Abstract
Abstract
Introduction
The short-term effectiveness of the PRomotion de l’ALIMentation et de l’Activité Physique–INÈgalités de Santé’ (PRALIMAP-INÈS) intervention to reduce social inequalities in overweight and obesity management among adolescents between 2012 and 2015 was demonstrated. This longitudinal mixed-methods study is a 10-year postintervention follow-up of the PRALIMAP-INÈS intervention with the aim of investigating social, economic, educational and health (especially weight) trajectories from adolescence to young adulthood.
Methods and analysis
Among adolescents enrolled in PRALIMAP-INÈS (n=1419), we estimate the number of participants to be 852. Adolescents who were included in the PRALIMAP-INÈS intervention will be contacted 10 years later and invited to participate in a follow-up visit. Participants will self-report their sociodemographic characteristics, body image perceptions, overweight/obesity care pathway, lifestyle and dietary behaviours and attitudes, psychological health and experience of the PRALIMAP-INÈS intervention. A check-up visit will be scheduled by a clinical research nurse to record waist circumference and weight and height for body mass index calculation and to construct the healthcare pathway from adolescence to young adulthood. 40 participants will be invited to participate in a semistructured interview conducted by a sociologist to deepen the understanding of trajectories regarding social aspects that are likely to influence health behaviours in participants.
Ethics and dissemination
The PRALIMAP-CINeCO trial was approved by French Persons Protection Committee (no. 2021-A00949-32) and a conformity declaration was made with French National Commission for Data Protection and Liberties. Results will be presented at conferences and published in international peer-reviewed journals.
Trial registration number
NCT05386017; Pre-results
Keywords: Adolescent, Life Change Events, Obesity, Schools, Follow-Up Studies
STRENGTHS AND LIMITATIONS OF THIS STUDY.
Adolescents who participated in a school-based intervention aimed at reducing social inequalities in overweight and obesity management will be contacted 10 years later when they are young adults.
Social, economic, educational and health determinants of changes in weight status, health behaviours and mental health from adolescence to young adulthood will be assessed.
Identifying, contacting and convincing young adults to participate in this study will be major challenges.
The use of contact information collected during adolescence, study feasibility and support from local media and stakeholders will maximise the chance of reaching participants.
Introduction
Social inequalities in overweight and obesity are strong.1 In France, the latest data show that almost half of the French population was affected by excess weight, with 17% suffering from obesity (body mass index (BMI) ≥30 kg/m2) and 2% suffering from severe and complex obesity (BMI ≥40 kg/m2)2 but the per cent with obesity increases to 24% for individuals in the lowest income category.3 Lifestyle changes involving healthy eating habits, increased physical activity levels and reduced sedentary activity levels are recommended to prevent and treat obesity.4 Adolescence is an important period for the development of new health-related behaviours, with a high probability of these behaviours being maintained in adulthood.5 The onset of these behaviours in adolescence affects the burden of disease in adults and the health and development of their children.6 Interventions to prevent and reduce overweight are not scarce,7 and the school setting is considered a facilitator for implementing prevention programmes and maybe a primary setting for obesity prevention efforts.8 9 In the PRomotion de l’ALIMentation et de l’Activité Physique (PRALIMAP) intervention,10 we showed that a screening and care strategy implemented in the school setting was effective in reducing overweight,11 12 however, social inequalities were identified,13 and there was no evidence that the PRALIMAP universal intervention was effective in reducing socioeconomic inequalities in weight status.14
In this context, the PRomotion de l’ALIMentation et de l’Activité Physique–INÈgalités de Santé (PRALIMAP-INÈS) intervention15 was implemented between 2012 and 2015 and aimed to investigate whether a strengthened management strategy to prevent and reduce overweight could have an effect on adolescents of lower socioeconomic status equivalent to that on adolescents of higher socioeconomic status. The PRALIMAP-INÈS intervention was a mixed, prospective and multicentre intervention including 35 state-run schools. The intervention included adolescents with overweight or obesity, aged 13–18 years for three consecutive academic years. One-year interventions were implemented with data collection before (time 0) and after the intervention (time 1, at the end of the academic year and time 2, 1 year later). The PRALIMAP-INÈS intervention included three arms: (1) standard management (ie, five 2-hour educational sessions) of overweight and obesity for adolescents from higher socioeconomic status, (2) standard management of overweight or obesity for one-third of adolescents from lower socioeconomic status and (3) standard and strengthened management (including, according to adolescents’ needs, motivational interviewing, physical activity equipment, food workshops, specialised hospital management of obesity) of overweight or obesity for two-thirds of adolescents from lower socioeconomic status. The main result—the difference in BMI z-score changes between arms 3 and 1—was a significant reduction in the weight social inequalities by 23.3%.16 In other words, it showed that a school-based socially adapted intervention grounded in the proportionate universalism principle was effective in reducing social inequalities.16 17
These results of the PRALIMAP-INÈS intervention were promising for the short-term effectiveness of interventions aimed at reducing social inequalities in weight status. However, the evidence in the literature highlights the elevated risk of obesity in adulthood18, and of excess and premature morbidity and mortality for adolescents with obesity19 20 and that intervention programmes targeting weight-related behaviours (eg, eating habits and physical activity) had shown no strong evidence of long-term effectiveness.21 The authors of these studies identified a lack of investigations of the maintenance of weight loss into young adulthood or the many psychological or socioenvironmental factors that might be important for successful weight loss.22 The transition from adolescence to adulthood is a key life stage23 and is typically considered to occur between 15–19 years (late adolescence) and 20–24 years (young adulthood) of age,6 characterised by life-changing transitions.24
Overall, psychological, behavioural and socioenvironmental changes from adolescence to young adulthood can progress in unfavourable directions. For example, a literature review25 indicated a decline in physical activity from adolescence to adulthood for boys as well as girls. To further investigate this result, the authors recommended investigating how a change in physical activity is associated with various contemporaneous social transitions. For eating habits, the Norwegian Longitudinal Health Behaviour Study showed that leaving home and leaving educational settings have strong negative associations with eating habits. The authors suggested that further research on the determinants of eating habit changes, disaggregated by sex, is needed to test this hypothesis.26 Few studies, especially in Europe, have investigated BMI trajectories from adolescence to young adulthood or personal, psychological, behavioural and socioenvironmental factors that are hypothesised to play a role.2426,29 In a review, Bates et al reported that none of the included studies reported using psychosocial factors to predict weight trajectories.30 However, the contribution of these factors is essential for identifying unhealthy trajectories at an early stage and diversifying and tailoring potential intervention strategies.
