Abstract
Background
Accrediting medical specialties programs are expected to influence and standardize training program quality, align curriculum with population needs, and improve learning environments. Despite global agreement on its necessity, methods vary widely. In the Chilean context, a recent new accreditation criteria includes research productivity in relation to educational research on resident programs, so we aimed to define it. What is the profile of publications in educational research produced by Chilean medical specialty residency programs in the last five years? Based on these results, we intend to analyze the potential impact of the new accreditation policy on medical specialty programs in Chile.
Methods
We performed a preliminary bibliometric search to identify the use of the term “resident” in literature. After that, we conducted a literature search, using a six-step approach to scoping reviews, including the appraisal of the methodological quality of the articles.
Results
Between 2019 and 2023, an average of 6.2 articles were published yearly (19%). The bibliometric analysis revealed that the dominant thematic area of the journals was clinical, accounting for 78.1%. Most articles focused on residents (84.38%), with only two articles including graduates as participants. One university was responsible for 62.50% of the articles and participated in all multicenter studies (9.38%). Surgical specialties produced 15 research articles focused on procedural training using simulation. Psychiatry was the second most productive specialty, with 5 articles (15.63%) covering standardized patients, well-being, and mental health assessment. The most frequent research focus within residency programs over the five-year period was teaching and learning methodologies, with 19 articles representing almost 60% of the total analyzed.
Conclusions
Research on medical education in Chile’s postgraduate residency programs is limited, with most studies concentrated in a few universities. The new accreditation criteria emphasize educational research, posing challenges for many institutions to meet higher standards. Understanding unexplored areas in educational research and learning from successful programs can enhance research productivity and align efforts with accreditation expectations. Continuous evaluation and new research on residents’ satisfaction, skills acquisition, and well-being are needed to ensure training quality and accountability.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12909-024-05986-y.
Keywords: Medical Education Accreditation, Quality Assurance, Accreditation policies, Educational standards
Background
The accreditation of medical educational programs is considered essential for supporting program improvement, ensuring the quality of education, and promoting diversity, equity, and population health [1]. Theoretically, this process can enhance healthcare outcomes by influencing and standardizing training program quality, aligning curriculum with population needs, and improving learning environments [2].
Although an agreement emphasizes the need for an accreditation system [3], a consensus on a single method has not yet been achieved. Accreditation based on standards is a fundamental principle common to most accreditation systems, though the format and specifications of these standards vary [4]. Regarding the areas covered by the standards, the Accreditation Council for Graduate Medical Education (ACGME) includes educational research as accreditation criteria [5].
In Chile, the “Comisión Nacional de Acreditación” (CNA-Chile) manages the accreditation process for institutions and programs, organizing criteria in dimensions, highlighting the importance of curricula relevance, quality assurance, and continuous improvement in medical training programs to meet the healthcare demands of the population. The accreditation of institutions and programs in Chile is framed by Law 21,091 on Higher Education. The new criteria, published in September 2021, came into full force on October 1, 2023 [6]. According to the fourth criterion in the first dimension of Institutional Accreditation, an institution meets the excellence standard if generates and promotes studies on teaching and learning on one own´s experience and developments in the discipline and profession; and considers the results to improve the training process [7]. The document “Quality Criteria and Standards for the Accreditation of Medical and Dental Specialties” considers nine criteria, which are operationalized in five dimensions. Each criterion has three levels of achievement and considers general research productivity [8]. The area experts committees have established guidelines for the expected productivity of the academic body (faculty/core) that considers the research published in WOS, Scopus, and Scielo to fulfill the accreditation criteria [9].
According to the Ministry of Education of Chile, in 2024, 365 medical specialties offered by 21 universities [10] are subject to this regulation.
Within the framework of a new policy, it is important to analyze whether the programs are prepared to respond to changes through an analysis that allows us to understand the initial level of compliance and comprehend and give meaning to the evaluation criteria. This way, the criteria are not perceived as strategically imposed tools but as effective mechanisms for continuous improvement [11].
Given that accreditation processes guide change and decision-making, and that postgraduate programs are required to conduct formative research as part of the institutions, we consider it relevant to analyze the productivity in educational research in Chilean residency programs from 2019 to 2024. The research question for this review is: What is the profile of publications on Chilean medical specialty residency programs over the last five years, in relation to the CNA accreditation criteria and the MMERSQI framework for educational research quality? Based on these results, we intend to analyze how recent research outputs align with evolving accreditation standards for medical specialty programs in Chile.
Methodology
The research team comprised eight researchers, each with specific expertise and roles. Two researchers held Ph.D. in Education, and four had master’s degrees in Medical Education. Additionally, two researchers had experience managing postgraduate clinical programs, and three were responsible for faculty development programs in Medical Education or Simulation. Five team members had received training in international simulation programs; two were current residents. All team members had content expertise, and five had experience conducting scoping reviews. A librarian assisted the team in developing the definitive search strategy.
We conducted the literature search in two parts. The first part was a preliminary bibliometric search to identify the use of the term “resident” in the literature, considering its general usage and potential for varied interpretations. This step was essential to define the research question and appropriately review the data found. The second part employed a six-step approach to scoping reviews [12], which included appraising the methodological quality of the articles using the modified Medical Education Research Study Quality Instrument (MMERSQI) [13] and the CNA-Chile criteria for medical specialty programs [9]. At least two independent researchers conducted each step of the analysis. The report was prepared following the PRISMA-S checklist for scoping reviews [14].
Results
Preliminary bibliometric search
To identify the term “resident” in the literature, we conducted a bibliometric search using Elsevier’s Scopus database. The search was limited to authors affiliated with institutions in Chile. The Scopus database offers extensive coverage for citation analysis, encompassing a broader range of journals and scientific publications compared to other databases (15–16). Additionally, Scopus provides advanced export functionality for structured data.
Using the “advanced search” functionality, we queried all publications containing the words “resident,” “residents,” “residency,” or “residencies’’ in their titles, abstracts, or keywords. The search was further refined to include “medical residency programs” and the word “medicine” in any field, with Chile as the affiliation country. The search period spanned from January 2019 to March 25, 2024. We exported the keywords defined by the authors and editors and the abstracts using Scopus’s export functionalities.
