Abstract
Using the vesicular stomatitis virus (VSV) pseudotype system, we studied the functional properties of the Ebola virus glycoprotein (GP). Amino acid substitutions at the GP cleavage site, which reduce glycoprotein cleavability and viral infectivity in some viruses, did not appreciably change the infectivity of VSV pseudotyped with GP. Likewise, removal of two acylated cysteine residues in the transmembrane region of GP showed no discernible effects on infectivity. Although most filoviruses are believed to target endothelial cells and hepatocytes preferentially, the GP-carrying VSV showed greater affinity for epithelial cells than for either of these cell types, indicating that Ebola virus GP does not necessarily have strong tropism toward endothelial cells and hepatocytes. Finally, when it was used to screen for neutralizing antibodies against Ebola virus GP, the VSV pseudotype system allowed us to detect strain-specific neutralizing activity that was inhibited by secretory GP (SGP). This finding provides evidence of shared neutralizing epitopes on GP and SGP molecules and indicates the potential of SGP to serve as a decoy for neutralizing antibodies.
Ebola virus, a filamentous, enveloped, negative-strand RNA virus in the family Filoviridae, causes severe hemorrhagic fever in humans and nonhuman primates (16). The fourth gene from the 3′ end of its nonsegmented genome encodes two glycoproteins: the nonstructural secretory glycoprotein (SGP), which is secreted from infected cells and is the primary product of the gene (16), and the envelope glycoprotein (GP), which is responsible for cell binding and penetration of the virus. The latter is expressed by transcriptional editing, resulting in the addition of an extra adenosine within a stretch of seven adenosines in the coding region of GP (19, 25). These glycoproteins have different proclivities for cell surface molecules. While SGP is reported to bind to neutrophils via the Fcγ receptor and to inhibit early neutrophil activation (30), GP is thought to contribute to the tissue tropism of Ebola virus, since a murine retroviral vector pseudotyped with Ebola virus GP more efficiently infected endothelial cells, the major targets of filoviruses (4, 16, 18, 20), than other cell types tested (30). However, the test panel used to establish this tropism did not include primate epithelial cells such as Vero cells, which are commonly used to propagate Ebola viruses.
For many enveloped viruses, cleavage activation of membrane glycoproteins by proteolytic enzymes is a prerequisite for fusion between the viral envelope and the cellular membrane, leading to virus entry into host cells. For some viruses, including the avian influenza and Newcastle disease viruses, the increased cleavability of surface glycoproteins by furin and other ubiquitous proprotein convertases is an important determinant of virulence (12). The Ebola virus GP also undergoes posttranslational proteolytic cleavage by furin into GP1 and GP2, which are covalently linked by disulfide bonds (26). Murine leukemia virus pseudotyped with a mutant GP lacking cleavage sites for furin recognition still efficiently mediated virus entry (29), suggesting that such cleavage is not essential for the membrane fusion activity of the GP. This observation questions the need for Ebola virus GP cleavage in viral infectivity, an issue warranting further study in a different experimental system, since viral glycoprotein cleavage is essential for some viruses (12).
Acylation is another posttranslational modification of viral glycoproteins. Fatty acids, mainly palmitic acids, are bound either as oxyesters to serine or threonine or via thioester linkages to cysteine residues of viral glycoproteins (23). The role of this modification depends on the viral proteins. While acylation appears to be involved in particle formation, including virus assembly and budding in influenza and Sindbis viruses (6, 11, 33), G protein function in vesicular stomatitis virus (VSV) is not affected without this modification (27). Although the GP of Marburg virus, another member of the filovirus group, is acylated (5), the contribution of this modification to filovirus GP function is unknown.
A pseudotype system of VSV that can be used to study the function of the Ebola virus GP without biosafety level 4 containment was previously developed (21). It relies on a recombinant VSV that contains the green fluorescent protein instead of the G protein gene and thus is not infectious unless a receptor binding and fusion protein is provided in trans. The infectivity of this recombinant VSV is efficiently complemented with Ebola virus GP. Using this system, we recently identified a conserved hydrophobic region at positions 524 to 539 as a fusion peptide (10). Here, we used this system to investigate the biological significance of the GP's proteolytic cleavage and acylation, as well as its cell tropism. We also tested the value of our VSV pseudotype system to screen for neutralizing antibodies against Ebola virus.
