Abstract
Role of FDG PET/CT in evaluation of biliary tract diseases remains relatively unexplored. PET/CT with FDG helps in evaluation of both infective / inflammatory as well as neoplastic diseases as increased glucose utilization is observed in both the conditions. In this article, we describe the spectrum of FDG PET/CT findings in various diseases affecting the biliary tract. Role of FDG PET/CT in neoplastic diseases involving the biliary duct has been described at the time of staging and response evaluation; in characterization of the intrahepatic mass (abscess v/s cholangiocarcinoma). In addition, we have discussed about the false positive FDG uptake along the biliary duct stent, which interfere with scan interpretation. Few of the benign conditions described are Langerhans cell histiocytosis and IgG4 related disease involving the biliary duct and adenomyomatosis and Xanthogranulomatous cholecystitis involving the gall bladder.
Keywords: Biliary tract disease, cholangiocarcinoma, fluorodeoxyglucose, gallbladder, positron emission tomography/computerized tomography, xanthogranulomatous cholecystitis
The biliary tract is subject to a wide variety of pathologic abnormalities, which include both benign and malignant etiologies. These conditions include inflammatory, infectious, malignant, congenital, and iatrogenic diseases. Biliary tract cancers (BTCs) include carcinoma gallbladder, cholangiocarcinoma (CCA), and ampullary carcinoma. CCA is subdivided into intrahepatic CCA (iCCA), hilar CCA (hCCA), and extrahepatic CCA (eCCA). BTCs are rare and invasive tumors that account for approximately 0.7% of all malignant tumors in adults; it is the most common hepatobiliary cancer after hepatocellular carcinoma and accounts for 3% of all gastrointestinal malignancies with a 5-year survival rate of only 2%.[1,2,3] Surgery is the only curative treatment; however, the majority of patients with BTC (60%–70%) present with advanced or metastatic disease; therefore, palliative locoregional and systemic therapies are the only options of treatment.[4] The overall survival of patients with iCCA depends on tumor size, number of tumors, positivity for lymph node metastasis, and vascular invasion.[2] Imaging plays a crucial role in the accurate diagnosis and staging of BTC as well as response assessment of therapy.[3] Information provided by conventional imaging techniques (such as computerized tomography [CT] or magnetic resonance imaging) for some patients still remains insufficient. The role of 18F-fluorodeoxyglucose (18F-FDG) positron emission tomography/CT (PET/CT) in the evaluation of biliary tract diseases is relatively unexplored.[5]
Lamarca et al. published a systematic review and meta-analysis on the role of FDG PET/CT for patients with BTC by studying 2125 patients. The role of PET/CT in diagnosis (T), staging (N/M), and relapse of BTC was assessed. The important conclusions of the study include the nonrecommendation of 18-FDG-PET for diagnosis (T) in the absence of cytology/histology. However, the authors recommend PET/CT to be used for staging (N/M) if the identification of occult sites of disease will alter management and also to identify relapse if suspicion persists following standard imaging. FDG PET/CT in the diagnosis of the primary tumor showed a pooled sensitivity of 91.7% (95% confidence interval [CI] 89.9–93.2) but had a low pooled specificity of 51.3% (95% CI 46.4–56.2) with the lowest specificity in hCCA (21.9%) and eCCA (27.7%).[5] CCA exhibits considerable variability in 18F-FDG uptake, which was correlated with a weak expression of hexokinase-2.[6] A pooled sensitivity of 88.4% (95% CI 82.6–92.8) and a pooled specificity of 69.1% (95% CI 63.8–74.1) were reported for the detection of lymph node invasion and a pooled sensitivity of 85.4% (95% CI 79.5–90.2) and a high pooled specificity of 89.7% (95% CI 86.0–92.7) for the detection of distant metastases. FDG PET/CT had a pooled sensitivity of 90.1% (95% CI 84.4–94.3) and a pooled specificity of 83.5% (95% CI 74.4–90.4) for the detection of relapse. The pooled proportion of change in management was observed in 15% (95% CI 11–20). 18-FDG-PET upstaged the disease with the identification of previously unknown sites of disease in 78% of patients.[5] Goel et al., in their prospective study, concluded that FDG PET/CT should be included in the preoperative staging workup of gallbladder cancer, particularly in locally advanced disease as PET/CT detected additional findings in 30.9% and altered the management of 23.4% of the cases due to detection of metastasis [Figures 1–5].[7]
Figure 1.
