Abstract
Eclipsed mitral regurgitation (MR) is a rare phenomenon of transient severe MR in patients with normal left ventricular function. This paper presents a case of a patient with recurrent heart failure exacerbations and transient, positional severe MR consistent with eclipsed MR, which improved after mitral transcatheter edge-to-edge repair.
Key Words: cardiac imaging, echocardiography, eclipsed mitral regurgitation, heart failure, valve disease
Graphical Abstract
History of Present Illness
An 83-year-old woman presented for outpatient evaluation of progressive dyspnea on exertion and multiple admissions for acute heart failure. She underwent bilateral pleural catheter placement at another institution for persistent transudative pleural effusions despite medical therapy for presumed heart failure with preserved ejection fraction (HFpEF). Due to her progressive dyspnea, she was referred for further evaluation.
Learning Objectives
-
•
To define eclipsed MR.
-
•
To identify underlying mechanisms of eclipsed MR using imaging and provocative maneuvers.
-
•
To identify treatment strategies of eclipsed MR based on underlying mechanisms.
Past Medical History
Her medical history was significant for chronic hypertension and paroxysmal atrial fibrillation status post 2 prior pulmonary vein isolation procedures. The second ablation was complicated by acute pericarditis, which was successfully treated with medical therapy. A subsequent transthoracic echocardiogram (TTE) revealed mild mitral and tricuspid regurgitation.
Differential Diagnosis
The differential diagnosis for her progressive dyspnea, recurrent heart failure exacerbations, and pleural effusions included HFpEF, stiff left atrial (LA) syndrome, dynamic mitral regurgitation (MR), cardiac amyloidosis, and constrictive pericarditis.
