Abstract
Background:
Roughly 10% of children aged 3 -17 in the USA are diagnosed with attention-deficit hyperactivity disorder (ADHD), and minorities are less likely to initiate common pharmacologic treatment. We conducted a review of the literature to examine meditation as a safe, effective, and low-cost alternative.
Methods:
We searched PubMed and other journals using "meditation," "mindfulness," "minority," related keywords, and relevant MeSH terms. Eligible studies involved racial/ethnic minorities in the USA, reported quantitative psychosocial outcomes, and were published in a peer-reviewed, English-language journal.
Results:
Out of 119 "hits," 111 were eliminated as duplicates or were not relevant. A full-text review of the remaining eight revealed that none fully met our eligibility criteria. Besides the obvious lack of studies, those reviewed reported incomplete demographic and clinical data. They also employed different and inconsistent research methodologies, interventions and modalities, and statistical analyses. This hindered understanding exactly which populations may benefit from meditation, and for which specific symptoms.
Conclusion:
We recommend a socio-ecological model in examining intervention modalities, especially in the context of intrapersonal, interpersonal, organizational, environmental, and policy domains. We also suggest the possible inclusion of research older than 10 years, conducted outside of the USA, on minority and non-minority populations, for supplementary and confirmatory data. We advocate for consistency in study design and data collection, which would help align research conducted in different countries. Searches should also include variations of meditation such as "mindfulness" and "guided imagery," and associated symptoms and comorbidities of ADHD, including "learning disorder" and "behavioral problems."
Keywords: Health disparity, Minority and vulnerable, Attention deficit disorder, Attention deficit disorder with hyperactivity, Mediation, Mindfulness
Introduction
Attention-deficit hyperactivity disorder (ADHD) is a neurodevelopmental condition that interferes with functioning and development in children, characterized by persistent patterns of inattention and hyperactivity-impulsivity.1 A 2009-2017 National Health Interview Survey found that nearly 10% of children aged 3-17 suffered from ADHD,2 with a slightly lower prevalence (9.85%) among non-Hispanic Black children.3 In the general population, ADHD co-occurs with anxiety disorder in 25% of children, and in 30%-40% of those who are clinically-referred. ADHD is present in 30 - 50% of children diagnosed with oppositional defiant disorder (ODD) and conduct disorder (CD).4 Children with CD also have an increased risk of bipolar disorder.5-9
There is evidence of an ethnic disparity in the diagnosis and treatment of ADHD among minority children.10-13 Parental attitudes toward mental health issues and medication use, and the underutilization of mental health services by minorities, appear to be contributing factors.14 Paradoxically, minority children may be over-diagnosed and over-treated for ADHD. Their abilities and behaviors may more often be subjectively viewed as problematic and atypical,15,16 requiring intervention and treatment. Possibly as a result, there is a disproportionately high percentage of minority children in special education.17,18
It is important to note that nearly 20% of patients do not respond well to commonly prescribed ADHD medication. Adverse side effects include mood, anxiety and sleep disorders, and substance misuse.19 It is therefore not surprising that over 70% of ADHD patients choose non-pharmacological interventions,20 of which meditation may be effective.21 Functional magnetic resonance imaging (fMRI) of the brains of ADHD patients has shown that meditation can counter hypo-activation in key regions including the anterior cingulate cortex, prefrontal cortices, parietal cortices, and the basal ganglia.22 Meditation may also influence the cerebral parenchyma, increasing gray matter thickness in many of these regions.22-25 Meditation may also be associated with neural and metabolic changes and responses that can ameliorate ADHD and associated comorbidities,26 and with the inhibition of the sympathetic nervous system.27
Credible and rigorous research that supports meditation-based interventions as comparable to, or more effective than, current standard-of-care could influence best practices in both pediatrics and psychiatry. The result may be a safe, effective, low-cost and accessible alternative to pharmacological interventions that would be especially beneficial for children from racial and ethnic minorities who suffer from ADHD.
Research aims
The primary aim of this study was to assess the efficacy and potential benefits of meditation as a treatment modality for minority, pediatric ADHD patients. Our objectives included reporting and discussing findings in the literature, identifying gaps and limitations in existing research, and to offer recommendations that would guide and shape future study. Through these, we sought to contribute to a better understanding of the role of meditation in addressing ADHD among pediatric patients from diverse racial and ethnic backgrounds.
