Abstract
Background
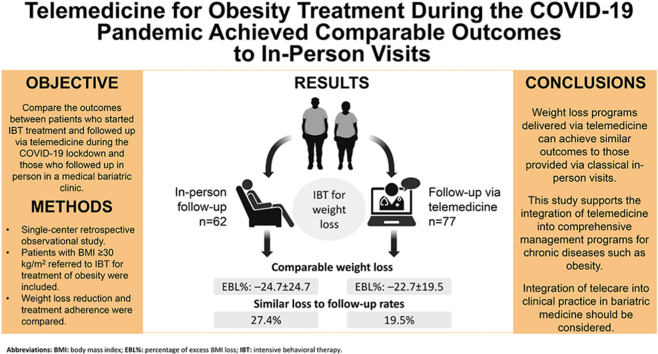
During the COVID-19 pandemic, weight loss programs rapidly transitioned to a virtual model, replacing in-person clinic visits. We sought to compare the observed weight loss and adherence to treatment between patients referred for intensive behavioral therapy (IBT) who were treated via telemedicine and those treated in person.
Methods
After IRB approval, we conducted a retrospective observational study of patients referred for clinical bariatric IBT between January 2019 and June 2021 who were followed in person or via telemedicine. The primary endpoint was the percentage of excess BMI loss (EBL%); secondary endpoints included treatment adherence, duration of follow-up, and number of completed visits.
Results
During the study period, 139 patients were seen for at least one IBT session for weight management: 62 were followed up in person (IP) and 77 via telemedicine (TM). The mean age, baseline BMI, and follow-up duration between the groups were similar. In the IP and TM groups, the EBL% was −24.7 ± 24.7 and −22.7 ± 19.5 (P = 0.989) and loss to follow-up after the first visit was 27.4% and 19.5% (P = 0.269), respectively.
Conclusion
For the management of obesity, weight loss programs delivered via telemedicine can achieve similar outcomes to those provided via classical in-person visits. This study suggests that the integration of telecare into clinical practice in bariatric medicine should be considered in the future. Emerging technologies may allow adequate patient follow-up in multiple scenarios, specifically non-critical chronic disorders, and bring unanticipated benefits for patients and healthcare providers.
Keywords: Healthcare delivery, Intensive behavioral therapy, Obesity, Obesity management, Telehealth, Telemedicine
Graphical abstract
1. Introduction
During the COVID-19 pandemic, healthcare systems were “between a rock and a hard place” worldwide. Healthcare providers were forced to transform and adapt their practices to reduce risks of unnecessary exposure while simultaneously not compromising patient outcomes. Although unprepared for this seismic change, the adoption of telemedicine among most medical specialties significantly surged during and after the pandemic as an approach to overcoming these circumstances [1]. Furthermore, as the pandemic worsened, some additional reasons emerged to support the adoption of telemedicine beyond infection prevention [2,3]. Increased acceptance and familiarity with the modality by the patients, specific regulatory changes, new reimbursement policies, perceived reduction in healthcare access barriers, and cost reductions were among these facilitators [[2], [3], [4], [5]].
Notably, transitioning to or incorporating telehealth models was certainly faster in specific clinical scenarios and specialties like endocrinology and mental health [6]. For example, a large number of common chronic conditions in adults such as diabetes, hypothyroidism, mental health disorders, and obesity need frequent medical monitoring and physician counseling; however, the treatment and clinical decision-making does not necessarily entail repeated physical examinations. In most of these conditions, key clinical indicators facilitate the diagnosis and the therapy and indicate the prognosis. For example, glucose or HbA1c in patients with diabetes; thyroid-stimulating hormone (TSH) and thyroxine (T4) levels in patients with hypothyroidism; specific clinical or risk scores in patients with mental health disorders; and weight or body mass index (BMI) in patients with obesity.
Interestingly, obesity is a complex condition associated with a high burden of disease and numerous related complications (i.e., endocrine disorders, cardiovascular disease, cancer, thromboembolic disease) [[7], [8], [9]]. Its treatment requires a multidisciplinary approach involving specialties such as psychology, family medicine, internal medicine, bariatric medicine, endocrinology, and bariatric surgery [10]. Nevertheless, for most patients, the starting therapeutic point is life style changes [11]. In this particular scenario, patient counseling as well as close monitoring of the key indicator (body weight) are critical. Therefore, weight loss programs, especially those using effective non-pharmacological strategies such as intensive behavioral therapy (IBT) [[12], [13], [14], [15], [16]], appear to be suitable for delivery via telemedicine. However, there is a paucity of data on patient outcomes treated for obesity with IBT via telemedicine.