All these elements justify a postintervention investigation of the PRALIMAP-INÈS intervention, to explore social, economic, educational and behavioural preventive and health trajectories31 as well as to explain these trajectories by socioeconomic status and weight status at the age of 15 years.
Methods and analysis
This study protocol follows the Standardised Protocol Items Recommendations Observational Studies checklist (see online supplemental material).
Aims
Primary objective
The primary objective is to evaluate the long-term (after 10 years) effect on BMI in participants of the PRALIMAP-INÈS intervention, a school-based overweight management intervention conducted with adolescents in 2012–2015.
Primary outcome measures
The primary outcome is the change in BMI from the time of inclusion in the PRALIMAP-INÈS intervention to 10 years after inclusion in the PRALIMAP-INÈS intervention.
Secondary objectives
The secondary objectives are as follows:
To describe the sociodemographic and health characteristics of participants.
To describe the care pathway for adolescents related to overweight or obesity and all the major health events occurring from the postintervention period to young adulthood.
To identify the determinants of changes in health and psychosocial characteristics during the transition from adolescence to young adulthood overall and by adolescent characteristics (ie, socioeconomic status and overweight course).
To identify trajectories of health status in adolescence according to the immediate effect of the PRALIMAP-INÈS intervention and according to the change after 10 years.
To deepen the understanding of the trajectories of participants with regard to social aspects that may influence health behaviour.
Secondary outcomes
The secondary outcomes are as follows:
For secondary objectives 1 and 2: Sociodemographic characteristics (age, sex, marital status, family situation, educational level, occupation type) and health characteristics (BMI and BMI z-score, physical activity and sedentary behaviour according to the Global Physical Activity Questionnaire (GPAQ),32 eating habits according to a food frequency questionnaire,33 tobacco and alcohol consumption using ad hoc questionnaire, quality of life using the Quality of life Short Form 12-item (SF12),34 health events, actions taken or medical follow-up related to overweight or obesity and any major events that occurred from the postintervention period to young adulthood;
For secondary objective 3: Changes in characteristics (social (eg, family situation, relationship with family using ad hoc questions), economic (eg, income, financial support using ad hoc questions), psychosocial (ie, coping using the Brief Cope questionnaire,35 self-esteem using the Rosenberg Self-Esteem (RSE) scale,36 emotion regulation using the Difficulties in Emotion Regulation Scale (DERS),37 the quality of life using the SF1234 and health events) and health behaviours (ie, eating habits from a food frequency questionnaire,33 eating disorders using the Eating Attitudes Test-26 (EAT),38 physical activity and sedentary behaviours using the GPAQ,32 temperament in eating and physical activity using self-reported questionnaires,39 alcohol and tobacco consumption and sleep quality using self-reported ad hoc questionnaires) from adolescence to young adulthood overall and according to adolescent characteristics (ie, socioeconomic status measured according to the WHO Family Affluence Scale (FAS)40 and overweight course).
For secondary objective 4: Improved, worsened or stable health characteristics (ie, BMI, weight status, body image perception using the Stunkard’s Figure Rating Scale,41 psychosocial characteristics and health behaviours (as detailed for secondary objective 3) according to the immediate effect of the PRALIMAP-INÈS intervention and according to the change after 10 years.
For secondary objective 5: Analyses of biographical interviews to gain a deeper understanding of participants’ trajectories in terms of social aspects that could influence health behaviours.
Study design
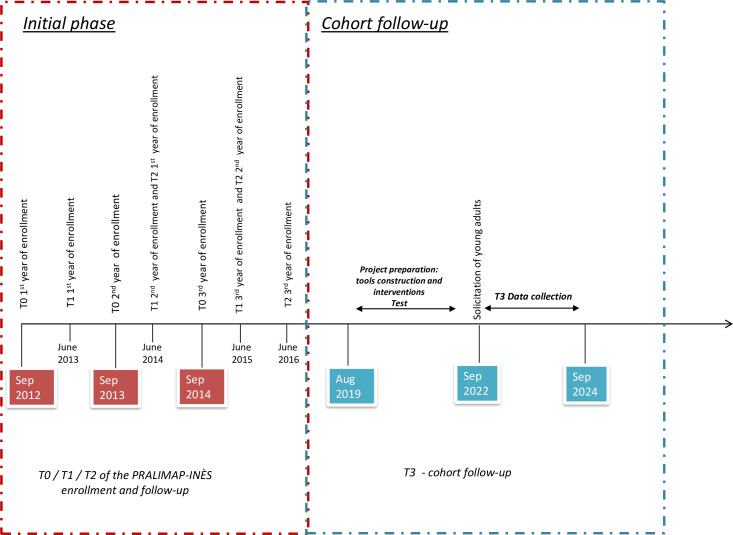
This study consists of a postintervention follow-up of the PRALIMAP-INÈS intervention,15 which was conducted in northeastern France, to describe and compare changes in health characteristics from adolescence to young adulthood. A mixed-methods, longitudinal follow-up study is proposed to investigate long-term social, economic, educational/professional and health (in particular weight) trajectories in adolescents who participated in the PRALIMAP-INÈS intervention. Figure 1 shows the sequence of the initial and postintervention phases. In the initial phase, three measurements were carried out (T0: inclusion; T1: follow-up at the end of the intervention; T2: follow-up 1 year after the end of the intervention). The next measurement time (T3: follow-up 10 years after the end of the intervention) constitutes the core of the present proposal.
Figure 1. Articulation with PRALIMAP-INÈS (initial phase) and PRALIMAP-CINeCO (cohort follow-up). PRALIMAP-CINeCO, PRomotion de l’ALIMentation et de l’Activité Physique–Cohorte INès e-COaching; PRALIMAP-INÈS, PRomotion de l’ALIMentation et de l’Activité Physique–INÈgalités de Santé.
Inclusion criteria
To be enrolled, a participant must:
Have participated in the PRALIMAP-INÈS intervention, and thus was considered eligible for this intervention (with a BMI above the IOTF threshold42 of reduced overweight of 1 kg/m² for age and sex and/or a waist circumference greater than the McCarthy cut-offs for age and sex43 and has completed a medical interview). All participants included in the PRALIMAP-INÈS intervention had given their consent to participate in the PRALIMAP-INÈS intervention.