Staging of intrahepatic cholangiocarcinoma (CCA). A 73 year old female presented with jaundice and pruritis for 1 month with elevated serum CA 19.9 levels of 500 U/L and on routine ultrasonography abdomen imaging was found to have a liver space occupying lesion. 18F fluorodeoxyglucose positron emission tomography/computerized tomography (CT) with triple phase CT abdomen study (a-h, orange and white arrows) revealed a metabolically active lobulated mass in the right lobe of the liver (maximum standardized uptake value of 8.0) showing arterial phase hyperenhancement with negligible washout in the portovenous phase, suggestive of intrahepatic CCA along with few metastatic upper abdominal lymph nodes
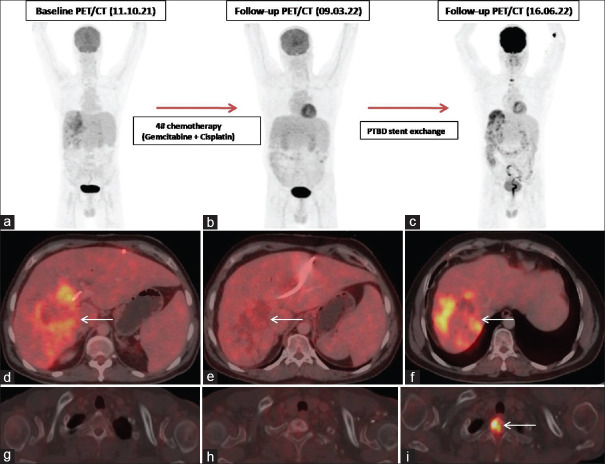
Figure 5.
Case of locally advanced perihilar-cholangiocarcinoma. Baseline PET/CT (a, d, g, white arrows) showed mass in the right lobe of the liver with metastases to multiple abdominal lymph nodes. USG guided FNAC of the mass revealed adenocarcinoma. Post left PTBD catheter exchange and 4 cycles of chemotherapy (Gemcitabine + Cisplatin), FDG PET/CT showed partial response to therapy (b, e, h, white arrows). Patient underwent PTBD stent exchange and follow-up FDG PET/CT was performed at 3months, which showed an interval increase in metabolic activity of the primary neoplastic disease as well as the multiple abdominal lymph nodes; there was interval appearance of a FDG avid lytic lesion in the D1 vertebra (c, f, i, white arrows). Overall scan features were indicative of Disease progression. This case highlights the importance of FDG PET/CT in response assessment of biliary tract cancers
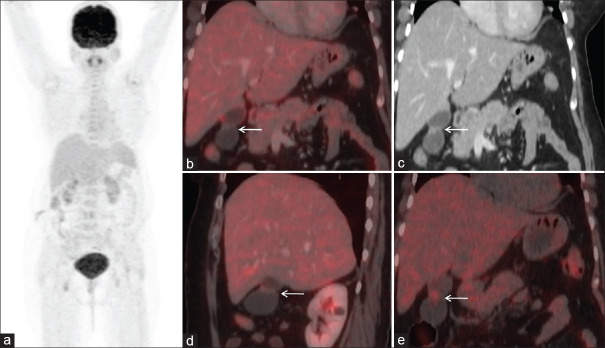
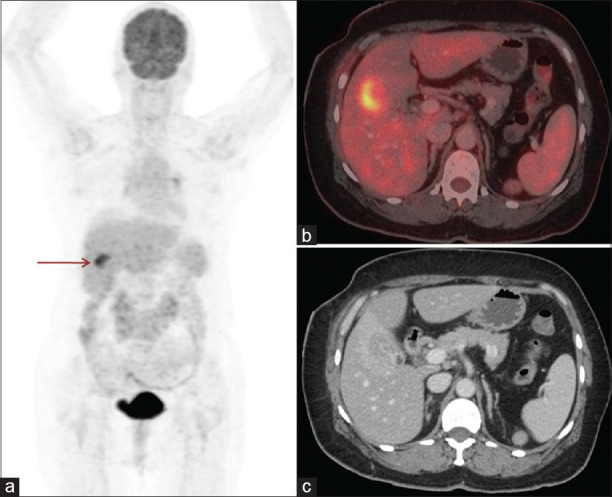
Figure 2.
