Abstract
Background
In Burkina Faso, only 70% of people living with HIV knew their status in 2018, while the first 95 target of the UNAIDS suggests that by 2025 at least 95% of people living with HIV (PLHIV) know their HIV status. Female sex workers (FSW) are one of the most HIV-vulnerable groups, making it crucial to estimate the rate and associated factors of HIV testing among FSW.
Methods
We conducted a cross-sectional study focused on FSW in five main cities of Burkina Faso (Ouagadougou, Bobo-Dioulasso, Koudougou, Tenkodogo, and Ouahigouya). A respondent-driven sampling (RDS) approach was used to recruit participants. Data were collected through in-person interviews between June and August 2022. The HIV testing rate in the past twelve months was examined by sociodemographic characteristics and risky behaviors. A modified Poisson regression in a generalized estimating equation with an exchangeable correlation structure was used to explore the associated factors of HIV testing.
Results
Of 1338 FSW (average age: 27.6 ± 7.25 years) HIV negative, 57.8% (95% CI: 54.2–61.3) reported having been tested for HIV in the last 12 months. Among those who started sex work before the age of 18, 48.0% (95% CI: 39.1–57.1) reported having been tested for HIV in the last 12 months. The HIV testing rate among FSWs within the last 12 months was independently associated with age, education level, and being member of an FSW supportive association. Indeed, FSW aged 25 years and more had a 14% higher rate of being tested for HIV within 12 months compared to those 15 to 24 years old (adjusted prevalence ratio (aPR): 1.14 [95%CI: 1.05–1.24]). The HIV testing rate among those who are not members of an FSW supportive association was 16% lower (aPR: 0.84 [95%CI: 0.72–0.97]) than those who are members of FSW supportive associations.
Conclusion
The HIV testing rate among FSW is low in Burkina Faso, suggesting an important challenge to reach the first 95% target of UNAIDS among FSW. Innovative diagnostic strategies for the early identification of HIV-infected FSW are essential to achieve the first 95 target by 2025 in Burkina Faso.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-19977-7.
Keywords: Female sex workers, HIV testing, Rate, Burkina Faso
Background
Early diagnosis is a global public health priority to control the HIV epidemic. Key populations including female sex workers (FSW), men who have sex with men (MSM), female transgenders (FTG), people who use injectable drugs (PUID), and prisoners, have a higher vulnerability to HIV compared to the general population [1]. In 2022, nearly 55% of new HIV infections among adults occurred in key populations and their partners [2]. HIV risk is 30 times greater in FSW than in other adult women [3]. Globally, new infections among FSW accounted for 7.7% of adult new infections [2]. This proportion remained stable between 2010 and 2022 [2]. Adolescent and youth FSW (15–19 years of age) significantly contribute to HIV new infection in sub-Saharan Africa. They represent 1.3% of the population but 10.6% of new infections [4]. Nearly half of new HIV infections are undiagnosed. While, WHO recommends HIV testing at least once a year for key populations to reach those with undiagnosed HIV as early as possible to engage them in prevention, treatment, and care [5].
Many barriers to HIV testing among FSW have been identified. Indeed, the systematic review by Tokar et al. [6] in 2018 showed that these barriers include the direct and indirect cost of HIV testing, stigma regarding FSW and HIV status, low perceived risk, and poor HIV knowledge. Stigmatization and discrimination by health professionals were identified as factors explaining why FSW missed the opportunity to go for routine HIV testing in health centers [7, 8]. The main facilitator of HIV testing among FSW was social support [6].
Like other sub-Saharan African (SSA) countries, Burkina Faso aims to end HIV transmission by 2030, which suggests zero HIV transmission in the country by 2030. The HIV prevalence has significantly decreased in the general population these recent years, from 7.17% in 1997 to 0.6% in 2021 [9]. However, the HIV epidemic is still concentrated among key populations that significantly contribute to the new HIV infection in the country. Many studies have reported a higher HIV prevalence among key populations like FSW. Indeed, Traoré et al. [10] reported in 2016 an HIV prevalence of 10.3% among professional FSW and 6.5% among part-time FSW, with only 6.5% being aware of their status. In 2017, Ouedraogo et al. [11] reported an HIV prevalence ranged from 13.0% in the city of Ouahigouya to 30.1% in Bobo Dioulasso, suggesting an increasing prevalence of HIV among this population. Halland et al. [12] showed in 2013 a low coverage of HIV services among key populations, including FSW in Burkina Faso. None of these studies have focused on HIV testing, while according to the report, only 70% of people living with HIV knew their status in 2018, which is far from the first goal of the UNAIDS cascade of care (95-95-95) [13–15]. Among the general population in Burkina Faso, Kirakoya-Samadoulougou et al. [16] showed a low coverage of HIV testing, close to 36% among women 15–49 years old. Studies in SSA showed a suboptimal uptake of HIV testing among FSW. Indeed, Mizinduka et al. [17] reported that 65.3% of FSW have been tested for HIV within the past 12 months in Tanzania. This proportion was 86% among FSW in Uganda, according to Muhindo et al. [18]. In the context of SSA, studies showed that HIV prevention strategies that aimed to remove some barriers to HIV testing, like risk perception, improving health education, peer education, and mitigating stigma regarding HIV and sex work, might help to significantly reduce the HIV incidence among FSW [17]. Our study aimed to estimate the HIV testing rate and its associated factors among FSW in Burkina Faso, to guide public health policy. This study might be essential to monitor progress toward reaching the first 95% and the elimination of HIV transmission by 2030.