Material and Methods
Study design and database search
We followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines28 in conducting our search of PubMed, Web of Science, PsycINFO, Embase, and Cochrane Review for relevant articles published between December, 2012 and December 2023, inclusive. We employed a large list of keywords that included “meditation,” “mindfulness,” and “attention deficit disorder with hyperactivity,” along with relevant MeSH terms (Table S1).
Search criteria
Inclusion criteria were established using a framework of population, intervention, a control or comparison group, and outcomes of interest (PICO).29 Eligible studies considered minority ADHD pediatric patients, age 17 and under, who were diagnosed with the following International Classification of Diseases (ICD) codes:
F90.0 Attention-deficit hyperactivity disorder, predominantly inattentive type.
F90.1 Attention-deficit hyperactivity disorder, predominantly hyperactive type.
F90.2 Attention-deficit hyperactivity disorder, combined type.
F90.8 Attention-deficit hyperactivity disorder, other type.
F90.9 Attention-deficit hyperactivity disorder, unspecified type.
We included ADHD populations with comorbidities such as anxiety, depression, CD, and substance use disorder.
Eligibility criteria
Eligible studies used meditation modalities to treat ADHD in minority pediatric populations in the USA. Studies that involved control or comparison groups used medication and/or current standard of care. Participants may also have received no intervention or treatment, or received placebos. Eligible studies were peer-reviewed, involved participants in the USA, and were published between December 2012 and December 2023, inclusive. Study measurements must have included (1) reduction (if any) of core symptoms, (2) global functioning/quality of life, and (3) social functioning. Functioning/quality of life and social function must have been measured through validated scales.
Study selection
We used Covidence, a systematic review platform (Veritas Health Innovation, Melbourne, Australia; http://www.covidence.org/) to screen potential studies in several stages for inclusion in our final review (Figure 1). In the first stage, two study members independently reviewed the titles and summaries of “hits” found in our initial search for terms and keywords relevant to our research aims. In the second stage, the abstracts of relevant studies were reviewed to confirm their potential inclusion. In the third stage, a full-text review was conducted to determine whether the article met eligibility criteria and should be included in our final analysis. To demonstrate reliability in our review process, we examined inter-rater consistency, and resolved discrepancies through discussion and consensus.
Figure 1.
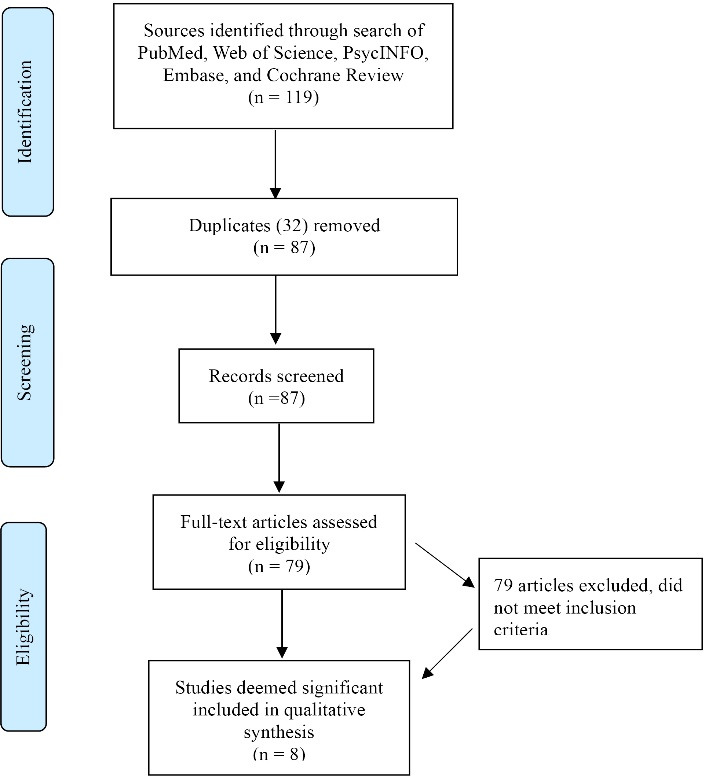
PRISMA Flow chart of source selection. Our initial search yielded 119 journal articles and manuscripts. Of these, none met our strict inclusion criteria. However, eight of these reported improvement through the use of meditation and related modalities
We limited our search to studies published in peer-reviewed journals between December 2012 and December 2023, inclusive. This was done primarily because meditation-based interventions are seen to have been increasingly utilized and promoted as an alternative or complementary treatment for ADHD only within the past decade. However, it is possible that earlier studies may have also proved relevant and useful.
