Abstract
Background:
There has been a marked increase in the number of Schenck knee dislocation (KD) I injuries reported in the multiligament knee (MLK) injury (MLKI) and KD literature.
Purpose:
To examine the heterogeneity of the Schenck KD I classification in the MLKI and KD literature.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A systematic literature search of PubMed, CINAHL, Scopus, Web of Science, EMBASE, and Cochrane Library was conducted for all studies that investigated KDs and/or MLKIs, utilized the Schenck or an MLKI classification system, and included patients with KD I or MLK 1 injuries. Pooled analysis determined the total number of KD I or MLK 1 injuries and the specific ligamentous tear patterns. Binary meta-analyses of the studies that reported neurovascular injury within each Schenck KD class compared the pooled odds ratio (OR) of vascular and neurological injury in unicruciate (KD I) and bicruciate (KD II-IV) injuries.
Results:
Included were 50 studies in which 3460 KD I injuries were reported out of 7872 KDs and MLKIs (43.9%). Of the 2912 patients reported to have had a Schenck KD I injury, 26 patients (0.9%) had a clinically and/or radiographically confirmed tibiofemoral KD. The overall prevalence of Schenck KD I injury with documented tibiofemoral KD was 26 of 7872 (0.3%). A total of 22 studies (n = 1702 patients) reported the specific ligamentous tear patterns; the most common patterns were posterior cruciate ligament (PCL)/lateral collateral ligament (LCL) (n = 526; 30.9%), anterior cruciate ligament (ACL)/LCL (n = 488; 28.7%), ACL/medial collateral ligament (MCL) (n = 408; 24.0%), and PCL/MCL (n = 198; 11.6%). Meta-analyses demonstrated that when compared with bicruciate KD or MLKI, unicruciate KD or MLKI was significantly less likely to have concomitant vascular injury (OR, 0.28; 95% CI, 0.15-0.51; P < .0001) and concomitant neurologic injury (OR, 0.49; 95% CI, 0.37-0.65; P < .00001).
Conclusion:
The number of true, clinically and/or radiographically confirmed unicruciate KDs was extremely rare, representing <1% of all reported Schenck KD I injuries. A misappropriation of these injury patterns as true KDs may be taking place, affecting outcome studies and potentially biasing published clinical results. An MLKI classification system must document whether a confirmed KD has occurred.
Keywords: knee dislocation, multiligament knee injury, Schenck classification, KD I, MLK 1
Our understanding of knee dislocations (KDs) and multiligament knee (MLK) injuries (MLKIs) has evolved over time. The use of standardized nomenclature and classification systems provides the backbone for clinicians and researchers to communicate and analyze similar injury patterns. A KD is defined as loss of the normal tibiofemoral articulation that is confirmed clinically and/or radiographically.15,52 The Schenck classification system stratifies KDs into distinct classes based on the specific pattern of complete ligamentous injuries with the primary goal of improving communication and operative planning among providers (Table 1).15,52 Within this classification system, a KD I is defined as a single cruciate ligament remaining intact with variable collateral ligament injury in the setting of a clinically and/or radiographically confirmed disruption to the tibiofemoral joint.15,52 A true Schenck KD I with a clinically and/or radiographically documented tibiofemoral dislocation has been proven to be a particularly rare knee injury pattern, with few cases reported in the literature.4,13,16,23,24,57
Table 1.
Modified Schenck Classification System for KDs a
| Classification | Description |
|---|---|
| KD I | Disruption of 1 cruciate (ACL or PCL) |
| KD II | Disruption of both cruciates (ACL + PCL) |
| KD III | Disruption of both cruciates (ACL + PCL) and either collateral (MCL or LCL) |
| KD III-M | Disruption of both cruciates (ACL + PCL) and MCL |
| KD III-L | Disruption of both cruciates (ACL + PCL) and LCL |
| KD IV | Disruption of both cruciates (ACL + PCL) and both collaterals (MCL + LCL) |
| KD V | Fracture/dislocation |
| Modifiers b | |
| -N | Nerve injury |
| -C | Vascular injury |
| -O | Open injury |
| -EM | Extensor mechanism injury |
ACL, anterior cruciate ligament; KDs, knee dislocations; L, designates torn LCL; LCL, lateral cruciate ligament; M, designates torn MCL; MCL, medial collateral ligament; PCL, posterior cruciate ligament.
Modifiers are added to indicate KDs with the respective concomitant injury: “-N” suffix indicates nerve injury and “-C” suffix indicates vascular injury. 15 The “-O” suffix was introduced by Held et al 19 to describe open KD. The “-EM” suffix was advocated by Medvecky et al 40 and Mojica et al. 41 Example: KD III-M-C indicates KD with complete tears of ACL, PCL, MCL, and concomitant popliteal artery injury.
Although the Schenck classification was initially intended for describing KDs, the lack of a designated MLKI classification system has led to its ubiquitous application to both KD and MLKI studies. Over the past decade, there has been a surge in the reporting of Schenck KD I injuries in the orthopaedic literature, which can largely be attributed to the inclusion of unicruciate MLKIs within the same Schenck KD I designation as unicruciate KDs.11,38,46 As a result, the uncertainty revolving around the definitions for MLKIs, KDs, and Schenck KD I injuries in recent study methodologies has led to challenges in determining clinically relevant differences in patients presenting with different ligamentous tear patterns in the context of MLKIs and KDs. A recent study demonstrated an increased neurovascular risk in documented tibiofemoral KDs compared with nondislocated MLKIs, suggesting clinical differences exist between these entities. 23 To help address this dilemma, the initial Surgical Timing and Rehabilitation (STaR) Trial for MLKI network investigators 49 proposed a separate MLKI classification system to distinguish between KDs and MLKIs (known as the MLKI anatomic classification system) with distinct categories according to ligamentous tear pattern from MLK 1 to MLK 4.
The Schenck classification system provides valuable anatomic information that can be used in treatment decision-making. However, in its current state, the KD I classification fails to capture the full spectrum of injury and does not adequately designate whether there has been a documented dislocation event. These deficiencies may limit its applicability in highlighting neurovascular injury risk and accuracy in predicting operative approaches and may not allow for optimal specificity for collecting patient-reported outcome measures.23,38 Further characterization and recognition of the distinct ligamentous injury patterns comprising the Schenck KD I classification may lead to improvements in operative planning, provider to provider communication, and methodology of future KD and MLKI studies.
The primary aim of this systematic review and meta-analysis was to examine the spectrum of reporting of Schenck KD I injuries in the orthopaedic literature. The secondary aim of this study was to characterize the current state of the Schenck KD I classification by determining (1) the overall prevalence of reported Schenck KD I injuries and various subclasses and (2) the odds of concomitant neurological and vascular injury in unicruciate injuries (KD I) compared with bicruciate injuries (KD II-IV).
Methods
This review was conducted in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2020 statement. Two reviewers (J.S.G. and A.M.) conducted the review independently, and a third reviewer was used to resolve any disagreements (Z.I.L.).
Search Strategy
A systematic literature search was conducted in PubMed, CINAHL, Scopus, Web of Science, EMBASE, and Cochrane Library with no language restrictions on June 19, 2023. The search was repeated on June 20, 2023, by a different author and yielded the same results. The search query used was the following: ((knee dislocation) OR (knee dislocations) OR (tibiofemoral dislocation) OR (multi ligament knee injury) OR (multi ligament knee injuries) OR (multiligament knee injury) OR (multiligament knee injuries) OR (multiple ligament knee injury) OR (multiple ligament knee injuries) OR (multiligamentous knee injury) OR (multiligamentous knee injuries) OR (multiligament knee reconstruction)) AND ((unicruciate injury) OR (intact cruciate) OR (intact PCL) OR (intact ACL) OR (Schenck) OR (Schenck classification) OR (anatomic classification) OR (class) OR (KD) OR (KD 1) OR (KD I) OR (MLI) OR (MLKI)).