Be enrolled in or receive social security benefits (ie, social security is the public health insurance system that covers all life risks).
Consent to participate in the T3 follow-up of the PRALIMAP-Cohorte INès e-COaching (CINeCO) study
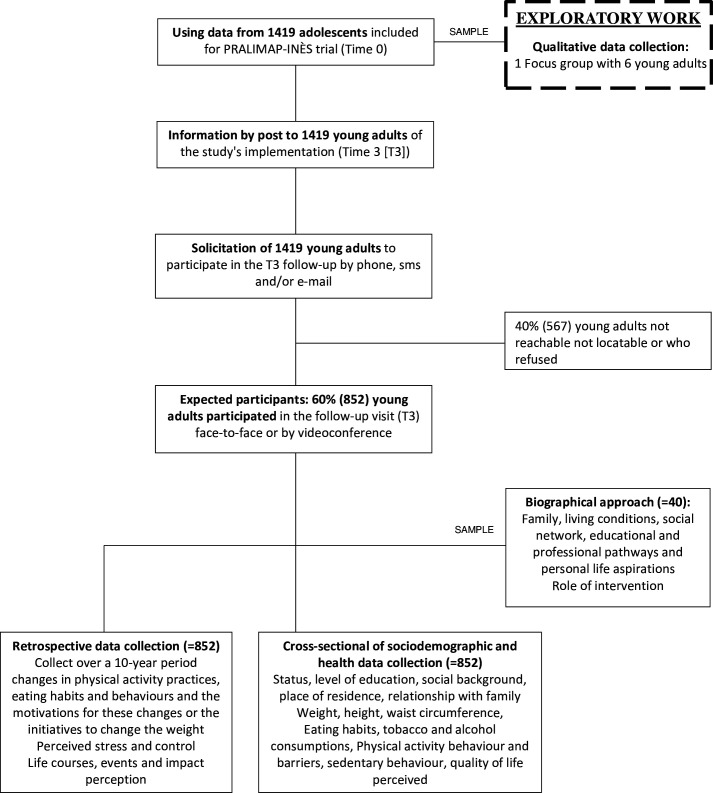
Recruitment
Adolescents who were included in the PRALIMAP-INÈS intervention (ie, n=1419) will be contacted by a clinical research associate or nurse and asked to participate in the study, given information about the process and asked to participate in a follow-up visit (figure 2). We estimated that 40% of adolescents may not be included in the current study (10%: unknown address, 15%: unsuccessfully contacted and 15%: declined to participate). Therefore, the potential number of participants will be 852 (60%). Clinical research associate or nurse will use contact details (home address, phone number, email address and parental address and phone number) and measurements collected during the PRALIMAP-INÈS at T0. Beforehand, an information letter will be sent to the address provided during the PRALIMAP-INÈS intervention to present the study to the participants and inform them that contact will be made. Accurate and regular supervision will be implemented by the research team to coordinate participant contact (who is solicited, who accepts and who declines).
Figure 2. PRALIMAP-CINeCO design. PRALIMAP-CINeCO, PRomotion de l’ALIMentation et de l’Activité Physique–Cohorte INès e-COaching; PRALIMAP-INÈS, PRomotion de l’ALIMentation et de l’Activité Physique–INÈgalités de Santé.
Patient and public involvement: An exploratory focus group with six participants from the PRALIMAP-INÈS intervention helped to define the contact strategy (exploratory work in figure 2). According to the opinions of the participants who participated in the focus group, it will be necessary to use multiple solicitation methods to maximise the success rate (mail, SMS, phone calls, social networks, etc). The focus group participants suggested using their network to mobilise their friends to participate in the follow-up (all of them were still in contact with their classmates) and offering financial incentives to participants. In addition, support from local media (television (TV) news, radio and newspapers) and stakeholders (eg, nurses) will help promote our study and recruit participants. Last, included participants were asked to talk about the study with participants who had participated in the PRALIMAP-INES intervention and with whom they were still in contact (this idea was proposed during the focus group).
Data collection
Training and meetings between the research team and surveyors will be organised before and during data collection to ensure data quality. The online data collection platform will be created and managed by a data manager. The data collected will be deidentified prior to analyses. The unintended effects of the study will be recorded by the study manager. To describe the sociodemographic and health characteristics of the participants, we will collect the following data at different times:
First step—phone call: The clinical research assistant or nurse will explain the study and encourage the participants to self-report by completing questionnaires (second step) and attending the medical visit (third step). During this discussion, the professional will collect general information (family status, occupation type/education level), anthropometric measures (height/weight) and data regarding the experience of the PRALIMAP-INÈS intervention. The consent for second and third steps will be asked of participants during the first step. If a participant refuses to participate, their reasons for refusal to participate will be recorded (eg, lack of time, no desire, already taken care of).
If a participant agrees, the second step will start and the third step will be planned. The information concerning the biographical approach study will be given with the possibility of solicitation by a sociologist.
Second step—self-report questionnaire: Participants will be invited to complete the self-report questionnaire online (estimated duration: 45 min) with a secure link to collect the following data:
Sociodemographic characteristics: Data on status (student, employee, etc), level of education, income, place of residence, family situation, relationship with family (financial support, material support, etc) and socioeconomic status using the FAS score will be collected.40 The FAS will be used to define socioeconomic status through six questions exploring the availability of a personal bedroom, bathrooms in the home, the presence of family cars, dishwashers and computers and opportunities for family holidays. It will be provided with a score ranging from 0 to 13, and the participants will then be dichotomised as ‘advantaged’ (ie, FAS score ≥6) and ‘less advantaged’ (ie, FAS score <6).44
Body image perception: Stunkard’s Figure Rating Scale will be used to assess the participants’ perceptions of their body shape as well as their ideal body shape.41
Care pathway related to overweight or obesity and all health components occurring during the last 10 years: health problems requiring medical or psychological care or that would have required care (but for which care was not received) and, more specifically, overweight/obesity comorbidities and personal initiatives to change weight will be investigated.