We searched using “meditation” as the main intervention in research that involved participants 17 years of age or younger diagnosed specifically with ADHD. We considered only those studies published in peer-reviewed journals between December 2012 and December 2023, inclusive. This was done primarily because meditation-based interventions are seen to have been increasingly utilized and promoted as an alternative or complementary treatment for ADHD only within the past decade.30-32
Results
Our search of the literature yielded 119 “hits” with 32 duplicates. We screened the titles and abstracts of the remaining 87 and eliminated 79 studies based on relevance and inclusion criteria. Through a full-text review of the remaining eight articles, we found that none fully met our eligibility criteria (Figure 1). However, these articles did report significant, although inconsistent, equivocal, and possibly subjective positive improvement through the use of meditation and related modalities. Moreover, cultural, socioeconomic, and clinical details of participants in these eight studies were often inconsistent and incomplete. This hindered identifying which interventions were effective for specific populations. Methodological differences across these studies also made it difficult to discern the most effective modalities and options for specific conditions and symptoms of ADHD.
Studies conducted outside of the USA
An individualized intervention conducted in Iran, for example, found perceptual-motor training and mindfulness associated with a statistically significant improvement among children with ADHD. However, this was found only in “certain subgroups (indicators) of attention deficit hyperactivity networks.”33 A family-centered program in Holland34 taught youths with ADHD mindfulness techniques, while their parents were trained in mindful parenting. In this qualitative study, many parents reported improvement in ADHD symptoms, although these were diverse and largely inconsistent.
Studies conducted in the USA
Several studies conducted in the USA35-39 did not meet our eligibility criteria, as they did not specifically examine ADHD. However, these reported improvement in associated symptoms such as impulsivity, behavioral dysregulation, and attentional capacity difficulties associated with reactive aggression. One of these studies involved “Coping Power” (CP),35 an evidence-based intervention for youth with disruptive behavior problems in suburban Alabama. It was compared to “Mindful Coping Power” (MCP), a variation of CP that incorporates elements of mindfulness. Children received their respective intervention during the school week in 45-minute sessions, while parent group sessions occurred once a week. The MCP intervention was associated with a statistically significant improvement in self-reported dysregulation, inhibitory control and breath awareness. However, no parent-reported improvement was statistically significant.
Another school-based mindfulness intervention39 involved third- through sixth-grade public charter school students, and their teachers. Both groups learned mindfulness practices together for 30-40 minutes per week over ten weeks. Ninety-three percent of the participants were Hispanic/Latino or African American. This intervention was associated with significantly higher cooperation levels, and significantly lower hyperactivity/inattention in the children, as reported by teachers. Males had significantly lower hyperactivity/inattention scores than those in the control group; this effect was not seen in females.
“Move Into Learning” is an eight-week mindfulness-based educational intervention consisting of yoga, music, and visual arts that was implemented among urban, underserved third graders.36 Although it did not consider ADHD per se, the researchers found a statistically significant improvement in hyperactivity, and in cognitive ability and inattentiveness. This improvement persisted through post-intervention and a two-month follow-up assessment. Interviews with the teachers also revealed their positive perceptions regarding the feasibility and usefulness of the intervention.
A study of high school students in a 12-week intervention program that employed yoga and meditation sessions37 found significant improvement in self-reported measures of attention and hyperactivity. Teachers also reported that students who completed the intervention were more attentive in class and presented better posture. A review38 of school-based, mind-body practices and interventions focused on children aged 2-18. It included yoga, meditation, mindfulness-based stress reduction, and relaxation training techniques. Although there was improvement in specific ADHD-related symptoms, it was unclear exactly which interventions and practices were most effective.
Other studies40-42 suggest that “acceptance and commitment” therapy, which relies heavily on mindfulness practices, may be effective for Black adolescents with comorbid ADHD, learning disorders, and behavior problems. Significant improvement was also seen in self-reported measures of attention and hyperactivity.