Investigations
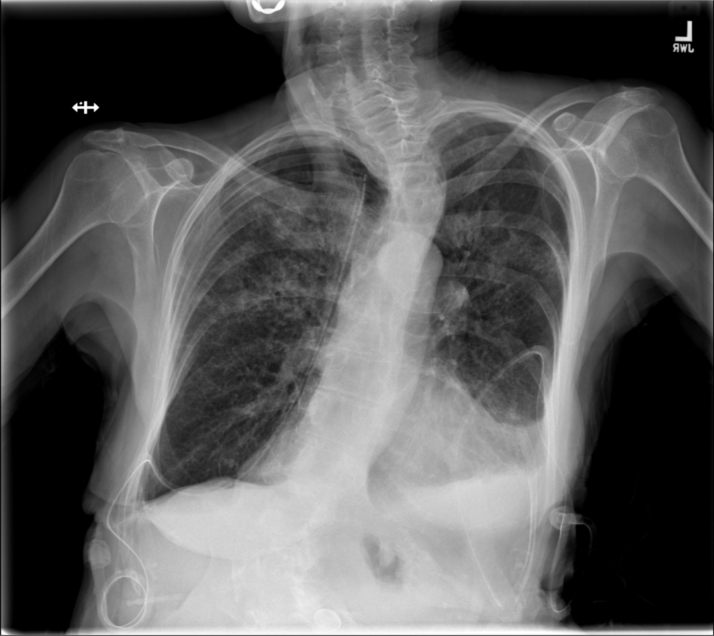
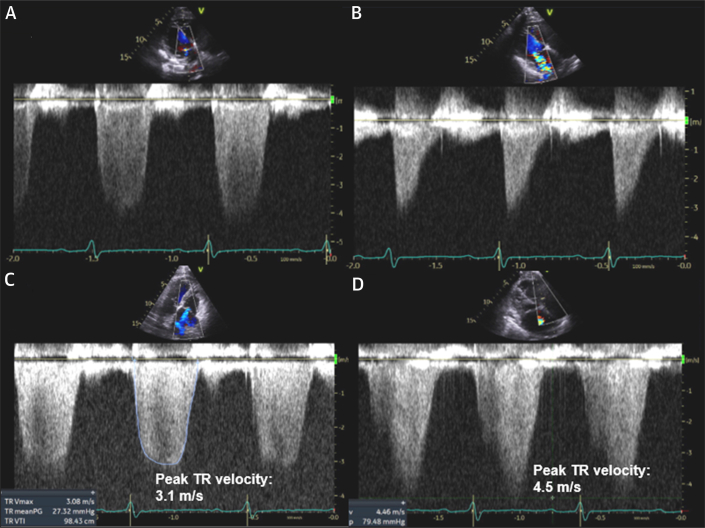
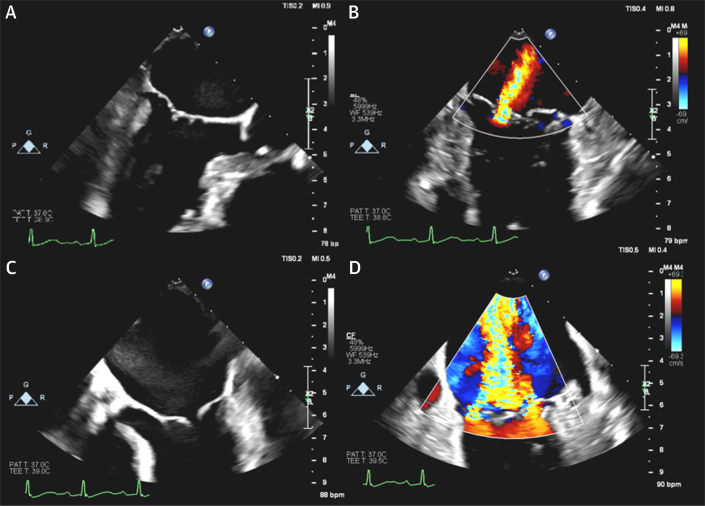
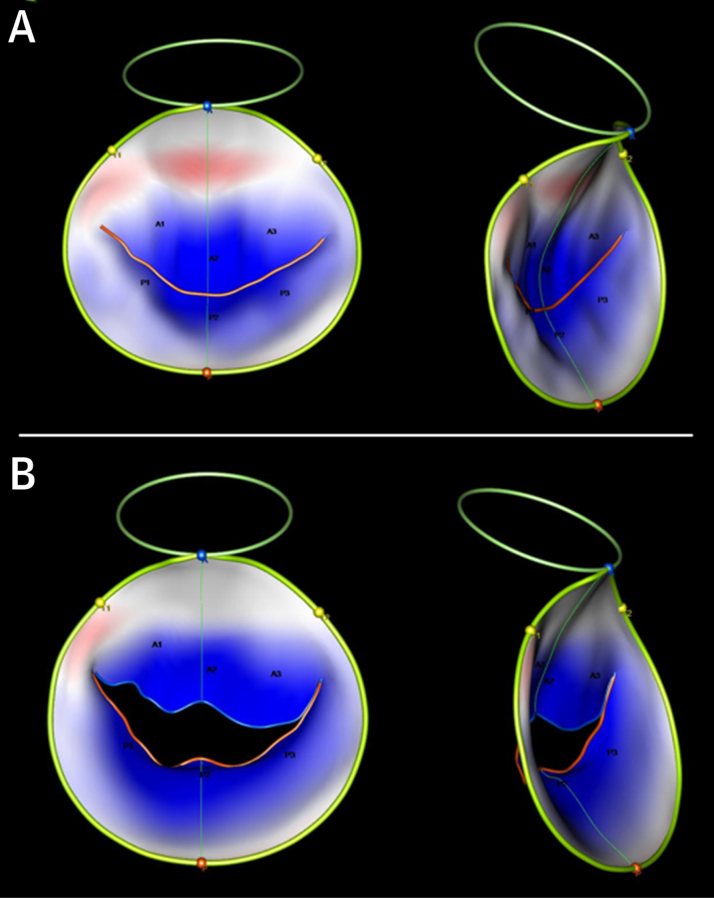
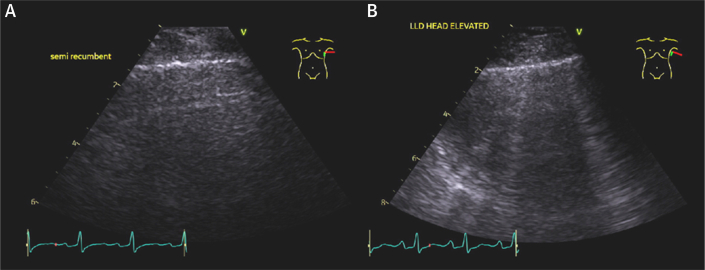
Due to acute heart failure symptomology, she was directly admitted to inpatient cardiology. Physical examination revealed crackles in the bilateral lung bases, jugular venous distention, and lower extremity edema. Chest radiograph showed a left-sided pleural effusion and thoracic scoliosis (Figure 1). A TTE in the semirecumbent position showed normal left ventricular (LV) size, preserved ejection fraction (62%), moderate central MR, and an estimated right ventricular systolic pressure (RVSP) of 48 mm Hg. On transition to the left lateral decubitus position (LLD), she developed new dyspnea and hypoxia, prompting additional imaging. This revealed new torrential MR with incomplete mitral leaflet coaptation and an increase in RVSP to 75 mm Hg (Figure 2, Video 1). These findings, in addition to new pulmonary vein systolic flow reversals, were redemonstrated on transesophageal echocardiogram (TEE) (Figure 3, Video 2) after additional diuresis and optimization of her volume status. With positional changes, 3-dimensional modeling of the mitral value using the 3-dimensional TEE datasets showed no significant difference in mitral value annular shape or measured diameter; however, there was an increase in tenting volume from 3.9 to 5.3 cm3 (Figure 4). Despite aggressive diuresis, repeat TTE showed similar findings including positional worsening of pulmonary edema by lung ultrasound with increased B-lines while positioned LLD (Figure 5).
