Abstract
Purpose
Compared with open surgery, arthroscopic anterior talofibular ligament (ATFL) repair has many advantages and good clinical outcome. Inferior extensor retinaculum (IER) reinforcement is a supplement procedure that increase the strength of the ATFL. There is still no gold standard for arthroscopic ATFL repair. The purposes of this study were to describe a simplified technique for arthroscopic ATFL repair with IER reinforcement and to analyze its preliminary clinical results.
Methods
Twenty-seven patients with chronic lateral ankle instability (CLAI) who underwent this simplified surgery were analyzed in this retrospective study. The patients’ characteristics and operative times were evaluated. Intraoperative photos, radiographs from the anterior drawer test and talar tilt test and postoperative MR images were recorded. The American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hindfoot score and visual analog scale (VAS) score were also recorded. With the assistance of a needle, we performed ATFL repair and IER reinforcement with one Pushlock anchor and nonabsorbable sutures.
Results
No complications namely skin necrosis, superficial fibular nerve injury or wound infection, were reported. The AOFAS score and VAS score improved from 64.74 ± 9.47 and 6.00 ± 1.56 to 90.74 ± 6.46 and 1.07 ± 1.09, respectively. The talar advancement and talar tilt angle were improved after surgery. One year after the operation, the ATFL appeared to be continuous on MR images.
Conclusion
In this study, we proposed a simple and effective arthroscopic ATFL repair with IER reinforcement technique. The short-term follow-up examination revealed satisfactory clinical outcomes. Our technique might be a new surgical option for the treatment of CLAI.
Keywords: Anterior talofibular ligament, Arthroscopy, Chronic lateral ankle instability, Clinical outcome
Introduction
The ankle joint is a complex hinged synovial joint. Owing to its ability to bear heavy loads and important role during walking, the ankle joint must be stabilized while still permitting full mobility. The ankle is also the most vulnerable joint [1–3]. The medial collateral ligaments (MCLs), lateral collateral ligaments (LCLs) and distal tibiofibular syndesmosis stabilize the ankle joint. The LCLs is a strong complex that stabilizes the lateral side of the ankle joint. It is composed of three distinct bands: the anterior talofibular ligament (ATFL), posterior talofibular ligament and calcaneofibular ligament. Among those ligaments, the ATFL is the weakest ligament with the lowest failure load among these ligament structures [4, 5]. Even after optimal conservative treatment, 10% to 30% of patients do not respond well and eventually develop chronic lateral ankle instability (CLAI) [6]. If CLAI persists, it can cause further problems such as asymmetric arthritis. Therefore, surgical treatment is suggested for CLAI patients for whom conservative treatment fails [7].
In 1966, Dr. Broström first proposed an open surgical method to repair the lateral ligament complex. Dr. Gould performed Inferior extensor retinaculum (IER) reinforcement as a supplement to the procedure proposed by Broström to increase the strength of the ATFL. This is called the Broström–Gould procedure. Broström's procedure is still the gold standard in the treatment of CLAI [8–15]. In the 1990s, arthroscopic repair of the ATFL was first proposed. However, it is not widely performed because it is more complex and time-consuming than conventional open surgery. Owing to its greater complexity, it is associated with a higher incidence of complications [16].
Despite the above limitations, arthroscopy provides a more comprehensive observation of the ankle joint and is advantageous for the diagnosis and treatment of the co-morbidity of ankle with ligament injury [17]. With the development of arthroscopic surgery, the arthroscopic Broström–Gould procedure has gradually replaced the traditional open Broström–Gould surgery [18–20].
Although a variety of arthroscopic techniques have been proposed for the repair of the ATFL of the ankle, there is still no gold standard for arthroscopic ATFL repair. In this study, we propose a simplified ankle arthroscopic ATFL repair technique that is repeatable, easy to learn and effective according to midterm follow-up data.
The purpose of this study was to introduce the details of this surgical technique. The patients’ mid-term clinical outcomes were described in this study.
Method
This study was conducted in accordance with the ethical standards (Declaration of Helsinki) and approved by the Medical Ethics Committee of our hospital. The inclusion criteria were as follows: [1] patients for whom 6 months of conservative treatment failed; [2] patients with CLAI who underwent this simplified arthroscopic ATFL repair technique between January 2021 and July 2022; and [3] patients who were followed up for at least 1 year. The exclusion criteria were as follows: [1] patients who were followed up at irregular intervals and [2] patients with concomitant severe intra-articular lesions such as infection, osteochondral lesions of the talus and rheumatic arthritis. In total, 27 patients were included in this study. Patient information was retrospectively collected by reviewing medical records.
Indication for simplified arthroscopic ATFL repair
The indications for this technique was: [1] CLAI after failure of 6 months of nonoperative [2]. Radiographs from the anterior drawer test or talar tilt test were positive [3]. MRI revealed tears in the ATFL.