We aimed to compare the outcomes between patients who started IBT treatment and followed up via telemedicine during the COVID-19 lockdown and those who followed up in person in a medical bariatric clinic the previous year. We hypothesized that the observed weight loss and treatment adherence were similar between the groups (H0).
2. Methods
2.1. Study design and settings
This single-center retrospective observational study analyzed de-identified data obtained from a prospectively maintained database of new patients who underwent IBT for weight loss between January 2019 and December 2021 by a single bariatric clinical professional (S. Munir) at St. Joseph's Hospital and Medical Center, Phoenix, AZ, U.S.A. The research protocol, analysis, and publication of the data were approved under the Norton Thoracic Institute (NTI) Foregut Umbrella Protocol (PHXU-21–500-136–73-18, project approval date: January 6, 2023) by the NTI Committee and The Institutional Review Board of St. Joseph's Hospital and Medical Center. Written patient consent was waived due to the study design, and good practice guidelines were followed according to the Declaration of Helsinki. The STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) statement and checklist were followed to ensure the high quality of the manuscript contents (Online Resource 1).
2.2. Study population
Consecutive patients with BMI ≥30 kg/m2 referred by any specialty to a clinical bariatrician (i.e., obesity medicine specialist) for IBT for the treatment of obesity who completed an initial appointment between January 2019 and June 2021 were identified. Patients with a history of bariatric surgery, lung transplant candidates or recipients, and those with incomplete records were excluded from the analysis. Two time periods were selected to create the cohorts, one before and one after the beginning of the COVID-19 lockdown. Patients in the first group (IP) attended an initial in-person visit between January 2019 and January 2020 and were subsequently followed up in the clinic within the IBT program until March 2020. The second group (TM) comprised patients who attended an initial virtual visit between June 2020 and June 2021 and were followed up using the same modality through December 2021.
2.3. Variables and data management
De-identified data was prospectively collected by one author (S. Munir) and stored in a secure database (Research Electronic Data Capture) at each patient visit, ensuring data consistency and accuracy (rather than retrospectively extracted from patient charts). The dataset included baseline demographic and anthropometric variables (i.e., sex, age, weight, height, BMI, and years of education), information related to the IBT intervention (i.e., modality type, primary medical indication for referral to obesity treatment, referral source, number of visits completed, total days under follow-up), presence of comorbidities (i.e., arterial hypertension, diabetes, hyperlipidemia, pulmonary disease, obstructive sleep apnea, degenerative disc disease, gastroesophageal reflux or hiatal hernia, mental health disorders, and others), and anthropometric data at each follow-up (i.e., weight and BMI). In-person visits included the measurement of patients' weights by the clinician. In contrast, the weight of subjects who attended telehealth appointments was self-measured using home scales or extracted from recent weights recorded during other medical appointments (i.e., ±7 days) if available.
2.4. Intensive behavioral therapy program
This program is provided by a single specialized medical bariatric physician. It is focused on intensive lifestyle modification by utilizing motivational interviewing, cognitive behavioral therapy, storytelling and role-playing, teaching coping skills and healthy eating habits, addressing food and other addictions, discussing patients' budgets, addressing the need for physical activity and barriers to physical activity, and counseling for body image and family-specific issues. Both IP and TM groups had standard visit calendars (i.e., initial visit of 60 min, second visit of 60 min at week two, and third visit of 30 min at week 5; subsequent visits are 30 min monthly until the determined goals are accomplished). The time between visits is reduced in cases where additional follow-up is required according to the obesity medicine specialist. If further treatment is required (due to, for example, not reaching expected goals, identification of eating disorders, or adjustments to medication doses), patients are referred to the indicated specialists (i.e., psychiatrist, endocrinologist, etc.).
2.5. Endpoints
The primary endpoint was the percentage of excess body mass index loss (EBL%); its formula was established as [(last follow-up BMI – initial visit BMI)/(initial visit BMI – 25)] × 100. Secondary endpoints included: i) loss to follow-up, defined as the proportion of patients who did not complete at least two visits within the IBT program, ii) length of the intervention (i.e., total days that each patient was followed), and iii) the number of completed visits within the program.
