Abstract
Linear immunoglobulin A bullous dermatosis (LABD) is a rare immune-mediated vesiculobullous disease that is reported to be induced by infections or medications. Atezolizumab is a monoclonal antibody that targets programmed cell death ligand-1 and has been used to treat multiple cancers. Here, we report a case of drug induced LABD following the administration of Atezolizumab.
Key words: linear IgA bullous dermatosis, atezolizumab
Introduction
Linear IgA bullous dermatosis (LABD) is a rare immunobullous disease, that affects 0.2-2.3 cases per one million yearly.1 It presents with an abrupt onset of urticarial plaques, vesicles and bullae, mostly on the face, scalp, and limbs. On histopathology, LABD shows a subepidermal blister with dermal neutrophilic infiltration seen by Hematoxylin and Eosin (H&E), and a linear deposition of IgA at the basement membrane zone seen by Direct Immunofluorescence (DIF). Although LABD is typically idiopathic, it may occasionally be provoked by infections or medications. In adults, drug-induced LABD accounts for 37.5% of cases, with vancomycin being the most frequently reported drug.2 Atezolizumab is a monoclonal antibody that inhibits programmed cell death ligand-1 (PD-L1). It is used as an anti-cancer treatment and exerts its effect by activating anti-tumor immune responses. PD-L1 inhibitors have been linked to several drug-induced dermatoses.3 Atezolizumab has been recently reported to cause LABD in one patient.4 Here, we report the second case of drug induced LABD following the administration of Atezolizumab.
Case Report
This was a 79-year-old man known to have Diabetes Mellitus and hepatocellular carcinoma (HCC). He presented to the emergency department with a 1-week history of a painful generalized rash. His symptoms started 2 weeks after getting a single dose of 1200 mg Atezolizumab and 750 mg Bevacizumab to treat his HCC. His medication history included Nivolumab and Lenvatinib, which were stopped 4 months earlier. On physical examination, he had multiple tender erythematous plaques, bullae and erosions in generalized distribution including the palms and soles (Figure 1A). The body surface area was ~10%, and Nikolsky sign was positive. The mucous membranes were also involved, with multiple erosions over the buccal mucosa, soft palate, and nasal mucosa. (Figure 1B). The differential diagnoses included Stevens-Johnson Syndrome (SJS), Bullous Pemphigoid, Pemphigus Vulgaris, Paraneoplastic Pemphigus, Generalized Bullous Fixed Drug Eruption, and LABD. Two 4-mm skin punch biopsies were taken for H&E and DIF. There was subepidermal blister with a linear neutrophilic band (Figure 2). DIF showed linear basal deposition of IgA, without IgG, IgM and C3. These findings were consistent with the diagnosis of LABD. After evaluating the patient medications and a review of the literature, it was decided that Atezolizumab was the most likely culprit drug. The patient was admitted for supportive management, and Atezolizumab was discontinued. The patient was started on Dexamethasone 4 mg IV twice daily. The patient condition rapidly improved, and he was discharged on Prednisone 25 mg daily on day 4. On 1-week follow-up, the patient had no active lesions, and there were no signs of recurrence. Two weeks later, the patient passed away due to cardio-pulmonary arrest secondary to locally advanced and metastatic HCC.
Discussion and Conclusions
LABD is a rare immune-mediated subepidermal vesiculobullous disease. The pathogenesis is thought to be due to circulating IgA antibodies directed against multiple basement membrane antigen including Bullous Pemphigoid Antigen 2 (BPAg2), type VII Collagen, and Laminin-332.1 LABD is usually idiopathic but may be rarely related to infections or medications. It has been linked to several drug classes such as antibiotics and non-steroidal anti-inflammatory agents.2 The most common reported drug is vancomycin accounting for 56% of all reported cases.2 The exact pathogenesis of drug induced LABD is not clear. T cells and cytokines were demonstrated to play a role in the pathogenesis. In one study of patients with drug-induced LABD, there was a significant increase in the levels of CD8+ cytotoxic T cells.5 Atezolizumab is a monocloncal antibody that selectively inhibits PD-L1, which leads to the inhibition of T-cell apoptosis.6 This may lead to increased levels of CD8+ T cells, which may explain the development of LABD in this case. However, for LABD, there has only been one reported case.4
Figure 1.
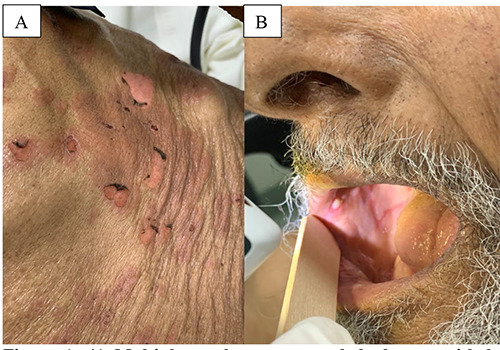
Multiple erythematous eroded plaques with hemorrhagic crusts over the (A) trunk; B) buccal mucosa.
Figure 2.
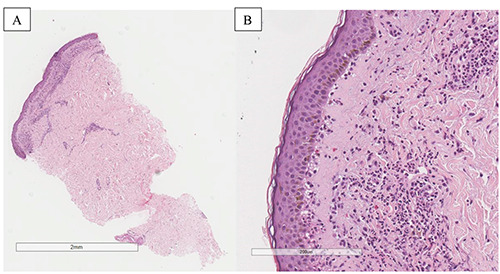
A) Low magnification of the skin punch biopsy with a moderate linear subepidermal mixede inflammatory infiltrate (hema-toxylin and eosin, 4×); B) Higher magnification of the skin punch biopsy which shows an early basal blister formation with vacuolar alteration in addition to the moderate linear subepidermal and perivascular neutrophils with scattered eosinophils (hematoxylin and eosin, 40×).
Availability of data and material
Data are available from the authors upon reasonable request.
References
- 1.Bernett CN, Fong M, Yadlapati S, Rosario-Collazo JA. Linear IgA dermatosis. Treasure Island (FL): StatPearls Publishing; 2022. [PubMed] [Google Scholar]
- 2.Lammer J, Hein R, Roenneberg S, et al. Drug-induced linear IgA bullous dermatosis: a case report and review of the literature. Acta Dermatol Venereol 2019;99:508-15. [DOI] [PubMed] [Google Scholar]
- 3.Sibaud V, Meyer N, Lamant L, et al. Dermatologic complications of anti-PD-1/PD-L1 immune checkpoint antibodies. Curr Opin Oncol 2016;28:254-63. [DOI] [PubMed] [Google Scholar]
- 4.Aguilar-Duran S, Mee J, Popat S, Heelan K. Atezolizumab-induced linear IgA bullous dermatosis. Br J Dermatol 2022;187:e193. [DOI] [PubMed] [Google Scholar]
- 5.Yawalkar N, Reimers A, Hari Y, et al. Drug-induced linear IgA bullous dermatosis associated with ceftriaxone-and metronidazole-specific T cells. Dermatology 1999;199:25-30. [DOI] [PubMed] [Google Scholar]
- 6.Herbst RS, Soria JC, Kowanetz M, et al. Predictive correlates of response to the anti-PD-L1 antibody MPDL3280A in cancer patients. Nature 2014;515:563-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available from the authors upon reasonable request.