To construct and visualize a co-occurrence network of relevant terms related to residents, we used VOSviewer software (version 1.6.20). We created a term co-occurrence map based on text data extracted from the abstract fields in Scopus, employing the full counting method (i.e., all occurrences of a term in a document are counted). Given the relatively low number of articles, we set a minimum occurrence threshold of 10 to ensure a significant and manageable number of relevant terms (∼ 300). Limiting the number of terms helped create a more readable map of co-occurring terms. A relevance score was computed for each term, and the top 60% most relevant terms (default parameter) were used for mapping. The mapping was automatically performed using the VOS clustering technique and visualized with the “network visualization” functionality [17].
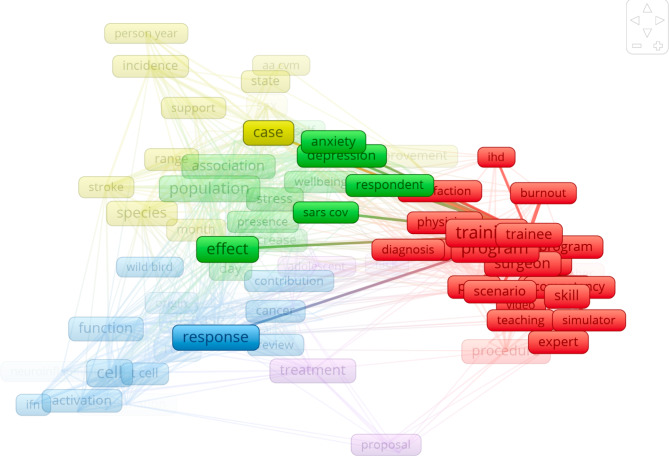
We identified five clusters associated with the term “resident.” The primary co-occurrence network was related to residency programs and resident training. The most frequently identified terms in this network included “training,” “program,” “surgeon,” “simulator,” “scenario,” and “trainee.” The secondary co-occurrence network was related to mental health, well-being, and Covid (Fig. 1). This preliminary approach will guide our subsequent methodological report [18].
Fig. 1.
Co-occurrence analysis using VosViewer
Identifying the research question
This scoping review aimed to examine and analyze research papers focused on Chilean medical specialty residency programs, with a particular emphasis on their alignment with the newly introduced CNA accreditation criterion regarding educational research in residency programs. The review sought to explore the extent and quality of educational research in this context, as evaluated using the MMERSQI framework [13]. The research question was: What is the profile of publications on Chilean medical specialty residency programs over the last five years, in relation to the CNA accreditation criteria and the MMERSQI framework for educational research quality? This analysis is intended to provide insights into how recent research outputs align with evolving accreditation standards, thereby highlighting the importance of robust educational research in meeting accreditation requirements.”
Identifying relevant Studies
A librarian assisted the team in building the search strategy using Medical Subject Headings (MeSH) and various databases. After three dedicated meetings to refine the strategy based on the papers found and the research team’s suggestions, we aimed to control for terms that introduced excessive “noise.”
As inclusion criteria, we decided to include only articles related to the formative process of residents and medical specialty programs, with authors affiliated in Chile, from January 2019 to March 2024. There was no language filter. We searched SCOPUS, Web of Science (WOS), Scielo, because these databases are accepted as part of the productivity for accreditation in the field and PubMed because is specific in the field (Table 1). It is important to note that PROSPERO does not accept scoping reviews, literature reviews, or mapping reviews (statement extracted from the website: PROSPERO Registration).
Table 1.
Search strategy
| Search strategy | Data Base | N° of articles 2019–2024 |
|---|---|---|
| ( KEY ( “internship and residency” ) OR TITLE-ABS-KEY ( resident OR residents OR residency OR residencies OR “medical residency program” OR “Medical specialty” OR specialization ) AND AFFILCOUNTRY ( chile ) ) AND ( LIMIT-TO ( DOCTYPE, “ar” ) ) AND ( LIMIT-TO ( EXACTKEYWORD, “Humans” ) OR LIMIT-TO ( EXACTKEYWORD, “Human” ) ) | SCOPUS | 235 |
| ((“medical residency program*“[Title/Abstract] OR “resident“[Title/Abstract] OR “residents“[Title/Abstract] OR “residency“[Title/Abstract] OR “residencies“[Title/Abstract] OR “residence“[Title/Abstract] OR “medical specialty“[Title/Abstract] OR “medical specialties“[Title/Abstract] OR “specialization“[Title/Abstract] OR “internship and residency“[MeSH Terms]) AND 2019/01/01:3000/12/12[Date - Publication] AND “chile“[Affiliation] AND “journal article“[Publication Type] AND “humans“[MeSH Terms]) AND (2019:3000/12/12[pdat]) | Pubmed | 275 |
| (“medical residency program*” OR “resident” OR “residents” OR “residency” OR “residencies” OR “residence” OR “medical specialty” OR “medical specialties” OR “specialization” OR “internship and residency”) AND Chile | Wos | 1.145 |
| (“medical residency program*” OR “resident” OR “residents” OR “residency” OR “residencies” OR “residence” OR “medical specialty” OR “medical specialties” OR “specialization” OR “internship and residency”) AND Chile | Scielo | 108 |
| TOTAL | 1763 |
Selecting studies to be included in the review
Once we collected the citations from the search, we consolidated the 1763 reports using Excel. One researcher (SA) eliminated duplicates (457), resulting in a corpus of 1306 abstracts for the first revision. Two researchers (SA and KM) independently reviewed titles and abstracts in a sample of 275 articles (21% of the corpus) to assess concordance in selecting papers for inclusion. The agreement between these reviewers was 94.5%. The remaining 1085 abstracts were filtered by one researcher (SA). This process excluded 1254 articles unrelated to the study topic, leaving a final corpus of 52 articles for the analysis phase.