Methods
Study setting
The study covered five cities in the country: Ouagadougou, Bobo-Dioulasso, Koudougou, Tenkodogo, and Ouahigouya. The cities were selected according to geographical disparities in HIV prevalence, cultural variation, and the crowd of sexual activities in these cities.
Study type and period
We conducted a cross-sectional study between June and August 2022. The survey took place at the same moment in each city. This study was based on a respondent-driven sampling method, which is among the best methods to reach hidden populations like FSW [19, 20].
Study population
The study population was FSW living in the five study towns, with at least 15 years old. Female sex workers are defined as girls and women who receive money or other gifts in exchange for sexual services, either regularly or occasionally. The inclusion criteria were: (i) being female at birth, 15 years old and above; (iii) using sex as the main income source in the last 12 months; (iii) having a valid coupon for the study (except seeds recruited by the investigators); (iv) being able to give valid consent; and (v) consenting to participate in the study. FSW with 15 years old were included in this study since a previous study showed that nearly one third of FSW in Burkina Faso started the sex work as minors [21]. FSWs with mental incapacity or any other disability that did not allow understanding of the study procedures were not included. For this analysis, we also exclude FSW living with HIV (who tested positive for HIV during the survey), since the HIV positive status might influence their HIV testing behavior. Furthermore, for those who know their HIV status, HIV testing is no longer useful.
Sample size and sampling
The following formula is used to determine the sample size according to a cross-sectional approach using the RDS method as proposed by Salganik [22].
 |
where:
n = sample size.
Deff = cluster effect.
Pa = prevalence of HIV shown by previous study [11].
SE: Standard Error of Pa which was set at 3% for Ouagadougou and 5% for other towns;
The sample size was estimated to be 1424; 578 of which was for Ouagadougou, the capital of Burkina Faso, 370 for Bobo-Dioulasso, the second biggest city, 203 for Koudougou, 203 for Ouahigouya, and 74 for Tenkodogo. Two seeds known as FSW leaders in their respective communities were the first to be recruited in each city. After being trained, a maximum of three coupons were given to each of the seeds in charge of recruiting other FSW. Each FSW recruited is given the possibility to recruit a maximum of three peers. Each coupon had a unique number that identified each person recruited, to avoid double inclusion in the survey.
Data collection
Data were collected through a behavioral survey followed by HIV testing after pre-test counseling. Behavioral data were collected during face-to-face interviews. The interview started by checking the eligibility criteria. Data collection started with seeds that were non-randomly selected with the contribution of community facilitators and key population associations. The first interview was conducted with the seeds in each city. Three coupons were given to each seed to invite the next participants. Each participant also received three coupons to invite new participants until the sample size was reached in each city. Data collectors were trained to ensure the quality of the data and respect of the inclusion process. Data were collected using a structured questionnaire programmed on a digital tablet using the CSPro application for electronic data collection. After the face-to-face interview using a behavioral questionnaire, the participant was invited for a rapid diagnostic test (RDT) for HIV.
Study variables
The outcome variable in the study is HIV testing in the past 12 months. Participants had to answer three successive questions. The first one was; “Have you ever been tested for HIV?”. The response was “yes” or “no”. If “yes”, the participant was invited to answer the second question, “If yes, when was the last time you were tested for HIV?” (see questionnaire in supplementary file). The responses were 1 “in the last 3 months”, 2 “more than 3 months ago and less than 6 months ago”, 3 “more than 6 months ago and less than a year (12 months) ago” and 4 “more than a year ago”. The third was “the last time you were tested for HIV, did you receive your test results?”. The response was “yes” or “no”. The outcome variable was treated as a binary variable by combining the three questions: FSW who reported HIV testing in the last 12 months and received their result (code = 1) versus other possibilities (code = 0).
The independent variables in the study included demographic and socio-economic variables, behavioral factor variables, and variables on HIV knowledge. For this analysis, we use age (15-24 years and 25 years and more), current marital status, educational level, monthly income (Dollars), age at first sex (< 18 and ≥ 18 years), age at initiation of sex work (< 18 and ≥ 18 years), history of drug use (Yes/No), condom use at last sex with clients (Yes/No), condom use at last sex with partners (Yes/No), history of previous incarceration in the last 12 months (Yes/No), lifetime history of alcohol consumption (Yes/No), lifetime history of drug use (Yes/No), HIV knowledge as defined by UNAIDS (Sufficient/Non-sufficient), number of biological children (none, one, two or three, more than three), membership in an FSW supportive association (Yes/No).
Data processing and analysis
The data collected using digital tablets and the application designed on CSPro were transferred to the STATA software for processing and analysis. The analysis was made using the Stata software, and all analyses were adjusted according to the RDS method. We estimated the rate of FSW HIV testing in the past 12 months in two ways; unweighted prevalence and RDS-weighted prevalence. For each way, a confidence interval was calculated and presented to different subgroups of demographics and risk behaviors. To identify associated factors of HIV testing in the last 12 months among female sex workers, we conducted a modified Poisson regression in a generalized estimating equation with an exchangeable correlation structure, as recommended [23]. This model was applied to derive the prevalence ratio and its confidence intervals. Variables with p-value < 0.25 in the bivariate modified Poisson regression were retained for the multivariate regression. All statistical tests were considered significant when p-value < 5%.