Study Inclusion and Exclusion Criteria
Studies were included if they met the following criteria: (1) access to full-text papers in English; (2) prospective and retrospective cohort studies, case-control studies, case reports, case series, or cross-sectional studies; (3) investigated KDs and/or MLKIs; (4) used the Schenck KD classification system or an MLKI classification system; (5) included patients with knee injuries classified as Schenck KD I or MLK 1; and (6) could sufficiently delineate the number of KDs and/or MLKIs in each Schenck KD or MLKI classification. For the purposes of this review, a Schenck KD I injury was defined as one of the following: (1) an MLKI with an intact cruciate ligament (anterior cruciate ligament [ACL] or posterior cruciate ligament [PCL]) plus either collateral ligament (lateral collateral ligament [LCL] and/or medial collateral ligament [MCL]) or (2) a clinically and/or radiologically confirmed tibiofemoral KD with an intact cruciate ligament and variable collateral ligament involvement (Table 1). Each reported Schenck KD I and MLK 1 injury was further categorized into a distinct subclass based on the ligamentous tear pattern and presence or absence of a clinically and/or radiographically confirmed tibiofemoral KD (Table 2).16,49 In each included study, unicruciate injuries were categorized as KD or MLKI based on the combination of definition(s) of KD and/or MLKI provided in the methodology and designation of KD or MLKI within the article title. Exclusion criteria were the following: (1) studies that did not include patients with knee injuries that were classified as Schenck KD I and (2) systematic reviews, review articles, commentaries, and animal studies. Two reviewers (J.S.G. and A.M.) independently made the study selection based on the inclusion and exclusion criteria. A third reviewer (Z.I.L.) resolved any disagreements.
Table 2.
| Suffix b | Schenck KD Subclass c | MLKI Subclass d | Ligaments Torn |
|---|---|---|---|
| -A | KD I−A | N/A d | ACL |
| -AM | KD I−AM | MLK 1−AM | ACL/MCL |
| -AL | KD I−AL | MLK 1−AL | ACL/LCL |
| -ALM | KD I−ALM | MLK 1−ALM | ACL/LCL/MCL |
| -P | KD I−P | N/A d | PCL |
| -PM | KD I−PM | MLK 1−PM | PCL/MCL |
| -PL | KD I−PL | MLK 1−PL | PCL/LCL |
| -PLM | KD I−PLM | MLK 1−PLM | PCL/LCL/MCL |
Suffix “A” or “P” designates torn cruciate ligament (ACL or PCL); suffix “M” or “L” designates torn collateral ligament (MCL or LCL). ACL, anterior cruciate ligament; AL, ACL/LCL; ALM, ACL/LCL/MCL; AM, ACL/MCL; KD, knee dislocation; LCL, lateral collateral ligament; MCL, medial collateral ligament; MLK, multiligament knee; MLKI, multiligament knee injury; PCL, posterior cruciate ligament; PL, PCL/LCL; PLM, PCL/LCL/MCL; PM, PCL/MCL.
Designates a clinically and/or radiologically confirmed tibiofemoral dislocation.
Designates multiligamentous knee injury without clinically and/or radiologically confirmed tibiofemoral dislocation.
Not applicable (N/A) as MLKI requires 2 or more complete ligament tears
Data Extraction
Data were collected independently by 2 authors (J.S.G. and A.M.), with a third author (Z.I.L.) resolving any discrepancies and disagreements. The following items were extracted from all included studies: first author name and publication year, country, study period, study design, inclusion/exclusion criteria, definition used for MLKI, definition used for KD, definition used for Schenck KD I injury, total number of included patients, and total number of patients with Schenck KD I injury. Additionally, the total number of Schenck KD I injuries with clinically and/or radiologically confirmed tibiofemoral dislocation, total number of Schenck KD I injuries with uncertain dislocation (or MLKI), and the specific ligamentous tear patterns were collected from studies that adequately reported these data or could be deduced with certainty from the data provided.
Data were extracted and aggregated from all included studies that reported on the incidence of vascular and/or neurological injuries within each Schenck KD classification. For the purposes of this review, a vascular injury was defined as occlusion, thrombosis, transection, intimal flap, or intimal tear, while an isolated arterial spasm did not constitute a vascular injury.11,39 A neurological injury was defined as any degree of impaired motor or sensory function in the tibial or peroneal nerves. 39
Risk of Bias
The quality assessment of the included studies was performed using the methodological index for nonrandomized studies checklist, which is deemed a reliable scoring system for the risk of bias in noncomparative and comparative studies. 56 The checklist uses 12 items, each of which is scored on a scale from 0 to 2. A score of 0 indicates “not reported,” a score of 1 indicates “reported but inadequate,” and a score of 2 indicates “reported and adequate.” The maximum score for a noncomparative study is 16, and the maximum score for a comparative study is 24.
Statistical Analysis
A simple pooling of data across all studies was performed to allow for interpretation of results regarding the general prevalence of Schenck KD I injuries with and without documented tibiofemoral dislocation and the specific Schenck KD I subclass. Given the rarity of Schenck KD I injuries with documented tibiofemoral dislocation and the limited description in the literature, comparative statistical analysis of the neurovascular outcomes was not possible. Separate binary meta-analyses were utilized to compare the respective pooled odds ratio (OR) of vascular and common peroneal nerve (CPN) injuries in unicruciate (KD I) and bicruciate (KD II-IV) KDs. KD V injuries were excluded from the meta-analyses since the specific ligament injuries could not be identified. Random-effects models were used to account for heterogeneity among the included studies. Heterogeneity between included studies was evaluated using the Cochran Q statistic in addition to the I2 statistic. An I2 of >50% was considered significant heterogeneity. All meta-analysis was conducted using the Statistical Package for Social Sciences (Version 26; IBM), and statistical significance was set at P ≤ .05.
Results
Search Results
The search query yielded a pooled result of 699 articles. After duplicate articles were removed, 369 articles were screened, and 299 articles were excluded based on the study title and abstract. Of the 70 remaining studies, 50 studies were eligible for inclusion in this review (Figure 1).
Figure 1.
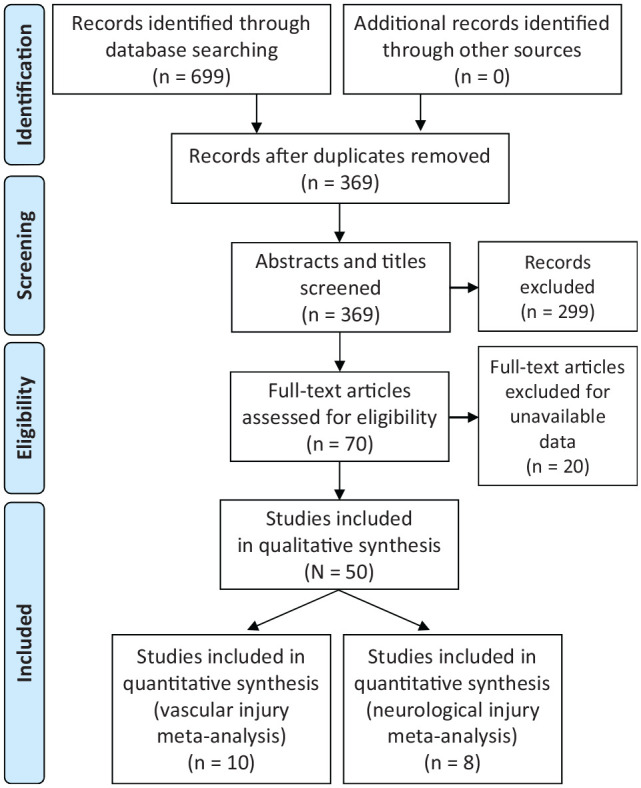
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart for literature screening.
