed, Embase, HINARI, Cochrane Library, Web of Science, Scopus, and Google Scholar. We also searched grey literature on open grey databases and hand-searched the references of included studies to identify additional literature. We limited our search to articles published in English between 2000 and 2023. The PubMed search strategy is presented in Additional File 1 (see Extended data 25 ,).
Study selection
We exported references to the EndNoteX7 database, and duplicates were removed. Two independent reviewers performed study selection over two stages: title and abstract review and full-text review against the predefined eligible criteria, using Covidence. All disagreements were resolved by discussion or consulting with authorship team members for a consensus. Studies that met the inclusion criteria were selected for data extraction and charting.
Data items and charting
A data extraction and charting form was developed and pilot-tested jointly with the research team to determine which variables to extract (Additional File 2) (see Extended data 25 ,). We extracted data on the following aspects: 1) general study characteristics; 2) sources of CBHIS data; 3) data generation; 4) pathways through which data were processed; 5) utilisation of CBHIS data; and 6) community accessibility to CBHIS data and empowerment. Data were extracted and exported from Covidence into Microsoft Excel software. One reviewer extracted data, and reviewers independently conducted quality checks of the extracted data. We resolved discrepancies by discussion between authors or consulting senior reviewers for a consensus.
Synthesis of results
We synthesised the findings using a thematic approach commonly used in scoping reviews. We followed the PRISMA-ScR reporting guideline to present our findings.
Results
Selection of sources of evidence
Our search strategy yielded 7,101 records, of which 362 duplicates were excluded. We screened 6,762 titles and abstracts and excluded 6,498 articles. We screened 264 articles and included 55 articles in this review. The PRISMA flow diagram of the selection process and summary of the search results is provided in Extended data 25 .
Characteristics of sources of evidence
We synthesised 55 studies from 27 African countries, primarily Eastern and Southern Africa, followed by the Western African region. Although the literature review considered publications from all African countries, Northern Africa was represented by only a single article from Egypt. Of these, 52 were research studies, and only three were project/programme reports. Most studies were quantitative (42%), followed by qualitative studies (33%). Table 1 presents the characteristics of the studies, including country, study design, and topical focus. A summary of all key findings is provided in Extended data 25 .
Table 1. Characteristics of the included studies.
| Category | Details | n (%) |
|---|---|---|
| Publication Type | Research Articles | 52 (95%) |
| Project/Programme Reports | 3 (5%) | |
| Year of publication | 2007–2013 | 4 (7%) |
| 2014–2020 | 35 (64%) | |
| 2021–2023 | 16 (29%) | |
| Type of Study | Quantitative | 23 (42%) |
| Qualitative | 18 (33%) | |
| Mixed Methods | 4 (7%) | |
| Project report; Thesis; Project evaluation (3 each) | 9 (16%) | |
| Workshop report | 1 (2%) | |
| Not reported | 1 (2%) | |
| Study design | Cross-sectional | 15 (27%) |
| Qualitative | 15 (27%) | |
| Project evaluation | 5 (9%) | |
| Randomised controlled trial | 5 (9%) | |
| Mixed methods | 4 (7%) | |
| Case study | 3 (5%) | |
| Cohort and Participatory action research (2 each) | 4 (7%) | |
| Phenomenological; Secondary analysis; Assessment report (1 each) | 3 (5%) | |
| Not reported | 1 (2%) | |
| Country | Kenya | 13 (23%) |
| Ethiopia | 13 (23%) | |
| South Africa; Malawi (6 each) | 12 (22%) | |
| Zambia | 3 (5%) | |
| Multi-country (3):
• Four countries: DRC, Egypt, Namibia, Mozambique • Seventeen West and Central African countries: Benin, Burkina Faso, Cameroon, Congo, DRC, Gambia, Ghana, Guinea Bissau, Ivory Coast, Liberia, Mali, Niger, Nigeria, Senegal, Sierra Leone, Chad, & Togo • Two countries: Kenya and Malawi |
3 (5%) | |
| Mali, Ghana, Uganda (2 each) | 6 (11%) | |
| Rwanda, Nigeria, Burkina Faso, Sierra Leone, Mozambique (1 each) | 5 (9%) | |
| Study setting | Health posts | 11 (20%) |
| Health facilities | 7 (13%) | |
| Primary care sites/units | 3 (5%) | |
| Community-based organizations (CBOs) | 2 (4%) | |
| Health Centre | 2 (4%) | |
| Health Office; National Health Insurance Pilot District | 2 (4%) | |
| Not reported | 28 (51%) | |
| Summary of CBHIS * | Sources of CBHIS data | 22 (40%) |
| Processes in generating CBHIS data | 51 (92%) | |
| CBHIS data pathways | 25 (45%) | |
| Utilisation of CBHIS data | 37 (67%) | |
| Community involvement and empowerment | 17 (31%) |
Note: *some studies report more than one detail
Synthesis of results
CBHIS data generation. CHWs are crucial for collecting CBHIS data. Included studies used various titles to describe CHWs based on their cadres and country of origin, including health extension workers (HEWs), community health volunteers (CHVs), community health extension workers (CHEWs), village pioneers, Health Surveillance Assistants (HSAs), community-based health workers (CBHWs), and village health teams (VHTs) ( Table 2). This paper uses CHWs as an all-encompassing term to cover all these designations for ease of reading and clarity. Table 2 summarises the CBHIS data collectors, standard data collection tools, and type of data collected.