Results
Participants’ characteristics
A total of 1425 FSW were recruited in the study; 87 of them were HIV-positive. Finally, 1338 HIV-negative FSW were included in this analysis. Most of them (40.8%) were recruited in Ouagadougou (546 FSW), 25.4% in Bobo-Dioulasso (340 FSW), 14% in Koudougou (187 FSW), 14.1% in Ouahigouya (188 FSW), and 5.8% in Tenkodogo (77 FSW). Nearly one-quarter (23.2%) of FSW were illiterate, 26.2% had attended primary school, and 50.7% had attended at least secondary school. Up to 11.4% of them had their first sex intercourse before 15 years old, 61.7% between 15 and 18 years old, and 26.9% after 18 years old. In all, 13.5% of FSW started the sex work before they turned 18.
Prevalence of HIV testing
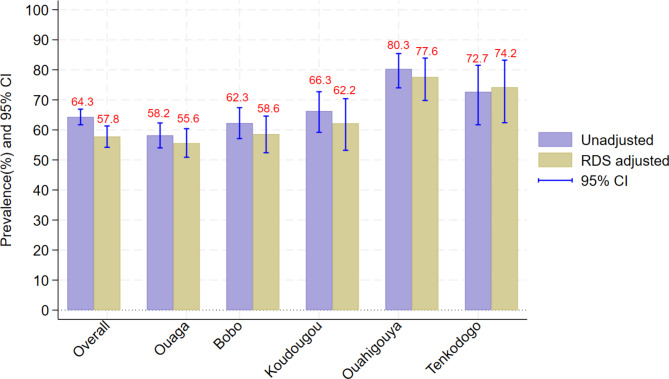
Among the 1338 FSW included in this study, 861 reported HIV testing in the last 12 months, which corresponds to an RDS-adjusted rate of 57.8% (95% IC: 54.2–61.3). As shown in Fig. 1, the RDS-adjusted rate of HIV testing in the last 12 months varied across the towns. It was 55.6% (95%CI: 50.9–60.4) in Ouagadougou, 58.6% (95% CI: 52.4–64.6) in Bobo-Dioulasso, 62.2% (95% CI: 53.2–70.4) in Koudougou, 77.6% (95% CI: 69.8–83.9) in Ouahigouya, and 74.2% (95% CI: 62.4–83.2) in Tenkodogo.
Fig. 1.
HIV testing rate in the last 12 months by study site
Table 1 shows HIV testing rate in the last 12 months for FSW by subgroups of sociodemographic and risk behavior characteristics in Burkina Faso. HIV testing rate is slightly higher among FSW who are married or divorced (60.3% (95% CI: 37.4–79.4) or 65.6% (95% CI: 58.8–71.9)), and illiterate (65.4% (95% CI: 58.1–72.0)). The HIV testing rate in the last 12 months of FSW who are members of an association and those who have a history of previous incarceration in the last 12 months was respectively 76.3% (95%CI:63.6-85.6) and 88.7% (95%CI: 58.0-97.8).
Table 1.
HIV testing in the last 12 months among FSW by socio-demographic and risk behavior characteristics in Burkina Faso
| Variable | Total | n | Unweighted rate (95%CI) | RDS weighted rate (95%CI) |
|---|---|---|---|---|
| Overall | 1338 | 861 | 64.3 (61.7–66.9) | 57.8 (54.2–61.3) |
| Age (years) | ||||
| 15–24 | 529 | 291 | 55.0 (50.7–59.2) | 48.3 (42.7–53.9) |
| 25years and more | 809 | 570 | 70.4 (67.2–73.5) | 63.9 (59.4–68.2) |
| Current marital status | ||||
| Single | 970 | 611 | 63.0 (59.9–66.0) | 55.3 (51.2–59.4) |
| Married | 30 | 17 | 56.7 (38.8–72.9) | 60.3 (37.4–79.4) |
| Divorced. Widowed | 338 | 233 | 68.9 (63.8–73.6) | 65.6 (58.8–71.9) |
| Educational level | ||||
| Illiterate | 310 | 219 | 70.6 (65.3–75.4) | 65.4 (58.1–72.0) |
| Primary school | 350 | 224 | 64.0 (58.8–68.9) | 56.4 (49.6–63.0) |
| Secondary or high school | 678 | 418 | 61.6 (57.9–65.2) | 54.7 (49.7–59.7) |
| Monthly income (dollars) | ||||
| < 175 | 372 | 215 | 57.8 (52.7–62.7) | 52.3 (45.7–58.8) |
| 175–350 | 454 | 295 | 65.0 (60.5–69.2) | 56.7 (50.4–62.8) |
| 350 and more | 512 | 351 | 68.6 (64.4–72.4) | 63.3 (57.7–68.6) |
| Age at first sex (years) | ||||
| < 18 | 744 | 474 | 63.7 (60.2–67.1) | 57.0 (52.3–61.6) |
| >=18 | 594 | 387 | 65.2 (61.2–68.9) | 58.8 (53.4–64.0) |
| Age at commencement of sex work (years) | ||||
| < 18 | 181 | 96 | 53.0 (45.7–60.2) | 48.0 (39.1–57.1) |
| >=18 | 1157 | 765 | 66.1 (63.3–68.8) | 59.7 (55.8–63.4) |
| History of injection drug use (ever) | ||||
| Yes | 11 | 7 | 63.6 (33.8–85.7) | 55.9 (22.8–84.5) |
| No | 1324 | 854 | 64.5 (61.9–67.0) | 58.0 (54.4–61.5) |
| Condom use at last sex with client | ||||
| Yes | 1130 | 737 | 65.2 (62.4–67.9) | 57.9 (54.1–61.8) |
| No | 74 | 44 | 59.4 (47.9–70.0) | 50.2 (36.4–64.1) |
| Condom use at last sex with partner | ||||
| Yes | 1099 | 722 | 58.2 (51.8–64.3) | 50.1 (41.9–58.3) |
| No | 239 | 139 | 65.7 (62.8–68.4) | 59.5 (55.6–63.3) |
| History of previous incarceration in last 12 months | ||||
| Yes | 13 | 11 | 84.6 (54.9–96.1) | 88.7 (58.0-97.8) |
| No | 1321 | 850 | 64.3 (61.7–66.8) | 57.8 (54.2–61.3) |
| Lifetime history of alcohol consumption | ||||
| Yes | 819 | 545 | 66.5 (63.2–69.7) | 59.3 (54.8–63.7) |
| No | 519 | 316 | 60.9 (56.6–65.0) | 55.4 (49.7–60.9) |
| Lifetime history of drug use | ||||
| Yes | 101 | 69 | 68.3 (58.6–76.6) | 62.7 (49.7–74.1) |
| No | 1237 | 792 | 64.0 (61.3–66.6) | 57.4 (53.7–61.0) |
| HIV knowledge | ||||
| Sufficient | 303 | 190 | 62.7 (57.1–68.0) | 56.3 (48.5–63.8) |
| Insufficient | 1035 | 671 | 64.8 (61.9–67.7) | 58.2 (54.2–62.1) |
| Number of biological children | ||||
| None | 441 | 245 | 55.5 (50.9–60.1) | 48.5 (42.4–54.5) |