Figure 1.
Chest Radiograph
Chest radiograph showing pulmonary vascular congestions, left pleural effusion, normal cardiac silhouette size, and thoracic scoliosis.
Figure 2.
Mitral and Tricuspid Continuous-Wave Doppler Waveforms in Semirecumbent and Left Lateral Decubitus Positions
Supine position: (A) baseline mitral regurgitation waveform and (C) peak tricuspid regurgitation velocity of 3.1 m/s and right ventricular systolic pressure of 48 mm Hg. Left lateral decubitus position: (B) triangular-shaped mitral regurgitation Doppler waveform consistent with rapid equalization of pressures between the left atrium and left ventricle and (D) acute increase in peak tricuspid regurgitation velocity to 4.5 m/s and right ventricular systolic pressure to 75 mm Hg.
Figure 3.
Transesophageal Echocardiogram in Systole
(A) Semirecumbent position at 30°: mitral leaflets coapt normally in this position with (B) moderate mitral regurgitation originating on the medial aspect of A2-P2. Left lateral decubitus position: (C) development of a large coaptation gap across the entire mitral valve commissure with (D) resultant torrential mitral regurgitation.
Figure 4.
3-Dimensional Mitral Valve Model
Three-dimensional mitral valve model showing an increase in tenting volume (blue shading) from (A) 3.9 cm3 in supine position to (B) 5.3 cm3 in left lateral decubitus position.
Figure 5.
Ultrasound of Left Lower Lung Lobe
Ultrasound of left lower lung lobe showing (A) minimal pulmonary edema in supine position with (B) an acute increase in pulmonary edema and B-lines in the left lateral decubitus position.