Table 2. Summary of CBHIS data generation processes.
| Data collectors | Data collection tools/templates | Type of data collected at the community level | Data submission | |
|---|---|---|---|---|
| Data generation processes | CHWs
• Ethiopia (HEWs) • Kenya (CHPs) • Egypt (Village pioneers-Raedat Refiat (RR)) • Namibia (HEWs) • Uganda (VHTs &CHEWs) • DRC/Zambia/South Africa/Nigeria/Rwanda/Sierra Leone/Mali (CHWs) • Malawi (HSAs) • Burkina Faso (CBHWs) • Mozambique (Agentes Polivalentes Elementares (APEs)) |
Paper-based tools
• Family folder (Ethiopia) • Household registers (Kenya, Egypt, Rwanda, Malawi) • CHWs service Logbook (Kenya) • Simple wall chart templates (Malawi) • Paper registers (Ghana, DRC, Zambia) • Forms/papers (Namibia, South Africa& Ghana) • Surveillance forms (Burkina Faso) Electronic-based tools • Mobile phone applications/technologies/mHealth tools Other sources of data: • Individual health records (health cards and integrated maternal and childcare (MCH) cards) • Assistant chief registers • Community outreach and meetings • Birth and death register • Village register • Under-five register • Household survey/visit form • Community treatment and tracking register • Referral form |
• Health Extension program component data (Ethiopia)
• Program data related to HIV, TB & Malaria (South Africa, Mozambique & Zambia & Namibia) • Child health data element (DRC, South Africa) • Maternal and child civil registration data (Nigeria & Ghana) • Maternal, Neonatal, and Child Health (MNCH) morbidity & mortality data (Sierra Leone) • Maternal and child health services data (Namibia, Malawi & Uganda) • Demographic, household sanitation, housing, health service utilization and coverage (commonly collected) • Supply chain management data (Kenya & Zambia) |
CHWs supervisors
• Ethiopia (HEW supervisors/ coordinators) • Kenya (community health assistants/officers (CHAs/CHOs)) • Egypt (RR supervisors) • Namibia (CHW supervisors) • Uganda (Health Centre (HC) III in-charge) • DRC (HC supervisors) • South Africa (Outreach Team Leaders/data captures) • Sierra Leone (CHWs peer supervisors) • Malawi (Senior HSAs) • Burkina Faso (CBHWs supervisors) • Funders department (South Africa) |
Note: CHEWs: Community Health Extension Workers; CHWs: Community Health Workers; CHPs: Community Health Promoters; DRC: Democratic Republic of Congo HEWs: Health Extension Workers; VHTs: Village Health Teams; HSAs: Health Surveillance Assistances; CBHWSs: Community Based Health Workers
CBHIS data sources. Data collection tools and information collected used by CHWs vary by country and services provided at the community level ( Table 2). CHWs commonly use standardised household registers during house visits to collect community data. Other data collection tools included simple wall charts 26 , CHW Integrated Daily Activity Register/logbooks 1 , individual health cards 1, 27, 28 , and surveillance forms 29 . The CHWs typically collect household data, including household demographics, sanitation, housing, health service utilisation, and coverage 30– 38 . For instance, in DRC and South Africa 39 , CBHIS focused on child health data, whereas in Uganda, Namibia, and Malawi, maternal and child health data were captured 1, 27, 28 . Sierra Leone’s 40 , Nigeria's 41 , and Ghana's 42 CBHIS includes Maternal, Neonatal, and Child Health (MNCH) mortality and morbidity data to inform health service delivery and development of interventions. Some of the CBHIS in Namibia 1 , Zambia 38 , Mozambique 43 , and South Africa 39, 44 collect program-specific data on HIV/AIDS and TB care, malaria data, and households’ eligibility for social support.
CBHIS data pathways. CHWs primarily use paper-based tools for data collection 38, 42, 45 ; however, some countries have adopted electronic-based systems (eCBHIS), such as mobile phone applications and mHealth tools 41– 53 ). In some instances, CHWs must use both manual and eCBHIS methods, as observed in Ethiopia 47, 54 and Ghana 42 . Additionally, mobile technology has been utilised to collect community health data, such as in Kenya, where the mHealth application has been used to collect non-communicable diseases, particularly diabetes and hypertension 55 , and a simple short message service (SMS) – based reporting to support the supply chain management 50 . A mobile-based eCBHIS was implemented in Zambia to monitor commodities stock levels 52 .
In paper-based systems, CHWs record household visits and activities in standardised Federal/National Ministry of Health (MoH) service delivery registers, which are then collated to complete monthly report forms. These report forms their respective catchment areas are then submitted to the supervisors, who aggregate the data in paper-based standardised MoH forms that are in turn submitted to the sub-national office (sub-county, county, district, or regional) for digital entry into the web-based national health information systems, the District Health Information System (DHIS2) 26, 56– 62 . Notably, data collected via paper-based systems are digitally entered into the DHIS2 database at the sub-national level 1, 11, 32 . However, this process faces several challenges. A significant issue is the lack of harmonisation between data collection tools used by CHWs and HMIS forms, resulting in incomplete or inaccurate data transfer 33, 63, 64 . The utilisation of paper-based tools introduces additional obstacles, including stockouts of these tools and insufficient storage capacities 57, 60 . CHWs frequently resort to storing data in their residences. This practice not only increases the risk of data loss but also compromises the confidentiality of sensitive information 11 .
In electronic-based systems, data on household visits or program-specific indicators are entered electronically by CHWs into electronic forms on the applications installed on their tablets or mobile phones and submitted electronically to the organisation’s database or sub-national or national HMIS, DHIS2 27, 37, 41, 51, 52 . The electronically aggregated data in the HMIS are made visible and accessible to CHWs supervisors, health managers, and data managers, who review data, trace data errors in data capture, track and analyse data, as well as send electronic feedback notes to CHWs 41, 51, 52 . Some applications have built-in data validation to ensure the completeness of data 41, 51 . However, in other instances, CBHIS data are directly conveyed to the department of funders, bypassing health facilities for electronic database recording 60 .
CBHIS data review/use meetings are intended to also create effective feedback mechanisms across healthcare service levels 1 . However, the implementation of these mechanisms was often limited to human resource constraints, as observed in Namibia, whereas in DRC, feedback mechanisms were reported to function better in areas with partner support, and in Uganda, feedback was reliant upon the provision of supportive supervision 1 .
The data flow for the CBHIS and feedback mechanisms varied depending on the country and tools used for data collection, whether paper-based or electronic-based. Figure 1 summarises the CBHIS data flow process.
