Abstract
Spontaneous recanalization of a coronary thrombus is an uncommon finding that may be confounded without intravascular imaging. There is little evidence regarding the functional impact of these lesions, which may be relevant to proper management. We present two cases of recanalized thrombus in which functional testing guided appropriate management.
Key Words: coronary angiography, fractional flow reserve, intravascular ultrasound, percutaneous coronary intervention, thrombus
Graphical Abstract
Spontaneous recanalization of a coronary thrombus (SRCT) is a rare finding on coronary angiography and may be underdiagnosed because of its variable angiographic appearance, which may mimic coronary dissection, unstable plaque, or chronic total occlusion; may be confused with calcium; or may even go unnoticed. The use of advanced imaging techniques such as intravascular ultrasonography or optical coherence tomography (OCT) allows accurate and definitive diagnosis. Nevertheless, the optimal management of these lesions is unclear, and there is little evidence of their functional significance, which could be beneficial in this context. Therefore, 2 cases of SRCT with functional testing are presented for consideration.
Learning Objectives
-
•
To note that the functional assessment of SRCT is a feasible strategy that provides a deeper understanding of the hemodynamic behavior and clinical impact of these lesions.
-
•
To understand that the integration of intravascular imaging and functional testing should be mandatory in the treatment strategy of lesions with misleading clinical significance.
Case 1
A 68-year-old man, a smoker with a history of alcohol abuse and bronchial hyperresponsiveness, was admitted in October 2021 for new-onset exertional angina. His vital signs were normal. Transthoracic echocardiography revealed a nondilated left ventricle with severe systolic dysfunction at the expense of anterior and anterolateral hypokinesis. The troponin analysis yielded negative results. In light of these findings, antiaggregation with 300 mg acetylsalicylic acid was initiated, and catheterization was requested. A radiolucent image was observed in a good-caliber intermedius branch (Figure 1). OCT demonstrated multiple lumens in the proximal vessel with a “honeycomb” appearance, consistent with SRCT (Figures 2A and 2B, Video 1). Given the patient's history of asthma, the use of adenosine to induce vasodilation was avoided. Instead, a nonhyperemic index was performed, which yielded a pathologic value (resting full-cycle ratio of 0.86) (Figure 3). After administration of 300 mg clopidogrel, a drug-eluting stent (DES) was implanted after balloon dilation, with good angiographic results and a negative posttreatment functional study result (Figure 4). After 33 months, the patient remained asymptomatic, with an improvement in left ventricular ejection fraction on transthoracic echocardiography, and he has not experienced any cardiac events (myocardial infarction, heart failure, cardiovascular death).
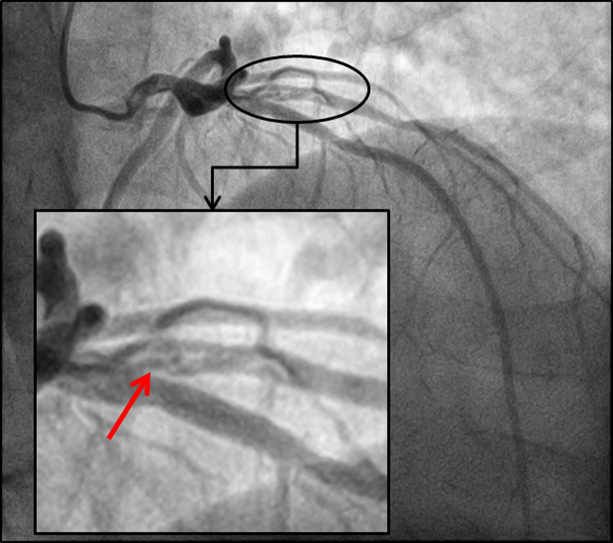
Figure 1.
Coronary Angiography, Right Anterior Oblique Cranial Projection
A radiolucent image is observed in the intermediate branch consistent with recanalized occlusion (arrow). The remaining vessels exhibited no significant lesions.