Charting the data
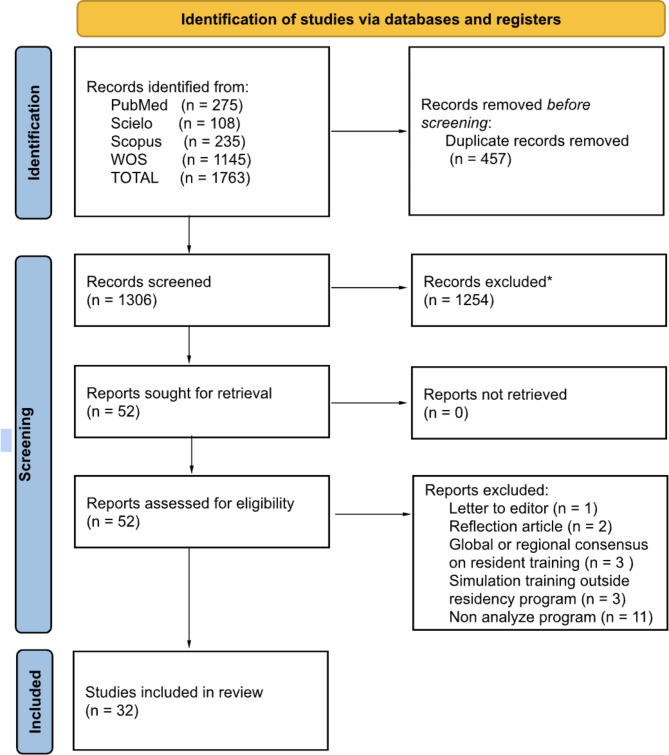
The team collaboratively developed the data extraction form, defining inclusion and exclusion criteria and the extraction system. The inclusion criteria encompassed articles related to the formative process of residents and medical specialty programs in Chile, from January 2019 to March 2024. The exclusion criteria included pilot testing of devices or simulators, regional or global consensus papers, reflections, editor letters, and articles assessing variables outside formative programs. The extraction categories included author, year, university of the program, program specialty, study population, elements of the formative process, instruments used for assessment, MMERSQI elements and score, main results, study limitations, and future directions. Two researchers (SA, KM) independently analyzed the 52 articles. Discrepancies were resolved by consensus between the two researchers (SA, KM), excluding 20 articles. Consequently, 32 articles were included in the final bibliometric and thematic analysis (Fig. 2).
Fig. 2.
Prisma flow. *All the records were excluded by a human because the term” resident” was related to a topic different form medical specialty programs (urban residents, CD4 residents, etc). We don’t use automation tools in the exclusion process
Collating, summarizing, and reporting the results
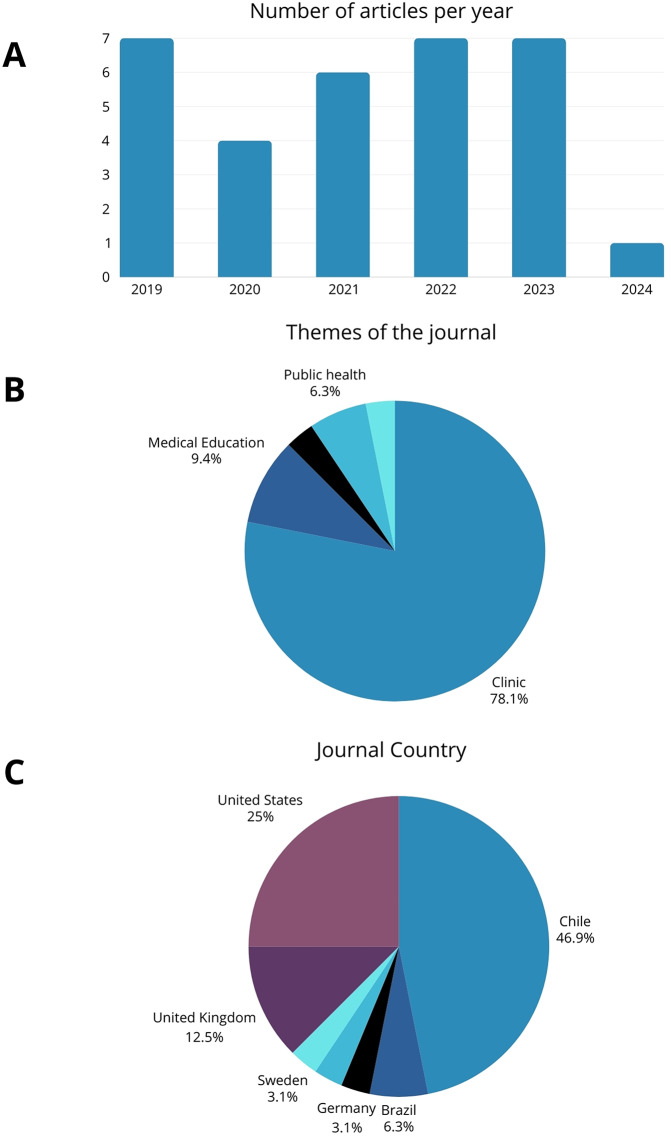
Between 2019 and 2023, an average of 6.2 articles were published yearly (Fig. 3.A). The bibliometric analysis revealed that the dominant thematic area of the journals was clinical, accounting for 78.1%. Additionally, three articles were published in specialized Medical Education journals and one in a Simulation journal (Fig. 3.B). The predominant language of the articles was English (59.38%), with 13 articles written in Spanish (40.62%). Most articles were retrieved from the Scopus database (84.85%), with two from Scielo and one each from WOS and PubMed (Fig. 3). Considering the group’s expertise, the sixth step of the review was performed by the senior researchers of the group (AD, XT, KM, SA).
Fig. 3.
Bibliometric synthesis of the articles included
Most articles focused on residents (84.38%), with only two articles including graduates as participants. One university accounted for 62.50% of the articles and participated in all multicenter studies (9.38%). Articles from other single institutions were produced by universities based in Concepción. Surgical specialties were the principal focus, with 15 research articles analyzing one program in that area. Psychiatry was the second primary specialty in productivity, with 5 articles representing 15.63% of the data analyzed (Table 2).
Table 2.
Descriptive information of the articles included in the final analysis
| Variables | Categories | n | % |
|---|---|---|---|
| Population | Residents | 27 | 84.38 |
| Teachers | 5 | 15.63 | |
| Graduates | 2 | 6.25 | |
| University | PUC | 20 | 62.50 |
| UChile | 5 | 15.63 | |
| Group of various chilean universities | 3 | 9.38 | |
| UdeC | 1 | 3.13 | |
| UCSC | 1 | 3.13 | |
| Type of Specialty | Primary | 29 | 90.63 |
| Secondary | 3 | 9.38 | |
| Medical Specialty Program | Multiple programs (surgery) | 6 | 18.75 |
| General surgery | 5 | 15.63 | |
| Psychiatry | 5 | 15.63 | |
| Orthopedics | 4 | 12.50 | |
| Internal Medicine | 3 | 9.38 | |
| Otorrinolaringology | 3 | 9.38 | |
| Anesthesiology | 2 | 6.25 | |
| Plastic Surgery | 2 | 6.25 | |
| Radiology | 2 | 6.25 | |
| Head and Neck Surgery | 1 | 3.13 | |
| Formative process assessed | Teaching-learning methodology | 18 | 56.25 |
| Learning assessment | 10 | 31.25 | |
| Training program evaluation | 4 | 12.50 | |
| Curricular design | 3 | 9.38 | |
| Student or faculty wellness | 2 | 6.25 | |
| Educational environment | 2 | 6.25 | |
| Admission process | 1 | 3.13 | |
| Graduation profile | 1 | 3.13 |
The appraisal of the methodological quality of the articles was conducted by estimating MMERSQI scores, which showed a mean of 51.19 ± 14.81 SD and ranged from 30 to 80 points. The seven articles with MMERSQI scores over 70 were published in WOS Q1 journals, in the fields of clinical and medical education, and originated from postgraduate programs at a single university (Table 4).
