Abstract
Background
There is a growing body of evidence on shared decision-making (SDM) training programs worldwide. However, there is wide variation in program design, duration, effectiveness, and evaluation in both academia (ie, medical school) and the practice setting. SDM training has been slow to integrate in practice settings.
Methods
A pilot study of 6 multidisciplinary clinicians was conducted using quantitative and qualitative methods to evaluate changes in participant understanding and implementation of SDM in the practice setting. A 2-rater criterion-based evaluation method was used to assess a simulation-based case study role-play program using 7 domains of SDM pre and post training. The authors assessed whether clinicians addressed each of the 7 domains or what fraction of each domain was addressed as part of their simulation case study role-play performance. Focus groups were conducted pre- and postintervention to provide feedback to participants and to understand the clinician experience in greater detail.
Results
The increase in improvement in SDM ranged from 17% to 37%, and 7 of 8 domains for which participants were rated showed significant improvement. The areas of greatest improvement were seen in determining a patient’s goals/preferences, including risk tolerance regarding treatments (+37%) and values and self-efficacy (+37%)
Conclusion
The results of this study reveal a significant shift in clinician awareness of a patient’s goals, preferences, and values. Postintervention, clinicians began to understand the value of building a partnership with their patients whereby the patient becomes an active participant in their clinical care.
Keywords: Telehealth, septoplasty, virtual visits, telemedicine, septal deviation, otolaryngology
Introduction
In 1982, The President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research reported on the ethical and legal requirements of informed consent for patients undergoing medical procedures.1 The report, Making Health Care Decisions: The Ethical and Legal Implications of Informed Consent in the Patient-Practitioner Relationships, defined informed consent as active decision-making between the patient and the practitioner, rooted in mutual respect and collaboration.1 Some believe this publication marked the beginning of the shared decision-making (SDM) movement. After decades of research, SDM is now widely accepted as a patient-centered approach that engages the practitioner and patient in a partnership to meet the patient’s health care goals.2 However, despite decades of research on SDM, practical integration into clinical practice remains low and evidence of its value related to improved outcomes is limited.3 Multiple barriers exist related to sustainable practices in complex health care setting.4 A critical component of SDM in clinical care is the development of comprehensive, evidence-based SDM training programs. Yet, despite a plethora of research studies reporting on SDM training programs, there remains a lack of clarity as to the type of training program that produces reliable and sustainable participant outcomes.2,5 Currently there is no universally accepted standard to measure training effectiveness.6
In a systematic review of SDM training programs, Müller et al identified a wide variation in program design, duration, effectiveness, and a standardized evaluation framework focused on participant learning outcomes and associated patient care quality.3 Most training programs provide an overview of theories and competencies, with emphasis placed on skill development through role play.7 Singh Ospina et al found very low-quality evidence for teaching SDM to medical students and concluded that there was a lack of evidence as to whether there was improvement in clinical skills, behaviors, and patient outcomes after SDM training was completed.8
Given the fiscal constraints facing organizations post–COVID-19 pandemic and the desire to integrate SDM as a standard of practice across disciplines, there is urgency to find a reliable, low-cost, easy-to-use training method that reduces variation and applies the best evidence in the practice setting. Harman et al conducted an 8-week program delivered over 4 weeks that included workshops, campaign messaging, a report card, and coaching. At 12 weeks postintervention, clinician peers used a 9-point Rochester Participatory Decision-Making Scale to evaluate SDM behaviors in inpatient pediatric and internal medicine hospitalists and trainees and found improvement on all 9 behaviors in scale.9 For emergency department physicians, Kanaria and Chen used a flipped classroom with precourse materials and in-class sessions that included role play with feedback.10 A faculty examiner assessed skill attainment using simulated patient encounters and checklist for critical actions. The researchers concluded that role play is an interactive way to teach SDM for the emergency department.10 Müller et al used a mixed-methods 12-hour skill training for physicians caring for patients with asthma.11 This training included a short training, videotaped consultations with simulated patients with asthma, video analysis in small group sessions, individual feedback, short presentations, group discussions, and practical exercises. Overall, physicians experienced a positive change in behavior and attitude. Bos–van den Hoek et al used an interdisciplinary team approach for training.12 The training consisted of a 1-group pre-/posttest design training format that included e-learning modules and 1 guided online or in-person training session. Surveys were conducted at baseline, after e-learning, and after full blended learning. Simulated consultations were completed at baseline and at the end of the program. Researchers concluded that blended learning can improve SDM support skills, knowledge, and confidence.12
Despite these efforts, a substantial gap remains between programs designed for research and practical applications for real-world clinical practice. The authors report here on an effort to develop and pilot a practical approach developed for busy health care clinicians, with a core assumption that prioritizing and implementing changes that matter most to patients does not have to be difficult when the right strategies and training tools are in place. Therefore, the purpose of the study was to test a practical, easily adaptable model for SDM training to an interdisciplinary team of clinical staff (ie, physicians, nurse practitioners, pharmacists, and social workers) in a large academic cancer center.