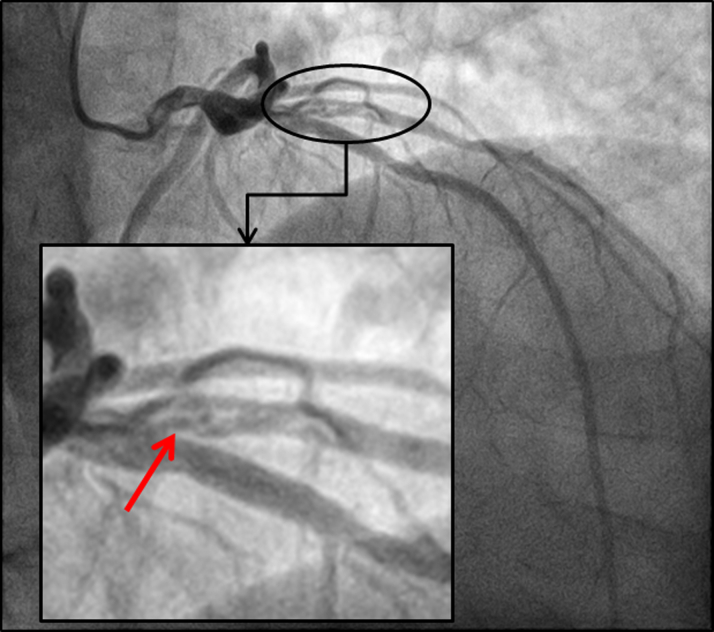
Figure 2.
Optical Coherence Tomography
Cross-sectional (A) and sagittal (B) views of the vessel exhibiting the typical pattern of “spider-web” microchannels.
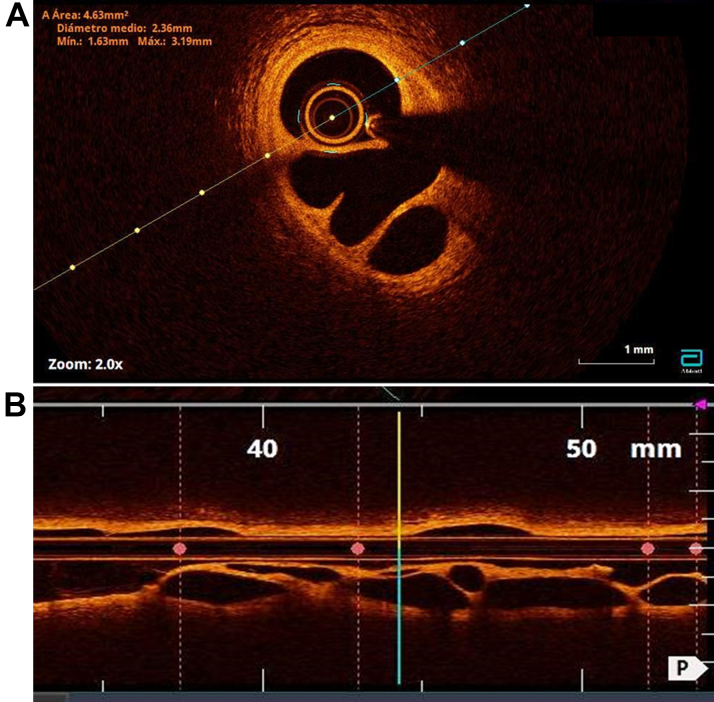
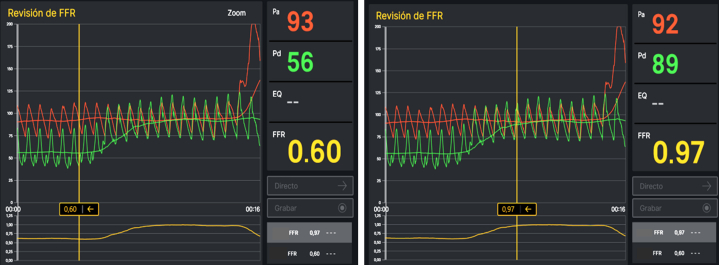
Figure 3.
Functional Study
Study of the intermediate branch with a pressure guidewire demonstrating the functional impact of the lesion (resting full-cycle ratio = 0.86).
Figure 4.
Coronary Angiography and Functional Study
A good angiographic result was achieved after stent implantation, and a negative resting full-cycle ratio value was recorded at the conclusion of the procedure.