| One child | 421 | 286 | 67.9 (63.3–72.2) | 60.4 (53.9–66.6) |
| Two or three | 384 | 271 | 70.6 (65.8–74.9) | 66.6 (60.2–72.5) |
| More than three | 92 | 59 | 64.1 (53.9–73.2) | 58.3 (44.6–70.8) |
| Membership in an FSW supportive association | ||||
| Yes | 104 | 82 | 78.8 (69.9–85.7) | 76.3 (63.6–85.6) |
| No | 1234 | 779 | 63.1 (60.4–65.8) | 56.5 (54.2–61.3) |
Associated factors of HIV testing
Table 2 shows the results of modified Poisson regression on HIV testing in the last 12 months among FSW in Burkina Faso. HIV testing among FSW was associated with age, education level, monthly income, history of incarceration, and membership in an FSW supportive association. FSW aged 25 years old and more had a 14% higher rate of HIV testing, as compared to less than 25 years (adjusted prevalence ratio (aPR): 1.14 [95%CI: 1.05–1.24], p = 0.003). The HIV testing rate for those who completed primary school was significantly lower (aPR: 0.89 [95%CI: 0.80–0.98], p = 0.022) compared to those who are illiterate. The HIV testing rate among FSW who completed secondary school was also lower (aPR: 0.89 [95% CI: 0.79–0.99], p = 0.044) as compared to the illiterate. Additionally, membership in an FSW supportive association appears to facilitate HIV testing for female sex workers. The HIV testing rate among those who are not members of an association is significantly lower, by a factor of 0.16, as compared to those who are members of FSW associations.
Table 2.
Factors associated with HIV testing in the last 12 months among FSW in Burkina Faso
| Variable | Crude PR [95%CI] | p | Adjusted PR [95%CI] | p |
|---|---|---|---|---|
| Age (years) | ||||
| 15–24 | 1 | 1 | ||
| 25 and more | 1.32 [1.20–1.46] | < 0.001 | 1.14 [1.05–1.24] | 0.003 |
| Current marital status | ||||
| Single | 1 | 1 | ||
| Married | 1.07 [0.72–1.60] | 0.728 | 1.05 [0.71–1.55] | 0.814 |
| Divorced. Widowed | 1.19 [0.98–1.44] | 0.064 | 1.07 [0.84–1.37] | 0.593 |
| Educational level | ||||
| Illiterate | 1 | 1 | ||
| Primary school | 0.86 (0.79–0.95) | 0.003 | 0.89 [0.80–0.98] | 0.022 |
| Secondary or high school | 0.84 (0.75–0.93) | 0.001 | 0.89 [0.79–0.99] | 0.044 |
| Monthly income (dollars) | ||||
| < 175 | 1 | 1 | ||
| 175–350 | 1.09 [0.88–1.34] | 0.433 | 1.10 [0.90–1.35] | 0.343 |
| 350 and more | 1.22 [1.03–1.42] | 0.018 | 1.26 [1.06–1.50] | 0.010 |
| Age at first sex (years) | ||||
| < 18 | 1 | |||
| >=18 | 1.03 [0.90–1.17] | 0.662 | ||
| Age at commencement of sex work (years) | ||||
| < 18 | 1 | 1 | ||
| >=18 | 1.24 [1.09–1.42] | 0.001 | 1.14 [0.99–1.31] | 0.069 |
| History of injection drug use (ever) | ||||
| Yes | 1 | |||
| No | 1.02 [0.51–2.06] | 0.948 | ||
| Condom use at last sex with client | ||||
| Yes | 1 | |||
| No | 0.86 [0.64–1.14] | 0.300 | ||
| Condom use at last sex with partner | ||||
| Yes | 1 | 1 | ||
| No | 1.18 [0.99–1.41] | 0.061 | 1.14 [0.95–1.36] | 0.152 |
| History of previous incarceration in last 12 months | ||||
| Yes | 1 | 1 | ||
| No | 0.67 [0.55–0.82] | < 0.001 | 0.73 [0.57–0.94] | 0.014 |
| Lifetime history of alcohol consumption | ||||
| Yes | 1 | 1 | ||
| No | 0.93 [0.83–1.04] | 0.183 | 0.97 [0.87–1.06] | 0.476 |
| Lifetime history of drug use | ||||
| Yes | 1 | |||
| No | 0.93 [0.76–1.13] | 0.457 | ||
| HIV knowledge | ||||
| Sufficient | 1 | |||
| Insufficient | 1.03 [0.92–1.15] | 0.580 | ||
| Number of biological children | ||||
| Neither | 1 | 1 | ||
| One child | 1.25 [1.11–1.40] | < 0.001 | 1.15 [0.98–1.34] | 0.078 |
| Two or three | 1.38 [1.19–1.60] | < 0.001 | 1.18 [0.93–1.49] | 0.167 |
| More than three | 1.19 [0.97–1.45] | 0.091 | 0.98 [0.75–1.28] | 0.906 |
| Membership in an FSW supportive association | ||||
| Yes | 1 | 1 | ||
| No | 0.76 [0.65–0.87] | < 0.001 | 0.84 [0.72–0.97] | 0.019 |
Discussion
Keys findings
To the best of our knowledge, this is the first study focused on HIV testing among FSW in the context of Burkina Faso, as many other SSA countries have subscribed to the target 95-95-95 of UNAIDS. From this target, it is expected that by 2025, 95% of people living with HIV will know their status [24]. To reach this target, it is recommended that key populations like FSW be tested for HIV at least once within 12 months for early HIV diagnosis. Our study showed that only 57.8% of FSW were testing for HIV in the past 12 months before the survey. The main associated factors of HIV testing were age, education level of FSW, monthly income, history of previous incarceration in last 12 months and being a member of the FSW association.