Definitions of MLKI, KD, and Schenck KD I Classification
A summary of the definitions used for MLKI, KD, and the Schenck KD I classification in all included studies is shown in Appendix Table A1. Of the 50 included studies, 21 studies ¶ provided a definition for MLKIs only, 9 studies # provided a definition for KDs only, 4 studies7,16,23,41 provided separate definitions for MLKI and KD, and 16 studies ** did not provide a definition for either MLKI or KD. There were 23 studies †† that included a definition of the Schenck KD I classification.
Prevalence of Schenck KD I Injury
All included studies reported knee injuries that were classified as Schenck KD I, with a total of 7872 patients sustaining an MLKI and/or KD. Of these patients, 3460 (43.9%) were reported as having a Schenck KD I injury. Seven studies4,13,16,23,24,45,57 described Schenck KD I as a clinically and/or radiologically confirmed tibiofemoral dislocation on initial presentation (Table 3).
Table 3.
Studies That Utilized Schenck Classification and Included KD I Injuries With Clinically and/or Radiographically Confirmed Tibiofemoral Dislocation a
| Lead Author (Year) | KD I Injury, n | KD Definition |
|---|---|---|
| Green 16 (2023) | 12 | Complete disruption of the normal tibiofemoral articulation with radiographic evidence at the time of presentation |
| Kahan 23 (2021) | 3 | Disruption on imaging of normal alignment of tibiofemoral articulation |
| Figueroa 13 (2021) | 1 | Complete loss of the tibiofemoral congruency that is confirmed radiographically |
| Kilicoglu 24 (2021) | 6 | Complete loss of tibiofemoral joint contact as verified by radiography or multiligamentous injury with gross knee instability confirmed on MRI and clinically by orthopaedic surgeon |
| Azar 4 (2011) | 1 | Definition not provided |
| Nicandri 45 (2010) | 2 | A knee that presented dislocated and required reduction, or a grossly unstable knee with MRI-documented bicruciate, 3-, or 4-ligament injury |
| Stannard 57 (2004) | 3 | A dislocated or grossly unstable knee with tears of at least both the anterior and the posterior cruciate ligaments as documented on MRI, with surgical confirmation of the pathology |
KD, knee dislocation; MRI, magnetic resonance imaging.
Of the 3460 patients with a Schenck KD I injury, 28 patients had a documented tibiofemoral KD (0.8%). The overall prevalence among the included studies of KD I injuries with documented tibiofemoral KD was 28 of 7872 (0.3%). The trend of reporting on KD I injuries is shown in Figure 2.
Figure 2.
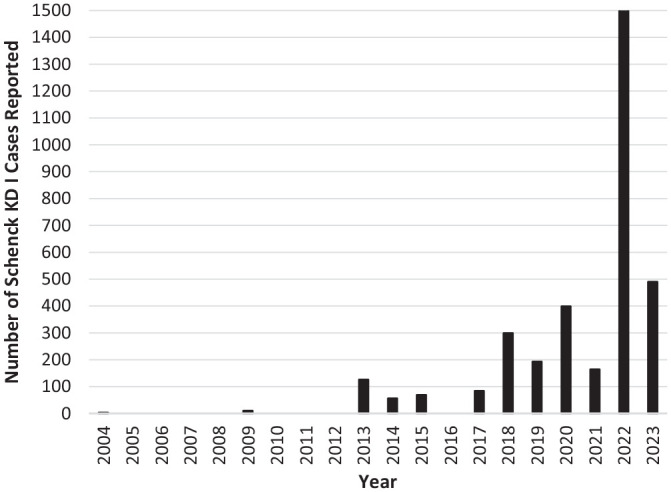
Annual reporting of Schenck knee dislocation (KD) I cases reported among studies that utilized the Schenck classification system.
Prevalence of Schenck KD I Subtypes
There were 22 studies ‡‡ (n = 1702 patients) that described the specific ligamentous tear patterns of the KD I injuries, which could therefore be further categorized into subclasses. The most common ligamentous tear patterns were PCL/LCL (n = 526; 30.7%), ACL/LCL (n = 487; 28.6%), ACL/MCL (n = 404; 23.7%), and PCL/MCL (n = 196; 11.5%). The distribution of KD I subclasses is shown in Table 4.
Table 4.
Prevalence of Schenck KD I Subclasses Among Included Studies That Utilized the Schenck Classification System and Reported Ligamentous Tear Patterns a
| Ligaments Torn | Subclass | KD I Injury, n | MLK 1 Injury, n |
|---|---|---|---|
| ACL | A | 10 | 0 |
| ACL/MCL | AM | 4 | 404 |
| ACL/LCL | AL | 1 | 487 |
| ACL/LCL/MCL | ALM | 0 | 33 |
| PCL | P | 0 | 0 |
| PCL/MCL | PM | 2 | 196 |
| PCL/LCL | PL | 3 | 523 |
| PCL/LCL/MCL | PLM | 0 | 39 |
A, designates torn ACL; ACL, anterior cruciate ligament; AL, ACL/LCL; ALM, ACL/LCL/MCL; AM, ACL/MCL; KD, knee dislocation; LCL, lateral collateral ligament; MCL, medial collateral ligament; MLK, multiligament knee; P, designates torn PCL; PCL, posterior cruciate ligament; PL, PCL/LCL; PLM, PCL/LCL/MCL; PM, PCL/MCL.
Risk of Vascular Injury
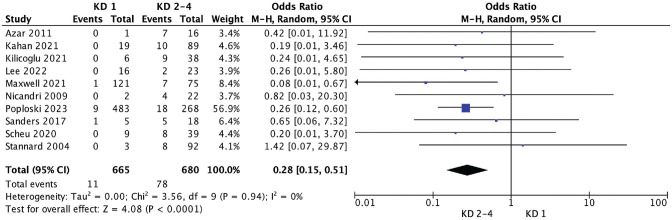
The vascular status of each Schenck KD classification was reported in 14 studies, §§ of which 10 studies ‖ ‖ reported sufficient data to calculate an OR for vascular injury between unicruciate injuries (KD I) and bicruciate injuries (KD II-IV). In these 10 studies, concomitant vascular injury was reported in 11/665 patients with unicruciate injuries classified as KD I (1.7%) and 78/680 patients with bicruciate injuries classified as KD II and IV (11.5%). Meta-analysis demonstrated that patients with unicruciate KD or MLKI were significantly less likely to have concomitant vascular injury when compared with patients with bicruciate KD or MLKI (OR, 0.28; 95% CI, 0.15-0.51; P < .0001). Heterogeneity of the pooled studies was insignificant (I2 = 0.00). The results of the meta-analysis can be visualized in the forest plot in Figure 3.
Figure 3.
Forest plot comparing the odds ratio of vascular injury between unicruciate (Schenck knee dislocation [KD] I) and bicruciate (Schenck KD II-IV) injuries. M-H, Mantel-Haenszel.
Risk of Neurologic Injury
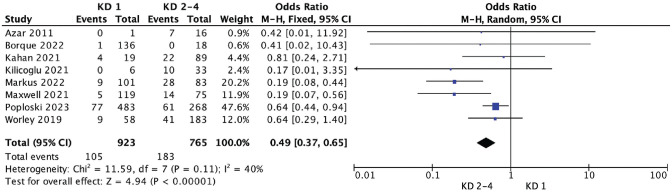
The neurologic status was reported in 14 studies, ¶¶ of which 8 studies4,10,23,24,36,38,49,64 reported sufficient data to calculate an OR for neurologic injury between unicruciate injuries (KD I) and bicruciate injuries (KD II-IV). In these 8 studies, concomitant neurologic injury was reported in 105/923 patients with unicruciate injuries (11.4%) and 183/765 patients with bicruciate injuries (23.9%). All neurologic injuries included in the meta-analysis were to the CPN. Meta-analysis demonstrated that patients with unicruciate KD or MLKI were significantly less likely to have concomitant neurologic injury when compared to patients with bicruciate KD or MLKI (OR = 0.49; 95% CI, 0.37-0.65; P < .00001). Heterogeneity of the pooled studies was insignificant (I2 = 0.40). The results of the meta-analysis can be visualized in the forest plot in Figure 4.