Proteolytic processing.
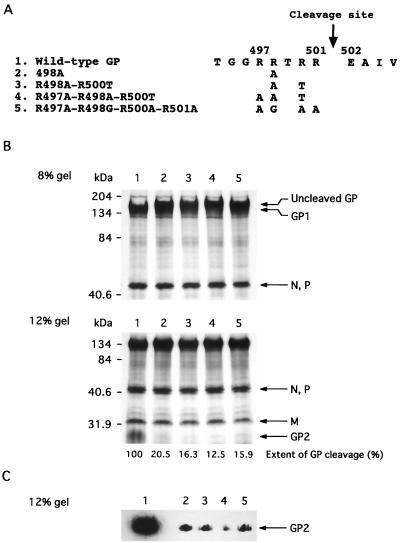
To determine the contribution of GP cleavage to the infectivity of Ebola virus, we first generated four mutant GPs with amino acid substitutions at the multibasic amino acid region (RRTRR at positions 497 to 501, an optimal motif for the proprotein convertase furin) (Fig. 1A). Both uncleaved GP and a cleaved product, GP1, were detected for all mutant GPs, while uncleaved GP was not found with wild-type GP (Fig. 1B, upper panel). A cleavage product, GP2, was detected in all mutant GP preparations (though in much lower amounts than in preparations of wild-type GP), even in that of a mutant lacking the furin recognition site (i.e., R497A-R498G-R500A-R501A) (Fig. 1B, lower panel). Immunoblotting analysis confirmed the presence of GP2 in virions with the mutant (Fig. 1C). Thus, our results support the notion that Ebola virus GP may be cleaved by proteases other than furin. We next determined the infectivity of VSVs pseudotyped with these GPs in 293 cells (Table 1). The titers of the viruses with the mutant GPs were not appreciably different from that of the virus carrying the wild-type GP, indicating a lack of correlation between cleavage efficiency and virus infectivity. These results are consistent with the observation of Wool-Lewis and Bates (29) using a retrovirus pseudotype system.
FIG. 1.
(A) Amino acid sequences of the cleavage sites of wild-type and mutant GPs. The Ebola virus GP is cleaved by furin at amino acid position 501 (22). For mutant GPs, only substituted residues are shown. (B) Cleavage of GPs incorporated into VSV virions. Wild-type and mutant GPs were cloned into a mammalian expression vector, pCAGGS/MCS (13, 14), and transfected into 293T cells, and VSVs pseudotyped with Ebola virus GP were generated as described previously (21). The viruses labeled with [35S]methionine were partially purified by centrifugation through 25% sucrose, and viral proteins were separated by sodium dodecyl sulfate-polyacrylamide (8 or 12%) gel electrophoresis (SDS-PAGE). Percentages of GP cleavage are indicated at the bottom of each lane. Lane 1, VSV complemented with wild-type GP; lanes 2, 3, 4, and 5, VSV complemented with mutant GPs R498A, R498A-R500T, R497A-R498A-R500T, and R497A-R498G-R500A-R501A, respectively. (C) Detection of GP2 in VSV virions by immunoblotting. To detect GP2, we generated wild-type and mutant GPs with a C-terminal FLAG tag. VSVs pseudotyped with these GPs were partially purified, and proteins were separated by SDS–12% PAGE under reducing conditions and subjected to immunoblotting using anti-FLAG monoclonal antibodies. Lane 1, VSV complemented with wild-type GP; lanes 2, 3, 4, and 5, VSV complemented with mutant GPs R498A, R498A-R500T, R497A-R498A-R500T, and R497A-R498G-R500A-R501A, respectively.
TABLE 1.