Discussion
Although we found no articles that met our rigorous eligibility criteria, our full-text review yielded findings and information which can help guide and inform future research. Articles examined in this stage often revealed incomplete cultural, socioeconomic, and clinical details of participants, perhaps as a function of study design and data collection. This hindered identifying which interventions may be the most effective for specific racial/ethnic and socioeconomic populations and (sub)groups. In addition, because of the substantial differences in research methodologies, modalities, and statistical analyses, it was difficult to determine which interventions and programs were the most effective in treating specific components and related symptoms of ADHD in minority children. Consistency in study design and data collection would also help align research conducted in the USA and in different countries.
A variety of meditation modalities have been applied in treating ADHD and related symptoms in children, with different levels and measures of success. To analyze, assess and organize these different approaches and modalities, we employed a unifying socio-ecological model43 of child development and environmental context relevant in promoting health-related behavioral change at home, in schools, and in other settings. We considered meditation modalities, interventions and programs as they may operate in and across intrapersonal, interpersonal, organizational, environmental, and policy levels of this framework.44
At the intrapersonal level, practices like mindfulness and yoga appear to empower children in enhancing self-regulation and attention. Family-based mindfulness programs at the interpersonal level improve communication and coping skills for both children, and for their families. The informed perspectives and participation of parents and educators may also operate at this level. Mindfulness-based classroom interventions are seen to act within the organizational domain. These allow administrators to adapt educational practices to better serve children with ADHD. Within environmental and policy domains, factors such as better access to resources and mental health services may significantly mitigate ADHD symptomatology.
Limitations
Our study focused exclusively on interventions for ADHD in racial and ethnic minorities within the USA. There may exist a substantial body of research involving non-minority children, or studies that involve various and diverse racial and ethnic groups. Excluding non-minority populations could potentially lead to an incomplete understanding of meditation interventions for ADHD.
We searched using “meditation” as the main intervention. A search of related modalities, variations, practices, and techniques such as “transcendentalism,” “mantra,” “yoga,” “chakra,” and “guided imagery” may have produced a larger number of “hits,” and could have yielded additional articles for consideration. Similarly, we considered only those studies that involved participants diagnosed specifically with ADHD. By expanding our search to include common ADHD comorbidities such as behavior or conduct problems, learning disorders, anxiety and depression, we may have increased the number of studies for potential inclusion.
We also recognize that valuable insight may exist in studies conducted outside of the USA. A more global perspective on ADHD interventions for children could offer supplementary or supporting material and contribute to the comprehensiveness of our findings. Future research may therefore incorporate a more diverse range of study populations and consider international perspectives to achieve a more holistic understanding of the efficacy of meditation in treating ADHD.
Conclusions and Recommendations
Our search of the literature returned no studies that met our strict eligibility criteria. This underscores the need for more comprehensive and standardized research in meditation and mindfulness interventions for ADHD in minority children. Cultural, socioeconomic, and clinical details of participants were often inconsistent and incomplete, which hindered identifying interventions that were effective for specific populations. In addition, methodological differences across studies made it difficult to discern the most effective modalities and options for specific conditions and symptoms of ADHD.
Despite these limitations, articles examined in our review process provided valuable insight into diverse approaches. By utilizing a unifying, socio-ecological model to analyze meditation modalities, we were able to discern their impact in different domains of child development and environmental contexts. Mindfulness and yoga interventions showed promise at the intrapersonal level, fostering self-regulation and attention in children. Family-based programs appeared beneficial at the interpersonal level, by enhancing communication and coping skills. Classroom interventions operated within the organizational domain, empowering administrators in adopting better educational practices for children with ADHD. Environmental and policy factors, such as improved access to resources and mental health services, were identified as crucial components in mitigating ADHD symptomatology.
While no studies fully met our eligibility criteria, findings from this review help lay a foundation for future research. Understanding the effects of meditation across diverse populations and settings is essential in developing safe, targeted and effective interventions for children with ADHD.
Acknowledgements
Heartfelt thanks to Kaveh Dehghan, MBA, for his exceptional support and wisdom in finalizing this manuscript; his assistance has been invaluable.
Competing Interests
None.
Ethical Approval
Not applicable.