Methods
A health profession’s continuing education group, a content expert in improvement and SDM, and clinical staff working at a large urban cancer center formed a collaborative partnership to codevelop a program based on the Practical Approach for SDM described by Oliver et al.13 The program was focused on SDM that emphasized patient-centered care by incorporating patient preferences and values in the determination of their health care choices. The team modified the program to specifically suit their context and population. They developed training materials to address SDM, checkpoint inhibitor therapy, and clinician–patient role-play methods. Team members included oncologists, nurse practitioners, a nurse coordinator, and a social worker. Each team member acted as their own control (N = 6), comparing their baseline preeducational intervention with postintervention findings. The 4-part training consisted of the following steps: 1) baseline assessments that included simulated case study role play and qualitative semi-structured interviews; 2) training interventions that included didactic videos on SDM, the non–small cell lung cancer (NSCLC) treatment, and simulation case role-play; 3) end-of-pilot simulation case study role play and qualitative semi-structured interviews; and 4) a focus group to understand participant experience at program completion (Table 1).
Table 1:
Sequence of steps for the pilot study
| Yale NSCLC SDM pilot—clinicians |
|---|
Baseline
|
Training interventions
|
End of pilot
|
Focus group
|
NSCLC, non–small cell lung cancer; SDM, shared decision-making.
Ethics review
This educational program assessment was determined to be exempt from institutional review board review for human subject’s research based on the Yale Institutional Review Board Research/Quality Improvement determination checklist process.
The pilot study assessed a representative sample of 6 NSCLC clinicians (2 physicians, 2 nurse practitioners, 1 nurse coordinator, and 1 social worker) at 2 time points, baseline and end of pilot, and focus group feedback to evaluate changes in their understanding and implementation of SDM in treatment discussions in the practice setting. Consideration was given to determining differences in observed performance based on years of experience (Figure 1). A full-time equivalent (FTE) is a unit of labor measurement that refers to the workload of a worker (a standard FTE is 40 hours of work per week).
Figure 1:
Percentage of full-time equivalent for each participant profession/specialty. N = 6 years of oncology care experience for each participant.
Intervention (exposure)
The training materials included 3 videos addressing each of the following:
SDM and Use of Decision Aids: Video
To ensure that patient-centered care incorporates patient-informed preferences, values, goals, and concerns, the training included a standard video addressing the domains of decision quality needed to be addressed as part of the SDM process in the practice setting between the clinician and patient. By encouraging clinicians to address their patients’ health concerns, clinicians can foster a partnership with their patients to collaborate and formulate truly informed shared decisions. SDM training addressed the domains of decision quality listed in Table 2.
Table 2:
Domains of decision quality in shared decision-making
| Domains of decision quality in SDM | |
|---|---|
| Reasonable options |
The clinician narrows the list of options to a limited menu of reasonable options. The SDM process then focuses on this menu. |
| Decision style preference | Style preference is articulated and respected by the patient and clinician. |
| Knowledge | The patient and clinician have a shared working knowledge of the most important information involved in the decision. |
| Risk/burden tolerance | Tolerances are discussed, articulated, and aligned with discussion of wellness options. |
| Accessibility | Insurance coverage status and out-of-pocket expenses, as applicable, are understood and factored into the decision. |
| Trade-off decisions | Trade-offs are made explicit, articulated, and understood by patient and clinician. |
| Readiness | The patient and clinician feel confident and comfortable in making the decision. |
| Activation, engagement, self-efficacy | The decision is realistically aligned with and encourages activation, self-efficacy, and engagement. |
SDM, shared decision-making.
Checkpoint Inhibitor Therapy in NSCLC: Video
State-of-the-science information on evidence-based checkpoint inhibitor therapies were discussed to enable clinicians to have more robust treatment discussions with their patients. Clinicians are provided with insights into the immune microenvironment and the role of checkpoint inhibitor immunotherapies in NSCLC. The efficacy, safety (including immune-related adverse events and burden of testing/visits), and indications for each of the currently US Food and Drug Administration–approved checkpoint inhibitors are discussed, as they are relevant to treatment discussions with the patients as part of SDM. Checkpoint inhibitors play an important role in the treatment of patients with NSCLC and are central to SDM discussions.14
Case Study Role-Play Videos
Two unfolding 1-hour case study role-play simulation scenarios are provided in the videos to emphasize methods for implementing SDM and the use of decision aids. The first case is a 56-year-old man with newly diagnosed stage IIIA NSCLC; the second case is a 69-year-old woman with stage IV NSCLC returning to treatment from a “chemotherapy holiday.” The videos discuss clinical evaluations, realistic treatment options, domains of decision quality, commonly asked questions, and decision aids appropriate for the treatment choices.
Outcomes
Assessments made at 2 time points, at baseline and at the end of the pilot, included qualitative semi-structured interviews and simulation case study role play. Simulation case study role-play scenarios were used to determine how effectively clinicians implemented the domains of decision quality into their practices. Note should be made that in the Yale program only 7 of the 8 domains were assessed. The “Availability” domain was not included due to time constraints of learners participating in the case role play. For assessments in SDM performance improved by the multidisciplinary Yale clinical team, baseline preintervention assessment was compared to the postintervention assessment (reported in this publication). The multidisciplinary group of clinicians served as their own control using a standard pre-/post design. A Likert rating scale was used to rate performance by a 2-rater system (0–4; 0 = no incorporation of SDM domains to 4 = incorporation of all SDM domains) by comparing baseline preintervention to postintervention observed performance in case study role-play scenarios. Professional patients were used in the case study role-play scenarios, and real-time feedback was provided to each of the multidisciplinary team members.