2.6. Data analysis
Descriptive statistics were applied to analyze the cohort characteristics; count and percentage are reported for categorical variables, whereas mean with standard deviation or median with interquartile range (IQR) are reported for continuous variables. Differences between IP and TM groups were assessed using Pearson's chi-squared for categorical variables. For continuous variables, distribution was determined using Q-Q plots and the Shapiro-Wilk test; in the case of normal distribution, the Student's t-test was used to compare the groups, and the Mann–Whitney U test was used when parametric assumptions were not satisfied. Spearman's rank correlation coefficient was employed to explore associations between covariates. Importantly, for primary endpoint analysis, patients who dropped out after the initial visit were excluded. The significance level (α) was set at 0.05. The software used for the analysis was SPSS Statistics v29.0 (IBM, SPSS Inc. Armonk, NY, USA).
3. Results
3.1. Demographic and clinical characteristics
During the study period, 147 patients were referred to the IBT program for weight loss guided by a single obesity medicine specialist. Five subjects were removed due to a history of lung transplantation and three because they were lung-transplant candidates, resulting in 139 that were seen for at least one IBT session: 62 in the IP group and 77 in the TM group (Fig. 1).
Fig. 1.
Study flow diagram.
Both groups were predominantly female (IP, 53 [85.5%]; TM, 60 [77.9%]), and most patients (IP, 46 [74.2%]; TM, 57 [74%]) had completed at least 12 years of formal education (i.e., starting from primary education). The mean age and baseline BMI were 51.5 ± 13.3 years and 39.6 ± 7.6 kg/m2 for the IP group and 50.2 ± 14.8 years and 41.5 ± 8.5 kg/m2 for the TM group. The most common comorbidity in both groups was hyperlipidemia, followed by diabetes mellitus in the IP group and gastroesophageal reflux disease (GERD) in the TM group. Besides weight, baseline characteristics, including BMI, were similar between the groups (Table 1). Importantly, 32 subjects (17 in the IP group and 15 in the TM group) were excluded from statistical analysis of the primary endpoint due to the lack of a follow-up visit within the pre-specified time frame. However, baseline characteristics were similar between the revised groups (Table 1), with the exception of mental health disorders (anxiety or depression), which were more prevalent in the TM group (38.7% vs. 17.8%, P = 0.020).
Table 1.
Baseline demographic and clinical characteristics.
| Covariate | IP (n = 62) | TM (n = 77) | P-value | IP with ≥2 visits (n = 45) | TM with ≥2 visits (n = 62) | P-value |
|---|---|---|---|---|---|---|
| Demographic and anthropometric | ||||||
| Sex, female | 53 (85.5) | 60 (77.9) | 0.256 | 37 (82.2) | 47 (75.8) | 0.636 |
| Age, years | 51.5 ± 13.3 | 50.2 ± 14.8 | 0.675 | 51.8 ± 13.9 | 50.7 ± 13.8 | 0.677 |
| Weight, kg | 105.5 ± 22 | 115.6 ± 26.4 | 0.044 | 109.1 ± 22.5 | 113.2 ± 24.9 | 0.574 |
| BMI, kg/m2 | 39.6 ± 7.6 | 41.5 ± 8.5 | 0.422 | 40.2 ± 7.5 | 40.5 ± 7.8 | 0.877 |
| Formal education | ||||||
| Years of education | 14.3 ± 2.4 | 14.1 ± 2.2 | 0.724 | 14.3 ± 2.6 | 14.2 ± 2.2 | 0.812 |
| <10 years | 2 (3.2) | 2 (2.6) | 0.880 | 2 (4.4) | 1 (1.6) | 0.852 |
| 10–12 years | 13 (21) | 18 (23.4) | 10 (22.2) | 14 (22.6) | ||
| 13–14 years | 21 (33.9) | 30 (38.9) | 14 (31.1) | 24 (38.7) | ||
| 15–16 years | 16 (25.8) | 19 (24.7) | 12 (26.7) | 16 (25.8) | ||
| 17–18 years | 7 (11.3) | 7 (9.1) | 5 (11.1) | 6 (9.7) | ||
| >18 years | 2 (3.2) | 1 (1.3) | 2 (4.4) | 1 (1.6) | ||
| Unknown | 1 (1.6) | 0 (0) | 0 (0) | 0 (0) | ||
| Comorbidities | ||||||
| Arterial hypertension | 24 (38.7) | 37 (48.1) | 0.270 | 20 (44.4) | 32 (51.6) | 0.464 |
| Prediabetes or diabetes mellitus | 25 (40.3) | 28 (36.4) | 0.228 | 19 (42.2) | 27 (43.4) | 0.891 |
| Hyperlipidemia | 28 (45.4) | 42 (54.5) | 0.271 | 21 (46.7) | 34 (54.8) | 0.404 |
| Pulmonary disease | 15 (24.2) | 26 (33.8) | 0.768 | 11 (24.4) | 13 (21) | 0.670 |
| OSA | 24 (38.7) | 26 (33.8) | 0.546 | 20 (44.4) | 24 (38.7) | 0.552 |
| Degenerative disc disease | 8 (12.9) | 13 (16.9) | 0.515 | 5 (11.1) | 12 (19.4) | 0.250 |
| GERD/HH | 24 (38.7) | 40 (51.9) | 0.120 | 22 (48.9) | 30 (48.4) | 0.959 |
| Mental health disorders | 12 (19.4) | 26 (22.8) | 0.058 | 8 (17.8) | 24 (38.7) | 0.020 |
| Other conditions | 49 (79) | 66 (85.7) | 0.300 | 34 (75.6) | 54 (87.1) | 0.123 |
Continuous values are presented as mean and standard deviation. Categorical variables are presented as count and proportions. Bold p-values represent statistical significance at p < 0.05. Abbreviations: BMI: body mass index; GERD: gastroesophageal reflux disease; HH: hiatal hernia; IP: in-person modality group; OSA: obstructive sleep apnea; TM: telemedicine modality group.