Supplementary Files
Table S1. PubMed, Web of Science, PsychInfo, Embase, and Cochrane Review keywords, MeSH terms, and search results
Funding Statement
This research was supported partly by NIH National Center for Advancing Translational Science (NCATS) UCLA CTSI Grant Number UL1TR001881.
References
- 1.American Psychiatric Association (APA) Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: APA; 2013. [Google Scholar]
- 2.Bitsko RH, Claussen AH, Lichstein J, Black LI, Jones SE, Danielson ML, et al. Mental health surveillance among children - United States, 2013-2019. MMWR Suppl. 2022;71(2):1–42. doi: 10.15585/mmwr.su7102a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zablotsky B, Black LI, Maenner MJ, Schieve LA, Danielson ML, Bitsko RH, et al. Prevalence and trends of developmental disabilities among children in the United States: 2009-2017. Pediatrics. 2019;144(4):e20190811. doi: 10.1542/peds.2019-0811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shortlidge EE, Rain-Griffith L, Shelby C, Shusterman GP, Barbera J. Despite similar perceptions and attitudes, postbaccalaureate students outperform in introductory biology and chemistry courses. CBE Life Sci Educ. 2019;18(1):ar3. doi: 10.1187/cbe.17-12-0289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Biederman J, Petty CR, Monuteaux MC, Mick E, Parcell T, Westerberg D, et al. The longitudinal course of comorbid oppositional defiant disorder in girls with attention-deficit/hyperactivity disorder: findings from a controlled 5-year prospective longitudinal follow-up study. J Dev Behav Pediatr. 2008;29(6):501–7. doi: 10.1097/DBP.0b013e318190b290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Busch B, Biederman J, Cohen LG, Sayer JM, Monuteaux MC, Mick E, et al. Correlates of ADHD among children in pediatric and psychiatric clinics. Psychiatr Serv. 2002;53(9):1103–11. doi: 10.1176/appi.ps.53.9.1103. [DOI] [PubMed] [Google Scholar]
- 7.Hammerness P, Geller D, Petty C, Lamb A, Bristol E, Biederman J. Does ADHD moderate the manifestation of anxiety disorders in children? Eur Child Adolesc Psychiatry. 2010;19(2):107–12. doi: 10.1007/s00787-009-0041-8. [DOI] [PubMed] [Google Scholar]
- 8.Wilens TE, Biederman J, Brown S, Tanguay S, Monuteaux MC, Blake C, et al. Psychiatric comorbidity and functioning in clinically referred preschool children and school-age youths with ADHD. J Am Acad Child Adolesc Psychiatry. 2002;41(3):262–8. doi: 10.1097/00004583-200203000-00005. [DOI] [PubMed] [Google Scholar]
- 9. Tannock R. ADHD with anxiety disorders. In: Brown TE, ed. ADHD Comorbidities: Handbook for ADHD Complications in Children and Adults. Arlington, VA: American Psychiatric Publishing; 2009. p. 131-55.
- 10.Coker TR, Elliott MN, Toomey SL, Schwebel DC, Cuccaro P, Tortolero Emery S, et al. Racial and ethnic disparities in ADHD diagnosis and treatment. Pediatrics. 2016;138(3):e20160407. doi: 10.1542/peds.2016-0407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morgan PL, Staff J, Hillemeier MM, Farkas G, Maczuga S. Racial and ethnic disparities in ADHD diagnosis from kindergarten to eighth grade. Pediatrics. 2013;132(1):85–93. doi: 10.1542/peds.2012-2390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ray GT, Levine P, Croen LA, Bokhari FA, Hu TW, Habel LA. Attention-deficit/hyperactivity disorder in children: excess costs before and after initial diagnosis and treatment cost differences by ethnicity. Arch Pediatr Adolesc Med. 2006;160(10):1063–9. doi: 10.1001/archpedi.160.10.1063. [DOI] [PubMed] [Google Scholar]
- 13.Slobodin O, Masalha R. Challenges in ADHD care for ethnic minority children: a review of the current literature. Transcult Psychiatry. 2020;57(3):468–83. doi: 10.1177/1363461520902885. [DOI] [PubMed] [Google Scholar]