Lifestyle and nutritional (eating habits and physical activity) attitudes and behaviours: Eating habits will be measured by a food frequency questionnaire,33 and eating disorders will be screened using the EAT.38 Physical activity and sedentary behaviours will be measured by the GPAQ.32 Temperament in eating and physical activity will be assessed using self-report questionnaires.39 Alcohol and tobacco consumption and sleep quality will be investigated using self-report ad hoc questionnaires. Participants will be asked about significant past changes (for at least 3 months) in their lifestyle and nutritional attitudes and behaviours.
Coping: The Brief Cope questionnaire will be used to measure effective and ineffective ways of coping with stressful life events.35
Self-esteem: The RSE scale will be used to assess self-esteem in participants.36
Emotional regulation: The DERS will be used to measure emotion regulation problems.37
Quality of life: Quality of life will be measured by the SF12.34 This short version of the SF-36 tool consists of 12 items. The physical health and mental health composite scores will be computed using the scores of the 12 items, ranging from 0 to 100, where 0 reflects the lowest health level and 100 reflects the highest health level.
In addition, the major life events, daily hassles and their impact, whether disruptive or not, on personal, school and professional life will be measured.
Experience of participating in the PRALIMAP-INÈS intervention: assess recollection regarding the experience in the study (positive, negative memories; utility).
Follow-up will be performed to ensure that the participants complete the questionnaires; if they do not complete the questionnaire, they will be contacted again before the medical visit (third step). If the questionnaire is not completed prior to the medical visit, it will be completed in person during the medical visit. A financial incentive (€20 gift card) was offered to participants who completed the questionnaire.
Third step—visit: The check-up visit will be performed by a clinical research nurse either face to face or by videoconference (if the participant cannot or does not wish to come in for the visit). Prior to recruitment, a procedure was established to standardise visits and measurements. The visit will last 1 hour, and the following data will be collected:
Height (with a measuring rod).
Weight, percentage of fat mass, percentage of lean body mass and estimated visceral fat level (shoes and socks off) (with a bioelectrical impedance scale (model: TANITA DC 430 MAS). Clinical research nurses were trained to use the bioelectrical impedance scale.
Waist circumference (with a measuring tape).
All measures taken to lose weight during the past 10 years (consultation, educational intervention type, frequency, etc) and all health events occurring during the past 10 years.
When the visit was conducted by videoconference, participants were asked to measure themselves (weight, height and waist circumference (using a measuring tape)) before the visit, if possible. Participants were then asked to report their measurements during the videoconference. The data collected by professionals will be directly input into a computer.
Semistructured biographical interview: To collect these data, 40 participants will be invited (asked during the third step) to participate in a 1-hour semistructured interview with a sociologist. Interviews were scheduled on a visit-by-visit basis. Once a participant agrees to be interviewed by the sociologist, the sociologist will contact the participant 2–6 weeks later to make an appointment. The interview will be conducted by telephone or videoconference or in the same place as the check-up visit. Building on life the theoretical framework of life trajectories and relying on a biographical approach,45 the objective is to deepen the comprehension of participants’ trajectories. From the individual narrative, dimensions such as family situation, living conditions, social network, educational and professional pathways and personal life aspirations will be evaluated as social determinants likely to affect health behaviour. The biographical approach indeed allows, from an individual’s discourse, the questioning of social resources mobilised by the individual and shaping their life—including heath and consequently obesity—trajectories. Moreover, the focus of the biographical approach is to consider the dynamics of trajectories and, from this perspective, to identify personal events and possible meaningful life bifurcations. Finally, the PRALIMAP-INÈS intervention will be integrated as a specific event in the trajectory and will be explored according to the above social dimensions. The interview guide was developed in working sessions with sociologists and members of the research team before the start of the study. The guide was then presented to the Coordination Committee, which suggested some edits. The edited guide was then tested and slightly revised (ie, follow-up questions) by the sociologists after the first interviews. The interview data will be audio recorded, transcribed verbatim and double-coded by two different sociologists. In case of discrepancies, a discussion between the sociologists will take place. If no agreement is reached after this discussion, the discrepancies will be discussed by the sociologists and Coordination Committee.
Statistical methods
Quantitative data will be analysed with SAS V.9.4 and R software, and qualitative data will be analysed with NVivo V.10 software.
Sample description: Sociodemographic characteristics, BMI, BMI z-score, weight status, eating habits, physical activity, sedentary behaviour, quality of life, and alcohol and tobacco consumption will be described using means (SDs) for continuous variables, frequencies (percentages) for categorical variables and the number of participants missing data. Comparisons of the initial data between the participants included in the PRALIMAP-CINeCO trial and those who declined to participate will be conducted using the χ2 test or Fisher’s exact test for categorical variables, and Student’s t-test for quantitative variables. Observations from participants with missing data may be imputed or excluded from analyses.
Primary outcome analysis: We will perform a comparative analysis of the change in BMI between T0/T1/T2 and T3 (10 years after inclusion in the PRALIMAP-INÉS intervention) by socioeconomic status and receipt of the PRALIMAP-INÈS intervention as follows:
Describing the change in BMI from adolescence to young adulthood by comparing data collected at the time of enrolment in the PRALIMAP-INÈS intervention (T0) and at the time of enrolment in the present study (T3).
Identifying and characterising change profiles of the transition from adolescence to young adulthood by trajectory analysis based on data collected at T0, T1, T2 and T3. Growth mixture modelling will be used to identify latent classes. Particular attention will be given to determining the number of classes using the shapes of different trajectories, the proportion of participants per class, log-likelihood, entropy, the posterior probability of membership and the Akaike and Bayesian information criteria.
In the second step, regression models (logistic and/or Cox regression models depending on the presence or absence of censored data) will be used to identify the potential effects of overweight (eg, duration of care management after the intervention, intervention participation) and socioeconomic status on social, educational and economic trajectories. Path analysis will also be used to disentangle the effects and identify the mediating factors.
Secondary outcomes analysis
Quantitative analysis: The same statistical methods used for the primary analysis will be used for the secondary analyses. We will perform a comparative analysis of the change of outcomes (BMI z-score, weight status, socioeconomic status, eating habits, physical activity, sedentary behaviour, quality of life, alcohol and tobacco consumption) between T0/T1/T2 and T3 by socioeconomic status and receipt of the PRALIMAP-INÈS intervention.
Qualitative analysis: The qualitative data will be collected for different purposes, and therefore, different approaches for analysis will be used.