To facilitate inter-rater reliability, a 2-rater system was used to assess whether clinicians addressed each domain or what fraction of each domain was addressed as part of their simulation case study role play. Immediately after baseline assessments, clinicians received training in SDM, current NSCLC checkpoint inhibitor therapy, and simulation case study role play.
Data analytic plan
Quantitative statistical analysis was performed to compare the Likert scale rating of baseline preintervention with postintervention rating. For comparison, a Likert scale rating of 0 to 4 was converted into a percentage using the formula: Percentage Rating = (Likert Scale Rating × 25)/100. This percentage rating was used to calculate the percentage change in domain addressed by subtracting the baseline preintervention rating from the postintervention percentage rating. Statistical significance was calculated using 2-tailed paired Student t-test on baseline preintervention and postintervention ratings. The standard deviation and the standard error of the mean were also calculated. Quantitative analysis, including data analysis and statistical computing, was performed using Microsoft Excel 2020 (version 16.43).
Qualitative assessment (focus group)
A focus group that included all participating SDM team members was held after completing the pilot training and assessment visits to allow clinicians to share their experiences in the SDM pilot. They were asked whether their understanding of SDM changed over the course of this program, whether they were now using SDM with their patients, what parts of the program they found helpful, what changes or additions they would make to their training, how they planned to sustain SDM in their practice with an interdisciplinary team, how SDM could be shared with other groups/departments, and whether their views on the value of SDM had changed. The goal was to assess the acceptability, feasibility, and repeatability of the program to inform future education, as well as to determine how SDM can be incorporated into the Yale system setting.
Results
SDM training empowered participants to show significant improvement in SDM during postintervention as compared to preintervention assessments. Improvement in SDM ranged from 17% to 37%; 7 of 8 domains (Table 2) for which participants were rated showed significant improvement (Figure 2). The areas of greatest improvement were seen in determining a patient’s risk tolerance regarding treatments (+37%, P = 0.002), as well as values and self-efficacy determining a patient’s goals/preferences (+37%, P = 0.003). The next greatest areas of improvement were shown in determining decision style preference, that is, the extent to which a patient wants to participate in the decision process (+34%, P = 0.004), followed by providing reasonable treatment options to patients (+30%, P = 0.004), and lastly providing enough working knowledge about the important information to make informed decisions (+23%, P = 0.002), discussing trade-offs (+23%, P = 0.003), and feeling ready, confident, and comfortable to make decisions (+23%, P = 0.005). The lowest increase, 17%, was seen in Accessibility, where insurance coverage, as well as any other out-of-pocket expenses for the treatment, was supposed to be the main focus of discussion and decision-making.
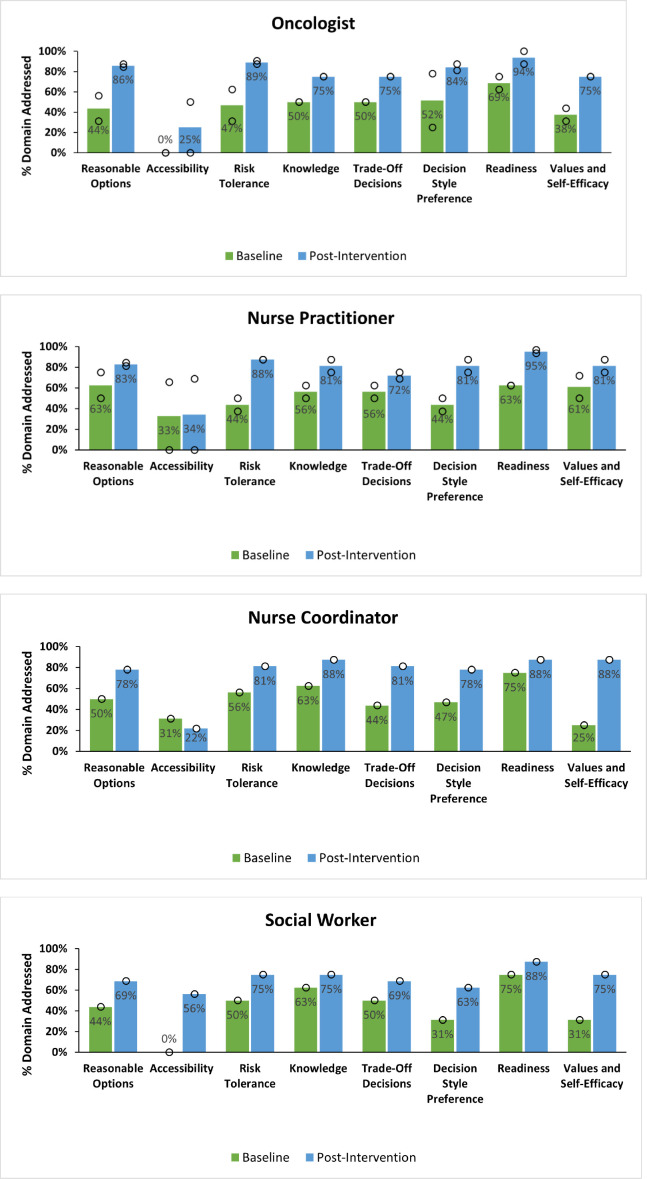
Figure 2:
Percentage of improvement seen by profession/specialty for all domains. Green = preintervention; blue = postintervention. Circles denote performance values in the distribution contributing to each average (bar). Oncologists, n = 2; nurse practitioners, n = 2; nurse coordinator, n = 1; social worker, n = 1.