Surgical technique
Patients were operated on the supine position with a pneumatic tourniquet on the thigh. Two portals and a 4.5 mm arthroscope were used in this surgery. The standard anteromedial portal was made just medial to the tibialis anterior tendon at the ankle joint line and served as the main visualization portal. The accessory anterolateral portal was made approximately 10 mm anterior to the fibula and 15 mm proximal to the tip of the lateral malleolus and served as a working portal. All patients were operated on by the same experienced surgeon.
Step 1. Tighten the ATFL with nonabsorbable sutures and a PushLock anchor
The hyperplastic synovial and hypertrophic scar tissue were removed to ensure a good surgical field. Once the ATFL was identified, the ligament quality was assessed to ensure that the ligament was suitable for repair [21]. Most repairable ATFLs appear distension or avulsion with normal thickness under arthroscopy. The PDS suture was folded back through the 18G needle to form a suture loop. The tip of the needle was then bent for 30 degrees (Fig. 1A). An 18G needle was used to suture the ATFL, and a PDS suture loop was introduced into the ankle joint through the ATFL tissue (Fig. 1B), and then pulled out of the joint (Fig. 1C). A nonabsorbable suture (WilSuture, REJOIN Medical, China) was then folded back and guided through the ATFL tissue (Fig. 1D). The end of the nonabsorbable suture was threaded through the loop to form a lasso (Fig. 1E). The lasso was tightened to lift the ATFL, and the lasso was fixed to the upper edge of the ATFL insertion point with PushLock anchors (PEEK PushLock, REJOIN Medical, China) (Fig. 1F, G).
Fig. 1.
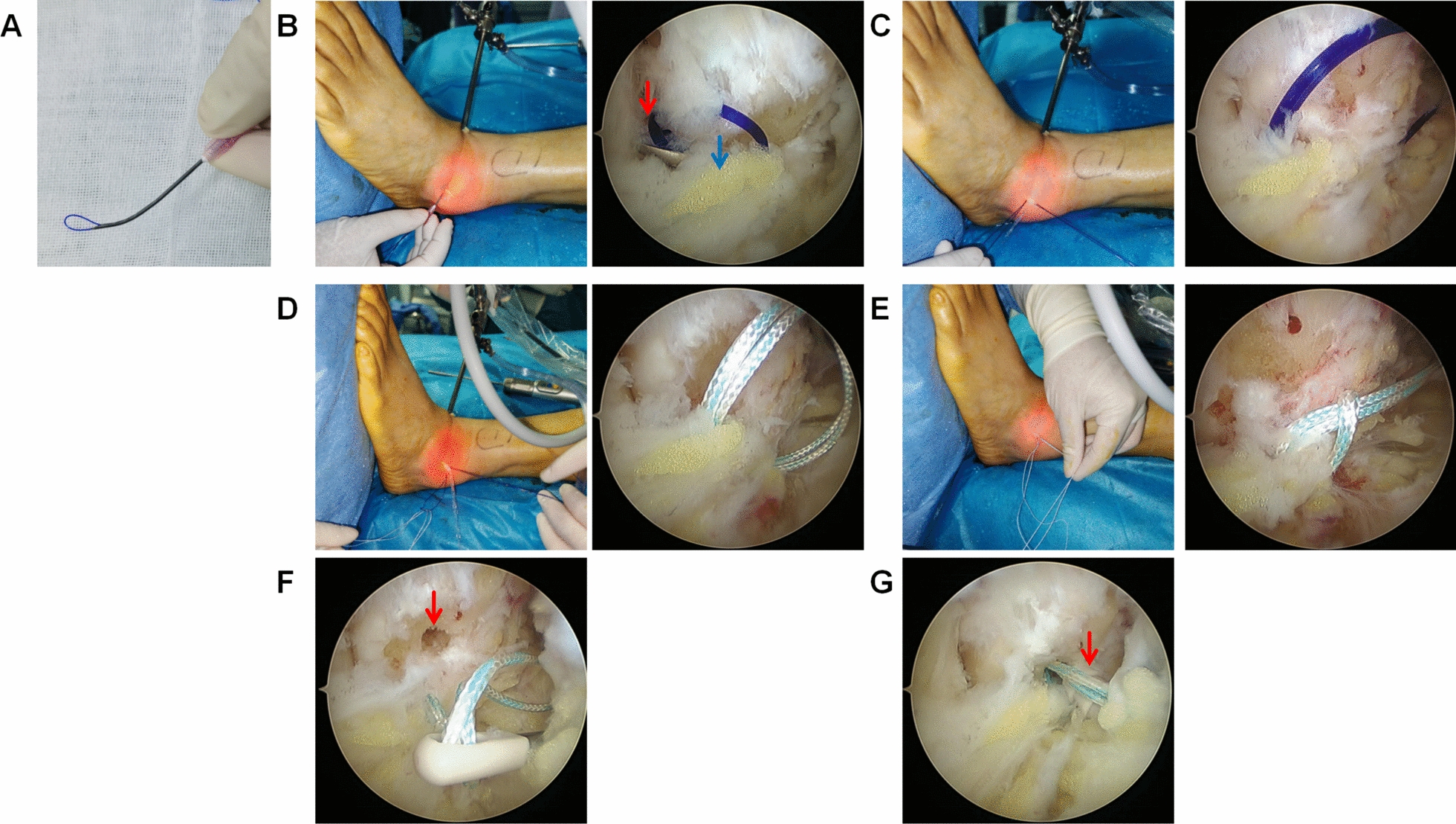
Tightening the ATFL with nonabsorbable Sutures and PushLock anchor. A PDS suture folded back through the needle to form a suture loop. The tip of needle was bent for 30 degrees. B The needle were punctured through the ATFL to introduce the PDS suture. The red arrow indicate the tip of needle. The blue arrow indicate the teared ATFL. C The needle was removed, and a PDS suture loop was formed. D A nonabsorbable suture was folded back and guided through ATFL tissue by the PDS suture. E The absorbable sutures were formed into a lasso loop. F The bone tunnel for PushLock was prepared. The arrow indicate the bone tunnel. G The ATFL was tightened by affixing the end of the lasso to the fibula with a PushLock anchors. The arrow indicate the PushLock anchors