Case 2
A 50-year-old man with a history of smoking and dyslipidemia was admitted in March 2023 for acute coronary syndrome with anterior ST-segment elevation. His vital signs were normal, and 300 mg of acetylsalicylic acid and 180 mg ticagrelor were administered. He underwent emergent catheterization, which revealed a subocclusive lesion in the middle left anterior descending artery. An opaque lesion was observed in the mid-right coronary artery (RCA) with diffuse disease of the distal vessel (Figure 5). At that time, angioplasty was performed in the left anterior descending artery, and a DES was implanted, with good results. Two weeks later, the patient was scheduled for a second procedure to study the RCA lesions. In the middle RCA, the opaque lesion was observed by intravascular ultrasonography, confirming the “Swiss cheese” morphology, and was functionally significant after pressure guidewire measurement (baseline fractional flow reserve [FFR] of 0.69) (Figures 6 and 7). Therefore, after balloon dilation, a DES was implanted at that level using a provisional stenting strategy, with good angiographic results and FFR normalization (post-hyperemia FFR 0.94) (Figures 7 and 8). Subsequently, the patient remained asymptomatic and had not experienced any cardiac events after 15 months of follow-up.
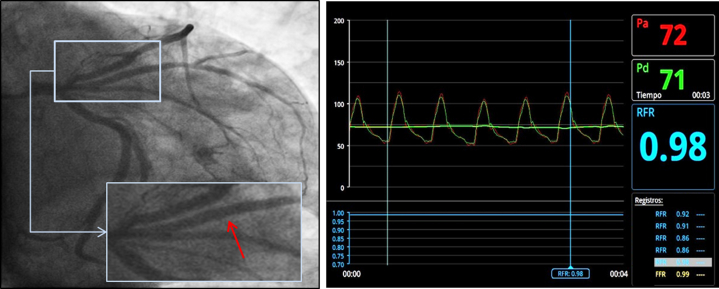
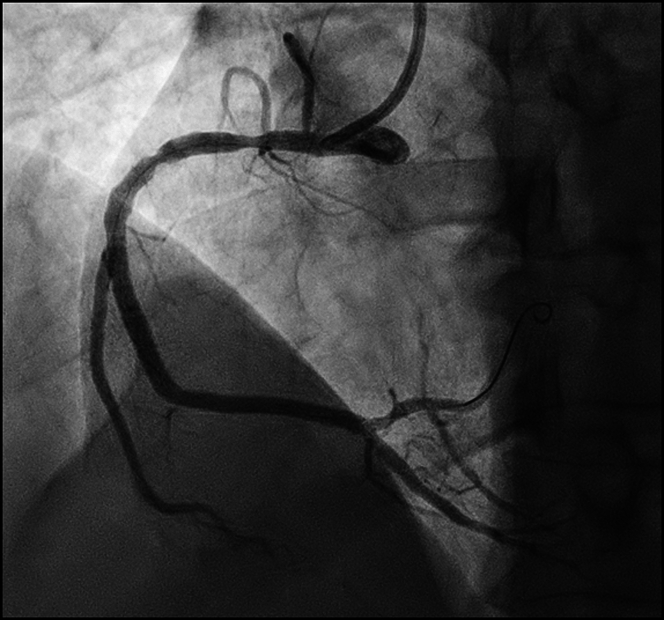
Figure 5.
Coronary Angiography, Right Anterior Oblique Projection
A nonsignificant stenosis in the proximal right coronary artery was detected, and a translucent image in the middle, after the bifurcation with the right ventricular branch, with the appearance of a spontaneous recanalized lesion (arrow).