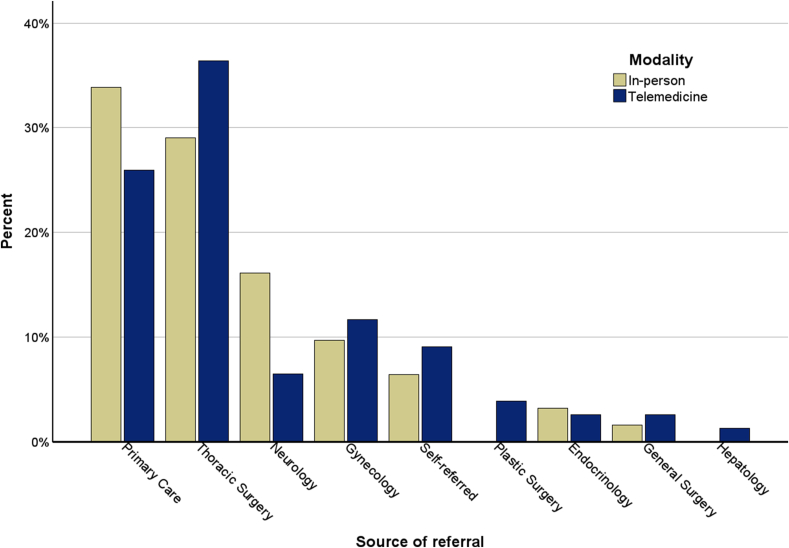
All patients were referred primarily for the management of obesity, with all having one or more complications. Table 2 presents the primary indication for referral; the leading cause in both groups was GERD with or without hiatal hernia and obesity. Other primary indications for the referral to obesity treatment included diabetes mellitus, hypertension, degenerative disc disease, polycystic ovary syndrome, and non-end-stage pulmonary diseases (i.e., idiopathic pulmonary fibrosis or chronic obstructive pulmonary disease). The most frequent referral sources in both groups were primary care physicians and thoracic surgeons (Fig. 2).
Table 2.
Primary indication for referral to management of obesity with intensive behavioral therapy (IBT).
| Covariate | IP (n = 62) | TM (n = 77) | P-value | IP with ≥2 visits (n = 45) | TM with ≥2 visits (n = 62) | P-value |
|---|---|---|---|---|---|---|
| Primary indication for referral to IBT program | ||||||
| Chronic back pain | 2 (3.2) | 0 (0) | 0.826 | 1 (2.2) | 0 (0) | 0.238 |
| Chronic cephalea | 2 (3.2) | 0 (0) | 0.826 | 2 (4.4) | 0 (0) | 0.094 |
| Chronic heart failure | 1 (1.6) | 1 (1.3) | 0.877 | 1 (2.2) | 1 (1.6) | 0.818 |
| Degenerative disc disease | 1 (1.6) | 5 (6.5) | 0.159 | 1 (2.2) | 5 (8.1) | 0.195 |
| Prediabetes or diabetes mellitus | 7 (11.3) | 9 (11.7) | 0.942 | 4 (8.9) | 9 (14.5) | 0.379 |
| GERD/HH | 13 (21) | 27 (35.1) | 0.069 | 13 (28.9) | 17 (27.4) | 0.867 |
| Hyperlipidemia | 0 (0) | 4 (5.2) | 0.069 | 0 (0) | 4 (6.5) | 0.082 |
| Hypertension | 6 (9.7) | 3 (3.9) | 0.169 | 5 (11.1) | 3 (4.8) | 0.223 |
| Incisional hernia | 1 (1.6) | 2 (2.6) | 0.702 | 1 (2.2) | 2 (3.2) | 0.756 |
| Obesity | 7 (11.3) | 12 (15.6) | 0.463 | 4 (8.9) | 9 (14.5) | 0.379 |
| Other conditions | 5 (8) | 7 (9.1) | 0.830 | 3 (6.7) | 6 (9.7) | 0.579 |
| Other endocrinological disorders | 1 (1.6) | 0 (0) | 0.263 | 1 (2.2) | 0 (0) | 0.238 |
| Other neurological disorders | 4 (6.5) | 1 (1.3) | 0.105 | 2 (4.4) | 0 (0) | 0.094 |
| Polycystic ovary syndrome | 4 (6.5) | 3 (3.9) | 0.493 | 2 (4.4) | 3 (4.8) | 0.924 |
| Pulmonary disease | 8 (12.9) | 3 (3.9) | 0.051 | 5 (11.1) | 3 (4.8) | 0.223 |
Variables are presented as count and proportions. Bold p-values represent statistical significance at p < 0.05. Abbreviations: GERD: gastro-esophageal reflux disease; HH: hiatal hernia; IP: in-person modality group; TM: telemedicine modality group.