Teaching and learning methodologies within residency programs were the most frequent research focus during the five-year period analyzed, with 18 articles representing almost 60% of the total analyzed [19–36]. Nearly 80% (15/18) of the teaching and learning methodologies articles described simulation as an educational strategy or assessment tool [19–21, 24–32, 34–36].
For instance, using simulated patients to teach and assess communication and collaboration abilities in radiology residency programs within an emergency radiology OSCE provides valuable information that complements traditional cognitive and technical assessments [19]. Similarly, the use of simulated patients to teach psychopathology was highly acceptable among psychiatry residents, who appreciated the methodology [34].
High-fidelity simulation was employed to validate the Spanish version of the instrument Anesthetic Non-Technical Skills, which assesses crisis management abilities in anesthesiology residents and can be used to evaluate residents’ performance in both simulation and real clinical settings [30].
Nine articles in the simulation area were related to procedural simulation training, assessing residents’ technical skills through low-fidelity simulations or animal models. These articles focused on general surgery training in trauma [26–28], open intestinal anastomosis [36], anesthesiology residents’ training in central venous access [25] and percutaneous dilatational tracheostomy [29], otorhinolaryngology training in laryngeal microsurgery skills [35], orthopedic residents’ training in arthroscopic partial meniscectomy [24] and forefoot osteotomy skills [32], and head and neck surgery residents’ skills in performing total parotidectomy [31]. The most common research protocol design was pre-post intervention assessment, conducted in the context of deliberate practice programs with on-site or remote feedback provided by trained simulation instructors.
In the case of training on percutaneous dilatational tracheostomy [29], the research team used data mining principles to define critical steps in the procedural training to guide and improve the feedback process. Conversely, the group focusing on central venous access training compared the performance between novices and experts to enhance the training program design and provide better feedback [25].
All the learning assessments described were implemented in simulation settings, using validated instruments to assess non-technical skills [30] or specific instruments to assess procedural skills (20–21, 24, 25, 26, 27, 28, 29, 30, 31, 32, 34, 35, 36, 37), or OSCE to assess communication and collaboration [19].
During the pandemic, the implementation of online peer teaching in internal medicine residency as a complementary resource to the traditional curriculum was evaluated using Kirkpatrick Level 1, showing the highest scores in learning environment and the lowest scores in teaching methodology [38]. A national survey applied to orthopedics residents across the country to assess the use of online emergency education revealed that 86% of residents reported their programs began using online education, primarily as webinars, with low representation of clinical telematic practice or online assessments [39].
The group of articles related to curriculum design is diverse in focus. One study focused on the needs analysis process related to the introduction and use of complementary and alternative education in psychiatry residency [40]. Another study assessed the curriculum by analyzing the perceptions and experiences related to feedback from residents and graduates of the psychiatry specialty at one university [41]. A third study assessed the satisfaction of plastic surgery graduates with the program [42].
Regarding the incorporation of complementary and alternative medicine instruction in different Chilean psychiatry programs, teachers from three university programs believed that their students should know about sleep hygiene (93.9%), stress management (89.8%), and motivational interviewing (71.4%). In contrast, the least valued contents were traditional Chinese medicine, homeopathic medicine, and manual medicine (massage, reiki, chiropractic), all with 2% each, and hypnosis and anthroposophic medicine, which was not considered by any respondents [40].
The perceptions of seven generations of graduates from a plastic surgery program showed a high level of satisfaction with the training in general, especially in body contour surgery and breast aesthetic surgery. Nonetheless, 63% of respondents considered the program duration to be insufficient [42].
The design and validation of the IMPRINT-15 produced a bi-dimensional, valid, and reliable questionnaire to evaluate the perceived quality by residents of the IM clinical rotations. This included dimensions related to the qualifications of the teachers and supervisors, the quality of the performance assessment instruments and system, the organization of activities, including the balance of time to promote well-being, and the existence of social support for the residents [43].
When assessing the learning environment, first-year residents, graduates from non-traditional universities, and non-surgical specialties residents showed better scores in PHEEM (Postgraduate Hospital Educational Environment) and ACLEEM (Ambulatory Care Learning Educational Environment). Residents who graduated from non-Chilean universities reported lower scores on both scales compared to Chilean graduates. The individual factors associated with higher PHEEM scores were age and male gender. The most critical areas for improvement were feedback from professors, protected time in hospital rotations, workload, adequate evaluation, and timely feedback [44].
Another aspect of the learning environment was explored in otorhinolaryngology medical specialties, addressing the perception of gender bias before the pandemic. Female residents felt their surgical abilities were negatively perceived compared to male residents, and they experienced sexist expressions during rotations, although sexual harassment was not reported as significant [45].
An attempt was made to measure the psychological impact of the pandemic on residents using scales for symptoms of depression and anxiety, correlated with a resilience scale. Up to a quarter of residents in internal medicine, anesthesiology, and emergency medicine had severe symptoms of depression during the first year of the pandemic [46].
One study collected teachers’ perceptions related to wellbeing in psychiatry programs. It found that teachers who had a self-care program or activities considered their program adequate for burnout management, significantly more so than those without a self-care program (F = 5.48, p = 0.023 ANOVA) [40].
The financing of specialization programs to encourage the renewal of academics was addressed in a study that analyzed 20 years of a Clinical University Hospital financing these specialization programs and wanted to assess if the objective of renewing academics in different clinical departments was successful. Academic development was remarkable in some specialties with important teaching and investigation activities. But in most, it did not have the impact that they were expecting. Results indicated a modest impulse of faculty development within clinical residencies a lack of educational projects, and teaching publications. The study highlighted the need for significant changes to achieve the objective of training new academics to replace the current faculty [47].