Staging of extrahepatic cholangiocarcinoma (CCA). A 58 year old male presented with jaundice for 2 months and with elevated serum CA 19.9 levels of 2043 U/mL. 18F fluorodeoxyglucose (FDG) positron emission tomography/computerized tomography (CT) with triple phase CT abdomen study (a-e, orange and white arrows) revealed a focal metabolically active enhancing soft tissue mass (maximum standardized uptake value [SUVmax] of 4.5) involving the distal common bile duct with resultant upstream moderate biliary tract dilatation. Figures 1 and 2 highlight the variability of FDG uptake in CCA depending on the location; as seen, the intrahepatic CCA shows higher SUVmax in comparison to the extrahepatic CCA
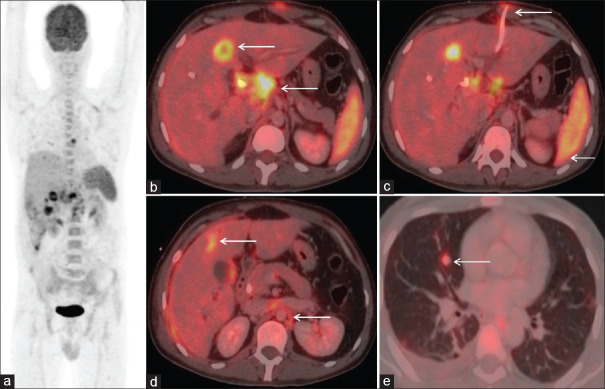
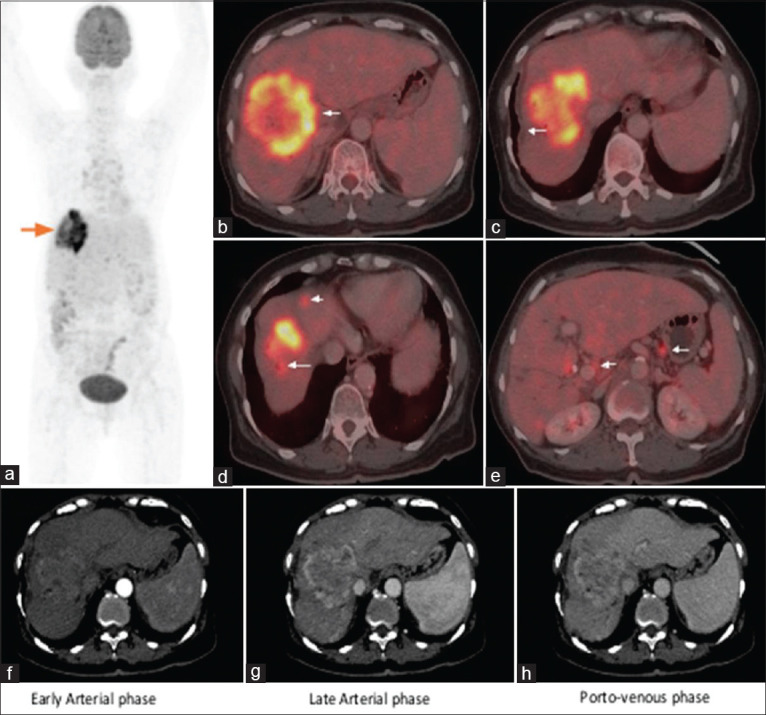
Figure 3.