Figure 1. A summary of the overall CBHIS data flow process.
Note: Figure 1: Illustrates an overall summary of the CBHIS data flow process for both paper- and electronic-based systems in African countries. It depicts the collection of community-level data, intermediate aggregation, digital entry for paper-based systems, and reporting levels. CHWs: Community Health Workers; DHIS2: District Health Information System; HMIS: Health Management Information Sytstem; PHC: Primary helthcare.
Utilisation of CBHIS data. At the national/federal level, the division/department responsible for health information systems receives community health data from sub-national levels, which is then transmitted to the division responsible for community health services within the Ministry of Health (MoH) 1 . The division of community health services utilises the data to track the progress of community health programs, create annual health sector performance reports, formulate policies, and provide feedback to decentralised levels. Ideally, all levels of the health system, including community, sub-national, and national, should review and utilise CBHIS data 1 . However, data producers and users often lack the core competencies of data analysis, interpretation, and synthesis, which, in turn, limit the demand and use of data in decision-making processes 1, 11, 65 .
The CBHIS data serves multiple stakeholders in healthcare. Government entities use it for policy decisions, resource allocation, and workforce planning 28, 38, 41 . NGOs and CBOs leverage these data to design targeted interventions, whereas funders allocate resources based on these data 57 . Health facilities rely on CBHIS data to inform service delivery strategies 12, 33 and optimise supply management 33, 50, 52 . Community health committees leverage this data for advocacy and community engagement 64 . Healthcare professionals incorporate CBHIS data into their decision-making processes to enhance service delivery 29, 52 . This diverse utilisation highlights the importance of improving community health outcomes across sectors. In Ethiopia and Malawi, CBHIS data is used to support health extension services 30, 54, 61, 66, 67 , whereas, in South Africa, CHWs use it for community activities and referrals to service providers 46 . In Namibia, the MoH uses it to inform future community health programmes 1 , while health managers in Ethiopia use it to monitor and evaluate community health services 54, 61 . In Kenya, CBHIS programme data is used to assess interventions 68 and design new ones, and in South Africa, regional coordinators use it for programme tracing and planning 60 . CBHIS data also supports collective activities such as community dialogue in Kenya, South Africa, Malawi, and Ethiopia to address the prevalent challenges in catchment areas/community units 12, 36, 56, 58 .
Moreover, CBHIS data is utilised in various ways by CHWs and healthcare providers in Ethiopia, Kenya, South Africa, Malawi, and Zambia, such as tracking people lost to follow-up for health services and scheduling house visits 12, 33, 37, 46, 68 , assessing the utilisation and coverage of maternal and newborn care services 69 , institutional delivery of immunisation 59, 69– 71 , monitoring trends in health service delivery and disease prevalence, and implementing mitigation strategies for disease outbreaks 12, 63 . CHWs also use this data to monitor community health supplies and commodity stock levels 33, 50, 52 and plan health resources at the sub-national and national levels 28, 38, 41 . While CBHIS data is crucial for improving community health programs and outcomes, challenges remain in effectively using data at the community level other than for reporting purposes 12, 26 .
Accessibility of CBHIS data and community empowerment. Community empowerment extends beyond the involvement, participation, or engagement of communities. It encompasses enhancing individual self-care and lifestyle choices; addressing sociopolitical power dynamics; supporting community-driven priorities and implementing strategies to improve health and reduce inequities. In practice, this often manifest through community dialogues, which also serve as platforms for sharing among stakeholders, including community members, leaders, representatives, community health committees, CHWs, and health providers. This collaborative approach to information-sharing has shown promising results in various African countries. Specifically, they have been successfully implemented in Ethiopia, Kenya, Malawi, and South Africa, where they have been effective for priority setting, planning, implementation, and evaluation of health interventions/programmes 36, 46, 56– 58, 68, 69, 72 .
CHWs collaborate with community health committees to initiate community dialogues. Community members can also access CBHIS data through wall charts/chalkboards displayed in community units, health centers, and clinics 26, 32, 33 . However, a study across 17 West and Central African countries revealed limited CBHIS data accessibility to community members beyond the CHWs, impeding community participation in data utilisation 73 . Although community dialogues have been associated with improved health indicators, health service utilisation, and health practices, including improved sanitation and hygiene practices, drug adherence, reduced stigma, increased family planning methods, immunisation, and maternal delivery 12, 36, 68 , direct evidence linking them to specific health outcomes is limited. Community empowerment in these community dialogues tends towards provider-led health promotion activities 36, 56– 58 rather than community-driven/demand-driven interventions that foster community accountability and tailor interventions to community needs.
Discussion
CHS is a crucial aspect of PHC and a vehicle for achieving UHC and other global health SDG priorities. To effectively deliver community health services, a functional and practical CBHIS is essential for countries to track their progress toward PHC and UHC. This scoping review aimed to synthesise evidence on the current practices of CBHIS data generation, data pathways across different health system levels, utilisation of CBHIS data, and accessibility of CBHIS data to communities to empower communities in African countries. The majority of articles reported on CBHIS data generation and use. Most CBHIS utilise paper-based systems, although some countries have adopted electronic/digital systems (eCBHIS) to record and transmit data to sub-national and national HMIS; data pathways vary by country. Multiple stakeholders utilise CBHIS data for decision-making, including policymaking, resource allocation, staffing, programme evaluations, and informing community health programmes and dialogues. Community dialogue is the most common strategy for community engagement, sharing CBHIS data, and empowering communities.
CHWs are crucial in generating data for the CBHIS. Different cadres of CHWs have distinct roles and include data collection, management, and dissemination. Although most countries rely on paper-based systems for data collection, some use electronic-based systems 1, 37, 45– 47 , or a combination of both 47, 54 . However, reported challenges included a lack of standardised data collection and compilation tools 1, 11 , inadequate personnel competencies 37, 51, 52 , and duplicate data entries in paper-based and electronic forms 1 , which can lead to limited data collection and loss, negatively impacting data quality. As countries transition to digitised systems, it is crucial to provide regular technical and supportive supervision to CHWs to tackle user- and system-related challenges associated with eCBHIS. To address these challenges, ongoing training of CHWs by Ministries of Health and partners is crucial. This training should be comprehensive and cover various aspects, including basic Information Communication Technology (ICT) skills, digital tools usage, and data analysis. Moreover, targeted training is crucial for timely, accurate, and complete data entry into eCBHIS 4, 47, 65, 74, 75 .