Three studies focused on the research abilities of residents. The first study used a quantitative approach to evaluate the number of publications where plastic surgery residents were authors, considering that investigation promotes the development of critical thinking and professional capabilities, finding that their real involvement in publishing is low. At the same time, they did get the opportunity to attend conferences [48]. The second evaluated research opportunities and limitations for plastic surgery residents in various countries, emphasizing the importance of research fellowships, protected time, and mentoring to increase academic productivity [49]. The third used a qualitative approach to analyze the facilitators and barriers to conducting research, strategies for introducing research into the curriculum, and the profile of research-motivated residents [33].
Discussion
The main result of this review is the low number of research papers found during the period analyzed, from only four universities, representing 19% of the universities in the medical specialties postgraduate educational system [10]. Additionally, surgical training programs followed by psychiatry programs concentrate 62.5% of the productivity in the medical education field. Considering that the number of medical specialties under the new regulation is 365 [10], a reduced number of medical specialty programs has antecedents to achieve the new accreditation criteria in the highest standard [9]. There is a challenge to the institutions and programs to address this new regulation, avoiding the undesirable effect of the quality assessment process being perceived as strategically imposed tools [11] and transforming the new criteria into an opportunity to strengthen effective mechanisms for quality improvement [2].
Another important finding is that educational research was mainly focused on residents’ satisfaction, skills, or well-being, with scarce reports involving graduates as participants or graduate profile analysis. One element to assess the effectiveness of a training program is the analysis of graduate profiles [9]. This process requires the inclusion of the perspectives of residents, faculty, graduates, employers, and relevant stakeholders in the occupational field [50]. Considering that the pandemic has accelerated changes in health systems globally, evaluating the current relevance of graduate profiles is an important recommendation that should be addressed in the future [51].
Even though the number of papers was reduced, an important number were published in clinical journals. Some of the articles with the higher MMERSQI scores were published in international specialized and high-impact Medical Education [23, 29, 43] or Simulation journals [32], accomplishing the excellence criteria related to dissemination to the relevant disciplinary communities at the national or international level, understanding that the discipline in this case is teaching and learning [9].
One of the most researched categories was simulation-based education (SBE), which has established itself as an important methodology in training surgical Chilean residents. This reflects its growing importance in postgraduate medical education in recent years. However, skill measurements focus on immediate verification of achievement in specific training programs, with little evidence of transfer to patients. Measurements of this nature could be relevant and add to the body of evidence that exists globally on this topic [51–54]. Challenges such as resource allocation, the need for trained instructors, the creation of realistic simulations, the use of virtual simulation or other simulation resources, and the assessment of non-technical [30] and communicational skills [19] must be addressed in more programs.
The differences between residents in their perceptions of the educational environment assessed with PHEEM and ACLEEM suggest that some groups may have unique advantages or different expectations contributing to their positive perceptions [44]. The areas identified for improvement—feedback, protected time, workload, and evaluation quality—are a field to design and assess the impact of interventions oriented to specific or personalized resident support. These interventions could be integrated into solutions that cover the mental health of residents, particularly those in internal medicine, anesthesiology, and emergency medicine, who experienced severe symptoms of depression during pandemics [46]. This underscores the urgent need for robust mental health support systems within medical residency programs. The transition to online peer teaching and the increased use of webinars were generally well received, although these methods should complement rather than replace in-person interactions.
The perception of gender bias in surgical specialties, where female residents felt their skills were undervalued [45], points to ongoing issues of equity and inclusion. Addressing these biases is crucial for creating a supportive environment for all residents. Self-care programs positively influenced burnout management, underscoring the importance of incorporating well-being initiatives into residency curricula [40].
The diverse approaches to curriculum design, including the integration of complementary and alternative medicine [40], reflect the dynamic nature of medical education. Curriculum research should continue to adapt to Chile’s changing landscape of healthcare. Studies on residents’ research capabilities highlighted challenges and opportunities for fostering academic productivity [33, 48, 49]. Fellowships, protected time, and mentoring were key factors supporting research activities [33]. In contrast, funding residency programs for new specialists to reinforce the faculty in various activities, including research, did not have the expected effect, raising the question of whether this is an effective means of achieving excellence in the new research-linked accreditation criteria [47].
The findings of this study have several implications for policymakers and educational institutions. Policies that support the development of high-quality residency programs, comprehensive mental health services, and inclusive learning environments are essential. Accreditation processes should incorporate these elements to ensure standardized, high-quality training. Additionally, promoting faculty development and research opportunities within residency programs can enhance academic performance and professional growth. The concrete implications of strategies or solutions will probably demand institutional support, resources, and researchers in the medical education field.
This study has some limitations. First, it focuses on research on medical residency in Chile, which can be interpreted as a limitation to generalisability. Even if the experiences of a single country reflect a particular reality, policy change can be understood as generalized processes, considering that they can drive changes in education and that accreditations are part of the educational system in many countries. In that sense, analyses of particular realities can offer insights for other researchers, administrators, or institutions, because assessing the gap between what the graduate education system has today and what is required in the immediate future, could guide decision-making. Otherwise, this review could serve as a model of analysis for other countries considering implementing similar changes.
A second limitation is that the databases we included were limited to Scopus, WOS, Pubmed and Scielo, and even if those criteria are sustained in the productivity orientations for accreditation in Healthcare programs, it still excludes journals of lower impact that could include some research in the field.
Analyzing the impact and the quality of educational research in postgraduate programs could be valuable to anticipate the challenges of new policies designed to improve education quality. Institutions could consider this information to implement mechanisms, including increased allocation of resources to promote educational research, to contribute to improving processes and outcomes in postgraduate education. Considering that all over the world there are efforts to reduce disparities, ensure sustainability, and improve global educational systems, these promotion policies could encourage countries with low productivity in educational research and also drive further changes to improve postgraduate programs.
Future research should explore the longitudinal impacts of simulation-based learning, gender biases in different medical specialties, and the long-term effects of the COVID-19 pandemic on residents’ mental health. Additionally, studies should investigate the transition from residency to independent practice to address the gaps identified in this research. and institutional support.