Characterization of liver space occupying lesion (SOL). 76-year-old woman presented with pain abdomen and loss of weight. Conventional anatomic imaging (both USG abdomen and CT abdomen) findings were favoring evolving abscess. For further evaluation patient was referred for PET/CT. 18F-FDG PET/CT (a-e, white arrows) showed a large hypodense mass with peripheral uptake in right lobe with central necrosis. Additional findings of few discrete FDG avid lesions in segments V & VI and multiple omental & peritoneal nodules also noted. Hence, differential of cholangiocarcinoma was reported. Subsequently biopsy of the liver SOL revealed adenocarcinoma (of biliary origin). FDG uptake is increased in both benign infective / inflammatory and malignant conditions, image guided biopsy is warranted in such cases for final conclusion
However, due to FDG uptake in active infection and inflammation, low specificity in diagnosis and evaluation of biliary tract diseases is reported. Common causes of false positive uptake include infection related false positives within the bile duct, co-existence of biliary stents [Figure 4], various benign conditions such as Tuberculosis, adenomyomatosis and cholecystitis.[5,8,9] Clinical and imaging findings of patients with benign conditions involving the biliary tract such as Langerhans cell histiocytosis (LCH) [Figure 6], IgG4 related sclerosing cholangitis [Figure 7], adenomyomatosis [Figure 8] and Xanthogranulomatous cholecystitis (XGC) [Figure 9] are described.[10,11,12]
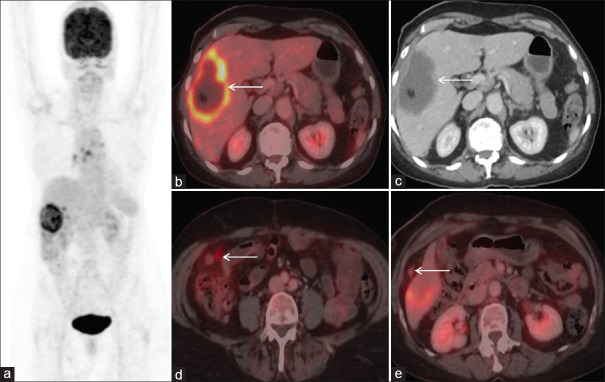
Figure 4.
28-year-old young male case of hilar cholangiocarcinoma (CCA) v/s carcinoma gall bladder (GB) post bilateral PTBD stenting with markedly elevated serum CA-19.9 levels (10,514U/mL) was referred for PET/CT two days after stenting. 18F-FDG PET/CT showed primary neoplastic mass in the porta hepatis region involving the primary biliary confluence, common hepatic duct (CHD), cystic duct and extending to involve the neck & proximal body of gall bladder with resultant mild-to-moderate bilobar IHBR (intrahepatic biliary radicle) dilatation with subtle pneumobilia on the right and metastatic lymph nodes (b, white arrow). Diffuse FDG uptake is noted along the stents (c, white arrow). Patient had disseminated metastatic disease to liver & retroperitoneal lymph nodes (image c, white arrow), omentum & peritoneum (d, white arrow) and bilateral lungs with mild bilateral pleural effusion (e). Also, in the MIP image (a) there is diffuse FDG uptake in spleen and bone marrow indicating activation of reticulo-endothelial system due to underlying active infection / inflammation. So, the final impression in such a case scenario was primary hilar CCA v/s GB with disseminated metastases and with co-existing active infective / inflammatory disease. This case highlights interpretation of PET/CT specially in cases of extrahepatic biliary tract involvement with the presence of stent
Figure 6.