HIV testing rate
In our study, only half of FSW was tested for HIV during the last 12 months. This proportion seems to be very low and does not meet the WHO recommendation for HIV testing among the key population. Indeed, WHO recommended an HIV test every 6 to 12 months among FSW [5]. A previous study conducted in 2013 in Burkina Faso using RDS methods reported an HIV testing rate among FSW of 36.4% in Ouagadougou and 64.4% in Bobo-Dioulasso, the country’s two major cities [25]. In Tanzania, Mizinduko et al. [17] reported that 65.3% of FSW tested for HIV in the past 12 months. In Iran, studies reported a decreasing prevalence of HIV testing among FSW (70.1% in 2015 and 44.7% in 2020) [26, 27]. Indeed, Tavakoli et al. [26] reported in 2020 a HIV testing rate within the last 12 months of 44.7%, which seems to be lower, as the authors stated, than those reported in 2015 by Shokoohi et al. [27] (70.1%). However, a higher rate of HIV testing has been reported in other studies. Indeed, Muhindo et al. [18] reported that the rate of HIV testing in the previous 12 months was 86% among FSW in Uganda in 2020. This high rate seems to be due to an HIV testing-specific program targeting FSW in Uganda [18, 28, 29]. Abdella et al. [3] noted that 89.6% of FSW who participated in their study conducted in 2022 in Ethiopia have been tested for HIV. These results highlighted that it is possible to significantly improve the uptake of HIV testing among FSW by effective specific programs, as shown in other studies [30, 31]. While, we did not explore barriers to HIV testing, previous studies in Burkina Faso indicate many barriers to HIV testing among FSW have been identified, and these include transportation costs, time constraints, formal/informal payments, stigma, and discrimination towards sex workers and HIV-positive people [6, 25]. Our results suggest an important gap in HIV testing among FSW in Burkina Faso despite the ongoing national policy to reduce the burden of HIV infection in the country. Indeed, the current national strategy drafted in 2021 aimed to reduce new HIV infections by 75% by 2025 [32]. To reach this goal, it is expected that 95% of the key populations, including FSW, use the package of HIV prevention services, which include community-based testing, self-testing, testing in health facilities, and other prevention strategies like condoms and lubricant used, behavior change Interventions, and pre-exposure prophylaxis [32]. As highlighted by Nnko et al. [33], there are many factors that might facilitate HIV prevention services, including the use of HIV testing. These factors are: awareness of the availability of HIV prevention services, and perception of the high quality of HIV prevention services, including ensuring confidentiality and the removal of some barriers regarding HIV stigma and fear of discrimination due to community intolerance of sex work.
Factors associated with HIV testing
This study found that HIV testing among FSW was significantly associated with age, education level, history of incarceration, monthly income, and being a member of the FSW association. Indeed, our study found that lower education was associated with higher HIV testing. As shown in Tokar et al.’s systematic review [6], the association between the education level of FSW and HIV testing is discussed in the literature. Indeed, studies reported that FSW with high education levels were more likely to be tested for HIV [18]. Others found no difference between FSWs with high education and those with low education [26, 34]. In Burkina Faso, Traore et al. [10] noted that higher education level was associated with higher HIV risk behavior, which could have suggested a higher HIV testing among FSW with higher education since HIV testing seems to increase with the self-perceived risk [18]. In our study, it was not possible to adjust the model by self-perceived HIV risk, while it is known that self-perceived risk is an important factor in the uptake of HIV testing [35]. Our results might be explained by the fact that some sites of sex work known are frequented mainly by uneducated women. In these sites HIV testing is often conducted by HIV associations. While the FSW with a high level of education might be in luxury sex work and they do not want to disclose their activity. Nevertheless, more studies are needed to understand the link between FSW education and their uptake of HIV testing.