Step 2 Reinforcement of the ATFL with the IER and joint capsule
The safe zone was the area between the peroneal brevis tendon and the dorsal cutaneous nerve of the superficial peroneal nerve. Operating within a safe zone can avoid iatrogenic superficial peroneal nerve and sural nerve injuries [17](Fig. 2A). Within the safe zone, a straight 18G needle (Fig. 2B) travels through the skin, subcutaneous tissue, IER, and joint capsule into the joint cavity (Fig. 2C). A PDS suture was introduced into the ankle joint through this needle and then used to guide one end of the nonabsorbable suture through the joint capsule, IER and skin (Fig. 2D). One centimeter from the previous entry point, the other end of the suture was guided out of the skin using the same method (Fig. 2E). An incision was made between the two ends of the suture. With the ankle placed in the neutral position, two ends of the suture were knotted subcutaneously to ensure that the ATFL was augmented by both the IER and the joint capsule (Fig. 2F). At the end of the procedure, the effectiveness of the sutures was confirmed arthroscopically, and ankle stability was checked via the anterior drawer test and talus tilt test.
Fig. 2.
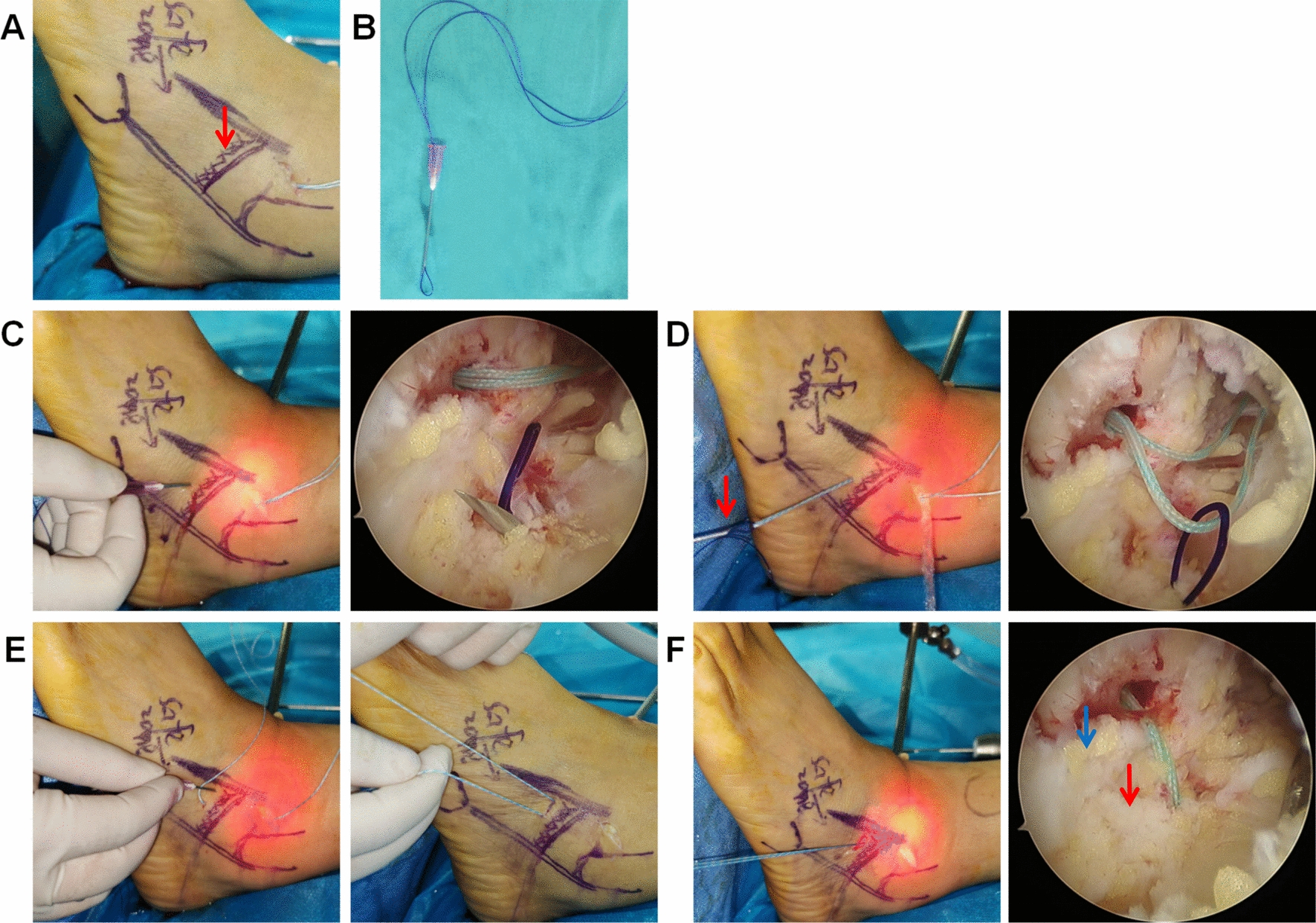
Reinforcement of the ATFL with the IER and joint capsule. A Safe zone: between the peroneal brevis tendon and the dorsal cutaneous nerve of the superficial peroneal nerve. The arrow indicate the surface projection of IER. B The PDS suture was folded back through the needle to form a suture loop. C The PDS suture was guided into the joint via an 18G needle within the safe zone. D One end of the nonabsorbable suture was guided through the joint capsule, IER and skin. The arrow indicate the needle. E The other end of the nonabsorbable suture was guided through the joint capsule, IER and skin. F The suture was knotted subcutaneously, and the joint capsule and IER were tightened to reinforce the ATFL. The blue arrow indicate the ATFL. The red arrow indicate the IER