The contextual adoption of mobile technology can help with the transition e.g., simple feature phones with simple SMS-based reporting systems have been successfully adopted in Ghana, Kenya, Malawi, and Zambia 4, 19 . Our review revealed an absence of policy guidance concerning data security and privacy aspects for both paper- and electronic-based CBHIS systems 11, 41 . For instance, CHWs were obliged to store paper-based data in their homes owing to insufficient storage, leading to lost data forms and the potential breach of confidentiality 11 . To enhance the security and privacy of CBHIS data in the healthcare sector, countries transitioning to digital systems should develop or update their eCBHIS policy frameworks. These frameworks should address the gaps in data security and privacy, safeguard community data and guide the implementation of data protection principles in eCBHIS 1, 76 .
CBHIS generates large amounts of data on healthcare services and population health, presenting opportunities for data-driven decision-making in the CHS. While efforts to enhance CBHIS have primarily focused on digitisation and improving data collection and quality, particularly at the community level, there is a disproportionate emphasis on the technical aspects of enabling data use 74, 77 , overlooking other factors that may hinder its effectiveness. Failure to consider critical elements, such as data analysis and interpretation capabilities across various levels of the health system, may impede the overall effectiveness The ultimate goal of CBHIS is to translate data into action, address health challenges, and improve the access and quality of community health services 77 . We indicate that CBHIS data can inform health system outcomes, resource allocation, and support administrative decision-making processes 45, 54, 57, 59, 66, 78 . Although CBHIS data offers valuable insights, empirical evidence demonstrating its impact on data-driven decision-making remains limited. In practice, several challenges impede the utilisation of CBHIS data, including fragmented reporting systems 13 , poor coordination between data producers and users 12, 13 , varied decentralisation of community health decisions 14 , and limited capacity of data producers and users to use data effectively 1, 11, 65 .
To ensure sustainable demand and use of data in decision-making, it is essential to develop the capacity of data producers and users in core competencies, such as data analysis, interpretation, and synthesis, at all levels of the health system, including the CHS. Investing in capacity-building for data producers and users on critical competencies can facilitate the functioning of CBHIS 79 . Lippeveld (2017) identified many barriers to data use related to organisational and behavioural factors 77 . The information use culture can act as both a barrier 12, 26 and a facilitator 80 in data utilisation. Negative organisational behaviour, such as the pressure senior health managers exert on providers to meet unrealistic service delivery targets, has contributed to false reporting and the denial of existing service delivery problems 77 . Conversely, community-led monitoring of health service delivery data has been demonstrated to promote positive organisational behaviour by enhancing the culture of information 77, 80 .
Community participation in health information generation and dissemination has been shown to increase community engagement and health information sharing and foster health system responsiveness through community activism 20, 80– 82 . However, community members face barriers to accessing and using health information. A multi-country study across 17 West and Central African nations found that community members lacked access to CBHIS data beyond that of CHWs, which hindered their participation in data utilisation 73 . This limits the involvement of end-users of care in developing interventions that align with local needs and are informed by local knowledge and priorities in a more effective and transformative way that helps empower marginalised and vulnerable population groups. Community data dissemination has shown positive results in various initiatives 80, 83, 84 . For instance, a randomised field experiment in nine districts in Uganda revealed that granting communities access to data increased their involvement, accountability, and community-led monitoring of PHC services 80 . Consequently, service utilisation and health outcomes improved significantly. This intervention emphasises the magnitude of community participation and a bottom-up approach to enhancing CHS service delivery and health outcomes. Integrating this approach with a structured top-down approach can lead to even better results 80 .
The results of our review carry with them some implications. The CHS require the availability of good-quality data, however, this on its own is insufficient to support the use of data in the CHS and broader health systems management decision-making. Although studies included in our review reported the utilisation of CBHIS data, there are deficiencies in comprehending the extent to which it's used or integrated in decision-making processes and policy formulation. The health authorities and practitioners may need to consider implementing interventions that explicitly focus on improving the link between CBHIS data collection and the use of data for decision-making. CHS activities, policies and guidelines may need to focus on capacity building of data producers and users in data management and data use competencies, including analysis, synthesis, interpretation, critical review of data, and data-informed decision making 1, 11, 65 . In addition, there is a need to focus on organisational culture and practice of monitoring, evaluation, and communication of data use interventions, and that encourages health managers, frontline health providers and users of health services, to take responsibility for using data to inform decision making 7, 77, 80 .
Our review suggests that there is limited access to CBHIS data beyond community dialogues and wall charts in community health units. Accessibility of CBHIS data to the community is essential to foster community participation in community health activities and accountability. An experimental study on information intervention in Uganda shows that disseminating data to community members can enhance community participation in CHS services, empower them and promote accountability of health providers at the community level 80 . However, there is a gap in studying the impact of community participation and empowerment on health outcomes.
There is a large and diverse body of literature on CBHIS data generation/production (data sources, data management, information products and dissemination) and systems performance (data quality and data use). However, there is a research gap on the links between data collection and data use, and between data use and systems impact, as well as components needed for the design and evaluation of CBHIS, to effectively support health system management decision-making. Implementation research approaches may also help understand data-driven decision-making mechanisms in operational settings 7 .
Strengths and limitations
We conducted a systematic and thorough evaluation of the existing literature. Our approach involved conducting a comprehensive literature search, employing duplicate article screening, and selecting articles by independent reviewers, with senior reviewers verifying and ensuring quality control. However, our review had some limitations. First, we only included published articles and grey literature, which may have led to the exclusion of other relevant documentation on CBHIS. Second, we did not consider non-English studies or grey literature, which could have resulted in the exclusion of articles from non-English-speaking African countries that may have been relevant to our review.