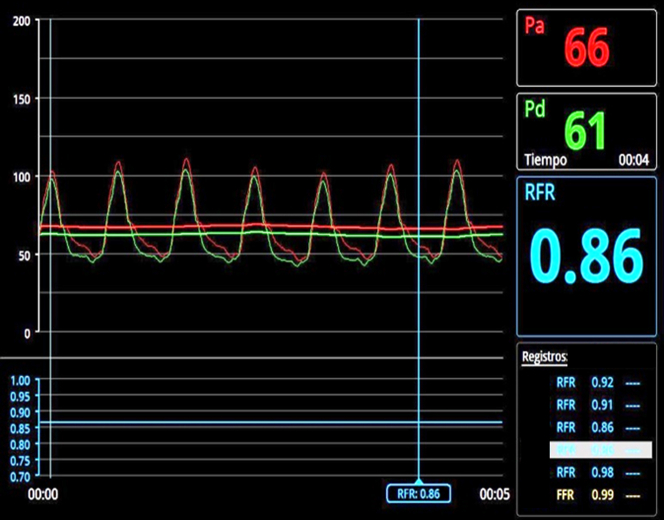
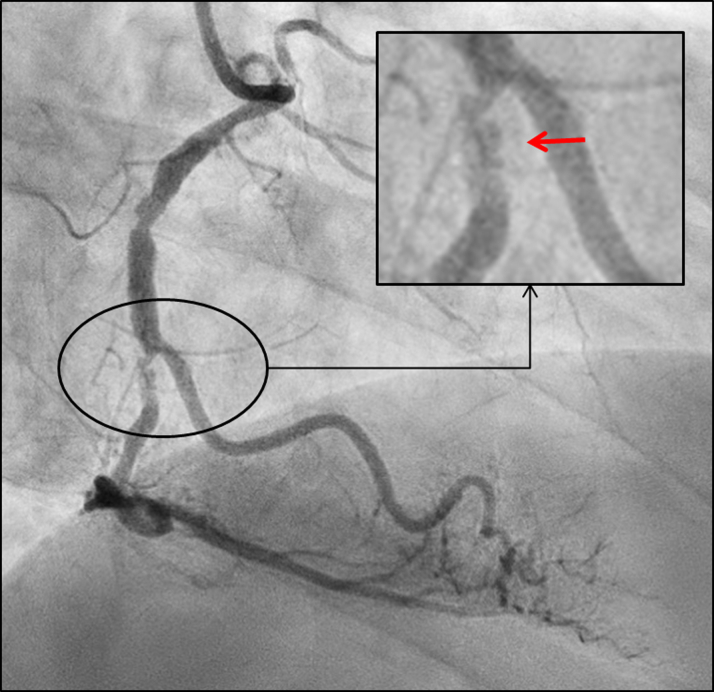
Figure 6.
Intravascular Ultrasonography
Cross-sectional view of the middle right coronary artery revealing the typical “honeycomb” pattern (A. raw image; B, colored dots indicating the microchannels).
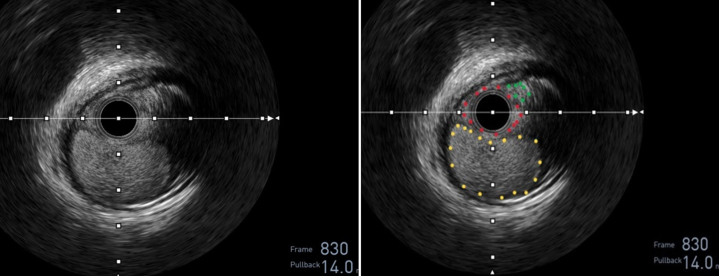
Figure 7.
Functional Study With Pressure Guidewire
The lesion exhibited significant drop in the distal vessel pressure (baseline fractional flow reserve distal (left) and proximal (right) to the lesion during retrieval of the guidewire (0.60 and 0.97, respectively).
Figure 8.
Coronary Angiography, Left Anterior Oblique Projection
A good angiographic result was achieved after stent implantation in the middle and distal right coronary artery.
Discussion
Spontaneous coronary recanalization was first documented in autopsy pathology studies, but its angiographic appearance has been described as braided, opaque, or pseudodissection. Later, this finding was correlated with imaging techniques showing multiple microchannels separated by smooth septa with high signal intensity, strong reflection, and weak attenuation, subsequently described as a “spider web,” “Swiss cheese,” “lotus root,” or “honeycomb” image.1, 2, 3, 4
The mechanism by which these microchannels are formed remains unknown. However, 3 main causes have been described.2,5 The most commonly reported cause is recanalization of a thrombus from a complicated plaque (OCT showing in situ dissection of an atherosclerotic plaque or other markers of complication such as rupture, erosion, or ulceration). Other potential causes include spontaneous coronary dissection or an embolus. In these cases we would mainly observe a healthy vessel or the dissection itself on the wall in the absence of the aforementioned atherosclerosis or complication markers. Other mechanisms, such as thrombosis in situ, can be postulated in the presence of ectatic vessels.2,3
The prevalence of this finding is only 0.1%, and it can affect any vessel (more frequently described in the RCA), although our first case is curiously the first described in an intermedius branch, to our knowledge. Its clinical presentation is highly variable, and it may present as stable angina, acute coronary syndrome, silent ischemia, or an incidental angiographic finding, being asymptomatic in up to one-third of patients.6
Angiographic severity alone is an inadequate criterion for determining the need for percutaneous coronary intervention, given the poor correlation with symptomatic status. In certain instances, the hemodynamic repercussions of SRCT are demonstrated either by the presence of symptoms or by a positive stress test result.1,2 In other patients, ischemia can be demonstrated by performing the functional test, which is especially useful in lesions that are not apparently severe. Canal tortuosity may explain the discrepancy between lumen reduction and symptomatic impact. This could be also useful in cases with paucisymptomatic or inconclusive ischemia test results. Unfortunately, functional testing has been used in a limited number of cases.