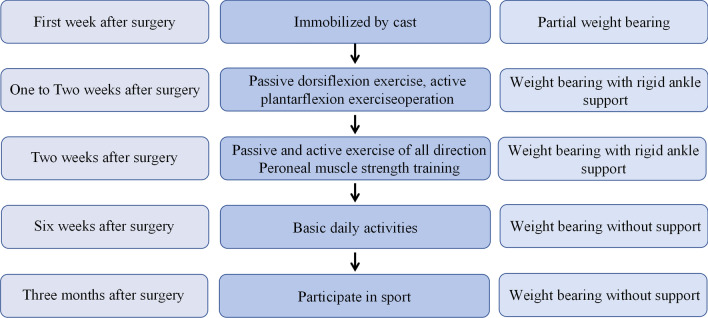
Postoperative protocol
The ankle was immobilized with a cast for 1 week to reduce the hemorrhage risk and swelling. After the cast was removed, rigid ankle support was needed for 5 weeks, and the patients were asked to wear it continuously during the night and intermittently during the day. Once cast was removed, patients were asked to perform passive dorsiflexion exercise and active plantar flexion exercises. Two weeks after surgery, the patients started passive and active exercise in all directions and peroneal muscle strength training. However, when performing plantar flexion exercises, the patients were asked to do so according to their ability. Six weeks after surgery, the patients were allowed to perform basic daily activities without additional support. Three months after surgery, the patients were allowed to increasingly participate in sports (Fig. 3).
Fig. 3.
Postoperative rehabilitation protocol
The patients were asked to follow up at 2 weeks and 1, 3, 6, 12, 18 and 24 months after surgery. The American Orthopaedic Foot and Ankle Society (AOFAS) ankle‒hindfoot score and visual analog scale (VAS) score were assessed before surgery and at the follow-up visit. MRI of the ankle was performed at 12 months after surgery. The MRI was used to evaluate the quality of ATFL.
Statistical analysis
All the continuous variables are presented as means ± standard deviations (means ± SDs). The normality of the data was tested using the Shapiro–Wilk test. Paired Student’s two tailed t test was used to determine differences in numerical data between two groups. Statistical significance was defined as a P value < 0.05. Statistical analysis was performed using SPSS Version 21.0 (IBM).
Results
We summarized the characteristics of the included patients in Table 1. The mean age of the patients was 33.96 ± 11.44 years (range, 19–53 years). Among the 27 patients, 11 (40.74%) were male, 16 (59.26%) were female, 14 left ankles were affected (51.85%) and 13 right ankles were affected (48.15%). The mean surgery time was 34.11 ± 8.18 min (range, 25–57 min) (Table 1).
Table 1.