- 14.Olaniyan O, dosReis S, Garriett V, Mychailyszyn MP, Anixt J, Rowe PC, et al. Community perspectives of childhood behavioral problems and ADHD among African American parents. Ambul Pediatr. 2007;7(3):226–31. doi: 10.1016/j.ambp.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 15.Brown TR, Xu KY, Glowinski AL. Cognitive behavioral therapy and the implementation of antiracism. JAMA Psychiatry. 2021;78(8):819–20. doi: 10.1001/jamapsychiatry.2021.0487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hays DG, Prosek EA, McLeod AL. A mixed methodological analysis of the role of culture in the clinical decision-making process. J Couns Dev. 2010;88(1):114–21. doi: 10.1002/j.1556-6678.2010.tb00158.x. [DOI] [Google Scholar]
- 17.Blanchett WJ. Disproportionate representation of African American students in special education: acknowledging the role of white privilege and racism. Educ Res. 2006;35(6):24–8. doi: 10.3102/0013189x035006024. [DOI] [Google Scholar]
- 18.Sullivan AL, Bal A. Disproportionality in special education: effects of individual and school variables on disability risk. Except Child. 2013;79(4):475–94. doi: 10.1177/001440291307900406. [DOI] [Google Scholar]
- 19.Ng QX. A systematic review of the use of bupropion for attention-deficit/hyperactivity disorder in children and adolescents. J Child Adolesc Psychopharmacol. 2017;27(2):112–6. doi: 10.1089/cap.2016.0124. [DOI] [PubMed] [Google Scholar]
- 20.Davis CC, Claudius M, Palinkas LA, Wong JB, Leslie LK. Putting families in the center: family perspectives on decision making and ADHD and implications for ADHD care. J Atten Disord. 2012;16(8):675–84. doi: 10.1177/1087054711413077. [DOI] [PubMed] [Google Scholar]
- 21.Krisanaprakornkit T, Ngamjarus C, Witoonchart C, Piyavhatkul N. Meditation therapies for attention-deficit/hyperactivity disorder (ADHD) Cochrane Database Syst Rev. 2010;2010(6):CD006507. doi: 10.1002/14651858.CD006507.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dickstein SG, Bannon K, Castellanos FX, Milham MP. The neural correlates of attention deficit hyperactivity disorder: an ALE meta-analysis. J Child Psychol Psychiatry. 2006;47(10):1051–62. doi: 10.1111/j.1469-7610.2006.01671.x. [DOI] [PubMed] [Google Scholar]
- 23.Brefczynski-Lewis JA, Lutz A, Schaefer HS, Levinson DB, Davidson RJ. Neural correlates of attentional expertise in long-term meditation practitioners. Proc Natl Acad Sci U S A. 2007;104(27):11483–8. doi: 10.1073/pnas.0606552104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grant JA, Duerden EG, Courtemanche J, Cherkasova M, Duncan GH, Rainville P. Cortical thickness, mental absorption and meditative practice: possible implications for disorders of attention. Biol Psychol. 2013;92(2):275–81. doi: 10.1016/j.biopsycho.2012.09.007. [DOI] [PubMed] [Google Scholar]
- 25.Pagnoni G, Cekic M. Age effects on gray matter volume and attentional performance in Zen meditation. Neurobiol Aging. 2007;28(10):1623–7. doi: 10.1016/j.neurobiolaging.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 26.Hölzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspect Psychol Sci. 2011;6(6):537–59. doi: 10.1177/1745691611419671. [DOI] [PubMed] [Google Scholar]
- 27.Jerath R, Edry JW, Barnes VA, Jerath V. Physiology of long pranayamic breathing: neural respiratory elements may provide a mechanism that explains how slow deep breathing shifts the autonomic nervous system. Med Hypotheses. 2006;67(3):566–71. doi: 10.1016/j.mehy.2006.02.042. [DOI] [PubMed] [Google Scholar]
- 28.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huang X, Lin J, Demner-Fushman D. Evaluation of PICO as a knowledge representation for clinical questions. AMIA Annu Symp Proc. 2006;2006:359–63. [PMC free article] [PubMed] [Google Scholar]