Figure 4.
Forest plot comparing the odds ratio of neurologic injury between unicruciate (Schenck knee dislocation [KD] I) and bicruciate (Schenck KD II-IV) injuries. M-H, Mantel-Haenszel.
Discussion
In this systematic review and meta-analysis, we examined the current reporting of Schenck KD I injuries in the orthopaedic literature to highlight the overall heterogeneity of the Schenck KD I classification and emphasize the importance of reporting the specific ligamentous tear patterns in unicruciate MLKIs and KDs. The most important finding in this study was that unicruciate injuries with documented tibiofemoral dislocation appear to be much rarer entities than unicruciate MLKIs and represent approximately 0.5% of all reported Schenck KD I injuries. Therefore, the Schenck KD I classification should be reserved for unicruciate injuries with concomitant tibiofemoral dislocation that are confirmed clinically and/or radiographically, and nondislocated MLKI should be included only in the recently described MLKI anatomic classification system. 49
Over the past decade, there has been an exponential rise in the reporting of Schenck KD I injuries that is most likely due to increased recognition of unicruciate MLKIs. In 2022, 11 studies ## reported a cumulative total of 1508 unicruciate MLKIs that were classified as Schenck KD I. Of these studies, Neilsen et al 46 reported 903 Schenck KD I injuries out of 1160 MLKIs from an online registry over a 12-year period (77.8%). This represents the largest total of Schenck KD I injuries reported in a single study and far exceeds the overall frequency of Schenck KD I injuries in the literature as determined by the current review (43.9%). The lack of an MLKI classification system has resulted in the inclusion of unicruciate MLKI into the Schenck KD I class, effectively eliminating any distinction between unicruciate KDs and MLKIs.
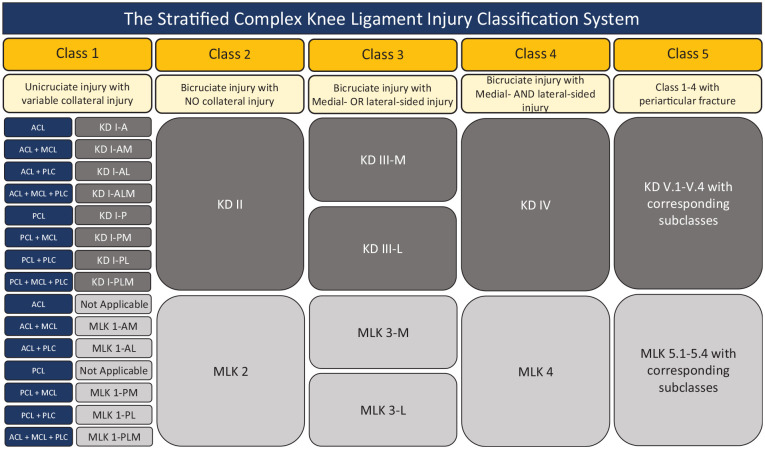
The initial STaR Trial Network investigators 49 proposed a separate MLKI anatomic classification system in which unicruciate MLKIs were broken down into subclasses based on the specific combination of ligaments torn. In alignment with this proposed MLKI classification, we endorse a similar stratification of unicruciate KDs within a modified Schenck KD I classification system and to separate the nondislocated MLKI from the true dislocation (Table 4). 16 For future studies, we recommend that unicruciate MLKIs without clinically and/or radiographically confirmed tibiofemoral dislocation should be denoted using the MLKI classification system nomenclature while those with a well-documented dislocation event should follow the proposed modification to the Schenck KD I class. As demonstrated by Kahan et al, 23 a documented KD carries a higher neurovascular risk than the nondislocated MLKI and a delineation of these differing injury patterns is warranted. Adopting a classification system that stratifies all KDs and MLKIs into classes/subclasses based on the pattern of ligament injury will provide a comprehensive and uniform algorithm for characterizing all complex knee injuries (Figure 5). Furthermore, the inclusion of suffixes for neurovascular injuries, extensor mechanism injuries, open injuries, and the subclassification of KD V injuries as described by Stannard et al 57 (eg, KD V.3L represents a knee fracture-dislocation with ACL, PCL and LCL/PLC injuries) allows for the most up-to-date and thorough description of the ligament and associated injuries that need to be included in the complex treatment decision-making process.19,40,41,57
Figure 5.
The stratified complex knee ligament injury classification system. ACL, anterior cruciate ligament; AL, ACL/LCL; ALM, ACL/LCL/MCL; AM, ACL/MCL; KD, knee dislocation; MCL, medial collateral ligament; MLK, multiligament knee; PCL, posterior cruciate ligament; PL, PCL/LCL; PLC, posterolateral corner; PLM, PCL/LCL/MCL; PM, PCL/MCL. Suffix “A” or “P” designates torn cruciate ligament (ACL or PCL). Suffix “M” or “L” designates torn collateral ligament (MCL or LCL).
KDs and MLKIs carry significant risk for concomitant vascular injury, and a high index of suspicion needs to be maintained for vascular injury in any MLKI. However, the current literature suggests that popliteal artery injuries are extraordinarily rare in the setting of a Schenck KD I injury, and the overall frequency is roughly 1%. a A systematic review conducted by Medina et al 39 determined that the overall frequency of vascular injury after KD was approximately 18%. Kim et al 25 reported a similar pooled incidence rate of vascular injury in MLKIs at 18.4%. However, in an updated meta-analysis based on the Medina et al study, Constantinescu et al 11 reported that the frequency of vascular injuries after KDs has decreased to 10.7% over the past 10 years. A significant contribution toward this apparent decline in the frequency of vascular injuries in patients reported as having KDs may partially be attributed to the increased incidence of reported Schenck KD I injuries during the past 10 years that in reality were MLKIs. 11 While the overall frequency of vascular injury in KDs has been documented extensively,11,25,39 this study aimed to directly examine the difference in the frequency of vascular injury between unicruciate injuries (Schenck KD I) and bicruciate injuries (Schenck KD II-IV).
The current meta-analysis found that unicruciate injuries (Schenck KD I) were 72% less likely to be associated with concomitant vascular injury compared with bicruciate injuries (Schenck KD II-IV). The popliteal artery is the most susceptible to injury due to the anatomic course of the artery, as it is tethered at the tendinous hiatus of the adductor magnus and tendinous arch of the soleus, while spanning the tibiofemoral joint.1,11,27,39 During a dislocation event, tibial translation can impose shearing forces or stretching of the popliteal artery and increase vascular morbidity. Involvement of both cruciates in Schenck KD II to IV injuries may lead to greater anteroposterior instability, subsequent tibial translation, and resultant impact on the popliteal artery, which could explain the increased incidence of vascular injury demonstrated in this study. In contrast, in Schenck KD I injuries, a single cruciate ligament remaining intact may protect the knee from excess tibial translation and subsequent vascular injury during tibiofemoral dislocation. It remains unclear if vascular injuries are more prominent in specific subclasses of Schenck KD I injuries, leaving an opportunity for future studies to further explore how specific patterns of cruciate and collateral involvement may influence vascular morbidity in these injuries.
The CPN is the most commonly injured nerve in KDs and MLKIs with a pooled incidence rate of 19.2% in the systematic review from Kim et al. 25 The literature suggests that KDs and MLKIs involving the posterolateral corner (PLC) are associated significantly more with concomitant CPN injury than those without PLC injury.22,49 Furthermore, findings from Markus et al 36 indicate that ACL involvement in MLKIs, especially in conjunction with PLC injury, is associated with significantly increased CPN injury. In the current study, concomitant CPN injury was 51% less likely to be associated with unicruciate injuries (Schenck KD I) compared with bicruciate injuries (Schenck KD II-IV). However, ambiguity regarding the ligamentous tear patterns of included Schenck KD I injuries limits the ability to properly elucidate the attributable risk of bicruciate involvement compared with KDs or MLKIs with an intact ACL or PCL, respectively. This problem underpins the importance of adopting separate KD and MLKI classification systems that make a clear distinction of cruciate and collateral involvement to better understand the relationship of dislocation events and anatomic, neurological, and vascular injuries.