Fig. 2.
Distribution of referral specialties across the groups.
3.2. Adherence to treatment
There was a higher proportion of loss to follow-up among the IP group than the TM group; however, this difference was not statistically significant (IP, 27.4% vs. TM, 19.5%, P = 0.269). The median total duration of the intervention (IP, 77 days [IQR 28–161] vs. TM, 74 days [IQR 22–153], P = 0.466) and the number of completed visits within the program (IP, 4 [3–7] vs. TM, 4 [][2–7], P = 0.585) were similar between both groups. Table 3 summarizes the data on secondary endpoints.
Table 3.
Adherence to treatment.
| IP (n = 62) | TM (n = 77) | P-value | |
|---|---|---|---|
| Adherence to treatment | |||
| Loss of follow-up | 17 (27.4) | 15 (19.5) | 0.269 |
| Duration of interventiona | |||
| Number of completed visits, median | 4 [3–7] | 4 [2–7] | 0.585 |
| Duration of follow-up, days | 77 [28–161] | 74.5 [22–153] | 0.466 |
Continuous values are presented as medians and interquartile range, and categorical variables are presented as count and proportions. Bold p-values represent statistical significance at p < 0.05. Abbreviations: IP: in-person modality group; TM: telemedicine modality group.
Calculated only for patients who completed ≥2 visits.
3.3. Bariatric outcomes
Weight loss was similar between the groups: mean EBL% of −24.7 ± 24.7 and −22.7 ± 19.5 in the IP and TM groups, respectively (P = 0.989; Fig. 3). By the same token, although not considered an a priori study endpoint, the percentage weight change did not differ between the groups (IP: –8.75 ± 9.13 vs. TM: –8.56 ± 7.92, P = 0.890). Of note, regardless of the modality of treatment, a higher EBL% was correlated with a greater number of years of formal education, rs= (−0.286 [CI95: −0.461, −0.089], P = 0.004). Moreover, the efficacy of IBT was strongly correlated with the number of completed visits by each participant, rs= (−0.741 [CI95: −0.820, −0.636], P < 0.001) as well as the duration of the intervention, rs= (−0.713 [CI95: −0.800, −0.597], P < 0.001).
Fig. 3.
Comparison of percentage of excess body mass index loss (EBL%) between both groups. The H0 hypothesis was accepted using the Mann–Whitney U test.
4. Discussion
This study provides valuable insights into understanding patient follow-up and interventions for chronic conditions such as obesity via telemedicine. A comparable efficacy of intervention was noted among patients receiving IBT remotely and those undergoing traditional in-person care (EBL% −24.7 ± 24.7 vs.–22.7 ± 19.5, P = 0.989). Moreover, although not statistically significant, the loss to follow-up trended lower among patients receiving virtual follow-ups (IP, 27.4% vs. TM, 19.5%, P = 0.269). Together these findings suggest that the adoption of telemedicine for patient follow-up in well-selected chronic conditions and using adequate interventions/treatments does not compromise patient outcomes but improves healthcare access and adherence to treatment most likely due to the removal of geographic or travel-associated costs barriers.