All professions showed improvement in SDM post training
Participants of the study were categorized into 4 different professions: oncology physician (n = 2), nurse practitioner (n = 2), nurse coordinator (n = 1), and social worker (n = 1). Improvement in SDM was seen in all the professions for all the domains (Figure 2), suggesting that SDM training exposure had a beneficial effect across different types of professionals. This was an important observation given that some busy practice groups may need to employ team-based multidisciplinary SDM approaches.
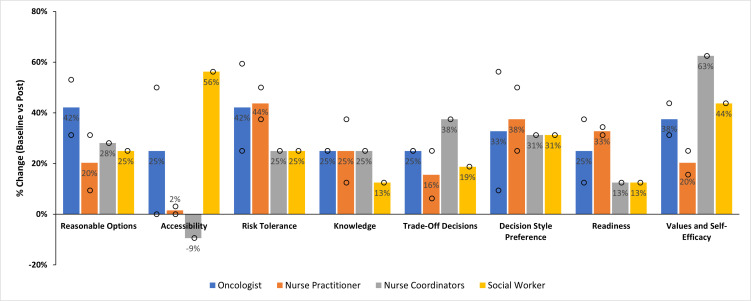
Considerable variation in improvement was seen in different domains by profession (Figure 3). It was found that there was remarkable increase in discussion about reasonable options among oncologists (+42%) as compared to nurse practitioners (+20%), nurse coordinator (+28%), and social worker (25%), though all the professions showed a similar increase (oncologists, +33%; nurse practitioners, +38%; nurse coordinator, +31%; and social worker, +31%) in determining decision style preferences. The oncologists, nurse practitioners, and nurse coordinator showed the same increase in providing the knowledge (25%); however, only a 13% increase was seen in the social worker. Both the oncologists and nurse practitioners showed more improvement for determining risk tolerance about treatments (oncologists, 42%; nurse practitioners, 44%) and readiness to make decisions (oncologists, 25%; nurse practitioners, 33%) as compared to nurse coordinator and social worker, showing only 25% increase in risk tolerance and 13% increase in readiness.
Figure 3:
Baseline vs post change by profession/specialty: Bars denote the average percentage of change in each domain by profession/specialty. Blue = oncologist, orange = nurse practitioner, gray = nurse coordinators, and yellow = social worker. Circles denote individual performance values in the distribution contributing to each average (bar). Domains are defined as Awareness (reasonable options, accessibility), Assessment (risk tolerance, knowledge, trade-off decisions), and Activation (readiness, values, and self-efficacy).
The increase in change among determining trade-off decisions and values and self-efficacy of patients’ goals/preferences followed similar patterns among professions, with the nurse coordinator showing the highest increase (trade-off decisions, 38%; values and self-efficacy, 63%), followed by the oncologists (trade-off decisions, 25%; values and self-efficacy, 38%), followed by the social worker (trade-off decisions, 19%; values and self-efficacy, 44%), and the least improvement was seen among the nurse practitioners (trade-off decisions, 16%; values and self-efficacy, 20%). Accessibility showed huge variation, as seen among professions as well, with the oncologists showing only 25% increase as compared to only a minimal 2% increase among the nurse practitioners and no increase in the nurse coordinator (showing negative value) as opposed to the very high 56% increase by the social worker, suggesting only the social worker gave importance to discussing and considering insurance options and the patient’s budget while considering the patient’s health care decisions.