Limitations
There were several limitations in the current review. We focused solely on studies that included unicruciate KDs and MLKIs and used the Schenck or MLKI classification system; we did not account for studies that reported injury patterns consistent with unicruciate KDs or MLKIs but did not explicitly classify them as Schenck KD I or MLK 1. Moreover, the inclusion of multiple studies from the same institution or research group may have accounted for the same patients additional times. Less than half of the included studies provided specific ligamentous tear patterns for the reported Schenck KD I injuries, which also leaves a significant quantity of unicruciate KDs and MLKIs in the literature to not be fully characterized. The data presented in this review therefore represent an approximation of the prevalence of Schenck KD I injuries reported in the literature.
In the meta-analysis for vascular and CPN injury, there were likely undetectable differences among the included studies despite the heterogeneity being determined as insignificant (<50%). Several included studies reported neurovascular injuries in patients with unicruciate KDs,4,24,45,57 while other studies reported on unicruciate MLKIs31,38,49,50,53 or included both KDs and MLKIs. 23 These inconsistencies in KD and MLKI reporting may have obscured the findings in this study, as documented dislocation has previously been found to carry an increased vascular risk, and it remains unclear how much the specific ligamentous injuries contribute. 23
This systematic review and meta-analysis highlights the marked increase in the reporting of unicruciate MLKI. Given the rarity of previously described Schenck KD I with documented dislocation and the prior lack of an MLKI classification system, this most likely represents a misappropriation of injuries into the Schenck classification, which is meant for dislocated knee injuries. This review provides valuable insight into the relative infrequency of true Schenck KD I injuries, the distribution of respective ligamentous tear patterns, or subclasses, and sufficient evidence of decreased neurovascular morbidity when a cruciate ligament remains intact in KDs and MLKIs. Widespread implementation of the MLKI classification system proposed by the initial STaR Trial Network investigators and the proposed modifications to the Schenck KD I classification may facilitate a more unified and systematic approach to differentiating these distinct injuries in future studies.
Conclusion
The number of true, clinically and/or radiographically confirmed unicruciate KDs is extremely rare, representing <1% of all reported Schenck KD I injuries. A misappropriation of these injury patterns as true KDs may be taking place, affecting outcome studies and potentially biasing published clinical results. An MLKI classification system must document whether a confirmed KD has occurred.
Appendix
Appendix Table A1.
Characteristics of the Included Studies (N = 50) a
| Study (Year) | Definitions | Study Period | Sample Size | KD I Injury, n (%) | MINORS Score b | ||
|---|---|---|---|---|---|---|---|
| MLKI | Knee Dislocation | Schenck KD | |||||
| Allen 2 (2015) | Grade 3 injury in ≥2 ligaments | NR | NR | 2007-2010 | 42 | 15 (35.7) | 17/24 |
| Atinga 3 (2022) | Acute injury involving ≥2 ligaments, or intra-articular fracture and injury of ≥1 ligament in patients with clinically suspected KD | NR | Single cruciate ligament injury | 2005-2018 | 115 | 1 (0.9) | 16/24 |
| Azar 4 (2011) | NR | NR | NR | 6-y period | 17 | 1 (5.9) | 11/16 |
| Bagherifard 5 (2019) | Tear of ≥2 of the 4 major knee ligaments (ACL, PCL, MCL, PLC [including LCL]) | NR | Injury of single cruciate ligament (ACL or PCL) | 2011-2016 | 41 | 15 (36.6) | 11/24 |
| Barrett 6 (2018) | NR | NR | NR | 2008-2015 | 32 | 16 (50.0) | 14/16 |
| Bi 7 (2022) | Involvement of ≥2 ligaments: ACL, PCL, MCL, LCL/PCL | TF dislocation at time of injury | NR | 2001-2020 | 190 | 73 (38.4) | 21/24 |
| Billieres 8 (2020) | Disruption of ≥2 of the 4 major ligaments | NR | Single cruciate ligament injury with 1 collateral ligament injury | 2013-2015 | 20 | 6 (30.0) | 13/16 |
| Born 9 (2014) | Disruption of ≥1 of the cruciate ligaments and ≥1 of the collateral ligaments through a documented or presumed KD event based on imaging, history, and pattern | NR | Single cruciate + collateral injury | 1992-2013 | 134 | 52 (38.8) | 16/24 |
| Borque 10 (2022) | ≥2 ligaments injured | NR | NR | 2001-2019 | 136 | 117 (86.0) | 13/24 |
| Djebara 12 (2022) | NR | NR | Single cruciate ligament injury | 2008-2013 | 29 | 12 (41.4) | 13/24 |
| Figueroa 13 (2021) | NR | Dislocated knee clinically or in plain radiograph with either ACL or PCL torn, with MCL or PLC complex tear | NR | NR | 1 | 1 (100.0) | 6/16 |
| Freychet 14 (2020) | NR | NR | NR | 1992-2015 | 40 | 6 (15.0) | 18/24 |
| Green 16 (2023) | Complete tear of ≥2 of the following: ACL, PCL, sMCL, LCL | Complete disruption of the normal TF articulation with radiographic evidence | Complete tearing of only a single cruciate ligament and clinical and/or radiological evidence of TF dislocation | 2001-2022 | 12 | 12 (100.0) | 8/16 |
| Hart 17 (2009) | NR | TF dislocation | Injury to 1 or both cruciate ligaments | 2002-2005 | 27 | 10 (37.0) | 17/24 |
| Hatch 18 (2018) | NR | NR | NR | 2006-2013 | 33 | 11 (33.3) | 14/24 |
| Hoit 20 (2021) | NR | NR | NR | 2011-2018 | 36 | 5 (13.9) | 22/24 |
| Hughes 21 (2022) | NR | NR | NR | 2009-2018 | 136 | 83 (61.0) | 11/24 |
| Kahan 23 (2021) | Injury to ≥2 of the following: ACL, PCL, MCL, LCL | Disruption on imaging of normal alignment of TF articulation | PCL- or ACL-intact KD with variable collateral involvement | 2001-2020 | 23 | 19 (82.6) | 16/24 |