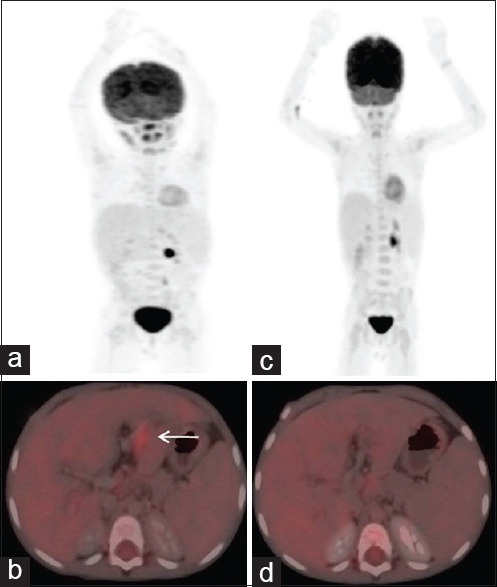
Langerhans cell histiocytosis (LCH) involving the biliary duct. 4-year-old child, case of biopsy proven multisystem LCH with risk organ involvement (liver & lung) presented with secondary sclerosing cholangitis, hepatosplenomegaly & growth failure. Post 2# of chemotherapy according to LCH 4 protocol and followed-by maintenance therapy in 2021, triple phase CT abdomen showed alternating segments of wall thickening with dilatation of the IHBRD and proximal extrahepatic ducts. FDG PET-CT performed showed ill-defined linear hypodensities along the portal vein and its branches with few adjacent subcentimetric cystic areas with mild metabolic activity in segment III of the liver, likely residual metabolically active periportal soft tissue infiltrates (a-b, white arrows). Also, few non metabolic thin-walled air cysts in bilateral lung parenchyma (pulmonary disease involvement) were noted. Post 2 cycles of salvage therapy with cytarabine and cladribine, follow up FDG PET/CT (c-d) revealed interval reduction in metabolic activity of previously noted infiltrate in relation to bile duct in segment III of liver. PSC may be an associated feature in 1-6% of children with LCH and FDG PET/CT can be used for response assessment to differentiate between active and healed lesions much earlier than conventional imaging which may help in adjusting the treatment[11,12]
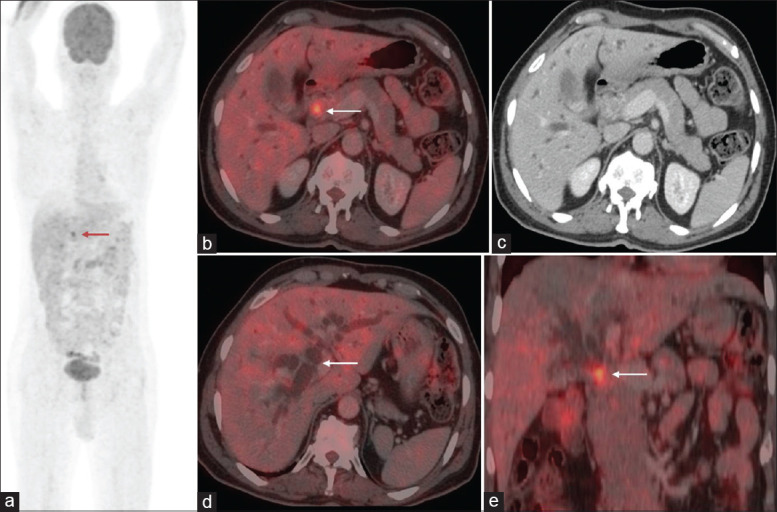
Figure 7.