Conclusion
Research on medical education within postgraduate residency training programs in Chile remains limited, with most publications concentrated in a few universities. Given the newly introduced accreditation criteria, relating to the importance of educational research, this lack of widespread research activity could impose challenges for many residency programs in meeting the higher standards of the accreditation. The knowledge of the unexplored areas and the synthesis of the success of other programs reporting their practices could provide insights to the institutions and programs, enhancing research productivity and broadening the scope of their educational research efforts to align more closely with institutional accreditation expectations. It is an opportunity for universities to incorporate this type of research into their development activities and to allocate resources for this purpose.
This review emphasizes the need for continuous evaluation and improvement of all residency programs to ensure training quality and provide public accountability through the accreditation process. Evaluating the effectiveness of training programs requires including perspectives from residents, faculty, graduates, employers, and stakeholders.
Some interesting and feasible areas for new research could be residents’ satisfaction, skills acquisition, the well-being of residents and educators, faculty development or residents as teachers, and graduate profile analysis, considering the new post-pandemic healthcare scenario.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors acknowledge the assisstance of Claudia Martinich, Reference Librarian for Clinical Fields at Universidad San Sebastián, Chile.
Author contributions
K.M. and S.A. developed the study ideas and formulated research goals. K.M., S.A., and X.T. designed the methodology and created models. S.A. handled programming, software development, implementation, and testing of code components. A.D. and P.R. verified the reproducibility of results and experiments. S.A and S.V applied statistical and computational techniques for data analysis. All authors contributed to performing experiments and data collection. R.C., S.V., and P.R. provided study materials, reagents, samples, and analysis tools. K.M., S.A., X.T., A.D., and C.A managed data annotation, cleaning, and maintenance. All authors were involved in drafting the initial manuscript and in critical review and revision. S.A. was responsible for data visualization. K.M. and S.A. oversaw research planning and execution, including mentoring and coordination.
Funding
There was no funding for this study.
Data availability
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bandiera G, Frank J, Scheele F, Karpinski J, Philibert I. Effective accreditation in postgraduate medical education: from process to outcomes and back. BMC Med Educ. 2020;20(S1). 10.1186/s12909-020-02123-3. [DOI] [PMC free article] [PubMed]
- 2.Frank JR, Taber S, van Zanten M, Scheele F, Blouin D, on behalf of the International Health Professions Accreditation Outcomes Consortium. The role of accreditation in 21st century health professions education: report of an International Consensus Group. BMC Med Educ. 2020;20(S1). 10.1186/s12909-020-02121-5. [DOI] [PMC free article] [PubMed]
- 3.World Health Organization. Transforming and scaling up health professionals’ education and training: World Health Organization guidelines. Geneva: WHO; 2013. [PubMed] [Google Scholar]
- 4.Fishbain D, Danon YL, Nissanholz-Gannot R. Accreditation systems for postgraduate medical education: a comparison of five countries. Adv Health Sci Educ. 2019;24(5):503–24. 10.1007/s10459-019-09880-x. [DOI] [PubMed] [Google Scholar]
- 5.Accreditation Council for Graduate Medical Education (ACGME). Common Program Requirements (Residency). Chicago: ACGME. 2023 [cited 2024 Jun 11]. https://www.acgme.org/about/policies-and-related-materials/
- 6.Gobierno de, Chile. Biblioteca Nacional de Chile. Ley 21091.2021. [cited 2024 Mar 25]. https://www.bcn.cl/leychile/navegar?idNorma=1118991
- 7.Comisión Nacional de Acreditación (CNA). Criterios y Estándares para la Acreditación de Universidades, Criterio 4. Santiago: CNA. 2020 [cited 2024 aug 25]. https://www.cnachile.cl/SiteAssets/Paginas/consulta_criterios_y_estandares/universidades.pdf
- 8.Comisión Nacional de Acreditación (CNA). Criterios y Estándares de Calidad para la Acreditación de Especialidades Médicas y Odontológicas, Criterio 2. Santiago: CNA; 2020 [cited 2024 abr 16]. https://www.cnachile.cl/noticias/SiteAssets/Paginas/Forms/AllItems/CyE%20ESPECIALIDADES%20M%C3%89DICAS%20y%20ODONTOL%C3%93GICAS%20%282%29%20%282%29.pdf
- 9.Comisión Nacional de Acreditación (CNA). Orientación de productividad Comité de área Especialidades Médica. Santiago: CNA; 2018 [cited 2024 aug 25]. https://www.cnachile.cl/SiteAssets/Paginas/Acreditacion-Postgrado/Orientaci%C3%B3n%20de%20productividad%20-%20Esp%20M%C3%A9dicas%20-%2009-03-2018.pdf
- 10.Ministerio de Educación (Mineduc). Bases de datos de la oferta académica en el sistema de educación superior en Chile. Servicio de Información de Educación Superior. Santiago: Mineduc; [n.d.] [cited 2024 May 16]. https://www.mifuturo.cl/bases-de-datos-de-oferta-academica
- 11.Kooli C. Governing and managing higher education institutions: the quality audit contributions. Eval Program Plann. 2019;77:101713. 10.1016/j.evalprogplan.2019.101713. [DOI] [PubMed] [Google Scholar]