- 30.Carsley D, Khoury B, Heath NL. Effectiveness of mindfulness interventions for mental health in schools: a comprehensive meta-analysis. Mindfulness. 2018;9(3):693–707. doi: 10.1007/s12671-017-0839-2. [DOI] [Google Scholar]
- 31.Felver JC, Clawson AJ, Morton ML, Brier-Kennedy E, Janack P, DiFlorio RA. School-based mindfulness intervention supports adolescent resiliency: a randomized controlled pilot study. Int J Sch Educ Psychol. 2019;7(Suppl 1):111–22. doi: 10.1080/21683603.2018.1461722. [DOI] [Google Scholar]
- 32.Zoogman S, Goldberg SB, Hoyt WT, Miller L. Mindfulness interventions with youth: a meta-analysis. Mindfulness. 2015;6(2):290–302. doi: 10.1007/s12671-013-0260-4. [DOI] [Google Scholar]
- 33. Farsi A, Pirian F. The effect of perceptual -motor training and mindfulness on performance and working memory in children with attention deficit hyperactivity disorder. Sport Psychol Stud. 2023. 10.22089/spsyj.2020.8905.1961 [DOI]
- 34.Siebelink NM, Bögels SM, Boerboom LM, de Waal N, Buitelaar JK, Speckens AE, et al. Mindfulness for children with ADHD and mindful parenting (MindChamp): protocol of a randomised controlled trial comparing a family mindfulness-based intervention as an add-on to care-as-usual with care-as-usual only. BMC Psychiatry. 2018;18(1):237. doi: 10.1186/s12888-018-1811-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Boxmeyer CL, Miller S, Romero DE, Powell NP, Jones S, Qu L, et al. Mindful coping power: comparative effects on children’s reactive aggression and self-regulation. Brain Sci. 2021;11(9):1119. doi: 10.3390/brainsci11091119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Klatt M, Harpster K, Browne E, White S, Case-Smith J. Feasibility and preliminary outcomes for Move-Into-Learning: an arts-based mindfulness classroom intervention. J Posit Psychol. 2013;8(3):233–41. doi: 10.1080/17439760.2013.779011. [DOI] [Google Scholar]
- 37.Saxena K, Verrico CD, Saxena J, Kurian S, Alexander S, Kahlon RS, et al. An evaluation of yoga and meditation to improve attention, hyperactivity, and stress in high-school students. J Altern Complement Med. 2020;26(8):701–7. doi: 10.1089/acm.2020.0126. [DOI] [PubMed] [Google Scholar]
- 38.Sprengel M, Fritts M. Sprengel M, Fritts MOA1302Utilizing mind-body practices in public schools: teaching self-regulation skills and fostering resilience in our next generation. BMC Complement Altern Med. 2012;12(Suppl 1):O50. doi: 10.1186/1472-6882-12-s1-o50. [DOI] [Google Scholar]
- 39. Willenbrink JB. Effects of a Mindfulness-Based Program on Children’s Social Skills, Problem Behavior, and Emotion Regulation [dissertation]. Milwaukee, WI: University of Wisconsin-Milwaukee; 2018.
- 40.Hayes SC, Levin ME, Plumb-Vilardaga J, Villatte JL, Pistorello J. Acceptance and commitment therapy and contextual behavioral science: examining the progress of a distinctive model of behavioral and cognitive therapy. Behav Ther. 2013;44(2):180–98. doi: 10.1016/j.beth.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Murrell AR, Steinberg DS, Connally ML, Hulsey T, Hogan E. Acting out to ACTing on: a preliminary investigation in youth with ADHD and co-morbid disorders. J Child Fam Stud. 2015;24(7):2174–81. doi: 10.1007/s10826-014-0020-7. [DOI] [Google Scholar]
- 42.Petts RA, Duenas JA, Gaynor ST. Acceptance and commitment therapy for adolescent depression: application with a diverse and predominantly socioeconomically disadvantaged sample. J Contextual Behav Sci. 2017;6(2):134–44. doi: 10.1016/j.jcbs.2017.02.006. [DOI] [Google Scholar]
- 43.Bronfenbrenner U. Toward an experimental ecology of human development. Am Psychol. 1977;32(7):513–31. doi: 10.1037/0003-066x.32.7.513. [DOI] [Google Scholar]
- 44.McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15(4):351–77. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. PubMed, Web of Science, PsychInfo, Embase, and Cochrane Review keywords, MeSH terms, and search results