IgG4 disease. A 41-year-old male, a known case of IgG4 related disease with CBD stricture and associated chronic pancreatitis (pancreatic head biopsy suggesting differential diagnosis of IgG4 related chronic pancreatitis) with serum IgG4 values of 5.86g/dL (0.03-2g/dL). FDG PETCT (a-e, white arrows) revealed intense metabolically active irregular enhancing circumferential wall thickening involving distal CBD down to the ampulla, with upstream dilatation of proximal CBD and bilateral IHBRD with metabolically active porto-caval and peripancreatic lymph nodes with marked diffuse atrophy of pancreas with evidence of abrupt narrowing of MPD at the head of pancreas region, resulting in upstream dilatation of MPD in its full length. Patient was treated with steroids. FDG PET-CT in evaluation of IgG4 related disease allows for early detection of inflammation that may precede structural changes, helps in guiding biopsy and to determine the extent of disease. Autoimmune pancreatitis is the commonest manifestation with IgG4 related sclerosing cholangitis being the most common extra pancreatic manifestation. Patten of FDG accumulation in the affected organs may help in diagnosis of IgG4 related diseases, for instance in pancreatic cancer there is focal FDG uptake compared to diffuse FDG uptake in autoimmune pancreatitis[10]
Figure 8.
Gall bladder adenomyomatosis. 68-year-old woman presented with complaints of pain abdomen; past history of acute necrotising pancreatitis was present. On evaluation with MRCP features of acute pancreatitis with cholelithiasis and segmental adenomyomatosis was reported. FDG PET/CT (a-e, white arrows) showed mildly metabolically active asymmetric hour glass thickening at the mid body region of gall bladder (SUVmax 1.5; FDG uptake remained the same even on the delayed images). Patient underwent simple cholecystectomy and histopathological examination of gall bladder specimen revealed cholecystitis with no evidence of dysplasia or malignancy. Adenomyomatosis is a benign inflammatory condition of the gall bladder with negligible or low FDG avidity (SUVmax<2.5). However, if there is acute inflammatory reaction surrounding the Rokitansky-Aschoff sinuses (RAS) it may show increased 18FDG uptake which may lead to a false positive result. Though FDG PET/CT is not performed for diagnosing adenomyomatosis of gallbladder, it may help in excluding gallbladder carcinoma when there is no significant FDG uptake at the lesion[8,9]
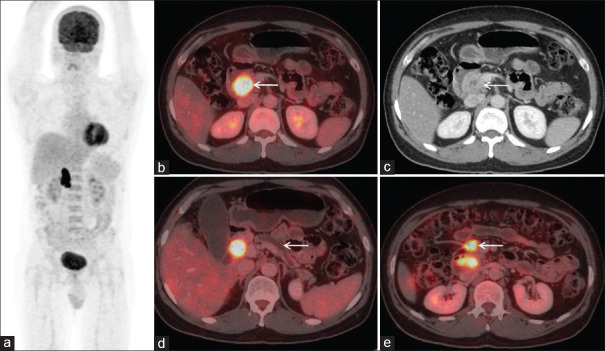
Figure 9.