- 12.Mak S, Thomas A. Steps for conducting a scoping review. J Grad Med Educ. 2022;14(5):565–7. 10.4300/JGME-D-22-00621.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al Asmri M, Haque MS, Parle JA, Modified Medical Education Research Study Quality. Instrument (MMERSQI) developed by Delphi consensus. BMC Med Educ. 2023;23(1):63. 10.1186/s12909-023-04033-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Page MJ, McKenzie JE, Bossuyt PM, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n. 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Falagas ME, Pitsouni EI, Malietzis GA, Pappas G. Comparison of PubMed, Scopus, Web of Science, and Google Scholar: strengths and weaknesses. FASEB J. 2008;22(2):338–342. http://www.ncbi.nlm.nih.gov/pubmed/17884971 [DOI] [PubMed]
- 16.Powell KR, Peterson SR. Coverage and quality: A comparison of Web of Science and Scopus databases for reporting faculty nursing publication metrics. Nurs Outlook. 2017. http://www.ncbi.nlm.nih.gov/pubmed/28377037 [DOI] [PubMed]
- 17.Van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84(2):523–538. http://www.ncbi.nlm.nih.gov/pubmed/20585380 [DOI] [PMC free article] [PubMed]
- 18.Kirby A. Exploratory bibliometrics: using VOSviewer as a preliminary Research Tool. Publications. 2023;11(1):10. 10.3390/pub11010010. [Google Scholar]
- 19.Garrido CF, Triviño BX, Henríquez LH, Cikutovic MP, Arau UR, Huete GA. Evaluación de habilidades transversales de comunicación y colaboración a través de un examen clínico objetivo estructurado de radiología de urgencias para residentes de un programa universitario de especialidad en radiología. Rev Chil Radiol. 2019 Mar [citado 2024 Jun 01];25(1):35–41. 10.4067/S0717-93082019000100035
- 20.Lira R, Salas-Morales J, Leiva L, de la Fuente R, Fuentes R, Delfino A, Nazal CH, Sepúlveda M, Arias M, Herskovic V, et al. Process-oriented feedback through process mining for surgical procedures in medical training: the ultrasound-guided central venous catheter placement case. Int J Environ Res Public Health. 2019;16(11):1877. 10.3390/ijerph16111877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tejos, Tejos R, Avila R, Inzunza M, Achurra P, Castillo R, Rosberg A, Cordero O, Kusanovich R, Bellolio F, Martínez J. Impact of a simulated laparoscopic training program in a three-year general surgery residency. ABCD Arq Bras Cir Dig. 2019;32(1). 10.1590/0102-672020190001e1436 [DOI] [PMC free article] [PubMed]
- 22.Alvarez ML, Lagos AE, Sepúlveda V, Napolitano C, González C. Otolaryngology residency strategies during the COVID-19 pandemic. Clin Teach. 2020;17(5):544–6. 10.1111/tct.13236. Disponible en:. [DOI] [PubMed] [Google Scholar]
- 23.Álvarez ML, Waissbluth S, González C, Napolitano C, Torrente M, Délano PH, et al. How the COVID-19 pandemic affects specialty training: an analysis of a nationwide survey among otolaryngology residents in Chile. Medwave. 2021;21(01):e8097–8097. 10.5867/medwave.2021.01.8097. Disponible en:. [DOI] [PubMed] [Google Scholar]
- 24.Ledermann G, Rodrigo A, Besa P, Irarrázaval S. Orthopaedic residents’ transfer of knee arthroscopic abilities from the simulator to the operating room. J Am Acad Orthop Surg. 2020;28(5):194–9. 10.5435/JAAOS-D-19-00245. [DOI] [PubMed] [Google Scholar]
- 25.Villagrán I, Moënne-Loccoz C, Aguilera V, García V, Reyes JT, Rodríguez S, et al. Biomechanical analysis of expert anesthesiologists and novice residents performing a simulated central venous access procedure. PLoS ONE. 2021;16(4). 10.1371/journal.pone.0250941. [DOI] [PMC free article] [PubMed]
- 26.Ortiz C, Vela J, Contreras C, Ávila R, Inzunza M, Quezada J et al. Achievement of effective cardiopulmonary trauma surgical skills training throughout the incorporation of a low-cost and easy to implement pulsatile simulation model. Injury. 2021;52(5):1215–20. 10.1016/j.injury.2020.12.004 [DOI] [PubMed]
- 27.Ortiz C, Belmar F, Rebolledo R, Vela J, Contreras C, Inzunza M et al. Validity argument for a simulation-based objective structured clinical examination scenario for evaluation of surgical skills in trauma. J Surg Res. 2021;268:507–13. 10.1016/j.jss.2021.06.069 [DOI] [PubMed]
- 28.Ortiz C, Vela J, Contreras C, Belmar F, Paul I, Zinco A et al. A new approach for the acquisition of trauma surgical skills: an OSCE type of simulation training program. Surg Endosc. 2022;36(11):8441–50. 10.1007/s00464-022-09098-w [DOI] [PMC free article] [PubMed]
- 29.Martínez JJ, Galvez-Yanjari V, de la Fuente R, Kychenthal C, Kattan E, Bravo S et al. Process-oriented metrics to provide feedback and assess the performance of students who are learning surgical procedures: The percutaneous dilatational tracheostomy case. Med Teach. 2022;44(11):1244–52. 10.1080/0142159x.2022.2073209 [DOI] [PubMed]
- 30.Delfino AE, Fuentes-López EA, de la Fuente RF, Altermatt FR. Cross-cultural adaptation and validation of the Spanish version of the Anesthetists’ Non-Technical Skills (ANTS) assessment tool. J Clin Anesth. 2023;84(111008):111008. 10.1016/j.jclinane.2022.111008 [DOI] [PubMed]
- 31.Jara Contreras R, Rappoport WD, Moraga TF, Soto MV, Aguilar NW. Programa de entrenamiento de parotidectomia en modelo cadavérico perfundido. Rev Cirugia. 2023;75(4). 10.35687/s2452-454920230041753
- 32.Ledermann G, Kuroiwa A, González N, Silva I, Villa A. Training program for orthopedic residents in forefoot osteotomy skills: Transference from a simulator to a cadaveric surgical scenario. Simul Healthc. 2023;18(3):181–6. 10.1097/sih.0000000000000678 [DOI] [PubMed]
- 33.Merino T, Rojas V, Fuentes-López E, Sánchez C, Pizarro M, Fuentes-Cimma J et al. Barriers for research activities in residency programs: A mix-methods study. Medwave. 2023;23(1):e2627. 10.5867/medwave.2023.01.2627 [DOI] [PubMed]
- 34.Salvo GL, Arrau GR. Implementación de docencia de postgrado y pregrado presencial y remota con pacientes simulados en psiquiatría. Rev Med Chil. 2023;151(1):113–9. 10.4067/s0034-98872023000100113 [DOI] [PubMed]
- 35.Santander MJ, Sepúlveda V, Iribarren J, Rosenbaum A, Albrich D, Varas J et al. Development and validation of a laryngeal microsurgery simulation training system for otolaryngology residents. Otolaryngol Head Neck Surg. 2023;169(4):971–87. 10.1002/ohn.376 [DOI] [PubMed]