Patient characteristics
| Characteristic | Value |
|---|---|
| Mean age in yrs | 33.96 ± 11.44 |
| Sex | |
| M | 11 |
| F | 16 |
| Mean follow-up period in months | 15.15 ± 3.43 |
| Ankle side treated | |
| Left | 14 |
| Right | 13 |
| Mean operative time in mins | 34.11 ± 8.18 |
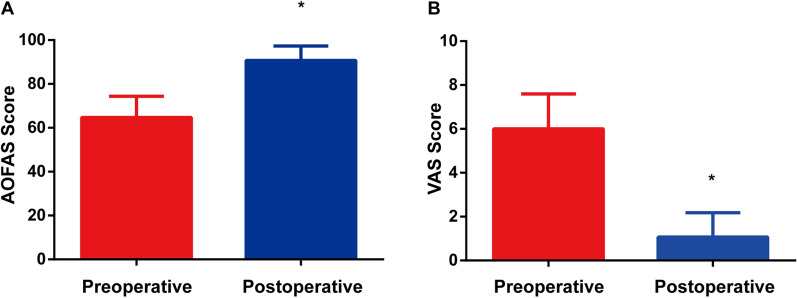
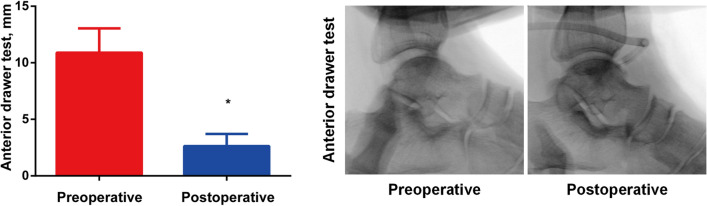
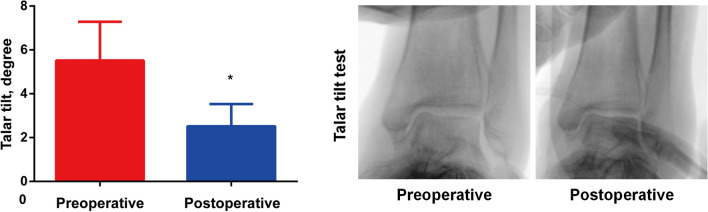
The mean follow-up time for patients was 15.15 ± 3.43 months (range, 12–24 months). None of the 27 patients experienced skin necrosis, superficial fibular nerve injury or wound infection. In all patients, the AOFAS score and VAS score improved. The AOFAS score improved from 64.74 ± 9.47 (range, 49–81) to 90.74 ± 6.46 (range, 74–100) (p < 0.05), and the mean VAS score improved from 6.00 ± 1.56 (range, 4–9) before surgery to 1.07 ± 1.09 (range, 0–4) (p < 0.05) at the last follow-up (Fig. 4). We also performed the anterior drawer test and talar tilt test before and after the surgery. The anterior drawer test improved from 10.89 ± 2.11 mm (range, 8–16) before surgery to 2.63 ± 1.06 mm (range, 1–5) (p < 0.05) after surgery (Fig. 5). The talar tilt improved from 5.52 ± 1.73 degrees (range, 3–8) before surgery to 2.52 ± 1.00 degrees (range, 1–5) (p < 0.05) postoperatively (Fig. 6).
Fig. 4.
Pain and function outcomes. A AOFAS score. B VAS score
Fig. 5.
Results of the anterior drawer test
Fig. 6.
Results of the talar tilt test
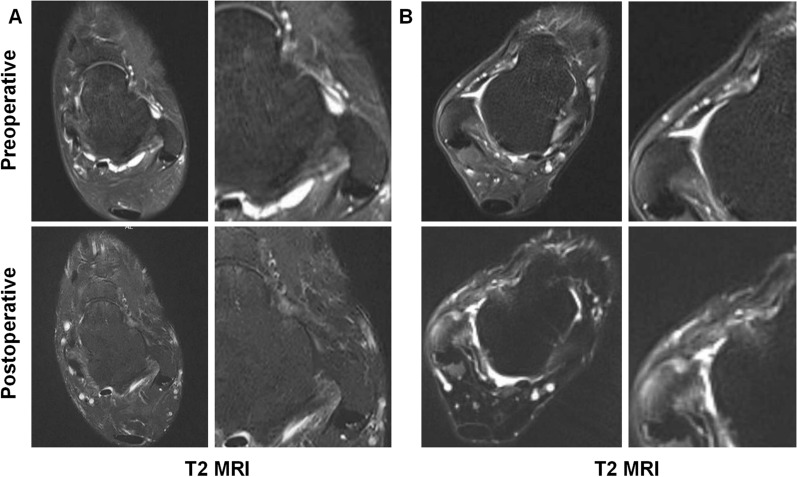
One year after the operation, all patients underwent MRI evaluation. Continuous and tense ATFLs were observed in 23 out of 27 patients (Fig. 7A). The remaining 4 patients presented hyperintense signals on T2-weighted imaging. However, they all reported significant improvement in symptoms. The shape of their ligament is basically continuous, with good tension (Fig. 7B).
Fig. 7.