Infectivities of VSVs pseudotyped with GP cleavage mutants
| Virus | Infectious unitsa (log10/ml) |
|---|---|
| Wild type | 5.41 ± 0.12 |
| Mutants | |
| R498A | 5.62 ± 0.20 |
| R498A-R500T | 5.57 ± 0.07 |
| R497A-R498A-R500T | 5.58 ± 0.12 |
| R497A-R498G-R500A-R501A | 5.44 ± 0.16 |
Infectious units were determined with 293 cells. The data are mean titers ± standard deviations of three independent experiments.
Thus, in two different pseudotype systems, the extent of Ebola virus GP cleavage by furin does not correlate with the level of viral infectivity conferred by this glycoprotein, suggesting that cleavage activation may not be required for Ebola virus GP function. There are precedents for viral glycoproteins able to promote infection without furin-mediated cleavage activation: the spike protein of mouse hepatitis virus (2, 8), Sindbis virus E2 (17), and murine leukemia virus envelope glycoprotein (32). Reverse genetics would allow one to determine whether cleavage activation is indeed dispensable in GP function and whether it is involved in either cell-to-cell fusion activity or viral pathogenicity, as shown for the mouse hepatitis virus (1, 7) and Sindbis virus (17), or whether a limited extent of cleaved GP molecules in virions is sufficient to confer infectivity to virions.
Acylation.
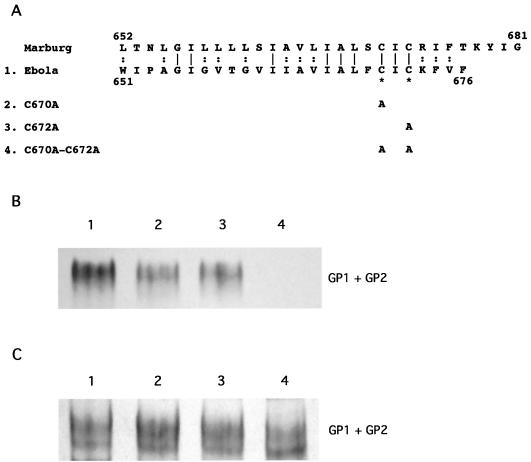
Marburg virus GP is posttranslationally acylated with palmitic acids at the Cys671 and Cys673 residues in the transmembrane anchor region of the molecule (5). Since the two cysteine residues are conserved among all filoviruses (Fig. 2A), we examined the role of these cysteine residues in Ebola GP acylation. Three mutant GPs, with a C-to-A alteration at position 670 (C670A) or position 672 (C672A) or both (C670A-C672A), were generated (Fig. 2A) and expressed in 293T cells. As shown in Fig. 2B, mutant GPs C670A and C672A labeled with [3H]palmitic acid showed reduced signals compared to wild-type GP when standardized by [3H]mannose labeling, while the C670A-C672A mutant was not labeled at all with [3H]palmitic acid. These results suggest that both of the two cysteine residues are acylated. To determine if these alterations affect GP function, we produced VSVs pseudotyped with each of these mutant GPs. There were no discernible differences in infectivities among the GP mutant VSVs compared with that of the wild-type GP virus (Table 2), suggesting that acylation is not required for Ebola virus GP functions and that the Ebola virus GP is acylated through a “default” mechanism by acyltransferases in eukaryotic cells, as was demonstrated for the VSV G protein (27).
FIG. 2.
(A) Amino acid sequences of the transmembrane domains of wild-type and mutant GPs. The cysteine residues (indicated by asterisks) at positions 670 and/or 672 were changed to alanine residues. (B and C) Labeling of GPs with either [3H]palmitic acid or [3H]mannose. Wild-type and mutant GP genes were cloned into pCAGGS/MCS and transfected into 293T cells. Twenty-four hours after transfection, cells were labeled with [3H]palmitic acid (B) or [3H]mannose (C). Cells were lysed and immunoprecipitated with antiserum to Zaire GP/SGP and then were subjected to SDS–8% PAGE under nonreducing conditions. Lane 1, wild-type GP; lane 2, C670A; lane 3, C672A; lane 4, C670A-C672A.
TABLE 2.
Infectivities of VSVs pseudotyped with GP acylation mutants
| Virus | Infectious unitsa (log10/ml) |
|---|---|
| Wild type | 5.99 ± 0.23 |
| Mutants | |
| C670A | 6.03 ± 0.27 |
| C672A | 6.05 ± 0.27 |
| C670A-C672A | 5.94 ± 0.26 |
As described in the footnote for Table 1.