Our findings are aligned with the growing body of evidence supporting the implementation and efficacy of remote IBT for obesity treatment [16,17]. A study conducted by Alencar et al. [17] in 2019 comparing weight loss of patients participating in a telehealth-based program to a control group (i.e., no intervention) revealed a significant difference in weight loss between groups (7.2 ± 4.4 vs. 1.5 ± 4.1 kg, P < 0.05). Moreover, a recent study published in 2022 by Tchang et al. [16] demonstrated that patients undergoing IBT via telemedicine or in-person during COVID-19 had a similar percentage of weight change (IP, −4.3% vs. TM, −5.8%, P = 0.41). In this study, the authors also accounted for prescribed weight-loss medications, which were similar between groups.
We also found that weight loss was significantly correlated with a greater number of formal years of education and the number of completed visits for both groups, which is in line with the association between the educational level of an individual or population and their overall health status [18]. This points to the important role of patient selection when using telehealth models. Healthcare providers are responsible to assess the “candidacy” of each individual before enrolling them into a specific remote follow-up program. Because this study was conducted in a lockdown situation, we were not able to choose which patients would benefit the most from each modality of care. However, under typical conditions, clinicians should be aware of not only the patient's education level but also access to technologies, proficiency in their use, and most importantly the overall patient condition.
On the other hand, it is essential to recognize that during the COVID-19 pandemic, stay-at-home orders had a significant overall negative impact on patient's health and interposed some limitations. Almandoz et al. [19] documented that 69.6% of individuals with obesity reported more difficulty achieving weight loss goals. Also the general population experience an increased prevalence of mental health disorders such as anxiety and depression (which was also found in our study) [20]. Interestingly, despite these adverse challenges, our study demonstrated that similar outcomes and clinical goals can be achieved via telemedicine.
Further, from a public health perspective, the accessibility and convenience afforded by telemedicine allow it to reach a larger patient population (which is important for chronic diseases with increased prevalence such as diabetes or obesity), potentially improving population-level health outcomes [21]. Interestingly a systematic review conducted in 2022 by De Simone et al. [22] assessed the implementation of telehealth during COVID-19 across different stakeholders. Clinicians were prone to present positive attitudes regarding the implementation of video telehealth visits, and patients reported higher satisfaction and a strong interest to continue care under this modality. In our experience and aligned with the evidence, healthcare providers may also experience unexpected benefits from the proper implementation of telemedicine [23,24]. These benefits include time optimization, schedule flexibility, and a potential reduction in burnout [24].
While emergent technologies are potent resources for patients, providers, and healthcare systems, their use comes with some challenges [21]. Telemedicine is susceptible to variable internal motivation experienced by patients, the loss of meaningful in-person doctor-patient interactions, technical issue, privacy concerns, and perceived lower treatment intensity [25]. Hence, there should be a strong rationale behind implementing a remote patient follow-up program. We believe that remote monitoring holds the potential to decrease unnecessary clinic visits for stable patients and improve the efficiency of healthcare practitioners in specific scenarios. Ultimately, adequate integration of telemedicine into health systems has the potential to transform clinical practice and benefit patient care, specifically in well-suited specialties such as endocrinology or bariatric medicine.
5. Limitations
Our study has some limitations. Due to its single-center, retrospective, observational design, there was a small sample size and lack of randomization, which limited the interpretation of results to hypothesis-generating conclusions; however, all the data was collected prospectively. Moreover, the referral source was heterogeneous, and the different time periods of the groups (i.e., before and during the COVID-19 pandemic) may have affected the health habits or behaviors of patients in each group. However, the demographic and clinical baseline characteristics of patients in each group were comparable. Importantly, we could not obtain data regarding some confounding factors including the use of medications (i.e., GLP-1 analogs, insulin, etc.) that could affect body weight and hence the study results. Notably, most of the data obtained from the TM group relies on self-reported weights, and the accuracy of the measurements cannot be guaranteed. Thus, the results from this and other studies need to be confirmed by an objective assessment of reported weight changes by conducting a non-inferiority, randomized controlled trial.
6. Conclusions
This study demonstrated that guided therapy for treating obesity via telemedicine provided similar results in terms of EBL% and treatment adherence to in-person therapy. This data supports the integration of telemedicine into comprehensive management programs for chronic diseases such as obesity where frequently repeated physical examination is not absolutely necessary. As telehealth models become an integral part of healthcare delivery, studies of their effectiveness for specific interventions can provide valuable evidence to help shape the future of clinical practices across diverse, well-suited specialties for telehealth, including bariatric medicine.
6.1. Key takeaways
-
•
Guided IBT for treating obesity via telemedicine provides clinical outcomes in terms of weight loss similar to in-person therapy.
-
•
Treatment adherence for weight loss was not compromised when using telemedicine; conversely, the loss to follow-up trended lower among patients receiving virtual follow-ups.