HIV testing was higher among older FSW compared to the youth. A similar finding was reported by Muhindo et al. [18]. This is due to the multiple vulnerabilities of young FSW, including lower access to HIV-related services [36]. As shown in other contexts [34], our study reported that FSW with higher levels of income were more likely to be tested for HIV compared to FSW with a lower level of income. There are other factors known to be associated with HIV testing. In Tanzania, Mizinduko et al. noted that the main factors of HIV testing among FSW were: condom use on the last day worked, self-perceived risk of HIV infection, stigmatization regarding the sex work, and peer education [17]. Stigmatization regarding sex work and HIV-positive people is among the leading factors in the low HIV testing rate among FSW. Peer-based prevention and social support are known to improve HIV testing among this specific population [31]. In our study we found that the membership of an FSW supportive association increased the HIV testing rate. Policymakers have to pay more attention to these factors in drafting specific interventions, in order to address the low rate of HIV testing among FSW. Motherhood in our study was not significantly associated with HIV testing among FSW after adjusting for other variables. While previous study showed that FSW who are mothers were more likely to be included in the HIV continuum of care since most of them seek antenatal/perinatal services in which HIV testing is highly recommended [37]. In the same order, a previous study of HIV risk relating to pregnancy conception desire showed that there was no difference between FSW who were trying to conceive (79%) compared to those who were not (82.0%). However, HIV risk was higher among FSW who were trying to conceive, with an HIV prevalence of 24.5% & 17.7% [38]. Integrating HIV prevention services into sexual and reproductive healthcare, contributes to increasing HIV service coverage among FSW [37].
Strengths and limitations of the study
As in other studies on HIV, face-to-face interviews, community intolerance of sex work, and HIV-positive stigma might cause social desirability bias in this study even if data collectors were well trained to avoid this bias. Since we collected information regarding HIV testing in the past 12 months, it might result in a recall bias. The survey was conducted in five cities of the country, and participants were recruited using the RDS approach; therefore, the results presented in this study might not be generalizable to all the FSW in the country. Some factors like self-perceived risk known to be associated with HIV testing, which might help us to better adjust the multivariate model, were not collected. Furthermore, this study has not explored barriers related to HIV testing which could be a limitation to understanding some factors associated, like the education of FSW. We might not have made causal inferences in this study due to its cross-sectional design. However, the RDS approach used in this study is among the best approaches to recruit participants from hidden populations like FSW [20, 39].
Conclusion
This study shows an important gap regarding HIV testing among FSW in Burkina Faso. Many factors have been identified to be associated with this lower rate of HIV testing among FSW. In the context of the ongoing national HIV prevention strategy, which aims to reduce new HIV infections by 75% by 2025, it is urgent to reinforce specific HIV prevention packages including community-based testing, self-testing to improve the HIV testing rate among FSW.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
Authors acknowledge the Secretariat permanent du Conseil national de lute contre le SIDA et les Infections sexuellement transmissibles (SP/CNLS-IST) of Burkina Faso, the Global Fund for Malaria, Tuberculosis, and HIV, the key population leaders and their organizations (Yerelon + in Ouagadougou; Yerelon in Bobo-Dioulasso; ACTI-PLUS in Koudougou; AMMIE in Ouahigouya and AJVLS in Tenkodogo) and study participants.
Abbreviations
- FSWs
Female sex workers
- HTC
HIV testing and counseling
- MSM
Men who have sex with another men
- PLHIV
People living with HIV
- RDS
Respondent-driven sampling
- SSA
Sub-Saharan Africa
- UNAIDS
Joint United Nations Programme on HIV/AIDS
- WHO
World Health Organization
Author contributions
KC, HGO, and SK conceived and designed the study. KC, HGO drafted the protocol with the input of SK and SZ, and OKZ. KC, HGO, SK, OKZ, SZ, DK, FS, AY, AAO supervised data collection. KC analyzed the data with the contribution of KD and AIO. KC wrote the first draft of the manuscript. HGO, OKZ, DK, SZ, CKT, SD, DLD, FS, AY, AAO, SO, and SK critically reviewed the manuscript. All authors read and approved the final version of this manuscript.
Funding
No funding received.
Data availability
The datasets used during the current study are available from the corresponding author upon reasonable request, with the permission of SP/CNLS-IST of Burkina Faso.
Declarations
Ethics approval and consent to participate
The protocol of this study was approved by the National Ethical Comity for Health Research (Comité d’Ethique pour la Recherche en Santé (CERS)) of Burkina Faso (Deliberation Number 2020-02-029 of February 5, 2020). All participants were given written informed consent before participating in the study. We were aware that for young participants, their parents or legal guardians’ consent was necessary. However, since sex work is stigmatized in Burkina Faso, most parents or legal guardians are not aware that their girls are engaged in female sex work. To guarantee the confidentiality and protect the private life of participants, we did not seek the consent of parents or legal guardians. We explained it in the protocol before submitting it to the National Ethical Committee. We obtained from the National Ethical Committee for Health Research (CERS) of Burkina Faso (Deliberation Number 2020-02-029 of February 5, 2020), a waiver for parental consent for illiterate participants above the age of 16. The National Ethical Committee has recommended the presence of witnesses or legal guardians during the consent process for illiterate participants aged 15 years old. Three participants aged 15 years were recruited. All of them had been to school. Regarding the recommendations of the National Ethical Committee of Burkina Faso, the presence of witnesses or legal guardians was thus not necessary during the consent process for them. All ethical requirements were guaranteed. We obtained ethical approval before starting the data collection.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ochonye B, Folayan MO, Fatusi AO, Bello BM, Ajidagba B, Emmanuel G, et al. Sexual practices, sexual behavior and HIV risk profile of key populations in Nigeria. BMC Public Health. 2019;19:1210. 10.1186/s12889-019-7553-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Korenromp EL, Sabin K, Stover J, Brown T, Johnson LF, Martin-Hughes R et al. New HIV Infections Among Key Populations and Their Partners in 2010 and 2022, by World Region: A Multisources Estimation. J Acquir Immune Defic Syndr. 1999. 2024;95 1 Suppl:e34–45. [DOI] [PMC free article] [PubMed]
- 3.Abdella S, Demissie M, Worku A, Dheresa M, Berhane Y. HIV prevalence and associated factors among female sex workers in Ethiopia, East Africa: a cross-sectional study using a respondent-driven sampling technique. eClinicalMedicine. 2022;51. [DOI] [PMC free article] [PubMed]
- 4.Howes A, Risher KA, Nguyen VK, Stevens O, Jia KM, Wolock TM, et al. Spatio-temporal estimates of HIV risk group proportions for adolescent girls and young women across 13 priority countries in sub-saharan Africa. PLOS Glob Public Health. 2023;3:e0001731. 10.1371/journal.pgph.0001731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Consolidated guidelines on HIV testing services. https://www.who.int/publications-detail-redirect/978-92-4-155058-1. Accessed 12 Mar 2024.