Although a standard therapeutic approach has not yet been identified, the treatment of these lesions with DES, drug-eluting balloons, and bioresorbable scaffolds has been the most reported in the literature, with generally favorable short-term and long-term outcomes.2,4,5 Although there is no documented evidence of microcirculation studies in these patients, given the possibility of embolization in the acute phase of the lesions, it is possible to identify alterations in microvascular disease indices.
Owing to the scarcity of studies using functional testing in SRCT, we believe it is important to present our 2 cases, which demonstrate a significant functional impairment before revascularization that disappeared after revascularization, and the patients demonstrated favorable evolution without cardiac events or mortality during the follow-up period.
We initially relied on this technique because the validity of pressure wire–guided revascularization compared with angiographic guidance has been well established in meta-analyses in atherosclerotic disease,7 but we assume that the physiological mechanism that produces positive results may be equally applicable in SCRT. It is noteworthy that the majority of patients with SRCT who underwent pressure guidance demonstrated a positive FFR. To date, only 1 case with a negative FFR has been identified that was managed medically, with a favorable outcome at 13 months of follow-up.6 This continues to raise questions about the optimal treatment approach, given the absence of cases in the literature with negative FFR without percutaneous coronary intervention.
Conclusions
Guiding the revascularization procedure of SRCT with functional testing seems to be a feasible and reliable strategy. Further studies are required to substantiate these findings.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For a supplemental video, please see the online version of this paper.
Appendix
Optical Coherence Tomography
Multiple microchannels separated by smooth septa with high signal intensity, strong reflection, and weak attenuation were detected, exhibiting the typical pattern of a “honeycomb” structure.
References
- 1.Vijayvergiya R., Kasinadhuni G., Revaiah P.C., et al. Role of intravascular imaging for the diagnosis of recanalized coronary thrombus. Cardiovasc Revasc Med. 2021;32:13–17. doi: 10.1016/j.carrev.2020.12.031. [DOI] [PubMed] [Google Scholar]
- 2.Spinu M., Homorodean C., Ober M.C., et al. Optical coherence tomography for in vivo identification, characterization and optimal treatment of spontaneous recanalization of coronary thrombus. In Vivo. 2020;34(2):745–756. doi: 10.21873/invivo.11834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kahata M., Satomi N., Otsuka M., et al. Honeycomb-like structure in spontaneous recanalized coronary thrombus demonstrated by serial angiograms: a case report. Eur Heart J Case Rep. 2020;4(5):1–4. doi: 10.1093/ehjcr/ytaa250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Souteyrand G., Valladier M., Amabile N., et al. Diagnosis and management of spontaneously recanalized coronary thrombus guided by optical coherence tomography: lessons from the French “lotus root” registry. Circ J. 2018;82(3):783–790. doi: 10.1253/circj.CJ-17-0810. [DOI] [PubMed] [Google Scholar]
- 5.Xu T., Shrestha R., Pan T., et al. Anatomical features and clinical outcome of a honeycomb-like structure in the coronary artery: reports from 16 consecutive patients. Coron Artery Dis. 2020;31(3):222–229. doi: 10.1097/MCA.0000000000000822. [DOI] [PubMed] [Google Scholar]
- 6.Gupta A., Rao K.R., Reddy S.S., et al. Optical coherence tomography characterization of spontaneous recanalized coronary thrombus: single center experience. J Thoracic Cardiovasc Res. 2022;14(4):220–227. doi: 10.34172/jcvtr.2022.30504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mangiacapra F, Paolucci L, Johnson NP et al. Systematic review and meta-analysis of randomized and nonrandomized studies on fractional flow reserve-guided revascularization. Rev Esp Cardiol (Engl Ed). Published online March 1, 2024. https://doi.org/10.1016/j.rec.2024.02.010 [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Optical Coherence Tomography
Multiple microchannels separated by smooth septa with high signal intensity, strong reflection, and weak attenuation were detected, exhibiting the typical pattern of a “honeycomb” structure.