-
•
Integrating telemedicine and telehealth technologies into comprehensive management programs for obesity may bring unanticipated benefits for patients and healthcare providers.
Author contributions
Conception and design: A.L, S.M and S.K.M. Data collection: S.M. Assembly of data and data analysis: A.L, R.S and S.K.M, Drafting of the manuscript: A.L and R.S. Substantial contribution to revision of the manuscript critically for important intellectual content: A.L, S.M and S.K.M. All the authors approved the final manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethics
The research protocol, analysis, and publication of the data were approved under the Norton Thoracic Institute (NTI) Foregut Umbrella Protocol (PHXU-21–500-136–73-18, date: January 6, 2023) by the NTI Research Committee and The Institutional Review Board of St. Joseph's Hospital and Medical Center. Written patient consent was waived due to the study design, and good practice guidelines were followed according to the Declaration of Helsinki.
Declaration of artificial intelligence (AI) and AI-assisted technologies
During the preparation of this work the author(s) did not use AI tools.
Data accessibility statement
The data analyzed in this study is stored in a secure Research cannot be shared outside of those authorized as research staff per protocol. Access to this dataset requires IRB approval; if needed, direct to the corresponding author.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors thank Kristine Nally for her editorial assistance.
Footnotes
Meeting presentation: Part of this data was presented as a poster at the annual meeting of The Obesity Society (Obesity Week), October 14–17, 2023, Dallas, Texas.
Contributor Information
Andrés R. Latorre-Rodríguez, Email: andres.latorre@commonspirit.org.
Raj H. Shah, Email: rajshah@arizona.edu.
Seema Munir, Email: seema.n.munir@gmail.com.
Sumeet K. Mittal, Email: sumeet.mittal@commonspirit.org.
References
- 1.Doraiswamy S., Abraham A., Mamtani R., Cheema S. Use of telehealth during the COVID-19 pandemic: scoping review. J Med Internet Res. 2020;22 doi: 10.2196/24087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson J.T., Bouchacourt L.M., Sussman K.L., Bright L.F., Wilcox G.B. Telehealth adoption during the COVID-19 pandemic: a social media textual and network analysis. DIGITAL HEALTH. 2022;8 doi: 10.1177/20552076221090041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shaver J. The state of telehealth before and after the COVID-19 pandemic. Prim Care Clin Off Pract. 2022;49:517–530. doi: 10.1016/j.pop.2022.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harris A., Hinman R.S., Lawford B.J., Egerton T., Keating C., Brown C., Metcalf B., Spiers L., Sumithran P., Quicke J.G., Bennell K.L. Cost‐effectiveness of telehealth‐delivered exercise and dietary weight loss programs for knee osteoarthritis within a twelve‐month randomized trial. Arthritis Care Res. 2023;75:1311–1319. doi: 10.1002/acr.25022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wade V.A., Karnon J., Elshaug A.G., Hiller J.E. A systematic review of economic analyses of telehealth services using real time video communication. BMC Health Serv Res. 2010;10:233. doi: 10.1186/1472-6963-10-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garcia J.P., Avila F.R., Torres-Guzman R.A., Maita K.C., Lunde J.J., Coffey J.D., Demaerschalk B.M., Forte A.J. A narrative review of telemedicine and its adoption across specialties. mHealth. 2024;10:19. doi: 10.21037/mhealth-23-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blokhin I.O., Lentz S.R. Mechanisms of thrombosis in obesity. Curr Opin Hematol. 2013;20:437–444. doi: 10.1097/MOH.0b013e3283634443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pati S., Irfan W., Jameel A., Ahmed S., Shahid R.K. Obesity and cancer: a current overview of Epidemiology, pathogenesis, outcomes, and management. Cancers. 2023;15:485. doi: 10.3390/cancers15020485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Powell-Wiley T.M., Poirier P., Burke L.E., Després J.-P., Gordon-Larsen P., Lavie C.J., Lear S.A., Ndumele C.E., Neeland I.J., Sanders P., St-Onge M.-P., On behalf of the American Heart Association Council on L., Cardiometabolic H., Council on C., Stroke N., Council on Clinical C., Council on E., Prevention, Stroke C Obesity and cardiovascular disease: a scientific statement from the American heart association. Circulation. 2021;143 doi: 10.1161/CIR.0000000000000973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Foster D., Sanchez-Collins S., Cheskin L.J. Multidisciplinary team–based obesity treatment in patients with diabetes: current practices and the state of the science. Diabetes Spectr. 