Work experience and FTE has no impact on improvement in SDM upon training
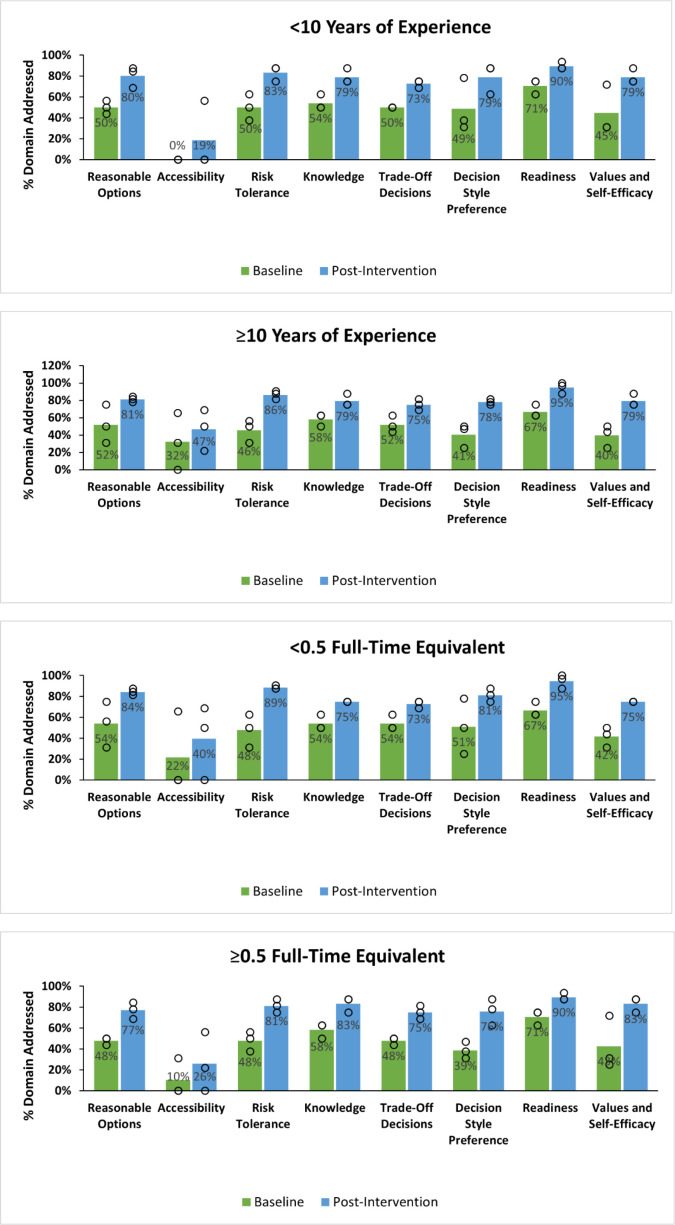
The work experience of the participants ranged from 1 to 20 years. The participants’ data were divided into 2 groups: 1) participants who had < 10 years of experience (n = 3), and 2) participants with ≥ 10 years of experience (n = 3). Both groups showed improved SDM practices upon training that they applied to providing patients with information and addressing their concerns so they could make more informed health care decisions (Figure 4).
Figure 4:
Pre- and postprogram changes by years of experience and FTE (N = 6). Bars denote the average percentage mastery of each performance domain for program participants (green = preprogram exposure; blue = postprogram exposure). Circles denote performance values in the distribution contributing to each average (bar). < 10 years of experience, n = 3; ≥ 10 years of experience, n = 3. < 0.5 FTE, n = 3; ≥ 0.5 FTE, n = 3. FTE = full-time equivalent.
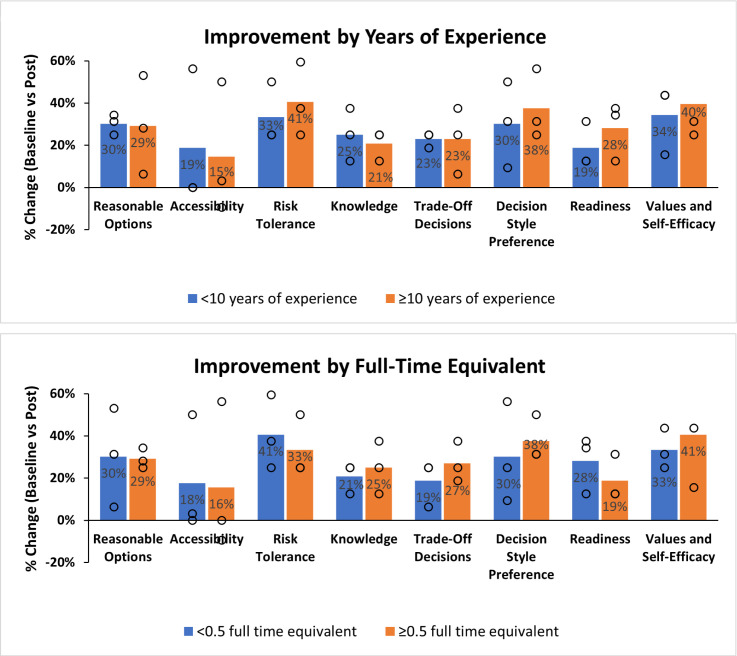
However, both groups showed very similar improvements across all the domains’ reasonable options (29% to 30%), decision style preference (30% to 38%), knowledge (21% to 25%), accessibility (15% to 19%), risk tolerance (33% to 41%), trade-off decisions (23%), readiness (19% to 28%), and values and self-efficacy (34% to 40%; Figure 5).
Figure 5:
Improvement by years of experience and FTE, N = 6. Bars denote the average percentage of mastery of each performance domain for program participants. Circles denote performance values in the distribution contributing to each average (bar). FTE = full-time equivalent. Less than 0.5 FTE, n = 3; ≥ 0.5 FTE, n = 3; < 10 years of experience, n = 3; ≥ 10 years of experience, n = 3.