Conclusion
CBHIS are transitioning from paper-based to electronic-based systems, aiming to improve data collection and pathway processes. However, several challenges, including fragmented reporting and limited capacity, impede the effective utilisation of CBHIS data. The successful adoption of CBHIS requires considering resource allocation and technology adoption within the context of the CHS and the broader health system. While efforts focus on the digitisation of CBHIS and enhancing data generation, overlooking other factors may hinder effectiveness. Developing core competencies in data analysis and interpretation among data producers and users across all health system levels is crucial. Community dialogue, while valuable for engagement, requires a shift from provider-driven/supply-side health promotion activities to community-driven/demand-side interventions. Community-driven approaches can enhance community participation in CBHIS, accountability, empowerment, health activism, and tailoring interventions to local needs. The renewed commitment to PHC presents an opportunity to optimise the functionality of CBHIS and accelerate progress towards UHC and other health-related SDGs.
Acknowledgment
This study is part of the African Health Observatory Platform on Health Systems and Policies (AHOP) projects. We thank Alex Maina, Research Librarian at the KEMRI-Wellcome Trust Research Programme, Kenya, who advised on and developed the search strategy. We also acknowledge the KEMRI-Wellcome Trust Research Programme for the infrastructural support to conduct this work.
Funding Statement
This work was supported by the Bill and Melinda Gates Foundation (grant no. ID OPP1198834) subcontracted to Benjamin Tsofa (Platform Lead, Kenya AHOP NC).
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
[version 3; peer review: 4 approved]
Data availability
Underlying data
All data underlying the results are available as part of the article and no additional source data are required.
Extended data
Havard Dataverse: Replication Data for: Examining the Development and Utilisation of Community-Based Health Information Systems (CBHIS) in Africa: A Scoping Review
https://doi.org/10.7910/DVN/ZH5JK8 25
This project includes the following extended data:
Additional File 1 (information search strategy)
Additional File 2 (data extraction form)
Additional File 3 (characteristics of included studies).
Reporting guidelines
Havard Dataverse: PRISMA_ScR Checklist for ‘Examining the development and utilisation of Community-Based Health Information Systems (CBHIS) in Africa: A Scoping Review’. https://doi.org/10.7910/DVN/ZH5JK8 25 .
Data are available under the terms of the Creative Commons Attribution 4.0 International license (CC-BY 4.0).
Authors contributions
Kuvuna B: Conceptualization, Data Curation, Formal analysis, Investigation, Methodology, Validation, Writing – Original Draft Preparation, Writing – Review & Editing; Nyanchoka M: Conceptualization, Formal analysis, Investigation, Methodology, Validation, Writing – Original Draft Preparation, Writing – Review & Editing; Guleid F: Conceptualization, Writing – Review & Editing; Ogutu M: Conceptualization, Writing – Review & Editing; Tsofa B: Conceptualization, Funding Acquisition, Investigation, Methodology, Project Administration, Validation, Writing – Review & Editing; Nzinga J: Conceptualization, Data Curation, Formal Analysis, Investigation, Methodology, Project Administration, Supervision, Validation, Writing – Original Draft Preparation, Writing – Review & Editing.
References
- 1. MCSP: National community health information systems in four African countries. Descriptions and lessons from the field. The Maternal and Child Survival Program (MCSP).2019. Reference Source
- 2. Africa Centres for Disease, Control and Prevention: Ministerial meeting on strengthening community health workforce, systems and programmes in Africa.2023. Reference Source
- 3. Agarwal S, Kirk K, Sripad P, et al. : Setting the global research agenda for Community Health Systems: literature and consultative review. Hum Resour Health. 2019;17(1): 22. 10.1186/s12960-019-0362-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mekonnen ZA, Chanyalew MA, Tilahun B, et al. : Lessons and implementation challenges of Community Health Information System in LMICs: a scoping review of literature. Online J Public Health Inform. 2022;14(1): e5. 10.5210/ojphi.v14i1.12731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zambruni JP, Rasanathan K, Hipgrave D, et al. : Community Health Systems: allowing Community Health Workers to emerge from the shadows. Lancet Glob Health. 2017;5(9):e866–e867. 10.1016/S2214-109X(17)30268-1 [DOI] [PubMed] [Google Scholar]
- 6. MEASURE Evaluation: Community-Based Health Information Systems in the global context a review of the literature. MEASURE Evaluation the Carolina Population Center UoNC,2016. Reference Source
- 7. Leon N, Balakrishna Y, Hohlfeld A, et al. : Routine Health Information System (RHIS) improvements for strengthened health system management. Cochrane Database Syst Rev. 2020;8(8): CD012012. 10.1002/14651858.CD012012.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. WHO: Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies.2010. Reference Source
- 9. Schneider H, Olivier J, Orgill M, et al. : The multiple lenses on the Community Health System: implications for policy, practice and research. Int J Health Policy Manag. 2022;11(1):9–16. 10.34172/ijhpm.2021.73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Russpatrick S, Sæbø J, Romedenne M, et al. : The state of Community Health Information Systems in West and Central Africa. J Global Health Rep. 2019;3: e2019047. 10.29392/joghr.3.e2019047 [DOI] [Google Scholar]