Imaging of typical cases. A Continuous and tense ATFLs were observed in 23 out of 27 patients. B Four patients had hyperintense signal at T2-weighted imaging but the shape of their ligament is basically continuous, with good tension
Discussion
Ankle sprains are common sports injuries, and the lateral ligament complex is the most common injury site [5, 18, 22]. The ATFL is located in the lateral ligament complex and is the most common site of injury [5, 23]. Conservative treatment is preferred for ankle sprains, but 30% of cases still progress CLAI even after optimal conservative treatment. If CLAI develops, it can cause further problems, such as asymmetric arthritis. Therefore, surgical intervention is needed for CLAI patients whose conservative treatment fails.
There are several operative options for the treatment of CLAI, such as anatomic repair or anatomic reconstruction of the ATFL and tenodesis [23, 24]procedures. The Brostrom technique and its modification are considered the gold standard [18, 25, 26]. With the development of technology, arthroscopic treatment of CLAI has gradually become a trend because it is less invasive and can be used to treat other intra-articular lesions simultaneously [4, 18, 23, 27, 28]. Several studies have shown that the clinical results of arthroscopic surgery are similar to those of open surgery [29–31]. Hence, arthroscopic ATFL repair of the ankle is gradually replacing the open surgery as the preferred method.
Suture anchors and lasso-loops are often used to repair the ATFL [32–34]. These suturing methods require knotting under arthroscopy. This is quite difficult for inexperienced surgeons and often extends the operation time. There is also a possibility of loose knots and knot irritation. In this study, we tightened the ATFL with nonabsorbable sutures and a PushLock anchor. Instead of tightening the ATFL with a knot, we fix the end of the lasso to the fibula using a pushlock. This is a knot–free procedure that is easy for junior surgeons to learn and shortens the total operation time. In addition, there is no possibility of loose knots or knot irritation. We also used a 30–degree bent 18G needle to suture the ATFL. This is a convenient way to lower the requirements for tools. Compared with traditional tools, needles are less likely to injure the ligament during suturing.
There are several surgeries designed to reinforce the ATFL. Arthroscopic Brostrom Repair With Suture Augmentation (ABR-S) and Arthroscopic Brostrom Repair With Suture Tape Augmentation (ABR-ST) [26, 35] are based on similar principles: the suture structure from the fibula tip to the talus tunnel is used to reinforce ATFL. These surgeries require multiple screws, which increases the complexity of surgery and the financial burden on patients. At the same time, the sutures do not have the elasticity and self-repair ability of soft body tissue. This may lead to stiffness of the ankle joint and postoperative suture failure. Thus, most surgeons opt for AFTL repair and IER reinforcement. A subcutaneous working space is often required for the reinforcement of the IER [33, 36]. In this study, we used a syringe needle to assist in the reinforcement of the IER together with the joint capsule within the safe zone. With this technique, there is no surgical trauma during the creation of subcutaneous working space.
During follow-up period, no cases of skin necrosis, superficial fibular nerve injury or wound infection were detected. In all patients, the AOFAS score and VAS score improved. At 12 months after the operation, the ATFL was continuous in all patients according to MRI. Although 4 patients presented hyperintense signals on T2-weighted imaging, they all reported significant improvement in symptoms and the shape of their ATFLs was basically continuous with good tension.
In this study, all 27 patients reported satisfactory clinical outcomes during follow-up visit. Hence, our new technique might be a new surgical option for the treatment of CLAI. However, its effectiveness should be further evaluated with a prospective randomized controlled study to comparing this technique with other techniques.
Conclusions
In summary, this novel surgical procedure is effective with the following simplifications: [1] It is a 2-portal, nondistraction arthroscopic technique that requires no special surgical tool other than conventional arthroscopic tools [2]. The ATFL was sutured using a 30-degree bent needle. There is a minimal risk of injuring the ligament during suturing [3]. Knotting is not required when reattachment of the ATFL; thus the possibility of loose knots or knot irritation [4]. The ATFL can be repaired, and the IER can be reinforced with one PushLock and nonabsorbable sutures. The mid-term follow-up revealed satisfactory clinical outcomes. We believe that this simplified procedure arthroscopic ATFL repair technique should be promoted.
Acknowledgements
We would like to thank our patients and colleagues for their support..
Abbreviations
- ABR-S
Arthroscopic Brostrom repair with suture augmentation
- ABR-ST
Arthroscopic Brostrom repair with suture tape augmentation
- AOFAS
American Orthopaedic Foot and Ankle Society
- ATFL
Anterior talofibular ligament
- CLAI
Chronic lateral ankle instability
- IER
Inferior extensor retinaculum
- LCLs
Lateral collateral ligaments
- MCLs
Medial collateral ligaments
- VAS
Visual analog scale
Author contributions
XC performed the surgery. XY, XL and YM collected and interpreted the patient’s clinical data. XY drafted the manuscript. YD and SC contributed to the revision. All authors read and approved the final manuscript.