The authors also investigated the impact of FTE on improvement of SDM upon training. This measure is normally used to compare the workloads across various contexts; in this case, the authors used this measure to compare workloads across multidisciplinary health care participants. Participants ranged from 0.1 to 1.0 as their FTE and were divided into 2 groups: 1 with participants with < 0.5 FTE (n = 3) and another with participants with ≥ 0.5 FTE (n = 3). Improvement in SDM was seen across all the domains irrespective of their FTE.
Moreover, improvements seen were very similar across the groups and were not impacted by FTE of the participants: reasonable options (29% to 30%), decision style preference (30% to 38%), knowledge (21% to 25%), accessibility (16% to 18%), risk tolerance (33% to 41%), trade-off decisions (19% to 27%), readiness (19% to 28%), and values and self-efficacy (33% to 41%; Figure 5). This implies that improvement in SDM is required among all the health care team professionals to improve the quality of patient health care.
Discussion
Over the course of the training interventions, the SDM pilot team evolved in their understanding of SDM. Clinicians who were novices and paternalistic in their approach to using SDM in patient encounters emerged conversant in SDM and expressed their intention to incorporate SDM into their practice settings. On the topic of reasonable options and working knowledge about the various treatment recommendations, some clinicians thought that the sharing of treatment options and general treatment information with patients constituted SDM and, therefore, they thought they were already practicing SDM. For example, during the baseline case role play, it appeared that, when providing treatment choices and product knowledge/information, 1 clinician had not allowed the patient to interject concerns and/or preferences. At the end of this pilot, there was improvement (30% and 27%, respectively) in the use of SDM methodology when discussing reasonable treatment options and a working knowledge of the pros and cons of each treatment; clinicians ensured their patients had a working knowledge of the choices that would be needed to decide. There was only a 13% increase in reasonable options for the social worker as compared to the oncologists, nurse practitioners, and nurse coordinator. This could be because a social worker may have less of an understanding of the science of NSCLC and its treatments as compared to that of physicians or nurses.
Regarding the discussion of risk tolerance during baseline case role play, only about half of the clinicians did discuss and assess the patient’s risk tolerance. If a patient does not have the opportunity to express risk concerns, they may not adhere to therapy.15,16 After the educational intervention that included the didactic SDM presentation and another demonstrating case role play incorporating SDM methodology, the clinicians improved 37% overall.
Decision style preference involves the determination as to whether a patient wants to make their health care decisions by themselves (guided by the clinician), as opposed to those on the other extreme who want their clinician to make all their health care decisions. At baseline, the authors found that only 45% of clinicians asked their patients how they like to make decisions. After implementing educational interventions, the results of these interventions showed that 79% of clinicians asked their patients about their decision style preference at the end of the pilot, representing a 34% improvement. Increased involvement of patients in their health care decisions can foster ownership in the decision, adherence to the treatment, and improved outcomes.
Regarding activation, engagement, and self-efficacy, only 42% of clinicians at baseline asked questions to determine whether their patient would go beyond the standard treatment of their NSCLC to maximize their overall health/wellness or whether they thought there is not much they could do to improve their wellness. Here again, the interventions resulted in an improvement of 37%, where 79% of clinicians were now making this determination. Not only is early treatment important, it is also important that the patient maintain their overall health for improved outcomes.
Posteducational intervention, statistically significant improvement was observed for all SDM domains, with the exceptions of Accessibility and Readiness. Accessibility determines whether a patient will have access to a specific treatment based on issues, such as insurance coverage and cost. Readiness indicates whether a patient has sufficient information to make a decision at that time, or whether the patient needs additional time (eg, to confer with family or to rereview options). Although there was improvement in the Readiness domain of decision quality, the improvement was not statistically significant, because clinicians were already asking their patients this question and making this determination. It was found that Accessibility was a least-focused domain during decision-making, and it was not fully factored into the decision-making process both during preintervention (16%) and postintervention (33%). This domain was not emphasized during the training program, which may explain this finding.
Finally, qualitative semi-structured interviews, comparing baseline preintervention to postintervention interviews, were used to assess change in the clinician’s understanding of SDM.17 At the onset of the program, prior to any training interventions, the mention of SDM to the 6 participants appeared to evoke a response that indicated it was a good practice, but too time consuming to achieve in a fast-paced practice setting environment. Each participant seemed to reflect that the burden of SDM rested on that individual’s shoulders, with the overall perception that SDM implementation was not realistic. However, although they had stressed the time constraints for implementing SDM, they stated that they were already using SDM techniques with their patients. In many instances, clinicians may be addressing some but not all of the SDM domains with their patients. This means that clinicians who are engaged in educational interventions that facilitate their use of SDM with their patients can change a patient’s perspective on their treatment choices for the better. For example, clinicians who provide patients with information to better understand the value of specific treatments may enable them to make better decisions. This could change a patient from being risk averse to becoming risk tolerant with regard to a specific treatment. A patient’s perspective on the domains of decision quality in multiple sclerosis are fluid, not static. By the time the SDM team participants gathered for the focus group, the camaraderie across the group was palpable and they were supportive of one another. They agreed to embark on a plan to implement SDM at their institution but did suggest that follow-up training be part of the plan. Overall, taken together among different domains of Awareness, Assessment, and Activation, physicians showed considerable trends of higher improvement as compared to other professions.