- 6.Tokar A, Broerse JEW, Blanchard J, Roura M. HIV Testing and Counseling among Female Sex workers: a systematic literature review. AIDS Behav. 2018;22:2435–57. 10.1007/s10461-018-2043-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Atuhaire L, Shumba CS, Mapahla L, Maposa I, Nyasulu PS. Factors associated with adherence to HIV testing guidelines among HIV-negative female sex workers in Kampala, Uganda. IJID Reg. 2022;4:25–32. 10.1016/j.ijregi.2022.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nakanwagi S, Matovu JKB, Kintu BN, Kaharuza F, Wanyenze RK. Facilitators and barriers to linkage to HIV Care among female sex workers receiving HIV Testing services at a community-based Organization in Periurban Uganda: a qualitative study. J Sex Transm Dis. 2016;2016:7673014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ministère de la. santé et de l’hygiène publique. Profil du Burkina Faso sur le VIH-IST.
- 10.Traore IT, Hema NM, Sanon A, Some F, Ouedraogo D, Some R, et al. HIV risk and behaviour among part-time versus professional FSW: baseline report of an interventional cohort in Burkina Faso. Sex Transm Infect. 2016;92:550–3. 10.1136/sextrans-2015-052038 [DOI] [PubMed] [Google Scholar]
- 11.Ouedraogo HG, Ky-Zerbo O, Baguiya A, Grosso A, Goodman S, Samadoulougou BC, et al. HIV among Female Sex Workers in five cities in Burkina Faso: a cross-sectional baseline survey to inform HIV/AIDS Programs. AIDS Res Treat. 2017;2017:1–11. 10.1155/2017/9580548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holland CE, Kouanda S, Lougué M, Pitche VP, Schwartz S, Anato S, et al. Using Population-size estimation and cross-sectional survey methods to evaluate HIV Service Coverage among Key populations in Burkina Faso and Togo. Public Health Rep. 2016;131:773–82. 10.1177/0033354916677237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Luong Nguyen LB, Yazdanpanah Y, Maman D, Wanjila S, Freedberg KA. Impact Des interventions impactant la cascade de soin de l’infection VIH et la prophylaxie pré-exposition dans le sud-ouest kenyan. Médecine Mal Infect. 2019;49:S36–7. 10.1016/j.medmal.2019.04.096 [DOI] [Google Scholar]
- 14.Conseil national de lutte contre le sida et les IST. Cadre stratégique national de lutte contre le VIH, le sida et les infections sexuellement transmissibles (CSN-SIDA) 2021–2025. Burkina Faso: Ministère de santé; 2021. [Google Scholar]
- 15.Secrétariat permanent du Conseil national de lutte contre le sida. et les IST, ministère de la sante programme sectoriel sante de lutte contre le sida et les IST. Normes et protocoles de prise en charge médicale des personnes vivant avec le VIH au Burkina FASO. Ministère de santé; 2021.
- 16.Kirakoya-Samadoulougou F, Jean K, Maheu-Giroux M. Uptake of HIV testing in Burkina Faso: an assessment of individual and community-level determinants. BMC Public Health. 2017;17:486. 10.1186/s12889-017-4417-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mizinduko M, Moen K, Pinkowski Tersbøl B, Likindikoki SL, Alexander Ishungisa M, Leyna GH, et al. HIV testing and associated factors among female sex workers in Tanzania: approaching the first 90% target? AIDS Care. 2023;35:850–8. 10.1080/09540121.2021.2014779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Muhindo R, Mujugira A, Castelnuovo B, Sewankambo NK, Parkes-Ratanshi R, Kiguli J, et al. HIV and syphilis testing behaviors among heterosexual male and female sex workers in Uganda. AIDS Res Ther. 2020;17:48. 10.1186/s12981-020-00306-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heckathorn DD, Respondent-Driven Sampling. A New Approach to the study of hidden Populations*. Soc Probl. 1997;44:174–99. 10.2307/3096941 [DOI] [Google Scholar]
- 20.Handcock MS, Gile KJ, Mar CM. Estimating hidden population size using respondent-driven sampling data. Electron J Stat. 2014;8:1491–521. 10.1214/14-EJS923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grosso AL, Ketende S, Dam K, Papworth E, Ouedraogo HG, Ky-Zerbo O, et al. Structural determinants of health among women who started selling sex as minors in Burkina Faso. J Acquir Immune Defic Syndr. 2015;68(Suppl 2):S162–70. 10.1097/QAI.0000000000000447 [DOI] [PubMed] [Google Scholar]
- 22.Salganik MJ. Variance estimation, design effects, and sample size calculations for respondent-driven sampling. J Urban Health. 2006;83(Suppl 1):98–112. [DOI] [PMC free article] [PubMed]
- 23.Selvaraj V, Boopathi K, Paranjape R, Mehendale S. A single weighting approach to analyze respondent-driven sampling data. Indian J Med Res. 2016;144:447–59. 10.4103/0971-5916.198665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.ONUSIDA, THE PATH THAT ENDS, AIDS: UNAIDS GLOBAL AIDS UPDATE. 2023. Geneva: Joint United Nations Programme on HIV/AIDS; 2023.