The responses to open questions of the self-report questionnaire (specifically care pathway related to overweight or obesity and all health components occurring during the last 10 years, and experience of participating in the PRALIMAP-INÈS intervention) and the data collected by interviews during the check-up visit related to lasting changes (for at least 3 months) in physical activity and sedentary behaviour, eating habits and the motivations for these changes or the initiatives to change weight will be analysed by identifying themes and clarifying links. The aim of this analysis of open responses is to reveal the meaning of specific themes by articulating theoretical hypotheses—here, in the light of the theoretical models available in the literature on the determinants of behaviour maintenance and change,46 and the data collected.
-
The analysis of the data obtained from the 40 biographical interviews will require a three-step analytical approach.
A comprehensive thematic analysis will be performed.47,49 Drawing from Glaser and Strauss’s grounded theory,50 this analytical approach aims to reveal the meaning of phenomena by articulating theoretical hypotheses—in our case on participants’ life trajectories—and empirical data. Each interview transcript will be carefully read to identify the main topics discussed throughout the interview corpus (vertical reading). A thematic analysis grid will be constructed based on the first reading of all the interviews and will then be used for coding the interviews. Then, horizontal reading, node by node, will be performed to develop a comprehensive scheme highlighting participants’ life trajectories with regard to social and personal determinants and how these may have shaped and impacted their health behaviour changes. NVivo software will be used.
The researcher will rework the interview transcript from a chronological perspective51 stating the start of the trajectories—in this case obesity—and its main stages (quitting school, starting a new professional experience, getting into a new relationship, etc). The participant will be contacted again to validate and eventually amend their life narrative. The aim is to link the reconstruction of the trajectory to social and personal resources identified during the interview. The analysis of life course events will also aid the identification of social and personal resources.
The analyses will involve a system for re-recoding qualitative data (eg, the number and type of events, changes introduced, motivations and any element that may emerge from qualitative analyses). The objective is to weight resources and evaluate their impacts on specific life events according to the answers on the self-report questionnaires, the measurements by the nurse and the data collected by the physician during the check-up visit.
Mixed approach analysis: Beyond the specific contributions of each method, we will use a convergent mixed-methods design that analyses and combines quantitative and qualitative data to best highlight our research hypotheses and more specifically explain the adolescence-adulthood transition when facing overweight and social disadvantage. When the setting and the participants are the same, the convergent mixed methods are appropriate52; for example, intentional sampling from the population participating in the quantitative phase occurs, and a subsample for the qualitative phase is identified.
In a convergent design, the order of presentation should be driven by choices made relative to how the data interact or ‘‘talk’’ to each other for integration.53 Our data will be organised to address parallel content, from several scales and interviews, and the results will be structured and described using a weaving pattern in which quantitative and qualitative findings are presented together thematically weaving back and forth between quantitative and qualitative data by theme or domain. The interdisciplinarity of the teams for data interpretation and analysis via this mixed approach is a key element.54 55
Discussion
Health-promoting behaviours adopted during adolescence can have significant long-term effects on health outcomes and overall well-being. Through this proposed 10-year follow-up study of the PRALIMAP-INÈS intervention, a school-based overweight management intervention in adolescents, we aim to increase knowledge of life course trajectories from adolescence to young adulthood regarding weight and health behaviours, and social, economic and educational dimensions. Indeed, the originality of this project lies in the long-term postintervention and life transition period of follow-up. Studies investigating the effectiveness of overweight management strategies in adolescents are common,56,58 but those investigating postintervention effects, especially during the transition from adolescence to adulthood are lacking. In a literature review, St George et al showed that only 1 of the 74 included obesity prevention interventions had a follow-up period that had a duration greater than 10 years but involved early childhood.59 However, childhood and adolescent obesity confer major risks of excess and premature morbidity and mortality, which may be evident before the age of 30 years in both sexes.19 60 The management of obesity requires follow-up lasting from several years to a lifetime, depending on the complexity, as recommended by the French National Authority for Health.61 Thus, in the current study, the analysis of scalable trajectories of health behaviours (eating habits, physical activity, sedentary behaviour, etc) from adolescence to young adulthood will allow for the identification of their determinants to take preventive measures for the development and maintenance of healthy behaviours.
One of the challenges, in this study, will be convincing the adolescents, who are now young adults to participate in this follow-up assessment. Precisely, estimating the number of young adults who cannot be located is difficult because the cohort attrition rates are variable. However, Booker et al62 showed that incentives were associated with an increase in retention rates, which improved with greater incentive value. To maximise our chances, first, the partnership with the regional education authority will facilitate the follow-up and acquisition of telephone information for young people who had mobile phones when they were included in the PRALIMAP-INÈS intervention. Second, we interviewed six young adults (included in the PRALIMAP-INÈS intervention) to obtain their opinions on the study process as envisaged and to assess the feasibility of the study. A contact guide and a focus interview grid were used as a framework. We thus explored the tools, collection methods (interview and online questionnaire) and solicitation methods (telephone, email, letter, social networks and profile of the people in charge of contacts) used during the interviews. The six people who participated had different profiles (men/women; student/employee; weight increase/stabilisation; participating or not in PRALIMAP-INÈS intervention activities), showing the need to adapt the methods (contact, call schedule and data collection methods). Finally, support from local media (TV news, radio and newspapers) and stakeholders (eg, nurses) will also be used to promote our study.
Beyond the scope of this study, appropriate support should be offered to young adults who participated in the PRALIMAP- INÈS intervention and who are still experiencing overweight or obesity and may be less willing to participate in an overweight and obesity prevention intervention. Using the Guidelines for Managing Overweight and Obesity in Adults as a framework, this support must integrate the principal components of comprehensive lifestyle modification, which include eating habits, physical activity and behaviour therapy.63 In addition, the technological revolution has profoundly changed living conditions and communication by facilitating the exchange of information and the development of social networks for more than a decade. New information and communication technologies are also being developed in the field of health.64,66 In this way, e-coaching for the management of overweight and obesity will be developed and proposed for young adults who are overweight or obesity at T3, and its effectiveness will be evaluated through a randomised controlled trial. This teleintervention could have important implications for social inequalities in weight status, which result from many factors, including territorial inequalities in access to care and services (eg, transportation difficulties, work schedules and lack of health professionals). For example, there is evidence that such interventions facilitate access to care by removing travel barriers and reducing costs for patients, promote access for young patients who are sometimes resistant to the constraints of face-to-face group sessions and encourage skill development and knowledge acquisition at an individual’s own pace. In this way, it will be useful to investigate the effect of the e-coaching intervention on social inequalities in weight status and their underlying mechanisms.