- 11. Regeru RN, Chikaphupha K, Bruce Kumar M, et al. : ‘Do you trust those data?’—A mixed-methods study assessing the quality of data reported by Community Health Workers in Kenya and Malawi. Health Policy Plan. 2020;35(3):334–45. 10.1093/heapol/czz163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Flora OC, Margaret K, Dan K: Perspectives on utilization of Community Based Health Information Systems in Western Kenya. Pan Afr Med J. 2017;27: 180. 10.11604/pamj.2017.27.180.6419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tilahun B, Teklu A, Mancuso A, et al. : Using health data for decision-making at each level of the health system to achieve Universal Health Coverage in Ethiopia: the case of an immunization programme in a low-resource setting. Health Res Policy Syst. 2021;19(Suppl 2): 48. 10.1186/s12961-021-00694-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kumar MB, Taegtmeyer M, Madan J, et al. : How do decision-makers use evidence in community health policy and financing decisions? A qualitative study and conceptual framework in four African countries. Health Policy Plan. 2020;35(7):799–809. 10.1093/heapol/czaa027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Walker D: Community-Based Health Information System guide: approaches and tools for development. MEASURE Evaluation, The Carolina Population Center UoNC,2019. Reference Source
- 16. Bakibinga P, Kamande E, Kisia L, et al. : Challenges and prospects for implementation of Community Health Volunteers' digital health solutions in Kenya: a qualitative study. BMC Health Serv Res. 2020;20(1): 888. 10.1186/s12913-020-05711-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kenya M: Electronic Community Health Information System (eCHIS) 2020 landscape assessment report.Ministry of Health, the Republic of Kenya, Services DoCH.2021. Reference Source
- 18. Owoyemi A, Osuchukwu JI, Azubuike C, et al. : Digital solutions for community and primary health workers: lessons from implementations in Africa. Front Digit Health. 2022;4: 876957. 10.3389/fdgth.2022.876957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Stanton MC, Mkwanda SZ, Debrah AY, et al. : Developing a community-led SMS reporting tool for the rapid assessment of lymphatic filariasis morbidity burden: case studies from Malawi and Ghana. BMC Infect Dis. 2015;15(1): 214. 10.1186/s12879-015-0946-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. van Pinxteren M, Colvin CJ, Cooper S: Using health information for community activism: a case study of the movement for change and social justice in South Africa. PLOS Glob Public Health. 2022;2(9): e0000664. 10.1371/journal.pgph.0000664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hailemariam T, Atnafu A, Gezie LD, et al. : Individual and contextual level enablers and barriers determining electronic Community Health Information System implementation in northwest Ethiopia. BMC Health Serv Res. 2023;23(1): 644. 10.1186/s12913-023-09629-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Arksey H, O'Malley L: Scoping studies: towards a methodological framework. Int J Soc Res Method. 2005;8(1):19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 23. Tricco AC, Lillie E, Zarin W, et al. : PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 24. Nyanchoka M, Kuvuna B, Guleid F, et al. : Examining the development and utilisation of Community-Based Health Information Systems (CBHISs) in Africa: a scoping review.2023. 10.17605/OSF.IO/U27MR [DOI] [PMC free article] [PubMed]
- 25. Beatrice K, Moriasi N, Fatuma G, et al. : Replication data for: examining the development and utilisation of Community-Based Health Information Systems (CBHIS) in Africa: a scoping review. V1 ed: Harvard Dataverse,2024. [Google Scholar]
- 26. Hazel E, Chimbalanga E, Chimuna T, et al. : Using data to improve programs: assessment of a data quality and use intervention package for Integrated Community Case Management in Malawi. Glob Health Sci Pract. 2017;5(3):355–66. 10.9745/GHSP-D-17-00103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Namatovu E, Kanjo C: Visibility in community health work mediated by mobile health systems: a case of Malawi. Electron J Inf Syst Dev Ctries. 2019;85(2): e12071. 10.1002/isd2.12071 [DOI] [Google Scholar]
- 28. Nanyonjo A, Kertho E, Tibenderana J, et al. : District health teams' readiness to institutionalize Integrated Community Case Management in the Uganda local health systems: a repeated qualitative study. Glob Health Sci Pract. 2020;8(2):190–204. 10.9745/GHSP-D-19-00318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Diallo CO, Schiøler KL, Samuelsen H, et al. : Information system as part of epidemic management in Burkina Faso: from plan to reality (Field Findings). BMC Public Health. 2022;22(1): 1726. 10.1186/s12889-022-14072-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mossie MY, Pfitzer A, Yusuf Y, et al. : Counseling at all contacts for postpartum contraceptive use: can paper-based tools help Community Health Workers improve continuity of care? A qualitative study from Ethiopia [version 2; peer review: 2 approved, 1 approved with reservations]. Gates Open Res. 2021;3:1652. 10.12688/gatesopenres.13071.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mash R, Du Pisanie L, Swart C, et al. : Evaluation of household assessment data collected by Community Health Workers in Cape Town, South Africa. S Afr Fam Pract (2004). 2020;62(1):e1–e6. 10.4102/safp.v62i1.5168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Næss M: Automated feedback systems for Community Health Workers-a case study from Malawi.2018. Reference Source
- 33. Kubalalika PJ: Lessons learned from introducing a Village Health Registry in Malawi. Online J Public Health Inform. 2018;10(2):e217. 10.5210/ojphi.v10i2.9117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chhetri A: Evaluation and development of android mHealth application for Community Health Workers in Malawi: comparison of commcare and DHIS2 tracker.2018. Reference Source [Google Scholar]
- 35. Mitsunaga T, Hedt-Gauthier BL, Ngizwenayo E, et al. : Data for program management: an accuracy assessment of data collected in household registers by Community Health Workers in Southern Kayonza, Rwanda. J Community Health. 2015;40(4):625–32. 10.1007/s10900-014-9977-9 [DOI] [PubMed] [Google Scholar]
- 36. Jeremie N, Akinyi C: Utilization of Community based Health Information Systems; management and community service delivery in Kenya. American Journal of Clinical Neurology and Neurosurgery. 2015;1(2):54–9. Reference Source [Google Scholar]