- 25.Papworth E, Grosso A, Ketende S, Wirtz A, Cange C, Kennedy C, Lebreton M, KyZerbo O, Anato S. and Baral S. Examining Risk Factors for HIV and Access to Services among Female Sex Workers (FSW) and Men who have Sex with Men (MSM) in Burkina Faso, Togo, and Cameroon. 2014.
- 26.Tavakoli F, Moradi G, Mirzazadeh A, Zarei B, Sharifi H. HIV testing and its associated factors among female sex workers in Iran in 2020: finding from a respondent-driven sampling survey. PLoS ONE. 2023;18:e0289307. 10.1371/journal.pone.0289307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shokoohi M, Noori A, Karamouzian M, Sharifi H, Khajehkazemi R, Fahimfar N, et al. Remaining gap in HIV Testing Uptake among female sex workers in Iran. AIDS Behav. 2017;21:2401–11. 10.1007/s10461-017-1844-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.When they. know that you are a sex worker, you will be the last person to be treated: Perceptions and experiences of female sex workers in accessing HIV services in Uganda - PubMed. https://pubmed.ncbi.nlm.nih.gov/28476153/. Accessed 17 Mar 2024. [DOI] [PMC free article] [PubMed]
- 29.Preference and uptake of different community-. based HIV testing service delivery models among female sex workers along Malaba-Kampala highway, Uganda, 2017 - PMC. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6833274/. Accessed 17 Mar 2024. [DOI] [PMC free article] [PubMed]
- 30.Chow EPF, Tung K, Tucker JD, Muessig KE, Su S, Zhang X, et al. Behavioral interventions improve Condom Use and HIV Testing Uptake among Female Sex workers in China: a systematic review and Meta-analysis. AIDS Patient Care STDs. 2015;29:454–60. 10.1089/apc.2015.0043 [DOI] [PubMed] [Google Scholar]
- 31.Traore IT, Meda N, Hema NM, Ouedraogo D, Some F, Some R, et al. HIV prevention and care services for female sex workers: efficacy of a targeted community-based intervention in Burkina Faso. J Int AIDS Soc. 2015;18:20088. 10.7448/IAS.18.1.20088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.CNLS-IST. Cadre stratégique national de lutte contre le VIH, le SIDA et les infections sexuellement transmissibles (CSN-SIDA) 2021–2025. Ouagadougou; 2020.
- 33.Nnko S, Kuringe E, Nyato D, Drake M, Casalini C, Shao A, et al. Determinants of access to HIV testing and counselling services among female sex workers in sub-saharan Africa: a systematic review. BMC Public Health. 2019;19:15. 10.1186/s12889-018-6362-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ahmadi S, Khezri M, Roshanfekr P, Karimi SE, Vameghi M, Ali D, et al. HIV testing and its associated factors among street-based female sex workers in Iran: results of a national rapid assessment and response survey. Subst Abuse Treat Prev Policy. 2021;16:43. 10.1186/s13011-021-00382-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pringle K, Merchant RC, Clark MA. Is self-perceived HIV Risk Congruent with reported HIV Risk among traditionally lower HIV Risk and Prevalence Adult Emergency Department patients? Implications for HIV Testing. AIDS Patient Care STDs. 2013;27:573–84. 10.1089/apc.2013.0013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grosso AL, Ketende S, Dam K, Papworth E, Ouedraogo HG, Ky-Zerbo O et al. Structural determinants of health among women who started selling sex as minors in Burkina Faso. J Acquir Immune Defic Syndr. 1999. 2015;68 Suppl 2:S162-170. [DOI] [PubMed]
- 37.Papworth E, Schwartz S, Ky-Zerbo O, Leistman B, Ouedraogo G, Samadoulougou C et al. Mothers who sell sex: a potential paradigm for integrated HIV, sexual, and reproductive health interventions among women at high risk of HIV in Burkina Faso. J Acquir Immune Defic Syndr. 1999. 2015;68 Suppl 2:S154-161. [DOI] [PubMed]
- 38.Schwartz SR, Papworth E, Ky-Zerbo O, Anato S, Grosso A, Ouedraogo HG, et al. Safer Conception needs for HIV Prevention among Female Sex Workers in Burkina Faso and Togo. Infect Dis Obstet Gynecol. 2014;2014:e296245. 10.1155/2014/296245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wejnert C, Pham H, Krishna N, Le B, DiNenno E. Estimating design effect and calculating sample size for Respondent-Driven Sampling studies of Injection Drug users in the United States. AIDS Behav. 2012;16:797–806. 10.1007/s10461-012-0147-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used during the current study are available from the corresponding author upon reasonable request, with the permission of SP/CNLS-IST of Burkina Faso.