- 36.Cruz Mackenna E, Morales Palma ÁJ, González Arestizábal T, Valenzuela Silva DJ, Csendes Juhasz A. Percepción e impacto en la confianza de los residentes de cirugía general de un curso de anastomosis intestinal abierta en un ambiente simulado. Rev Cir. 2024;76(1). 10.35687/s2452-454920240011913
- 37.Vela J, Cárcamo L, Contreras C, Arenas C, Ramos JP, Rebolledo R, Varas J, Martínez J, Jarufe N, Achurra P. Self-confidence on acquired surgical skills to deal with severe trauma patients in recently graduated surgeons. Arq Bras Cir Dig. 2021;34(1):e1561. 10.1590/0102-672020210001e1561. PMID: 34008705; PMCID: PMC8121062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ramírez Carreño A, Carrillo Hurtado F, Uribe Sanzana G. Formación entre pares. Experiencia digital sincrónica en tiempos de pandemia. Rev Med Chil. 2022;150(8):1060–2. 10.4067/s0034-98872022000801060 [DOI] [PubMed]
- 39.Figueroa F, Figueroa D, Calvo-Mena R, Narvaez F, Medina N, Prieto J. Orthopedic surgery residents’ perception of online education in their programs during the COVID-19 pandemic: should it be maintained after the crisis? Acta Orthop. 2020;91(5):543–6. 10.1080/17453674.2020.1776461 [DOI] [PMC free article] [PubMed]
- 40.Pacheco B, Fritzsche M, Bedregal P. Medicina integrativa en la enseñanza de la Psiquiatría: actitudes y conocimientos respecto a la medicina complementaria y alternativa en docentes de programas de la especialidad. Rev Med Chil. 2022;150(1):107–14. 10.4067/s0034-98872022000100107 [DOI] [PubMed]
- 41.Rubí González PS, De la Barra Vivallos L, Schaefer H, Vergara-Barra P. The role of feedback in training psychiatrists. J Ment Health Train Educ Pract. 2019;14(4):242–50. 10.1108/jmhtep-02-2019-0009
- 42.Sepúlveda PS, Quispe VD, Selman BL, Larraín CE, Danilla ES, Erazo CC et al. Análisis del programa de formación de Cirugía Plástica y Reparadora de la Universidad de Chile: encuesta a egresados 2011–2017. Rev cir. 2019;71(3):203–9. 10.4067/s2452-45492019000300203
- 43.Díaz LA, Sepúlveda P, Abbott E, Fuentes-López E, Letelier LM, Riquelme A, et al. Residents get no… satisfactiona problem to face during internal medicine rotations: development and psychometric properties of the IMPRINT-15. Postgrad Med J. 2019;95(1120):96–101.Available from: http://dx.doi.org/10.1136/postgradmedj-2018-136187. [DOI] [PubMed]
- 44.González C, Ahtamon A, Brokering W, Budge MC, Cadagan MJ, Jofre P et al. Percepción del ambiente educacional de postgrado en residentes de especialidades médicas de universidades chilenas. Rev Med Chil. 2022;150(3):381–90. 10.4067/s0034-98872022000300381 [DOI] [PubMed]
- 45.Chuang C, Ángela RL, Lara AP, Ximena, Pineda D, Rodrigo, Nicolás N, Andrés, Pereira P, Carla. ¿Igualdad de género en otorrinolaringología? Rev. Otorrinolaringol. Cir. Cabeza Cuello. 2019 Dic [citado 2024 Jun 07];79(4):387–394. http://www.scielo.cl/scielo.php?script=sci_arttext&pid=S0718-48162019000400387&lng=es. 10.4067/S0718-48162019000400387
- 46.Ponce CE, Maureira Moreno V, Aranda GF, Bracchiglione J, Varas C. Impacto en la salud mental en residentes de tres programas de especialización médica de la Universidad de Valparaíso durante la pandemia por COVID-19. Rev Med Chil. 2022;150(9):1239–47. 10.4067/s0034-98872022000901239 [DOI] [PubMed]
- 47.Miranda VC, Rojas C. MG. Becas para la formación de médicos especialistas académicos del Hospital Clínico de la Universidad de Chile. Rev Med Chil. 2022;150(11):1477–83. 10.4067/s0034-98872022001101477 [DOI] [PubMed]
- 48.Navia T, Alfonso YáñezC, Gonzalo, González B, José Tomás LópezO, Aldo CC, Álvaro, Dagnino U, Bruno et al. Participación de residentes de cirugía plástica de Chile en la publicación científica: Revisión de los últimos 20 años. Rev. cir. 2020 Dic [citado 2024 Jun 07];72(6):551–558. http://www.scielo.cl/scielo.php?script=sci_arttext&pid=S2452-45492020000600551&lng=es. 10.35687/s2452-45492020006595
- 49.Navia A, Berner JE, Ramirez J, Will P, Tejos R, Dagnino B et al. Evaluation of research opportunities and limitations for plastic surgery residents: An international survey. Ann Plast Surg. 2021;87(5):488–92. 10.1097/sap.0000000000002839 [DOI] [PubMed]
- 50.Centro Interuniversitario de Desarrollo (CINDA). (2017). Evaluación del logro de perfiles de egreso: Experiencias universitarias. Copygraph. Retrieved from https://cinda.cl/wp-content/uploads/2017/07/evaluacion-del-logro-de-perfiles-de-egreso-experiencias-universitarias.pdf
- 51.Frenk J, Chen LC, Chandran L, Groff EOH, King R, Meleis A, Fineberg HV. Challenges and opportunities for educating health professionals after the COVID-19 pandemic. Lancet. 2022;400(10362):1539–56. 10.1016/S0140-6736(22)02092-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zendejas B, Cook DA, Bingener J, Huebner M, Dunn WF, Sarr MG, Farley DR. Simulation-based mastery learning improves patient outcomes in laparoscopic inguinal hernia repair. Ann Surg. 2011;254(3):502–11. 10.1097/SLA.0b013e31822c6994. [DOI] [PubMed] [Google Scholar]
- 53.Gallagher AG, Seymour NE, Jordan-Black JA, Bunting BP, McGlade K, Satava RM. Prospective, randomized assessment of transfer of training (ToT) and transfer effectiveness ratio (TER) of virtual reality simulation training for laparoscopic skill acquisition. Ann Surg. 2013;257(6):1025–31. 10.1097/SLA.0b013e318284f658. [DOI] [PubMed] [Google Scholar]
- 54.Schwab B, Teitelbaum EN, Barsuk JH, Soper NJ, Hungness ES. Single-stage laparoscopic management of choledocholithiasis: an analysis after implementation of a mastery learning resident curriculum. Surgery. 2018;163(3):503–8. 10.1016/j.surg.2017.10.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analysed during this study are included in this published article [and its supplementary information files].