Is cell tropism controlled by the GP?
Filoviruses infect endothelial cells and hepatocytes both in vivo and in vitro (4, 16, 18, 20). The destruction of these cells by virus infection is thought to explain the hemorrhagic manifestations characteristic of filovirus infections (20). A previous study suggested that the GP contributes to such cell tropism because a GP-pseudotyped retrovirus infects endothelial cells more efficiently than other cells (30); however, the cells normally used for in vitro propagation of filoviruses (e.g., kidney cells such as Vero cells) were not included in the test panel. To reassess the cell tropism of the Ebola virus GP, we tested the susceptibilities of human endothelial cells (human umbilical vein endothelial cells and human microvascular endothelial cells) and primate kidney cells (human 293 and African green monkey Vero cells) to VSV pseudotyped with the GP of the Zaire (VSVΔG*-ZaireGP) or Reston (VSVΔG*-RestonGP) strain of Ebola virus (Table 3). The endothelial cells were much less susceptible to viral infection than were human kidney epithelial cells (approximately 100- and 1,000-fold-lower infectivities than those seen with the 293 and Vero cell lines, respectively). We cannot attribute this difference to the inability of VSV to replicate in these cells, as VSV carrying the VSV G protein (VSVΔG*-VSVG) replicated nearly as well in endothelial cells as in kidney cells. A human liver cell line, HepG2, was also less susceptible than 293 cells to VSV pseudotyped with Ebola GPs. These data indicate that endothelial cells and hepatocytes are not necessarily the preferred targets of Ebola virus GP, and further, the tissue tropism of Ebola virus may not be determined by the receptor preference of the GP.
TABLE 3.
Infectivities of VSVs pseudotyped with Ebola virus GP for different cell lines
| Cells | Infectious unitsa (log10/ml)
|
||
|---|---|---|---|
| VSVΔG*-ZaireGP | VSVΔG*-RestonGP | VSVΔG*-VSVG | |
| 293 | 6.76 ± 0.03 | 6.80 ± 0.03 | 8.86 ± 0.02 |
| Vero | 7.13 ± 0.05 | 7.08 ± 0.03 | 9.35 ± 0.04 |
| Human umbilical vein endothelial cells | 4.68 ± 0.02 | 4.80 ± 0.07 | 7.77 ± 0.03 |
| Human microvascular endothelial cells | 4.37 ± 0.08 | 4.40 ± 0.08 | 7.53 ± 0.04 |
| HepG2 | 5.41 ± 0.12 | 5.31 ± 0.05 | 9.43 ± 0.02 |
| MDCK | 6.02 ± 0.14 | 6.10 ± 0.08 | 8.08 ± 0.14 |
| MDBK | 3.57 ± 0.10 | 3.70 ± 0.09 | 7.69 ± 0.02 |
Cells were infected with viruses from the same batch. The data are mean titers ± standard deviations of three independent experiments.
Recently, it was shown that expression of the GP, but not the other proteins of Ebola virus, induced cytotoxic effects in endothelial cells (31). Cell rounding and detachment were also observed in human epithelial cells expressing GP (3, 22). Thus, disruption of cell functions by GP may be involved in Ebola virus pathogenesis, although our results suggest that the tissue tropism of this virus is not solely determined by this protein.
Detection of virus-neutralizing antibodies.