2017;30:244–249. doi: 10.2337/ds17-0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wadden T.A., Tronieri J.S., Butryn M.L. Lifestyle modification approaches for the treatment of obesity in adults. Am Psychol. 2020;75:235–251. doi: 10.1037/amp0000517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bradley L.E., Forman E.M., Kerrigan S.G., Goldstein S.P., Butryn M.L., Thomas J.G., Herbert J.D., Sarwer D.B. Project HELP: a remotely delivered behavioral intervention for weight regain after bariatric surgery. Obes Surg. 2017;27:586–598. doi: 10.1007/s11695-016-2337-3. [DOI] [PubMed] [Google Scholar]
- 13.Kraschnewski J.L., Kong L., Bryce C.L., Francis E.B., Poger J.M., Lehman E.B., Helbling S., Soleymani T., Mancoll R.E., Villalobos V., Yeh H.-C. Intensive behavioral Therapy for weight loss in patients with, or At-Risk of, type 2 Diabetes: results from the PaTH to health diabetes study. Preventive Medicine Reports. 2023;31 doi: 10.1016/j.pmedr.2022.102099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lv N., Azar K.M.J., Rosas L.G., Wulfovich S., Xiao L., Ma J. Behavioral lifestyle interventions for moderate and severe obesity: a systematic review. Prev Med. 2017;100:180–193. doi: 10.1016/j.ypmed.2017.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sockalingam S., Leung S.E., Ma C., Tomlinson G., Hawa R., Wnuk S., Jackson T., Urbach D., Okrainec A., Brown J., Sandre D., Cassin S.E. Efficacy of telephone-based cognitive behavioral therapy for weight loss, disordered eating, and psychological distress after bariatric surgery: a randomized clinical trial. JAMA Netw Open. 2023;6 doi: 10.1001/jamanetworkopen.2023.27099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tchang B.G., Morrison C., Kim J.T., Ahmed F., Chan K.M., Alonso L.C., Aronne L.J., Shukla A.P. Weight loss outcomes with telemedicine during COVID-19. Front Endocrinol. 2022;13 doi: 10.3389/fendo.2022.793290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alencar M.K., Johnson K., Mullur R., Gray V., Gutierrez E., Korosteleva O. The efficacy of a telemedicine-based weight loss program with video conference health coaching support. J Telemed Telecare. 2019;25:151–157. doi: 10.1177/1357633X17745471. [DOI] [PubMed] [Google Scholar]
- 18.Zajacova A., Lawrence E.M. The relationship between education and health: reducing disparities through a contextual approach. Annu Rev Publ Health. 2018;39:273–289. doi: 10.1146/annurev-publhealth-031816-044628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Almandoz J.P., Xie L., Schellinger J.N., Mathew M.S., Gazda C., Ofori A., Kukreja S., Messiah S.E. Impact of COVID‐19 stay‐at‐home orders on weight‐related behaviors among patients with obesity. Clinical Obesity. 2020;10 doi: 10.1111/cob.12386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kupcova I., Danisovic L., Klein M., Harsanyi S. Effects of the COVID-19 pandemic on mental health, anxiety, and depression. BMC Psychol. 2023;11:108. doi: 10.1186/s40359-023-01130-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gajarawala S.N., Pelkowski J.N. Telehealth benefits and barriers. J Nurse Pract. 2021;17:218–221. doi: 10.1016/j.nurpra.2020.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.De Simone S., Franco M., Servillo G., Vargas M. Implementations and strategies of telehealth during COVID-19 outbreak: a systematic review. BMC Health Serv Res. 2022;22:833. doi: 10.1186/s12913-022-08235-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee M.S., Nambudiri V.E. Electronic consultations and clinician burnout: an antidote to our emotional pandemic? J Am Med Inf Assoc. 2021;28:1038–1041. doi: 10.1093/jamia/ocaa300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Patt D., O'Neill C. Telemedicine and burnout—how enhancing operational support can improve digital health tools. Cancer J. 2024;30:31–33. doi: 10.1097/PPO.0000000000000698. [DOI] [PubMed] [Google Scholar]
- 25.Moulaei K., Sheikhtaheri A., Fatehi F., Shanbehzadeh M., Bahaadinbeigy K. Patients' perspectives and preferences toward telemedicine versus in-person visits: a mixed-methods study on 1226 patients. BMC Med Inf Decis Making. 2023;23:261. doi: 10.1186/s12911-023-02348-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data analyzed in this study is stored in a secure Research cannot be shared outside of those authorized as research staff per protocol. Access to this dataset requires IRB approval; if needed, direct to the corresponding author.