- 37. Schuttner L, Sindano N, Theis M, et al. : A mobile phone-based, Community Health Worker program for referral, follow-up, and service outreach in rural Zambia: outcomes and overview. Telemed J E Health. 2014;20(8):721–8. 10.1089/tmj.2013.0240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hamainza B, Killeen GF, Kamuliwo M, et al. : Comparison of a mobile phone-based malaria reporting system with source participant register data for capturing spatial and temporal trends in epidemiological indicators of malaria transmission collected by Community Health Workers in rural Zambia. Malar J. 2014;13(1): 489. 10.1186/1475-2875-13-489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Odendaal W, Lewin S, McKinstry B, et al. : Using a mHealth system to recall and refer existing clients and refer community members with health concerns to primary healthcare facilities in South Africa: a feasibility study. Glob Health Action. 2020;13(1): 1717410. 10.1080/16549716.2020.1717410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. O'Connor EC, Hutain J, Christensen M, et al. : Piloting a Participatory, Community-Based Health Information System for strengthening community-based health services: findings of a cluster-randomized controlled trial in the slums of Freetown, Sierra Leone. J Glob Health. 2019;9(1): 010418. 10.7189/jogh.09.010418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Asangansi I, Macleod B, Meremikwu M, et al. : Improving the routine HMIS in Nigeria through mobile technology for community data collection. J Health Inform Dev Ctries. 2013;7(1). Reference Source [Google Scholar]
- 42. Ohemeng-Dapaah S, Pronyk P, Akosa E, et al. : Combining vital events registration, verbal autopsy and electronic medical records in rural Ghana for improved health services delivery. Stud Health Technol Inform. 2010;160(Pt 1):416–420. 10.3233/978-1-60750-588-4-416 [DOI] [PubMed] [Google Scholar]
- 43. Karajeanes E, Bila D, Luis M, et al. : The infomóvel—an information system for managing HIV/AIDS patients in rural areas of Mozambique. BMC Med Inform Decis Mak. 2023;23(1): 187. 10.1186/s12911-023-02281-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Swartz A, LeFevre AE, Perera S, et al. : Multiple pathways to scaling up and sustainability: an exploration of digital health solutions in South Africa. Global Health. 2021;17(1): 77. 10.1186/s12992-021-00716-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Rothstein JD, Jennings L, Moorthy A, et al. : Qualitative assessment of the feasibility, usability, and acceptability of a mobile client data app for community-based maternal, neonatal, and child care in rural Ghana. Int J Telemed Appl. 2016;2016(1): 2515420. 10.1155/2016/2515420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Tshikomana RS, Ramukumba MM: Implementation of mHealth applications in community-based health care: insights from Ward-Based Outreach Teams in South Africa. PLoS One. 2022;17(1): e0262842. 10.1371/journal.pone.0262842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Bogale TN, Teklehaimanot SM, Fufa Debela T, et al. : Barriers, facilitators and motivators of electronic Community Health Information System use among health workers in Ethiopia. Front Digit Health. 2023;5: 1162239. 10.3389/fdgth.2023.1162239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Miiro C, Oyama C, Aoki Y, et al. : Bridging the gap between community health workers’ digital health acceptance and actual usage in Uganda: exploring key external factors based on technology acceptance model.2023. 10.21203/rs.3.rs-3546017/v1 [DOI] [Google Scholar]
- 49. Yang JE, Lassala D, Liu JX, et al. : Effect of mobile application user interface improvements on minimum expected home visit coverage by community health workers in Mali: a randomised controlled trial. BMJ Glob Health. 2021;6(11): e007205. 10.1136/bmjgh-2021-007205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Andersson SR, Hassanen S, Momanyi AM, et al. : Using Human-Centered Design to adapt supply chains and digital solutions for Community Health Volunteers in nomadic communities of Northern Kenya. Glob Health Sci Pract. 2021;9(Suppl 1):S151–S67. 10.9745/GHSP-D-20-00378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Mengesha W, Steege R, Kea AZ, et al. : Can mHealth improve timeliness and quality of health data collected and used by health extension workers in rural Southern Ethiopia? J Public Health (Oxf). 2018;40(suppl_2):ii74–ii86. 10.1093/pubmed/fdy200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Biemba G, Chiluba B, Yeboah-Antwi K, et al. : A mobile-based Community Health Management Information System for Community Health Workers and their supervisors in 2 districts of Zambia. Glob Health Sci Pract. 2017;5(3):486–494. 10.9745/GHSP-D-16-00275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Gatara MC: Mobile-health tool use and Community Health Worker performance in the Kenyan context: a comparison of Task-Technology Fit perspectives. mHealth Ecosystems and Social Networks in Healthcare.2016;20:55–77. 10.1007/978-3-319-23341-3_5 [DOI] [Google Scholar]
- 54. Chewicha K, Azim T: Community Health Information System for family centered health care: scale-up in Southern Nations Nationalities and People’s Region. Ethiop Ministry Health Q Health Bulletin. 2013;5(1):49–51. Reference Source [Google Scholar]
- 55. Viljoen A, Klinker K, Wiesche M, et al. : Design principles for mHealth application development in rural parts of developing countries: the case of noncommunicable diseases in Kenya. IEEE Trans Eng Manag. 2023;70(3):894–911. 10.1109/TEM.2021.3072601 [DOI] [Google Scholar]
- 56. Wekesa RN: Utilization of the Health Information Management System by community health workers in the AMREF facility in Kibera, Nairobi County, Kenya.Unpublished Masters Degree in Public Health, Monitoring and Evaluation Project, Kenyatta University, Nairobi, Kenya,2014. Reference Source [Google Scholar]
- 57. Pepela WD, Odhiambo-Otieno GW: Community Health Information System utility: a case of Bungoma County Kenya. Int Res J Public Env Health. 2016;3(4):75–86. 10.15739/irjpeh.16.010 [DOI] [Google Scholar]
- 58. Mambo S, Odhiambo-Otieno GW, Ochieng’-Otieno G, et al. : Assessing the influence of process interventions of community health volunteers on use of community based health management information systems in selected counties, Kenya. Int J Sci Res Pub. 2018;8(8). 10.29322/IJSRP.8.8.2018.p8003 [DOI] [Google Scholar]
- 59. Bayeh B: Process evaluation of Community Health Information System in West Gojjam Zone Amhara Regional State. Ethiopia: UOG.2021.