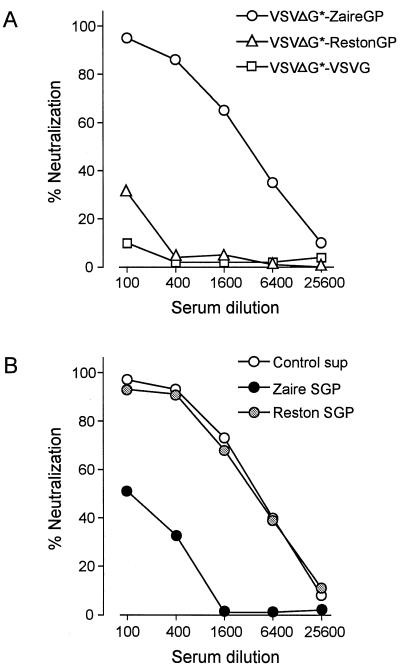
Although it is still unclear whether or not neutralizing antibodies can be produced in animals infected with Ebola virus (9, 15), it was shown that antiserum to Zaire GP and SGP reduced the infectivity of a murine retrovirus pseudotyped with the Zaire GP (28). Here, we tested whether our Ebola virus GP-pseudotyped VSV can be used to detect subtype-specific neutralizing antibodies. As shown in Fig. 3A, serum against Zaire GP/SGP neutralized the infectivity of VSV with Zaire GP but not with Reston GP, providing evidence for subtype-specific neutralizing epitopes on Ebola virus GP molecules. Moreover, the neutralizing activity was markedly reduced in the presence of Zaire SGP but not Reston SGP (Fig. 3B). Since GP and SGP appear to bind to distinct cell surface molecules (30), this neutralization-inhibition effect does not seem to reflect competition between these glycoproteins toward cell surface molecules. The results suggest that GP and SGP share neutralizing epitopes, most of which are distinct among different subtypes; they also suggest that SGP may serve as a decoy for adsorbing neutralizing antibodies.
FIG. 3.
(A) Strain-specific neutralization of VSV pseudotyped with the Ebola virus GP by antiserum to Zaire GP/SGP. The VSVs pseudotyped with Zaire GP (VSVΔG*-ZaireGP), Reston GP (VSVΔG*-RestonGP), or VSV G protein (VSVΔG*-VSVG) (104 infectious units) were incubated with serial dilutions of the antiserum for 1 h at room temperature. The infectivity was assayed by incubating the reaction mixture with 293 cells and counting the number of green fluorescent protein-positive cells. (B) Strain-specific inhibition of neutralizing activity of GP antiserum by SGP. The antiserum was incubated with 5 μg of Zaire SGP, Reston SGP, or control culture supernatant (Control sup) per ml for 1 h at room temperature and then mixed with VSVΔG*-ZaireGP. The infectivity of the virus was then assayed as described above.
The VSV pseudotype system described here has many potential research applications besides the study of the specific amino acid residues involved in GP function. It could be used, for example, to identify the cell surface molecule required for Ebola virus entry into cells. Because VSV can replicate in a wide variety of cells (i.e., cell tropism of the pseudotyped virus is likely to be controlled only by GP), our system would also be advantageous for identifying Ebola virus receptors. Finally, it might serve as a rapid screen for anti-Ebola neutralizing antibodies or drugs that inhibit GP function.
Acknowledgments
We thank Krisna Wells and Martha McGregor for excellent technical assistance and John Gilbert for editing the manuscript.
Support for this work came from NIAID Public Health Service research grants and from the Japan Health Sciences Foundation. S.W. is the recipient of the Japan Society for Promotion of Science Postdoctoral Fellowship for Research Abroad.