| Kilicoglu 24 (2021) | NR | Complete loss of TF joint contact verified by radiography or multiligament injury with gross knee instability confirmed on MRI and clinically by orthopaedic surgeon | NR | 1997-2013 | 42 | 6 (14.3) | 12/24 |
| Kosy 26 (2018) | NR | NR | Single cruciate with collateral ligament injury | 2004-2016 | 188 | 27 (14.4) | 9/24 |
| Krych 28 (2014) | NR | NR | NR | 1992-2013 | 27 | 4 (14.8) | 18/24 |
| Krych 29 (2015) | NR | Ligamentous reconstruction for either a PCL-based multiligament injury or a minimum of 3 surgically treated ligaments | NR | 1993-2010 | 122 | 25 (20.5) | 11/24 |
| Labarre 30 (2023) | Disruption of ≥2 of the 4 ligaments, including >1 cruciate ligament | NR | NR | 2010-2020 | 235 | 99 (42.1) | 15/24 |
| Lee 31 (2022) | NR | NR | ACL or PCL injured | 2015-2018 | 42 | 16 (38.1) | 10/16 |
| Levy 33 (2015) | NR | Injury to multiple ligaments of the knee | NR | 1992-2013 | 125 | 29 (23.2) | 10/24 |
| Li 34 (2022) | Complete tear in ≥2 cruciate and/or collateral ligaments, with or without injuries of meniscus, nerves, arteries, or periarticular fractures | NR | 2 ligaments ruptured, 1 cruciate ligament and 1 collateral ligament, ACL/PCL + MCL/LCL/PCL | 2012-2020 | 97 | 29 (29.9) | 10/24 |
| Lian 35 (2020) | ≥2 ligaments injured | NR | NR | 2011-2018 | 108 | 57 (52.8) | 10/24 |
| Markus 36 (2022) | Injury to ≥2 of the 4 major ligaments: ACL, PCL, MCL, LCL | NR | NR | 2001-2021 | 221 | 101 (45.7) | 9/16 |
| Marwan 37 (2018) | NR | NR | MLI with involvement of just 1 of the cruciate ligaments | 2008-2016 | 49 | 5 (10.2) | 10/16 |
| Maxwell 38 (2021) | Grade 2 or 3 injury to ≥2 ligaments | NR | NR | 2011-2015 | 287 | 121 (42.2) | 8/24 |
| Mojica 41 (2023) | Injury to ≥2 of the 4 major ligaments: ACL, PCL, MCL, LCL/PLC | Recorded if TF dislocation was documented on initial radiographs or a documented reduction occurred in the emergency room | NR | 2011-2020 | 24 | 7 (29.2) | 16/24 |
| Mygind-Klavsen 43 (2017) | NR | NR | ACL or PCL injured | 2002-2010 | 196 | 57 (29.1) | 12/24 |
| Neri 44 (2019) | Complete injury to a combination of ≥2 of the 4 major ligaments (ACL, PCL, MCL, PLC) | NR | 1 cruciate ligament tear combined with a complete medial or lateral side injury | 1986-2017 | 256 | 144 (56.3) | 17/24 |
| Nicandri 45 (2010) | NR | Knee that presented dislocated and required reduction, or a grossly unstable knee with MRI documented bicruciate, 3-, or 4-ligament injury | Dislocations associated with multiligament injuries that did not include both cruciate ligaments | 2004-2005 | 35 | 2 (5.7) | 9/24 |
| Nielsen 46 (2022) | NR | NR | Tear of single cruciate ligament and either 1 or both collateral ligaments | 2005-2017 | 1160 | 903 (77.8) | 14/24 |
| Otto 47 (2020) | NR | Combined rupture of multiple ligaments leading to loss of the continuity of TF articulation | NR | 2014-2016 | 14 | 6 (42.9) | 11/24 |
| Patel 48 (2021) | ≥2 of the 4 major ligaments disrupted | NR | Involvement of ACL or PCL | 2011-2018 | 108 | 56 (51.9) | 14/24 |
| Poploski 49 (2023) | Assigned on the basis of all ligaments that had a grade 3 (complete) tear or were clinically incompetent and required surgical repair/reconstruction | NR | All injuries involving a single cruciate ligament and the medial and/or lateral side | 2011-2015 | 773 | 483 (62.5) | 8/24 |
| Sanders 50 (2017) | ≥2 ligaments injured | NR | NR | 1992-2004 | 48 | 9 (18.8) | 17/24 |
| Sanders 51 (2018) | ≥2 ligaments injured | NR | NR | 2006-2013 | 61 | 25 (41.0) | 11/24 |
| Scheu 53 (2020) | NR | NR | Injury to a single cruciate ligament. IA = ACL injured, PCL, LCL, MCL intact; IP = PCL injured, ACL, LCL, MCL intact | 2012-2017 | 50 | 9 (18.0) | 10/24 |
| Schlumberger 54 (2020) | NR | NR | Rupture of PCL and PCL/LCL or MCL | 2004-2019 | 1000 | 366 (36.6) | 9/24 |
| Shamrock 55 (2022) | Disruption of ≥2 of the 4 major ligaments | NR | NR | 2003-2018 | 207 | 125 (60.4) | 9/16 |
| Stannard 57 (2004) | NR | Dislocated or grossly unstable knee with tears of at least both ACL and PCL, documented on MRI with surgical confirmation | Dislocations associated with multiligamentous injuries that did not include both cruciate ligaments | 1996-2002 | 134 | 3 (2.2) | 13/24 |
| Tardy 58 (2017) | NR | All ligament injuries that involved ≥2 major ligaments | Injury to 1 cruciate ligament and associated collateral ligament injury | 2003-2011 | 39 | 18 (46.2) | 17/24 |
| Werner 61 (2014) | Disruption of ≥2 primary ligaments | NR | NR | 2001-2013 | 238 | 126 (52.9) | 18/16 |
| Woodmass 62 (2018) | ≥2 ligaments injured | NR | MLKI involving ACL or PCL | 2004-2013 | 23 | 7 (30.4) | 12/16 |
| Woodmass 63 (2018) | NR | NR | NR | NR | 20 | 6 (30.0) | 10/16 |
| Worley 64 (2019) | ≥2 ligaments injured | NR | NR | 12-y period | 357 | 58 (16.2) | 19/24 |
| Worley 65 (2022) | ≥2 ligaments injured | NR | NR | 12-y period | 231 | 32 (13.9) | 16/16 |
ACL, anterior cruciate ligament; IA, Schenck KD Subclass IA (knee dislocation with isolated ACL injury); IP, Schenck KD Subclass IP (knee dislocation with isolated PCL injury); KD, knee dislocation; LCL, lateral collateral ligament; MCL, medial collateral ligament; MINORS, methodological index for nonrandomized studies; MLI, multiligament injury; MLKI, multiligament knee injury; MRI, magnetic resonance imaging; NR, not reported; PCL, posterior cruciate ligament; PLC, posterolateral corner; sMCL, superficial medial collateral ligament; TF, tibiofemoral.
For noncomparative studies (maximum score = 16), a score of 0 to 5 indicates very low quality, a score of 6 to 9 indicates low quality, a score of 10 to 13 indicates fair quality, and a score of 14 to 16 indicates good quality. For comparative studies (maximum score = 24), a score of 0 to 12 indicates poor quality, a score of 13 to 18 indicates fair quality, and a score of 19 to 24 indicates excellent quality.
Footnotes
Final revision submitted December 24, 2023; accepted January 13, 2024.