Although this pilot was not conducted during the COVID-19 pandemic, online virtual case role-play simulations and educational trainings that facilitate the incorporation of SDM into the clinical practice setting could be practical, feasible, and acceptable for the busy clinician. COVID-19 has amplified the benefits and importance of interconnectivity and has facilitated its thrust into a new post–COVID-19 era in which virtual technologies will be increasingly used for professional development and clinical care.
Focus group findings
During the focus group discussions, all of the multidisciplinary team members were asked questions about the pilot regarding their experience, what they had learned, whether it was feasible and acceptable to implement SDM in their practice as a result of their learnings, misconceptions they might have had before this training, and in what situations they planned to use SDM. In discussing whether implementation of SDM within the clinical setting was feasible, members of the team believed it could and should be implemented. Many team members stated that, prior to this initiative, they thought all aspects of SDM with each patient needed to be managed by the treating clinician, which represented a time requirement that they did not have in their practice day. However, by tapping into a multidisciplinary approach to SDM, they learned that SDM could be a shared responsibility across a multidisciplinary team that shares the information. By finding out what is important to the patient, the clinician may be able to limit the discussion of treatments to those that are within the patient’s preferences.
Overall, educational training empowered all team members to show pre- to posteducation improvement in SDM. In their own words, members indicated that the educational training and case simulations improved their understanding of SDM and skills for implementing SDM (Table 3). The team found that the training and decision aid tools served as a roadmap for guidance in addressing patients’ goals, values, and preferences, as well as evidence-based treatments. Utilizing these skills, the empowered NSCLC team can improve clinician–patient decision-making and patient-centric care. The training process also facilitated team building and encouraged ongoing participation in SDM, suggesting consideration for team-based approaches.
Table 3:
Focus group comments at completion of the pilot study
| “Take away” messages from Yale NSCLC team members at the focus group |
|---|
| “SDM changed the way I interact with my patients”—MD |
| “Patients need more time to process information before making a decision . . . do not rush the decision process”—MD |
| “SDM training made me more mindful of patient concerns”—NP |
| “Real-time feedback is . . . critical . . . role play is different in your head than when you say it out loud”—MD |
| “I would like to bring this information [SDM] back to my team of pharmacists to show them the process . . . it’s . . . eye-opening”—Pharmacist |
| “Well designed pilot”—NP |
MD, doctor of medicine; NP, nurse practitioner; NSCLC, non–small cell lung cancer; SDM, shared decision-making.
Limitations
This study's small sample size made it difficult to generalize the results and likely introduced increased type II error risk. Also, results were limited to changes in participant understanding and implementation of SDM in the practice setting. Additionally, this study did not evaluate the adaptation of new skills in a clinical practice with patients and also did not thoroughly assess experience. The authors refer to a qualitative study of learner experience by Hakim et al for this.17 Finally, the pre/post cohort design of the study was of short duration and did not include a control group, which could have introduced confounding risks, limiting the authors’ ability to assess for causal relationship between the exposure and outcomes. Overall, this study was an initial pilot. Future studies would benefit from the addition of the patient-level outcomes, longitudinal controlled designs, and more complex cases with a focus on specialty practices.
Conclusion
This study evaluated changes in participant understanding and practice (knowledge and skills) of SDM using an adaptable, practical approach for evaluation and training of clinical staff using a 2-rater evaluation method that followed 7 of 8 domains of SDM pre- and posttraining. Results revealed a significant shift in clinician awareness of a patient’s goals, preferences, and values for care that is unique to each individual. Although immediate exposure effects were noted, future studies are needed to assess sustainability and durability of the training program effects on feasibility, acceptability, utility, and participant knowledge and skills. In particular, the domains-based approach the authors used in the intervention shows promise for standardizing training effectiveness in future studies.
Overall, this pilot study’s results are encouraging and indicate that influencing clinician behaviors through practical training has the power to impact SDM practice, which may in turn beneficially impact the quality of care and associated outcomes for patients. By working in partnership with an interdisciplinary health care team that has the capability to facilitate SDM, patients may have a greater chance to receive the care they prefer when given the opportunity to have an open, honest, and heartfelt discussion about what matters most.
Financial Disclosures.
Dr Adelson reports personal fees from Projects In Knowledge Powered by Kaplan (PIK) during the conduct of the study; other from Genentech, outside the submitted work. Drs Alexander, Davies, and Hakim report personal fees from PIK during the conduct of the study. Dr Agrawal, Ms Ingram, Ms Peterson, and Ms Rudell have no relevant financial relationships to disclose. Dr Oliver reports consulting fees from PIK during the conduct of the study; and limited methodology consulting fees from PIK outside of the submitted work.