Management
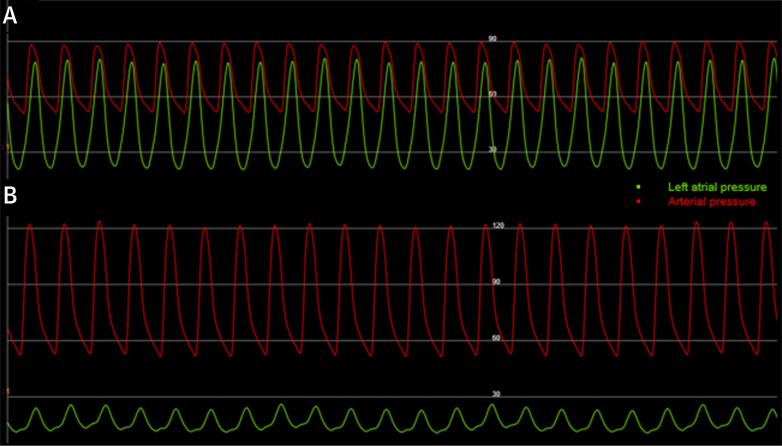
She was deemed a high-risk surgical candidate due to her age and frailty; therefore, a mitral transcatheter edge-to-edge repair (TEER) was pursued. Under TEE guidance, transeptal puncture was performed for LA access with pressure transduction showing severely elevated mean LA pressure of 45 mm Hg with V waves reaching 79 mm Hg. A single mitral valve clip was deployed in the A2-P2 segment of the mitral valve with immediate improvement in mean LA and V-wave pressures to 15 and 22 mm Hg, respectively (Figure 6). Intraprocedural TEE showed improvement in MR severity (Video 3), resolution of pulmonary vein systolic flow reversals, and improvement in mitral valve tenting volume to 3.3 cm3.
Figure 6.
Intraprocedural Pressure Recording
(A) Pretranscatheter edge-to-edge repair (mean left atrial pressure 45 mm Hg and V waves 79 mm Hg). (B) Post-transcatheter edge-to-edge repair (mean left atrial pressure 17 mm Hg and V waves 25 mm Hg).
Discussion
Eclipsed MR was originally described in 2008 and was defined as transient severe MR in patients with normal LV function and dimensions in the absence of epicardial coronary artery disease.1 There are few cases reported to date; therefore, the true prevalence remains unknown. This patient’s baseline characteristics share many common features with those previously reported,1,2 including postmenopausal women with multiple cardiovascular risk factors (eg, hypertension, diabetes), microvascular dysfunction, and conduction or rhythm disorders (eg, atrial fibrillation). Patients often presented with recurrent, severe heart failure exacerbations and pulmonary edema, frequently requiring intensive care admission.1, 2, 3 In many cases, the patients’ presentations were previously attributed to HFpEF because the features of eclipsed MR were frequently absent on imaging without provocation. The dynamic nature of this condition may contribute to this being a clinically under-recognized, and therefore poorly understood, entity.
Various underlying mechanisms of eclipsed MR have been described in the literature. In a case series of 3 patients, Avierinos et al1 described transient massive MR with apical leaflet tenting triggered by methylergonovine injection. Nitroglycerin administration resulted in resolution of these findings in all 3 patients, leading the authors to conclude that epicardial coronary vasospasm was the likely culprit.1 A few other cases reported similar associations,2 but not all. In a case series of 6 patients with eclipsed MR, Breen et al2 described additional mechanisms including a rate-dependent left bundle branch block, provoked with exercise, resulting in apical leaflet tenting and reduced coaptation. Additionally, they described 2 patients with eclipsed MR that was provoked with maneuvers to increase LV preload (eg, leg elevation, LLD positioning). TEE in these patients showed an increase in the mitral annular diameter with severe MR; however, no leaflet tenting was observed.2 We hypothesize that the mechanism of eclipsed MR in the present case was due to papillary muscle displacement with movement to the LLD position, possibly related to the patient’s severe scoliosis, leading to leaflet tenting and malcoaptation. Increased LV loading conditions in the LLD position may have contributed to these dynamic changes as well. The lack of significant change in mitral annulus dimensions with 3-dimensional modeling argues against changes in the mitral annulus as a cause of the transient MR in this case.