The results of this study may provide insight into the life course from adolescence to young adulthood regarding weight reduction or stabilisation at the end of school-based obesity management (ie, the PRALIMAP-INÈS intervention). Specifically, this study will increase the knowledge of the social, economic and educational determinants of changes in weight status, health behaviours and mental health from adolescence to young adulthood. Such knowledge could contribute to the prevention of harmful trajectories from adolescence and could be essential for policy-makers to diversify and tailor intervention strategies aimed at addressing socioeconomic inequalities in weight status.
Ethics and dissemination
The PRALIMAP-CINeCO trial has been approved by the French Persons Protection Committee (no. 2021-A00949-32) and a conformity declaration with the French National Commission for Data Protection and Liberties has been made. This trial was registered at ClinicalTrials.gov (NCT05386017). The data will be kept for at least 15 years after the research is completed. The results will be presented at conferences and published in international peer-reviewed journals. Authorship eligibility will follow ICMJE recommendations.
supplementary material
Acknowledgements
The authors would like to thank the PRALIMAP-INÈS participants for their participation. The sponsor of the study is CHRU de Nancy (Direction de la Recherche et de l’Innovation).
Footnotes
Funding: This study is funded by the Agence Nationale de la Recherche (Grant number: ANR-20-CE36-0006-01).
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2023-083090).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Author note: A Y O is the principal investigator of the study.
Contributor Information
Karine Legrand, Email: k_legrand@orange.fr.
Florian Manneville, Email: florian.manneville@univ-lorraine.fr.
Johanne Langlois, Email: johanne.langlois@lecnam.net.
Philip Böhme, Email: p.bohme@chru-nancy.fr.
Arnaud Dosda, Email: a.dosda@chru-nancy.fr.
Mélanie Beguinet, Email: M.BEGUINET@chru-nancy.fr.
Serge Briançon, Email: serge.briancon@univ-lorraine.fr.
Elisabeth Spitz, Email: elisabeth.spitz@univ-lorraine.fr.
Edith Lecomte, Email: edith.lecomte@lecnam.net.
Abdou Y Omorou, Email: y.omorou@chru-nancy.fr.
References
- 1.OECD Obesity Update 2017. 2017. http://www.oecd.org/health/health-systems/Obesity-Update-2017.pdf Available.
- 2.Fontbonne A, Currie A, Tounian P, et al. Prevalence of Overweight and Obesity in France: The 2020 Obepi-Roche Study by the 'Ligue Contre l’Obésité.'. J Clin Med. 2023;12:925. doi: 10.3390/jcm12030925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matta J, Zins M, Feral-Pierssens AL, et al. Prévalence du surpoids, de l’obésité et des facteurs de risque cardio-métaboliques dans la cohorte Constances. Bull Epidemiol Hebd. 2016:640–6. [Google Scholar]
- 4.Martin A, Booth JN, Laird Y, et al. Physical activity, diet and other behavioural interventions for improving cognition and school achievement in children and adolescents with obesity or overweight. Cochrane Database Syst Rev. 2018;3:CD009728. doi: 10.1002/14651858.CD009728.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Frech A. Healthy Behavior Trajectories between Adolescence and Young Adulthood. Adv Life Course Res. 2012;17:59–68. doi: 10.1016/j.alcr.2012.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sawyer SM, Afifi RA, Bearinger LH, et al. Adolescence: a foundation for future health. Lancet. 2012;379:1630–40. doi: 10.1016/S0140-6736(12)60072-5. [DOI] [PubMed] [Google Scholar]
- 7.Militello LK, Kelly S, Melnyk BM, et al. A Review of Systematic Reviews Targeting the Prevention and Treatment of Overweight and Obesity in Adolescent Populations. J Adolesc Health. 2018;63:675–87. doi: 10.1016/j.jadohealth.2018.07.013. [DOI] [PubMed] [Google Scholar]
- 8.Arlinghaus KR, Cepni AB, Helbing RR, et al. Response to school-based interventions for overweight and obesity: A systematic scoping review. Clin Obes. 2022;12:e12557. doi: 10.1111/cob.12557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Silveira JAC, Taddei J, Guerra PH, et al. Effectiveness of school-based nutrition education interventions to prevent and reduce excessive weight gain in children and adolescents: a systematic review. J Pediatr (Rio J) 2011;87:382–92. doi: 10.2223/JPED.2123. [DOI] [PubMed] [Google Scholar]
- 10.Briançon S, Bonsergent E, Agrinier N, et al. PRALIMAP: study protocol for a high school-based, factorial cluster randomised interventional trial of three overweight and obesity prevention strategies. Trials. 2010;11:119. doi: 10.1186/1745-6215-11-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bonsergent E, Thilly N, Legrand K, et al. Process evaluation of a school-based overweight and obesity screening strategy in adolescents. Glob Health Promot. 2013;20:76–82. doi: 10.1177/1757975913483330. [DOI] [PubMed] [Google Scholar]
- 12.Bonsergent E, Agrinier N, Thilly N, et al. Overweight and obesity prevention for adolescents: a cluster randomized controlled trial in a school setting. Am J Prev Med. 2013;44:30–9. doi: 10.1016/j.amepre.2012.09.055. [DOI] [PubMed] [Google Scholar]
- 13.Langlois J, Omorou AY, Vuillemin A, et al. Association of socioeconomic, school-related and family factors and physical activity and sedentary behaviour among adolescents: multilevel analysis of the PRALIMAP trial inclusion data. BMC Public Health. 2017;17:175. doi: 10.1186/s12889-017-4070-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Manneville F, Omorou AY, Legrand K, et al. Universal School-Based Intervention Does Not Reduce Socioeconomic Inequalities in Weight Status among Adolescents. Child Obes. 2019;15:532–40. doi: 10.1089/chi.2019.0042. [DOI] [PubMed] [Google Scholar]