- 60. August V: Factors influencing the implementation of a Community Based Information System and data use by Community Health Workers for the planning and management of HIV/AIDS programmes in Chris Hani District, Eastern Cape.2022. Reference Source
- 61. Ejeta LT, Leta Y, Abuye M, et al. : Implementing the Urban Community Health Information System in Ethiopia: lessons from the pilot-tests in Addis Ababa, Bishoftu and Hawassa. Ethiop J Health Develop. 2020;34(2):49–53. Reference Source [Google Scholar]
- 62. Dusabe-Richards JN, Tesfaye HT, Mekonnen J, et al. : Women Health Extension Workers: capacities, opportunities and challenges to use ehealth to strengthen equitable health systems in southern Ethiopia. Can J Public Health. 2016;107(4–5):e355–e61. 10.17269/cjph.107.5569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Kasambara A, Kumwenda S, Kalulu K, et al. : Assessment of implementation of the Health Management Information System at the district level in southern Malawi. Malawi Med J. 2017;29(3):240–6. 10.4314/mmj.v29i3.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Kirk K, McClair TL, Dakouo SP, et al. : Introduction of digital reporting platform to integrate community-level data into health information systems is feasible and acceptable among various community health stakeholders: a mixed-methods pilot study in Mopti, Mali. J Glob Health. 2021;11: 07003. 10.7189/jogh.11.07003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Simen-Kapeu A, Reserva ME, Ekpini RE: Galvanizing action on Primary Health Care: analyzing bottlenecks and strategies to strengthen Community Health Systems in West and Central Africa. Glob Health Sci Pract. 2021;9(Suppl 1):S47–S64. 10.9745/GHSP-D-20-00377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Yarinbab TE, Assefa MK: Utilization of HMIS data and its determinants at health facilities in East Wollega zone, Oromia regional state, Ethiopia: a health facility based cross-sectional study. Med Health Sci. 2018;7(1):4–9. Reference Source [Google Scholar]
- 67. Daka DW, Wordofa MA, Abdi KL, et al. : Health extension workers' digital literacy and their attitude towards community-level electronic health information systems in Tiro Afata Woreda, Southwest Ethiopia. Ethiop J Health Dev. 2022;36(2). Reference Source [Google Scholar]
- 68. Jeremie N, Kaseje D, Olayo R, et al. : Utilization of community-based health information systems in decision making and health action in Nyalenda, Kisumu County, Kenya. Univers J Med Sci. 2014;2(4):37–42. 10.13189/ujmsj.2014.020401 [DOI] [Google Scholar]
- 69. Karim AM, Fesseha Zemichael N, Shigute T, et al. : Effects of a Community-Based Data for Decision-Making intervention on maternal and newborn health care practices in Ethiopia: a dose-response study. BMC Pregnancy Childbirth. 2018;18(Suppl 1): 359. 10.1186/s12884-018-1976-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Zegeye AH, Kara NM, Bachore BB, et al. : Utilization of Community Health Information System and associated factors in health posts of Hadiya zone, southern Ethiopia. J Med Physiol Biophys. 2020;63:13–22. 10.7176/JMPB/63-03 [DOI] [Google Scholar]
- 71. Tigabu S, Medhin G, Jebena MG, et al. : The effect of Community Health Information System on health care services utilization in rural Ethiopia. Ethiop J Health Sci. 2023;33(1):15–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Ngugi AK, Odhiambo R, Agoi F, et al. : Cohort profile: the Kaloleni/Rabai Community Health and demographic surveillance system. Int J Epidemiol. 2020;49(3):758–759. 10.1093/ije/dyz252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Russpatrick S, Sæbø J, Romedenne M, et al. : The state of Community Health Information Systems in West and Central Africa. J Glob Health Rep. 2019;3: e2019047. 10.29392/joghr.3.e2019047 [DOI] [Google Scholar]
- 74. Byrne E, Sæbø JI: Routine use of DHIS2 data: a scoping review. BMC Health Serv Res. 2022;22(1): 1234. 10.1186/s12913-022-08598-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Penn L, Goffe L, Haste A, et al. : Management Information Systems for community based interventions to improve health: qualitative study of stakeholder perspectives. BMC Public Health. 2019;19(1): 105. 10.1186/s12889-018-6363-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Ogonjo FA, Achieng R, Zalo M: An overview of data protection in Kenyan health sector. Strathmore University;2022. Reference Source [Google Scholar]
- 77. Lippeveld T: Routine health facility and community information systems: creating an information use culture. Glob Health Sci Pract. 2017;5(3):338–40. 10.9745/GHSP-D-17-00319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Chanyalew MA, Yitayal M, Atnafu A, et al. : Routine health information system utilization for evidence-based decision making in Amhara national regional state, northwest Ethiopia: a multi-level analysis. BMC Med Inform Decis Mak. 2021;21(1): 28. 10.1186/s12911-021-01400-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Nutley T: Improving data use in decision making: an intervention to strengthen health systems. MEASURE Evaluation,2012. Reference Source [Google Scholar]
- 80. Björkman M, Svensson J: Power to the people: evidence from a randomized field experiment on community-based monitoring in Uganda. Q J Econ. 2009;124(2):735–69. 10.1162/qjec.2009.124.2.735 [DOI] [Google Scholar]
- 81. Karuga R, Kok M, Luitjens M, et al. : Participation in primary health care through community-level health committees in Sub-Saharan Africa: a qualitative synthesis. BMC Public Health. 2022;22(1): 359. 10.1186/s12889-022-12730-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Kretchy IA, Okoibhole LO, Sanuade OA, et al. : Scoping review of Community Health Participatory Research projects in Ghana. Glob Health Action. 2022;15(1): 2122304. 10.1080/16549716.2022.2122304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Rifkin SB: Examining the links between community participation and health outcomes: a review of the literature. Health Policy Plan. 2014;29 Suppl 2(suppl_2):ii98–ii106. 10.1093/heapol/czu076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Baptiste S, Manouan A, Garcia P, et al. : Community-led monitoring: when community data drives implementation strategies. Curr HIV/AIDS Rep. 2020;17(5):415–421. 10.1007/s11904-020-00521-2 [DOI] [PMC free article] [PubMed] [Google Scholar]