REFERENCES
- 1.Bos E C, Heijnen L, Luytjes W, Spaan W J. Mutational analysis of the murine coronavirus spike protein: effect on cell-to-cell fusion. Virology. 1995;214:453–463. doi: 10.1006/viro.1995.0056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bos E C, Luytjes W, Spaan W J. The function of the spike protein of mouse hepatitis virus strain A59 can be studied on virus-like particles: cleavage is not required for infectivity. J Virol. 1997;71:9427–9433. doi: 10.1128/jvi.71.12.9427-9433.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chan S Y, Ma M C, Goldsmith M A. Differential induction of cellular detachment by envelope glycoproteins of Marburg and Ebola (Zaire) viruses. J Gen Virol. 2000;81:2155–2159. doi: 10.1099/0022-1317-81-9-2155. [DOI] [PubMed] [Google Scholar]
- 4.Fisher-Hoch S P, McCormick J B. Experimental filovirus infections. Curr Top Microbiol Immunol. 1999;235:117–143. doi: 10.1007/978-3-642-59949-1_8. [DOI] [PubMed] [Google Scholar]
- 5.Funke C, Becker S, Dartsch H, Klenk H-D, Muhlberger E. Acylation of the Marburg virus glycoprotein. Virology. 1995;208:289–297. doi: 10.1006/viro.1995.1151. [DOI] [PubMed] [Google Scholar]
- 6.Gaedigk-Nitschko K, Ding M X, Levy M A, Schlesinger M J. Site-directed mutations in the Sindbis virus 6K protein reveal sites for fatty acylation and the underacylated protein affects virus release and virion structure. Virology. 1990;175:282–291. doi: 10.1016/0042-6822(90)90210-i. [DOI] [PubMed] [Google Scholar]
- 7.Gombold J L, Hingley S T, Weiss S R. Fusion-defective mutants of mouse hepatitis virus A59 contain a mutation in the spike protein cleavage signal. J Virol. 1993;67:4504–4512. doi: 10.1128/jvi.67.8.4504-4512.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hingley S T, Leparc-Goffart I, Weiss S R. The spike protein of murine coronavirus mouse hepatitis virus strain A59 is not cleaved in primary glial cells and primary hepatocytes. J Virol. 1998;72:1606–1609. doi: 10.1128/jvi.72.2.1606-1609.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ignatyev G M. Immune response to filovirus infections. Curr Top Microbiol Immunol. 1999;235:205–217. doi: 10.1007/978-3-642-59949-1_11. [DOI] [PubMed] [Google Scholar]
- 10.Ito H, Watanabe S, Sanchez A, Whitt M A, Kawaoka Y. Mutational analysis of the putative fusion domain of Ebola virus glycoprotein. J Virol. 1999;73:8907–8912. doi: 10.1128/jvi.73.10.8907-8912.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ivanova L, Schlesinger M J. Site-directed mutations in the Sindbis virus E2 glycoprotein identify palmitoylation sites and affect virus budding. J Virol. 1993;67:2546–2551. doi: 10.1128/jvi.67.5.2546-2551.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Klenk H-D, Garten W. Host cell proteases controlling virus pathogenicity. Trends Microbiol. 1994;2:39–43. doi: 10.1016/0966-842x(94)90123-6. [DOI] [PubMed] [Google Scholar]
- 13.Kobasa D, Rodgers M E, Wells K, Kawaoka Y. Neuraminidase hemadsorption activity, conserved in avian influenza A viruses, does not influence viral replication in ducks. J Virol. 1997;71:6706–6713. doi: 10.1128/jvi.71.9.6706-6713.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Niwa H, Yamamura K, Miyazaki J. Efficient selection for high-expression transfectants with a novel eukaryotic vector. Gene. 1991;108:193–199. doi: 10.1016/0378-1119(91)90434-d. [DOI] [PubMed] [Google Scholar]
- 15.Peters C J, Khan A S. Filovirus diseases. Curr Top Microbiol Immunol. 1999;235:85–95. doi: 10.1007/978-3-642-59949-1_6. [DOI] [PubMed] [Google Scholar]
- 16.Peters C J, Sanchez A, Rollin P E, Ksiazek T G, Murphy F A. Filoviridae: Marburg and Ebola viruses. In: Fields B N, Knipe D M, Howley P M, editors. Fields virology. Philadelphia, Pa: Lippincott-Raven Publishers; 1996. pp. 1161–1176. [Google Scholar]