- 15.Legrand K, Lecomte E, Langlois J, et al. Reducing social inequalities in access to overweight and obesity care management for adolescents: The PRALIMAP-INÈS trial protocol and inclusion data analysis. Contemp Clin Trials Commun. 2017;7:141–57. doi: 10.1016/j.conctc.2017.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Omorou AY, Langlois J, Böhme P, et al. Proportionate universalism intervention is effective for tackling nutritional social gradient in adolescents: the PRALIMAP-INÈS mixed randomised trial. Public Health (Fairfax) 2023;221:79–86. doi: 10.1016/j.puhe.2023.06.006. [DOI] [PubMed] [Google Scholar]
- 17.Briançon S, Legrand K, Muller L, et al. Effectiveness of a socially adapted intervention in reducing social inequalities in adolescence weight. The PRALIMAP-INÈS school-based mixed trial. Int J Obes. 2020;44:895–907. doi: 10.1038/s41366-020-0520-z. [DOI] [PubMed] [Google Scholar]
- 18.Wang LY, Chyen D, Lee S, et al. The association between body mass index in adolescence and obesity in adulthood. J Adolesc Health. 2008;42:512–8. doi: 10.1016/j.jadohealth.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 19.Horesh A, Tsur AM, Bardugo A, et al. Adolescent and Childhood Obesity and Excess Morbidity and Mortality in Young Adulthood-a Systematic Review. Curr Obes Rep. 2021;10:301–10. doi: 10.1007/s13679-021-00439-9. [DOI] [PubMed] [Google Scholar]
- 20.Jebeile H, Kelly AS, O’Malley G, et al. Obesity in children and adolescents: epidemiology, causes, assessment, and management. Lancet Diabetes Endocrinol. 2022;10:351–65. doi: 10.1016/S2213-8587(22)00047-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oude Luttikhuis H, Baur L, Jansen H, et al. Interventions for treating obesity in children. Cochrane Database Syst Rev. 2009 doi: 10.1002/14651858.CD001872.pub2. [DOI] [PubMed] [Google Scholar]
- 22.Watts AW, Loth KA, Peterson C, et al. Characteristics of a Favorable Weight Status Change From Adolescence to Young Adulthood. J Adolesc Health. 2016;58:403–9. doi: 10.1016/j.jadohealth.2015.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sweeting H, Smith E, Neary J, et al. 'Now I care': a qualitative study of how overweight adolescents managed their weight in the transition to adulthood. BMJ Open. 2016;6:e010774. doi: 10.1136/bmjopen-2015-010774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stok FM, Renner B, Clarys P, et al. Understanding Eating Behavior during the Transition from Adolescence to Young Adulthood: A Literature Review and Perspective on Future Research Directions. Nutrients. 2018;10:667. doi: 10.3390/nu10060667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Corder K, Winpenny E, Love R, et al. Change in physical activity from adolescence to early adulthood: a systematic review and meta-analysis of longitudinal cohort studies. Br J Sports Med. 2019;53:496–503. doi: 10.1136/bjsports-2016-097330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Winpenny EM, van Sluijs EMF, White M, et al. Changes in diet through adolescence and early adulthood: longitudinal trajectories and association with key life transitions. Int J Behav Nutr Phys Act. 2018;15:86. doi: 10.1186/s12966-018-0719-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Elsenburg LK, Smidt N, Hoek HW, et al. Body Mass Index Trajectories from Adolescence to Early Young Adulthood: Do Adverse Life Events Play a Role? Obesity (Silver Spring) 2017;25:2142–8. doi: 10.1002/oby.22022. [DOI] [PubMed] [Google Scholar]
- 28.McGinty SM, Osganian SK, Feldman HA, et al. BMI Trajectories from Birth to Young Adulthood. Obesity (Silver Spring) 2018;26:1043–9. doi: 10.1002/oby.22176. [DOI] [PubMed] [Google Scholar]
- 29.Neumark-Sztainer D, Wall MM, Chen C, et al. Eating, Activity, and Weight-related Problems From Adolescence to Adulthood. Am J Prev Med. 2018;55:133–41. doi: 10.1016/j.amepre.2018.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bates S, Bayley T, Norman P, et al. A Systematic Review of Methods to Predict Weight Trajectories in Health Economic Models of Behavioral Weight-Management Programs: The Potential Role of Psychosocial Factors. Med Decis Making. 2020;40:90–105. doi: 10.1177/0272989X19889897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mumford EA, Liu W, Hair EC, et al. Concurrent trajectories of BMI and mental health patterns in emerging adulthood. Soc Sci Med. 2013;98:1–7. doi: 10.1016/j.socscimed.2013.08.036. [DOI] [PubMed] [Google Scholar]
- 32.Rivière F, Widad FZ, Speyer E, et al. Reliability and validity of the French version of the global physical activity questionnaire. J Sport Health Sci. 2018;7:339–45. doi: 10.1016/j.jshs.2016.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fédération Nationale des Observatoires Régionaux de la Santé; 2009. Harmoniser les études en nutrition un guide de bonnes pratiques pour les études régionales et locales.https://sante.gouv.fr/IMG/pdf/guide_fnors_nutrition.pdf Available. [Google Scholar]
- 34.Gandek B, Ware JE, Aaronson NK, et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol. 1998;51:1171–8. doi: 10.1016/s0895-4356(98)00109-7. [DOI] [PubMed] [Google Scholar]
- 35.Muller L, Spitz E. Validation du Brief COPE sur une population française. L’Encéphale. 2003;29:507–18. [PubMed] [Google Scholar]
- 36.Rosenberg M. Basic Books; 1979. Conceiving the self.https://www.apa.org/obesity-guideline/rosenberg-self-esteem.pdf Available. [Google Scholar]
- 37.Hallion LS, Steinman SA, Tolin DF, et al. Psychometric Properties of the Difficulties in Emotion Regulation Scale (DERS) and Its Short Forms in Adults With Emotional Disorders. Front Psychol. 2018;9:539. doi: 10.3389/fpsyg.2018.00539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Garner DM, Garfinkel PE. The Eating Attitudes Test: an index of the symptoms of anorexia nervosa. Psychol Med. 1979;9:273–9. doi: 10.1017/s0033291700030762. [DOI] [PubMed] [Google Scholar]
- 39.Godefroy V, Trinchera L, Romo L, et al. Modelling the effect of temperament on BMI through appetite reactivity and self-regulation in eating: a Structural Equation Modelling approach in young adolescents. Int J Obes. 2016;40:573–80. doi: 10.1038/ijo.2016.6. [DOI] [PubMed] [Google Scholar]