Funding
This research was supported by the Medical Technology Innovation Project of The Second Affiliated Hospital of Chongqing Medical University and the Natural Science Foundation of Chongqing (CSTB2023NSCQ-BHX0006).
Availability of data and materials
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
This was an observational study. The Medical Ethics Committee at the Second Affiliated Hospital of Chongqing Medical University waived the requirement for ethical approval. All involved patients were allowed to report their data and have voluntarily signed the consent forms.
Consent for publication
All involved patients provided informed consent for the publication of their data.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Azevedo SSA, Sassi LB, Martins TB, Menezes FS, Migliorini F, Maffulli N, et al. Epidemiology of injuries in young volleyball athletes: a systematic review. J Orthop Surg Res. 2023;18(1):748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferran NA, Maffulli N. Epidemiology of sprains of the lateral ankle ligament complex. Foot Ankle Clin. 2006;11(3):659–62. [DOI] [PubMed] [Google Scholar]
- 3.Bridgman SA, Clement D, Downing A, Walley G, Phair I, Maffulli N. Population based epidemiology of ankle sprains attending accident and emergency units in the West Midlands of England, and a survey of UK practice for severe ankle sprains. Emerg Med J. 2003;20(6):508–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al-Mohrej OA, Al-Kenani NS. Chronic ankle instability: Current perspectives. Avicenna J Med. 2016;6(04):103–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hur ES, Bohl DD, Lee S. Lateral ligament instability: review of pathology and diagnosis. Curr Rev Musculoskeletal Med. 2020;13:494–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Glazebrook M, Eid M, Alhadhoud M, Stone J, Matsui K, Takao M. Percutaneous ankle reconstruction of lateral ligaments. Foot Ankle Clin. 2018;23(4):581–92. [DOI] [PubMed] [Google Scholar]
- 7.Ferran NA, Oliva F, Maffulli N. Ankle instability. Sports Med Arthrosc Rev. 2009;17(2):139–45. [DOI] [PubMed] [Google Scholar]
- 8.Pellegrini MJ, Sevillano J, Ortiz C, Giza E, Carcuro G. Knotless modified arthroscopic-Broström technique for ankle instability. Foot Ankle Int. 2019;40(4):475–83. [DOI] [PubMed] [Google Scholar]
- 9.Behrens SB, Drakos M, Lee BJ, Paller D, Hoffman E, Koruprolu S, Digiovanni CW. Biomechanical analysis of Brostrom versus Brostrom-Gould lateral ankle instability repairs. Foot Ankle Int. 2013;34(4):587–92. [DOI] [PubMed] [Google Scholar]
- 10.Cao S, Wang C, Wang X, Ma X. Percutaneous inferior extensor retinaculum augmentation technique for chronic ankle instability. Orthop Surg. 2022;14(5):977–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dalmau-Pastor M, Yasui Y, Calder JD, Karlsson J, Kerkhoffs GM, Kennedy JG. Anatomy of the inferior extensor retinaculum and its role in lateral ankle ligament reconstruction: a pictorial essay. Knee Surg Sports Traumatol Arthrosc. 2016;24:957–62. [DOI] [PubMed] [Google Scholar]
- 12.Dalmau-Pastor M, Malagelada F, Kerkhoffs GM, Manzanares MC, Vega J. X-shaped inferior extensor retinaculum and its doubtful use in the Bröstrom-Gould procedure. Knee Surg Sports Traumatol Arthroscopy. 2018;26:2171–6. [DOI] [PubMed] [Google Scholar]
- 13.Jeong BO, Kim MS, Song WJ, SooHoo NF. Feasibility and outcome of inferior extensor retinaculum reinforcement in modified Broström procedures. Foot Ankle Int. 2014;35(11):1137–42. [DOI] [PubMed] [Google Scholar]
- 14.Lee SH, Cho HG, Yang JH. Additional inferior extensor retinaculum augmentation after all-inside arthroscopic anterior talofibular ligament repair for chronic ankle instability is not necessary. Am J Sports Med. 2021;49(7):1721–31. [DOI] [PubMed] [Google Scholar]
- 15.Park S, Kim T, Lee M, Park Y. Absence of ATFL remnant does not affect the clinical outcomes of the modified broström operation for chronic ankle instability. Knee Surg Sports Traumatol Arthrosc. 2020;28:213–20. [DOI] [PubMed] [Google Scholar]
- 16.Zeng G, Hu X, Liu W, Qiu X, Yang T, Li C, Song W. Open Broström-Gould repair vs arthroscopic anatomical repair of the anterior talofibular ligament for chronic lateral ankle instability. Foot Ankle Int. 2020;41(1):44–9. [DOI] [PubMed] [Google Scholar]
- 17.Flores SF, Santos NR. Arthroscopic treatment of lateral ankle instability. Is there a safe zone? An anatomic study. Foot Ankle Surg. 2020;26(1):61–5. [DOI] [PubMed] [Google Scholar]