- 17.Russell D L, Dalrymple J M, Johnston R E. Sindbis virus mutations which coordinately affect glycoprotein processing, penetration, and virulence in mice. J Virol. 1989;63:1619–1629. doi: 10.1128/jvi.63.4.1619-1629.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ryabchikova E I, Kolesnikova L V, Netesov S V. Animal pathology of filoviral infections. Curr Top Microbiol Immunol. 1999;235:145–173. doi: 10.1007/978-3-642-59949-1_9. [DOI] [PubMed] [Google Scholar]
- 19.Sanchez A, Trappier S G, Mahy B W, Peters C J, Nichol S T. The virion glycoproteins of Ebola viruses are encoded in two reading frames and are expressed through transcriptional editing. Proc Natl Acad Sci USA. 1996;93:3602–3607. doi: 10.1073/pnas.93.8.3602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schnittler H J, Feldmann H. Molecular pathogenesis of filovirus infections: role of macrophages and endothelial cells. Curr Top Microbiol Immunol. 1999;235:175–204. doi: 10.1007/978-3-642-59949-1_10. [DOI] [PubMed] [Google Scholar]
- 21.Takada A, Robison C, Goto H, Sanchez A, Murti K G, Whitt M A, Kawaoka Y. A system for functional analysis of Ebola virus glycoprotein. Proc Natl Acad Sci USA. 1997;94:14764–14769. doi: 10.1073/pnas.94.26.14764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Takada, A., S. Watanabe, H. Ito, K. Okazaki, H. Kida, and Y. Kawaoka. Downregulation of β1 integrins by Ebola virus glycoprotein: implication for virus entry. Virology, in press. [DOI] [PubMed]
- 23.Towler D A, Gordon J I, Adams S P, Glaser L. The biology and enzymology of eukaryotic protein acylation. Annu Rev Biochem. 1988;57:69–99. doi: 10.1146/annurev.bi.57.070188.000441. [DOI] [PubMed] [Google Scholar]
- 24.Volchkov V E. Processing of the Ebola virus glycoprotein. Curr Top Microbiol Immunol. 1999;235:35–47. doi: 10.1007/978-3-642-59949-1_3. [DOI] [PubMed] [Google Scholar]
- 25.Volchkov V E, Becker S, Volchkova V A, Ternovoj V A, Kotov A N, Netesov S V, Klenk H-D. GP mRNA of Ebola virus is edited by the Ebola virus polymerase and by T7 and vaccinia virus polymerases. Virology. 1995;214:421–430. doi: 10.1006/viro.1995.0052. [DOI] [PubMed] [Google Scholar]
- 26.Volchkov V E, Feldmann H, Volchkova V A, Klenk H-D. Processing of the Ebola virus glycoprotein by the proprotein convertase furin. Proc Natl Acad Sci USA. 1998;95:5762–5767. doi: 10.1073/pnas.95.10.5762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Whitt M A, Rose J K. Fatty acid acylation is not required for membrane fusion activity or glycoprotein assembly into VSV virions. Virology. 1991;185:875–878. doi: 10.1016/0042-6822(91)90563-q. [DOI] [PubMed] [Google Scholar]
- 28.Wool-Lewis R J, Bates P. Characterization of Ebola virus entry by using pseudotyped viruses: identification of receptor-deficient cell lines. J Virol. 1998;72:3155–3160. doi: 10.1128/jvi.72.4.3155-3160.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wool-Lewis R J, Bates P. Endoproteolytic processing of the Ebola virus envelope glycoprotein: cleavage is not required for function. J Virol. 1999;73:1419–1426. doi: 10.1128/jvi.73.2.1419-1426.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yang Z Y, Delgado R, Xu L, Todd R F, Nabel E G, Sanchez A, Nabel G J. Distinct cellular interactions of secreted and transmembrane Ebola virus glycoproteins. Science. 1998;279:1034–1037. doi: 10.1126/science.279.5353.1034. [DOI] [PubMed] [Google Scholar]
- 31.Yang Z Y, Duckers H J, Sullivan N J, Sanchez A, Nabel E G, Nabel G J. Identification of the Ebola virus glycoprotein as the main viral determinant of vascular cell cytotoxicity and injury. Nat Med. 2000;6:886–889. doi: 10.1038/78645. [DOI] [PubMed] [Google Scholar]
- 32.Zavorotinskaya T, Albritton L M. Failure to cleave murine leukemia virus envelope protein does not preclude its incorporation in virions and productive virus-receptor interaction. J Virol. 1999;73:5621–5629. doi: 10.1128/jvi.73.7.5621-5629.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zurcher T, Luo G, Palese P. Mutations at palmitylation sites of the influenza virus hemagglutinin affect virus formation. J Virol. 1994;68:5748–5754. doi: 10.1128/jvi.68.9.5748-5754.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]