Footnotes
Author Contributions: Dr Alexander: Oversight/leadership of all manuscript preparation activities, as well as discussion/limitations/conclusion. Dr Hakim: Introduction and reviews of the manuscript. Ms Rudell, Ms Ingram, and Dr Davies: Methods and review of the manuscript. Dr Agrawal: Statistical analysis. Ms Peterson: Reviews of the manuscript. Dr Adelson: Clinical lead, methods, and review of the manuscript. Dr Oliver: lead methodologist, mentorship of Drs Alexander and Hakim: analysis and reviews and edits of the manuscript.
Conflict of Interest: This work was developed using data from Projects In Knowledge Powered by Kaplan (PIK). The results and findings are entirely the authors’ own and were not influenced by thoughts or opinions from PIK.
Funding: None declared
Data-Sharing Statement: Underlying data are owned by Projects In Knowledge. Data are not available for public access.
References
- 1. Michigan Law Review . Making Health Care Decisions: A Report on the Ethical and Legal Implications of Informed Consent in the Patient-Practitioner Relationship. Volume 1, 82 Mich. L. Rev. 839; 1984. Accessed 16 August 2024. https://repository.law.umich.edu/mlr/vol82/iss4/21 [Google Scholar]
- 2. Elwyn G, Durand MA, Song J, et al. A three-talk model for shared decision making: Multistage consultation process. BMJ. 2017;359:j4891. 10.1136/bmj.j4891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Müller E, Strukava A, Scholl I, et al. Strategies to evaluate healthcare provider trainings in shared decision-making (SDM): A systematic review of evaluation studies. BMJ Open. 2019;9(6):e026488. 10.1136/bmjopen-2018-026488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Elwyn G, Frosch DL, Kobrin S. Implementing shared decision-making: Consider all the consequences. Implement Sci. 2016;11(1):114. 10.1186/s13012-016-0480-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Coates D, Clerke T. Training interventions to equip health care professionals with shared decision-making skills: A systematic scoping review. J Contin Educ Health Prof. 2020;40(2):100–119. 10.1097/CEH.0000000000000289 [DOI] [PubMed] [Google Scholar]
- 6. Norful AA, Dillon J, Baik D, George M, Ye S, Poghosyan L. Instruments to measure shared decision-making in outpatient chronic care: A systematic review and appraisal. J Clin Epidemiol. 2020;121:15–19. 10.1016/j.jclinepi.2020.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Leyland R, Heath M, Neve H, Maynard V. Structured reflection on shared decision making. Clin Teach. 2021;18(1):55–61. 10.1111/tct.13233 [DOI] [PubMed] [Google Scholar]
- 8. Singh Ospina N, Toloza FJK, Barrera F, Bylund CL, Erwin PJ, Montori V. Educational programs to teach shared decision making to medical trainees: A systematic review. Patient Educ Couns. 2020;103(6):1082–1094. 10.1016/j.pec.2019.12.016 [DOI] [PubMed] [Google Scholar]
- 9. Harman SM, Blankenburg R, Satterfield JM, et al. Promoting shared decision-making behaviors during inpatient rounds: A multimodal educational intervention. Acad Med. 2019;94(7):1010–1018. 10.1097/ACM.0000000000002715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kanzaria HK, Chen EH. Shared decision making for the emergency provider: Engaging patients when seconds count. MedEdPORTAL. 2020;16:10936. 10.15766/mep_2374-8265.10936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Müller E, Diesing A, Rosahl A, Scholl I, Härter M, Buchholz A. Evaluation of a shared decision-making communication skills training for physicians treating patients with asthma: A mixed methods study using simulated patients. BMC Health Serv Res. 2019;19(1):612. 10.1186/s12913-019-4445-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bos–van den Hoek DW, Smets EMA, Ali R, et al. A blended learning for general practitioners and nurses on skills to support shared decision-making with patients about palliative cancer treatment: A one-group pre-posttest study. Patient Educ Couns. 2023;112:107712. 10.1016/j.pec.2023.107712 [DOI] [PubMed] [Google Scholar]
- 13. Oliver BJ, Rudell E, Ingram M. A practical approach for developing shared decision-making knowledge, skills, and capability in busy healthcare professionals: Development, methods, and initial experience of a virtual continuing education program for practicing clinicians. Int J Integr Care. 2023;24(2). 10.5334/ijic.6554 [DOI] [Google Scholar]
- 14. Jain P, Jain C, Velcheti V. Role of immune-checkpoint inhibitors in lung cancer. Therapeutic Advances in Respiratory Disease. 2018;12:1753465817750075. 10.1177/1753465817750075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Suh WN, Kong KA, Han Y, et al. Risk factors associated with treatment refusal in lung cancer. Thorac Cancer. 2017;8(5):443–450. 10.1111/1759-7714.12461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. McMullen S, Hess LM, Kim ES, et al. Treatment decisions for advanced non-squamous non-small cell lung cancer: Patient and physician perspectives on maintenance therapy. Patient. 2019;12(2):223–233. 10.1007/s40271-018-0327-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hakim H, Alexander C, Rudell E, et al. Learner experience, acceptability, feasibility, and impact of a simulation-based educational program to build frontline capability for shared decision making in a major academic oncology center caring for people with non-small cell lung cancer: A qualitative study. J Cancer Educ. 2023;27:456–462. 10.1007/s13187-012-0371-y [DOI] [Google Scholar]