- 40.Hartley JEK, Levin K, Currie C. A new version of the HBSC Family Affluence Scale - FAS III: Scottish Qualitative Findings from the International FAS Development Study. Child Indic Res. 2016;9:233–45. doi: 10.1007/s12187-015-9325-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stunkard AJ, Sørensen T, Schulsinger F. Use of the Danish Adoption Register for the study of obesity and thinness. Res Publ Assoc Res Nerv Ment Dis. 1983;60:115–20. https://pubmed.ncbi.nlm.nih.gov/6823524/ Available. [PubMed] [Google Scholar]
- 42.Cole TJ, Bellizzi MC, Flegal KM, et al. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–3. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McCarthy HD, Jarrett KV, Crawley HF. The development of waist circumference percentiles in British children aged 5.0-16.9 y. Eur J Clin Nutr. 2001;55:902–7. doi: 10.1038/sj.ejcn.1601240. [DOI] [PubMed] [Google Scholar]
- 44.Boyce W, Torsheim T, Currie C, et al. The Family Affluence Scale as a Measure of National Wealth: Validation of an Adolescent Self-Report Measure. Soc Indic Res. 2006;78:473–87. doi: 10.1007/s11205-005-1607-6. [DOI] [Google Scholar]
- 45.Bessin M. Parcours de vie et temporalités biographiques: quelques éléments de problématique Life courses and biographical temporalities: some problematic elements. Inf soc. 2010;156:12–21. doi: 10.3917/inso.156.0012. [DOI] [Google Scholar]
- 46.Davis R, Campbell R, Hildon Z, et al. Theories of behaviour and behaviour change across the social and behavioural sciences: a scoping review. Health Psychol Rev. 2015;9:323–44. doi: 10.1080/17437199.2014.941722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Balard F, Kivits J, Voléry I, et al. L’analyse qualitative en santé. Armand Colin; 2016. Qualitative analysis in health. [Google Scholar]
- 48.Kaufmann JC. L’entretien compréhensif. Armand Colin; 2016. The comprehensive interview 4th issue. [Google Scholar]
- 49.Lejeune C. Manuel d’analyse Qualitative: Analyser sans Compter Ni Classer [Qualitative Analysis Manual: Analyzing without Counting or Ranking. De Boeck Supérieur. Louvain-la-Neuve; 2019. [Google Scholar]
- 50.Glaser B, Strauss A. Discovery of grounded theory: strategies for qualitative research. Routledge; 2017. [Google Scholar]
- 51.Grossetti M. Les narrations quantifiées: Une méthode mixte pour étudier des processus sociaux. Terrains & travaux; 2011. Quantified narratives: a mixed method for studying social processes; pp. 19–161. [Google Scholar]
- 52.Creswell JW. A concise introduction to mixed methods research. SAGE; 2015. [Google Scholar]
- 53.Fetters MD, Freshwater D. Publishing a Methodological Mixed Methods Research Article. J Mix Methods Res. 2015;9:203–13. doi: 10.1177/1558689815594687. [DOI] [Google Scholar]
- 54.Bujold M, Hong QN, Ridde V, et al. Cahiers scientifiques de l’ACFAS. 2018. Oser les défis des méthodes mixtes en sciences sociales et sciences de la santé taking on the challenges of mixed methods in the social and health sciences. [Google Scholar]
- 55.Kivits J, Ricci L, Minary L. Interdisciplinary research in public health: the 'why' and the 'how.'. J Epidemiol Community Health. 2019;73:1061–2. doi: 10.1136/jech-2019-212511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Brown T, Moore TH, Hooper L, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2019;7:CD001871. doi: 10.1002/14651858.CD001871.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hargreaves D, Mates E, Menon P, et al. Strategies and interventions for healthy adolescent growth, nutrition, and development. Lancet. 2022;399:198–210. doi: 10.1016/S0140-6736(21)01593-2. [DOI] [PubMed] [Google Scholar]
- 58.Motevalli M, Drenowatz C, Tanous DR, et al. Management of Childhood Obesity-Time to Shift from Generalized to Personalized Intervention Strategies. Nutrients. 2021;13:1200. doi: 10.3390/nu13041200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.St George SM, Agosto Y, Rojas LM, et al. A developmental cascade perspective of paediatric obesity: A systematic review of preventive interventions from infancy through late adolescence. Obes Rev. 2020;21:e12939. doi: 10.1111/obr.12939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vazquez CE, Cubbin C. Socioeconomic Status and Childhood Obesity: a Review of Literature from the Past Decade to Inform Intervention Research. Curr Obes Rep. 2020;9:562–70. doi: 10.1007/s13679-020-00400-2. [DOI] [PubMed] [Google Scholar]
- 61.Haute Autorité de Santé Guide du parcours de soins: surpoids et obésité de l’adulte care pathway guide: overweight and obesity in adults. 2023. [28-Nov-2023]. https://www.has-sante.fr/upload/docs/application/pdf/2023-02/guide._parcours_surpoids-obesite_de_ladulte.pdf Available. Accessed.
- 62.Booker CL, Harding S, Benzeval M. A systematic review of the effect of retention methods in population-based cohort studies. BMC Public Health. 2011;11:249. doi: 10.1186/1471-2458-11-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wadden TA, Tronieri JS, Butryn ML. Lifestyle modification approaches for the treatment of obesity in adults. Am Psychol. 2020;75:235–51. doi: 10.1037/amp0000517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Calcaterra V, Verduci E, Vandoni M, et al. Telehealth: A Useful Tool for the Management of Nutrition and Exercise Programs in Pediatric Obesity in the COVID-19 Era. Nutrients. 2021;13:3689. doi: 10.3390/nu13113689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Willis EA, Szabo-Reed AN, Ptomey LT, et al. Distance learning strategies for weight management utilizing social media: a comparison of phone conference call versus social media platform. Rationale and design for a randomized study. Contemp Clin Trials. 2016;47:282–8. doi: 10.1016/j.cct.2016.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zamanzadeh V, Zirak M, Hemmati Maslakpak M, et al. Distance education and diabetes empowerment: A single-blind randomized control trial. Diabetes Metab Syndr Clin Res Rev. 2017;11:S247–51. doi: 10.1016/j.dsx.2016.12.039. [DOI] [PubMed] [Google Scholar]