One or more of the authors has declared the following potential conflict of interest or source of funding: R.C.S. has received education payments from Gemini Mountain Medical and hospitality payments from Smith+Nephew and Desert Mountain Medical. M.J.A. has received education payments from Arthrex, consulting fees from Bodycad and DePuy/Medical Device Business Services, and nonconsulting fees from Arthrex. M.J.M. consulting fees and nonconsulting fees from Smith+Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
ORCID iD: Jay Moran  https://orcid.org/0000-0001-6247-3047
https://orcid.org/0000-0001-6247-3047
References
- 1. Aktan Ikiz ZA, Ucerler H, Ozgur Z. Anatomic variations of popliteal artery that may be a reason for entrapment. Surg Radiol Anat. 2009;31(9):695-700. [DOI] [PubMed] [Google Scholar]
- 2. Allen BJ, Krych AJ, Engasser W, et al. Medial patellofemoral ligament tears in the setting of multiligament knee injuries rarely cause patellar instability. Am J Sports Med. 2015;43(6):1386-1390. [DOI] [PubMed] [Google Scholar]
- 3. Atinga A, Pearce DH, Whelan DB, Naraghi A, White LM. The accuracy of routine knee MR imaging in detection of acute neurovascular injury following multiligamentous knee injury. Skeletal Radiol. 2022;51(5):981-990. [DOI] [PubMed] [Google Scholar]
- 4. Azar FM, Brandt JC, Miller RH, 3rd, Phillips BB. Ultra-low-velocity knee dislocations. Am J Sports Med. 2011;39(10):2170-2174. [DOI] [PubMed] [Google Scholar]
- 5. Bagherifard A, Jabalameli M, Ghaffari S, et al. Short to mid-term outcomes of single-stage reconstruction of multiligament knee injury. Arch Bone Jt Surg. 2019;7(4):346-353. [PMC free article] [PubMed] [Google Scholar]
- 6. Barrett IJ, Krych AJ, Pareek A, et al. Short- to mid-term outcomes of anatomic MCL reconstruction with Achilles tendon allograft after multiligament knee injury. Knee Surg Sports Traumatol Arthrosc. 2018;26(10):2952-2959. [DOI] [PubMed] [Google Scholar]
- 7. Bi AS, Mojica ES, Markus DH, et al. Risk of postoperative stiffness following multiligamentous knee injury surgery is not affected by obesity: a multicenter study. Arthroscopy. 2022;38(12):3175-3181. [DOI] [PubMed] [Google Scholar]
- 8. Billières J, Labruyère C, Steltzlen C, et al. Multiligament knee injuries treated by one-stage reconstruction using allograft: postoperative laxity assessment using stress radiography and clinical outcomes. Orthop Traumatol Surg Res. 2020;106(5):937-944. [DOI] [PubMed] [Google Scholar]
- 9. Born TR, Engasser WM, King AH, et al. Low frequency of symptomatic venous thromboembolism after multiligamentous knee reconstruction with thromboprophylaxis. Clin Orthop Relat Res. 2014;472(9):2705-2711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Borque KA, Jones M, Balendra G, et al. High return to play rate following treatment of multiple-ligament knee injuries in 136 elite athletes. Knee Surg Sports Traumatol Arthrosc. 2022;30(10):3393-3401. [DOI] [PubMed] [Google Scholar]
- 11. Constantinescu D, Luxenburg D, Syros A, et al. Vascular injury after knee dislocation: a meta-analysis update. J Am Acad Orthop Surg. 2023;31(4):e198-e206. [DOI] [PubMed] [Google Scholar]
- 12. Djebara A, Pujol N. Long-term functional outcomes of multiligament knee reconstructions with lateral injuries. Orthop Traumatol Surg Res. 2022;108(3):103240. [DOI] [PubMed] [Google Scholar]
- 13. Figueroa F, Sandoval A, Figueroa D. Schenck’s knee dislocation (KD) I injury: An uncommon pattern. J Clin Orthop Trauma. 2021;16:230-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Freychet B, Kennedy NI, Sanders TL, et al. No difference between single and staged posterolateral corner surgical procedures in the multiligament injured/dislocated knee. Knee Surg Sports Traumatol Arthrosc. 2020;28(7):2170-2176. [DOI] [PubMed] [Google Scholar]
- 15. Goebel CP, Domes C. Classifications in brief: the Schenck classification of knee dislocations. Clin Orthop Relat Res. 2020;478(6):1368-1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Green JS, Yalcin S, Moran J, et al. Examining the Schenck KD I classification in patients with documented tibiofemoral knee dislocations: a multicenter retrospective case series. Orthop J Sports Med. 2023;11(6):23259671231168892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hart JM, Blanchard BF, Hart JA, Montgomery SC, Schoderbek R, Miller MD. Multiple ligament knee reconstruction clinical follow-up and gait analysis. Knee Surg Sports Traumatol Arthrosc. 2009;17(3):277-285. [DOI] [PubMed] [Google Scholar]
- 18. Hatch GFR, 3rd, Villacis D, Damodar D, Dacey M, Yi A. Quality of life and functional outcomes after multiligament knee reconstruction. J Knee Surg. 2018;31(10):970-978. [DOI] [PubMed] [Google Scholar]
- 19. Held M, Scheepers W, von Bormann R, et al. Inclusion of open injuries in an updated Schenck classification of knee dislocations based on a global Delphi consensus study. J ISAKOS. 2022;7(5):95-99. [DOI] [PubMed] [Google Scholar]
- 20. Hoit G, Rubacha M, Chahal J, Khan R, Ravi B, Whelan DB. Is there a disadvantage to early physical therapy after multiligament surgery for knee dislocation? A pilot randomized clinical trial. Clin Orthop Relat Res. 2021;479(8):1725-1736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hughes JD, Lynch AD, Smith CN, Musahl V, Irrgang JJ. External fixation increases complications following surgical treatment of multiple ligament knee injuries. Knee Surg Sports Traumatol Arthrosc. 2022;30(1):161-166. [DOI] [PubMed] [Google Scholar]
- 22. Kahan JB, Li D, Schneble CA, et al. The pathoanatomy of posterolateral corner ligamentous disruption in multiligament knee injuries is predictive of peroneal nerve injury. Am J Sports Med. 2020;48(14):3541-3548. [DOI] [PubMed] [Google Scholar]
- 23. Kahan JB, Schneble CA, Li D, et al. Increased neurovascular morbidity is seen in documented knee dislocation versus multiligamentous knee injury. J Bone Joint Surg Am. 2021;103(10):921-930. [DOI] [PubMed] [Google Scholar]
- 24. Kilicoglu OI, Pehlivanoglu T, Demirel M, Chodza M, Balcı HI, Asık M. The impact of the ligamentous injury pattern and associated neurovascular injury on ultimate knee function in patients with traumatic knee dislocations. J Knee Surg. 2021;34(14):1495-1502. [DOI] [PubMed] [Google Scholar]
- 25. Kim SH, Park Y, Kim B, Lee DH, Pujol N. Incidence of associated lesions of multiligament knee injuries: a systematic review and meta-analysis. Orthop J Sports Med. 2021;9(6):23259671211010409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kosy JD, Matteliano L, Rastogi A, Pearce D, Whelan DB. Meniscal root tears occur frequently in multi-ligament knee injury and can be predicted by associated MRI injury patterns. Knee Surg Sports Traumatol Arthrosc. 2018;26(12):3731-3737. [DOI] [PubMed] [Google Scholar]
- 27. Kropman RHJ, Kiela G, Moll FL, de Vries JP. Variations in anatomy of the popliteal artery and its side branches. Vasc Endovascular Surg. 2011;45(6):536-540. [DOI] [PubMed] [Google Scholar]
- 28. Krych AJ, Giuseffi SA, Kuzma SA, Stuart MJ, Levy BA. Is peroneal nerve injury associated with worse function after knee dislocation? Clin Orthop Relat Res. 2014;472(9):2630-2636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Krych AJ, Sousa PL, King AH, Engasser WM, Stuart MJ, Levy BA. Meniscal tears and articular cartilage damage in the dislocated knee. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):3019-3025. [DOI] [PubMed] [Google Scholar]
- 30. Labarre C, Kim SH, Pujol N. Incidence and type of meniscal tears in multilligament [sic] injured knees. Knee Surg Sports Traumatol Arthrosc. 2023;31(2):465-474. [DOI] [PubMed] [Google Scholar]
- 31. Lee JH, Cook JL, Wilson N, Rucinski K, Stannard JP. Outcomes after multiligament knee injury reconstruction using novel graft constructs and techniques. J Knee Surg. 2022;35(5):502-510. [DOI] [PubMed] [Google Scholar]