A 65 year old woman was evaluated for pain abdomen and elevated serum CA 19.9 levels (529.5 U/mL). Computerized tomography (CT) abdomen and magnetic resonance cholangiopancreatography features were suggestive of carcinoma gallbladder (GB). Fluorodeoxyglucose (FDG) positron emission tomography (PET)/CT was done to rule out distant metastases and showed FDG avid heterogeneously enhancing asymmetrical wall thickening involving fundus and body of GB (brown arrow) with few adjacent locoregional lymph nodes (a-c). PET/CT scan findings favor neoplastic disease. She underwent extended cholecystectomy with hilar lymphadenectomy. However, histopathology of the GB specimen revealed xanthogranulomatous cholecystitis (XGC), and the hepatoduodenal lymph node was reactive. FDG PET/CT helps in differentiating benign and malignant GB lesions with sensitivity and specificity ranging from 75% to 78% and 82% to 100%, respectively.[8] However, false positive FDG uptake is noted due to the presence of inflammatory cells in XGC which have high rates of glucose metabolism similar to malignant cells; only histopathology is definitive[8]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published, and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Tariq NU, McNamara MG, Valle JW. Biliary tract cancers: Current knowledge, clinical candidates and future challenges. Cancer Manag Res. 2019;11:2623–42. doi: 10.2147/CMAR.S157092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee Y, Yoo IR, Boo SH, Kim H, Park HL, Hyun OJ. The role of F-18 FDG PET/CT in intrahepatic cholangiocarcinoma. Nucl Med Mol Imaging. 2017;51:69–78. doi: 10.1007/s13139-016-0440-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elias Y, Mariano AT, Jr, Lu Y. Detection of primary malignancy and metastases with FDG PET/CT in patients with cholangiocarcinomas: Lesion-based comparison with contrast enhanced CT. World J Nucl Med. 2016;15:161–6. doi: 10.4103/1450-1147.167605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Manne A, Woods E, Tsung A, Mittra A. Biliary tract cancers: Treatment updates and future directions in the era of precision medicine and immuno-oncology. Front Oncol. 2021;11:768009. doi: 10.3389/fonc.2021.768009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lamarca A, Barriuso J, Chander A, McNamara MG, Hubner RA, ÓReilly D, et al. (18)F-fluorodeoxyglucose positron emission tomography ((18)FDG-PET) for patients with biliary tract cancer: Systematic review and meta-analysis. J Hepatol. 2019;71:115–29. doi: 10.1016/j.jhep.2019.01.038. [DOI] [PubMed] [Google Scholar]
- 6.Paudyal B, Oriuchi N, Paudyal P, Tsushima Y, Higuchi T, Miyakubo M, et al. Clinicopathological presentation of varying 18F-FDG uptake and expression of glucose transporter 1 and hexokinase II in cases of hepatocellular carcinoma and cholangiocellular carcinoma. Ann Nucl Med. 2008;22:83–6. doi: 10.1007/s12149-007-0076-1. [DOI] [PubMed] [Google Scholar]
- 7.Goel S, Aggarwal A, Iqbal A, Gupta M, Rao A, Singh S. 18-FDG PET-CT should be included in preoperative staging of gall bladder cancer. Eur J Surg Oncol. 2020;46:1711–6. doi: 10.1016/j.ejso.2020.04.015. [DOI] [PubMed] [Google Scholar]
- 8.Maldjian PD, Ghesani N, Ahmed S, Liu Y. Adenomyomatosis of the gallbladder: Another cause for a “hot” gallbladder on 18F-FDG PET. AJR Am J Roentgenol. 2007;189:W36–8. doi: 10.2214/AJR.05.1284. [DOI] [PubMed] [Google Scholar]
- 9.Lee KF, Hung EH, Leung HH, Lai PB. A narrative review of gallbladder adenomyomatosis: What we need to know. Ann Transl Med. 2020;8:1600. doi: 10.21037/atm-20-4897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhao Z, Wang Y, Guan Z, Jin J, Huang F, Zhu J. Utility of FDG-PET/CT in the diagnosis of IgG4-related diseases. Clin Exp Rheumatol. 2016;34:119–25. [PubMed] [Google Scholar]
- 11.Jessop S, Crudgington D, London K, Kellie S, Howman Giles R. FDG PET-CT in pediatric langerhans cell histiocytosis. Pediatr Blood Cancer. 2020;67:e28034. doi: 10.1002/pbc.28034. [DOI] [PubMed] [Google Scholar]
- 12.Jain S, Karunanithi S, Singla S, Kumar A, Bal C, Kumar R. 18F-FDG PET/CT in worsening of primary sclerosing cholangitis concomitant with improved langerhans cell histiocytosis. Rev Esp Med Nucl Imagen Mol. 2014;33:386–7. doi: 10.1016/j.remn.2013.12.005. [DOI] [PubMed] [Google Scholar]