- 18.Araoye I, De Cesar NC, Cone B, Hudson P, Sahranavard B, Shah A. Results of lateral ankle ligament repair surgery in one hundred and nineteen patients: do surgical method and arthroscopy timing matter? Int Orthop. 2017;41(11):2289–95. [DOI] [PubMed] [Google Scholar]
- 19.Feng SM, Maffulli N, Ma C, Oliva F. All-inside arthroscopic modified Brostrom-Gould procedure for chronic lateral ankle instability with and without anterior talofibular ligament remnant repair produced similar functional results. Knee Surg Sport TRA. 2021;29(8):2453–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nery C, Raduan F, Del BA, Asaumi ID, Cohen M, Maffulli N. Arthroscopic-assisted Brostrom-Gould for chronic ankle instability: a long-term follow-up. Am J Sport Med. 2011;39(11):2381–8. [DOI] [PubMed] [Google Scholar]
- 21.Thes A, Odagiri H, Elkaim M, Lopes R, Andrieu M, Cordier G, et al. Arthroscopic classification of chronic anterior talo-fibular ligament lesions in chronic ankle instability. Orthop Traumatol-sur. 2018;104(8S):S207–11. [DOI] [PubMed] [Google Scholar]
- 22.Kobayashi T, Tanaka M, Shida M. Intrinsic risk factors of lateral ankle sprain: a systematic review and meta-analysis. Sports Health. 2016;8(2):190–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aicale R, Maffulli N. Chronic lateral ankle instability: topical review. Foot Ankle Int. 2020;41(12):1571–81. [DOI] [PubMed] [Google Scholar]
- 24.Allegra F, Boustany SE, Cerza F, Spiezia F, Maffulli N. Arthroscopic anterior talofibular ligament reconstructin in chronic ankle instability: two years results. Injury. 2020;51(Suppl 3):S56-62. [DOI] [PubMed] [Google Scholar]
- 25.Wittig U, Hohenberger G, Ornig M, Schuh R, Leithner A, Holweg P. All-arthroscopic reconstruction of the anterior talofibular ligament is comparable to open reconstruction: a systematic review. Efort Open Rev. 2022;7(1):3–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lan R, Piatt ET, Bolia IK, Haratian A, Hasan L, Peterson AB, et al. Suture tape augmentation in lateral ankle ligament surgery: current concepts review. Foot Ankle Orthop. 2021;6(4):1758323290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Corte-Real N, Caetano J. Ankle and syndesmosis instability: consensus and controversies. Efort Open Rev. 2021;6(6):420–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moorthy V, Sayampanathan AA, Yeo N, Tay KS. Clinical outcomes of open versus arthroscopic Brostrom procedure for lateral ankle instability: a meta-analysis. J Foot Ankle Surg. 2021;60(3):577–84. [DOI] [PubMed] [Google Scholar]
- 29.Zhou YF, Zhang ZZ, Zhang HZ, Li WP, Shen HY, Song B. All-inside arthroscopic modified brostrom technique to repair anterior talofibular ligament provides a similar outcome compared with open brostrom-gould procedure. Arthroscopy. 2021;37(1):268–79. [DOI] [PubMed] [Google Scholar]
- 30.Brown AJ, Shimozono Y, Hurley ET, Kennedy JG. Arthroscopic versus open repair of lateral ankle ligament for chronic lateral ankle instability: a meta-analysis. Knee Surg Sport TRA. 2020;28(5):1611–8. [DOI] [PubMed] [Google Scholar]
- 31.Yeo ED, Lee KT, Sung IH, Lee SG, Lee YK. Comparison of all-inside arthroscopic and open techniques for the modified brostrom procedure for ankle instability. Foot Ankle Int. 2016;37(10):1037–45. [DOI] [PubMed] [Google Scholar]
- 32.Takao M, Matsui K, Stone JW, Glazebrook MA, Kennedy JG, Guillo S, et al. Arthroscopic anterior talofibular ligament repair for lateral instability of the ankle. Knee Surg Sport TRA. 2016;24(4):1003–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Guillo S, Odagiri H. All-inside endoscopic Brostrom-gould technique. Arthrosc Tec. 2020;9(1):e79-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang Y, Han J, Wu H, Zhi X, Lian J, Xu F, et al. Arthro-Brostrom with endoscopic retinaculum augmentation using all-inside lasso-loop stitch techniques. BMC Musculoskel Dis. 2022;23(1):795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vega J, Montesinos E, Malagelada F, Baduell A, Guelfi M, Dalmau-Pastor M. Arthroscopic all-inside anterior talo-fibular ligament repair with suture augmentation gives excellent results in case of poor ligament tissue remnant quality. Knee Surg Sport TRA. 2020;28(1):100–7. [DOI] [PubMed] [Google Scholar]
- 36.Cordier G, Lebecque J, Vega J, Dalmau-Pastor M. Arthroscopic ankle lateral ligament repair with biological augmentation gives excellent results in case of chronic ankle instability. Knee Surg Sport TRA. 2020;28(1):108–15. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.