- 32. Lee JJ, Choi YJ, Shin KY, Choi CH. Medial meniscal tears in anterior cruciate ligament-deficient knees: effects of posterior tibial slope on medial meniscal tear. Knee Surg Relat Res. 2011;23(4):227-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Levy NM, Krych AJ, Hevesi M, et al. Does age predict outcome after multiligament knee reconstruction for the dislocated knee? 2- to 22-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):3003-3007. [DOI] [PubMed] [Google Scholar]
- 34. Li X, Hou Q, Zhan X, Chang L, Ma X, Yuan H. The accuracy of MRI in diagnosing and classifying acute traumatic multiple ligament knee injuries. BMC Musculoskelet Disord. 2022;23(1):43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lian J, Patel NK, Nickoli M, et al. Obesity is associated with significant morbidity after multiligament knee surgery. J Knee Surg. 2020;33(6):525-530. [DOI] [PubMed] [Google Scholar]
- 36. Markus DH, Mojica ES, Bi A, et al. Relationship between peroneal nerve and anterior cruciate ligament involvement in multiligamentous knee injury: a multicenter study. J Am Acad Orthop Surg. 2022;30(22):e1461-e1466. [DOI] [PubMed] [Google Scholar]
- 37. Marwan Y, Kulkarni S, Addar A, et al. Anterolateral ligament injury in knee dislocations. Arthroscopy. 2018;34(6):1891-1897. [DOI] [PubMed] [Google Scholar]
- 38. Maxwell GT, Warth RJ, Amin A, et al. Multiple ligament knee injuries: does the knee dislocation classification predict the type of surgical management? J Knee Surg. 2021;34(3):273-279. [DOI] [PubMed] [Google Scholar]
- 39. Medina O, Arom GA, Yeranosian MG, Petrigliano FA, McAllister DR. Vascular and nerve injury after knee dislocation: a systematic review. Clin Orthop Relat Res. 2014;472(9):2621-2629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Medvecky MJ, Kahan JB, Richter DL, et al. Extensor mechanism disruption impacts treatment of dislocated and multiligament injured knees: treatment and Schenck classification recommendations based on a global Delphi method. J Bone Joint Surg Am. 2023;105(13):1012-1019. [DOI] [PubMed] [Google Scholar]
- 41. Mojica ES, Bi AS, Vasavada K, et al. Poorer functional outcomes in patients with multi-ligamentous knee injury with concomitant patellar tendon ruptures at 5 years follow-up. Knee Surg Sports Traumatol Arthrosc. 2023;31(1):325-331. [DOI] [PubMed] [Google Scholar]
- 42. Moran J, Schneble CA, Katz LD, et al. Examining the bone bruise patterns in multiligament knee injuries with peroneal nerve injury. Am J Sports Med. 2022;50(6):1618-1626. [DOI] [PubMed] [Google Scholar]
- 43. Mygind-Klavsen B, Nielsen TG, Lind MC. Outcomes after posterior cruciate ligament (PCL) reconstruction in patients with isolated and combined PCL tears. Orthop J Sports Med. 2017;5(4):2325967117700077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Neri T, Myat D, Beach A, Parker DA. Multiligament knee injury: injury patterns, outcomes, and gait analysis. Clin Sports Med. 2019;38(2):235-246. [DOI] [PubMed] [Google Scholar]
- 45. Nicandri GT, Dunbar RP, Wahl CJ. Are evidence-based protocols which identify vascular injury associated with knee dislocation underutilized? Knee Surg Sports Traumatol Arthrosc. 2010;18(8):1005-1012. [DOI] [PubMed] [Google Scholar]
- 46. Nielsen TG, Sørensen OG, Lind M. A comparison of multi-ligament reconstruction and isolated anterior cruciate ligament reconstruction at one year follow-up: results from the Danish Knee Ligament Reconstruction Registry. J Exp Orthop. 2022;9(1):30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Otto A, Helal A, Imhoff FB, et al. Promising clinical and magnetic resonance imaging results after internal bracing of acute posterior cruciate ligament lesions in multiple injured knees. Knee Surg Sports Traumatol Arthrosc. 2020;28(8):2543-2550. [DOI] [PubMed] [Google Scholar]
- 48. Patel NK, Lian J, Nickoli M, et al. Risk factors associated with complications after operative treatment of multiligament knee injury. Orthop J Sports Med. 2021;9(3):2325967121994203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Poploski KM, Lynch AD, Burns TC, et al. Presentation and surgical management of multiple ligament knee injuries: a multicenter study from the Surgical Timing and Rehabilitation (STaR) Trial for MLKIs network. J Bone Joint Surg Am. 2023;105(8):607-613. [DOI] [PubMed] [Google Scholar]
- 50. Sanders TL, Johnson NR, Levy NM, et al. Effect of vascular injury on functional outcome in knees with multi-ligament injury: a matched-cohort analysis. J Bone Joint Surg Am. 2017;99(18):1565-1571. [DOI] [PubMed] [Google Scholar]
- 51. Sanders TL, Johnson NR, Pareek A, et al. Satisfactory knee function after single-stage posterolateral corner reconstruction in the multi-ligament injured/dislocated knee using the anatomic single-graft technique. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1258-1265. [DOI] [PubMed] [Google Scholar]
- 52. Schenck RC. The dislocated knee. Instr Course Lect. 1994;43:127-136. [PubMed] [Google Scholar]
- 53. Scheu M, Espinoza GF, Mellado CA, Díaz PA, Garín AF, O’Connell LA. Varus mechanism is associated with high incidence of popliteal artery lesions in multiligament knee injuries. Int Orthop. 2020;44(6):1195-1200. [DOI] [PubMed] [Google Scholar]
- 54. Schlumberger M, Schuster P, Eichinger M, et al. Posterior cruciate ligament lesions are mainly present as combined lesions even in sports injuries. Knee Surg Sports Traumatol Arthrosc. 2020;28(7):2091-2098. [DOI] [PubMed] [Google Scholar]
- 55. Shamrock AG, Hall JR, Hajewski CJ, An Q, Duchman KR. Cartilage and meniscus injuries are more common in patients undergoing delayed multiligament reconstruction. J Knee Surg. 2022;35(5):560-565. [DOI] [PubMed] [Google Scholar]
- 56. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712-716. [DOI] [PubMed] [Google Scholar]
- 57. Stannard JP, Sheils TM, Lopez-Ben RR, McGwin Jr G, Robinson JT, Volgas DA. Vascular injuries in knee dislocations: the role of physical examination in determining the need for arteriography. J Bone Jt Surg Ser A. 2004;86(5):910-915. [PubMed] [Google Scholar]
- 58. Tardy N, Boisrenoult P, Teissier P, Steltzlen C, Beaufils P, Pujol N. Clinical outcomes after multiligament injured knees: medial versus lateral reconstructions. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):524-531. [DOI] [PubMed] [Google Scholar]
- 59. Wascher DC, Schenck RC, Treme GP, Richter DL. The knee dislocation classification system is simple, reproducible, and allows communication among surgeons. J Knee Surg. 2022;35(9):1044-1045. [DOI] [PubMed] [Google Scholar]
- 60. Werner BC, Gwathmey FW Jr, Higgins ST, Hart JM, Miller MD. Ultra-low velocity knee dislocations: patient characteristics, complications, and outcomes. Am J Sports Med. 2014;42(2):358-363. [DOI] [PubMed] [Google Scholar]
- 61. Werner BC, Hadeed MM, Gwathmey FW, Jr, Gaskin CM, Hart JM, Miller MD. Medial injury in knee dislocations: what are the common injury patterns and surgical outcomes? Clin Orthop Relat Res. 2014;472(9):2658-2666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Woodmass JM, O’Malley MP, Krych AJ, et al. Revision multiligament knee reconstruction: clinical outcomes and proposed treatment algorithm. Arthroscopy. 2018;34(3):736-744.e3. [DOI] [PubMed] [Google Scholar]
- 63. Woodmass JM, Sanders TL, Johnson NR, et al. Posterolateral corner reconstruction using the anatomical two-tailed graft technique: clinical outcomes in the multiligament injured knee. J Knee Surg. 2018;31(10):1031-1036. [DOI] [PubMed] [Google Scholar]
- 64. Worley JR, Brimmo O, Nuelle CW, Cook JL, Stannard JP. Incidence of concurrent peroneal nerve injury in multiligament knee injuries and outcomes after knee reconstruction. J Knee Surg. 2019;32(6):560-564. [DOI] [PubMed] [Google Scholar]
- 65. Worley JR, Brimmo O, Nuelle CW, et al. Revision anterior cruciate ligament reconstruction after surgical management of multiligament knee injury. J Knee Surg. 2022;35(1):72-77. [DOI] [PubMed] [Google Scholar]