The optimal therapeutic strategy for eclipsed MR is unclear and likely depends on the underlying mechanism. For instance, in 2 patients with severe MR provoked by left bundle branch block reported by Breen et al,2 one patient had resolution of heart failure exacerbations with cardiac resynchronization therapy, whereas another died a few days postoperatively after surgical mitral valve replacement (MVR). Similarly, those with underlying coronary vasospasm also had resolution of heart failure episodes with calcium channel blockers without the need for surgical intervention.2 In the reported cases undergoing surgical MVR, many had complicated postoperative courses with high morbidity and mortality.2,4 In a case series by Milleron et al,4 5 patients underwent MVR and 2 died a few days postoperatively, whereas the others required extended intensive care stays for inotropic support. There is only one previously reported case treated with mitral TEER in a patient with exercise-induced eclipsed MR.3 Similar to this case, the present patient had an excellent postprocedural course after mitral TEER with a dramatic improvement in her MR, LA pressures, and symptoms. Given the high morbidity and mortality associated with surgical intervention, TEER may be an attractive option for these high-risk patients and should be considered in appropriate candidates. Further data are needed to determine the underlying prevalence, mechanisms, and optimal therapy for this complex condition.
Follow-Up
After mitral TEER, the patient reported a substantial and persistent improvement in her dyspnea and a reduction in pleural drain output. She was discharged home on low-dose diuretics, and pleural drains were removed at 3-month follow-up.
Conclusions
In postmenopausal women with cardiovascular risk factors and unexplained episodic heart failure, consider evaluation for eclipsed MR with imaging and provocative maneuvers. Treatment should be guided by the underlying mechanism. Given the high morbidity and mortality associated with surgical MVR, mitral TEER may be an effective alternative for these high-risk patients.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this paper.
Appendix
Premitral Transcatheter Edge-to-Edge Repair Transthoracic Echocardiogram
Premitral Transcatheter Edge-to-Edge Repair Transesophageal Echocardiogram
Postmitral Transcatheter Edge-to-Edge Repair Transesophageal Echocardiogram
References
- 1.Avierinos J.F., Thuny F., Tafanelli L., et al. Eclipsed mitral regurgitation: a new form of functional mitral regurgitation for an unusual cause of heart failure with normal ejection fraction. Cardiology. 2008;110(1):29–34. doi: 10.1159/000109403. [DOI] [PubMed] [Google Scholar]
- 2.Breen T.J., Jain C.C., Tan N.Y., Miranda W.R., Nishimura R.A. Paroxysmal severe mitral regurgitation. Mayo Clin Proc. 2021;96(1):86–91. doi: 10.1016/j.mayocp.2020.06.001. [DOI] [PubMed] [Google Scholar]
- 3.Umei T.C., Shiraishi Y., Tsuruta H., et al. Transcatheter mitral valve repair effective and safe for refractory eclipsed mitral regurgitation-induced cardiogenic shock: a case report. Circ Cardiovasc Imaging. 2021;14(7):e012641. doi: 10.1161/CIRCIMAGING.121.012641. [DOI] [PubMed] [Google Scholar]
- 4.Milleron O., Bouleti C., Mazouz S., et al. Eclipsed mitral regurgitation: an unusual cause of acute heart failure. Eur Heart J Cardiovasc Imaging. 2017;18(10):1163–1169. doi: 10.1093/ehjci/jew192. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Premitral Transcatheter Edge-to-Edge Repair Transthoracic Echocardiogram
Premitral Transcatheter Edge-to-Edge Repair Transesophageal Echocardiogram
Postmitral Transcatheter Edge-to-Edge Repair Transesophageal Echocardiogram